Abstract
Objective:
To compare the long-term outcome 9 years after removal of two different types of fixed retainers used for stabilization of the mandibular anterior segment.
Materials and Methods:
Sixty-four children who had undergone orthodontic treatment with fixed appliances in both arches were divided into two groups depending on which kind of retainer being used. Twenty-eight of the patients had a canine-to-canine retainer bonded to the canines and 36 had a bonded twistflex retainer 3-3, bonded to each tooth. Measurements were made on study models and lateral head radiographs, before and after treatment, 6 years after treatment, and 12 years after treatment, with a mean of 9.2 years after removal of the retainers.
Results:
No significant differences were found between the two groups at the long-term follow-up according to Little's Irregularity Index or available space for the mandibular incisors. The overjet and overbite were reduced after treatment in both groups and stayed stable throughout the observation period. Also, no differences in bonding failures between the two retainers were found.
Conclusions:
Both a canine-to-canine retainer bonded only to the canines and a twistflex retainer 3-3 bonded to each tooth can be recommended. However, neither of the retention types prevented long-term changes of mandibular incisor irregularity or available space for the mandibular incisors after removal of the retainers.
Keywords: Long-term stability, Irregularity Index, Orthodontic retainers, Relapse
INTRODUCTION
Bonded lingual retainers are an important and often-used retention appliance in orthodontic treatment because they are independent of patient cooperation, nearly invisible, and easy to fabricate, but they need regular check-ups. Studies have shown that bonded retainers represent an efficient and reliable retention appliance for long-term use.1–6
For retention of the mandibular incisors with a fixed retention appliance, two different fixed retainers can be used, either a canine-to-canine retainer bonded only to the canines or a retainer bonded to each of the mandibular incisors and canines.7,8 Although these retainers are widely used, only a limited number of studies can be found concerning their long-term effectiveness. In a Cochrane review,9 there was only one randomized clinical trial10 that assessed the mandibular incisor alignment after 3 years of retention.
Furthermore, few studies have analyzed the long-term outcome after removal of the retainers.11 In most studies, the retainers were still in place at follow-up, and the long-term follow-up was only 5 years posttreatment.5,6
When tooth positions during 24 months of retention were compared, it was found that the canine-to-canine retainer induced frequent relapse of incisors not bonded to the retainer compared with the retainer attached to six teeth.12 In addition, another study13 concluded a high failure rate, 34.9% for each of these two retainers, but the canine-to-canine retainer failed significantly less often than did the retainer with six bonding sites. As to comfort, the canine-to-canine retainer was given a significantly poorer rating.12
There are different advantages and disadvantages ascribed to the two types of retainers. However, few studies have been published that compare different types of bonded mandibular retainers and their capacity for maintaining long-term stability, that is, more than 5 years after retention removal. Therefore, the aim of the present study was to compare the long-term outcome 9 years after removal of two different types of fixed retainers used for stabilization of the mandibular anterior segment.
The null hypothesis was that there would be no difference in mandibular incisor stability between the two different mandibular retainers in a long-term perspective.
MATERIALS AND METHODS
The study comprised 64 children (23 boys and 41 girls) who had undergone orthodontic treatment between 1980 and 1995 for Class II malocclusion, deep and/or bite, and/or crowding of the maxillary and mandibular incisors at the Department of Orthodontics, Institute for Postgraduate Dental Education in Jönköping, Sweden. Long-term records were required for participation in the study. Treatment consisted of fixed edgewise appliances (0.018-inch) in both jaws. No interproximal enamel reduction or circumferential supracrestal fiberotomy was performed.
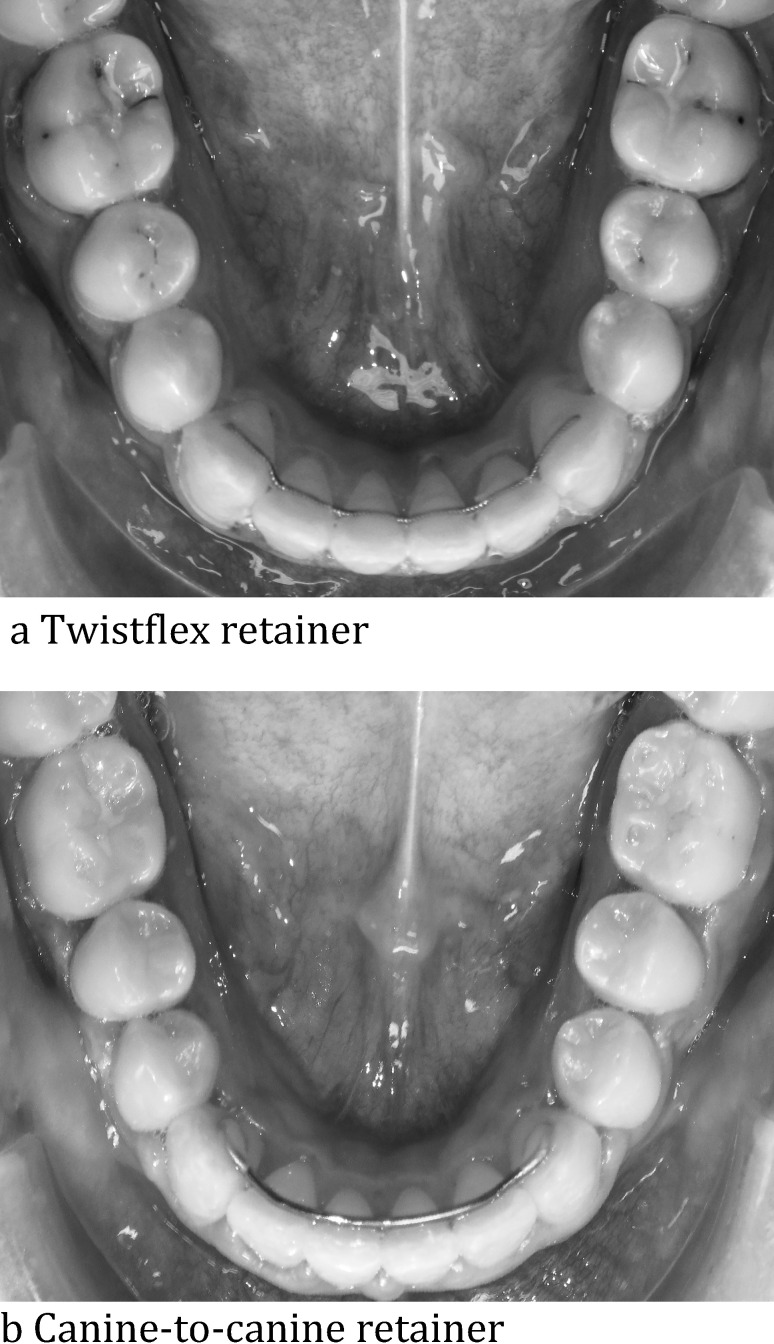
The sample was divided into two groups, depending on which kind of mandibular retainer was used. Twenty-eight of the patients had a canine-to-canine retainer (0.028-inch spring hard wire) bonded to the canines (group 1, Figure 1a), and 36 had a bonded twistflex retainer (0.0195-inch) bonded lingually to all mandibular incisors and canines (group 2, Figure 1b, Table 1). Each group consisted of both extraction (64%) and nonextraction (36%) cases. All retainers were custom-made in the laboratory and were bonded with composite.
Figure 1.
Twistflex retainer and canine-to-canine retainer.
Table 1.
Mean Age and Number of Subjects (Boys/Girls) in Groups 1 And 2, at the Four Registration Points
|
|
T0a |
T1 |
T2 |
T3 |
||||||||||||||||
| n |
Boys |
Girls |
Mean |
SD |
n |
Boys |
Girls |
Mean |
SD |
n |
Boys |
Girls |
Mean |
SD |
n |
Boys |
Girls |
Mean |
SD |
|
| Group 1b | 28 | 13 | 15 | 12.5 | 1.47 | 28 | 13 | 15 | 15.1 | 1.57 | 26 | 12 | 14 | 21.2 | 2.45 | 24 | 11 | 13 | 27.0 | 2.51 |
| Group 2 | 36 | 10 | 26 | 13.2 | 4.18 | 36 | 10 | 26 | 16.1 | 4.36 | 36 | 10 | 26 | 22.4 | 4.13 | 28 | 6 | 22 | 27.8 | 4.14 |
T0 indicates before treatment; T1, after treatment; T2, 6 years after treatment; T3, 12 years after treatment.
Group 1 indicates canine-to-canine retainer; group 2, twistflex retainer.
Methods
The Ethics Committee of Linköping, Sweden, approved the protocol (2014/381−31).
The measurements were performed on dental casts using a sliding digital calliper (Mitutoyo 500−171 Kanagawa, Japan) with an accuracy of 0.01 mm. Measurements were made at four time points: T0, before orthodontic treatment; T1, immediately after treatment, that is, at the start of retention; T2, 6 years after treatment, that is, a mean of 3.6 years after the retainer was removed; and T3, 12 years after treatment, that is, a mean of 9.2 years after retainer removal (Table 2). There were no registrations at retainer removal; thus, the study measured changes after retainer removal.
Table 2.
Number of Years with Retention and Time After Retention for Groups 1 and 2
|
|
Reta Time |
Ret Out–T2b |
Ret Out–T3 |
Time, T0–T1 |
Time, T1–T2 |
Time, T1–T3 |
||||||||||||
| n |
Y |
SD |
n |
Y |
SD |
n |
Y |
SD |
n |
Y |
SD |
n |
Y |
SD |
n |
Y |
SD |
|
| Group 1c | 28 | 2.6 | 2.48 | 26 | 3.7 | 2.52 | 24 | 9.3 | 2.79 | 28 | 2.6 | 0.94 | 26 | 6.2 | 1.99 | 24 | 11.7 | 2.05 |
| Group 2 | 36 | 3.0 | 1.66 | 35 | 3.5 | 1.93 | 28 | 9.1 | 1.86 | 36 | 2.9 | 1.76 | 36 | 6.3 | 2.26 | 28 | 12.2 | 1.82 |
Ret indicates retainer or retention.
T0 indicates before treatment; T1, after treatment; T2, 6 years after treatment; T3, 12 years after treatment.
Group 1 indicates canine-to-canine retainer; group 2, twistflex retainer.
The measured variables were Irregularity Index according to Little14 (LII; the summed displacement of the anatomic contact points of the mandibular anterior teeth), intercanine width (cusp tip to cusp tip of the mandibular canines), intercanine perimeter distance (arch perimeter length between the mesial contact points of the canines), available mandibular incisor space (intercanine perimeter distance minus summed tooth width of the four mandibular incisors), two different lateral arch lengths (mesial contact point of the mandibular first molar to the mesial contact point of the canines or to the mesial contact point of the central incisors), overjet, and overbite (Figures 2 and 3). Also, the tooth width of the mandibular incisors was measured at T0 and T3.
Figure 2.
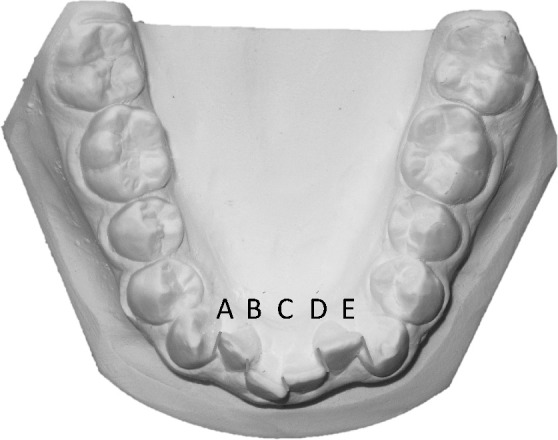
Little's Irregularity Index.
Figure 3.
Variables measured on dental casts.
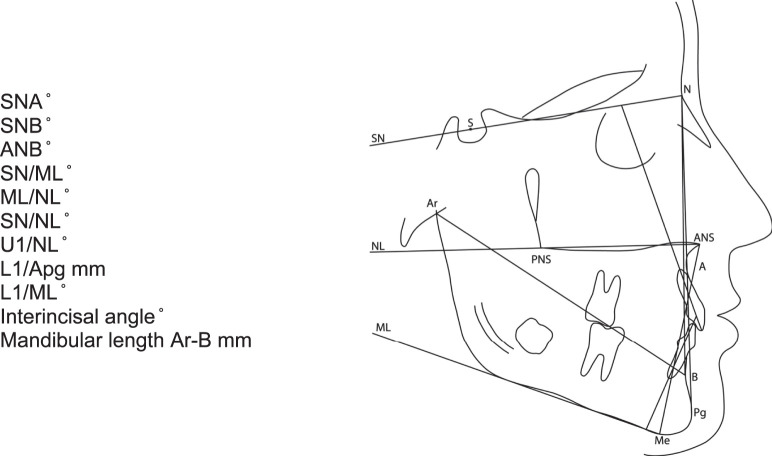
Sagittal and vertical relationships between the jaws as well as incisor inclination and mandibular length were evaluated on lateral head radiographs. Reference lines and points are shown in Figure 4. All measurements on the lateral head radiographs were made to the nearest half-degree or 0.5 mm with correction for enlargement. Cephalometric reference points and measurements were assessed according to Björk15 and Solow16 with the following addition: Ar-B, which is the distance from articulare to point B.
Figure 4.
Cephalometric reference points and lines.
All registrations and measurements were made by one author. At T2 and T3, there were no retention appliances in place and thereby a blinded evaluation was possible, that is, the examiner was unaware as to which group the patients belonged to or whether casts were taken at T2 or T3. In addition, notes of any retainer bonding failures were obtained from the patient files.
Statistical Analysis
Sample size estimation was based on a significance level of 0.05 and 90% power to detect a clinically meaningful difference of 1.5 mm of LII.14 The estimate revealed that 21 patients in each group was sufficient. Arithmetic means and standard deviations (SDs) on group level were calculated for each variable at T0, T1, T2, and T3.
The sample was normally distributed according to the Kolmogorov-Smirnov test.
Significant differences in means in and between groups were tested by one-way analysis of variance using the Statistical Package for Social Sciences (version 22.0, SPSS Inc, Chicago, Ill). P values less than 5% (P < .05) were considered statistically significant. When significant differences were found between groups, the Bonferroni correction was used.
Error of the Measurements
The same examiner measured 24 randomly selected cases at two separate time points with a 4-week interval. The mean error of the measurements according to Dahlberg's formula17 for the linear variables was 0.1 mm. The largest measurement error was 0.5 mm for intercanine width, 0.5 mm for intercanine perimeter distance, and 0.5 mm for left lateral arch length. Error measurements for the cephalometric angular variables were a mean 0.8°. The greatest measurement error was noted for the maxillary incisor inclination, 3.3°.
No significant differences between the two series of records were found using paired t-tests in most of the measurements (in mm) except for the left lateral arch length (range, 0.1 to 0.5), available space (range, −0.3 to 0.2), tooth width 32 (range, −0.1 to 0.1), tooth width 41 (range, −0.1 to 0.1), and L1/Apg (range, −0.1 to 1.3). The systematic error was within the boundaries given above.
RESULTS
Distribution according to age and gender can be seen in Table 1. Teatment started in group 1 at a mean age of 12.5 years (SD 1.47) and 13.2 years (SD 4.18) in group 2 (Table 1). T0–T1 was 2.6 years (SD 0.94) for group 1 and 2.9 years (SD 1.76) for group 2 (Table 2). Mean postretention time was 9.3 years (SD 2.79) for group 1 and 9.1 years (SD 1.86) for group 2 (Table 2). Most of the patients were between 25 and 30 years of age at the last registration (T3).
Little's Irregularity Index
LII14 was 4.5 mm for group 1 and 4.7 mm for group 2 before treatment and after treatment LII was 1.9 mm and 1.6 mm, respectively. Nine years after retention, LII was 4.2 mm in group 1 vs 4.4 mm in group 2. There were no significant intergroup differences, but within each group, several significant differences were found between the four registrations (T0–T3).
Available Space
Available space in the mandibular anterior segment showed similar results as LII (Table 3). For both groups, the available space in the mandibular anterior segment increased after treatment. Six and 12 years after treatment, the available space had decreased in both groups, and for group 1, it was equivalent to that before treatment with no significant intergroup differences (Table 3).
Table 3.
Mean Values MM and Number of Subjects for 14 Variables at the 4 Registration Points Measured on Study Models and the Differences in Mean Values Between Groups 1 and 2.
| Variables |
Group 1 (Canine-to-Canine Retainer) |
Group 2 (Twistflex Retainer) |
|||||
| n |
Mean |
SD |
n |
Mean |
SD |
P
|
|
| Little's Irregularity Index | |||||||
| T0a | 28 | 4.5 | 3.46 | 35 | 4.7 | 2.96 | NSb |
| T1 | 28 | 1.9 | 1.36 | 36 | 1.6 | 1.07 | NS |
| T2 | 26 | 3.2 | 2.01 | 36 | 3.4 | 2.16 | NS |
| T3 | 24 | 4.2 | 2.52 | 28 | 4.4 | 2.31 | NS |
| Available space, mand 3-3 | |||||||
| T0 | 28 | −1.9 | 2.59 | 35 | −2.1 | 2.51 | NS |
| T1 | 28 | −0.1 | 0.45 | 36 | −0.1 | 0.30 | NS |
| T2 | 26 | −1.3 | 1.16 | 36 | −0.8 | 0.84 | NS |
| T3 | 24 | −2.0 | 1.45 | 28 | −1.3 | 1.01 | NS |
| Intercanine width | |||||||
| T0 | 27 | 26.3 | 1.92 | 34 | 25.6 | 1.72 | NS |
| T1 | 28 | 26.2 | 1.63 | 36 | 25.8 | 1.66 | NS |
| T2 | 26 | 25.7 | 1.49 | 36 | 25.2 | 1.63 | NS |
| T3 | 24 | 25.2 | 1.62 | 28 | 24.7 | 1.66 | NS |
| Intercanine perimeter distance | |||||||
| T0 | 27 | 24.3 | 1.24 | 34 | 23.5 | 1.42 | NS |
| T1 | 28 | 24.9 | 1.12 | 36 | 24.1 | 1.59 | NS |
| T2 | 26 | 24.1 | 0.89 | 36 | 23.3 | 1.66 | NS |
| T3 | 23 | 23.4 | 1.13 | 28 | 22.7 | 1.88 | NS |
| Lateral arch length, left 2-6 | |||||||
| T0 | 28 | 20.2 | 2.60 | 36 | 20.3 | 2.49 | NS |
| T1 | 28 | 18.9 | 3.65 | 36 | 19.4 | 3.32 | NS |
| T2 | 26 | 18.6 | 3.64 | 36 | 18.9 | 3.52 | NS |
| T3 | 24 | 18.4 | 3.57 | 28 | 18.8 | 3.46 | NS |
| Lateral arch length, right 2-6 | |||||||
| T0 | 28 | 19.9 | 2.47 | 36 | 20.0 | 2.45 | NS |
| T1 | 28 | 18.4 | 3.57 | 36 | 19.5 | 3.35 | NS |
| T2 | 26 | 17.7 | 3.80 | 36 | 19.1 | 3.28 | NS |
| T3 | 24 | 17.4 | 3.69 | 28 | 19.0 | 3.29 | NS |
| Lateral arch length, left central-6 | |||||||
| T0 | 28 | 29.8 | 2.26 | 36 | 29.6 | 2.38 | NS |
| T1 | 28 | 28.5 | 3.28 | 36 | 28.9 | 3.10 | NS |
| T2 | 26 | 27.6 | 3.34 | 36 | 27.9 | 3.04 | NS |
| T3 | 24 | 27.2 | 3.05 | 28 | 27.7 | 3.07 | NS |
| Lateral arch length, right central-6 | |||||||
| T0 | 28 | 29.5 | 2.19 | 36 | 29.6 | 2.57 | NS |
| T1 | 28 | 28.0 | 3.22 | 36 | 29.0 | 3.20 | NS |
| T2 | 26 | 27.2 | 3.26 | 36 | 28.1 | 3.13 | NS |
| T3 | 24 | 26.8 | 3.11 | 28 | 27.9 | 3.12 | NS |
| Tooth width, 32 | |||||||
| T0 | 28 | 6.3 | 0.32 | 36 | 6.1 | 0.36 | NS |
| T3 | 24 | 6.3 | 0.30 | 28 | 6.0 | 0.39 | NS |
| Tooth width, 31 | |||||||
| T0 | 28 | 5.7 | 0.33 | 36 | 5.5 | 0.31 | NS |
| T3 | 24 | 5.7 | 0.32 | 28 | 5.5 | 0.33 | NS |
| Tooth width, 41 | |||||||
| T0 | 28 | 5.6 | 0.32 | 36 | 5.5 | 0.36 | NS |
| T3 | 24 | 5.6 | 0.31 | 27 | 5.4 | 0.37 | NS |
| Tooth width 42 | |||||||
| T0 | 28 | 6.3 | 0.40 | 36 | 6.0 | 0.39 | * |
| T3 | 24 | 6.3 | 0.41 | 28 | 5.9 | 0.36 | ** |
| Overjet | |||||||
| T0 | 28 | 6.3 | 3.32 | 36 | 7.5 | 3.04 | NS |
| T1 | 28 | 3.2 | 0.91 | 36 | 3.3 | 1.13 | NS |
| T2 | 26 | 3.6 | 1.58 | 36 | 3.9 | 1.68 | NS |
| T3 | 24 | 3.7 | 1.91 | 28 | 4.0 | 1.46 | NS |
| Overbite | |||||||
| T0 | 28 | 3.7 | 2.62 | 36 | 3.5 | 1.79 | NS |
| T1 | 28 | 2.5 | 1.12 | 36 | 2.4 | 1.07 | NS |
| T2 | 26 | 2.8 | 1.80 | 36 | 2.7 | 1.39 | NS |
| T3 | 24 | 2.9 | 1.85 | 28 | 2.9 | 1.20 | NS |
T0 indicates before treatment; T1, after treatment; T2, 6 years after treatment; T3, 12 years after treatment.
NS indicates not significant; * P = .05; **P = .01.
Overjet, Overbite
Both overjet and overbite were reduced after treatment in both groups and then fairly stable throughout the observation period. There were no significant differences between the two groups (Table 3).
Intercanine Width
The intercanine width was almost the same before and after treatment in both groups, and over time, the intercanine width decreased approximately 1 mm in both groups (Table 3).
Intercanine Perimeter Distance
Intercanine perimeter distance increased during treatment by 0.6 mm in both groups. At T2, it had decreased, and it further decreased at T3, 0.9 mm for group 1 and 0.8 mm for group 2 (Table 3).
Arch Length
Both variables for arch length (from the first molar to the canine or to the central incisor) decreased after treatment and continued to decrease 6 and 12 years after treatment in both groups (Table 3).
Tooth Width
There was a small but significant difference in mandibular right lateral incisor width between groups 1 and 2 (Table 3).
Cephalometric Variables
No significant intergroup differences were found for any of the variables measured on the lateral head radiographs at the four time points (Table 4).
Table 4.
Mean Values MM and Number of Subjects for the Cephalometric Variables at the Four Registration Points, Measured on Lateral Head Radiographs and the Differences in Mean Values Between Groups 1 and 2
| Variables |
Group 1 (Canine-to-Canine Retainer) |
Group 2 (Twistflex Retainer) |
|||||
| n |
Mean |
SD |
n |
Mean |
SD |
P
|
|
| SNA, ° | |||||||
| T0a | 28 | 81.0 | 3.55 | 35 | 81.3 | 3.03 | NSb |
| T1 | 17 | 80.4 | 3.33 | 31 | 80.0 | 3.35 | NS |
| T2 | 14 | 79.5 | 3.84 | 24 | 79.8 | 3.23 | NS |
| T3 | 18 | 80.5 | 4.31 | 22 | 79.5 | 2.99 | NS |
| SNB, ° | |||||||
| T0 | 28 | 76.7 | 4.02 | 35 | 76.0 | 2.64 | NS |
| T1 | 17 | 77.3 | 4.43 | 31 | 76.2 | 3.16 | NS |
| T2 | 14 | 76.8 | 5.16 | 24 | 75.9 | 3.20 | NS |
| T3 | 18 | 78.0 | 5.54 | 22 | 75.7 | 3.07 | NS |
| ANB, ° | |||||||
| T0 | 28 | 4.3 | 2.88 | 35 | 5.3 | 3.76 | NS |
| T1 | 17 | 3.2 | 2.35 | 31 | 3.7 | 1.35 | NS |
| T2 | 14 | 2.7 | 2.54 | 24 | 3.9 | 1.79 | NS |
| T3 | 18 | 2.4 | 2.50 | 22 | 3.9 | 1.89 | NS |
| SN/ML, ° | |||||||
| T0 | 28 | 32.8 | 6.10 | 35 | 35.4 | 4.90 | NS |
| T1 | 17 | 32.4 | 7.25 | 31 | 34.7 | 6.02 | NS |
| T2 | 14 | 31.8 | 8.71 | 24 | 33.4 | 6.56 | NS |
| T3 | 18 | 30.7 | 8.35 | 22 | 35.4 | 4.60 | NS |
| ML/NL, ° | |||||||
| T0 | 28 | 26.0 | 5.28 | 35 | 28.9 | 5.04 | NS |
| T1 | 17 | 26.2 | 7.58 | 31 | 28.2 | 6.15 | NS |
| T2 | 14 | 23.8 | 8.18 | 24 | 26.5 | 5.89 | NS |
| T3 | 18 | 23.7 | 7.39 | 22 | 28.3 | 4.93 | NS |
| SN/NL, ° | |||||||
| T0 | 28 | 6.8 | 3.31 | 35 | 6.5 | 3.11 | NS |
| T1 | 17 | 6.1 | 2.67 | 31 | 6.4 | 3.32 | NS |
| T2 | 14 | 8.0 | 3.14 | 24 | 6.9 | 3.30 | NS |
| T3 | 18 | 7.1 | 3.81 | 22 | 7.0 | 3.07 | NS |
| U1/NL, ° | |||||||
| T0 | 28 | 110.7 | 10.47 | 34 | 108.2 | 8.84 | NS |
| T1 | 17 | 105.3 | 10.72 | 31 | 103.4 | 6.48 | NS |
| T2 | 14 | 109.2 | 9.93 | 24 | 106.0 | 6.45 | NS |
| T3 | 18 | 108.8 | 11.79 | 22 | 103.9 | 7.59 | NS |
| L1/Apg, mm | |||||||
| T0 | 28 | 1.1 | 3.81 | 34 | 0.4 | 2.67 | NS |
| T1 | 17 | 0.9 | 3.01 | 31 | 1.8 | 2.03 | NS |
| T2 | 14 | 1.4 | 3.10 | 24 | 1.9 | 1.85 | NS |
| T3 | 18 | 1.2 | 3.59 | 22 | 1.4 | 2.05 | NS |
| L1/ML, ° | |||||||
| T0 | 28 | 93.8 | 5.57 | 34 | 92.3 | 7.81 | NS |
| T1 | 17 | 92.9 | 6.29 | 31 | 95.8 | 8.59 | NS |
| T2 | 14 | 95.1 | 7.28 | 24 | 96.9 | 7.71 | NS |
| T3 | 18 | 93.2 | 7.14 | 22 | 94.1 | 5.96 | NS |
| Interincisal angle, ° | |||||||
| T0 | 28 | 128.8 | 11.42 | 34 | 127.6 | 12.42 | NS |
| T1 | 17 | 134.6 | 8.36 | 31 | 130.7 | 9.51 | NS |
| T2 | 14 | 131.8 | 11.01 | 24 | 129.7 | 6.67 | NS |
| T3 | 18 | 133.2 | 11.85 | 22 | 132.9 | 8.31 | NS |
| Ar-B, mm | |||||||
| T0 | 28 | 94.7 | 5.64 | 30 | 97.1 | 10.10 | NS |
| T1 | 17 | 99.4 | 7.42 | 26 | 102.4 | 9.63 | NS |
| T2 | 14 | 103.3 | 7.61 | 20 | 103.3 | 5.42 | NS |
| T3 | 18 | 108.1 | 6.17 | 20 | 105.6 | 5.72 | NS |
T0 indicates before treatment; T1, after treatment; T2, 6 years after treatment; T3, 12 years after treatment.
NS indicates not significant.
Table 5.
Mean Values MM Between the Four Registrations (T0, T1, T2, T3) for Subjects Measured on Study Models at the Four Registration Points for Groups 1 and 2
|
|
Group 1 Canine-to-Canine-Retainer |
Group 2 Twistflex Retainer |
||||
| Mean |
SD |
P
|
Mean |
SD |
P
|
|
| Little's Irregularity Index | ||||||
| T0a | 4.5 | 3.14 | T0 ≠ T1** | 4.9 | 3.23 | T0 ≠ T1*** |
| T1 | 1.8 | 1.44 | T1 ≠ T2*, T1 ≠ T3* | 1.5 | 1.10 | T1 ≠ T2, T3*** |
| T2 | 3.4 | 2.07 | T2 ≠ T3* | 3.5 | 2.28 | T2 ≠ T3*** |
| T3 | 4.1 | 2.56 | 4.3 | 2.32 | ||
| Available space, mand 3-3 | ||||||
| T0 | −1.8 | 2.48 | T0 ≠ T1* | −1.9 | 2.26 | T0 ≠ T1** |
| T1 | −0.1 | 0.50 | T1 ≠ T2**, T1 ≠ T3*** | −0.1 | 0.33 | T1 ≠ T2, T3*** |
| T2 | −1.4 | 1.20 | T2 ≠ T3* | −0.9 | 0.91 | T2 ≠ T3*** |
| T3 | −1.9 | 1.51 | −1.3 | 1.02 | ||
| Intercanine width | ||||||
| T0 | 26.4 | 1.75 | T0 ≠ T3*, | 25.6 | 1.61 | T0 ≠ T3** |
| T1 | 26.2 | 1.57 | T1 ≠ T2*, T1 ≠ T3** | 25.8 | 1.75 | T1 ≠ T2, T3** |
| T2 | 25.6 | 1.58 | 25.0 | 1.57 | T2 ≠ T3* | |
| T3 | 25.3 | 1.68 | 24.6 | 1.68 | ||
| Intercanine perimeter distance | ||||||
| T0 | 24.4 | 1.20 | T0 ≠ T3* | 23.4 | 1.52 | |
| T1 | 24.9 | 1.12 | T1 ≠ T2, T3*** | 23.9 | 1.72 | T1 ≠ T2, T3*** |
| T2 | 23.9 | 0.86 | T2 ≠ T3* | 23.1 | 1.74 | T2 ≠ T3* |
| T3 | 23.5 | 1.06 | 22.6 | 1.90 | ||
| Lateral arch length, left 2-6 | ||||||
| T0 | 20.5 | 2.51 | T0 ≠ T2, T3* | 20.4 | 2.22 | T0 ≠ T3* |
| T1 | 19.1 | 3.66 | T1 ≠ T2**, T1 ≠ T3*** | 19.5 | 3.20 | T1 ≠ T2*, T1 ≠ T3** |
| T2 | 18.5 | 3.66 | T2 ≠ T3* | 19.0 | 3.46 | T2 ≠ T3*** |
| T3 | 18.4 | 3.57 | 18.8 | 3.46 | ||
| Lateral arch length, right 2-6 | ||||||
| T0 | 20.1 | 2.42 | T0 ≠ T2, T3** | 20.2 | 2.01 | NSb |
| T1 | 18.3 | 3.61 | T1 ≠ T2, T3** | 19.7 | 3.28 | |
| T2 | 17.6 | 3.76 | 19.2 | 3.22 | ||
| T3 | 17.4 | 3.80 | 19.0 | 3.29 | ||
| Lateral arch length, left central-6 | ||||||
| T0 | 29.9 | 2.32 | T0 ≠ T2**, T0 ≠ T3*** | 29.6 | 2.10 | T0 ≠ T2*, T0 ≠ T3** |
| T1 | 28.6 | 3.30 | T1 ≠ T2, T3*** | 28.9 | 3.00 | T1 ≠ T2, T3*** |
| T2 | 27.5 | 3.29 | T2 ≠ T3* | 27.9 | 3.00 | T2 ≠ T3** |
| T3 | 27.2 | 3.17 | 27.7 | 3.10 | ||
| Lateral arch length, right central-6 | ||||||
| T0 | 29.6 | 2.20 | T0 ≠ T2**, T0 ≠ T3*** | 29.7 | 2.11 | T0 ≠ T2*, T0 ≠ T3** |
| T1 | 28.0 | 3.31 | T1 ≠ T2**, T1 ≠ T3*** | 29.1 | 3.16 | T1 ≠ T2, T3*** |
| T2 | 27.1 | 3.22 | T2 ≠ T3* | 28.2 | 3.06 | T2 ≠ T3** |
| T3 | 26.8 | 3.21 | 27.9 | 3.12 | ||
| Overjet | ||||||
| T0 | 6.1 | 3.33 | T0 ≠ T1, T2, T3** | 7.4 | 3.10 | T0 ≠ T1, T2, T3*** |
| T1 | 3.1 | 0.92 | 3.3 | 0.94 | ||
| T2 | 3.5 | 1.67 | 3.8 | 1.57 | ||
| T3 | 3.7 | 1.98 | 4.0 | 1.46 | ||
| Overbite | ||||||
| T0 | 3.5 | 2.64 | NS | 3.6 | 1.65 | T0 ≠ T1* |
| T1 | 2.2 | 0.93 | 2.4 | 0.84 | ||
| T2 | 2.8 | 1.82 | 2.8 | 1.17 | ||
| T3 | 2.8 | 1.87 | 2.9 | 1.20 | ||
T0 indicates before treatment; T1, after treatment; T2, 6 years after treatment; T3, 12 years after treatment.
NS indicates not significant.
P = .05; ** P = .01; *** P = .001.
Extraction Vs Nonextraction
There was no difference in mandibular incisor stability between the patients who had extractions before fixed appliances and those who had no teeth taken out.
Bonding Failures
Bonding failures were found in 32% of the patients with the canine-to-canine retainer and 44% in the twistflex group. The group differences were not statistically significant, however, in some patients; the twistflex retainer came loose more than once.
DISCUSSION
The main result of this study was that there were no differences at the long-term follow-up between the two groups. Thus, the null hypothesis was confirmed. In addition, LII and available space in the mandible were equivalent for both groups before treatment and 12 years after treatment. Furthermore, the important treatment outcomes, overjet and overbite, decreased during treatment and were stable 12 years after treatment. Consequently, either retention method can, from a stability point of view, be recommended as long as the retention is in place.
Studies published on long-term stability of the mandibular incisors after orthodontic treatment show that long-term alignment of the mandibular anterior segment is variable and unpredictable.18 More than 70% of the cases had moderate or severe crowding prior to treatment whereas after retention (at least 10 years after removal of all retainer devices), more than 70% were classified as showing moderate or severe crowding but in different proportions.18 In another study, only 10% of the cases had an acceptable mandibular alignment (LII < 3.5 mm) 20 years postretention.19
In our study, we found patterns similar to those of earlier studies,18,19 that is, relapse of the corrected mandibular incisor irregularity and available incisor space. Consequently, in our study of 64 patients, 42% had an LII of 3.5 mm or less 12 years after treatment. Similar results have also been presented 14 years postretention20; thus, in 78 patients, 47.7% had an LII of 3.5 mm or less.
A long-term follow-up study found that postretention crowding and incisor irregularity increased more frequently in the mandible than in the maxilla.21 Different pretreatment variables such as increased mesiodistal incisor dimension, severe crowding and incisor irregularity, arch length deficiency, and arch constriction, were found to be associated factors in the process of postretention and the resultant increase of crowding and incisor irregularity.
Another study pointed out that more factors than just the type of retention appliance can influence the long-term stability of the mandibular incisors, for example, soft tissue pressure, growth, function, the contact relationship between the maxillary and mandibular incisors, and length of retention.22
In our study, the length of retention was a mean 2.6 years (SD 2.48) for the canine-to-canine retainer and a mean 3.0 years (SD 1.66) for the twistflex retainer. In the study by Edman Tynelius et al.,11 the retention time was 2 years, and LII increased during the 5-year period without retention.
The question is, For how long can the retainer wire be expected to retain the treatment corrections and when is the wire only obstructing normal development? It is likely that 2.5 to 3 years is enough. When retainers are used long-term, it is important to have continuous check-ups to minimize negative side effects such as gingival retraction, buccally standing premolars, and changes in mandibular arch form.
It was found that the groups were equal when comparing cephalometric outcomes, but greater mandibular growth was found in group 1, the group with more boys than girls. However, at the last registration, all patients had reached adulthood, but in both groups, a certain amount of growth can be seen, in agreement with Pancherz et al.23
In this study, some cases had extractions carried out and some were nonextraction cases, with the same distribution of extractions in each group. No difference in mandibular incisor stability was found, regardless of extractions. Similar results have been shown in two other studies.24,25
In both groups, retainer breakage was frequent; for instance, 32% in group 1 and 44% in group 2 experienced retainer failure, meaning retainers had become unattached from one or more teeth. The bonding failure rate was highest during the first year after treatment. This could be one reason for a very small amount of incisor irregularity. The failure rate in another study26 was 46.9% over a 6-month period after debond. Moreover, a review by Iliadi et al.27 evaluated the risk of failure of fixed orthodontic retention protocols and concluded that there was a lack of evidence in selecting the optimal protocol and materials for fixed orthodontic retention.
CONCLUSIONS
Both retention methods, a mandibular canine-to-canine retainer bonded to the canines or a mandibular twistflex retainer 3-3 bonded to each tooth, can be recommended since both are equally effective during the retention period.
However, after removal of the retainers, neither of the retention types prevent long-term changes in mandibular incisor irregularity or available space therefor.
REFERENCES
- 1.Zachrisson BU. Long-term experience with direct-bonded retainers: update and clinical advice. J Clin Orthod. 2007;41:728–737. [PubMed] [Google Scholar]
- 2.Al Yami EA, Kuijpers-Jagtman AM, van't Hof MA. Stability of orthodontic treatment outcome: follow-up until 10 years postretention. Am J Orthod Dentofacial Orthop. 1999;115:300–304. doi: 10.1016/s0889-5406(99)70333-1. [DOI] [PubMed] [Google Scholar]
- 3.Segner D, Heinrici B. Bonded retainers-clinical reliability. J Orofac Orthop. 2000;61:352–358. doi: 10.1007/pl00001905. [DOI] [PubMed] [Google Scholar]
- 4.Booth FA, Edelman JM, Proffit WR. Twenty-year follow-up of patients with permanently bonded mandibular canine-to-canine retainers. Am J Orthod Dentofacial Orthop. 2008;133:70–76. doi: 10.1016/j.ajodo.2006.10.023. [DOI] [PubMed] [Google Scholar]
- 5.Renkema AM, Al-Assad S, Bronkhorst E, Weindel S, Katsaros C, Lisson JA. Effectiveness of lingual retainers bonded to the canines in preventing mandibular incisor relapse. Am J Orthod Dentofacial Orthop. 2008;134:179e1–e8. doi: 10.1016/j.ajodo.2008.06.003. [DOI] [PubMed] [Google Scholar]
- 6.Renkema AM, Renkema A, Bronkhorst E, Katsaros C. Long-term effectiveness of canine-to-canine bonded flexible spiral wire lingual retainers. Am J Orthod Dentofacial Orthop. 2011;139:614–621. doi: 10.1016/j.ajodo.2009.06.041. [DOI] [PubMed] [Google Scholar]
- 7.Zachrisson BU. Important aspects of long term stability. J Clin Orthod. 1997;31:562–583. [PubMed] [Google Scholar]
- 8.Profitt WR. Retention. In: Proffit W, Fields H, Sarver D, editors. Contemporary orthodontics. 5th ed. St Louis, MO: Elsevier Mosby-Year Book;; 2013. pp. 615–616. [Google Scholar]
- 9.Littlewood SJ, Millett DT, Doubleday B, Bearn DR, Worthington HV. Retention procedures for stabilizing tooth position after treatment with orthodontic braces. Cochrane Database Syst Rev. 2006. (1): CD002283. [DOI] [PubMed]
- 10.Artun J, Spadafora AT, Shapiro PA. A 3-year follow-up study of various types of orthodontic canine-to-canine retainers. Eur J Orthod. 1997;19:501–509. doi: 10.1093/ejo/19.5.501. [DOI] [PubMed] [Google Scholar]
- 11.Edman Tynelius G, Petrén S, Bondemark L, Lilja-Karlander E. Five-year postretention outcomes of three retention methods—a randomized controlled trial. Eur J Orthod. 2015;37:345–353. doi: 10.1093/ejo/cju063. [DOI] [PubMed] [Google Scholar]
- 12.Störmann I, Ehmer U. A prospective randomized study of different retainer types. J Orofac Orthop. 2002;63:42–50. doi: 10.1007/s00056-002-0040-6. [DOI] [PubMed] [Google Scholar]
- 13.Scheibe K, Ruf S. Lower bonded retainers: survival and failure rates particularly considering operator experience. J Orofac Orthop. 2010;71:300–307. doi: 10.1007/s00056-010-1015-7. [DOI] [PubMed] [Google Scholar]
- 14.Little RM. The irregularity index. A quantitative score of mandibular anterior alignment. Am J Orthod. 1975;68:554–563. doi: 10.1016/0002-9416(75)90086-x. [DOI] [PubMed] [Google Scholar]
- 15.Björk A. The face in Profile. Uppsala, Sweden: Svensk Tandl Tidsk;; 1947. 40(suppl 1). [Google Scholar]
- 16.Solow B. The pattern of craniofacial associations. Acta Odontol Scand. 1966. 24(suppl 46).
- 17.Dahlberg G. Statistical Methods for Medical and Biological Students. New York: Interscience Publications;; 1940. [Google Scholar]
- 18.Little RM, Wallen TR, Riedel RA. Stability and relapse of mandibular anterior alignment—first premolar extraction cases treated by traditional edgewise orthodontics. Am J Orthod. 1981;80:350–365. doi: 10.1016/0002-9416(81)90171-8. [DOI] [PubMed] [Google Scholar]
- 19.Little RM, Riedel RA, Årtun J. An evaluation of changes in mandibular anterior alignment from 10 to 20 years postretention. Am J Orthod. 1988;93:423–428. doi: 10.1016/0889-5406(88)90102-3. [DOI] [PubMed] [Google Scholar]
- 20.Årtun J, Garol JD, Little RM. Long-term stability of mandibular incisors following successful treatment of Class II, Division 1, malocclusions. Angle Orthod. 1996;66:229–238. doi: 10.1043/0003-3219(1996)066<0229:LTSOMI>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 21.Kahl-Nieke B, Fischbach H, Schwarze CW. Post-retention crowding and incisor irregularity: A long term follow-up. Evaluation of stability and relapse. Br J Orthod. 1995;22:249–257. doi: 10.1179/bjo.22.3.249. [DOI] [PubMed] [Google Scholar]
- 22.Johnston CD, Littlewood S. Retention in orthodontics. Br Dent J. 2015;218:119–122. doi: 10.1038/sj.bdj.2015.47. [DOI] [PubMed] [Google Scholar]
- 23.Pancherz H, Bjerklin K, Hashemi K. Late adult skeletofacial growth after adolescent Herbst Therapy: a 32-year longitudinal follow-up study. Am J Orthod Dentofacial Orthop. 2015;147:19–28. doi: 10.1016/j.ajodo.2014.06.011. [DOI] [PubMed] [Google Scholar]
- 24.Rossouw PE, Preston CB, Lombard C. A longitudinal evaluation of extraction versus nonextraction treatment with special reference to the posttreatment irregularity of the lower incisors. Semin Orthod. 1999;5:160–170. doi: 10.1016/s1073-8746(99)80007-3. [DOI] [PubMed] [Google Scholar]
- 25.Zafarmand AH, Qamari A, Zafarmand MM. Mandibular incisor re-crowding: is it different in extraction and non-extraction cases? Oral Health Dent Manag. 2014;13:669–674. [PubMed] [Google Scholar]
- 26.Taner T, Aksu M. A prospective clinical evaluation of mandibular lingual retainer survival. Eur J Orthod. 2012;34:470–474. doi: 10.1093/ejo/cjr038. [DOI] [PubMed] [Google Scholar]
- 27.Iliadi A, Kloukos D, Gkantidis N, Katsaros C. Failure of fixed orthodontic retainers: a systematic review. J Dent. 2015;43:876–896. doi: 10.1016/j.jdent.2015.05.002. [DOI] [PubMed] [Google Scholar]