Abstract
Objective:
To examine medium- to long-term orthodontic treatment stability and its possible association with certain variables.
Materials and Methods:
In a retrospective longitudinal study of 70 postretention patients, the Peer Assessment Rating (PAR) index was measured at the start (T1) and end (T2) of treatment and between 4 and 10 years afterwards (T3). The stability was considered absolute when the T2 and T3 values were identical and relative when the difference was within the ±5 range.
Results:
Among the 70 patients, 65.8% were female and 34.2% were male. Their mean age was 14.5 years. The mean treatment length was 2.4 years. The mean retention phase was 3.3 years. The mean pre- and posttreatment PAR scores were 29.8 (T1) and 6.3 (T2). The mean T1–T2 difference was 23.6. The mean T2–T3 difference was −0.39.
Conclusions:
Within the study, 7.1% presented absolute stability and 68.6% presented relative stability. Lower anterior segment alignment and overbite were the most unstable occlusal features and tended to worsen. Fixed retainer (odds ratio [OR] 0.31; 95% confidence interval [CI] 0.10–0.98) as a protective factor and years without retention (OR 1.32; 95% CI 1.03–1.68) as a risk factor are predictor variables of instability in the case of lower anterior segment alignment. The PAR value at the end of treatment (OR 1.29; 95% CI 1.08–1.54) and extractions (OR 4.76; 95% CI 1.05–21.6) before treatment are predictors for midline instability.
Keywords: Long-term stability, Relapse, Treatment outcome, Orthodontic retainer and retention, Follow-up study
INTRODUCTION
The long-term stability of orthodontic treatment remains one of the main challenges for orthodontists. Studies to analyze the stability of treatments during the initial posttreatment years have drawn attention to an improvement in occlusal contact during the first year due to settling.1 Al Yami et al.2 stated that the maximum movement takes place during the first two posttreatment years, while Greco et al.3 observed a decrease in movement 4 years after the treatment had ended.
The frequency of relapse varies by follow-up time. In the long term, relapse values of 30% have been reported.4 Other researchers5 state that between 30% and 50% of cases maintain an acceptable alignment after 10 years, but barely 10% do so after 20 years. This result reflects how unstable orthodontic treatment is as well as ignorance related to the reasons for this instability and reinforces the need to inform patients about long-term expectations for the treatment. It should be remembered that the patients' satisfaction in the follow-up stage is associated only with their occlusal status at that moment, not with the initial malocclusion or with their occlusion when the treatment ended.6
The methods for assessing stability have traditionally measured independent occlusal features in study models, while occlusal indices assess malocclusion as a whole rather than a specific occlusal relationship or tooth position.7 The Peer Assessment Rating, or PAR, is a very comprehensive index that measures malocclusion on all three spatial planes based on eight components that are weighted to obtain the overall score.8 It has been used to assess treatment results at long-term follow-up and in numerous other studies.2,6,7,9–11
The objective of this study is to examine orthodontic treatment stability in the medium to long term and to ascertain which variables may be associated with it.
MATERIALS AND METHODS
The criteria for inclusion in this retrospective study were as follows: patients treated with fixed appliances and having a complete clinical record, with casts made at the start and end of treatment and during the follow-up stage. The criteria for exclusion from the study were patients with an incomplete clinical history or any kind of deterioration of the casts that prevented measurements from being made and cases that ended in early retainer debonding.
The sample size was estimated at a minimum of 63 for a two-tailed test to compare mean PAR values with a minimum difference of 5, a standard deviation of 10, a 1-α confidence level of 0.95, and 80% power.
The PAR was measured at three points: T1 (initial or pretreatment), T2 (end of treatment), and T3 (between 4 and 10 years after the end of treatment).
The sample was selected by reviewing the records of a total of 1270 posttreatment patients from a private orthodontic practice and 440 from the orthodontics teaching unit at the University of Valencia dental clinic. The inclusion criteria were met by 325 patients, of whom 70 were selected at random (45 from the private practice and 25 from the university clinic). Patients for whom T3 models were not available were contacted in order to obtain these models.
The casts were used to measure the eight occlusal components of the PAR index.8 The PAR index measures the alignment of the upper and lower anterior sectors, buccal occlusion on three planes (antero-posterior, transverse, and vertical), overjet, overbite and/or open bite, and midline alignment. The ratings of the individual components are weighted and added together to give a total score (the PAR value).
The measurements were made by a single orthodontist who underwent PAR index diagnostic criteria standardization and was calibrated against a gold standard (an orthodontist experienced in using the PAR index). The calibration exercise assessed the validity of the measurements of 20 randomly selected cases. The measurements were then repeated in their entirety by the same examiner to test reproducibility. In both cases the agreement was measured by the intraclass correlation coefficient (ICC). The ICC interexaminer agreement was 0.93 for the T1 PAR values, 0.81 for the T2 values, and 0.85 for the T3 values. The ICC intraexaminer agreement was >0.90 for the T1, T2, and T3 PAR values, 0.93.
The following variables were obtained from the differences between PAR values:
Degree of improvement, divided into three categories: Improved—PAR value reduced by under 22 points and/or a percentage change greater than 30%; Greatly improved—reduction of at least 22 points in the total value and/or percentage change greater than 70%; and Worse–No different—reduction less than 30%.12
Quality. The quality of treatment of the sample patients was considered high when over 70% of cases had improved, of which over 40% had to be greatly improved, and when an almost negligible minimum of cases (maximum 5%) had worsened.8
Stability. This variable was classified as follows: a zero difference between the T2 and T3 PAR values was classed as “absolute stability”; a difference in these values within the ±5 range was classed as “relative stability”; and differences greater than ±5 between the T2 and T3 PAR values were classed as “instability.” When measuring stability, each occlusal feature was considered stable when there were no changes between the T2 and T3 measurements and unstable in all the remaining cases, distinguishing between improvement and worsening.
The following variables were recorded from the clinical history of the patient: gender, Angle class, premolar extractions or lack thereof, presence or otherwise of wisdom teeth at T3, type of retainer used, age upon starting treatment, length of treatment, and duration of the retention phase.
The data were analyzed with SPSS software (version 22.0, Chicago, Ill). The means and 95% confidence intervals (CIs) of the quantitative variables and the percentages and 95% CIs of the categorical variables were calculated. A multivariate linear regression model was constructed with the study variables as independent variables and stability as the dependent variable. The alpha (α) significance level for evaluating statistical inference was set at 0.05 for all of the tests. A forward Wald stepwise logistic regression model was constructed with the occlusal features of the PAR index as the dependent variables and pretreatment PAR (T1), posttreatment PAR (T2), fixed retainer, gender (male), wisdom teeth at T3, extractions, retention phase in years, years without retention, and length of treatment as the independent variables.
RESULTS
Of the 70 patients included in the study, 65.8% were female (n = 46) and 34.2% were male (n = 24). Their mean age was 14.5 years at start of treatment. The mean length of treatment was 2.4 years. Table 1 describes the patients included in the study sample.
Table 1.
Description of the Study Samplea
| Age at start of treatment, y | 14.4 (95% CI 12.0–16.7) |
| range: min. 9.0, max. 41.2 | |
| Length of treatment, y | 2.4 (95% CI 2.1–2.6) |
| range: min. 0.8, max. 7.33 | |
| Duration of retention, y | 3.3 (95% CI 2.85–3.69) |
| range: min. 0.3, max. 7.6 | |
| Years without retention, y | 2.6 (95% CI 2.0–3.1) |
| range: min. 0, max. 8.1 | |
| Gender, % | Female 65.8 (n = 46) |
| Male 34.2 (n = 24) | |
| Premolar extractions, % | Yes 31.4 (n = 22) |
| No 68.6 (n = 48) | |
| Presence of wisdom teeth, % | Yes 82.9 (n = 58) |
| No 17.1 (n = 12) | |
| Type of retainer, % | Fixed 70 (n = 49) |
| Removable 30 (n = 21) |
CI indicates confidence interval; min., minimum; and max., maximum.
The mean pretreatment PAR (T1) was 29.8 (95% CI 27.2–32.5). The mean posttreatment PAR (T2) was 6.3 (95% CI 5.3–7.3). The mean difference between the T1 and T2 PAR values was 23.6 (95% CI 20.8–26.4). Figure 1 shows the distribution of cases by pretreatment (T1) and posttreatment (T2) PAR values. Concerning the quality of orthodontic treatment, the posttreatment (T2) values met the criteria for a high standard of treatment. Improvement was seen in 97% of the cases (with 47% greatly improved), and only 3% were worse or no different.
Figure 1.
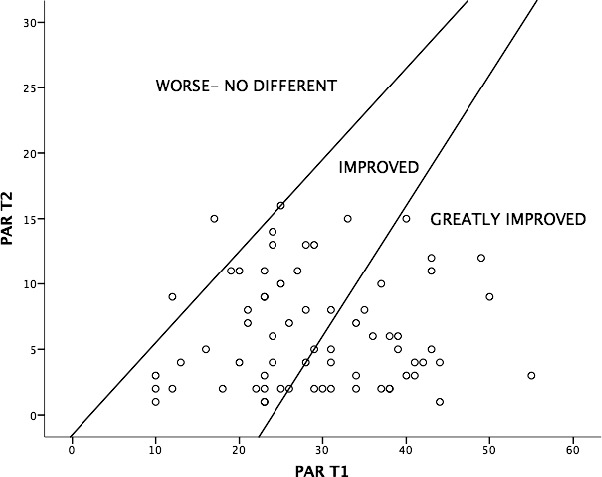
Distribution of cases by T1 and T2 PAR values, classified by degree of improvement at end of treatment.
The difference between the T2 and T3 PAR values was −0.39 (95% CI −1.6 to 0.8), indicating slight worsening in the sample. Figure 2 shows the difference between the T2 and T3 PAR values. At T3, 7.1% of the cases presented absolute stability, 68.6% relative stability, and 24.4% instability.
Figure 2.
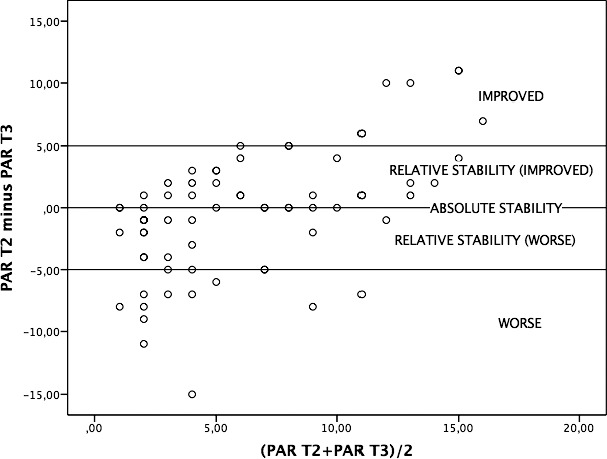
Distribution of cases by difference between T2 and T3 PAR values, classified by degree of absolute or relative stability.
Table 2 shows the distribution of the occlusal features included in the PAR index by percentages of stability, instability (improved), and instability (worse). The most unstable occlusal feature was overbite (42.9%), followed by anterior-posterior buccal occlusion (55.7%). In the percentage of cases that worsened, overbite (28.5%) and lower anterior segment alignment (28.6%) were the features that worsened most.
Table 2.
Percentage of Patients Whose Occlusal Features Remained Stable, Improved, or Worsened Between T2 and T3a
|
|
% Stability (95% CI) |
% Instability |
|
| % Improved (95% CI) |
% Worse (95% CI) |
||
| Upper anterior segments | 77.1 (66.1–85.4) | 8.6 (3.9–17.4) | 14.3 (7.9–24.3) |
| Lower anterior segments | 67.1 (55.5–77.0) | 4.3 (1.5–11.9) | 28.6 (19.3–40.1) |
| Buccal occlusion: antero-posterior | 42.9 (31.9–54.5) | 40.0 (29.3–51.7) | 17.1 (10.1–27.6) |
| Buccal occlusion: vertical | 100.0 (94.8–100.0) | 0.0 (0.0–5.2) | 0.0 (0.0–5.2) |
| Buccal occlusion: transverse | 81.2 (70.7–88.8) | 5.7 (2.3–13.8) | 7.1 (3.1–15.6) |
| Overjet | 70.0 (58.4–79.4) | 15.7 (9.0–25.9) | 14.3 (7.9–24.3) |
| Overbite | 55.7 (44.1–66.7) | 15.7 (9.0–25.9) | 28.5 (19.3–40.1) |
| Open bite | 82.7 (72.4–89.9) | 8.6 (3.9–17.4) | 8.6 (3.9–17.4) |
| Midline | 85.7 (75.6–92.1) | 7.1 (3.1–15.6) | 7.1 (3.1–15.6) |
T2 indicates posttreatment PAR; T3, 4 to 10 years after treatment; and 95% CI, 95% confidence interval.
The multivariate logistic regression model found that the number of years without retention was a predictor for a risk of mandibular alignment instability (odds ratio [OR] 1.32; 95% CI 1.03–1.68), while a fixed retainer was a predictive factor for protection against instability (OR 0.31; 95% CI 0.10–0.98). The PAR value at T2 (end of treatment) (OR 1.29; 95% CI 1.08–1.54) and extractions (OR 4.76; 95% CI 1.05–21.6) were predictive factors for a risk of midline instability (Table 3). No association was found between any of the independent variables and instability in upper anterior segments, lower anterior segments, antero-posterior buccal occlusion, vertical buccal occlusion, transverse buccal occlusion, overjet, overbite, or open bite.
Table 3.
Stepwise Logistic Regression Using Wald Forward Selection. The Variables Removed From the Models Were Pretreatment PAR (T1), Posttreatment PAR (T2), Fixed Retainer, Gender (Male), Wisdom Teeth at T3, Extractions, Retention Phase in Years, Years Without Retention, and Length of Treatment
| Dependent Variables (Predictors of Instability) |
R2 of the Model (Nagelkerke) |
Predictive Variables |
Odds Ratio |
Significance |
| Lower anterior segment alignment | 0.207 | Fixed retainer | 0.311 (0.100–0.976) | .045* |
| Years without retention | 1.319 (1.033–1.684) | .026* | ||
| Center line | 0.267 | T2 PAR | 1.289 (1.083–1.535) | .004** |
| Extractions | 4.757 (1.049–21.570) | .043* |
P < .05; ** P < .01.
Multivariate logistic regression with instability as the dependent variable did not result in significant or predictive variables in the model, although the T2 PAR value (posttreatment) and years without retention were the variables nearest to significance (Table 4).
Table 4.
Stepwise Logistic Regression Using Wald Forward Selection, With Instability as the Dependent Variable: R2 = 0.165
|
|
Odds Ratio |
Significance |
| Pretreatment PAR (T1) | 0.99 (0.93–1.05) | .658 |
| Posttreatment PAR (T2) | 1.14 (0.99–1.31) | .074 |
| Fixed retainer | 1.54 (0.38–6.14) | .545 |
| Gender (male) | 0.64 (0.18–2.29) | .495 |
| Wisdom teeth at T3 | 0.33 (0.04–2.60) | .296 |
| Extractions | 2.13 (0.55–8.25) | .275 |
| Retention period, y | 1.43 (0.83–2.47) | .197 |
| Years without retention | 1.51 (0.96–2.37) | .072 |
| Length of treatment, y | 0.86 (0.46–1.62) | .643 |
| Age at start of treatment, y | 0.96 (0.89–1.04) | .350 |
DISCUSSION
The quality of the treatment received by the study sample population may be considered high according to the PAR index criteria, as 97% of the cases improved (with 47% greatly improved) and only 3% worsened or showed no difference.
The concept of stability has been a subject of debate. Al Yami et al.2 considered the treatment stable when the PAR value remained unchanged between T2 and T3. Other authors, such as Ormiston et al.10 and de Freitas et al.,13 allowed a small margin of variation. Consequently, the present study considered both absolute stability, when there was no difference between T2 and T3 PAR values (7.1% of cases), and relative stability, when the difference lay within the ±5 points range (68.6%).
On comparing the stability of the different variables, midline presented the highest percentage of stable results. By percentages of worse results, lower anterior segment alignment was the least stable feature, agreeing with the findings of the study by Shah.14 Indeed, Yu et al.5 noted that 10 years after the orthodontic treatment ended, only 30% to 50% of patients presented correct lower incisor alignment.
Lower anterior segment alignment showed absolute stability in 67.1% of cases in the present study, a very similar proportion to that obtained by Renkema et al.15 The stability was greater (77.14%) in the upper arch. Naraghi et al.16 observed stability in 89% of patients and Andrén et al.17 found 70% stability, agreeing with the findings of López-Areal and Gandía.18
Anteroposterior buccal occlusion was stable in 42.9% of the patients in the present study, similar to the 44.65% obtained by Uhde et al.19 Transverse buccal occlusion was stable in 87.4% of the present cases, although Schiffman and Tuncay20 observed long-term relapse in between 40% and 64% of cases. The percentage of overjet was 70%, a similar level to that obtained in other studies.19,21 Overbite remained stable in 55.7% of cases, similar to the 44% obtained by Dyer et al.21 although this was the feature with the highest percentage of worsening (28.6%), together with lower anterior segment alignment (28,5%).21 Open bite was very stable (82.7%), a higher percentage than the 61.9% obtained by Janson et al.22 or the 63% stability of Smithpeter and Covell.23
Of all the occlusal features studied, predictive variables for instability were only encountered for lower anterior sector alignment and midline. For lower anterior alignment, a fixed retainer was a protective variable, and the number of years without retention was linked to a risk of instability. A high T2 (posttreatment) PAR value and extractions were both related to a lack of midline stability. Nevertheless, Atack et al.24 did not find any significance regarding the type of retainer.
Regarding extracting or not extracting teeth, several authors have not observed greater stability in patients who have undergone extractions, while others have found greater crowding when extractions have been performed.25,26 However, yet others, such as Boley et al.,27 have observed greater stability when teeth are extracted from patients with marked initial incisor irregularity. Garib et al.28 concluded that a third of the patients treated with four premolar extractions experienced reopening of extraction spaces. They found that 13.7% of the spaces reopened, more frequently in the maxilla than in the mandible, but this tended to decrease by 5 years after treatment.28
The present study found that the presence or otherwise of wisdom teeth at T3 lacked predictive value, joining the doubts and controversy among a number of authors on this subject.29,30
The factor of age at start of treatment continues to be debated. The present study found no association with stability, in agreement with the findings of some other authors.15 Others31,32 argue that starting at an early age makes treatment easier and confers greater stability, but Park et al.33 indicated that in an adolescent, the retention period has to be longer than normal, as the treatment was received at a younger age. Length of treatment was also not found to be related to stability in this study, agreeing with the findings of Renkema et al.15
On examining the relationship between the variables analyzed and long-term stability, no significant differences by gender were observed, in agreement with the findings of other studies.9,26 Other authors25 have found greater crowding in females. In contrast, another study10 encountered more long-term instability in males, suggesting that the cause could be greater residual growth. Gender influences stability, and women have a greater tendency to relapse in the first 10–15 postretention years.34
The degree of initial malocclusion was not found to be a predictive value or related to long-term stability, agreeing with Naraghi et al.16 Hoybjerg et al.1 concluded that patients with a high initial discrepancy index presented significantly greater deterioration of occlusion 1 year into the retention phase, but these authors did not assess the long-term results.
PAR T2 (posttreatment) and years without retention did not prove significant in the logistic regression model but did present values close to the significance level. Therefore, the higher the T2 PAR value, the higher the possible risk of instability. This agrees with the findings of Ormiston et al.10 and de Freitas et al.13 regarding the duration of retention and long-term stability. According to Littlewood et al.,35 there is no scientific evidence concerning the best duration of retention for avoiding relapses.
Some authors36 have indicated that long-term relapse is influenced not only by the result of the orthodontic treatment but also by physiological changes in the dentition and the tissues and forces that surround it.
The main limitation of this study was sample selection. The availability of quality records with a posttreatment period of between 4 and 10 years makes it difficult to obtain a large sample. Other authors37 have also used small samples owing to the need to meet the selection criteria. Nevertheless, it should be mentioned that the sample was of the size calculated prior to the study. Regarding the question of whether the follow-up time was adequate for assessing medium- to long-term stability, this study employed a similar follow-up time to that used by other researchers,3 who have considered that at 4 years posttreatment, the main instability-related changes have already taken place.
CONCLUSIONS
At the end of the follow-up period only 7.1% of cases presented absolute stability, while 68.6% presented relative stability.
Lower anterior segment alignment and overbite are the most unstable occlusal features and tend to worsen.
Of the variables related to instability, not wearing a fixed retainer and years without retention are the only predictive variables that significantly increase the risk of lower incisor alignment instability.
A high PAR score at the end of treatment and extractions before treatment are predictive variables that significantly increase the risk of midline instability.
ACKNOWLEDGMENT
The authors wish to thank Mary-Georgina Hardinge for translating the manuscript into English.
REFERENCES
- 1.Hoybjerg AJ, Currier GF, Kadioglu O. Evaluation of 3 retention protocols using the American Board of Orthodontics cast and radiograph evaluation. Am J Orthod Dentofacial Orthop. 2013;144:16–22. doi: 10.1016/j.ajodo.2013.02.022. [DOI] [PubMed] [Google Scholar]
- 2.Al Yami EA, Kuijpers-Jagtman AM, Van't Hof MA. Stability of orthodontic treatment outcome: follow-up until 10 years postretention. Am J Orthod Dentofacial Orthop. 1999;115:300–304. doi: 10.1016/s0889-5406(99)70333-1. [DOI] [PubMed] [Google Scholar]
- 3.Greco PM, English JD, Briss BS, et al. Posttreatment tooth movement: for better or for worse. Am J Orthod Dentofacial Orthop. 2010;138:552–558. doi: 10.1016/j.ajodo.2010.06.002. [DOI] [PubMed] [Google Scholar]
- 4.Sadowsky C, Sakols EI. Long-term assessment of orthodontic relapse. Am J Orthod. 1982;82:456–463. doi: 10.1016/0002-9416(82)90312-8. [DOI] [PubMed] [Google Scholar]
- 5.Yu Y, Sun J, Lai W, Wu T, Koshy S, Shi Z. Interventions for managing relapse of the lower front teeth after orthodontic treatment. Cochrane Database Syst Rev. 2013;6:1–20. doi: 10.1002/14651858.CD008734.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maia NG, Normando AD, Maia FA, Ferreira MA, Alves MS. Factors associated with orthodontic stability: a retrospective study of 209 patients. World J Orthod. 2010;11:61–66. [PubMed] [Google Scholar]
- 7.Begole EA, Sadowsky C. Methodologies for evaluating long-term stability of dental relationships after orthodontic treatment. Semin Orthod. 1999;5:142–150. doi: 10.1016/s1073-8746(99)80005-x. [DOI] [PubMed] [Google Scholar]
- 8.Richmond S, Shaw WC, Roberts CT, Andrews M. The PAR Index (Peer Assessment Rating): methods to determine outcome of orthodontic treatment in terms of improvement and standards. Eur J Orthod. 1992;14:180–187. doi: 10.1093/ejo/14.3.180. [DOI] [PubMed] [Google Scholar]
- 9.Birkeland K, Furevik J, Bøe OE, Wisth PJ. Evaluation of treatment and post-treatment changes by the PAR Index. Eur J Orthod. 1997;19:279–288. doi: 10.1093/ejo/19.3.279. [DOI] [PubMed] [Google Scholar]
- 10.Ormiston JP, Huang GJ, Little RM, Decker JD, Seuk GD. Retrospective analysis of long-term stable and unstable orthodontic treatment outcomes. Am J Orthod Dentofacial Orthop. 2005;128:568–574. doi: 10.1016/j.ajodo.2004.07.047. quiz 669. [DOI] [PubMed] [Google Scholar]
- 11.Pavlow SS, McGorray SP, Taylor MG, Dolce C, King GJ, Wheeler TT. Effect of early treatment on stability of occlusion in patients with Class II malocclusion. Am J Orthod Dentofacial Orthop. 2008;133:235–244. doi: 10.1016/j.ajodo.2006.02.038. [DOI] [PubMed] [Google Scholar]
- 12.Bernas AJ, Banting DW, Short LL. Effectiveness of Phase I orthodontic treatment in an undergraduate teaching clinic. J Dent Educ. 2007;71:1179–1186. [PubMed] [Google Scholar]
- 13.de Freitas KM, Janson G, de Freitas MR, Pinzan A, Henriques JF, Pinzan-Vercelino CR. Influence of the quality of the finished occlusion on postretention occlusal relapse. Am J Orthod Dentofacial Orthop. 2007;132:428.e9–428.e14. doi: 10.1016/j.ajodo.2007.02.051. [DOI] [PubMed] [Google Scholar]
- 14.Shah AA. Postretention changes in mandibular crowding: a review of the literature. Am J Orthod Dentofacial Orthop. 2003;124:298–308. doi: 10.1016/s0889-5406(03)00447-5. [DOI] [PubMed] [Google Scholar]
- 15.Renkema AM, Al-Assad S, Bronkhorst E, Weindel S, Katsaros C, Lisson JA. Effectiveness of lingual retainers bonded to the canines in preventing mandibular incisor relapse. Am J Orthod Dentofacial Orthop. 2008;134:179e1–179e8. doi: 10.1016/j.ajodo.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 16.Naraghi S, Andrén A, Kjellberg H, Mohlin BO. Relapse tendency after orthodontic correction of upper front teeth retained with a bonded retainer. Angle Orthod. 2006;76:570–576. doi: 10.1043/0003-3219(2006)076[0570:RTAOCO]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 17.Andrén A, Naraghi S, Mohlin BO, Kjellberg H. Pattern and amount of change after orthodontic correction of upper front teeth 7 years postretention. Angle Orthod. 2010;80:620–625. doi: 10.2319/090709-506.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.López-Areal L, Gandía JL. Relapse of incisor crowding: a visit to the prince of Salina. Med Oral Patol Oral Cir Bucal. 2013;18:e356. doi: 10.4317/medoral.18514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Uhde MD, Sadowsky C, BeGole EA. Long-term stability of dental relationships after orthodontic treatment. Angle Orthod. 1983;53:240–252. doi: 10.1043/0003-3219(1983)053<0240:LSODRA>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 20.Schiffman PH, Tuncay OC. Maxillary expansion: a meta analysis. Clin Orthod Res. 2001;4:86–96. doi: 10.1034/j.1600-0544.2001.040205.x. [DOI] [PubMed] [Google Scholar]
- 21.Dyer KC, Vaden JL, Harris EF. Relapse revisited—again. Am J Orthod Dentofacial Orthop. 2012;142:221–227. doi: 10.1016/j.ajodo.2012.03.030. [DOI] [PubMed] [Google Scholar]
- 22.Janson G, Nakamura A, Chiqueto K, Castro R, De Freitas MR, Henriques JFC. Treatment stability with the eruption guidance appliance. Am J Orthod Dentofacial Orthop. 2007;131:717–728. doi: 10.1016/j.ajodo.2005.04.048. [DOI] [PubMed] [Google Scholar]
- 23.Smithpeter J, Covell D., Jr Relapse of anterior open bites treated with orthodontic appliances with and without orofacial myofunctional therapy. Am J Orthod Dentofacial Orthop. 2010;137:605–614. doi: 10.1016/j.ajodo.2008.07.016. [DOI] [PubMed] [Google Scholar]
- 24.Atack N, Harradine N, Sandy JR, Ireland AJ. Which way forward? Fixed or removable lower retainers. Angle Orthod. 2007;77:954–959. doi: 10.2319/103106-449.1. [DOI] [PubMed] [Google Scholar]
- 25.Goldberg AI, Behrents RG, Oliver DR, Buschang PH. Facial divergence and mandibular crowding in treated subjects. Angle Orthod. 2012;83:381–388. doi: 10.2319/061912-505.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Myser SA, Campbell PM, Boley J, Buschang PH. Long-term stability: postretention changes of the mandibular anterior teeth. Am J Orthod Dentofacial Orthop. 2013;144:420–429. doi: 10.1016/j.ajodo.2013.05.004. [DOI] [PubMed] [Google Scholar]
- 27.Boley JC, Mark JA, Sachdeva RC, Buschang PH. Long-term stability of Class I premolar extraction treatment. Am J Orthod Dentofacial Orthop. 2003;124:277–287. doi: 10.1016/s0889-5406(03)00448-7. [DOI] [PubMed] [Google Scholar]
- 28.Garib DG, Bressane LB, Janson G, Gribel BF. Stability of extraction space closure. Am J Orthod Dentofacial Orthop. 2016;149:24–30. doi: 10.1016/j.ajodo.2015.06.019. [DOI] [PubMed] [Google Scholar]
- 29.Bishara SE. Third molars: a dilemma! Or is it? Am J Orthod Dentofacial Orthop. 1999;115:628–633. doi: 10.1016/s0889-5406(99)70287-8. [DOI] [PubMed] [Google Scholar]
- 30.Lindauer SJ, Laskin DM, Tüfekçi E, Taylor RS, Cushing BJ, Best AM. Orthodontists' and surgeons' opinions on the role of third molars as a cause of dental crowding. Am J Orthod Dentofacial Orthop. 2007;132:43–48. doi: 10.1016/j.ajodo.2005.07.026. [DOI] [PubMed] [Google Scholar]
- 31.Haruki T, Little RM. Early versus late treatment of crowded first premolar extraction cases: postretention evaluation of stability and relapse. Angle Orthod. 1998;68:61–68. doi: 10.1043/0003-3219(1998)068<0061:EVLTOC>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 32.Kerosuo H, Heikinheimo K, Nyström M, Väkiparta M. Outcome and long-term stability of an early orthodontic treatment strategy in public health care. Eur J Orthod. 2013;35:183–189. doi: 10.1093/ejo/cjs087. [DOI] [PubMed] [Google Scholar]
- 33.Park H, Boley JC, Alexander RA, Buschang PH. Age-related long-term posttreatment occlusal and arch changes. Angle Orthod. 2010;80:247–253. doi: 10.2319/042109-226.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Zinad K, Schols AM, Schols JG. Another way of looking at treatment stability. Angle Orthod. 2016. Feb 26, [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 35.Littlewood S, Millett D, Doubleday B, Bearn D, Worthington H. Retention procedures for stabilising tooth position after treatment with orthodontic braces. Cochrane Database Syst Rev. 2006;29:1. doi: 10.1002/14651858.CD002283.pub3. [DOI] [PubMed] [Google Scholar]
- 36.Oh H, Ma N, Feng PP, et al. Evaluation of posttreatment stability after orthodontic treatment in the mixed and permanent dentitions. Angle Orthod. 2016. May 23, [Epub ahead of print] [DOI] [PMC free article] [PubMed]
- 37.Janson G, Camardella LT, Araki JDV, De Freitas MR, Pinzan A. Treatment stability in patients with Class II malocclusion treated with 2 maxillary premolar extractions or without extractions. Am J Orthod Dentofacial Orthop. 2010;138:16–22. doi: 10.1016/j.ajodo.2008.08.033. [DOI] [PubMed] [Google Scholar]


