Abstract
Asian Americans are the fastest growing U.S. immigrant group, projected to become the largest immigrant group by 2065, but the quantity of research on Asian Americans’ health has not mirrored changing demographics. Asian Americans have been understudied for more than 25 years, with only 0.17% of NIH expenditures allocated to projects including Asian American, Native Hawaiian, and Pacific Islander populations (Ðoàn et al., 2019). This disproportionality may result in part from the model minority stereotype (MMS) being extended to health, perpetuating the idea that Asian Americans are well-positioned with regard to health status and therefore associated research is not essential. Accordingly, the aims for this manuscript are threefold: a) bring attention to the inadequate representation of the Asian American population in health-related science, b) question the MMS in health, c) outline potential pathways through which the MMS limits what is knowable on Asian American health issues and needs. We discuss the limited meaningfulness of non-representative aggregated statistics purporting the model minority image and provide counterexamples. We also present a stereotype-constraints model with the MMS contributing to a bottleneck for Asian American health-related knowledge, accompanied by present-day circumstances (e.g., sparse data, few psychologists/ behavioral medicine scientists focused on Asian American health). We conclude with initial recommendations for addressing MMS-associated constraints in psychology and more broadly.
Keywords: Asian, model minority, health, cancer, understudied populations, stereotype
Asian Americans are the fastest growing immigrant group in the U.S. and are projected to become the largest immigrant group by 2065, outnumbering Hispanic/Latinx Americans (Lopez et al., 2017). Yet, support for research on Asian Americans’ health has not mirrored changing demographics. Asian Americans, Native Hawaiians, and Pacific Islanders1 (AANHPIs) were 6% of the U.S. population in 2018 (Chen, 2019), but only 0.2% of the 2018 NIH clinical research budget was allocated to AANHPI-specific projects (Ðoàn et al., 2019). In fact, underrepresentation of AANHPIs has persisted for more than 25 years, with an average of 0.17% of NIH expenditures involving, but not necessarily focusing on, AANHPI populations (Chen, 2019). One reason for the disproportionality in funding and research may be that, as several scholars have suggested (e.g., Chen & Hawks, 1995; Ibaraki et al., 2014), the longstanding model minority stereotype (MMS) has been applied to Asian Americans’ health.
The MMS arose following two media articles in 1966: New York Times Magazine’s “Success Story, Japanese-American Style” (Petersen, 1966) and the U.S. News and World Report’s “Success Story of One Minority in U.S.” about Chinese Americans. Promoted as self-sufficient and successful despite holding a minority status, Asian Americans were pitted against other racial minorities in part to uphold structural inequalities amid the civil rights movement (Kawai, 2005). The MMS represented a marked change from the previously negative stereotypes (e.g., “yellow peril” (Hurh & Kim, 1989)) applied pan-ethnically before, during, and after World War II to enact anti-Asian immigration policies and colonization of Asian/Pacific Islander (A/PI) countries (Kawai, 2005).
Following the creation of the MMS, one adverse consequence has been a perpetuation of the MMS in mental and physical health—that Asian Americans are well-off and not in need of scientific or clinical attention. Because others have described the MMS’ influence upon Asian Americans’ mental health (e.g., Cokley et al., 2013; Kiang et al., 2017; Lee et al., 2009; Sue et al., 1995), this manuscript primarily examines the MMS in relation to Asian Americans’ physical health and the ways psychology can help narrow the knowledge gaps. Understanding contributors to Asian Americans’ health2 is relevant for all areas of psychology; preventing or managing chronic disease and promoting physical health in Asian Americans is within the jurisdiction of psychological science (McDonald, O’Connell, & Suls, 2015) and practice, as biopsychosocial factors collectively determine physical health over the life course (Adler, 2009). However, very little research on Asian Americans’ physical health is available, and the MMS needs to be overcome to advance all Asian Americans’ health.
Are(n’t) Asian Americans a Model Minority in Health?
A first step to dismantle the MMS is to consider whether data meaningfully support the contention that Asian Americans are a model minority in health. The model minority image of Asian Americans can be prompted via cursory understanding of aggregated Asian data. To present examples of how this might occur, the following statements are purposefully presented to reflect lay discourse surrounding Asian Americans’ health as a “model minority”: a) Asian American adults are “less likely than all U.S. adults to be [self-reporting] fair or poor health” (p. 1; Bloom & Black, 2016); b) Compared to other racial/ethnic groups, Asian Americans have the lowest rates of hypertension and the lowest mortality rate from heart disease (National Center for Health Statistics, 2019); c) Cancer burden, measured in age-standardized disability-adjusted life years, is lowest for Asian Americans for all cancers combined (Lortet-Tieulent et al., 2016).
These types of statements make it seem that Asian Americans are indeed a model minority on indicators of health. Arriving at such conclusions is not particularly meaningful for a multitude of reasons, however. Of major importance, despite the evidence that more than a third of U.S. Asians have limited English proficiency (LEP), surveys typically are not provided in Asian languages and suffer from sampling bias (Islam et al., 2010). When sampling is more inclusive, disparities are evident. For example, Chinese immigrant cancer survivors have a higher mortality rate than U.S.-born Chinese cancer survivors (Gomez et al., 2010).
Asians are also one of the most diverse groups in the U.S., with widely varying backgrounds (e.g., immigration histories) across more than 37 ethnocultural groups (Kagawa-Singer et al., 2010). U.S. Asians also experience the largest within-group wealth gap, in which the lowest income strata show the least growth from 1970-2016, compared to other racial/ethnic groups (Kochhar & Cilluffo, 2018). In that variations in historical and SES-related factors are relevant for health disparities (Adler, 2009; Myers, 2009), deriving “model minority” conclusions about Asian Americans’ health holds little substantive meaning.
Asian Americans Are Not a Model Minority: Within-group Data Tell a Story of Disparities
Within-group examination of aggregated data seemingly supporting the MMS provides evidence that the MMS is inaccurate. Revisiting the earlier example statements on health perceptions, heart disease, and cancer burden provides proof-of-concept. First, although U.S. Asians are less likely overall (10.4%) than all others (12.4%) to report fair/poor health, a significantly higher proportion of Vietnamese adults (16.8%) report fair/poor health than do non-Hispanic White adults (NHWs) (Bloom & Black, 2016), and LEP Vietnamese adults are even more likely to report fair/poor health after adjusting for SES, nativity, and language proficiency (Kandula et al., 2007). Second, despite having the lowest rates of hypertension and heart disease mortality as an aggregated group, many Asians have greater proportionate mortality3 from hypertension than NHW counterparts (i.e., Chinese women=1.69, Filipino women=1.50, Asian Indian women=1.46, Korean women=1.30, Japanese women=1.23, Chinese men=1.27, Filipino men=1.38, Asian Indian men=1.18; Jose et al., 2014). Asian Indian men and women and Filipino men also are more likely than NHWs to die from ischemic heart disease (Jose et al., 2014); Asian Indian men and Vietnamese men have the highest premature mortality due to ischemic heart disease (Iyer et al., 2019). Third, although cancer burden is lowest for Asian Americans for all cancers combined, Asian Americans have higher cancer burden compared to NHWs for specific cancers (i.e., stomach and liver for both men and women; gallbladder for men; cervical and non-Hodgkin lymphoma for women; Lortet-Tieulent et al., 2016).
Casting East Asians as a Model Minority Is Misleading
An acontextual ascription of the MMS to the typically light-skinned East Asians4, presumed to have higher status in the U.S. (Kuo et al., 2020), is also a misstep. East Asians in the U.S. are diverse across many health-related demographics (e.g., region, SES). For example, Koreans in Los Angeles have the lowest median net financial worth among the largest Asian groups, with lower net worth compared to Latinos (~$20,000 gap) and African Blacks (>$45,000 gap) (De La Cruz-Viesca et al., 2016). Moreover, many East Asians with LEP (~1/3; Pew Research Center, 2013) are not adequately represented in health-relevant studies.
Counterevidence for East Asians as a model minority in health is particularly evident in cancer control science5. Cancer has been the leading cause of mortality in Asian Americans since the 2000s6 (Chen et al., 2018). Below we present non-exhaustive examples across the cancer control continuum suggesting that it is erroneous to apply the MMS to Asians, including East Asians, given their vulnerabilities in cancer risk, preventive behaviors, and cancer-related outcomes. Often, data show greater disparities for the LEP, foreign-born, less U.S.-acculturated.
Example 1: Living Environments Associated with Cancer Risk
Asian Americans are at greater risk for exposure to environmental health hazards than NHWs (e.g., Houston et al., 2014; Payne-Sturges & Gee, 2006). Notably, Chinese and Korean populations in the U.S. have higher cancer incidence due to carcinogenic air pollutants than do Black, Hispanic, NHW and American Indian groups (Grineski et al., 2017), and neighborhoods with higher (versus lower) proportions of non-English speaking Asians have greater cancer risk from air pollutants (Grineski et al., 2017). In California, Korean and Japanese women have greater exposure to mammary gland carcinogens than NHW women (Quach et al., 2014).
Example 2: Human Papillomavirus (HPV) Vaccination
HPV vaccination is an effective method of preventing cervical cancer in women. However, compared to other foreign-born women of color, foreign-born Asian women have the lowest adjusted odds of HPV vaccine initiation compared to U.S.-born NHWs (OR=0.26; Agénor et al., 2018). This disparity is of special concern for East Asians because >76% of Chinese and Koreans in the U.S. are foreign-born (Pew Research Center, 2013). Also, compared to all U.S. women (88%; Marlow et al., 2013), Korean women in California have the lowest HPV awareness (41%) followed by Vietnamese (48%) and Chinese (49%) women (Becerra et al., 2020). Asian American women with LEP have even lower HPV awareness (17%) (Becerra et al., 2020). In that HPV awareness is one of the best predictors of HPV vaccination (Bastani et al., 2011), LEP East Asian foreign-born women may be at increased risk for cervical cancer.
Example 3: Breast Cancer Incidence, Mortality, and Mammography Use
A/PIs in the U.S. evidenced the highest increase in breast cancer incidence relative to other racial/ethnic groups between 2012-2016 (DeSantis et al., 2019), a pattern also observed for younger Koreans and Southeast Asians in California (Gomez et al., 2017). Breast cancer-specific mortality is greater for foreign-born Chinese, Filipina, South Asian (Asian Indian, Pakistani, Sri Lankan, or Bangladeshi), Korean, and Vietnamese women than U.S.-born Japanese women (Gomez et al., 2010). Mammography can be important for preventing cancer-specific mortality (Gomez et al., 2019) but, compared to NHWs, Asians are the only racial/ethnic group less likely to have received a mammogram, statistically controlling for breast cancer risk factors, SES, and health care resources (Elewonibi et al., 2018). Asians also had the lowest rate of up-to-date mammography in 2018, compared to other racial/ethnic groups (American Cancer Society, 2019). In California, Korean and South Asian women have the lowest mammography use among the largest Asian groups (Chawla et al., 2015; Gomez et al., 2017).
Example 4: Quality of Life in Cancer Survivorship
Aggregate data on health-related quality of life (QOL) in cancer survivorship may show that A/PIs, in general, report similar levels of QOL as NHWs (e.g., Luckett et al., 2011). However, accruing research suggests that some Asians fare relatively poorly. Chinese and Vietnamese immigrant breast cancer survivors report lower QOL (e.g., physical and emotional well-being) compared to NHW and Japanese American women (Kagawa-Singer et al., 2017). Other MMS counter examples for East Asians include findings that Chinese immigrant breast cancer survivors: have significantly lower QOL compared with NHW norms7 (Lu et al., 2018); have a higher rate of sleep disturbance compared to NHWs (Gonzalez & Lu, 2018); are less likely to have physical health-related distress resolved than NHWs (Wang et al., 2012); and, among less acculturated survivors, have worse physical functioning than NHWs (Wang et al., 2019). Chinese and Vietnamese breast cancer survivors with LEP also report lower QOL and greater symptom distress (J. K. Yi et al., 2011). Research with Chinese immigrant breast cancer survivors hint at reasons for potential disparities: women mentioned feeling stigmatized because of their cancer diagnosis, kept it a secret from family, co-workers, and friends, and labeled themselves as tainted, undesirable, or handicapped (Lu et al., 2014; Warmoth et al., 2017).
Summary
A broad-strokes conclusion of Asian Americans’ health advantage is erroneous. The “model minority” conclusion becomes even more problematic when limitations of existing studies are considered, including non-representativeness of adults of low SES or with LEP; racial/ethnic comparisons made without appropriate adjustments (e.g., lower BMI thresholds for some subgroups (Fang et al., 2019)); and prevalence measured by self-reported diagnoses (National Center for Health Statistics, 2019). When health-related disparities are interrogated, the inaccuracy of the MMS with regard to Asian American health merits acknowledgment.
The MMS Constrains Understanding of Asian American Health Issues and Needs
If the MMS is not supported by evidence, why is it that the health of Asian Americans remains under-examined? Among the many possible reasons, the pervasiveness of the MMS (Wong et al., 1998) since the 1960s may be part of the explanation. With infinite information to process in the social world, people naturally use strategies to be cognitively efficient (Allport, 1954) and the automatic application of stereotypes (Bargh, 1984; Devine, 1989) can stem from both implicit bias and explicit attitudes within one’s awareness (Dovidio & Gaertner, 2010).
Americans, including Asian Americans, may perceive and expect U.S. Asians to be a model minority, in addition to perceiving that the MMS is a shared reality (Chao et al., 2013). The MMS might persist in part because people better store and emphasize information matching a presumably shared stereotype than stereotype-inconsistent information (Kashima, 2000). As such, we propose that the MMS is an invisible cultural force (Gone, 2011) shaping socioecological systems over time (Bronfenbrenner, 1977; Johnson et al., 1995). What results is a bottlenecked understanding of Asian Americans’ health (Figure 1). We present a stereotype-constraints model, in which constraints upon advancing the science of Asian Americans’ health occur at multiple levels (funding/policies, research/healthcare, public). We also postulate that the MMS is reified by present-day circumstances of sparse, non-representative data on Asian Americans’ health, and a paucity of psychological scientists who study Asian Americans’ health (Figure 1). We are not suggesting that the lack of relevant science stems solely from the MMS, but that the MMS potentially acts as one key contributor.
Figure 1.
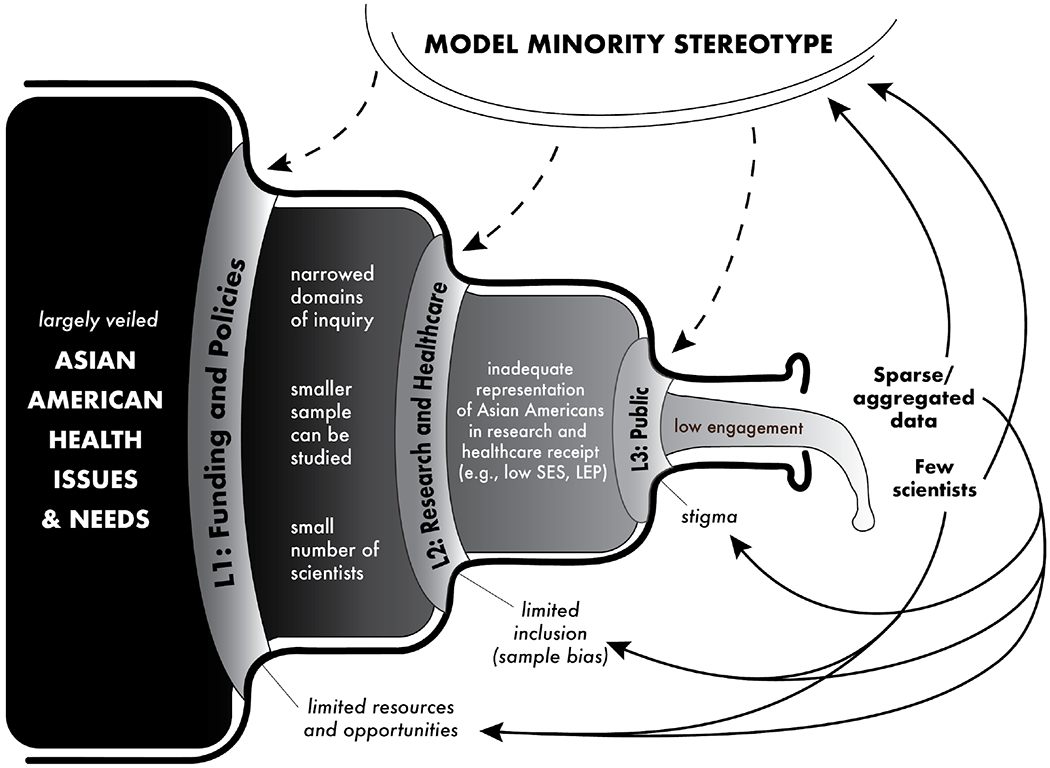
Stereotype-Constraints Model: Flow of Knowledge for Asian American Health Bottlenecked by the Model Minority Stereotype
Note. SES = socioeconomic status, LEP = limited English proficiency
Level One: Funding and Policies
Following the advent of the MMS, misunderstanding of limited, extant, A/PI health data (e.g., the Heckler Report (Heckler, 1985)) has contributed to the notion that most or all Asian Americans are better positioned in health than are other racial/ethnic groups. Such perceptions can contribute to a low preference for Asian Americans benefiting from redistributive funding/policies (Chao et al., 2010). Additionally, funding/policy decisions can be made under suboptimal and time-pressured conditions, perhaps allowing greater room for using heuristics and implicit stereotypes (Chugh, 2004) that “model minority” Asians may not need increased funding or inclusive policies. Although direct evidence of the MMS in funding and policy decision making is absent at present, the disproportionately low allocation of funds to improve Asian American health suggests the effects of the MMS.
Akin to the neglect of Asian Americans in U.S. mental health policy (Nagayama Hall & Yee, 2012), Asian Americans have been overlooked in health-related funding and policies that would foster the understanding of Asian American health issues. In 2012, large charitable foundation support of a range of services (e.g., arts, education, health) for A/PIs (4%) was lowest compared to support of services for Black (22%), Hispanic/Latino (18%), and Native American (6%) populations (Foundation Center, 2012). Only 0.2% of NIH expenditures from 1992-2018 were for research including A/PIs, with just 10.8% of those 529 awards (i.e., 0.005% of NIH expenditures) being A/PI population-centered training awards (Ðoàn et al., 2019) essential for retaining researchers as independent investigators (Nikaj & Lund, 2019). Asian Americans also were not a focus in the 2010 NIH Centers for Population Health and Health Disparities program funding designated to promote health equity by “[building] research teams that are transdisciplinary” and “training a new generation of health disparities researchers” in cancer and cardiovascular disease (p. S395; Golden et al., 2015). The communities served by the 10 funded centers were: African American (four grants), Hispanic/Latino (three grants), rural (two grants), and American Indian/Alaska Native (one grant) (Golden et al., 2015). Such funding trends constrain the growth of the scientific community investigating Asian American health and restrict the efforts needed to characterize the scope of Asian American health issues.
Similarly, health science-related policies within the context of the MMS may contribute to additional constraints. Although Asian American health research need not be led entirely by Asian American researchers, the majority foreign-born, LEP, and ethnoculturally diverse Asian American subpopulations would benefit from research incorporating an understanding of cultural values maintained across generations (LaFromboise et al., 1993). Moreover, conducting culturally appropriate research often requires deep pre-existing knowledge (Kreuter & Haughton, 2006) of the underlying cultural structures (Resnicow et al., 1999). Researchers of Asian descent with both cultural knowledge and language fluency offer strengths in conducting research with understudied Asian communities, but policies have not encouraged their training. For example, Asian American researchers are the only racial minority group explicitly excluded from eligibility for diversity-related NIH funding. Only recently, a clause added that researchers from other racial/ethnic groups should participate if they can “[demonstrate] convincingly to be underrepresented by the grantee institution” (Department of Health and Human Services, 2018). In response to policy that did not clarify the eligibility for underrepresented Asians until 2018, Asian researchers interested in Asian American health may not have pursued such funding (Ðoàn et al., 2019). Furthermore, diversity initiatives for mentorship at universities largely have overlooked Asian Americans, perhaps in part due to the MMS, despite evidence that greater support is warranted (Chin & Kameoka, 2019).
In summary, the MMS likely constrains what is possible to know about Asian American health, via limited resources/opportunities as determined by funding and policies. Potential consequences include narrowed domains of research by what is deemed fundable, smaller segments of the Asian American population represented through funding, a small number of Asian American health-focused scientists supported to conduct research, and the stunting of budding Asian American health researchers’ careers.
Level Two: Research and Healthcare Provision
As shown in Figure 1, consequences of the MMS at the level of funding/policies compounds to how the MMS may constrain knowledge of Asian American health at the level of research and healthcare provision. Narrowed research domains, a disproportionately small Asian American population represented by funded proposals, and few Asian American health-focused scientists may result in little available evidence to justify nuanced research in Asian subpopulations. The MMS may also constrain Asian American health science by influencing what type of research is conducted by the larger scientific community. Errors in information synthesis (e.g., conclusions supporting the MMS based on data excluding LEP Asians in poor health) and cognitive tendencies to retain stereotype-confirming information (Kashima, 2000) can contribute to the absence of Asian Americans in studies, particularly when the requisite, added complexity of research designs poses a barrier. The works of and/or collaborations with community-connected, language-proficient, multicultural scientists promises to propel inclusion of a wider range of Asian Americans in research. Yet, limited support for those researchers at the funding/policy level likely constrains the pool of scientists.
As an illustration, a brief search of 10 scientific journals in health psychology and behavioral medicine8 suggests that health psychology is not immune to the potential effects of the MMS. From 1900-2020, of the 10,075 U.S.-based articles, only 95 (0.94%) were studies mentioning Asian Americans in the title, abstract, or keywords, and 54% of the 95 contained within-group or ethnic-specific analyses. Additionally, mirroring evidence that a minority of scientists examining racial/ethnic groups are researchers of color (Hartmann et al., 2013; Roberts et al., 2020), 28.6% of the 77 corresponding authors were Asian.9 A minority of the corresponding authors were housed in psychology departments at the time of publication (28.2% for all authors, 11.7% for Asian authors), suggesting that a majority of health psychology/behavioral medicine research including Asian Americans is neither being conducted in psychology nor does it have Asian researchers as senior authors.10 Research on Asian American health foregone, possibly in part from MMS-associated barriers for scientists, limits relevant knowledge.
The MMS may also have serious healthcare implications, determining how many clinically screened, diagnosed, or treated Asian Americans are available for recruitment to health research. Stereotypes influence decision-making processes (Dovidio & Gaertner, 2000), particularly when time is limited (Macrae et al., 1994) as is common in healthcare settings. Implicit racial biases also influence healthcare providers’ decision making (Dovidio & Fiske, 2012) and the quality of patient-provider communication (Maina et al., 2018), especially in the case of subjective interpretation of patients’ self-reports (Soares et al., 2019). Unfortunately, the influence of the MMS on medical screening, diagnosis, and care for Asian Americans is yet to be studied. Investigation is needed to test whether the MMS adds to existing barriers in health care, especially for LEP patients whose physicians perceive inadequate time for discussion or report not trying as hard for patients displaying distrust (Guerra et al., 2007).
When the MMS is primed in undergraduate students, Asian Americans are perceived as having better mental health and, in a symptom recall task, fewer clinical mental health symptoms are remembered for vignettes depicting an Asian vs. a NHW person (Cheng et al., 2017). Such MMS-produced effects may exist in healthcare, as suggested by health disparities data. In an evaluation of emergency medical management of pain across racial/ethnic groups, Asians were least likely (OR=0.69) to receive a pain assessment and were less likely than NHWs to receive pain medication for traumatic injuries (OR=0.76), after adjusting for age, gender, insurance status, and geographic location (Kennel et al., 2019). In another example with care coordination, which is a primary predictor of A/PIs’ lower ratings for received care (Collins et al., 2017), A/PIs’ primary care providers had the lowest patient-provided ratings (vs. NHW patients’ ratings) for having patients’ medical records or relevant information prepared during visits, having up-to-date information on care from specialists, and having timely follow-up on test results (Martino et al., 2016). Similarly, recent data show that Asians get less expedient care prior to cancer diagnosis compared to NHWs, Blacks, and Hispanics (Farias et al., 2020).
MMS effects may also be stronger in health domains with “known” group advantage, such as with Asian Americans’ low base rate of alcohol use disorders. In a vignette study of psychologists in training, Asians were less likely than NHWs to be given an alcohol use disorder diagnosis despite a clinical description that warranted one (Cheng et al., 2018). Supporting prior findings that medical professionals can stereotype minority patients (Van Ryn & Burke, 2000), an image of the healthy and accommodating Asian American could result in missing healthcare needs (e.g., potentially lower referral to screenings; Ibaraki et al., 2014).
Data on smoking cessation recommendations are another good example of the possibility that the MMS affects health care. Smoking is a risk factor for many cancers, particularly lung cancer, a leading cause of cancer-related mortality in Asian Americans. Although Asians have the lowest smoking prevalence in the U.S. (9.0%; Jamal et al., 2018), within-group smoking prevalence is highest for Koreans (20.0%) and Vietnamese men (24.4%) (Martell et al., 2016).11 Smoking cessation recommendations are critical due to the role of second-hand smoke in lung cancer mortality (Samet et al., 2009) affecting Asians with low smoking prevalence (Thompson et al., 2016). Yet, 2000-2015 National Health Interview Survey data from cigarette smokers show that Asians were the least likely to receive advice to quit from healthcare professionals (34.2%) compared to American Indian/Alaska Native (38.1%), Hispanic (42.2%), Black (55.7%) and NHW adults (60.2%), with smoking cessation recommendations decreasing linearly only for Asians (U.S. Department of Health and Human Services, 2020).
In summary, the MMS likely constrains what is possible to know about Asian American health via underrepresentation of Asian Americans, especially those with LEP, in research and reliance on samples of Asian Americans who are already receiving health care, which excludes those who are never screened, referred, or diagnosed and who drop out from inadequate care.
Level Three: Public Awareness
Paralleling the public’s overestimated perception of Asian Americans’ wealth (Kuo et al., 2020), the public may overestimate the good health of Asian Americans per the MMS. Any pre-existing influence of the MMS upon public awareness is likely magnified by the consequences of the MMS at Levels One and Two. A consequence could be less engagement of Asian Americans in activities that foster health-related knowledge, such as taking part in research, engaging in community discourse about health, and creating community behavioral norms.
Asian Americans may be persuaded to match in-group attitudes when they perceive that their community believes the MMS (Chao et al., 2013; Stangor et al., 2001). A perceived shared belief in the MMS would then transfer to social norms about health and health-related behaviors (Ajzen, 1985; Rosenstock, 1974). To the extent that the MMS is internalized, perceived susceptibility to illness will be lower, as will perceived threat to health and perceived benefits of taking preventive actions (Rosenstock, 1974). Data on preventive health behaviors are suggestive of a MMS effect on Asian Americans’ health awareness. Asians who smoke have the lowest intention to quit in the next six months compared to all other U.S. racial/ethnic groups (Soulakova et al., 2017). Asian Americans, particularly those with LEP (Kao et al., 2016), are less likely to engage in recommended leisure-time physical activity than non-Asians (Kandula & Lauderdale, 2005). Also, despite a greater proportion of Asian Americans living with undiagnosed type 2 diabetes (due to atypical presentations in lower BMI and younger age; CDC, 2019), they are the least likely to get screened (Tung et al., 2017) and may not request it (Hsu et al., 2015) in the absence of diagnosed hypertension (P. Tran et al., 2020).
The MMS may also contribute to Asian Americans’ lower engagement in health advocacy and activities fostering knowledge about Asian American health, by increasing psychological distress (i.e., depression, anxiety, stress; Atkin et al., 2018) and negative attitudes toward help-seeking (Gupta et al., 2011; Kim & Lee, 2014). Being aware of the MMS or of close others endorsing the MMS (Sinclair et al., 2006) may create a sense of being aberrant when Asian Americans experience health problems, contributing to feelings of stigma or shame. For example, Asian American youth with low academic performance (therefore violating the MMS) experienced worse health in the forms of greater suicide risk and substance abuse in comparison to African American youth with low academic performance (Whaley & Noel, 2013). A study of Asian American women suicide survivors also noted the negative influences of the MMS (Noh, 2018) upon health and stigma, but more research is needed on this topic.
Within-group discrimination may also be present (Richeson & Sommers, 2016) and, for some Asian Americans, negative interpersonal consequences for breaking a stereotype (Phelan & Rudman, 2010) may add to existing barriers (e.g., LEP, mistrust) for engaging in the community or in research. In instances where healthcare provision is perceived as discriminatory based on the MMS, any cultural tendencies to endure problems alone (Chou & Feagin, 2015) along with MMS internalization, may discourage some Asian Americans from advocacy or social activism (J. Tran & Curtin, 2017) relevant to health.
Summary
We propose that, over time, the MMS and its associated constraints have collectively bottlenecked the knowledge base on Asian American health, thereby contributing to the maintenance of the MMS and obscuring an accurate portrait of Asian Americans’ health (Figure 1). The present context of sparse data and few Asian American health scientists serves to strengthen the MMS-associated constraints upon each level (i.e., funding/policies, research/healthcare, public awareness) and to sustain the knowledge-constraining mechanisms (e.g., limited resources/opportunities, limited inclusion, stigma/shame). Specifically, the MMS’ influence on funding and policies have likely contributed to barring the development of foundational data and the next generation of Asian American health-focused scientists. If indeed researchers are directed away from examining a wider range of Asian American health issues, as a result of lack of funding, hard-to-find mentorship, heuristic thinking, and low public engagement in research and community health, then the consequences of sparse data and few scientists will continually perpetuate the MMS in health. The current knowledge deficit does not mean that important needs and disparities do not exist; more awareness and deliberate effort are needed to probe inter- and intra-group variations while acknowledging that what is presently knowable is only a partial window into Asian American health.
Recommendations for Demarginalizing the Health-related Needs of Asian Americans
As stated throughout, the associations between the MMS and how it might function to hinder knowledge regarding Asian American health are largely unexamined. More psychological research is needed to test which existing structures are most in need of change. Certainly, additional possible mechanisms could be added to the stereotype-constraints model (e.g., MMS-induced perceptions of threat (Maddux, Galinsky, Cuddy, & Polifroni, 2008) affecting the various levels of constraint), and sociocultural factors unrelated to the MMS also constrain knowledge on Asian American health. Nevertheless, we offer recommendations for psychological research and initiatives to demarginalize the health-related needs of Asian Americans masked by the MMS given the: pervasiveness of the MMS, evidence of Asian Americans being disproportionately under-studied, small literature examining nuances in Asian Americans’ health, and data suggesting possibilities of the MMS “at play”.
Investigate and Address Proximal Contributors Maintaining the MMS
The circumstances of sparse, non-representative, or aggregated data and few Asian American health-focused scientists may be the primary proximal contributors maintaining the MMS and its influences on health (Figure 1). In that stereotypes partly depend on being conditioned by what information is available (Tversky & Kahneman, 1973), efforts are needed to increase sample representativeness (e.g., people with low SES or LEP) for comprehensive data on Asian American health and to carefully present data, which in turn may help bolster the pool of scientists who will use, create, and disseminate such information. Assuming the presence of factors important for reducing stereotypes (e.g., motivation to process new information (Devine, 1989; Fiske et al., 1999) and egalitarian goals (Moskowitz et al., 1999)), repetition of exposure to and acknowledgment of stereotype-disconfirming information (Kawakami et al., 2000) may ameliorate consequences of the MMS on Asian American health science over time.
Moving beyond sampling contributing to the predominantly Western, educated, industrialized, rich, and democratic (WEIRD) data in psychology (Henrich et al., 2010), population-focused approaches including community-based participatory research (CBPR) could help generate needed data. For example, in a pilot study of expressive writing with Mandarin/Cantonese-speaking U.S. cancer survivors, CBPR procedures involving community partners at every phase contributed to a successful 95% recruitment rate over four months and 100% intervention compliance (Lu et al., 2012). Continued community partnership promoted the completion of an expressive writing RCT in 96 Mandarin/Cantonese-speaking U.S. cancer survivors (Lu et al., 2017). Other successful CBPR studies reaching LEP participants via lay health workers also provide precedent (e.g., smoking cessation in Vietnamese Americans (Tsoh et al., 2015); colorectal cancer screening in Hmong (Tong et al., 2017)).
By incorporating community-based approaches to investigate biopsychosocial correlates of health, psychology has much to contribute to understanding variations in Asian American health not fully explained by demographic and health care access factors (Elewonibi et al., 2018; Ryu et al., 2013). Many understudied topics are also in need of psychological research (e.g., sleep (M. H. Hall et al., 2009) and eating behaviors (Argueza et al., 2020)), particularly using multilevel designs. Contributions from psychology also are needed to test and revise existing constructs and models (Nagayama Hall et al., 2016) in order to increase knowledge for improving Asian Americans’ health. What is effective in non-Asian populations may not function similarly in Asian Americans with diverse sociocultural backgrounds. For example, research with primarily NHW adults has found emotional disclosure to be beneficial for a variety of outcomes including QOL (Frattaroli, 2006). However, emotional disclosure did not enhance QOL at 6-month follow-up in an expressive writing RCT with Mandarin/Cantonese-speaking Chinese American women (Lu et al., 2017); Surprisingly, the cancer-facts control condition was more effective by helping women cognitively process the cancer experience. A follow-up trial found that a culturally tailored condition combining cognitive reappraisal and emotional disclosure was most beneficial (Lu et al., 2018).
More broadly, to combat the MMS, careful presentation and use of Asian American health statistics are needed. For aggregate Asian American data, findings should be presented in abstracts and discussion sections with an understanding that the MMS may perpetuate the invisibility of Asian American health needs. In line with a health equity perspective (Srinivasan & Williams, 2014), findings should also be framed in a manner that best advocates for the Asian American community, especially when health disparities remain despite improvements (e.g., liver cancer incidence declining for A/PIs, but still exceeding incidence in Black and NHW groups). In describing any overall Asian American group advantage, a conscientious approach is required which involves presenting any existing within-group distinctions (e.g., age, sex, income, education, cultural practices) as well as emphasizing limitations of the data. Taking the extra step to examine added dimensions of variation and conscientious presentation can reduce the likelihood that the pan-ethnic term “Asian American”, originally coined to bring benefit to a marginalized community (Spickard, 2007), is misapplied and masks needs within the Asian American community. More research is needed to clarify when, for whom, and in what context Asian American health resilience occurs, and interpretation of findings should convey respect toward a racial minority community that historically has been “other”-ized.
Act to Change Mechanisms of MMS-Associated Constraints
Another avenue to confront the bottlenecked knowledge base on Asian American health is to target potential mechanisms of MMS-associated constraints.
Level One: Advocating for Funding and Policy to Increase Resources and Opportunities
Greater advocacy is needed for increased funding of Asian American health science and improved policies promoting the inclusion of Asian American communities and development of Asian American health-focused behavioral scientists. Fortunately, some policies supporting the advancement of Asian American health have been implemented over time12. An examination of publications on the Web of Science including the keywords “health”, “behavior”, “psychology”, with “Asian American”13 reveals some benefit for the body of knowledge in Asian American health, segmented by periods before and after key policy changes12,14. The number of publications on Asian Americans in psychology/behavioral medicine increased over the past several decades14, with the largest growth15 (392%) between 1990-1999 and 2000-2009. However, narrowing of the gap has stalled, with the growth rate between 2000-2009 and 2010-2019 (179%) being nearly equivalent to non-Asian American psychology/behavioral medicine literature (180%). Similar to the JAMA report on NIH expenditures (Ðoàn et al., 2019), Asian Americans remain substantially underrepresented in the psychology/behavioral medicine literature over three decades: 0.75% during 1990-1999, 1.26% during 2000-2009, and 1.26% during 2010-2019. Increasing funding for the science of Asian American health and the number of Asian American health-focused behavioral scientists and scientific reviewers is crucial.
Institutional initiatives should also be bolstered to meet the mentorship and training needs of future Asian American health-focused scientists. Funding of training institutes for the development of grant proposals, methodologic and analytic skills, and culturally appropriate research designs is needed. Workshops to maximize the use of large public-use datasets would benefit trainees, as would organized opportunities to build networks of collaborators and mentors. Recommendations are available for mentoring future scientists of Asian heritage while attending to cultural influences (e.g., Chin & Kameoka, 2019) and diverse backgrounds (Wyatt et al., 2019), which also may be useful for developing institutional initiatives.
Level Two: Shifting Research and Healthcare Infrastructure toward Inclusive Practice
Health science needs greater inclusion of Asian samples—particularly the often-excluded LEP, foreign-born immigrants. A large proportion of health research is with relatively wealthy, educated, NHW persons in universities or academic medical centers, and a shift is needed to examine understudied groups in diverse contexts (Croyle, 2015; Henrich et al., 2010). Cross-institutional and transdisciplinary efforts to harmonize data collection efforts are needed (Ðoàn et al., 2019) alongside small population research (Srinivasan et al., 2015). Team science may be especially relevant for hard-to-reach Asian samples; options for pursuing collaborations are rapidly expanding with latest technologies for communication and research.
Regarding the MMS and healthcare provision, research is warranted to determine maximally effective approaches. Self-management of biases is possible with practice (Dovidio & Fiske, 2012), and training healthcare professionals to be aware of the potential harms of the MMS on decision making, referrals, diagnoses, and treatment could be useful. Preventive action can also be taken, given substantial evidence that suboptimal, stressful, and time-pressured environments can lead to increased stereotyping and use of heuristics (Dovidio & Fiske, 2012; Macrae et al., 1994). For instance, performance metrics to improve efficiency or reduce costs can result in reduced time with patients, and reforming these types of healthcare system structures may be beneficial. It may also be prudent to develop objective, standardized procedures that reduce the influence of heuristics or implicit bias in medical settings (Soares et al., 2019). Improved healthcare provision for all Asian Americans will provide opportunities for advancing Asian American health science as well.
Level Three: Raising Public Awareness and Reducing Stigma
Raising the public’s awareness about the inaccuracy of the MMS in health and its contribution to the invisibility of Asian Americans’ health needs is important, particularly within Asian American communities. How this might be achieved, however, remains an empirical question in light of the vast diversity in the Asian American population. If perception of a shared reality of the MMS can be created through media (Chao et al., 2013), can media be harnessed to reshape such perceptions? Presenting accurate information about the MMS and others’ views of the MMS, particularly by in-group members (Stangor et al., 2001), may help alter a perceived shared reality, although stereotypes are hard to change (Finnegan et al., 2015). In addition, implementation intention planning with specificity of when and how the MMS will be countered cognitively or behaviorally may reduce effects of the MMS (Mendoza et al., 2010).
Strategies from mental health research also might be applied to physical health-related stigma such as increasing social contact (Corrigan et al., 2012; Pettigrew & Tropp, 2006) with Asian Americans coping with physical health conditions. In this era of increased technology use, with frequent use and acceptability in some Asian communities (J. A. Lee et al., 2017; Perrin, 2016), sharing Asian American narratives in video, picture, or e-print may raise awareness about healthy behaviors or chronic conditions. For older adults less familiar with social media or the internet, collaborative education and resource provision in community settings (e.g., Ma et al., 2015) could be effective. Public campaigns and advocacy encouraging supporting family members’ and friends’ participation in health research for collective well-being may also be fruitful, given that social support and interdependence orientation can facilitate positive preventive health behaviors (Dong & Liu, 2017; Zhao et al., 2014), and lacking social support is a primary barrier to Asian Americans’ research participation (George et al., 2014). Another promising direction may be to involve community residents as researchers and disseminators of research with citizen science (King et al., 2019), which could have long-term positive effects for Asian Americans’ engagement in social activism and community health.
Conclusion
For far too long Asian Americans’ health has been under-examined, at least in part because of the socially crafted MMS contributing to a knowledge disparity in Asian American health. Steps are in progress to move the field of psychology, and health science more generally, in the right direction. Still, substantial progress is needed to demarginalize Asian Americans’ unmet health needs, obscured by the MMS.
Supplementary Material
Public Significance:
The model minority stereotype applied to Asian Americans’ health needs to be interrogated and overcome to advance all Asian American populations’ health and well-being.
Acknowledgments
Jacqueline H. J. Kim was supported by the National Institute of Mental Health (T32MH015750; PI: Dunkel Schetter) and the National Cancer Institute (K99CA246058; PI: Kim). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
We are grateful to Kimberly Martin for providing feedback on the manuscript. We also acknowledge Amy Ko, Lisa Bang, Yuri Ceriale, Josephine Tang, Iris Kang, Nikki Lumauod, and Shawn Hwang for their assistance with administrative tasks and literature reviews.
Footnotes
We have no known conflicts of interest to disclose.
Though our main focus is on Asian Americans as defined by the “Asian” racial/ethnic category in the 1997 Office of Management and Budget Federal Register Notice (Office of Management and Budget, 1997), we present aggregated data on AANHPIs or Asian/Pacific Islanders (A/PIs) when the original source does not present disaggregated information. We do not intend to suggest that NHs/PIs should be subsumed under an umbrella term of Asians. We also use the term “Asian(s)” when referring to the U.S. racial categorization as presented in the original sources; we do not intend to solely refer to immigrants who are not naturalized.
including physical health-related mental health
When the proportionate mortality ratio is >1, hypertension accounts for a larger percentage of deaths in the comparison group than the NHW reference group.
There also are naturally darker-skinned East Asians.
“Cancer control science is the conduct of basic and applied research in the behavioral, social, and population sciences to create or enhance interventions that, independently or in combination with biomedical approaches, reduce cancer risk, incidence, morbidity and mortality, and improve quality of life” (National Cancer Institute, 2011)
Until 2012 when cancer became the leading cause of death for Hispanics/Latinos (Chen et al., 2018)
Although the Chinese breast cancer survivors lived in the U.S. for 18 years on average, their QOL indicated by the Functional Assessment of Cancer Therapy-General Scale (FACT-G) was low (M=73.3), compared with NHW female cancer patients (normative value=82.1 (Brucker et al., 2005)) and breast cancer survivors (M=84.3 (Rogers et al., 2015)). A difference of 5–7 points is deemed clinically significant.
Web of Science search of “(CU=(USA) AND TS=(asian OR korean OR chinese OR filipin* OR asian indian OR vietnamese OR thai OR cambodian OR hmong OR burmese OR bangladesh* OR indonesian OR japanese OR laotian OR malay* OR mongolia* OR pakistan* OR singapore* OR sri lanka* OR taiwan OR myanmar OR bhutan* OR nepal* OR brunei OR asian american)) AND DOCUMENT TYPES: (Article)” in Health Psychology Review, Health Psychology, Psychosomatic Medicine, Annals of Behavioral Medicine, Translational Behavioral Medicine, International Journal of Behavioral Medicine, Journal of Psychosomatic Research, Journal of Behavioral Medicine, International Journal of Clinical and Health Psychology, British Journal of Health Psychology. See Supplemental Appendix A for details.
As in Hartmann et al. (2013), race/ethnicity was solicited via email. Authors were informed that their names would not be associated with the summary count (56% response rate). For non-responders with last names of potential Asian origin, as in Roberts et al. (2020), two coders independently examined online images for agreement upon Asian ethnicity.
Similarly, when examining NIH chartered review group members in behavioral health-relevant study sections (ARM, BMIO, IPTA, PDRP, PRDP, SPIP, PPAH, APDA, MESH, NMB, NNRS, CIHB, CLHP, DIRH, HDEP, HSOD, BGES, SSPA, SSPB), 41 (10.82%) of the 379 members were affiliated with Psychology, and an estimated 0.26% are Asian in Psychology (1 person; 2.4% of the 41).
Rates are likely underestimated in national surveys conducted in English.
1999: 1st White House Initiative on A/PIs “to improve the quality of life of [A/PIs] through increased participation in Federal programs where such persons may be underserved” (The White House, 1999); 2000: 1st NCI-funded Asian American cancer network (Chen et al., 2018) and the launch of the NIMHD (Minority Health and Health Disparities Research and Education Act of 2000, 2000); 2009: Restoration of the White House workgroup for A/PIs (The White House, 2009); and 2011: Revision of U.S. data collection standards to include AANHPI subgroups (U.S. Department of Health and Human Services, 2011)
Web of Science search with (TS=(Asian American AND health AND behavior) OR TS=(Asian American AND health AND psychology)) AND CU=(USA) AND LANGUAGE: (English) AND DOCUMENT TYPES: (Article)
Asian American: 60 (1990-1999), 295 (2000-2009), 823 (2010-2019) vs. non-Asian American: 8,085 (1990-1999), 23,045 (2000-2009), 64,557 (2010-2019). Asian American numbers from the Web of Science search are overestimates because they include articles not centrally focused on Asian Americans.
((# pubs more recent decade – # pubs earlier decade) / # pubs earlier decade)*100. For example, the growth rate for Asian American publications between periods 1990-1999 and 2000-2009 = ((295-60)/60)*100 = 392%
References
- Adler NE (2009). Health disparities through a psychological lens. The American Psychologist, 64(8), 663–673. [DOI] [PubMed] [Google Scholar]
- Agénor M, Abboud S, Delgadillo JG, Pérez AE, Peitzmeier SM, & Borrero S (2018). Intersectional nativity and racial/ethnic disparities in human papillomavirus vaccination initiation among U.S. women: a national population-based study. Cancer Causes & Control, 29(10), 927–936. [DOI] [PubMed] [Google Scholar]
- Ajzen I (1985). From intentions to actions: a theory of planned behavior. In Kuhl J & Beckman J (Eds.), Action control: A theory of planned behavior (pp. 11–39). Springer-Verlag. [Google Scholar]
- Allport GW (1954). The nature of prejudice. Addison-Wesley Pub. Co. [Google Scholar]
- Argueza BR, Sokal-Gutierrez K, & Madsen KA (2020). Obesity and obesogenic behaviors in Asian American children with immigrant and US-born mothers. International Journal of Environmental Research and Public Health, 17(5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Atkin AL, Yoo HC, Jager J, & Yeh CJ (2018). Internalization of the model minority myth, school racial composition, and psychological distress among Asian American adolescents. Asian American Journal of Psychology, 9(2), 108–116. [Google Scholar]
- Bargh JA (1984). Automatic and conscious processing of social information. In Wyer RS Jr. & Srull TK (Eds.), Handbook of social cognition (Vol. 3, pp. 1–43). Lawrence Erlbaum Associates Publishers. [Google Scholar]
- Bastani R, Glenn BA, Tsui J, Chang LC, Marchand EJ, Taylor VM, & Singhal R (2011). Understanding suboptimal human papillomavirus vaccine uptake among ethnic minority girls. Cancer Epidemiology, Biomarkers & Prevention, 20(7), 1463–1472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Becerra MB, Avina RM, Mshigeni S, & Becerra BJ (2020). Low human papillomavirus literacy among Asian-American women in California: an analysis of the California Health Interview Survey. Journal of Racial and Ethnic Health Disparities. [DOI] [PubMed] [Google Scholar]
- Bloom B, & Black LI (2016). Health of non-Hispanic Asian Adults: United States, 2010-2014. [PubMed]
- Bronfenbrenner U (1977). Toward an experimental ecology of human development. The American Psychologist, 32(7), 513–531. [Google Scholar]
- Brucker PS, Yost K, Cashy J, Webster K, & Cella D (2005). General population and cancer patient norms for the Functional Assessment of Cancer Therapy-General (FACT-G). Evaluation & the Health Professions, 28(2), 192–211. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2019, May 7). Diabetes and Asian Americans. Diabetes Resources & Publications. https://www.cdc.gov/diabetes/library/spotlights/diabetes-asian-americans.html [Google Scholar]
- Chao MM, Chiu CY, Chan W, Mendoza-Denton R, & Kwok C (2013). The model minority as a shared reality and its implication for interracial perceptions. Asian American Journal of Psychology, 4(2), 84–92. [Google Scholar]
- Chao MM, Chiu C-Y, & Lee JS (2010). Asians as the model minority: implications for US government’s policies. Asian Journal of Social Psychology, 13(1), 44–52. [Google Scholar]
- Chawla N, Breen N, Liu B, Lee R, & Kagawa-Singer M (2015). Asian American women in California: A pooled analysis of predictors for breast and cervical cancer screening. American Journal of Public Health, 105(2), e98–e109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen MS (2019). Rectifying disparities in funding of Asian American, Native Hawaiian, and Pacific Islander research by the US National Institutes of Health. JAMA Network Open, 2(7), e197561–e197561. [DOI] [PubMed] [Google Scholar]
- Chen MS, Chow EA, & Nguyen TT (2018). The Asian American Network for Cancer Awareness, Research, and Training (AANCART)’s contributions toward reducing Asian American cancer health disparities, 2000-2017. Cancer, 124, 1527–1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen MS, & Hawks BL (1995). A debunking of the myth of healthy Asian Americans and Pacific Islanders. American Journal of Health Promotion, 9(4), 261–268. [DOI] [PubMed] [Google Scholar]
- Cheng AW, Chang J, O’Brien J, Budgazad MS, & Tsai J (2017). Model minority stereotype: influence on perceived mental health needs of Asian Americans. Journal of Immigrant and Minority Health, 19(3), 572–581. [DOI] [PubMed] [Google Scholar]
- Cheng AW, Iwamoto DK, & McMullen D (2018). Model minority stereotype and the diagnosis of alcohol use disorders: implications for practitioners working with Asian Americans. Journal of Ethnicity in Substance Abuse, 17(3), 255–272. [DOI] [PubMed] [Google Scholar]
- Chin D, & Kameoka VA (2019). Mentoring Asian American scholars: stereotypes and cultural values. The American Journal of Orthopsychiatry, 89(3), 337–342. [DOI] [PubMed] [Google Scholar]
- Chugh D (2004). Societal and managerial implications of implicit social cognition: why milliseconds matter. Social Justice Research, 17(2), 203–222. [Google Scholar]
- Cokley K, McClain S, Enciso A, & Martinez M (2013). An examination of the impact of minority status stress and impostor feelings on the mental health of diverse ethnic minority college students. Journal of Multicultural Counseling and Development, 41(2), 82–95. [Google Scholar]
- Collins RL, Haas A, Haviland AM, & Elliott MN (2017). What matters most to whom: racial, ethnic, and language differences in the health care experiences most important to patients. Medical Care, 55(11), 940–947. [DOI] [PubMed] [Google Scholar]
- Corrigan PW, Morris SB, Michaels PJ, Rafacz JD, & Rusch N (2012). Challenging the public stigma of mental illness: a meta-analysis of outcome studies. Psychiatric Services, 63(10), 963–973. [DOI] [PubMed] [Google Scholar]
- Croyle RT (2015). Contribution to the war on cancer. The American Psychologist, 70(2), 221–224. [DOI] [PubMed] [Google Scholar]
- De La Cruz-Viesca M, Chen Z, Ong PM, Hamilton D, & Darity WA Jr. (2016). The color of wealth in Los Angeles. Duke University, The New School, the University of California, Los Angeles and the Insight Center for Community Economic Development. http://www.aasc.ucla.edu/besol/Color_of_Wealth_Report.pdf
- Department of Health and Human Services. (2018, January 25). PA-18-586: research supplements to promote diversity in health-related research. https://grants.nih.gov/grants/guide/pa-files/PA-18-586.html
- DeSantis CE, Ma J, Gaudet MM, Newman LA, Miller KD, Goding Sauer A, Jemal A, & Siegel RL (2019). Breast cancer statistics, 2019. CA: A Cancer Journal for Clinicians, 69(6), 438–451. [DOI] [PubMed] [Google Scholar]
- Devine PG (1989). Stereotypes and prejudice: their automatic and controlled components. Journal of Personality and Social Psychology, 56(1), 5–18. [Google Scholar]
- Ðoàn LN, Takata Y, Sakuma K-LK, & Irvin VL (2019). Trends in clinical research including Asian American, Native Hawaiian, and Pacific Islander participants funded by the US National Institutes of Health, 1992 to 2018. JAMA Network Open, 2(7), e197432–e197432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dong X, & Liu A (2017). Variations between sources of social support and cancer screen behaviors in U.S. Chinese older adults. The Journals of Gerontology. Series A, Biological Sciences and Medical Sciences, 72(S1), S26–S31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dovidio JF, & Fiske ST (2012). Under the radar: how unexamined biases in decision-making processes in clinical interactions can contribute to health care disparities. American Journal of Public Health, 102(5), 945–952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dovidio JF, & Gaertner SL (2000). Aversive racism and selection decisions: 1989 and 1999. Psychological Science, 11(4), 315–319. [DOI] [PubMed] [Google Scholar]
- Dovidio JF, & Gaertner SL (2010). Intergroup bias. In Fiske ST, Gilbert DT, & Lindzey G (Eds.), Handbook of social psychology (Vol. 2, pp. 1084–1121). John Wiley & Sons, Inc. [Google Scholar]
- Elewonibi BR, Thierry AD, & Miranda PY (2018). Examining mammography use by breast cancer risk, race, nativity, and socioeconomic status. Journal of Immigrant and Minority Health, 20(1), 59–65. [DOI] [PubMed] [Google Scholar]
- Fang J, Zhang Z, Ayala C, Thompson-Paul AM, & Loustalot F (2019). Cardiovascular health among non-Hispanic Asian Americans: NHANES, 2011-2016. Journal of the American Heart Association, 8(13), 2011–2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farias AJ, Ochoa CY, Toledo G, Bang SI, Hamilton AS, & Du XL (2020). Racial/ethnic differences in patient experiences with health care in association with earlier stage at breast cancer diagnosis: findings from the SEER-CAHPS data. Cancer Causes & Control, 31(1), 13–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finnegan E, Garnham A, & Oakhill J (2015). Social consensus feedback as a strategy to overcome spontaneous gender stereotypes. Discourse Processes, 52(5-6), 434–462. [Google Scholar]
- Fiske ST, Lin M, & Neuberg S (1999). The continuum model: ten years later. In Chaiken S & Trope Y (Eds.), Dual-process theories in social psychology (pp. 231–254). Guilford Press. [Google Scholar]
- Foundation Center. (2012). Aggregate fiscal data of grants from FC 1000 foundations, for ethnic or racial minorities. http://data.foundationcenter.org/#/fc1000/population_group:minorities/all/total/list/2012
- Frattaroli J (2006). Experimental disclosure and its moderators: a meta-analysis. Psychological Bulletin, 132(6), 823–865. [DOI] [PubMed] [Google Scholar]
- George S, Duran N, & Norris K (2014). A systematic review of barriers and facilitators to minority research participation among African Americans, Latinos, Asian Americans, and Pacific Islanders. American Journal of Public Health, 104(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golden SH, Ferketich A, Boyington J, Dugan S, Garroutte E, Kaufmann PG, Krok J, Kuo A, Ortega AN, Purnell T, & Srinivasan S (2015). Transdisciplinary cardiovascular and cancer health disparities training: experiences of the centers for population health and health disparities. American Journal of Public Health, 105, S395–S402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomez SL, Clarke CA, Shema SJ, Chang ET, Keegan THM, & Glaser SL (2010). Disparities in breast cancer survival among Asian women by ethnicity and immigrant status: a population-based study. American Journal of Public Health, 100(5), 861–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomez SL, Von Behren J, McKinley M, Clarke CA, Shariff-Marco S, Cheng I, Reynolds P, & Glaser SL (2017). Breast cancer in Asian Americans in California, 1988–2013: increasing incidence trends and recent data on breast cancer subtypes. Breast Cancer Research and Treatment, 164(1), 139–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gomez SL, Yao S, Kushi LH, & Kurian AW (2019). Is breast cancer in Asian and Asian American women a different disease? JNCI: Journal of the National Cancer Institute, 111, 1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gone JP (2011). Is psychological science a-cultural? Cultural Diversity & Ethnic Minority Psychology, 17(3), 234–242. [DOI] [PubMed] [Google Scholar]
- Gonzalez BD, & Lu Q (2018). Sleep disturbance among Chinese breast cancer survivors living in the USA. Supportive Care in Cancer, 26(6), 1695–1698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grineski SE, Collins TW, & Morales DX (2017). Asian Americans and disproportionate exposure to carcinogenic hazardous air pollutants: a national study. Social Science and Medicine, 185, 71–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guerra CE, Schwartz JS, Armstrong K, Brown JS, Halbert CH, & Shea JA (2007). Barriers of and facilitators to physician recommendation of colorectal cancer screening. Journal of General Internal Medicine, 22(12), 1681–1688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta A, Szymanski DM, & Leong FTL (2011). The “model minority myth”: internalized racialism of positive stereotypes as correlates of psychological distress, and attitudes toward help-seeking. Asian American Journal of Psychology, 2(2), 101–114. [Google Scholar]
- Hall MH, Matthews KA, Kravitz HM, Gold EB, Buysse DJ, Bromberger JT, Owens JF, & Sowers M (2009). Race and financial strain are independent correlates of sleep in midlife women: the SWAN sleep study. Sleep, 32(1), 73–82. [PMC free article] [PubMed] [Google Scholar]
- Hartmann WE, Kim ES, Kim JHJ, Nguyen TU, Wendt DC, Nagata DK, & Gone JP (2013). In search of cultural diversity, revisited: recent publication trends in cross-cultural and ethnic minority psychology. Review of General Psychology, 17(3), 243–254. [Google Scholar]
- Heckler MM (1985). Report of the Secretary’s Task Force on Black and minority health (Vol. 1). U.S. Department of Health and Human Services. [Google Scholar]
- Henrich J, Heine SJ, & Norenzayan A (2010). The weirdest people in the world? The Behavioral and Brain Sciences, 33(2-3), 61–83. [DOI] [PubMed] [Google Scholar]
- Houston D, Li W, & Wu J (2014). Disparities in exposure to automobile and truck traffic and vehicle emissions near the Los Angeles-Long Beach port complex. American Journal of Public Health, 104(1), 156–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsu WC, Araneta MRG, Kanaya AM, Chiang JL, & Fujimoto W (2015). BMI cut points to identify at-risk Asian Americans for type 2 diabetes screening. Diabetes Care, 38(1), 150–158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurh WM, & Kim KC (1989). The “success” image of Asian Americans: its validity, and its practical and theoretical implications. Ethnic and Racial Studies, 12(4), 512–538. [Google Scholar]
- Ibaraki AY, Nagayama Hall GC, & Sabin JA (2014). Asian American cancer disparities: the potential effects of model minority health stereotypes. Asian American Journal of Psychology, 5(1), 75–81. [Google Scholar]
- Islam NS, Khan S, Kwon S, Jang D, Ro M, & Trinh-Shevrin C (2010). Methodological issues in the collection, analysis, and reporting of granular data in Asian American populations: historical challenges and potential solutions. Journal of Health Care for the Poor and Underserved, 21(4), 1354–1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iyer DG, Shah NS, Hastings KG, Hu J, Rodriguez F, Boothroyd DB, Krishnan AV, Falasinnu T, & Palaniappan L (2019). Years of potential life lost because of cardiovascular disease in Asian-American subgroups, 2003-2012. Journal of the American Heart Association, 8(7), 2003–2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jamal A, Phillips E, Gentzke AS, Homa DM, Babb SD, King BA, & Neff LJ (2018). Current cigarette smoking among adults-United States, 2016 (Vol. 67). https://www.cdc.gov/mmwr/cme/conted_info.html#weekly. [DOI] [PMC free article] [PubMed]
- Johnson KW, Anderson NB, Bastida E, Kramer BJ, Williams D, & Wong M (1995). Panel II: macrosocial and environmental influences on minority health. Health Psychology, 14(7), 601–612. [DOI] [PubMed] [Google Scholar]
- Jose PO, Frank ATH, Kapphahn KI, Goldstein BA, Eggleston K, Hastings KG, Cullen MR, & Palaniappan LP (2014). Cardiovascular disease mortality in Asian Americans. Journal of the American College of Cardiology, 64(23), 2486–2494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kagawa-Singer M, Lu Q, & Valdez Dadia A (2017). 5R01CA158314-05 final report on culture, social support, and quality of life: Asian American breast cancer survivors. [Google Scholar]
- Kagawa-Singer M, Valdez Dadia A, Yu MC, & Surbone A (2010). Cancer, culture, and health disparities: time to chart a new course? CA: A Cancer Journal for Clinicians, 60(1), 12–39. [DOI] [PubMed] [Google Scholar]
- Kandula NR, & Lauderdale DS (2005). Leisure time, non-leisure time, and occupational physical activity in Asian Americans. Annals of Epidemiology, 15(4), 257–265. [DOI] [PubMed] [Google Scholar]
- Kandula NR, Lauderdale DS, & Baker DW (2007). Differences in self-reported health among Asians, Latinos, and Non-Hispanic Whites: the role of language and nativity. Annals of Epidemiology, 17(3), 191–198. [DOI] [PubMed] [Google Scholar]
- Kao D, Carvalho Gulati A, & Lee RE (2016). Physical activity among Asian American adults in Houston, Texas: data from the Health of Houston Survey 2010. Journal of Immigrant and Minority Health, 18(6), 1470–1481. [DOI] [PubMed] [Google Scholar]
- Kashima Y (2000). Maintaining cultural stereotypes in the serial reproduction of narratives. Personality & Social Psychology Bulletin, 26(5), 594–604. [Google Scholar]
- Kawai Y (2005). Stereotyping Asian Americans: the dialectic of the model minority and the yellow peril. Howard Journal of Communications, 16(2), 109–130. [Google Scholar]
- Kawakami K, Dovidio JF, Moll J, Hermsen S, & Russin A (2000). Just say no (to stereotyping): effects of training in the negation of stereotypic associations on stereotype activation. Journal of Personality and Social Psychology, 78(5), 871–888. [DOI] [PubMed] [Google Scholar]
- Kennel J, Withers E, Parsons N, & Woo H (2019). Racial/ethnic disparities in pain treatment: evidence from Oregon emergency medical services agencies. Medical Care, 57(12), 924–929. [DOI] [PubMed] [Google Scholar]
- Kiang L, Huynh VW, Cheah CSL, Wang Y, & Yoshikawa H (2017). Moving beyond the model minority. Asian American Journal of Psychology, 8(1), 1–6. [Google Scholar]
- Kim PY, & Lee D (2014). Internalized model minority myth, Asian values, and help-seeking attitudes among Asian American students. Cultural Diversity & Ethnic Minority Psychology, 20(1), 98–106. [DOI] [PubMed] [Google Scholar]
- King AC, Winter SJ, Chrisinger BW, Hua J, & Banchoff AW (2019). Maximizing the promise of citizen science to advance health and prevent disease. Preventive Medicine, 119(2019), 44–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kochhar R, & Cilluffo A (2018). Income inequality in the U.S. is rising most rapidly among Asians. Pew Research Center. [Google Scholar]
- Kreuter MW, & Haughton LT (2006). Integrating culture into health information for African American women. The American Behavioral Scientist, 49(6), 794–811. [Google Scholar]
- Kuo EE, Kraus MW, & Richeson JA (2020). High-status exemplars and the misperception of the Asian-White wealth gap. Social Psychological and Personality Science, 11(3), 397–405. [Google Scholar]
- LaFromboise T, Coleman HLK, & Gerton J (1993). Psychological impact of biculturalism: evidence and theory. Psychological Bulletin, 114(3), 395–412. [DOI] [PubMed] [Google Scholar]
- Lee JA, Nguyen H, Park J, Tran L, Nguyen T, & Huynh Y (2017). Usages of computers and smartphones to develop dementia care education program for Asian American family caregivers. Healthcare Informatics Research, 23(4), 338–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee S, Juon H-S, Martinez G, Hsu CE, Robinson ES, Bawa J, & Ma GX (2009). Model minority at risk: expressed needs of mental health by Asian American young adults. Journal of Community Health, 34(2), 144–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopez G, Ruiz NG, & Patten E (2017, September 8). Key facts about Asian Americans, a diverse and growing population. http://www.pewresearch.org/fact-tank/2017/09/08/key-facts-about-asian-americans/
- Lortet-Tieulent J, Soerjomataram I, Lin CC, Coebergh JWW, & Jemal A (2016). U.S. burden of cancer by race and ethnicity according to disability-adjusted life years. American Journal of Preventive Medicine, 51(5), 673–681. [DOI] [PubMed] [Google Scholar]
- Luckett T, Goldstein D, Butow PN, Gebski V, Aldridge LJ, McGrane J, Ng W, & King MT (2011). Psychological morbidity and quality of life of ethnic minority patients with cancer: a systematic review and meta-analysis. The Lancet Oncology, 12(13), 1240–1248. [DOI] [PubMed] [Google Scholar]
- Lu Q, Gallagher MW, Loh A, & Young L (2018). Expressive writing intervention improves quality of life among Chinese-American breast cancer survivors: a randomized controlled trial. Annals of Behavioral Medicine, 52(11), 952–962. [DOI] [PubMed] [Google Scholar]
- Lu Q, Wong CCY, Gallagher MW, Tou RYW, Young L, & Loh A (2017). Expressive writing among Chinese American breast cancer survivors: a randomized controlled trial. Health Psychology, 36(4), 370–379. [DOI] [PubMed] [Google Scholar]
- Lu Q, You J, Man J, Loh A, & Young L (2014). Evaluating a culturally tailored peer-mentoring and education pilot intervention among Chinese Breast cancer survivors using a mixed-methods approach. Oncology Nursing Forum, 41(6), 629–637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lu Q, Zheng D, Young L, Kagawa-Singer M, & Loh A (2012). A pilot study of expressive writing intervention among Chinese-speaking breast cancer survivors. Health Psychology, 31(5), 548–551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma GX, Fang C, Tan Y, Feng Z, Ge S, & Nguyen C (2015). Increasing cervical cancer screening among Vietnamese Americans: a community-based intervention trial. Journal of Health Care for the Poor and Underserved, 26(2 Suppl), 36–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Macrae CN, Bodenhausen GV, Milne AB, & Jetten J (1994). Out of mind but back in sight: stereotypes on the rebound. Journal of Personality and Social Psychology, 67(5), 808–817. [Google Scholar]
- Maddux WW, Galinsky AD, Cuddy AJC, & Polifroni M (2008). When being a model minority is good … and bad: realistic threat explains negativity toward Asian Americans. Personality & Social Psychology Bulletin, 34(1), 74–89. [DOI] [PubMed] [Google Scholar]
- Maina IW, Belton TD, Ginzberg S, Singh A, & Johnson TJ (2018). A decade of studying implicit racial/ethnic bias in healthcare providers using the implicit association test. Social Science & Medicine, 199, 219–229. [DOI] [PubMed] [Google Scholar]
- Marlow LAV, Zimet GD, McCaffery KJ, Ostini R, & Waller J (2013). Knowledge of human papillomavirus (HPV) and HPV vaccination: an international comparison. Vaccine, 31(5), 763–769. [DOI] [PubMed] [Google Scholar]
- Martell BN, Garrett BE, & Caraballo RS (2016). Disparities in adult cigarette smoking — United States, 2002-2005 and 2010-2013 (Vol. 65). [DOI] [PubMed]
- Martino SC, Elliott MN, Hambarsoomian K, Weech-Maldonado R, Gaillot S, Haffer SC, & Hays RD (2016). Racial/ethnic disparities in medicare beneficiaries’ care coordination experiences. Medical Care, 54(8), 765–771. [DOI] [PubMed] [Google Scholar]
- Mendoza SA, Gollwitzer PM, & Amodio DM (2010). Reducing the expression of implicit stereotypes: reflexive control through implementation intentions. Personality & Social Psychology Bulletin, 36(4), 512–523. [DOI] [PubMed] [Google Scholar]
- Moskowitz GB, Gollwitzer PM, Wasel W, & Schaal B (1999). Preconscious control of stereotype activation through chronic egalitarian goals. Journal of Personality and Social Psychology, 77(1), 167–184. [Google Scholar]
- Myers HF (2009). Ethnicity- and socio-economic status-related stresses in context: an integrative review and conceptual model. Journal of Behavioral Medicine, 32(1), 9–19. [DOI] [PubMed] [Google Scholar]
- Nagayama Hall GC, & Yee AH (2012). U.S. mental health policy: addressing the neglect of Asian Americans. Asian American Journal of Psychology, 3(3), 181–193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nagayama Hall GC, Yip T, & Zárate MA (2016). On becoming multicultural in a monocultural research world: a conceptual approach to studying ethnocultural diversity. The American Psychologist, 71(1), 40–51. [DOI] [PubMed] [Google Scholar]
- National Cancer Institute. (2011). Cancer control framework and synthesis rationale. https://cancercontrol.cancer.gov/od/about.html
- National Center for Health Statistics. (2019). Racial and ethnic disparities in heart disease. Health, United States Spotlight. https://www.cdc.gov/nchs/hus/spotlight/HeartDiseaseSpotlight_2019_0404.pdf
- Nikaj S, & Lund PK (2019). The impact of individual mentored career development (K) awards on the research trajectories of early-career scientists. Academic Medicine, 94(5), 708–714. [DOI] [PubMed] [Google Scholar]
- Noh E (2018). Terror as usual: the role of the model minority myth in Asian American women’s suicidality. Women & Therapy, 41(3-4), 316–338. [Google Scholar]
- Office of Management and Budget. (1997). Revisions to the standards for the classification of federal data on race and ethnicity.
- Payne-Sturges D, & Gee GC (2006). National environmental health measures for minority and low-income populations: tracking social disparities in environmental health. Environmental Research, 102(2), 154–171. [DOI] [PubMed] [Google Scholar]
- Perrin A (2016). English-speaking Asian Americans stand out for their technology use. Pew Research Center. http://www.pewresearch.org/fact-tank/2016/02/18/english-speaking-asian-americans-stand-out-for-their-technology-use/ [Google Scholar]
- Petersen W (1966). Success story, Japanese-American style. New York Times Magazine, 9(6), 20–43. [Google Scholar]
- Pettigrew TF, & Tropp LR (2006). A meta-analytic test of intergroup contact theory. Journal of Personality and Social Psychology, 90(5), 751–783. [DOI] [PubMed] [Google Scholar]
- Pew Research Center. (2013). The rise of Asian Americans. http://www.pewsocialtrends.org/files/2013/04/Asian-Americans-new-full-report-04-2013.pdf
- Phelan JE, & Rudman LA (2010). Reactions to ethnic deviance: the role of backlash in racial stereotype maintenance. Journal of Personality and Social Psychology, 99(2), 265–281. [DOI] [PubMed] [Google Scholar]
- Quach T, Liu R, Nelson DO, Hurley S, Von Behren J, Hertz A, & Reynolds P (2014). Disaggregating data on Asian American and Pacific Islander women to provide new insights on potential exposures to hazardous air pollutants in California. Cancer Epidemiology, Biomarkers & Prevention, 23(11), 2218–2228. [DOI] [PubMed] [Google Scholar]
- Resnicow K, Baranowski T, Ahluwalia JS, & Braithwaite RL (1999). Cultural sensitivity in public health: defined and demystified. Ethnicity and Disease, 9(1), 10–21. [PubMed] [Google Scholar]
- Richeson JA, & Sommers SR (2016). Toward a social psychology of race and race relations for the twenty-first century. Annual Review of Psychology, 67, 439–463. [DOI] [PubMed] [Google Scholar]
- Roberts SO, Bareket-Shavit C, Dollins FA, Goldie PD, & Mortenson E (2020). Racial inequality in psychological research: trends of the past and recommendations for the future. Perspectives on Psychological Science, 1745691620927709. [DOI] [PubMed] [Google Scholar]
- Rogers LQ, Courneya KS, Anton PM, Hopkins-Price P, Verhulst S, Vicari SK, Robbs RS, Mocharnuk R, & McAuley E (2015). Effects of the BEAT Cancer physical activity behavior change intervention on physical activity, aerobic fitness, and quality of life in breast cancer survivors: a multicenter randomized controlled trial. Breast Cancer Research and Treatment, 149(1), 109–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenstock IM (1974). Historical origins of the Health Belief Model. Health Education Monographs, 2(4), 328–335. [DOI] [PubMed] [Google Scholar]
- Ryu SY, Crespi CM, & Maxwell AE (2013). What factors explain disparities in mammography rates among Asian-American immigrant women? A population-based study in California. Women’s Health Issues, 23(6), e403–e410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Samet JM, Avila-Tang E, Boffetta P, Hannan LM, Olivo-Marston S, Thun MJ, & Rudin CM (2009). Lung cancer in never smokers: clinical epidemiology and environmental risk factors. Clinical Cancer Research, 15(18), 5626–5645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sinclair S, Hardin CD, & Lowery BS (2006). Self-stereotyping in the context of multiple social identities. Journal of Personality and Social Psychology, 90(4), 529–542. [DOI] [PubMed] [Google Scholar]
- Soares WE, Knowles KJ, & Friedmann PD (2019). A thousand cuts: racial and ethnic disparities in emergency medicine. Medical Care, 57(12), 921–923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soulakova JN, Li J, & Crockett LJ (2017). Race/ethnicity and intention to quit cigarette smoking. Preventive Medicine Reports, 5, 160–165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spickard P (2007). Whither the Asian American coalition? Pacific Historical Review, 76(4), 585–604. [Google Scholar]
- Srinivasan S, Moser RP, Willis G, Riley W, Alexander M, Berrigan D, & Kobrin S (2015). Small is essential: importance of subpopulation research in cancer control. American Journal of Public Health, 105(S3), S371–S373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Srinivasan S, & Williams SD (2014). Transitioning from health disparities to a health equity research agenda: the time is now. Public Health Reports, 129(SUPPL. 2), 71–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stangor C, Sechrist GB, & Jost JT (2001). Changing racial beliefs by providing consensus information. Personality & Social Psychology Bulletin, 27(4), 486–496. [Google Scholar]
- Sue S, Sue DW, Sue L, & Takeuchi DT (1995). Psychopathology among Asian Americans: a model minority? Cultural Diversity and Mental Health, 1(1), 39–51. [PubMed] [Google Scholar]
- Thompson CA, Gomez SL, Hastings KG, Kapphahn K, Yu P, Shariff-Marco S, Bhatt AS, Wakelee HA, Patel MI, Cullen MR, & Palaniappan LP (2016). The burden of cancer in Asian Americans: a report of national mortality trends by Asian ethnicity. Cancer Epidemiology, Biomarkers & Prevention, 25(10), 1371–1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong EK, Nguyen TT, Lo P, Stewart SL, Gildengorin GL, Tsoh JY, Jo AM, Kagawa-Singer ML, Sy AU, Cuaresma C, Lam HT, Wong C, Tran MT, & Chen MS Jr. (2017). Lay health educators increase colorectal cancer screening among Hmong Americans: a cluster randomized controlled trial. Cancer, 123(1), 98–106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torre LA, Sauer AMG, Chen MS, Kagawa-Singer M, Jemal A, & Siegel RL (2016). Cancer statistics for Asian Americans, Native Hawaiians, and Pacific Islanders, 2016: converging incidence in males and females. CA: A Cancer Journal for Clinicians, 66(3), 182–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran J, & Curtin N (2017). Not your model minority: own-group activism among Asian Americans. Cultural Diversity & Ethnic Minority Psychology, 23(4), 499–507. [DOI] [PubMed] [Google Scholar]
- Tran P, Tran L, & Tran L (2020). Sociodemographic, socioeconomic, and clinical factors associated with diabetes screening in Asian Americans. Journal of Public Health. [Google Scholar]
- Tsoh JY, Burke NJ, Gildengorin G, Wong C, Le K, Nguyen A, Chan JL, Sun A, McPhee SJ, & Nguyen TT (2015). A social network family-focused intervention to promote smoking cessation in Chinese and Vietnamese American male smokers: a feasibility study. Nicotine & Tobacco Research, 17(8), 1029–1038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tung EL, Baig AA, Huang ES, Laiteerapong N, & Chua K-P (2017). Racial and ethnic disparities in diabetes screening between Asian Americans and other adults: BRFSS 2012-2014. Journal of General Internal Medicine, 32(4), 423–429. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tversky A, & Kahneman D (1973). Availability: a heuristic for judging frequency and probability. Cognitive Psychology, 5(2), 207–232. [Google Scholar]
- U.S. Department of Health and Human Services. (2020). Smoking cessation: a report of the Surgeon General. U.S. Department of Health and Human Services. https://www.hhs.gov/sites/default/files/2020-cessation-sgr-full-report.pdf [PubMed]
- Van Ryn M, & Burke J (2000). The effect of patient race and socio-economic status on physicians’ perceptions of patients. Social Science and Medicine, 50(6), 813–828. [DOI] [PubMed] [Google Scholar]
- Wang JHY, Adams I, Huang E, Ashing-Giwa K, Gomez SL, & Allen L (2012). Physical distress and cancer care experiences among Chinese-American and non-Hispanic White breast cancer survivors. Gynecologic Oncology, 124(3), 383–388. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang JHY, Gomez SL, Brown RL, Davis K, Allen L, Huang E, Chentsova Dutton Y, & Schwartz MD (2019). Factors associated with Chinese American and white cancer survivors’ physical and psychological functioning. Health Psychology, 38(5), 455–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Warmoth K, Cheung B, You J, Yeung NCY, & Lu Q (2017). Exploring the social needs and challenges of Chinese American immigrant breast cancer survivors: a qualitative study using an expressive writing approach. International Journal of Behavioral Medicine, 24(6), 827–835. [DOI] [PubMed] [Google Scholar]
- Wong P, Lai CF, Nagasawa R, & Lin T (1998). Asian Americans as a Model Minority: self-perceptions and perceptions by other racial groups. Sociological Perspectives, 41(1), 95–118. [Google Scholar]
- Wyatt GE, Chin D, Milburn N, Hamilton A, Lopez S, Kim A, Stone JD, & Belcher HME (2019). Mentoring the mentors of students from diverse backgrounds for research. The American Journal of Orthopsychiatry, 89(3), 321–328. [DOI] [PubMed] [Google Scholar]
- Yi JK, Swartz MD, & Reyes-Gibby CC (2011). English proficiency, symptoms, and quality of life in Vietnamese- and Chinese-American breast cancer survivors. Journal of Pain and Symptom Management, 42(1), 83–92. [DOI] [PubMed] [Google Scholar]
- Zhao N, Huh J, Murphy ST, Chatterjee JS, & Baezconde-Garbanati L (2014). Self-construal as a predictor of Korean American women’s intention to vaccinate daughters against human papillomavirus. Asian American Journal of Psychology, 5(2), 96–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


