Abstract
Objective:
To examine the current trends in surgical-orthodontic treatment for patients with Class III malocclusion using time-series analysis.
Materials and Methods:
The records of 2994 consecutive patients who underwent orthognathic surgery from January 1, 2004, through December 31, 2015, at Seoul National University Dental Hospital, Seoul, Korea, were reviewed. Clinical data from each surgical and orthodontic treatment record included patient's sex, age at the time of surgery, malocclusion classification, type of orthognathic surgical procedure, place where the orthodontic treatment was performed, orthodontic treatment modality, and time elapsed for pre- and postoperative orthodontic treatment.
Results:
Out of the orthognathic surgery patients, 86% had Class III malocclusion. Among them, two-jaw surgeries have become by far the most common orthognathic surgical treatment these days. The age at the time of surgery and the number of new patients had seasonal variations, which demonstrated opposing patterns. There was neither positive nor negative correlation between pre- and postoperative orthodontic treatment time. Elapsed orthodontic treatment time for both before and after Class III orthognathic surgeries has been decreasing over the years.
Conclusion:
Results of the time series analysis might provide clinicians with some insights into current surgical and orthodontic management.
Keywords: Time series analysis, Class III malocclusion, Two-jaw surgery
INTRODUCTION
In certain countries, Class III patients occupy a considerable proportion of orthognathic surgery patients.1–4 Correction of skeletal Class III malocclusions is the most frequent reason to seek an orthognathic surgery consultation.2,5 With increasing demand for improved facial esthetics and advances in surgical techniques, clinicians must be aware of changing trends in the management of severe Class III malocclusion patients.
Single-jaw surgeries are less invasive and more predictable than two-jaw surgeries.6,7 However, for patients with severe Class III malocclusion one-jaw surgery alone may be insufficient to achieve a harmonious profile or an optimal occlusion. For skeletal Class III treatment, the combination of two-jaw surgery with an additional genioplasty has become a common surgical procedure.5,8–11 In recent years, an increase in the proportion of two-jaw surgeries has also been perceived at the author's institution.
A time series is a sequence of observations that are arranged according to the time of their outcome. Decomposing a time series separates the data into a trend component and a seasonal component if they exist.12–14 The time-series analysis has been popular in the medical field and the social sciences. However, as of July 9, 2016, an Internet search using PubMed, revealed only a few papers that applied the time-series method in dentistry. Furthermore time-series analysis articles have not appeared yet in orthodontic journals.
The purpose of this study was to examine the current trends in surgical-orthodontic treatment for patients with Class III malocclusion at Seoul National University Dental Hospital over the past decade using time-series analysis.
MATERIALS AND METHODS
This was a retrospective cohort study of all patients who underwent orthognathic surgical procedures from January 1, 2004, through December 31, 2015, at Seoul National University Dental Hospital, Seoul, Korea (IRB S-D 20140025).
Among the patients reviewed, 116 patients who had a diagnosis of cleft lip and palate or craniofacial syndromes, or who had nonconventional orthognathic surgical procedures (ie, osteotomies for distraction osteogenesis, condylar reconstruction) were excluded (Table 1).
Table 1.
All of the Orthognathic Surgery Patients from January 1, 2004, to December 31, 2015
| Variables |
Frequency |
|
| n |
% |
|
| All of the orthognathic surgery patients reviewed (N = 2994) | ||
| Female | 1534 | 51.2 |
| Male | 1460 | 48.8 |
| Total | 2994 | 100.0 |
| Patients with congenital anomalies | ||
| None | 2878 | 96.1 |
| Patients with cleft | 68 | 2.3 |
| Other anomalies | 48 | 1.6 |
| Patients without anomalies (N = 2878) | ||
| Sex | ||
| Female | 1495 | 51.9 |
| Male | 1383 | 48.1 |
| Total | 2878 | 100.0 |
| Classification | ||
| Class I malocclusion | 138 | 4.8 |
| Class II malocclusion | 274 | 9.5 |
| Class III malocclusion | 2466 | 85.7 |
| Total | 2878 | 100.0 |
| Place of orthodontic treatment performed | ||
| The same institution | 1404 | 46.9 |
| Private practice, transferred for the surgery | 1590 | 53.1 |
Clinical data collected from each medical and dental record included demographic and clinical variables: (1) gender; (2) age at the time of surgery; (3) pre- and postsurgical orthodontic treatment time; (4) type of orthognathic surgery, including adjunctive surgical procedures such as genioplasty or para-nasal augmentation performed; (5) place where the supportive orthodontic treatment was performed; and (6) whether orthodontic treatment was carried out with or without extracting the upper premolars.
For variables with a continuous value, median rather than mean was reported because the median is less influenced by extreme values.15 Age and time comparisons were performed using Wilcoxon tests. The time-series analysis was performed using the free statistics software language R (R Development Core Team, software #R3.3.1, Vienna, Austria).14 To make future forecasts, the additive Holt-Winters prediction function was applied.12
RESULTS
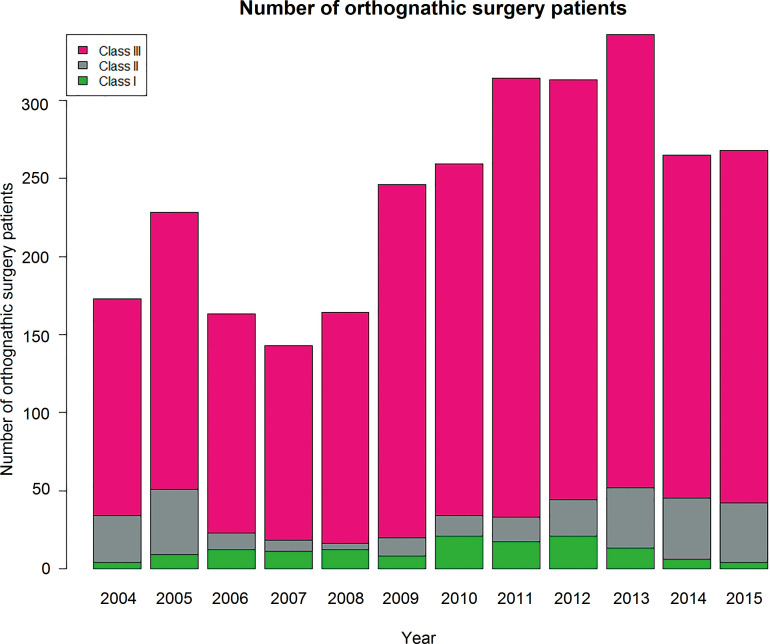
Of the total orthognathic surgeries performed, 86% were for Class III malocclusion (2446; median age, 22 years) (Tables 1 and 2). Over the past decade, Class III malocclusions have continued to account for the highest proportion of surgery patients (Figure 1).
Table 2.
Class III Orthognathic Surgery Patients (N = 2466) from January 1, 2004, to December 31, 2015
| Variables |
Frequency |
|
| n |
% |
|
| Sex | ||
| Female | 1203 | 48.8 |
| Male | 1263 | 51.2 |
| Total | 2466 | 100.0 |
| Place of orthodontic treatment performed | ||
| University orthodontists | 1157 | 46.9 |
| Private practice, transfer for the surgery only | 1309 | 53.1 |
| Extraction except third molars | ||
| Non extraction | 1239 | 50.2 |
| Extraction | 1227 | 49.8 |
| Surgery | ||
| One-jaw surgery | 431 | 17.5 |
| Two-jaw surgery | 2055 | 82.5 |
| Maxillary surgery | ||
| None | 405 | 16.4 |
| Le Fort 1 | 2016 | 81.8 |
| Le Fort 2 | 31 | 1.3 |
| Le Fort 3 | 3 | 0.1 |
| Anterior segment osteotomya | 70 | 2.9 |
| Mandibular surgery | ||
| None | 28 | 1.1 |
| Sagittal split ramus osteotomy | 2113 | 85.7 |
| Intraoral vertical ramus osteotomy | 301 | 12.2 |
| Anterior segment osteotomya | 5 | 0.0 |
| Adjunctive surgerya | ||
| Genioplasty | 1227 | 49.8 |
| Paranasal augmentation | 80 | 3.2 |
| Zygoma reduction | 82 | 3.3 |
Percentages total more than 100 because of multiple surgical procedures.
Figure 1.
Class III malocclusions continue to dominate the highest proportion of surgery patients.
The proportion between female and male patients was not statistically different. The ratio was approximately 50:50 and has not changed substantially over time.
More than half of the patients undergoing orthognathic surgery were referred from private orthodontic offices where they had received orthodontic treatment. Patients who received orthodontic treatment from private practitioners and who were treated at the school department of orthodontics did not show significantly different characteristics in terms of sex, type of orthognathic surgery, or orthodontic treatment modality.
The proportion of patients who experienced orthodontic treatment with extraction was about 50% (Table 2). The time-series analysis did not show an obvious seasonal variation or clear trend regarding extractions.
Type of Orthognathic Surgery Procedures
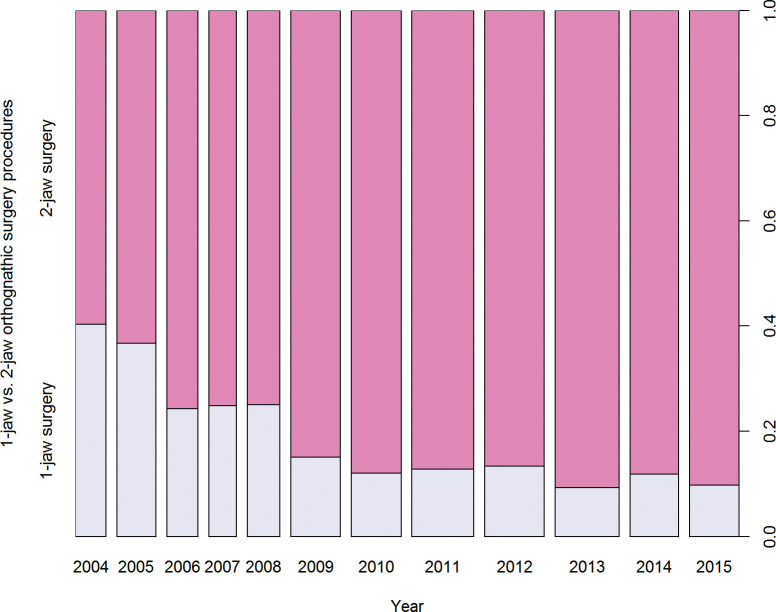
Two-jaw surgeries were by far the most common type of orthognathic surgical treatment. An increase in two-jaw surgeries and a concurrent reduction in one-jaw surgeries was noted in recent years. The percentage increased about 90% since 2010 (Table 2; Figure 2). Comparison of patients undergoing one-jaw and two-jaw surgery revealed no significant difference in patient characteristics reviewed. There were no differences among the patients' sex, age, and proportion of extractions.
Figure 2.
Two-jaw surgeries have become by far the most common type of orthognathic surgical treatment.
For mandibular setbacks, the procedures commonly carried out were sagittal split ramus osteotomies (85% of patients) followed by intraoral vertical ramus osteotomies (12%). Among the maxillary surgical procedures, the Le Fort I osteotomy was the most frequent (82% of patients). Of the additional surgeries, genioplasties were most commonly performed in half of the patients (Tables 2).
The Number of Class III Orthognathic Surgery Patients
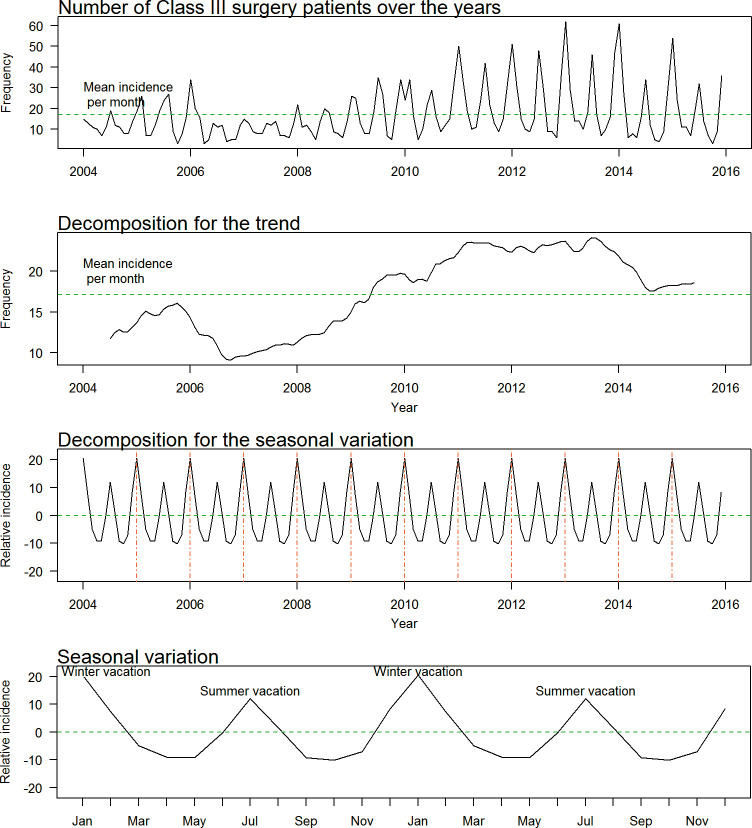
As a result of the time-series analysis, the trend component showed that the number of patients treated for Class III malocclusion seemed to have decreased from the year 2006 to about 2009, followed by a steady increase from 2009 to 2013. A small decrease since 2013 was then observed.
A clear seasonal variation demonstrated peaks every winter and summer. The seasonal variation indicated that the heights of peaks coincided with the 1-month summer and 2-month winter breaks at schools in Korea (Figure 3).
Figure 3.
The time-series analysis results of the number of Class III orthognathic surgery patients treated.
The predicted number of patients that will receive Class III orthognathic surgery in the future is shown in Figure 4.
Figure 4.
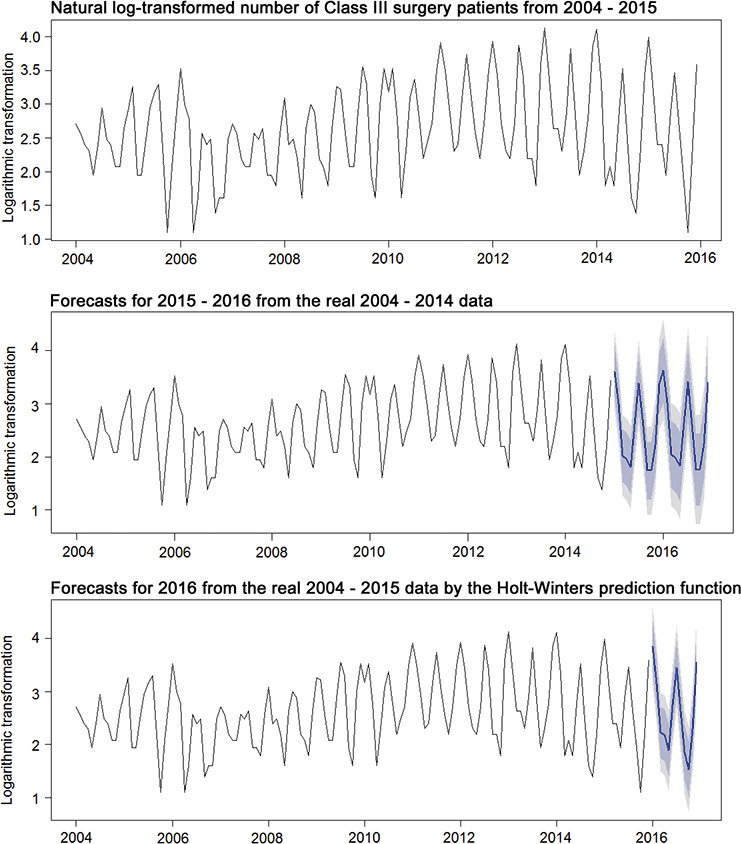
In the log-transformed time series, the size of the seasonal fluctuations and random fluctuations seemed to be roughly constant over time (top). The forecasts (middle) were compared with the real data (bottom). The forecasts were depicted as a solid blue line, the 80% prediction interval as a light blue shaded area, and the 95% prediction interval as a gray shaded area.
Age at Time of Surgery, Pre- and Postsurgical Orthodontic Treatment Time
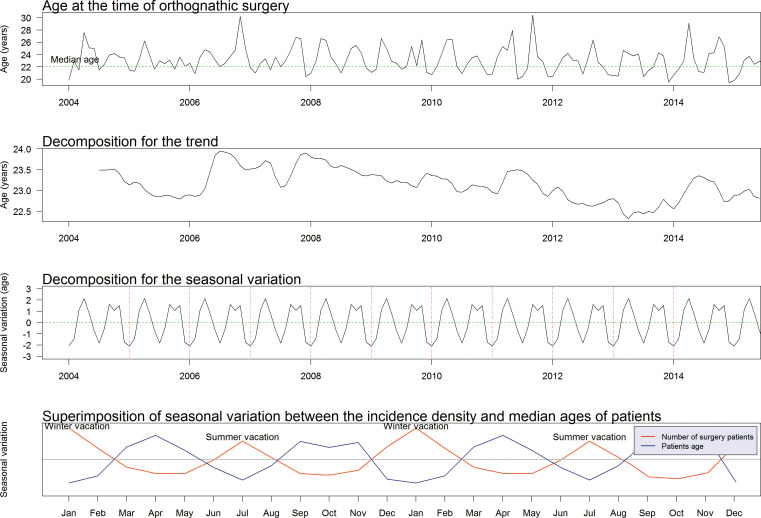
The time-series analysis demonstrated a slightly decreasing trend in the median age over time. The median age at the time of orthognathic surgery was 22 years and did not differ between female and male patients.
The seasonal variation of age showed an opposite pattern compared with the number of patients, which suggested that surgeries were performed for younger patients who were likely college students hoping to receive their surgical procedures during their summer and winter breaks (Figure 5).
Figure 5.
The median age at the time of orthognathic surgery demonstrated a slightly decreasing trend over the years (second from top). A large-scale view of the seasonal variation of age in blue showed an opposite pattern compared with the number of patients in red (bottom).
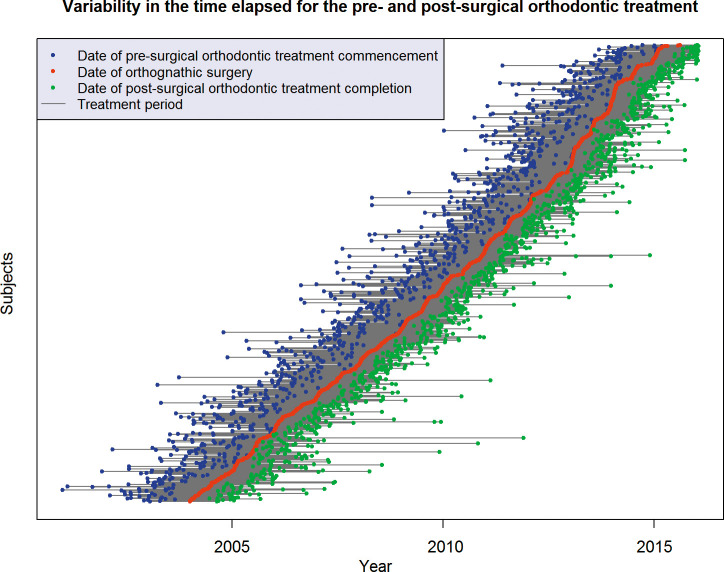
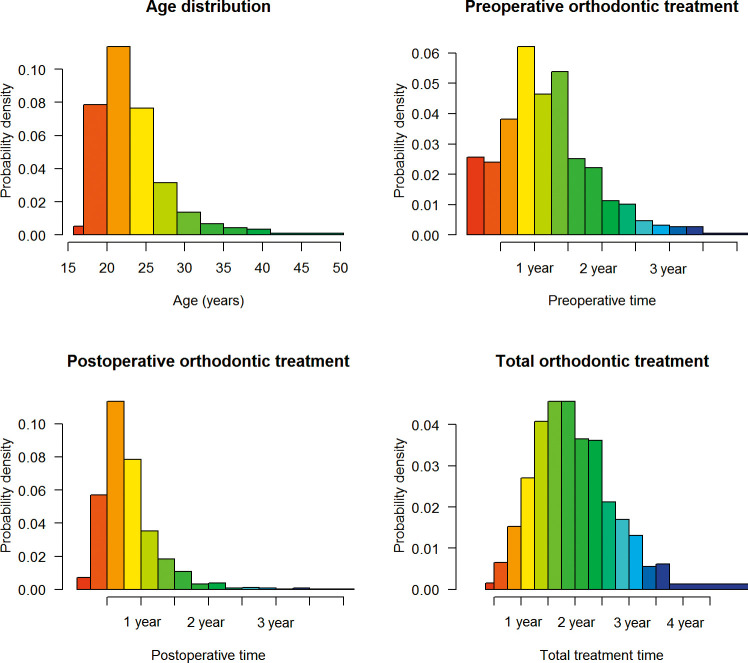
As depicted in Figure 6, the time elapsed for the pre- and postsurgical orthodontic treatment was highly variable for each individual patient undergoing Class III orthognathic surgery. When histograms were depicted, all of the time-related variables demonstrated skewed distribution. The long tails on the right side indicate that several patients were older or received longer orthodontic treatment than usual (Figure 7).
Figure 6.
The time elapsed for the pre- and postsurgical orthodontic treatment time was highly variable.
Figure 7.
All of the time-related variables demonstrated substantially skewed distribution.
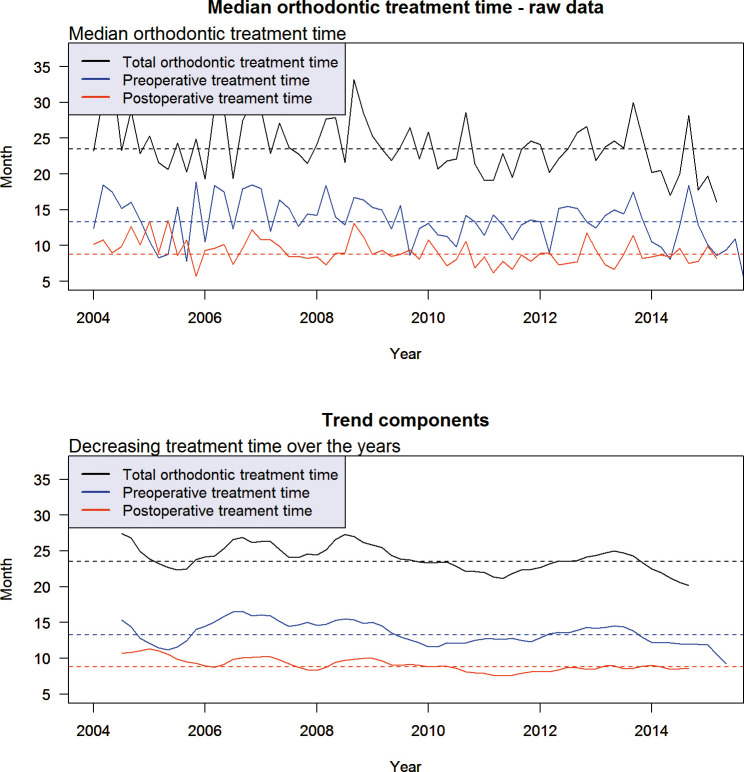
There was neither positive nor negative correlation between pre- and postoperative orthodontic treatment time (P = .4286). The results of the time-series analysis demonstrated that times required for orthodontic treatment before and after Class III orthognathic surgeries have been decreasing over the years (Figure 8).
Figure 8.
The times required for orthodontic treatment before and after Class III orthognathic surgeries have been decreasing over the years.
The median time for orthodontic treatment is shown in Table 3. In cases involving extraction treatment, the duration for the pre- and postoperative orthodontics was extended significantly. This was not different between genders or between one-jaw and two-jaw surgeries.
Table 3.
Supportive Orthodontic Treatment Time (Months) of the Class III Surgery Patients
| Variables |
Median (Months) |
IQR |
P Valuea |
| Preoperative orthodontic treatment time (month) | |||
| Pooled data | 13.4 | (9.3, 18.4) | |
| Extraction | |||
| Nonextraction | 10.7 | (7.4, 15.2) | <.0001 |
| Extraction | 16.6 | (12.4, 21.6) | |
| Surgery | |||
| One-jaw surgery | 14.1 | (10.3, 20.2) | .1456 |
| Two-jaw surgery | 13.3 | (9.0, 18.4) | |
| Postoperative orthodontic treatment time (month) | |||
| Pooled data | 8.7 | (6.5, 11.8) | |
| Extraction | |||
| Nonextraction | 8.3 | (6.1, 10.9) | <.0001 |
| Extraction | 9.4 | (7.2, 12.4) | |
| Surgery | |||
| One-jaw surgery | 8.4 | (6.0, 11.4) | .1139 |
| Two-jaw surgery | 8.8 | (6.6, 11.9) | |
| Total orthodontic treatment time (month) | |||
| Pooled data | 23.4 | (17.9, 30.0) | |
| Extraction | |||
| Nonextraction | 19.3 | (15.3, 25.5) | <.0001 |
| Extraction | 26.7 | (22.1, 32.4) | |
| Surgery | |||
| One-jaw surgery | 22.8 | (18.3, 30.5) | .8476 |
| Two-jaw surgery | 23.5 | (17.8, 29.7) | |
Result of the two-sample Wilcoxon test to compare the treatment time between the two groups; IQR indicates interquartile range.
DISCUSSION
The time-series analysis is a sophisticated statistical method that can reveal greater information than a cursory observation of data. This study is the first attempt to examine the current trends in surgical-orthodontic management using the time-series analysis. Tables 1 through 3 demonstrate the typical way results are presented. However, since the data set in this study is primarily dealing with time-related characteristics, a time-series analysis and its graphic visualization are more informative and easier to understand than multiple tables. In addition, through decomposition, meaningful signals from noise can be extracted by time-series analysis.12,14 Without decomposition, the trend and the seasonal variation would not be as apparent.
The results showed that patients with Class III malocclusion were predominant (roughly 90%). This is expected in Korea whose population has the highest known prevalence of Class III malocclusions (approximately one-fifth of its population).2,4,6,7,16–18 Another contributing reason for the predominance of patients undergoing Class III orthognathic surgery may be that patients with Class III malocclusion are more insecure about the appearance of their facial profile.3,17
In recent years, the increase in the proportion of two-jaw surgeries was substantial. Two-jaw surgeries with mandibular setback (98%) and concomitant maxillary osteotomy (83%) were by far the most common type of surgical procedures. Regarding patient's sex, age, and proportion of extraction orthodontic treatment, there was no significant difference between patients undergoing one-jaw and two-jaw surgery. Since two-jaw surgeries control both jaws, two-jaw surgeries can produce a better profile and occlusion than simple one-jaw surgeries. Two-jaw surgeries can also help prevent aggravating sleep apnea by advancing the maxilla, thus limiting the amount required to set back the mandible.19–21
This study's predominance of two-jaw approaches for correction of skeletal Class III malocclusion may be due to the fact that this investigation was performed in an academic center. Referrals from general dentists play an important role in maintaining the number of orthognathic surgery patients.22 The high incidence of two-jaw surgeries may reflect the greater severity of dentofacial deformities seen in the university dental hospital.11 It is also possible that the more complex cases that need two-jaw surgery have moved from the private practice surgeons to academic oral surgeons at university hospitals.
Over this past decade, the number of male patients was much the same as the female patients, which was similar to previous reports in the United States in 201421 and in Singapore in 2006.1 Meanwhile, a 2014 report in Brazil demonstrated females were more prevalent among orthognathic surgery patients at a ratio of 6:4.3
In this study, the number of surgery patients did not decrease over time. However, in the United States, the situation seemed to be different. For example, a 2014 report from the University of Pennsylvania,23 a 2005 article from Cleveland, Ohio,10 a 2008 US questionnaire survey,11 and the 2014 JCO Study of Orthodontic Diagnosis and Treatment Procedures15 all found a decrease in the number of orthognathic surgery patients. Most oral surgeons, plastic surgeons, and orthodontists in the United States claim that monetary reimbursement from insurance providers was the major reason for the reduction in the number of surgical procedures.11,23 Another major reason may be due to advances in orthodontic techniques, such as the use of orthodontic mini-implants and mini-plates, which may have reduced the necessity of orthognathic surgical procedures.7,15,24,25
In the United States, patients with Class III malocclusion occupied only 30% of the patients seeking orthognathic surgery consultation.26 In Brazil, Class III surgery patients were predominant at 55%,3 and in Singapore, the percentage of patients with Class III malocclusion reached 68%.1
The estimated treatment time is the second most important issue considered by patients, next to treatment fees.27 Orthognathic surgery may lead to prolonged treatment time.28 Table 3 indicates that total treatment time may last longer than 2 years and 2 months for extraction patients, or less than 20 months otherwise. The increased duration of treatment time in patients undergoing orthognathic surgery may simply be a reflection of the severity of the case. Treatment time might have also been affected by students delaying surgery until the school break periods. However, other factors, such as the number of missed appointments and number of primary doctors and/or residents, can affect the treatment time.27
As shown in Figure 7, time variables are likely to be skewed. To have the distribution normalized so that it can be handled by parametric statistical inferential tests, variance stabilizing transformation methods were applied, including logarithmic, square root, and square root of the square root transformations. However, no data transformation methods were successful in obtaining normal Gaussian distribution. This was suggestive of the impossibility in handling the time variables with a simple parametric statistical analysis. In Figure 6, the long and outstanding line spikes are outliers that were supposed to be located in the long right-hand sided tails of the histograms shown in Figure 7. From the clinical point of view, the skewed distribution of all of the time-related variables seemed to reflect the real clinical situation.
After applying the time-series analysis, decreasing patterns of presurgical, postsurgical, and, thus, total orthodontic treatment times were observed (Figure 8). This trend of shorter treatment times is likely due to advances in surgical procedures and improvement of stability after surgery as well as effective orthodontic treatment mechanics.
To further decrease treatment time, a “surgery first” approach has been proposed by some advocates. It is presented as a new concept and purports shorter treatment times. However, before the 1980s, most surgeons did not want orthodontists to perform presurgical orthodontic treatment. In fact, from the beginning, orthognathic surgeries were surgery first. Papers advocating surgery first demonstrate significantly shorter orthodontic treatment. However, there are serious issues regarding the statistical analyses in the papers published by the advocates for surgery first. Most studies of the surgery first approach have a limited number of subjects. The statistical analyses also do not consider the skewed distribution of the time variables. The comparisons would have been more appropriately assessed with nonparametric analyses.
The present study also has several limitations. First, because of Korea's limited ethnic diversity, ethnic influence could not be considered. Second, because all of the orthognathic surgery patients were treated at a single academic institution, it would be impossible to verify or generalize the trends investigated at large. However, it may be also true that, although academic surgeons constitute a relatively small percentage of oral and maxillofacial surgeons nationally, they may perform a significant proportion of the total number of orthognathic surgeries.11
CONCLUSION
Results of the time-series analysis might provide clinicians with some insights into current trends in surgical and orthodontic management.
ACKNOWLEDGMENTS
We would like to thank Dr Richard Donatelli of the University of Florida College of Dentistry, Dr Michael Spoon of the University of Rochester Medical Center, and Dr Steven Lindauer of the Virginia Commonwealth University for their assistance in reviewing and refining the English language of the manuscript.
This study was supported in part by grant 02-2014-0003 from the Seoul National University Dental Hospital Research Fund.
REFERENCES
- 1.Chew MT. Spectrum and management of dentofacial deformities in a multiethnic Asian population. Angle Orthod. 2006;76:806–809. doi: 10.1043/0003-3219(2006)076[0806:SAMODD]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 2.Jung MH. Age, extraction rate and jaw surgery rate in Korean orthodontic clinics and small dental hospitals. Korean J Orthod. 2012;42:80–86. doi: 10.4041/kjod.2012.42.2.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sato FR, Mannarino FS, Asprino L, de Moraes M. Prevalence and treatment of dentofacial deformities on a multiethnic population: a retrospective study. Oral Maxillofac Surg. 2014;18:173–179. doi: 10.1007/s10006-013-0396-3. [DOI] [PubMed] [Google Scholar]
- 4.Lee SJ, Kim TW, Suhr CH. Recognition of malocclusion and orthodontic treatment. Korean J Orthod. 1994;24:193–198. [Google Scholar]
- 5.Lee YS, Suh HY, Lee SJ, Donatelli RE. A more accurate soft-tissue prediction model for Class III 2-jaw surgeries. Am J Orthod Dentofacial Orthop. 2014;146:724–733. doi: 10.1016/j.ajodo.2014.08.010. [DOI] [PubMed] [Google Scholar]
- 6.Suh HY, Lee SJ, Lee YS, et al. A more accurate method of predicting soft tissue changes after mandibular setback surgery. J Oral Maxillofac Surg. 2012;70:e553–e562. doi: 10.1016/j.joms.2012.06.187. [DOI] [PubMed] [Google Scholar]
- 7.Suh HY, Lee SJ, Park HS. Use of mini-implants to avoid maxillary surgery for Class III mandibular prognathic patient: a long-term post-retention case. Korean J Orthod. 2014;44:342–349. doi: 10.4041/kjod.2014.44.6.342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Johnston C, Burden D, Kennedy D, Harradine N, Stevenson M. Class III surgical-orthodontic treatment: a cephalometric study. Am J Orthod Dentofacial Orthop. 2006;130:300–309. doi: 10.1016/j.ajodo.2005.01.023. [DOI] [PubMed] [Google Scholar]
- 9.Bailey LJ, Cevidanes LH, Proffit WR. Stability and predictability of orthognathic surgery. Am J Orthod Dentofacial Orthop. 2004;126:273–277. doi: 10.1016/S0889540604005207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zins JE, Bruno J, Moreira-Gonzalez A, Bena J. Orthognathic surgery: is there a future? Plast Reconstr Surg. 2005;116:1442–1450. doi: 10.1097/01.prs.0000182400.70095.8b. [DOI] [PubMed] [Google Scholar]
- 11.Zins JE, Morrison CM, Gonzalez AM, Altus GD, Bena J. Follow-up: orthognathic surgery. Is there a future? A national survey. Plast Reconstr Surg. 2008;122:555–562. doi: 10.1097/PRS.0b013e31817d543c. [DOI] [PubMed] [Google Scholar]
- 12.Coghlan A. A Little Book of R For Time Series. Release 0.2. 2016 Available at: https://media.readthedocs.org/pdf/a-little-book-of-r-for-timeseries/latest/a-little-book-of-r-for-time-series.pdf Accessed May 1,
- 13.Brockwell PJ, Davis RA. Introduction to Time Series and Forecasting. New York, NY: Springer;; 2002. [Google Scholar]
- 14.R Development Core Team. R: A Language and Environment for Statistical Computing. Vienna, Austria: R Foundation for Statistical Computing;; 2016. [Google Scholar]
- 15.Keim RG, Gottlieb EL, Vogels DS, III, Vogels PB. 2014 JCO study of orthodontic diagnosis and treatment procedures, part 1: results and trends. J Clin Orthod. 2014;48:607–630. [PubMed] [Google Scholar]
- 16.Lee SJ, Kim TW, Nahm DS. Transverse implications of maxillary premolar extraction in Class III presurgical orthodontic treatment. Am J Orthod Dentofacial Orthop. 2006;129:740–748. doi: 10.1016/j.ajodo.2006.02.002. [DOI] [PubMed] [Google Scholar]
- 17.Kim JY, Lee SJ, Kim TW, Nahm DS, Chang YI. Classification of the skeletal variation in normal occlusion. Angle Orthod. 2005;75:311–319. doi: 10.1043/0003-3219(2005)75[311:COTSVI]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 18.Lee YS, Lee SJ, An H, Donatelli RE, Kim SH. Do Class III patients have a different growth spurt than the general population? Am J Orthod Dentofacial Orthop. 2012;142:679–689. doi: 10.1016/j.ajodo.2012.07.009. [DOI] [PubMed] [Google Scholar]
- 19.Boyd SB, Walters AS, Song Y, Wang L. Comparative effectiveness of maxillomandibular advancement and uvulopalatopharyngoplasty for the treatment of moderate to severe obstructive sleep apnea. J Oral Maxillofac Surg. 2013;71:743–751. doi: 10.1016/j.joms.2012.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hsieh YJ, Liao YF. Effects of maxillomandibular advancement on the upper airway and surrounding structures in patients with obstructive sleep apnoea: a systematic review. Br J Oral Maxillofac Surg. 2013;51:834–840. doi: 10.1016/j.bjoms.2012.11.010. [DOI] [PubMed] [Google Scholar]
- 21.Peacock ZS, Lee CC, Klein KP, Kaban LB. Orthognathic surgery in patients over 40 years of age: indications and special considerations. J Oral Maxillofac Surg. 2014;72:1995–2004. doi: 10.1016/j.joms.2014.03.020. [DOI] [PubMed] [Google Scholar]
- 22.Bibona K, Shroff B, Best AM, Lindauer SJ. Communication practices and preferences between orthodontists and general dentists. Angle Orthod. 2015;85:1042–1050. doi: 10.2319/111714-826.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ford B. Trends in orthognathic surgery: a national survey of orthodontists. Paper presented at: 2014 American Association of Oral and Maxillofacial Surgeons Meeting, Honolulu, Hi, USA.
- 24.Lee SJ, Ahn SJ, Lee JW, Kim SH, Kim TW. Survival analysis of orthodontic mini-implants. Am J Orthod Dentofacial Orthop. 2010;137:194–199. doi: 10.1016/j.ajodo.2008.03.031. [DOI] [PubMed] [Google Scholar]
- 25.Lee SJ, Lin L, Kim SH, Chung KR, Donatelli RE. Survival analysis of a miniplate and tube device designed to provide skeletal anchorage. Am J Orthod Dentofacial Orthop. 2013;144:349–356. doi: 10.1016/j.ajodo.2013.03.026. [DOI] [PubMed] [Google Scholar]
- 26.Severt TR, Proffit WR. The prevalence of facial asymmetry in the dentofacial deformities population at the University of North Carolina. Int J Adult Orthodon Orthognath Surg. 1997;12:171–176. [PubMed] [Google Scholar]
- 27.Peppers EC, Leggitt VL, Caruso JM, Neufeld R, Green J. The effect of changes in primary attending doctor coverage frequency on orthodontic treatment time and results. Angle Orthod. 2015;85:1051–1056. doi: 10.2319/120214-866.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Arad I, Jandu J, Bassett P, Fleming PS. Influence of single-jaw surgery vs bimaxillary surgery on the outcome and duration of combined orthodontic-surgical treatment. Angle Orthod. 2011;81:983–987. doi: 10.2319/030211-150.1. [DOI] [PMC free article] [PubMed] [Google Scholar]