Abstract
Background
The COVID-19 pandemic has led to unprecedented stress on health care systems, and has affected acute coronary syndrome treatment at every step. This study aimed to examine the impact of COVID-19 on patient presentations with acute coronary syndromes during the first and second pandemic wave in Melbourne, Victoria.
Method
A retrospective cohort study of adults presenting with cute coronary syndrome during the first pandemic wave from 1 March 2020 to 31 April 2020 and the second pandemic wave from 1 July 2020 to 31 August 2020 was compared to a control period from 1 March to 31 April 2019 at a single sub-tertiary referral centre in Melbourne, Victoria servicing a catchment area with a relatively high incidence of COVID-19 cases.
Results
Three-hundred-and-thirty-five (335) patients were hospitalised with acute coronary syndromes across all three time periods. The total number of patients presenting with an acute coronary syndrome was reduced during the pandemic, with a higher proportion of ST elevation myocardial infarctions. Ischaemic times increased with time from symptom onset to first medical contact rising from 191 minutes in the control period to 292 minutes in the first wave (p=0.06) and 271 minutes in the second wave (p=0.06). Coronary angiography with subsequent revascularisation significantly increased from 55% in the control period undergoing revascularisation to 69% in the first wave (p<0.001) and 74% in the second wave (p<0.001).
Conclusion
A concerning reduction in acute coronary presentations occurred during the COVID-19 pandemic, associated with longer ischaemic times and a higher proportion requiring revascularisation. It is crucial that public awareness campaigns are instituted to address the contributing patient factors in future waves.
Keywords: Acute coronary syndrome, COVID-19, Myocardial infarction, Public health
Introduction
In December 2019, cases of coronavirus disease 2019 (COVID-19) caused by a novel coronavirus (SARS-CoV-2) emerged in Wuhan City, China [1]. The first case of COVID-19 was detected in Australia on 25 January 2020, with the declaration of a national pandemic on 27 February [2]. The COVID-19 pandemic has led to rapid changes in allocation of health care resources and has placed unprecedented stress on health care systems. The challenge for government and health systems has been to find a balance between restricting services and activity to limit viral transmission, while maintaining essential health care services to manage both Coronavirus respiratory disease and urgent non-communicable medical conditions such as cardiac diseases.
Acute coronary syndromes (ACS) are common, acute medical conditions where prompt assessment and management reduces mortality and morbidity; and delays to treatment are associated with poorer outcomes [3,4]. In ST-elevation myocardial infarction (STEMI), every 10-minute reperfusion delay results in an additional 0.34 deaths per 100 percutaneous coronary intervention (PCI)-treated patients, rising to 3.34 additional deaths per 100 for haemodynamically unstable PCI-treated patients [5]. The pandemic environment has affected ACS treatment at every step from patient presentation to hospital treatment and disposition. Published reports from Italy, Spain, England and the USA have all reported decreases in ACS presentation volumes of up to 50% during the COVID-19 pandemic [[6], [7], [8], [9], [10]]. Similar reports have also documented significant delays from symptom-onset to presentation and revascularisation [11,12].
The Australian state of Victoria has a population of 5.93 million and observed an initial rise of COVID-19 cases in March and April 2020, primarily in returned travellers and their direct contacts. Prompt government-instituted physical distancing policies and restrictions on public gatherings effectively suppressed this ‘first wave,’ leading to a decline in cases in May 2020 [13]. Subsequent relaxation of restrictions in June 2020 however resulted in a larger ‘second wave’ resurgence in COVID-19 cases, with an increased incidence of asymptomatic carriage and community transmission [2].
Alterations to patterns of patient presentation and cardiac care systems have raised concerns that cardiac morbidity and mortality may be increased during the COVID-19 pandemic [14]. The possibility of patients with ACS symptoms not presenting to hospital or presenting with significant delays has the potential to result in worse outcomes due to reinfarction, cardiac arrest and reduced myocardial salvage.
Our aim was to examine the impact of the Victorian pandemic response on patient dependent factors that include ACS presentation volumes and delays to medical contact; as well as institutional factors such as delays to revascularisation, and any effect on outcomes including 30-day mortality and morbidity.
Material and Methods
We conducted a retrospective study of ACS presentations to Northern Health, a sub-tertiary referral centre with 24-hour primary PCI services in Melbourne, Australia. Northern Health has an annual PCI volume of over 600 cases per annum and services a catchment area where 26.4% (5,048 of the 19,096 cases) of Victoria’s laboratory confirmed COVID-19 cases were located between January 25 2020 and August 31 2020 [2,15,16].
Time periods examined were the first wave of transmission from 1 March 2020 to 31 April 2020, and the second wave of transmission from 1 July 2020 to 31 August 2020. The control period was the corresponding period from the previous year 1 March to 31 April 2019. A single control time period was chosen rather than an average across multiple years as our institution’s ACS presentations have increased from year-to-year. Total ACS presentations to Northern Health were also collected for 1 July 2019 to 31 August 2019 to assess potential impact of seasonal variation, as well as 1 November to 31 December 2019 and 2020 to assess the impact of relaxation of public health restrictions [17]. Sensitivity analysis was conducted comparing ischaemic times from 1 July to 31 August 2019 to the second wave, to assess consistency with comparing the second wave to the control period (Appendix 1).
We identified eligible adult patients who presented to our institution and were confirmed to have ACS utilising International Statistical Classification of Diseases and Health Related Problems 10 (ICD-10) discharge coding for ACS (I20.0, I21 and I22). Patients were included if they presented to hospital with primary symptoms of ACS such as chest pain, dyspnoea or angina-equivalents. Information from the medical record was collected on baseline characteristics of the patient, time of symptom onset and method of presentation. In the event of stuttering symptoms, we restricted the coding for symptom-to-door time to one week as has been described previously [18].
Subjects were excluded if they were diagnosed with a type II non-ST elevation myocardial infarction (NSTEMI) without presenting symptoms of ACS, developed a de-novo ACS while already admitted to hospital or were electively admitted to hospital for cardiac or non-cardiac procedures.
Measures of interest were the number of hospital presentations with ACS, proportion of STEMI presentations, proportion of patients undergoing PCI, time from symptom onset to first medical contact and door-to-balloon (DTB) times in patients presenting with STEMI. Time from symptom onset to first medical contact was defined as duration from first patient reported symptom to the time of presentation to local medical officer, arrival of ambulance service or time triaged at the emergency department if self-presenting. Outcome data collected was 30-day composite of major adverse cardiac events (MACE), which included in-hospital cardiac arrest, cardiac death, myocardial infarction at 30 days and unplanned revascularisation at 30 days. Cardiac death was defined as any death due to an evident cardiac cause, any death related to percutaneous coronary intervention (PCI), unwitnessed death, or death of unknown causes. Myocardial infarction was defined according to the fourth universal definition [19]. All patients undergoing PCI are routinely followed up at 30 days by our institution.
All data were collected by the authors, who subsequently reviewed, analysed and interpreted the results. Data was analysed using GraphPad Prism version 8.3.1 (GraphPad Software, San Diego, CA, USA). The descriptive data were presented as frequency with percentage, or as a median with an interquartile range, or as a mean with standard deviation as appropriate. Categorical data was compared by Chi-Square test or Fisher’s exact as appropriate for each variable. Continuous variables were compared using Mann-Whitney U test. Differences were considered significant if p<0.05.
The study was approved by The Northern Health Research Governance Office.
Results
The entire study cohort over all three time periods comprised 335 hospitalisations for ACS. This included 96 for STEMI (28.7%), 195 for NSTEMI (58%), 32 for unstable angina (UA) (9.3%) and other diagnoses in 3% (six Takotsubo cardiomyopathy, four myocardial infarctions with nonobstructive coronary arteries, two myopericarditis, one aortic dissection, one severe aortic stenosis). Sixty-six (66)/211 (31.3%) participants were excluded from the control period, 61/169 (36.1%) from the first wave, 74/156 (47.4%) from the second wave. Baseline demographic characteristics (Table 1 ) were well matched between the control, first wave and second wave time periods with no significant differences in age or gender. There were no confirmed COVID-19 cases in patients presenting with ACS during the first or second wave.
Table 1.
Baseline characteristics.
| Control Period, (March–April 2019, n=145) | First Wave, (March–April 2020, n=108) | Second Wave, (July–August 2020, n=82) | |
|---|---|---|---|
| Age (yr)∗ | 65.7±15.2 | 64.1±14.5 | 63.8±14.09 |
| Gender (male) | 98 (67.6%) | 76 (70.4%) | 60 (73.2%) |
| Hypertension | 95 (65.5%) | 72 (66.7%) | 48 (58.5%) |
| Dyslipidaemia | 99 (68.3%) | 81 (75.0%) | 54 (65.9%) |
| Diabetes | 63 (43.5%) | 42 (38.9%) | 27 (32.9%) |
| Previous percutaneous coronary intervention | 33 (22.8%) | 29 (26.9%) | 8 (9.8%) |
| Previous coronary artery bypass graft | 4 (2.8%) | 3 (2.8%) | 2 (2.4%) |
| Stroke/TIA | 11 (7.6%) | 5 (4.6%) | 2 (2.4%) |
| Peripheral vascular disease | 8 (5.5%) | 2 (1.9%) | 3 (3.7%) |
| Obesity (BMI≥35) | 20 (13.8%) | 11 (10.2%) | 4 (4.9%) |
| Admission medications | |||
| Single antiplatelet | 34 (23.5%) | 23 (21.3%) | 21 (25.6%) |
| Dual antiplatelet | 20 (13.8%) | 23 (21.3%) | 3 (3.7%) |
| Statin | 63 (43.5%) | 53 (49.1%) | 26 (31.7%) |
| ACE-I/ARB/ARNI | 67 (46.2%) | 55 (50.1%) | 26 (21.7%) |
Median ± Std deviation.
Abbreviations: ACE, angiotensin converting enzyme; ARB, angiotensin receptor blocker; ARNI, angiotensin receptor-neprilysin inhibitor; BMI, body mass index; TIA, transient ischaemic attack.
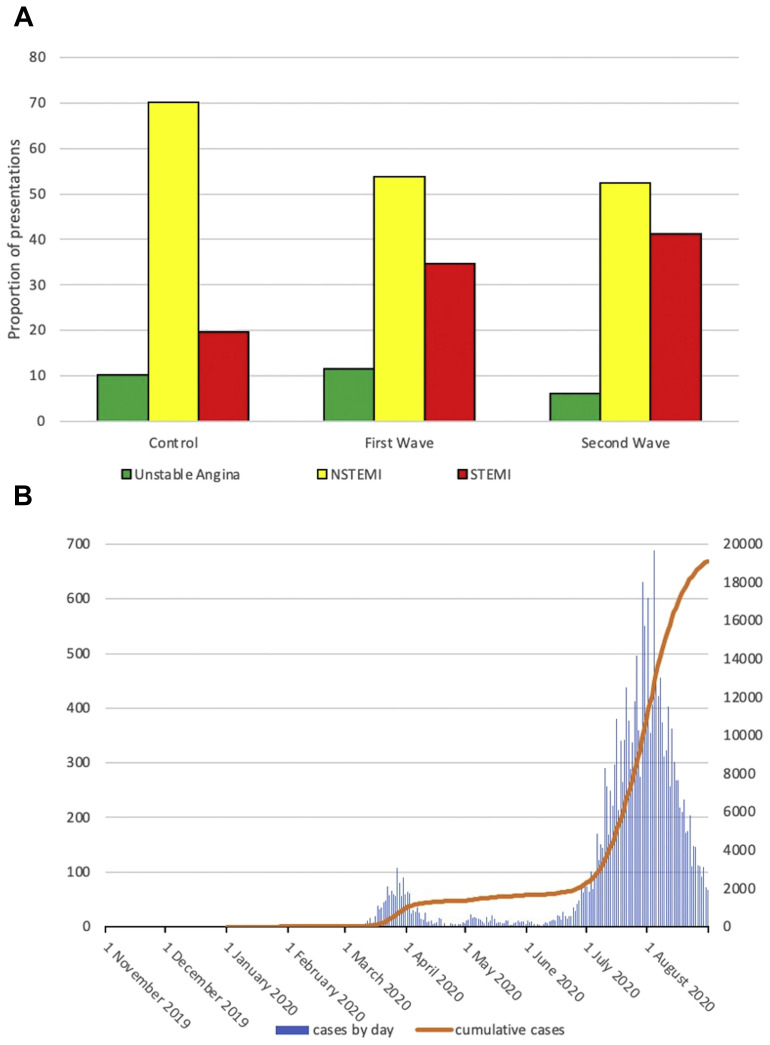
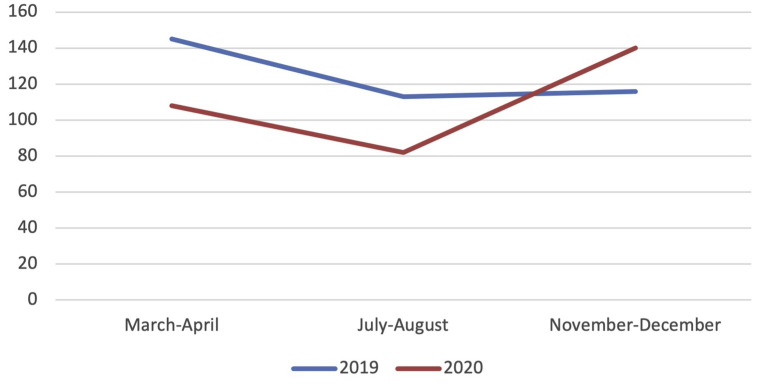
There was a reduction in the total number of patients presenting with ACS between the control and first wave (Table 2 ). There was also a reduction in total presentations in the second wave compared to the same time period in 2019. The reduction was predominantly in UA and NSTEMI presentations, with a higher proportion of STEMI accounting for 33.3% of ACS presentations in the first wave and 40.2% in the second wave, compared to 18.6% of ACS presentations in the control period (Figure 1 A). There was evidence of a rebound surge in ACS presentations as restrictions were eased in November 2020, with 140 total ACS presentations in November–December 2020 compared to 116 in the same period of 2019 (Table 2 and Figure 2 ).
Table 2.
Presentations.
| March–April 2019 | March–April 2020 (First-Wave) | July–August 2019 | July–August 2020 (Second Wave) | November–December 2019 | November–December 2020 (Relaxation) | |
|---|---|---|---|---|---|---|
| STEMI | 25 (17.3%) | 37 (34.2%) | 36 (31.8%) | 33 (40.2%) | 40 (34.5%) | 38 (27.1%) |
| NSTEMI | 105 (72.4%) | 61 (56.5%) | 73 (64.6%) | 43 (52.4%) | 63 (54.3%) | 83 (59.3%) |
| UA | 15 (10.3%) | 10 (9.3%) | 4 (3.5%) | 6 (7.3%) | 13 (11.2%) | 19 (13.6%) |
| Total ACS | 145 | 108 | 113 | 82 | 116 | 140 |
| Excluded | 66/211 (31%) | 61/169 (36%) | 91/204 (45%) | 74/156 (47%) | 69/185 (37%) | 91/231 (39%) |
Abbreviations: STEMI, ST elevation myocardial infarction; NSTEMI; non ST elevation myocardial infarction; UA, unstable angina; ACS, acute coronary syndrome.
Figure 1.
A: Proportion of acute coronary syndrome (ACS) presentations illustrating increased proportion of ST elevation myocardial infarction (STEMI) presentations with reduction in non ST elevation myocardial infarction (NSTEMI) presentations corresponding to a control period, first wave and second wave. B: Victorian COVID-19 cases by day and cumulative cases.
Figure 2.
Acute Coronary Syndrome Presentations.
There was a numerical increase in median time from symptom onset to first medical contact from 191 minutes in the control period to 292 minutes in the first wave (p=0.06) and 271 minutes in the second wave (p=0.06) that did not reach statistical significance (Table 3 ). There was no change in method of first medical contact, with a similar proportion of self-presentation to the emergency department, ambulance service or local medical officer (Appendix 2). In patients presenting with STEMI, median DTB time was 59 minutes in the control period. There was a 9-minute increase in median DTB time between the control and the first wave (p=0.09). There was a statistically significant increase in median DTB time during the second wave of 13.5 minutes compared to the control period (p=0.04) (Table 3). The method of first medical contact for subjects who experienced a STEMI was predominantly via the ambulance service with 80% of subjects with STEMI in the control period compared to 70% and 76% of subjects during the first and second wave respectively having first contact with the ambulance service (Appendix 2).
Table 3.
Ischaemic Time.
| Control Period, (March–April 2019, n=145) | First Wave, (March–April 2020, n=108) | Control vs First Wave | Second Wave, (July–August 2020, n=82) | Control vs. Second Wave | |
|---|---|---|---|---|---|
| Time to medical contact (minutes)a | 191 (80–764) | 292 (97–1,767) | p=0.06 | 271 (79–2,932) | p=0.06 |
| Door to balloon (DTB) time (min) for ST elevation myocardial infarction (STEMI) patientsa | 59 (34–74) | 68 (48–98) | p=0.09 | 72.5 (43–119) | p=0.04 |
| Total ischaemic time (mins) for STEMI patientsa | 137 (102–307) | 267 (13–1,124) | p=0.06 | 293 (157-3,796) | p=0.02 |
| Proportion DTB ≤60 min | 60.9% (14/23) | 43.75% (14/32) | p=0.28 | 44.8% (13/29) | p=0.28 |
| Proportion DTB ≤90 min | 87.0% (20/23) | 71.9% (23/32) | p=0.32 | 65.5% (19/29) | p=0.11 |
| Thrombolysed STEMI | 3/26 (12%) | 4/36 (11%) | 5/33 (15.2%) | ||
| Out of hospital cardiac arrest | 4 (2.8%) | 1 (0.9%) | 6 (7.3%) |
Median (IQR).
There was a trend to longer median ischaemic time in STEMI patients from 137 minutes in the control group to 267 minutes in the first wave (p=0.06), with a statistically significant increase in the second wave to 293 minutes (p=0.02). There was a trend towards a decrease in the proportion of STEMI patients that met the DTB target of 90 minutes from 87% in the control period to 71.9% in the first wave and 65.5% in the second wave (Table 3).
During the first and second wave periods patients with ACS were more likely to undergo invasive management, with 88% in the first wave (p=0.02) and 89% in the second wave (p=0.01) compared to 75% in the control period undergoing coronary angiography. There was a higher proportion of revascularisation with either coronary artery bypass grafting (CABG) or PCI during the pandemic waves, with 55% of patients being revascularised in the control period compared to 68.5% in the first wave (p<0.0001) and 74.4% in the second wave (p<0.0001, Table 4 ).
Table 4.
In-hospital management and outcomes [21].
| Control Period, (March–April 2019, n=145) | First Wave, (March–April 2020, n=108) | Control vs First Wave | Second Wave, (July–August 2020, n=82) | Control vs. Second Wave | |
|---|---|---|---|---|---|
| Angiogram during index admission | 109 (75.2%) | 95 (88%) | p=0.02 | 73 (89%) | p=0.01 |
| PCI during index admission | 63 (43.4%) | 64 (59.3%) | p=0.02 | 53 (64.6%) | p<0.001 |
| CABG referral from admission | 11 (7.6%) | 15 (13.9%) | p=0.14 | 13 (15.9%) | p=0.07 |
| Index revascularisation | 74 (54.5%) | 79 (68.5%) | p<0.001 | 61 (74.4%) | p<0.001 |
| Death | 9 (6.2%) | 5 (4.6%) | p=0.78 | 6 (10.3%) | p=0.08 |
| 30-d myocardial infarction | 5 (3.5%) | 3 (2.8%) | p=0.99 | 1 (1.7%) | p=0.99 |
| 30-d revascularisation | 2 (1.4%) | 1 (0.9%) | p=0.99 | 1 (1.7%) | p=0.46 |
| 30-d MACE | 14 (9.6%) | 8 (7.4%) | p=0.65 | 8 (9.7%) | p=0.99 |
| Peak measured troponin I (ng/L) n<16 ng/L for women, n<26 ng/L for men | 2,019 (126–14,505) | 2,057 (175–20,710) | p=0.83 | 3,652 (753–41,033) | p=0.02 |
| Admitted ICU | 6 (4.1%) | 2 (1.9%) | p=0.47 | 5 (6.1%) | p=0.53 |
Abbreviations: PCI, percutaneous coronary intervention; CABG, coronary artery bypass graft; MACE, major adverse cardiac event.
Thirty (30)-day MACE was not different between groups, with 9.6% of patients meeting the composite endpoint in the control period compared with 7.4% in the first wave (p=0.65) and 9.7% in the second wave (p=0.99), although there was a numerical increase in 30-day mortality in the second wave (Table 4).
Discussion
This is the first study to-date assessing the impact of the COVID-19 outbreak on all comer ACS presentations in Australia. Additionally, this is the first study examining the association between local COVID-19 infections and ACS presentations and management across sequential waves. During the first and second wave of the COVID-19 outbreak in Melbourne, there was a reduction in patients admitted with ACS to our centre. We found a trend of increased total ischaemic time in the first wave with a significant increase in total ischaemic time in the second wave, with delays in both symptom to first medical contact in all patients with ACS as well as an increase in median DTB time in patients presenting with STEMI.
Timely diagnosis and effective management of ACS is required in order to prevent significant morbidity and mortality with the benefit greatest in patients presenting with STEMI. Time from first medical contact to primary PCI is a strong predictor of adverse outcomes with every 10-minute delay associated with increased mortality in patients presenting with STEMI [5]. Our observations suggest a need for proactive interventions to address both system and patient related factors that are leading to reduced presentation and delayed management of patients experiencing ACS during a pandemic.
Our findings of reduced presentations of UA and NSTEMI admissions were consistent with data from the United Kingdom that found STEMI presentations remained relatively stable, whilst UA and NSTEMI admissions reduced [6]. Previous Australian reported data found no change in absolute number of patients undergoing PCI for ACS [11]. We observed a concerning absolute reduction in ACS presentations with a higher proportion of patients presenting with ACS undergoing invasive management with angiography and revascularisation. Interestingly, there has been no corresponding increase in out of hospital cardiac arrests observed in Victoria [20], contrary to Italian observations where there were increased rates of out of hospital cardiac arrest [21].
It is possible that actual rates of ACS may have reduced due to reduction in participation in aerobic exercise, reduced air pollution and changes in lifestyle and diet associated with the pandemic environment [22]. Increased rates of out of hospital cardiac arrest in Italy and New York do not support the hypothesis of reduced background ACS incidence [21,23]. Another possible explanation for the reduction in NSTEMI and UA presentations without a similar decrease in STEMI presentations is that the background incidence of ACS has not changed, and rather patients with less severe symptoms have avoided or delayed presenting to hospital. Our findings of increased proportions of invasive angiography and revascularisation during the pandemic period supports a reduction in lower acuity presentations. Furthermore, as a result of delayed treatment some patients may have progressed to more severe acute coronary syndromes, and we observed a rebound 20% increase in ACS presentations to our institution in November–December 2020 following relaxation of public health restrictions compared to the previous year (Figure 2). It is reasonable to expect that patients who have had untreated ACS may develop delayed morbidity from reinfarction and heart failure not evident in our duration of follow-up; and health care services will need to be prepared to detect and manage these long-term sequelae in the coming months to years, with further research required to establish if this is the case.
There are multiple mechanisms by which the pandemic environment and necessary public health measures that have been implemented to reduce COVID-19 transmission may be influencing health care-seeking behaviours of patients with ACS. Physical distancing measures may have led to the isolation of vulnerable patients [24], who, separated from friends, family and colleagues may lack the means or the encouragement to seek medical attention. Conventional and social media coverage during the pandemic periods may also have dissuaded patients from presenting to hospital, both due to the fear of contracting COVID-19 within a high-risk environment, as well as a conscientious desire not to overburden the health care system [6,12].
Both patient and system related delays may have influenced ischaemic times during the COVID-19 outbreak, and we observed a statistically significant increase in DTB and total ischaemic times during the second pandemic wave. Median DTB times in patients presenting with STEMI during the first and second wave compared to the control period increased by 9 and 15 minutes respectively, with associated reduction in proportion of STEMI presenters revascularised within 60 and 90 minutes. Increased DTB time has been noted at other centres [25] and may be due to the increased time required to assess, transport and commence angiography with appropriate use of personal protective equipment (PPE) to reduce risk to staff. Further delays may arise in assessment to determine if early intubation is required utilising negative pressure precautions prior to transfer to the catheterisation laboratory. Given DTB is a well-established surrogate marker of outcomes following STEMI this is of great concern [[26], [27], [28]]. Whilst our study was not powered to detect increased mortality, there was a trend to higher mortality in the second wave. Concerningly, we found a trend to increased median time from symptom onset to first medical contact which increased in the first and second waves by 100 and 80 minutes respectively (p=0.06 and p=0.06 respectively). Timely revascularisation is crucial to preventing morbidity and mortality in patients presenting with STEMI [[3], [4], [5]] and increased ischaemic times during the COVID-19 pandemic have been associated with increased mortality and morbidity [25,29]. It is possible that ambulance arrival may have been delayed due to changes in PPE requirements and infection control, with documented deterioration of ambulance response times in Victoria during the COVID-19 pandemic [30]. This may have contributed to the observed increased ischaemic time.
During the pandemic the proportion of patients undergoing angiography has increased at our centre. Seventy-five per cent (75%) of ACS presenters in the control period were managed with an invasive strategy, which rose to approximately 90% in the COVID-19 era. Revascularisation rates significantly increased during the pandemic waves compared to the control period, with a greater proportion of patients undergoing PCI or referral for CABG. This may reflect increased average acuity of ACS presentations during the pandemic, potentially due to disease progression from increased ischaemic time or due to patients with less severe symptoms avoiding hospital presentation.
Proactive public awareness campaigns addressing avoidance behaviours and public fear are necessary in order to reduce COVID-19 collateral damage [24]. The reductions in presentations and delay from symptom onset to first medical contact is of serious concern. The effectiveness of public awareness campaigns in COVID-19 has been demonstrated in Britain where the implementation of a publicity campaign resulted in partial recovery in the decline in ACS admissions [6]. System factors that have increased DTB times contribute minimally to the increased ischaemic time and are unlikely to change given the necessity of maintaining staff safety. Hospital avoidance behaviours within the community, evident by reductions and delays in emergency department presentations, likely represent the most effective target for public health campaigns [6,12,31].
Limitations
This study has several limitations. This is a single centre retrospective study that was defined by coding data and it is possible that patients may have been excluded due to misclassification. These results may be a local phenomenon in the setting of a high number of local COVID-19 cases and may not be generalised to areas where case numbers are lower. We are unable to determine the number of patients who died prior to presentation [20], although there has not been an increase in out of hospital cardiac arrest Victoria wide. We are unable to determine if patients with ACS did not seek care or if there has been any change in the background incidence of ACS. There was a higher proportion of patients excluded in the second wave. The higher proportion of excluded in wave two may be due to a winter seasonal effect with more type II NSTEMI secondary to lower respiratory tract infections. The higher proportion of excluded subjects are similar for July–August 2019, where 45% of subjects were excluded for type II NSTEMI. This study is restricted to patients with confirmed ACS only, and does not assess the behaviours of patients presenting with chest pain symptoms where ACS is excluded. Finally, limiting follow-up duration to 30 days may not have captured all adverse outcomes associated with health care avoidance and treatment delays, in particular long-term sequalae such as heart failure, and arrhythmias.
Conclusion
This observational study demonstrates a concerning reduction in ACS presentations during the COVID-19 pandemic, with a trend to longer ischaemic times. The DTB time, an established surrogate marker of outcome following STEMI, in the second pandemic wave was significantly increased which is concerning. The longer ischaemic times are likely multifactorial, arising predominantly due to patient factors but also system factors. It is crucial that public awareness campaigns are instituted to address these patient factors. Following the pandemic, as restrictions were eased, we found a surge in ACS presentations. Health care systems need to continue to adapt and institute interventions in order to minimise cardiac collateral damage as the COVID-19 pandemic continues.
Financial Disclosures
No relevant disclosures.
Footnotes
Supplementary data associated with this article can be found, in the online version, at https://doi.org/10.1016/j.hlc.2021.07.023.
Appendices. Supplementary Data
References
- 1.Zhou F., Yu T., Du R., Fan G., Liu Y., Liu Z., et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet. 2020;395(10229):1054–1062. doi: 10.1016/S0140-6736(20)30566-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Services DoHaH Victorian coronavirus (COVID-19) data 2020. https://www.dhhs.vic.gov.au/victorian-coronavirus-covid-19-data Available from:
- 3.Terkelsen C.J., Sørensen J.T., Maeng M., Jensen L.O., Tilsted H.-H., Trautner S., et al. System delay and mortality among patients with STEMI treated with primary percutaneous coronary intervention. JAMA. 2010;304(7):763–771. doi: 10.1001/jama.2010.1139. [DOI] [PubMed] [Google Scholar]
- 4.Cannon C.P., Gibson C.M., Lambrew C.T., Shoultz D.A., Levy D., French W.J., et al. Relationship of symptom-onset-to-balloon time and door-to-balloon time with mortality in patients undergoing angioplasty for acute myocardial infarction. JAMA. 2000;283(22):2941–2947. doi: 10.1001/jama.283.22.2941. [DOI] [PubMed] [Google Scholar]
- 5.Scholz K.H., Maier S.K.G., Maier L.S., Lengenfelder B., Jacobshagen C., Jung J., et al. Impact of treatment delay on mortality in ST-segment elevation myocardial infarction (STEMI) patients presenting with and without haemodynamic instability: results from the German prospective, multicentre FITT-STEMI trial. Eur Heart J. 2018;39(13):1065–1074. doi: 10.1093/eurheartj/ehy004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mafham M.M., Spata E., Goldacre R., Gair D., Curnow P., Bray M., et al. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;396(10248):381–389. doi: 10.1016/S0140-6736(20)31356-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Solomon M.D., McNulty E.J., Rana J.S., Leong T.K., Lee C., Sung S.-H., et al. The Covid-19 pandemic and the incidence of acute myocardial infarction. N Engl J Med. 2020;383(7):691–693. doi: 10.1056/NEJMc2015630. [DOI] [PubMed] [Google Scholar]
- 8.Garcia S., Albaghdadi M.S., Meraj P.M., Schmidt C., Garberich R., Jaffer F.A., et al. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol. 2020;75(22):2871. doi: 10.1016/j.jacc.2020.04.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.De Filippo O., D’Ascenzo F., Angelini F., Bocchino P.P., Conrotto F., Saglietto A., et al. Reduced rate of hospital admissions for ACS during Covid-19 outbreak in Northern Italy. N Engl J Med. 2020;383(1):88–89. doi: 10.1056/NEJMc2009166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rodríguez-Leor O., Alvarez-Álvarez B., Ojeda S., Martín-Moreiras J., Rumoroso J., López-Palop R., et al. Impact of the COVID-19 pandemic on interventional cardiology activity in Spain. REC: Interventional Cardiology (English Edition) 2020;2(2):82–89. . [Google Scholar]
- 11.Toner L., Koshy A.N., Hamilton G.W., Clark D., Farouque O., Yudi M.B. Acute coronary syndromes undergoing percutaneous coronary intervention in the COVID-19 era: comparable case volumes but delayed symptom onset to hospital presentation. Eur Heart J Qual Care Clin Outcomes. 2020;6(3):225–226. doi: 10.1093/ehjqcco/qcaa038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tam C.F., Cheung K.S., Lam S., Wong A., Yung A., Sze M., et al. Impact of Coronavirus Disease 2019 (COVID-19) outbreak on ST-segment-elevation myocardial infarction care in Hong Kong, China. Circ Cardiovasc Qual Outcomes. 2020;13(4):e006631. doi: 10.1161/CIRCOUTCOMES.120.006631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Saul A., Scott N., Crabb B.S., Majumdar S.S., Coghlan B., Hellard M.E. Victoria’s response to a resurgence of COVID-19 has averted 9,000-37,000 cases in July 2020. Med J Aust. 2020 doi: 10.5694/mja2.50872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schiavone M., Gobbi C., Biondi-Zoccai G., D'Ascenzo F., Palazzuoli A., Gasperetti A., et al. Acute coronary syndromes and Covid-19: exploring the uncertainties. J Clin Med. 2020;9(6):1683. doi: 10.3390/jcm9061683. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lefkovits J., Brennan A., Dinh D., Stub D., Carruthers H., Doyle J., et al. August 2019. The Victorian Cardiac Outcome Registry Annual Report 2018.; 2019. Report No.: 6. [Google Scholar]
- 16.Department of Health and Human Services All Victorian SARS-CoV-2 cases by local government area, postcode and acquired source. https://discover.data.vic.gov.au/dataset/all-victorian-sars-cov-2-cases-by-local-government-area-postcode-and-acquired-source Available from:
- 17.Department of Health and Human Services Victoria’s raodmap for reopening - How we live in Metropolitan Melbourne 2020. https://www.amaze.org.au/wp-content/uploads/2020/09/Victoria-roadmap-Melbourne-Metro_0.pdf Available from:
- 18.Ajani A.E., Szto G., Duffy S.J., Eccleston D., Clark D.J., Lefkovits J., et al. The foundation and launch of the Melbourne Interventional Group: a collaborative interventional cardiology project. Heart Lung Circ. 2006;15(1):44–47. doi: 10.1016/j.hlc.2005.08.001. [DOI] [PubMed] [Google Scholar]
- 19.Thygesen K., Alpert J.S., Jaffe A.S., Chaitman B.R., Bax J.J., Morrow D.A., et al. Fourth universal definition of myocardial infarction (2018) Eur Heart J. 2019;40(3):237–269. doi: 10.1093/eurheartj/ehy462. [DOI] [PubMed] [Google Scholar]
- 20.Ball J., Nehme Z., Bernard S., Stub D., Stephenson M., Smith K. Collateral damage: hidden impact of the COVID-19 pandemic on the out-of-hospital cardiac arrest system-of-care. Resuscitation. 2020;156:157–163. doi: 10.1016/j.resuscitation.2020.09.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Baldi E., Sechi G.M., Mare C., Canevari F., Brancaglione A., Primi R., et al. Out-of-hospital cardiac arrest during the Covid-19 outbreak in Italy. N Engl J Med. 2020;383(5):496–498. doi: 10.1056/NEJMc2010418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Allahwala U.K., Denniss A.R., Zaman S., Bhindi R. Cardiovascular disease in the post-COVID-19 Era - the impending tsunami? Heart Lung Circ. 2020;29(6):809–811. doi: 10.1016/j.hlc.2020.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Lai P.H., Lancet E.A., Weiden M.D., Webber M.P., Zeig-Owens R., Hall C.B., et al. Characteristics associated with out-of-hospital cardiac arrests and resuscitations during the Novel Coronavirus Disease 2019 pandemic in New York City. JAMA Cardiol. 2020;5(10):1154–1163. doi: 10.1001/jamacardio.2020.2488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Wong L., Hawkins J., Langness S., Murrell K.L., Iris P., Sammann A. Where are all the patients? Addressing Covid-19 fear to encourage sick patients to seek emergency care. NEJM Catal. 2020 [Google Scholar]
- 25.De Rosa S., Spaccarotella C., Basso C., Calabrò M.P., Curcio A., Filardi P.P., et al. Reduction of hospitalizations for myocardial infarction in Italy in the COVID-19 era. Eur Heart J. 2020;41(22):2083–2088. doi: 10.1093/eurheartj/ehaa409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.De Luca G., Suryapranata H., Ottervanger J.P., Antman E.M. Time delay to treatment and mortality in primary angioplasty for acute myocardial infarction: every minute of delay counts. Circulation. 2004;109(10):1223–1225. doi: 10.1161/01.CIR.0000121424.76486.20. [DOI] [PubMed] [Google Scholar]
- 27.McNamara R.L., Wang Y., Herrin J., Curtis J.P., Bradley E.H., Magid D.J., et al. Effect of door-to-balloon time on mortality in patients with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2006;47(11):2180–2186. doi: 10.1016/j.jacc.2005.12.072. [DOI] [PubMed] [Google Scholar]
- 28.Brodie B.R., Webb J., Cox D.A., Qureshi M., Kalynych A., Turco M., et al. Impact of time to treatment on myocardial reperfusion and infarct size with primary percutaneous coronary intervention for acute myocardial infarction (from the EMERALD Trial) Am J Cardiol. 2007;99(12):1680–1686. doi: 10.1016/j.amjcard.2007.01.047. [DOI] [PubMed] [Google Scholar]
- 29.Popovic B., Varlot J., Metzdorf P.A., Jeulin H., Goehringer F., Camenzind E. Changes in characteristics and management among patients with ST-elevation myocardial infarction due to COVID-19 infection. Catheter Cardiovasc Interv. 2021;97(3):E319–E326. doi: 10.1002/ccd.29114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Andrew E., Nehme Z., Stephenson M., Walker T., Smith K. The impact of the COVID-19 pandemic on demand for emergency ambulances in Victoria, Australia. Prehosp Emerg Care. 2021:1–8. doi: 10.1080/10903127.2021.1944409. [DOI] [PubMed] [Google Scholar]
- 31.Jennings G.L.R. COVID, ACE inhibitors/ARBs, and cardiovascular diseases. Med J Aust. 2020;212(11):502–503. doi: 10.5694/mja2.50622. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.