Abstract
Aims
It is important to understand the rate of complications associated with the increasing burden of revision shoulder arthroplasty. Currently, this has not been well quantified. This review aims to address that deficiency with a focus on complication and reoperation rates, shoulder outcome scores, and comparison of anatomical and reverse prostheses when used in revision surgery.
Methods
A Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) systematic review was performed to identify clinical data for patients undergoing revision shoulder arthroplasty. Data were extracted from the literature and pooled for analysis. Complication and reoperation rates were analyzed using a meta-analysis of proportion, and continuous variables underwent comparative subgroup analysis.
Results
A total of 112 studies (5,379 shoulders) were eligible for inclusion, although complete clinical data was not ubiquitous. Indications for revision included component loosening 20% (601/3,041), instability 19% (577/3,041), rotator cuff failure 17% (528/3,041), and infection 16% (490/3,041). Intraoperative complication and postoperative complication and reoperation rates were 8% (230/2,915), 22% (825/3,843), and 13% (584/3,843) respectively. Intraoperative and postoperative complications included iatrogenic humeral fractures (91/230, 40%) and instability (215/825, 26%). Revision to reverse total shoulder arthroplasty (TSA), rather than revision to anatomical TSA from any index prosthesis, resulted in lower complication rates and superior Constant scores, although there was no difference in American Shoulder and Elbow Surgeons scores.
Conclusion
Satisfactory improvement in patient-reported outcome measures are reported following revision shoulder arthroplasty; however, revision surgery is associated with high complication rates and better outcomes may be evident following revision to reverse TSA.
Cite this article: Bone Jt Open 2021;2(8):618–630.
Keywords: Total shoulder arthroplasty, Replacement, Revision, Systematic review and meta-analysis, Complications, Outcomes, revision shoulder arthroplasty, total shoulder arthroplasty, revision surgery, postoperative complications, intraoperative complications, Shoulder, patient-reported outcome measures (PROMs), rotator cuff, American Shoulder and Elbow Surgeons (ASES) score, humeral fractures
Introduction
The prevalence of shoulder arthroplasty has increased dramatically over the past decade, with a projected growth rate exceeding that for lower limb arthroplasty.1 This is in part due to arthroplasty becoming the accepted primary or salvage treatment for diverse pathologies including arthritis, fractures, avascular necrosis, and rotator cuff tears. Furthermore, the success of modern shoulder arthroplasty and advances in prosthetic design has led to an expansion of shoulder arthroplasty surgery in younger patients.2
The lifetime risk of revision following shoulder arthroplasty is reported to be as high as one in four, with patients aged 60 and under having a fourfold higher risk of revision compared to those over 85 years of age.2 Hence, the exponential rise in primary surgery has been associated with a corresponding increase in the demand for revision surgery. However, compared to hip and knee arthroplasty, this burden remains relatively low, which means most individual surgeons have limited experience and outcome data on revision arthroplasty.
Common indications for revision include glenoid wear, component loosening, infection, periprosthetic fracture, cuff failure, and instability. Many of the principles used in revision shoulder arthroplasty are derived from the more extensive lower limb literature, however revision shoulder arthroplasty poses some specific challenges such as the unique microbiological environment of the shoulder; the reliance on coordinated muscle function for stability; the proximity of neurovascular structures; and the relatively lower bone stock available.
There is currently no consensus for uniform implant selection in revision surgery, although there is a trend towards reverse total shoulder arthroplasty (TSA) as the favoured option.3,4 Nevertheless, anatomical TSA continues to have a role in revision surgery for particular modes of failure where the rotator cuff remains intact.5
Although we know that inferior functional results6-10 and a higher incidence of complications (up to 50%)10-12 are associated with revision compared to primary shoulder arthroplasty, there is sparse data available on the specific outcomes and complications of revision arthroplasty. A recent systematic review provides some insight into this area, with comparisons made between European and North American practice.13 The authors identified similar practice in most aspects of revision shoulder arthroplasty between European and North American surgeons with a 17% reported overall complication rate.
This study aimed to comprehensively search the literature and present the relevant collated data on revision shoulder arthroplasty with a focus on complication and reoperation rates, shoulder outcome scores, and comparison of these metrics between anatomical and reverse TSA, when used in revision surgery.
Methods
This systematic review was registered on the PROSPERO database (Registration ID: CRD42019150698) and conducted as per the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) protocol.14
Search and data collection
All English language papers reporting clinical data for revision shoulder arthroplasty were included in this study. Abstracts from scientific meetings, unpublished reports, case reports, and review articles were excluded. Patients with a minimum of 24 months’ follow-up after revision surgery were included in quantitative synthesis of PROMs, postoperative complication data, and reoperation data. Patients with inadequate or no follow-up were included for the purpose of studying intraoperative complications but were excluded when synthesizing postoperative outcomes.
Embase and MEDLINE databases were searched on 6 April 2021 for all articles published since 2001. References of all included studies were subsequently screened for further articles eligible for inclusion. For search strategy employed see Supplementary Material. Search results and included papers were managed using spreadsheet software. One reviewer (VR) screened study titles followed by abstract and full manuscript review, where necessary, to determine appropriateness for inclusion. Three reviewers (RJM, MD, JP) assessed identified studies for confirmation of eligibility and any disagreement was resolved by consensus. One reviewer (VR) performed initial data collation followed by cross-checking by a second reviewer (MD).
Basic data collected from individual studies, where reported, included cohort demographics, indication for revision, index surgery, final implant used in revision, pre- and postoperative shoulder outcome scores, intra- and postoperative complications, and reoperations. Due to inconsistency in reporting terminology, some indications and complications were grouped to enable easier understanding and classification of reported data (see Table I). In studies that reported outcomes for the same cohort at multiple timepoints, only data from the most recent timepoint was included.
Table I.
Grouping of selected complications used to classify indications and outcomes.
| Complication | Description |
|---|---|
| Component loosening | Glenoid or humeral component dissociation, screw failure, malposition, migration, or material disassembly following arthroplasty. |
| Instability | Recurrent dislocations due to a defect in the prosthesis |
| Rotator cuff failure | Insufficiency or tear in rotator cuff muscles |
| Glenoid failure | Glenoid disease following hemiarthroplasty (arthritis/erosion/arthrosis) or glenoid component failure (polyethylene wear or broken hardware) following anatomical TSA |
| Baseplate failure | Polyethylene wear or broken hardware in baseplate of glenoid component following reverse TSA |
| Fracture sequalae | Nonunion, malunion, or failure following fracture fixation |
| Radiological complications* | Component or bone lucency, subsidence, scapular notching, or radiological loosening. |
| Wound problems | Wound infection or impaired healing post-surgery. |
Includes radiological inconsistencies reported as a complication and requiring reintervention as a result. Radiological outcomes were not studied in this systematic review.
TSA, total shoulder arthroplasty.
Methodological Index for Non-Randomised Studies (MINORS) was chosen for risk of bias assessment; this was performed at outcome level. Each individual study included in this review was scored for its methodological quality and risk of bias using the 12-item index provided by MINORS,15 which deems ideal global scores of 16 and 24 for non-comparative and comparative studies, respectively.
Statistical analysis
Pooled descriptive analysis of collected data was used to understand patient demographic details, indications for revision, and frequency of different index and revision surgical procedures. Complication rates used the number of patients with at least one complication/reoperation as the numerator and total number of patients studied as the denominator. Results were pooled across different studies using a meta-analysis of proportion;16 which involves using a Freeman-Tukey transformation to calculate an overall rate, weighted according to the reported rates and sample size of each study. This was performed using MedCalc software (Belgium) and random-effects model was used to account for variability in effect estimates. Results are presented in the form of a forest plot, with each study represented by its weight, reported rate and 95% confidence interval (95% CI). Heterogeneity testing employed the I2 statistic, describing the percentage variation between studies;17 a value greater than 50% was considered ‘substantial heterogeneity’ for the purpose of this study.
PROMs were studied using minimal clinically important difference (MCID), a measure of responsiveness that represents the smallest subjective difference in shoulder outcome score corresponding to a clinically important change to the patient.18 Change in mean score over follow-up duration for each reported study was used to identify proportion of studies that achieved MCID.
Sub-groups were defined as 1) shoulders revised to reverse TSA and 2) shoulders revised to anatomical TSA. Complication rates were compared using chi-squared and Fisher’s exact test; with results summarized using percentages and odds ratio (OR). OR greater than 2 with a 95% CI not spanning null value (OR = 1) was considered clinically relevant. Shoulder outcome scores were pooled across reported studies using frequency-weighted means and compared between sub-groups using independent-samples t-test. Statistical tests were performed using SPSS software v26.0.0.0 (USA) and a p-value less than 0.05 was considered statistically significant for this study.
Results
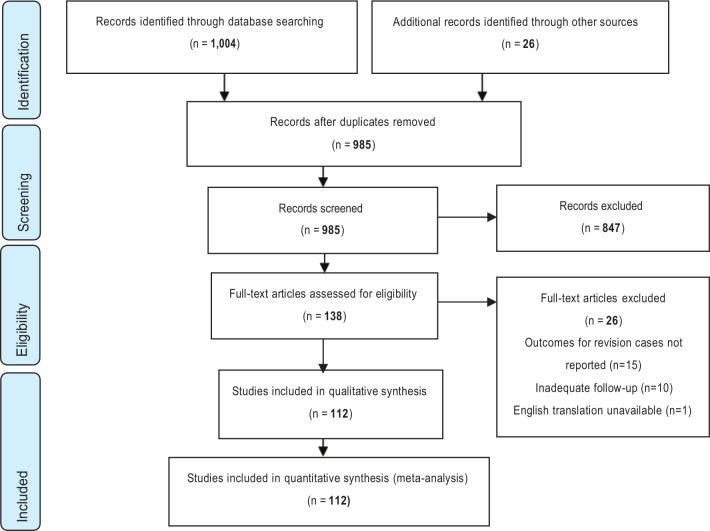
Overall, 112 studies were deemed eligible for inclusion (Figure 1); 84 were level IV studies, 27 level III, and one level II, all of which reported clinical data for patients undergoing revision shoulder arthroplasty. All studies included cohorts with adequate follow-up periods apart from one,19 which reported intraoperative data for a group of patients not followed up after revision surgery. This study was included in the systematic review as it was deemed eligible to study intraoperative complications; but was excluded for the purpose of analyzing postoperative outcomes. For a list of individual studies with cohort size and reported complications see Supplementary Table i.
Fig. 1.
Flowchart outlining the process of study selection for this systematic review.
A total of 57 of 112 (51%) studies achieved ideal global MINORS scores. Scores from the remaining studies ranged from 12 to 15 for level IV and 19 to 23 for level III studies. All studies were deemed eligible to be included in quantitative synthesis; for individual study scores see Supplementary Material II.
Overall, 5,379 shoulders in 5,225 patients having undergone revision shoulder arthroplasty were included. Complete demographic data for patients undergoing revision was reported in 85 out of 112 (76%) studies. Pooled demographic and clinical data with indications for revision are presented in Table II. The mean age of patients at revision surgery was 67 years (21 to 84) and 60% of patients were female. Follow-up duration was reported in 3,240 of 3,474 (93%) shoulders with adequate follow-up; the cohort was followed up for a mean of 48 months (24 to 113). Of the shoulders with available data regarding index and revision procedures (See Table II), the most common index procedure was hemiarthroplasty (50%, 1,645/3,295) and the majority of shoulders were revised to reverse TSA (67%, 3,341/5,004). Of the shoulders with available data regarding indication for revision (see Table II), the most common indications were component loosening (20%, 601/3,041), instability (19%, 577/3,041), rotator cuff failure (17%, 528/3,041), and infection (16%, 490/3,041).
Table II.
Demographic data of the pooled cohort.
| Variable | Reported studies (n = 112) |
Shoulders with available data (n = 5,379) | Result | % | |
|---|---|---|---|---|---|
| Mean age at revision, yrs (range) | 105* | 5,225 | 67 (21 to 84) | ||
| Mean follow-up, mths | 107† | 3,609 | 48 | ||
| Sex | 101‡ | 4,862 | Female | 2,925/4,862 | 60 |
| Male | 1,910/4,862 | 40 | |||
| Index surgery | 100§ | 3,295 | Hemiarthroplasty | 1,645/3,295 | 50 |
| Anatomical TSA | 1,152/3,295 | 35 | |||
| Revere TSA | 402/3,295 | 15 | |||
| Revision surgery | 109¶ | 5,004 | Reverse TSA | 3,341/5,004 | 67 |
| Anatomical TSA | 1,213/5,004 | 24 | |||
| Hemiarthroplasty | 348/5,004 | 7 | |||
| Resection arthroplasty | 43/5,004 | <1 | |||
| Antibiotic spacer implantation | 41/5,004 | <1 | |||
| Indication for revision surgery | 90** | 3,041 | Component loosening | 601/3,041 | 20 |
| Instability | 577/3,041 | 19 | |||
| Rotator cuff failure | 528/3,041 | 17 | |||
| Infection | 490/3,041 | 16 | |||
| Glenoid failure | 401/3,041 | 13 | |||
| Baseplate failure | 83/3,041 | 3 | |||
| Pain and stiffness | 62/3,041 | 2 | |||
| Fracture sequelae | 59/3,041 | 2 | |||
| Periprosthetic fracture | 58/3,041 | 2 | |||
| Tuberosity resorption | 18/3,041 | < 1 | |||
Intraoperative complications were reported in 50 of 112 studies (45%). Of 2,915 shoulders, 230 (8%) had an intraoperative complication during revision shoulder arthroplasty; reported complications are presented in Table III. Of the 230 intraoperative complications, 162 (70%) were iatrogenic fractures and of these, 91 of 162 (56%) involved the humerus. The weighted global intraoperative complication rate was 7.9% (95% CI 5.5 to 10.6; see Supplementary Material III) with substantial heterogeneity between studies (I2 = 77.7% (95% CI 70.9 to 82.9)).
Table III.
Reported intraoperative complications during revision shoulder arthroplasty.
| Intraoperative complication | Reported (n = 230) | % |
|---|---|---|
| Iatrogenic humeral fracture | 91/230 | 40 |
| Iatrogenic glenoid fracture | 4/230 | 2 |
| Unspecified iatrogenic fracture | 67/230 | 29 |
| Cement extrusion | 17/230 | 7 |
| Shaft perforation | 10/230 | 4 |
| Nerve injury | 9/230 | 4 |
| Humerus fissure | 6/230 | 3 |
| Antibiotic related complication | 3/230 | 1 |
| Iatrogenic cuff tears | 2/230 | < 1 |
| Bony window | 1/230 | < 1 |
| Vascular injury | 1/230 | < 1 |
| Unspecified intraoperative complication | 19/230 | 9 |
Postoperative complications were reported in 111 of 112 studies. Of 3,843 shoulders included in this analysis, 825 (21%) reported a postoperative complication following revision shoulder arthroplasty; reported complications are presented in Table IV. Instability was the most commonly reported postoperative complication (26%, 215/825), followed by component loosening (19%, 158/825), infection (16%, 129/825), and periprosthetic fracture (12%, 100/825). The weighted global postoperative complication rate was 21.9% (95% CI 19.2 to 24.7, see Supplementary Material IV) with substantial heterogeneity between studies (I2 = 76.4%, 95% CI 71.7 to 80.2).
Table IV.
Reported postoperative complications following revision shoulder arthroplasty.
| Postoperative complication | Reported (total = 825) | % |
|---|---|---|
| Instability | 215/825 | 27 |
| Component loosening | 163/825 | 17 |
| Infection | 118/825 | 14 |
| Periprosthetic fracture | 101/825 | 13 |
| Rotator cuff failure | 52/825 | 7 |
| Pain and stiffness | 46/825 | 6 |
| Haematoma | 32/825 | 4 |
| Radiological complications | 12/825 | 2 |
| Wound problems | 12/825 | 1 |
| Glenoid failure | 17/825 | 1 |
| Baseplate failure | 11/825 | 1 |
| Nerve injuries | 9/825 | 1 |
| Fracture sequelae | 8/825 | 1 |
| Graft failure | 6/825 | < 1 |
| Heterotopic ossification | 3/825 | < 1 |
| Deltoid insufficiency | 2/825 | < 1 |
| Cement extrusion | 2/825 | < 1 |
| Pulmonary embolism | 2/825 | < 1 |
| Arthrofibrosis | 1/825 | < 1 |
| Deep vein thrombosis | 1/825 | < 1 |
| Pectoralis major rupture | 1/825 | < 1 |
| Subacromial impingement | 1/825 | < 1 |
| Hemarthrosis | 1/825 | < 1 |
| Unspecified postoperative complication | 9/825 | 1 |
Reoperation rate was reported in 111 of 112 studies. Of 3,843 shoulders, 584 (15%) shoulders underwent reoperation following revision shoulder arthroplasty; reported reoperations are presented in Table V. Of 533 reoperations, 232 (40%) reoperations stated need for revision of one or both components of the shoulder prosthesis, 45 (8%) reoperations did not require component revision, and 307 (58%) reoperation procedures were not specified. The weighted global reoperation rate was 13.3% (95% CI 11.5 to 15.3, see Supplementary Material IV) with substantial heterogeneity among studies (I2 = 66.1% (95% CI 58.7 to 72.2)).
Table V.
Reported reoperations following revision shoulder arthroplasty.
| Reoperation | Reported (total = 584) | % |
|---|---|---|
| Revision shoulder arthroplasty | 181/584 | 40 |
| Open/closed reduction under general anaesthetic | 11/584 | 2 |
| Irrigation and debridement | 8/584 | 1 |
| Arthroscopic excision | 8/584 | 1 |
| Open reduction internal fixation | 7/584 | 1 |
| Surgical drainage of haematoma | 5/584 | 1 |
| Subscapularis repair | 2/584 | < 1 |
| Subacromial decompression | 1/584 | < 1 |
| Surgical neurolysis | 1/584 | < 1 |
| Cement removal | 1/584 | < 1 |
| Open excision of heterotopic ossification | 1/584 | < 1 |
| Reoperation not specified | 307/584 | 58 |
Shoulder outcome scores were reported pre- and postoperatively in 55 of 112 (49%) studies; these are presented in Table VI. The American Shoulder and Elbow Surgeons (ASES) score55 was reported in 27 of 55 (49%) studies and Constant score56 was reported in 28 of 55 (51%) studies. MCID was achieved in 48 of 55 (87%) studies; this required a 21- and eight-point improvement in ASES and Constant scores respectively.18,57 ASES score was reported in 21 of 48 (44%) studies that achieved MCID and Constant score was reported in 27 of 48 (56%) studies that achieved MCID.
Table VI.
Functional outcome scores before and after revision shoulder arthroplasty.
| Mean ASES score | Mean Constant scores | ||||||||
|---|---|---|---|---|---|---|---|---|---|
|
Author and year
of publication |
Cases | Preop | Postop |
Change in
score > MCID? |
Author and year
of publication |
Cases | Preop | Postop |
Change in
score > MCID? |
| Cox et al58 | 72 | 33.7 | 51.1 | No | Jaiswal et al59 | 26 | 35.06 | 59.69 | Yes |
| Crosby et al60 | 102 | 32.56 | 58.7 | Yes | Werner et al38 | 50 | 11.1 | 39.5 | Yes |
| Hernandez et al61 | 65 | 21.4 | 67.7 | Yes | Antoni et al62 | 37 | 26.9 | 53.3 | Yes |
| Kohan et al63 | 19 | 35 | 65 | Yes | Cisneros et al64 | 40 | 16.79 | 58.09 | Yes |
| Otto et al50 | 35 | 24.4 | 40.8 | No | Ortmaier et al65 | 50 | 18.5 | 49.3 | Yes |
| Stephens et al28 | 58 | 45.6 | 52.9 | No | Wieser et al66 | 45 | 24 | 45 | Yes |
| Kelly et al48 | 30 | 54.8 | 71.8 | No | Melis et al67 | 37 | 31.6 | 75.6 | Yes |
| Deutsch et al68 | 32 | 34 | 39 | No | Valenti et al69 | 30 | 24.47 | 51.57 | Yes |
| Walker et al 201270 | 22 | 38.5 | 67.5 | Yes | Kany et al71 | 29 | 27 | 60 | Yes |
| Weber-Spickschen et al72 | 15 | 12 | 36 | Yes | Bonnevialle et al73 | 42 | 54.2 | 79.3 | Yes |
| Holcomb et al74 | 14 | 36 | 70 | Yes | Werner et al75 | 14 | 8.9 | 41 | Yes |
| Lee et al40 | 12 | 32.25 | 64.17 | Yes | Farshad et al30 | 37 | 23 | 46 | Yes |
| Budge et al76 | 15 | 38.2 | 68.3 | Yes | Flury et al21 | 21 | 16.6 | 56 | Yes |
| Schubkegel et al77 | 14 | 33 | 72 | Yes | Beekman et al78 | 5 | 50.2 | 64.2 | Yes |
| Wiater et al53 | 44 | 41.8 | 59.9 | No | Postacchini et a51 | 16 | 38.7 | 50.6 | Yes |
| Stephens et al52 | 32 | 29.7 | 70.6 | Yes | Hoffelner et al22 | 11 | 24 | 40 | Yes |
| Levy et al79 | 29 | 22.3 | 52.1 | Yes | Geervilet et al80 | 11 | 67.1 | 96.1 | Yes |
| Patel et al81 | 28 | 24 | 66 | Yes | Natera et al82 | 23 | 24.26 | 84 | Yes |
| Chacon et al20 | 25 | 31.7 | 69.4 | Yes | Valenti et al69 | 10 | 39.4 | 71 | Yes |
| Levy et al83 | 19 | 29.1 | 61.2 | Yes | Castagna et al84 | 26 | 25.28 | 47.88 | Yes |
| Holschen et al85 | 28 | 19.2 | 58.5 | Yes | Muh et al86 | 26 | 25.2 | 27.3 | No |
| Cuff et al87 | 17 | 31.9 | 57.0 | Yes | Hartel et al88 | 19 | 19.8 | 38.7 | Yes |
| Johnston et al32 | 13 | 19.6 | 58.9 | Yes | Gohlke et al47 | 25 | 12.67 | 45.08 | Yes |
| Andersen et al25 | 5 | 32 | 54.4 | Yes | Pellegrini et al89 | 21.7 | 39.5 | Yes | |
| Franke et al36 | 123 | 31 | 55 | Yes | Grubhofer et al90 | 48 | 26.8 | 43 | Yes |
| Gorman et al44 | 98 | 35 | 58 | Yes | Crosby et al27 | 73 | 24 | 71.91 | Yes |
| Franke et al35 | 113 | 30 | 59 | Yes | Elhassan et al91 | 21 | 27.80 | 65.09 | Yes |
| De Wilde et al92 | 4 | 14 | 66 | Yes | |||||
ASES, American Shoulder and Elbow Surgeons; MCID, minimal clinically important difference.
Reported postoperative complications were separated into subgroups of those occurring following revision to anatomical TSA or to reverse TSA from data provided in 81 of 111 (73%) studies that reported postoperative outcome data.20-30–33,37,38-58–79,81–85-53,58-79,81-85,87,88,92-122,123,124,125,126,127,128-130,131-133 This included 455 complications in 2,073 shoulders revised to reverse TSA and 174 complications in 601 shoulders revised to anatomical TSA. The incidence and OR of postoperative complications in the two groups is presented in Table VII.
Table VII.
Postoperative complications following revision to reverse total shoulder arthroplasty versus anatomical total shoulder arthroplasty: reported incidence and odds ratio.
| Postoperative complication | RTSA cases (n = 2,073) |
% | ATSA cases (n = 601) |
% | p-value | OR* | |
|---|---|---|---|---|---|---|---|
| RTSA | ATSA | ||||||
| Instability | 134 | 6.46 | 51 | 8.49 | 0.084† | 1.34 (0.96 to 1.88) |
|
| Component loosening | 92 | 4.44 | 22 | 3.66 | 0.405† | 1.22 (0.76 to 1.96) |
|
| Infection | 60 | 2.89 | 16 | 2.66 | 0.765† | 1.09 (0.62 to 1.91) |
|
| Periprosthetic fracture | 75 | 3.62 | 9 | 1.50 | 0.009† | 2.47 (1.23 to 4.96) |
|
| Pain and stiffness | 14 | 0.68 | 21 | 3.49 | < 0.001† | 5.33 (2.70 to 10.54) |
|
| Rotator cuff failure | 3 | 0.14 | 35 | 5.82 | < 0.001‡ | 42.67 (13.08 to 139.24) |
|
| Haematoma | 24 | 1.16 | 1 | 0.17 | 0.027‡ | 7.02 (0.95 to 52.06) | |
| Glenoid failure | - | - | 5 | 0.83 | |||
| Baseplate failure | 10 | 0.48 | - | - | |||
| Fracture sequelae | 1 | 0.05 | 1 | 0.17 | 0.399‡ | 3.45 (0.23 to 55.30) |
|
| Radiological complications | 12 | 0.58 | 0 | 0.00 | 0.080‡ | 7.29 (0.43 to 123.39) |
|
| Nerve injuries | 6 | 0.29 | 1 | 0.17 | 1.000‡ | 1.74 (0.21 to 14.50) |
|
| Wound problems | 6 | 0.29 | 1 | 0.17 | 1.000‡ | 1.74 (0.21 to 14.50) |
|
| Others | 15 | 0.72 | 6 | 1.00 | |||
| Unspecified | 3 | 0.14 | 5 | 0.83 | |||
| Overall complication rate | 455 | 21.95 | 174 | 28.95 | < 0.001† | 1.45 (1.18 to 1.78) |
|
Odds ratio (OR) with 95% confidence interval. OR greater than 2 with 95% CI not spanning null value (OR = 1) was considered clinically relevant.
Compared using chi-squared test.
Compared using Fisher's exact test.
ATSA, anatomical total shoulder arthroplasty; OR, odds ratio; RTSA, revision total shoulder arthroplasty.
In the group revised to anatomical TSA, compared to those revised to reverse TSA, there was a significantly higher incidence of postoperative complications using a chi-squared test (OR 1.5 (95% CI 1.2 to 1.8); p < 0.001), with a clinically relevant higher incidence of pain and stiffness (OR 5.3 (95% CI 2.7 to 10.5); p < 0.001) and rotator cuff failure (OR 42.7 (95% CI 13.1 to 139.2); p < 0.001) following revision.
In the group revised to reverse TSA, there was a clinically relevant higher incidence of periprosthetic fracture (OR 2.5 (95% CI 1.2 to 5.0); p < 0.009, chi-squared test) following revision.
There was no clinically relevant difference in the incidence of instability, component loosening, infection, haematoma formation, fracture sequelae, radiological complications, nerve injuries, or wound problems between the two groups.
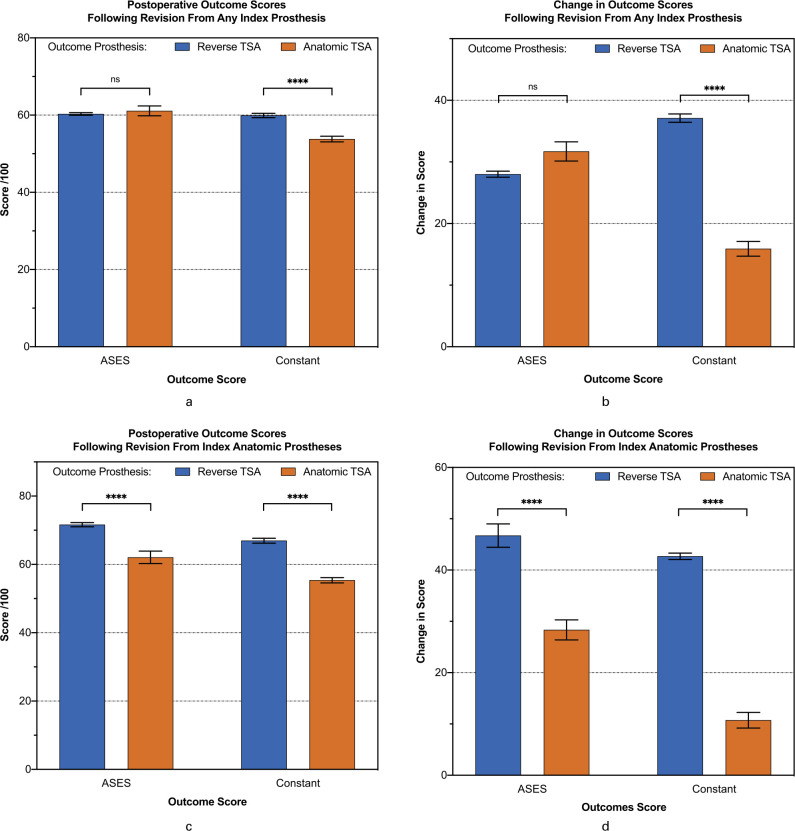
Reported shoulder outcome scores were separated into subgroups of those occurring following revision to anatomical TSA or to reverse TSA from data provided in 45 of 55 (82%) studies that reported PROMs. ASES score was reported in 22 of 45 studies,20,28,32,48,50,52,53,58,60,61,63,68,70,72,74,76,77,79,81,83,85,87 and Constant score was reported in 23 out of 45 studies.21,22,27,38,47,51,59,62,64-67,69,73,75,78,82,84,88,90–92,118 This included outcomes for 1,208 shoulders revised to reverse TSA (669 reported using ASES and 539 reported using Constant score) and 162 shoulders revised to anatomical TSA (42 reported using ASES and 120 reported using Constant score). Comparison of postoperative scores and changes in scores following revision to anatomical and reverse TSA are presented in Figures 2a and 2b, respectively.
Fig. 2.
American Shoulder and Elbow Surgeons (ASES) and Constant scores following revision shoulder arthroplasty. a) Postoperative scores (absolute score) following revision from any type of index prosthesis to reverse or anatomical total shoulder arthroplasty (TSA). b) Change in scores (postoperative score minus preoperative score) following revision from any type of index prosthesis to reverse or anatomical TSA. c) Postoperative scores (absolute score) following revision from index anatomical TSA only to reverse or anatomical TSA. d) Change in scores (postoperative score minus preoperative score) following revision from anatomical TSA only to reverse or anatomical TSA. Independent-samples t-test use for comparison of mean values (ns, no significant difference; ****, p < 0.0001).
When Constant scores were compared using an independent-samples t-test, the group revised to reverse TSA from any type of index prosthesis demonstrated a significantly higher postoperative score when compared to those revised to anatomical TSA (p < 0.001) (mean difference 6.1 (95% CI 3.7 to 8.5) and change in score (p < 0.001) (mean difference 21.2 (95% CI 18.1 to 24.3) following revision. When ASES scores were compared, there was no significant difference in the postoperative score (p = 0.571) and change in score (p = 0.072) between the two groups.
Outcomes scores for shoulders revised from index anatomical TSA were reported in 14 of 112 (13%) studies; ASES score was reported in five (36%) studies,68,70,72,77,81 and Constant score in nine (64%) studies.22,27,62,64,67,69,73,84,91 This included outcomes for 216 shoulders with index anatomical TSA revised to reverse TSA (45 reported using ASES and 171 reported using Constant score) and 102 shoulders with index anatomical TSA revised to a second anatomical TSA (29 reported using ASES and 73 reported using Constant score). Comparison of postoperative score and change in score following revision is presented in Figures 2c and 2d, respectively.
When ASES and Constant scores were compared, the group with index anatomical TSA revised to reverse TSA, in comparison to those revised to anatomical TSA, reported a significantly higher postoperative score (p < 0.001) (ASES mean difference 9.6 (95% CI 5.7 to 13.4); Constant mean difference 11.6 (95% CI 7.7 to 15.5)) and change in score following revision (ASES mean difference 18.4 (95% CI 13.2 to 23.6); Constant mean difference 32.0 (95% CI 28.2 to 35.7); p < 0.001).
Discussion
The meta-analysis data demonstrated overall rates for intraoperative complications, postoperative complications, and reoperations following revision shoulder arthroplasty of 8%, 22%, and 13%, respectively. The most commonly reported intraoperative and postoperative complications were iatrogenic humeral fractures and instability, respectively. Overall, 87% of studies with reporting outcome scores demonstrated an improvement in PROMs of a greater magnitude than the MCID.
A higher incidence of postoperative complications was reported in shoulders that were revised to anatomical TSA, compared to reverse TSA, however this did not reach our predetermined clinically relevant threshold. There was a clinically relevant higher incidence of pain and stiffness, and rotator cuff failure following revision to anatomical TSA versus reverse TSA, although clear objective definitions of these two outcomes are difficult to ascertain from the literature investigated. Conversely, there was a clinically relevant higher incidence of periprosthetic fractures following revision to reverse TSA, versus anatomical TSA. Revision from any index prosthesis to reverse TSA, versus revision to anatomical TSA, resulted in greater absolute postoperative Constant score as well as perioperative improvement in Constant score. Furthermore, revision of index anatomical TSA to reverse TSA, versus revision to a second anatomical TSA, achieved greater absolute postoperative and perioperative improvement in both ASES and Constant scores.
Iatrogenic fractures during shoulder arthroplasty are relatively uncommon, although they can be a challenge to manage when they arise during revision surgery.134 Reports indicate that intraoperative fracture results in increased operating time, higher blood loss, and poorer postoperative outcomes.120,135 Our findings suggest that humeral fractures have a higher incidence compared to glenoid fractures, which is consistent with results from other studies.12,120 Fracture during prosthesis explantation is the most likely cause, with removal of stemmed humeral components being the riskiest stage of the procedure according to our data. The fracture risk can occur when removing a cemented stem, removing cement itself, or explanting an uncemented stem, however evidence to suggest which of these was the most likely was not demonstrable in our results due to lack of individual case data. Future use of exchangeable modular, short-stemmed, and stemless humeral prostheses may have an impact on reducing intraoperative fracture risk.
A high incidence of postoperative instability following revision was expected (6% in this meta-analysis) as it is commonly reported following primary reverse TSA,136-138 and two-thirds of the shoulders included in the present study were revised to a reverse prosthesis. Despite this presumption, subgroup analysis found no difference in incidence of instability following revision to reverse or anatomical TSA. We speculate this may be due to inconsistency in terminology used by individual studies to report instability, as well as the differences in presentation of instability occurring in anatomical and reverse TSAs. The clinical relevance of this comparison may be limited.
The clinically relevant higher incidence of pain and stiffness following revision to anatomical TSA may be attributable to dynamic cuff dysfunction from chronic cuff disease. Less substantial soft-tissue release in anatomical arthroplasty or postoperative immobilization following subscapularis repair may also be factors contributing to stiffness in anatomical revision. There was a comparatively higher rate of cuff failure as a reported complication following anatomical TSA, which was a predictable finding and clinically unimportant when comparing complication rates.
The clinically relevant higher incidence of postoperative periprosthetic fracture following revision to reverse TSA was an unexpected finding; periprosthetic fractures are thought to be uncommon, with low incidence rates previously reported following reverse TSA.12,139,140 We believe this is an incidental finding and acknowledge that the result is subject to bias, as multiple factors that increase risk of fractures have not been taken into consideration when comparing the two groups, such as age, bone density, and presence of other comorbidities. Surgical technique used in revision, individual prosthetic design, and preferential use of press fit stems could have contributed to this result. Additionally, fracture location may have influenced this result, with tuberosity fractures perhaps more likely in reverse implants due to them occupying a larger proportion of the metaphysis, the lower neck cut required for implantation, and the increased retraction on the humerus required to implant a glenosphere.
Revision to reverse TSA from any index prosthesis resulted in better outcome scores versus revision to anatomical TSA. Previous studies have demonstrated better outcomes for revision to an anatomical prosthesis when used appropriately (i.e. revision for isolated glenoid arthrosis or failure in the presence of an intact rotator cuff).68,101 Our findings raise the possibility that conversion to reverse TSA may result in equally good, if not better, outcomes even in these situations. This notion should be tempered by the fact that this systematic review did not specifically evaluate the use of anatomical and reverse TSA in this context and hence a definitive conclusion should not be inferred, given the heterogeneity of preoperative pathology and broad inclusion criteria used. Physical and functional integrity of the rotator cuff are distinct states that would influence outcomes following revision to anatomical TSA, hence it may be prudent to further investigate how to preoperatively differentiate these states in the setting of an existing arthroplasty.
The quality of our data is linked to the accuracy of studies used in this systematic review, all of which were retrospective in nature. Most of the studies used for quantitative synthesis were of level IV evidence (77% of all studies), highlighting the need for more robust studies on outcomes following revision shoulder arthroplasty.
The strength of our evidence is affected by strong heterogeneity among studies, affirmed from high I2 values (range 69% to 76%) found in meta-analyses of complication and reoperation data. The random-effects model was used to help account for heterogeneity in reported rates, but the high variance indicates potential external bias if applied to other populations.17
The high heterogeneity indicates a significant degree of methodological or clinical variance in the included studies. Results from individual articles may have been influenced by hidden confounding factors that were not extractable from published data. An example of this is the operating surgeon’s experience and surgical technique used in revision, which was not reported in most studies. Similarly, many shoulder implant systems have been updated over time to address problems with the original implant design, and it was not possible to determine whether an original or updated design was used in revision from these articles.
This systematic review used a non-specific inclusion criterion to generate a generic analysis of all types of revision shoulder arthroplasty. Concomitant procedures performed during revision were not taken into consideration in this study, potentially introducing performance bias into our results. Intraoperative osteotomies, rotator cuff repairs, and use of bone grafts for complex reconstructions is associated with inferior outcomes following revision.32,34,61,140 Thus, inclusion of these cases in our study might have resulted in underestimation of clinical outcome.
Outcomes for individual subgroups analyzed in this systematic review were not extractable from all studies, making our findings from subgroup analyses unrepresentative of every revision case. Statistical analyses were applied to pooled raw data collected from eligible studies, but a formal comparative meta-analysis of results was not appropriate due to lack of homogeneity in study types.
The findings from this systematic review suggest high complication and reoperation rates following revision shoulder arthroplasty, which warrants effective and open communication to patients contemplating both revision and primary shoulder arthroplasty. Our findings provide a greater insight into the available literature on outcomes following revision shoulder arthroplasty, but also illustrate the frailties of the existing literature, particularly in terms of informing decision-making around what type of revision prosthesis to consider.
In conclusion, in this systematic review we demonstrated that revision shoulder arthroplasty results in improved PROMs but is associated with a high incidence of intraoperative complications (8%), postoperative complications (22%), and reoperations (13%). It appears that revision to reverse TSA demonstrates superior outcomes than revision to anatomical TSA, however decision-making should still be on a case-by-case basis given the inherent flaws in the existing literature.
Take home message
- Revision to reverse total shoulder arthroplasty is associated with better outcomes than revision to anatomical total shoulder arthroplasty (TSA).
- Intraoperative complication rate was 8%, postoperative complications rate was 22%, and reoperation rate was 13% following revision shoulder arthroplasty.
- Outcomes from revision shoulder arthroplasty show clinically important improvement in patient-reported outcome measures (PROMs).
- Revision to reverse geometry TSA rather than to anatomical TSA from any index procedure appears to result in lower complication rates and better postoperative outcome scores.
Acknowledgements
Many thanks to Mr Tom Roper (Clinical Librarian – Brighton and Sussex University Hospitals NHS Trust) for his advice on search strategy.
Footnotes
Author contributions: V. Ravi: Investigation, Formal analysis, Writing - original draft.
R. J. Murphy: Supervision, Formal analysis, Validation, Software, Writing - review and editing.
R. Moverley: Formal analysis, Writing - original draft.
M. Derias: Data curation, Formal analysis, Writing - review and editing.
J. Phadnis: Conceptualization, Supervision, Methodology, Writing - review and editing.
Funding statement: The author or one or more of the authors have received or will receive benefits for personal or professional use from a commercial party related directly or indirectly to the subject of this article. In addition, benefits have been or will be directed to a research fund, foundation, educational institution, or other non-profit organization with which one or more of the authors are associated. Open access was self-funded.
ICMJE COI statement: J. Phadnis reports consultancy payments from Wright Medical, unrelated to this study.
Twitter: Follow R. James Murphy @Dr_Rich_Murphy
Supplementary material: Search strategy used for database search, MINORS score for individual studies, and forest plots from meta-analysis of proportion.
References
- 1.Day JS, Lau E, Ong KL, Williams GR, Ramsey ML, Kurtz SM. Prevalence and projections of total shoulder and elbow arthroplasty in the United States to 2015. J Shoulder Elbow Surg. 2010;19(8):1115–1120. [DOI] [PubMed] [Google Scholar]
- 2.Craig RS, Lane JCE, Carr AJ, Furniss D, Collins GS, Rees JL. Serious adverse events and lifetime risk of reoperation after elective shoulder replacement: Population based cohort study using hospital episode statistics for England. BMJ. 2019;364:l298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Khatib O, Onyekwelu I, Yu S, Zuckerman JD. Shoulder arthroplasty in New York state, 1991 to 2010: Changing patterns of utilization. J Shoulder Elbow Surg. 2015;24(10):e286-91. [DOI] [PubMed] [Google Scholar]
- 4.Schairer WW, Nwachukwu BU, Lyman S, Craig EV, Gulotta LV. National utilization of reverse total shoulder arthroplasty in the United States. J Shoulder Elbow Surg. 2015;24(1):91–97. [DOI] [PubMed] [Google Scholar]
- 5.Petersen SA, Hawkins RJ. Revision of failed total shoulder arthroplasty. Orthop Clin North Am. 1998;29(3):519–533. [DOI] [PubMed] [Google Scholar]
- 6.Austin L, Zmistowski B, Chang ES, Williams GR. Is reverse shoulder arthroplasty a reasonable alternative for revision arthroplasty? Clin Orthop Relat Res. 2011;469(9):2531–2537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Boileau P, Watkinson D, Hatzidakis AM, Hovorka I. Neer Award 2005: the Grammont reverse shoulder prosthesis: results in cuff tear arthritis, fracture sequelae, and revision arthroplasty. J Shoulder Elbow Surg. 2006;15(5):527–540. [DOI] [PubMed] [Google Scholar]
- 8.Dines JS, Fealy S, Strauss EJ, et al. Outcomes analysis of revision total shoulder replacement. J Bone Joint Surg Am. 2006;88-A(7):1494–1500. [DOI] [PubMed] [Google Scholar]
- 9.Sajadi KR, Kwon YW, Zuckerman JD. Revision shoulder arthroplasty: an analysis of indications and outcomes. J Shoulder Elbow Surg. 2010;19(2):308–313. [DOI] [PubMed] [Google Scholar]
- 10.Wall B, Nové-Josserand L, O’Connor DP, Edwards TB, Walch G. Reverse total shoulder arthroplasty: A review of results according to etiology. J Bone Joint Surg Am. 2007;89-A(7):1476–1485. [DOI] [PubMed] [Google Scholar]
- 11.Saltzman BM, Chalmers PN, Gupta AK, Romeo AA, Nicholson GP. Complication rates comparing primary with revision reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2014;23(11):1647–1654. [DOI] [PubMed] [Google Scholar]
- 12.Zumstein MA, Pinedo M, Old J, Boileau P. Problems, complications, reoperations, and revisions in reverse total shoulder arthroplasty: A systematic review. J Shoulder Elbow Surg. 2011;20(1):146–157. [DOI] [PubMed] [Google Scholar]
- 13.Knowles NK, Columbus MP, Wegmann K, Ferreira LM, Athwal GS. Revision shoulder arthroplasty: A systematic review and comparison of north american vs. European outcomes and complications. J Shoulder Elbow Surg. 2020;29(5):1071–1082. [DOI] [PubMed] [Google Scholar]
- 14.Moher D, Liberati A, Tetzlaff J, Altman DG, Group P, PRISMA Group . Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int J Surg. 2010;8(5):336–341. [DOI] [PubMed] [Google Scholar]
- 15.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological index for non-randomized studies (minors): Development and validation of a new instrument. ANZ J Surg. 2003;73(9):712–716. [DOI] [PubMed] [Google Scholar]
- 16.Nyaga VN, Arbyn M, Aerts M. METAPROP: A stata command to perform meta-analysis of binomial data. Arch Public Health. 2014;72(1):39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Higgins JPT, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tashjian RZ, Hung M, Keener JD, et al. Determining the minimal clinically important difference for the american shoulder and elbow surgeons score, simple shoulder test, and visual analog scale (VAS) measuring pain after shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26(1):144–148. [DOI] [PubMed] [Google Scholar]
- 19.Ingoe HM, Holland P, Cowling P, Kottam L, Baker PN, Rangan A. Intraoperative complications during revision shoulder arthroplasty: A study using the National Joint Registry Dataset. Shoulder Elbow. 2017;9(2):92–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chacon A, Virani N, Shannon R, Levy JC, Pupello D, Frankle M. Revision arthroplasty with use of a reverse shoulder prosthesis-allograft composite. J Bone Joint Surg Am. 2009;91-A(1):119–127. [DOI] [PubMed] [Google Scholar]
- 21.Flury MP, Frey P, Goldhahn J, Schwyzer H-. K, Simmen BR. Reverse shoulder arthroplasty as a salvage procedure for failed conventional shoulder replacement due to cuff failure--midterm results. Int Orthop. 2011;35(1):53–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hoffelner T, Moroder P, Auffarth A, Tauber M, Resch H. Outcomes after shoulder arthroplasty revision with glenoid reconstruction and bone grafting. Int Orthop. 2014;38(4):775–782. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Merolla G, Tartarone A, Sperling JW, Paladini P, Fabbri E, Porcellini G. Early clinical and radiological outcomes of reverse shoulder arthroplasty with an eccentric all-polyethylene glenosphere to treat failed hemiarthroplasty and the sequelae of proximal humeral fractures. Int Orthop. 2017;41(1):141–148. [DOI] [PubMed] [Google Scholar]
- 24.Trappey GJ, O'Connor DP, Edwards TB. What are the instability and infection rates after reverse shoulder arthroplasty? Clin Orthop Relat Res. 2011;469(9):2505–2511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Andersen JR, Williams CD, Cain R, Mighell M, Frankle M. Surgically treated humeral shaft fractures following shoulder arthroplasty. J Bone Joint Surg Am. 2013;95-A(1):9–18. [DOI] [PubMed] [Google Scholar]
- 26.Foruria AM, Oh LS, Sperling JW, Cofield RH. Anteromedial approach for shoulder arthroplasty: Current indications, complications, and results. J Shoulder Elbow Surg. 2010;19(5):734–738. [DOI] [PubMed] [Google Scholar]
- 27.Crosby LA, Wright TW, Zuckerman JD. Revision total shoulder arthroplasty without humeral component removal. Bull Hosp Jt Dis (2013). 2015;73 Suppl 1:S136–S139. [PubMed] [Google Scholar]
- 28.Stephens BC, Simon P, Clark RE, et al. Revision for a failed reverse: a 12-year review of a lateralized implant. J Shoulder Elbow Surg. 2016;25(5):e115:124–e124. [DOI] [PubMed] [Google Scholar]
- 29.Rasmussen JV, Olsen BS, Al-Hamdani A, Brorson S. Outcome of revision shoulder arthroplasty after resurfacing hemiarthroplasty in patients with glenohumeral osteoarthritis. J Bone Joint Surg Am. 2016;98-A(19):1631–1637. [DOI] [PubMed] [Google Scholar]
- 30.Farshad M, Grogli M, Catanzaro S, Gerber C. Revision of reversed total shoulder arthroplasty. Indications and outcome BMC Musculoskelet Disord. 2012;13(1):160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hattrup SJ. Revision total shoulder arthroplasty for painful humeral head replacement with glenoid arthrosis. J Shoulder Elbow Surg. 2009;18(2):220–224. [DOI] [PubMed] [Google Scholar]
- 32.Johnston PS, Creighton RA, Romeo AA. Humeral component revision arthroplasty: outcomes of a split osteotomy technique. J Shoulder Elbow Surg. 2012;21(4):502–506. [DOI] [PubMed] [Google Scholar]
- 33.Tseng W-J, Lansdown DA, Grace T, et al. Outcomes of revision arthroplasty for shoulder periprosthetic joint infection: A three-stage revision protocol. J Shoulder Elbow Surg. 2019;28(2):268–275. [DOI] [PubMed] [Google Scholar]
- 34.Van Thiel GS, Halloran JP, Twigg S, Romeo AA, Nicholson GP. The vertical humeral osteotomy for stem removal in revision shoulder arthroplasty: results and technique. J Shoulder Elbow Surg. 2011;20(8):1248–1254. [DOI] [PubMed] [Google Scholar]
- 35.Franke KJ, Christmas KN, Downes KL, Mighell MA, Frankle MA. Does the etiology of a failed hemiarthroplasty affect outcomes when revised to a reverse shoulder arthroplasty? J Shoulder Elbow Surg. 2020;29(7):S156S149:S149–S156. [DOI] [PubMed] [Google Scholar]
- 36.Franke KJ, Christmas KN, Simon P, Mighell MA, Frankle MA. The effect of glenoid bone loss and rotator cuff status in failed anatomic shoulder arthroplasty after revision to reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2021;30(4):844–849. [DOI] [PubMed] [Google Scholar]
- 37.Ozgur SE, Sadeghpour R, Norris TR. Revision shoulder arthroplasty with a reverse shoulder prosthesis : Use of structural allograft for glenoid bone loss. Orthopade. 2017;46(12):1055–1062. [DOI] [PubMed] [Google Scholar]
- 38.Werner BS, Abdelkawi AF, Boehm D, et al. Long-term analysis of revision reverse shoulder arthroplasty using cemented long stems. J Shoulder Elbow Surg. 2017;26(2):273–278. [DOI] [PubMed] [Google Scholar]
- 39.Grosso MJ, Sabesan VJ, Ho JC, Ricchetti ET, Iannotti JP. Reinfection rates after 1-stage revision shoulder arthroplasty for patients with unexpected positive intraoperative cultures. J Shoulder Elbow Surg. 2012;21(6):754–758. [DOI] [PubMed] [Google Scholar]
- 40.Lee SH, Kim SJ, Kook SH, Kim JW. Two-Stage revision of infected shoulder arthroplasty using prosthesis of antibiotic-loaded acrylic cement: minimum three-year follow-up. Int Orthop. 2018;42(4):867–874. [DOI] [PubMed] [Google Scholar]
- 41.Owens CJ, Sperling JW, Cofield RH. Utility and complications of long-stem humeral components in revision shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22(7):e7:12–e12. [DOI] [PubMed] [Google Scholar]
- 42.Padegimas EM, Lawrence C, Narzikul AC, et al. Future surgery after revision shoulder arthroplasty: The impact of unexpected positive cultures. J Shoulder Elbow Surg. 2017;26(6):975–981. [DOI] [PubMed] [Google Scholar]
- 43.Thangarajah T, Ajami S, Coathup M, et al. Revision shoulder arthroplasty for failed humeral head resurfacing hemiarthroplasty. Shoulder Elbow. 2019;11(2 Suppl):35–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gorman RA, Christmas KN, Simon P, et al. Optimizing humeral stem fixation in revision reverse shoulder arthroplasty with the cement-within-cement technique. J Shoulder Elbow Surg. 2020;29(7S):S16S9. [DOI] [PubMed] [Google Scholar]
- 45.Dezfuli B, King JJ, Farmer KW, Struk AM, Wright TW. Outcomes of reverse total shoulder arthroplasty as primary versus revision procedure for proximal humerus fractures. J Shoulder Elbow Surg. 2016;25(7):1133–1137. [DOI] [PubMed] [Google Scholar]
- 46.Dilisio MF, Miller LR, Siegel EJ, Higgins LD. Conversion to reverse shoulder arthroplasty: Humeral stem retention versus revision. Orthopedics. 2015;38(9):779:e773. [DOI] [PubMed] [Google Scholar]
- 47.Gohlke F, Rolf O. [Revision of failed fracture hemiarthroplasties to reverse total shoulder prosthesis through the transhumeral approach : method incorporating a pectoralis-major-pedicled bone window]. Oper Orthop Traumatol. 2007;19(2):185–208.. [Article in German] [DOI] [PubMed] [Google Scholar]
- 48.Kelly JD, Zhao JX, Hobgood ER, Norris TR. Clinical results of revision shoulder arthroplasty using the reverse prosthesis. J Shoulder Elbow Surg. 2012;21(11):1516–1525. [DOI] [PubMed] [Google Scholar]
- 49.Mahylis JM, Puzzitiello RN, Ho JC, Amini MH, Iannotti JP, Ricchetti ET. Comparison of radiographic and clinical outcomes of revision reverse total shoulder arthroplasty with structural versus nonstructural bone graft. J Shoulder Elbow Surg. 2019;28(1):e9e1:e1–e9. [DOI] [PubMed] [Google Scholar]
- 50.Otto RJ, Clark RE, Frankle MA. Reverse shoulder arthroplasty in patients younger than 55 years: 2- to 12-year follow-up. J Shoulder Elbow Surg. 2017;26(5):792–797. [DOI] [PubMed] [Google Scholar]
- 51.Postacchini R, Castagna A, Borroni M, Cinotti G, Postacchini F, Gumina S. Total shoulder arthroplasty for the treatment of failed hemiarthroplasty in patients with fracture of the proximal humerus. J Shoulder Elbow Surg. 2012;21(11):1542–1549. [DOI] [PubMed] [Google Scholar]
- 52.Stephens SP, Paisley KC, Giveans MR, Wirth MA. The effect of proximal humeral bone loss on revision reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2015;24(10):1519–1526. [DOI] [PubMed] [Google Scholar]
- 53.Wiater BP, Baker EA, Salisbury MR, et al. Elucidating trends in revision reverse total shoulder arthroplasty procedures: a retrieval study evaluating clinical, radiographic, and functional outcomes data. J Shoulder Elbow Surg. 2015;24(12):1915–1925. [DOI] [PubMed] [Google Scholar]
- 54.Gaeremynck P, Amouyel T, Saab M, et al. Clinical and radiological outcomes of 17 reverse shoulder arthroplasty cases performed after failed humeral head resurfacing. Orthop Traumatol Surg Res. 2019;105(8):1495–1501. [DOI] [PubMed] [Google Scholar]
- 55.Richards RR, An KN, Bigliani LU, et al. A standardized method for the assessment of shoulder function. J Shoulder Elbow Surg. 1994;3(6):347–352. [DOI] [PubMed] [Google Scholar]
- 56.Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214(214):160. [PubMed] [Google Scholar]
- 57.Torrens C, Guirro P, Santana F. The minimal clinically important difference for function and strength in patients undergoing reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2016;25(2):262–268. [DOI] [PubMed] [Google Scholar]
- 58.Cox JL, McLendon PB, Christmas KN, Simon P, Mighell MA, Frankle MA. Clinical outcomes following reverse shoulder arthroplasty-allograft composite for revision of failed arthroplasty associated with proximal humeral bone deficiency: 2- to 15-year follow-up. J Shoulder Elbow Surg. 2019;28(5):900–907. [DOI] [PubMed] [Google Scholar]
- 59.Jaiswal A, Malhotra A, Hay S, Kelly CP. Revision shoulder arthroplasty for failed surface replacement hemiarthroplasty. Musculoskelet Surg. 2019;103(1):69–75. [DOI] [PubMed] [Google Scholar]
- 60.Crosby LA, Wright TW, Yu S, Zuckerman JD. Conversion to reverse total shoulder arthroplasty with and without humeral stem retention: The role of a convertible-platform stem. J Bone Joint Surg Am. 2017;99-A(9):736–742. [DOI] [PubMed] [Google Scholar]
- 61.Hernandez NM, Chalmers BP, Wagner ER, Sperling JW, Cofield RH, Sanchez-Sotelo J. Revision to reverse total shoulder arthroplasty restores stability for patients with unstable shoulder prostheses. Clin Orthop Relat Res. 2017;475(11):2716–2722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Antoni M, Barthoulot M, Kempf JF, Clavert P. Revisions of total shoulder arthroplasty: Clinical results and complications of various modalities. Orthop Traumatol Surg Res. 2016;102(3):297–303. [DOI] [PubMed] [Google Scholar]
- 63.Kohan EM, Chalmers PN, Salazar D, Keener JD, Yamaguchi K, Chamberlain AM. Dislocation following reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26(7):1238–1245. [DOI] [PubMed] [Google Scholar]
- 64.Cisneros LGN, Atoun E, Abraham R, Tsvieli O, Bruguera J, Levy O. Revision shoulder arthroplasty: Does the stem really matter? J Shoulder Elbow Surg. 2016;25(5):747–755. [DOI] [PubMed] [Google Scholar]
- 65.Ortmaier R, Resch H, Matis N, et al. Reverse shoulder arthroplasty in revision of failed shoulder arthroplasty-outcome and follow-up. Int Orthop. 2013;37(1):67–75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wieser K, Borbas P, Ek ET, Meyer DC, Gerber C. Conversion of stemmed hemi- or total to reverse total shoulder arthroplasty: advantages of a modular stem design. Clin Orthop Relat Res. 2015;473(2):651–660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Melis B, Bonnevialle N, Neyton L, et al. Glenoid loosening and failure in anatomical total shoulder arthroplasty: is revision with a reverse shoulder arthroplasty a reliable option? J Shoulder Elbow Surg. 2012;21(3):342–349. [DOI] [PubMed] [Google Scholar]
- 68.Deutsch A, Abboud JA, Kelly J, et al. Clinical results of revision shoulder arthroplasty for glenoid component loosening. J Shoulder Elbow Surg. 2007;16(6):706–716. [DOI] [PubMed] [Google Scholar]
- 69.Valenti P, Valle P, Sauzieres P, et al. Uncemented metal-back glenoid component in revision of aseptic glenoid loosening: a prospective study of 10 cases with a minimum follow-up of 2 years. Arch Orthop Trauma Surg. 2014;134(6):785–791. [DOI] [PubMed] [Google Scholar]
- 70.Walker M, Willis MP, Brooks JP, Pupello D, Mulieri PJ, Frankle MA. The use of the reverse shoulder arthroplasty for treatment of failed total shoulder arthroplasty. J Shoulder Elbow Surg. 2012;21(4):514–522. [DOI] [PubMed] [Google Scholar]
- 71.Kany J, Amouyel T, Flamand O, Katz D, Valenti P. A convertible shoulder system: is it useful in total shoulder arthroplasty revisions? Int Orthop. 2015;39(2):299–304. [DOI] [PubMed] [Google Scholar]
- 72.Weber-Spickschen TS, Alfke D, Agneskirchner JD. The use of a modular system to convert an anatomical total shoulder arthroplasty to a reverse shoulder arthroplasty: clinical and radiological results. Bone Joint J. 2015;97-B(12):1662–1667. [DOI] [PubMed] [Google Scholar]
- 73.Bonnevialle N, Melis B, Neyton L, et al. Aseptic glenoid loosening or failure in total shoulder arthroplasty: Revision with glenoid reimplantation. J Shoulder Elbow Surg. 2013;22(6):745–751. [DOI] [PubMed] [Google Scholar]
- 74.Holcomb JO, Cuff D, Petersen SA, Pupello DR, Frankle MA. Revision reverse shoulder arthroplasty for glenoid baseplate failure after primary reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2009;18(5):717–723. [DOI] [PubMed] [Google Scholar]
- 75.Werner BS, Boehm D, Gohlke F. Revision to reverse shoulder arthroplasty with retention of the humeral component: good outcome in 14 patients followed for a mean of 2.5 years. Acta Orthop. 2013;84(5):473–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Budge MD, Moravek JE, Zimel MN, Nolan EM, Wiater JM. Reverse total shoulder arthroplasty for the management of failed shoulder arthroplasty with proximal humeral bone loss: Is allograft augmentation necessary? J Shoulder Elbow Surg. 2013;22(6):739–744. [DOI] [PubMed] [Google Scholar]
- 77.Schubkegel TA, Kwon YW, Zuckerman JD. Analysis of intermediate outcomes of glenoid bone grafting in revision shoulder arthroplasty. Am J Orthop. 2014;43(5):216–219. [PubMed] [Google Scholar]
- 78.Beekman PDA, Katusic D, Berghs BM, Karelse A, De Wilde L. One-stage revision for patients with a chronically infected reverse total shoulder replacement. J Bone Joint Surg Br. 2010;92-B(6):817–822. [DOI] [PubMed] [Google Scholar]
- 79.Levy J, Frankle M, Mighell M, Pupello D. The use of the reverse shoulder prosthesis for the treatment of failed hemiarthroplasty for proximal humeral fracture. J Bone Joint Surg Am. 2007;89-A(2):292–300. [DOI] [PubMed] [Google Scholar]
- 80.Geervliet PC, Houtveen M, Sierevelt IN, Visser CPJ, van Noort A. Revision of failed resurfacing Hemiarthroplasty: midterm results, survival, and group comparison. Orthopedics. 2019;42(1):e117e111. [DOI] [PubMed] [Google Scholar]
- 81.Patel DN, Young B, Onyekwelu I, Zuckerman JD, Kwon YW. Reverse total shoulder arthroplasty for failed shoulder arthroplasty. J Shoulder Elbow Surg. 2012;21(11):1478–1483. [DOI] [PubMed] [Google Scholar]
- 82.Natera L, Bruguera J, Atoun E, Levy O. Revision shoulder arthroplasty from resurfacing to non-cemented short-stem reverse prosthesis. Rev Esp Cir Ortop Traumatol. 2016;60(3):175–183. [DOI] [PubMed] [Google Scholar]
- 83.Levy JC, Virani N, Pupello D, Frankle M. Use of the reverse shoulder prosthesis for the treatment of failed hemiarthroplasty in patients with glenohumeral arthritis and rotator cuff deficiency. J Bone Joint Surg Br. 2007;89-B(2):189–195. [DOI] [PubMed] [Google Scholar]
- 84.Castagna A, Delcogliano M, de Caro F, et al. Conversion of shoulder arthroplasty to reverse implants: clinical and radiological results using a modular system. Int Orthop. 2013;37(7):1297–1305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Holschen M, Siemes M-K, Witt K-A, Steinbeck J. Five-Year outcome after conversion of a hemiarthroplasty when used for the treatment of a proximal humeral fracture to a reverse total shoulder arthroplasty. Bone Joint J. 2018;100-B(6):761–766. [DOI] [PubMed] [Google Scholar]
- 86.Muh SJ, Streit JJ, Lenarz CJ, et al. Resection arthroplasty for failed shoulder arthroplasty. J Shoulder Elbow Surg. 2013;22(2):247–252. [DOI] [PubMed] [Google Scholar]
- 87.Cuff DJ, Virani NA, Levy J, et al. The treatment of deep shoulder infection and glenohumeral instability with debridement, reverse shoulder arthroplasty and postoperative antibiotics. J Bone Joint Surg Br. 2008;90-B(3):336–342. [DOI] [PubMed] [Google Scholar]
- 88.Hartel BP, Alta TD, Sewnath ME, Willems WJ. Difference in clinical outcome between total shoulder arthroplasty and reverse shoulder arthroplasty used in hemiarthroplasty revision surgery. Int J Shoulder Surg. 2015;9(3):69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Pellegrini A, Legnani C, Macchi V, Meani E. Two-stage revision shoulder prosthesis vs. Permanent articulating antibiotic spacer in the treatment of periprosthetic shoulder infections. Orthop Traumatol Surg Res. 2019;105(2):237–240. [DOI] [PubMed] [Google Scholar]
- 90.Grubhofer F, Imam MA, Wieser K, Achermann Y, Meyer DC, Gerber C. Staged revision with antibiotic spacers for shoulder prosthetic joint infections yields high infection control. Clin Orthop Relat Res. 2018;476(1):146–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Elhassan B, Ozbaydar M, Higgins LD, Warner JJP. Glenoid reconstruction in revision shoulder arthroplasty. Clin Orthop Relat Res. 2008;466(3):599–607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.De Wilde L, Mombert M, Van Petegem P, Verdonk R. Revision of shoulder replacement with a reversed shoulder prosthesis (Delta iii): Report of five cases. Acta Orthop Belg. 2001;67(4):348–353. [PubMed] [Google Scholar]
- 93.Abdel MP, Hattrup SJ, Sperling JW, Cofield RH, Kreofsky CR, Sanchez-Sotelo J. Revision of an unstable hemiarthroplasty or anatomical total shoulder replacement using a reverse design prosthesis. Bone Joint J. 2013;95-B(5):668–672. [DOI] [PubMed] [Google Scholar]
- 94.Aibinder WR, Schoch B, Schleck C, Sperling JW, Cofield RH. Revisions for aseptic glenoid component loosening after anatomic shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26(3):443–449. [DOI] [PubMed] [Google Scholar]
- 95.Alentorn-Geli E, Clark NJ, Assenmacher AT, et al. What are the complications, survival, and outcomes after revision to reverse shoulder arthroplasty in patients older than 80 years? Clin Orthop Relat Res. 2017;475(11):2744–2751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Antuna SA, Sperling JW, Cofield RH, Rowland CM. Glenoid revision surgery after total shoulder arthroplasty. J Shoulder Elbow Surg. 2001;10(3):217–224. [DOI] [PubMed] [Google Scholar]
- 97.Black EM, Roberts SM, Siegel E, Yannopoulos P, Higgins LD, Warner JJP. Reverse shoulder arthroplasty as salvage for failed prior arthroplasty in patients 65 years of age or younger. J Shoulder Elbow Surg. 2014;23(7):1036–1042. [DOI] [PubMed] [Google Scholar]
- 98.Black EM, Roberts SM, Siegel E, Yannopoulos P, Higgins LD, Warner JJP. Failure after reverse total shoulder arthroplasty: What is the success of component revision? J Shoulder Elbow Surg. 2015;24(12):1908–1914. [DOI] [PubMed] [Google Scholar]
- 99.Carroll RM, Izquierdo R, Vazquez M, Blaine TA, Levine WN, Bigliani LU. Conversion of painful hemiarthroplasty to total shoulder arthroplasty: long-term results. J Shoulder Elbow Surg. 2004;13(6):599–603. [DOI] [PubMed] [Google Scholar]
- 100.Cheung EV, Sperling JW, Cofield RH. Polyethylene insert exchange for wear after total shoulder arthroplasty. J Shoulder Elbow Surg. 2007;16(5):574–578. [DOI] [PubMed] [Google Scholar]
- 101.Cheung EV, Sperling JW, Cofield RH. Revision shoulder arthroplasty for glenoid component loosening. J Shoulder Elbow Surg. 2008;17(3):371–375. [DOI] [PubMed] [Google Scholar]
- 102.Cil A, Veillette CJH, Sanchez-Sotelo J, Sperling JW, Schleck C, Cofield RH. Revision of the humeral component for aseptic loosening in arthroplasty of the shoulder. J Bone Joint Surg Br. 2009;91-B(1):75–81. [DOI] [PubMed] [Google Scholar]
- 103.Groh GI, Wirth MA. Results of revision from hemiarthroplasty to total shoulder arthroplasty utilizing modular component systems. J Shoulder Elbow Surg. 2011;20(5):778–782. [DOI] [PubMed] [Google Scholar]
- 104.Holschen M, Franetzki B, Witt K-A, Liem D, Steinbeck J. Conversions from anatomic shoulder replacements to reverse total shoulder arthroplasty: do the indications for initial surgery influence the clinical outcome after revision surgery? Arch Orthop Trauma Surg. 2017;137(2):167–172. [DOI] [PubMed] [Google Scholar]
- 105.Holschen M, Franetzki B, Witt K-A, Liem D, Steinbeck J. Is reverse total shoulder arthroplasty a feasible treatment option for failed shoulder arthroplasty? A retrospective study of 44 cases with special regards to stemless and stemmed primary implants. Musculoskelet Surg. 2017;101(2):173–180. [DOI] [PubMed] [Google Scholar]
- 106.Merolla G, Wagner E, Sperling JW, Paladini P, Fabbri E, Porcellini G. Revision of failed shoulder hemiarthroplasty to reverse total arthroplasty: analysis of 157 revision implants. J Shoulder Elbow Surg. 2018;27(1):75–81. [DOI] [PubMed] [Google Scholar]
- 107.Ortmaier R, Resch H, Hitzl W, Mayer M, Stundner O, Tauber M. Treatment strategies for infection after reverse shoulder arthroplasty. Eur J Orthop Surg Traumatol. 2014;24(5):723–731. [DOI] [PubMed] [Google Scholar]
- 108.Rhee PC, Sassoon AA, Schleck CD, Harmsen WS, Sperling JW, Cofield RH. Revision total shoulder arthroplasty for painful glenoid arthrosis after humeral head replacement: the posttraumatic shoulder. J Shoulder Elbow Surg. 2011;20(8):1255–1264. [DOI] [PubMed] [Google Scholar]
- 109.Sabesan VJ, Ho JC, Kovacevic D, Iannotti JP. Two-Stage reimplantation for treating prosthetic shoulder infections. Clin Orthop Relat Res. 2011;469(9):2538–2543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Sanchez-Sotelo J, Sperling JW, Rowland CM, Cofield RH. Instability after shoulder arthroplasty: results of surgical treatment. J Bone Joint Surg Am. 2003;85-A(4):622–631. [PubMed] [Google Scholar]
- 111.Sassoon AA, Rhee PC, Schleck CD, Harmsen WS, Sperling JW, Cofield RH. Revision total shoulder arthroplasty for painful glenoid arthrosis after humeral head replacement: the nontraumatic shoulder. J Shoulder Elbow Surg. 2012;21(11):1484–1491. [DOI] [PubMed] [Google Scholar]
- 112.Scalise JJ, Iannotti JP. Bone grafting severe glenoid defects in revision shoulder arthroplasty. Clin Orthop Relat Res. 2008;466(1):139–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Sheth M, Sholder D, Padegimas EM, et al. Failure of anatomic total shoulder arthroplasty with revision to another anatomic total shoulder arthroplasty. Arch Bone Jt Surg. 2019;7(1):19–23. [PMC free article] [PubMed] [Google Scholar]
- 114.Sheth MM, Sholder D, Abboud J, et al. Revision of failed hemiarthroplasty for painful glenoid arthrosis to anatomic total shoulder arthroplasty. J Shoulder Elbow Surg. 2018;27(10):1884–1890. [DOI] [PubMed] [Google Scholar]
- 115.Sheth MM, Sholder D, Getz CL, Williams GR, Namdari S. Revision of failed hemiarthroplasty and anatomic total shoulder arthroplasty to reverse total shoulder arthroplasty. J Shoulder Elbow Surg. 2019;28(6):1074–1081. [DOI] [PubMed] [Google Scholar]
- 116.Streubel PN, Simone JP, Cofield RH, Sperling JW. Revision of failed humeral head resurfacing arthroplasty. Int J Shoulder Surg. 2016;10(1):21–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Uri O, Bayley I, Lambert S. Hip-inspired implant for revision of failed reverse shoulder arthroplasty with severe glenoid bone loss. improved clinical outcome in 11 patients at 3-year follow-up. Acta Orthop. 2014;85(2):171–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Valenti P, Kilinc AS, Sauzières P, Katz D. Results of 30 reverse shoulder prostheses for revision of failed hemi- or total shoulder arthroplasty. Eur J Orthop Surg Traumatol. 2014;24(8):1375–1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Wagner ER, Hevesi M, Houdek MT, Cofield RH, Sperling JW, Sanchez-Sotelo J. Can a reverse shoulder arthroplasty be used to revise a failed primary reverse shoulder arthroplasty? Bone Joint J. 2018;100-B(11):1493–1498. [DOI] [PubMed] [Google Scholar]
- 120.Wagner ER, Houdek MT, Elhassan BT, Sanchez-Sotelo J, Cofield RH, Sperling JW. What are risk factors for intraoperative humerus fractures during revision reverse shoulder arthroplasty and do they influence outcomes? Clin Orthop Relat Res. 2015;473(10):3228–3234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Wagner ER, Houdek MT, Hernandez NM, Cofield RH, Sánchez-Sotelo J, Sperling JW. Cement-within-cement technique in revision reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26(8):1448–1453. [DOI] [PubMed] [Google Scholar]
- 122.Wagner ER, Statz JM, Houdek MT, Cofield RH, Sánchez-Sotelo J, Sperling JW. Use of a shorter humeral stem in revision reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2017;26(8):1454–1461. [DOI] [PubMed] [Google Scholar]
- 123.Glanzmann MC, Kolling C, Schwyzer H-K, Audigé L. Conversion to hemiarthroplasty as a salvage procedure for failed reverse shoulder arthroplasty. J Shoulder Elbow Surg. 2016;25(11):1795–1802. [DOI] [PubMed] [Google Scholar]
- 124.Buchalter DB, Mahure SA, Mollon B, Yu S, Kwon YW, Zuckerman JD. Two-Stage revision for infected shoulder arthroplasty after minimum 2-year follow-up. Journal of Shoulder and Elbow Surgery. 2017;26(5):e163. [DOI] [PubMed] [Google Scholar]
- 125.Strickland JP, Sperling JW, Cofield RH. The results of two-stage re-implantation for infected shoulder replacement. J Bone Joint Surg Br. 2008;90-B(4):460–465. [DOI] [PubMed] [Google Scholar]
- 126.Hsu JE, Gorbaty JD, Whitney IJ, Matsen FA. Single-Stage revision is effective for failed shoulder arthroplasty with positive cultures for Propionibacterium. Journal of Bone and Joint Surgery. 2016;98(24):2047–2051. [DOI] [PubMed] [Google Scholar]
- 127.Sperling JW, Cofield RH. Humeral windows in revision shoulder arthroplasty. J Shoulder Elbow Surg. 2005;14(3):258–263. [DOI] [PubMed] [Google Scholar]
- 128.Klatte TO, Junghans K, Al-Khateeb H, et al. Single-Stage revision for peri-prosthetic shoulder infection: outcomes and results. Bone Joint J. 2013;95-B(3):391–395. [DOI] [PubMed] [Google Scholar]
- 129.Mileti J, Sperling JW, Cofield RH. Reimplantation of a shoulder arthroplasty after a previous infected arthroplasty. J Shoulder Elbow Surg. 2004;13(5):528–531. [DOI] [PubMed] [Google Scholar]
- 130.Ghijselings S, Stuyck J, Debeer P. Surgical treatment algorithm for infected shoulder arthroplasty: a retrospective analysis of 17 cases. Acta Orthop Belg. 2013;79(6):626–635. [PubMed] [Google Scholar]
- 131.Ince A, Seemann K, Frommelt L, Katzer A, Loehr JF. One-Stage exchange shoulder arthroplasty for peri-prosthetic infection. J Bone Joint Surg Br. 2005;87(6):814–818. [DOI] [PubMed] [Google Scholar]
- 132.Jawa A, Shi L, O'Brien T, O’Brien T, et al. Prosthesis of antibiotic-loaded acrylic cement (PROSTALAC) use for the treatment of infection after shoulder arthroplasty. J Bone Joint Surg Am. 2011;93(21):2001–2009. [DOI] [PubMed] [Google Scholar]
- 133.Sheth M, Sholder D, Abboud J, Lazarus M, Williams G, Namdari S. Revision of Anatomic Total Shoulder Arthroplasty to Hemiarthroplasty: Does it work. Arch Bone Jt Surg. 2020;8(2):147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Zhou HS, Chung JS, Yi PH, Li X, Price MD. Management of complications after reverse shoulder arthroplasty. Curr Rev Musculoskelet Med. 2015;8(1):92–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Athwal GS, Sperling JW, Rispoli DM, Cofield RH. Periprosthetic humeral fractures during shoulder arthroplasty. J Bone Joint Surg Am. 2009;91-A(3):594–603. [DOI] [PubMed] [Google Scholar]
- 136.Bufquin T, Hersan A, Hubert L, Massin P. Reverse shoulder arthroplasty for the treatment of three- and four-part fractures of the proximal humerus in the elderly: a prospective review of 43 cases with a short-term follow-up. J Bone Joint Surg Br. 2007;89-B(4):516–520. [DOI] [PubMed] [Google Scholar]
- 137.John M, Pap G, Angst F, et al. Short-Term results after reversed shoulder arthroplasty (delta III) in patients with rheumatoid arthritis and irreparable rotator cuff tear. Int Orthop. 2010;34(1):71–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Werner CML, Steinmann PA, Gilbart M, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the delta III reverse-ball-and-socket total shoulder prosthesis. J Bone Joint Surg Am. 2005;87-A(7):1476–1486. [DOI] [PubMed] [Google Scholar]
- 139.García-Fernández C, Lópiz-Morales Y, Rodríguez A, López-Durán L, Martínez FM. Periprosthetic humeral fractures associated with reverse total shoulder arthroplasty: incidence and management. Int Orthop. 2015;39(10):1965–1969. [DOI] [PubMed] [Google Scholar]
- 140.Wierks C, Skolasky RL, Ji JH, McFarland EG. Reverse total shoulder replacement: intraoperative and early postoperative complications. Clin Orthop Relat Res. 2009;467(1):225–234. [DOI] [PMC free article] [PubMed] [Google Scholar]