Abstract
Aims
Elective orthopaedic services have had to adapt to significant system-wide pressures since the emergence of COVID-19 in December 2019. Length of stay is often recognized as a key marker of quality of care in patients undergoing arthroplasty. Expeditious discharge is key in establishing early rehabilitation and in reducing infection risk, both procedure-related and from COVID-19. The primary aim was to determine the effects of the COVID-19 pandemic length of stay following hip and knee arthroplasty at a high-volume, elective orthopaedic centre.
Methods
A retrospective cohort study was performed. Patients undergoing primary or revision hip or knee arthroplasty over a six-month period, from 1 July to 31 December 2020, were compared to the same period in 2019 before the COVID-19 pandemic. Demographic data, American Society of Anesthesiologists (ASA) grade, wait to surgery, COVID-19 status, and length of hospital stay were recorded.
Results
A total of 1,311 patients underwent hip or knee arthroplasty in the six-month period following recommencement of elective services in 2020 compared to 1,527 patients the year before. Waiting time to surgery increased in post-COVID-19 group (137 days vs 78; p < 0.001). Length of stay also significantly increased (0.49 days; p < 0.001) despite no difference in age or ASA grade. There were no cases of postoperative COVID-19 infection.
Conclusion
Time to surgery and length of hospital stay were significantly higher following recommencement of elective orthopaedic services in the latter part of 2020 in comparison to a similar patient cohort from the year before. Longer waiting times may have contributed to the clinical and radiological deterioration of arthritis and general musculoskeletal conditioning, which may in turn have affected immediate postoperative rehabilitation and mobilization, as well as increasing hospital stay.
Cite this article: Bone Jt Open 2021;2(8):655–660.
Keywords: COVID-19, Arthroplasty, Length of Stay, Coronavirus, Orthopaedics, COVID-19 infection, total hip and knee arthroplasty, arthroplasty surgery, hip and knee arthroplasty, Anesthesiologists, hip and knee arthroplasty, hips, infection, musculoskeletal conditioning, arthritis
Introduction
The NHS underwent major restructuring during the first surge of COVID-19 between March and June 2020. Staff were re-deployed and nonurgent surgery cancelled to create additional capacity for COVID-19 patients and relieve the pressure facing critical care services.1,2 Following easing of measures and recommencement of elective surgery, The British Orthopaedic Association and Royal College of Surgeons produced guidelines to ensure patient safety and to control the flow of patient perioperative pathway.3
Waiting lists for consultations and surgery for elective hip and knee arthroplasty have subsequently soared. The effects of this are not benign. Patients have reported a significant deterioration in their health status and quality of life.4,5 Furthermore, a cohort of patients on the waiting lists who would be willing to accept the increased risks associated with COVID-19 to undergo surgery on an urgent basis.6 There is a real necessity to resume arthroplasty services expediently but safely. Strategies to improve safety include preoperative shielding and COVID-19 testing, ‘green zones’ within hospitals or across entire hospitals, and reducing length of hospital stay.7
Even in the pre-COVID-19 era, reducing patient length of stay (LOS) following total hip and knee arthroplasty was a key priority, with the aim to reduce infection risk from prolonged inpatient contact and expedite rehabilitation. Enhanced recovery and “prehabilitation”, with preoperative input from physiotherapy and occupational therapy, aim to improve the transition to normality postoperatively. Enhanced recovery pathways have shown reduced LOS, improved patient-reported outcomes, fewer complications, and reduced hospital costs,8,9 with some centres even pushing to pursue arthroplasty as a safe day case procedure.10 In this current COVID-19 era this becomes ever more important. Mortality following all trauma and orthopaedic surgery is undoubtedly higher for COVID-19-positive patients, shown in several studies of hip fracture patients.11-16 Reported as between 13% and 20% in trauma patients, nosocomial infection is a significant risk and hence delayed discharge may directly contribute to morbidity.15,16
In this regional elective orthopaedic unit, COVID-19 has affected the patient pathway. There are some positive aspects to this: preoperatively there is now more emphasis on virtual review for anaesthetic assessment and the consent process. Preoperative assessment stratifies patient risk according to their American Society of Anesthesiologists (ASA) Score,17 with patients of ASA 3 and 4 or those for complex surgery including bilateral arthroplasty or revision being deemed high-risk. All referred patients were accepted for surgery after COVID-19, however those at a significantly high risk had increased precautions and appropriate preoperative planning. All arthroplasty patients are provided with a leaflet about the preoperative optimization process at the time of booking, however preoperative physiotherapy and occupational therapy have become largely virtual.18 This helps to reduce the risk of nosocomial infection to individual patients, and prevents transmission in the wider public and among healthcare staff. Follow-up appointments have also been largely telephone-based, and have been well received by most patients, again reducing risk of disease transmission.
Assessing the impact of these changes on length of stay is important not only for patient outcomes and safety, but for nationwide planning for restarting elective services and confronting the waiting list. The aim of this study was to determine the effects of COVID-19 on LOS following hip and knee arthroplasty at a regional elective orthopaedic centre.
Methods
A retrospective cohort data analysis from a high-volume, multi-surgeon, UK elective orthopaedic hospital was performed. As such, there were no pressures for beds for medical patients during either time period. Elective surgery at a high-volume elective orthopaedic centre after the first surge of COVID-19 on 16 June 2020 with a two-week period of non-arthroplasty surgery, following which arthroplasty surgery re-commenced on 1 July 2020.
All patients attending for arthroplasty; including hip arthroplasty, knee arthroplasty, and revision surgery over a six-month period between 1 July 2020 and 24 December 2020 were identified. A cohort between the 1 July 2019 and 24 December 2019 was selected to represent the pre-COVID period.
Following resumption of services a number of changes to the pathway were instituted in line with guidance from the Royal College of Surgeons. Preoperatively these included virtual preoperative assessment to avoid unnecessary additional hospital visits, and virtual and patient-led prehabilitation. All patients were provided with a booklet explaining the procedure and postoperative rehabilitation. Furthermore, patients received an information leaflet regarding risks and complications secondary to COVID-19. The importance of prompt discharge to reduce the risk of hospital-acquired COVID-19 was emphasized from the beginning of the patient pathway. Lists in the post-COVID-19 phase were smaller to allow changes required for COVID-19-safe anaesthesia and increased levels of personal protective equipment. Patients were required to isolate for 14 days pre-op, this subsequently reduced to three days and 14 days postoperatively to reduce COVID-19 risk. Postoperative access to the High Dependency Unit was unchanged.
Data collected included demographics, ASA grade, time from booking to surgery, and LOS. LOS was defined as time from admission to time of discharge). Hospital notes and microbiology testing were reviewed to assess for COVID-19 status while in hospital. Ethical approval was not required. All data had been previously collected and no patient identifiable information was stored. Local audit approval was obtained.
Statistical analysis
Data analysis was performed using the Statistical Package for the Social Sciences (SPSS, v. 23, 2015; IBM, USA). Age was compared between groups assessed using an independent-samples t-test (normally distributed data). Categorical variables (sex, ASA grade) were assessed using a chi-squared test or a Fisher’s exact test. Non-parametric, continuous data (time to surgery, LOS) were assessed using a Mann-Whitney U test. A p-value < 0.05 was defined as statistically significant.
Results
Between 1 July 2019 and 24 December 2019, 1,527 primary and revision hip and knee arthroplasties were undertaken, of which 912 (59.72%) were female and 615 (40.28%) were male. In the six-month period in 2020 following recommencement of elective services, 1,311 primary and revision hip and knee arthroplasties were undertaken. This represents an 86% return to normal activity compared to the same period in 2019. A total of 787 (60.03%) were female and 524 (39.97%) were male. The mean age in 2020 was 68.35 years (standard deviation (SD) 10.61) compared to 69.75 (SD 10.49) before COVID-19, a difference of 1.4 years, which was statistically significant (p = 0.001, independent-samples t-test) See Table I for baseline demographics between 2019 and 2020. Figure 1 shows comparative distribution in ASA grade.
Table I.
Patient baseline demographics.
| Demographic | 2019 | 2020 |
|---|---|---|
| Number | 1,527 | 1,311 |
| Sex F:M, n (%) | 912 (59.72): 615 (40.28) | 787 (60.03): 524 (39/97) |
| Mean age, yrs (SD) | 69.75 (10.49) | 68.35 (10.61) |
| ASA grade (mean) | 2.11 | 2.09 |
ASA, American Society of Anesthesiologists; SD, standard deviation.
Fig. 1.
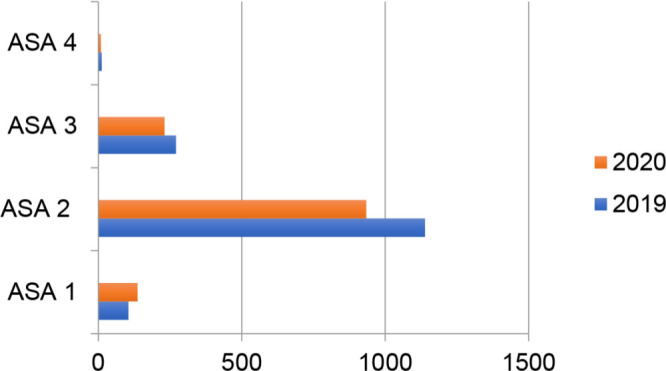
Comparative range of American Society of Anesthesiologists (ASA) grades between 2019 and 2020.
Unsurprisingly, waiting time to surgery has significantly increased from 78 days before the COVID pandemic to 137 days in 2020 (p < 0.001, Mann-Whitney U test). Mean LOS has also increased from 3.07 days (SD 1.92) to 3.56 (SD 2.28), resulting in a statistically significant increase of 0.49 (p < 0.001, Mann-Whitney U test). No patient developed COVID-19 during their hospital stay.
Table II displays LOS stratified by arthroplasty type. This demonstrates an increased effect of length of stay on hips more than knees and revision surgery greater than primary procedures.
Table II.
Length of stay data stratified by type of arthroplasty procedure.
| Year | Type of arthroplasty procedure | LOS | LOS SD | p-value* |
|---|---|---|---|---|
| Hip (primary and revision) | 0.001 | |||
| 2019 | 738 | 2.89 | 1.85 | |
| 2020 | 674 | 3.24 | 2.26 | |
| Hip primary | 0.001 | |||
| 2019 | 697 | 2.84 | 1.77 | |
| 2020 | 646 | 3.24 | 2.24 | |
| Hip revision | 0.519 | |||
| 2019 | 41 | 3.63 | 2.76 | |
| 2020 | 28 | 4.11 | 2.96 | |
| Knee (primary and revision) | 0.001 | |||
| 2019 | 789 | 3.30 | 1.97 | |
| 2020 | 637 | 3.85 | 2.25 | |
| Knee primary | 0.001 | |||
| 2019 | 758 | 3.22 | 1.89 | |
| 2020 | 607 | 3.83 | 2.00 | |
| Knee revision | 0.360 | |||
| 2019 | 31 | 4.52 | 5.64 | |
| 2020 | 30 | 4.53 | 2.78 |
Mann-Whitney U test.
LOS, length of stay; SD, standard deviation.
Table III displays the discharge destination of patients in both time periods. There is a significant reduction in those discharged to NHS or local authority care homes following the COVID-19 surge in 2020 of more than 1% (p = 0.002, Fisher’s exact test), which would be expected to have a direct impact on the length of hospital stay. One patient in 2020 was discharged to a hotel – again this would be expected to contribute to reduced length of stay.
Table III.
Discharge destination of patients across 2019 and 2020.
| Destination | 2019, n (%) | 2020, n (%) |
|---|---|---|
| Home - usual residence | 1,504 (98.49) | 1,305 (99.54) |
| Temporary place of residence (e.g. hotel) | 0 (0) | 1 (0.08) |
| Other provider (general ward) | 4 (0.26) | 2 (0.15) |
| NHS care home | 10 (0.65) | 1 (0.08) |
| Local authority care home | 9 (0.59) | 2 (0.15) |
| Care home (social services/NHS) | 23 (1.5) | 5 (0.38) |
There were no cases of postoperative COVID-19 infection reported within 14 days for the 2020 primary and revision arthroplasty surgery cohort.
Discussion
This study shows that despite an identical inpatient service and an identical, if not trending towards younger and healthier, patient cohort, there has been an increased LOS following recommencement of elective orthopaedic services. Half a day may not seem immediately clinically relevant. However, this would mean the difference between a morning discharge, which would release a bed for the following day’s list, and an evening discharge, which may not.19 This is particularly important for resource planning in general hospitals where resumption of a normal arthroplasty service is further hindered by lack of ring-fenced orthopaedic beds and constant pressure for beds for medical patients. With the majority of previous publications based upon acute hip fracture and trauma populations, this is the first study to review length of stay as an independent factor in a purely elective population.14-16
The reasons for this increase are likely to be complex and difficult to disentangle. We have shown a significantly increased waiting time to surgery. This may have led to a deterioration of disease and reduction in musculoskeletal conditioning.19,20 Studies have shown that an increased wait to surgery is accompanied with increased pain and restriction of function.21 Radiologically more severe disease may also contribute to increased surgical complexity and operating time, as well as increasing the patient’s rehabilitative requirements.22
Prehabilitation of patients is vital in preparing them for both surgery and the postoperative functional recovery. This involves patient education in clinic and by preoperative physiotherapy assessment. Both of these encounters have become largely virtual in the post-COVID-19 era. The efficacy of these virtual interventions in the more elderly population typically suitable for arthroplasty is yet to be determined.23 This may lead to reduced patient engagement due to confusion or apathy, and therefore ultimately impact on the LOS.24 However, they do provide a means of reducing the risk of COVID-19 transmission within patients and the general population, and enable potentially more appointments more regularly for struggling patients.
Social restrictions, including limited use of sports facilities or gyms, as well as reduction in outdoor movement, may also contribute through lack of rehabilitation and add to patient anxiety. Family support at home may be reduced due to national restrictions in travel. Home visits are limited to reduce the risk of contamination, and equipment delivery may be delayed, all of which may hinder expeditious discharge postoperatively. Added to this, high levels of staff sickness and isolation are likely to contribute to potentially a less optimal service than pre-COVID-19 allowed, which has been demonstrated in studies.13,25 Many of these more subtle reasons are beyond the scope of this study but are likely to be the main limitations. Operating time and blood loss, which may indicate increased complexity of surgery, were not evaluated. Added to these potential limitations to early discharge is the potential effect of the postponement of elective operating on surgeons themselves. Studies of human factors have shown that after prolonged periods without practising, skills diminish in pilots. This has not yet been shown to be the case in surgeons, but with this in mind many lists have had reduced numbers of patients added in order to reduce pressure on operating surgeons, anaesthetists, and theatre staff.26,27
Following the introduction of fast-track pathways and improved perioperative pain management strategies, LOS following arthroplasty has dramatically reduced in the recent past. Indeed, with an optimal set-up including physiotherapy, occupational therapy, and social care, as well as minimally invasive operative techniques, some centres even offer a same-day service.10,20 LOS is often reported in the literature as a key marker of quality of patient care, and affects patient experience and satisfaction. Optimizing the LOS to a minimum safe duration not only reduces costs, but also lessens the risk of nosocomial infection, which has become a key factor in maintaining patient safety in the COVID-19 pandemic, and its importance has been well demonstrated in vulnerable hip fracture and emergency general surgical groups.13-16
Many factors can increase the duration of hospital admission, including those related to the patient (advanced age, female sex, raised BMI), and those related to the pathways and procedures. Traditionally patient factors were thought to be the main drivers of prolonged admission, however more recent literature reflects the importance of other systemic factors including the surgeon, operative technique, and site of care.20,28 Given that these non-patient-related factors can affect LOS, it would be reasonable to expect that a global pandemic may influence these, as we have shown. Interestingly we have demonstrated that despite fewer postoperative patients requiring social services or NHS care home admission since COVID-19, which would be expected to assist in expeditious discharge, the LOS is still significantly increased. This may reflect reasons discussed above, such as lack of home support and reduced transport home, but is an interesting discovery.
The NHS in England (NHSE) have provided guidelines to assist in expediting patient discharge from hospital, in order to minimize the risk of contracting COVID-19, as there is a recognized increased mortality risk in inpatients.13 Our findings of increased LOS directly contradict this objective, and may reflect the importance of systemic changes in the patient pathway.
Major arthroplasty is both clinically and financially extremely effective.29 The belief that postponing this ‘elective’ service will not cause any lasting and significant harm is wrong and every effort should be made to resuming normal services. This will require adapting to a new normal as it is likely that COVID-19 will be a barrier for several years to come. With the changes to our patient pathway described, we have shown that resuming elective surgery can be safe. No patients developed COVID-19 while in hospital in a six-month period.
Understanding the reasons behind the increased LOS seen in this study is vitally important for improving efficiency in an even more pressurized service, resource planning, and ultimately improving patient outcomes. The next stage to assess the impact of increased waiting time will be to assess patient-reported outcomes before and after the COVID-19 pandemic, and quantify the clinical and likely radiological deterioration condition from an increased wait for surgery.
We acknowledge that the effect of prolonged waiting times for arthroplasty surgery have not been determined in terms of clinical function with patient-reported outcome measures (PROMs), or radiologically in terms of disease progression, however authors have demonstrated that patients reported increasing pain with increasing wait, to the extent they are willing to risk being inoculated with COVID-19. A prospective study evaluating PROMs and radiological severity is required, and the authors are endeavouring to perform this.
In conclusion, in the post COVID-19 era, it is vital to manage the flow of the arthroplasty patient pathway. We demonstrate that LOS in the post-COVID-19 cohort is significantly increased, despite a younger cohort and an increased importance on expeditious discharge. This may have a detrimental impact on clinical and radiological disease, and further delay rehabilitation. As we ready ourselves for resuming elective services following the second, even larger COVID-19 surge, prioritization of arthroplasty patients must be made paramount. Virtual pre- and post-surgical assessment may assist in expediting the surgical flow and service delivery in the longer term.
Take home message
- In the post COVID-19 era, it is vital to manage the flow of the arthroplasty patient pathway.
- Longer waiting times may have contributed to the clinical and radiological deterioration of arthritis and general musculoskeletal conditioning, which may in turn have affected immediate postoperative rehabilitation and mobilization, as well as increased hospital stay.
Footnotes
Author contributions: G. Green: Conceptualized the study, Wrote and edited the manuscript.
Y. Vyrides: Collected the data, Edited the manuscript.
S. Abbott: Wrote and edited the manuscript.
I. Afzal: Collected the data, Conducted the statistical analysis.
D. Kader: Conducted the final editing process.
S. Radha: Conceptualized the study idea, Analyzed the data, Edited the manuscript.
Funding statement: No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.
Open access funding: Open access funding for this study was provided by the South West London Elective Orthopaedic Centre.
References
- 1.NHS England . Redeploying your secondary care medical workforce safely. https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/C0666_Redeploying-your-secondary-care-medical-workforce-safely-v-2_14July.pdf (date last accessed last accessed 23/06/2020 at 22:25).
- 2.NHS England . Clinical guide for the management of surge during the coronavirus pandemic: rapid learning. https://www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/C0167-specialty-guide-surge-based-on-current-hospital-experience-v2.pdf (date last accessed 23 June 2020).
- 3.Royal College of Surgeons . COVID-19 toolkit: guidance for recovery of surgical services. recovery of surgical services during and after COVID-19 — Royal College of Surgeons. https://www.rcseng.ac.uk/ (date last accessed 2021).
- 4.Huntley D, Ashdown T, Harland W, Ashdown T, Harland W, Anakwe R. Waiting lists for symptomatic joint arthritis are not benign. Bone Jt Open. 2020;1(8):508–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Scott CEH, MacDonald DJ, Howie CR. 'Worse than death' and waiting for a joint arthroplasty. Bone Joint J. 2019;101-B(8):941–950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Madanipour S, Al-Obaedi O, Ayub A, Iranpour F, Subramanian P. Resuming elective hip and knee arthroplasty in the COVID-19 era: a unique insight into patient risk aversion and sentiment. Ann R Coll Surg Engl. 2021;103(2):104-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kader N, Clement ND, Patel VR, Caplan N, Banaszkiewicz P, Kader D. The theoretical mortality risk of an asymptomatic patient with a negative SARS-CoV-2 test developing COVID-19 following elective orthopaedic surgery. Bone Joint J. 2020;102-B(9):1256–1260. [DOI] [PubMed] [Google Scholar]
- 8.Larsen K, Hansen TB, Thomsen PB, Christiansen T, Søballe K. Cost-Effectiveness of accelerated perioperative care and rehabilitation after total hip and knee arthroplasty. J Bone Joint Surg Am. 2009;91-A(4):761–772. [DOI] [PubMed] [Google Scholar]
- 9.Hu Z-C, He L-J, Chen D, ZC H, et al. An enhanced recovery after surgery program in orthopedic surgery: a systematic review and meta-analysis. J Orthop Surg Res. 2019;14(1):77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lazic S, Boughton O, Kellett CF, Kader DF, Villet L, Rivière C. Day-Case surgery for total hip and knee replacement: how safe and effective is it? EFORT Open Rev. 2018;3(4):130–135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Karayiannis PN, Roberts V, Cassidy R, et al. 30-Day mortality following trauma and orthopaedic surgery during the peak of the COVID-19 pandemic: a multicentre regional analysis of 484 patients. Bone Jt Open. 2020;1(7):392–397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Clement ND, Hall AJ, Makaram NS, et al. IMPACT-Restart: the influence of COVID-19 on postoperative mortality and risk factors associated with SARS-CoV-2 infection after orthopaedic and trauma surgery. Bone Joint J. 2020;102-B(12):1774–1781. [DOI] [PubMed] [Google Scholar]
- 13.COVIDSurg Collaborative . Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396(10243):27–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clement ND, Ng N, Simpson CJ, et al. The prevalence, mortality, and associated risk factors for developing COVID-19 in hip fracture patients: a systematic review and meta-analysis. Bone Joint Res. 2020;9(12):873–883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hall AJ, Clement ND, Farrow L, et al. IMPACT-Scot report on COVID-19 and hip fractures. Bone Joint J. 2020;102-B(9):1219–1228. [DOI] [PubMed] [Google Scholar]
- 16.Kayani B, Onochie E, Patil V, et al. The effects of COVID-19 on perioperative morbidity and mortality in patients with hip fractures. Bone Joint J. 2020;102-B(9):1136–1145. [DOI] [PubMed] [Google Scholar]
- 17.Saklad M. Grading of patients for surgical procedures. Anesthesiol. 1941;2(5):281–284. [Google Scholar]
- 18.South West London Elective Orthopaedic Centre . Information on surgery during the COVID-19 pandemic.
- 19.Vergara I, Bilbao A, Gonzalez N, Escobar A, Quintana JM. Factors and consequences of waiting times for total hip arthroplasty. Clin Orthop Relat Res. 2011;469(5):1413–1420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McCulloch R, Cottingham P, Chrismas B, Pearce O. Is it time we changed how we measure length of stay for hip and knee arthroplasty? J Am Acad Orthop Surg Glob Res Rev. 2017;1(6):e032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pietrzak JRT, Maharaj Z, Erasmus M, Sikhauli N, Cakic JN, Mokete L. Pain and function deteriorate in patients awaiting total joint arthroplasty that has been postponed due to the COVID-19 pandemic. World J Orthop. 2021;12(3):152–168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lizaur-Utrilla A, Martinez-Mendez D, Miralles-Muñoz FA, Marco-Gomez L, Lopez-Prats FA. Negative impact of waiting time for primary total knee arthroplasty on satisfaction and patient-reported outcome. Int Orthop. 2016;40(11):2303–2307. [DOI] [PubMed] [Google Scholar]
- 23.Youlden DJ, Dannaway J, Enke O. Radiographic severity of knee osteoarthritis and its relationship to outcome post total knee arthroplasty: a systematic review. ANZ J Surg. 2020;90(3):237–242. [DOI] [PubMed] [Google Scholar]
- 24.Yeşilyaprak SS, Yıldırım Meriç Şenduran, Tomruk M, Ertekin Özge, Algun ZC, Candan Algun Z. Comparison of the effects of virtual reality-based balance exercises and conventional exercises on balance and fall risk in older adults living in nursing homes in turkey. Physiother Theory Pract. 2016;32(3):191–201. [DOI] [PubMed] [Google Scholar]
- 25.Oussedik S, Zagra L, Shin GY, D'Apolito R, Haddad FS. Reinstating elective orthopaedic surgery in the age of COVID-19. Bone Joint J. 2020;102-B(7):807–810. [DOI] [PubMed] [Google Scholar]
- 26.Ferrara P, Rabini A, Maggi L, et al. Effect of pre-operative physiotherapy in patients with end-stage osteoarthritis undergoing hip arthroplasty. Clin Rehabil. 2008;22(10-11):977–986. [DOI] [PubMed] [Google Scholar]
- 27.NHS . Sickness Absence Rates May 2020, Provisional Statistics - NHS Digital.
- 28.Dexter F, Epstein RH, Elhakim M, Loftus RW, Seering MS. Erratum for: strategies for daily operating room management of ambulatory surgery centers following resolution of the acute phase of the COVID-19 pandemic. J Clin Anesth. 2020;66:109936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jenkins PJ, Clement ND, Hamilton DF, Gaston P, Patton JT, Howie CR. Predicting the cost-effectiveness of total hip and knee replacement: a health economic analysis. Bone Joint J. 2013;95-B(1):115–121. [DOI] [PubMed] [Google Scholar]


