Multisystem inflammatory syndrome in children (MIS-C), also called pediatric inflammatory multisystem syndrome, is characterized by a wide range of symptoms and can present a diagnostic challenge given its myriad presentations. On top of the more well-known inflammatory manifestations of MIS-C, recent reports have also surfaced of MIS-C causing increased intracranial pressure.1 , 2 MIS-C can present similarly to other systemic inflammatory disorders such as Kawasaki disease and can be especially difficult to distinguish from Kawasaki disease if a Kawasaki-like presentation is accompanied by a positive test for coronavirus disease 2019 (COVID-19).3
In adults, ocular manifestations of COVID-19 include nonspecific symptoms such as conjunctival hyperemia, chemosis, epiphora, and increased secretions.4 However, there is a relative paucity of literature regarding ocular manifestations of COVID-19 in children relative to adults. Some documented pediatric symptoms include a similar conjunctivitis presentation, along with increased conjunctival discharge, ocular pain, and eyelid swelling,5 but pediatric MIS-C is far from completely characterized.
Here we present a pediatric patient who developed bilateral papilledema and abducens nerve palsy in the setting of MIS-C to highlight the potential increased intracranial hypertension and neurologic complications of this inflammatory condition. Institutional review board approval was obtained at the Washington University in St. Louis, and consent was provided by the patient’s parents.
A 12-year-old boy with no past medical history and a past ocular history of myopia, astigmatism, and mild amblyopia OD presented to our institution in May 2020 with fever, vomiting, and diarrhea. These symptoms were accompanied by headache, fatigue, dysgeusia, photophobia, and 2 episodes of epistaxis on the day of presentation. The patient’s father had experienced similar symptoms and anosmia following recent domestic travel but was not tested for COVID-19. The patient did not have any respiratory or ophthalmic symptoms at presentation. Rapid streptococcal antigen and COVID-19 reverse transcription polymerase chain reaction tests were performed, both of which were negative, and the patient was discharged home. The patient returned 3 days later for persistent intermittent fever and diarrhea and was admitted. An infectious disease panel was notable for positive severe acute respiratory syndrome coronavirus 2 IgG.
Erythrocyte sedimentation rate and C-reactive protein were elevated at 30 mm/h and 325.0 mg/L, respectively. Complete blood count was notable for reduced hemoglobin (12.0 g/dL), hematocrit (35.4%), and platelets (57,000/µL). During his hospital stay, the patient developed shock, hypotension, hypercoagulability, hyponatremia, acute kidney failure, and acute respiratory failure. An electrocardiogram showed first-degree atrioventricular block, and repeat echocardiograms showed coronary artery dilation and systolic dysfunction indicative of myocarditis. The patient was diagnosed with MIS-C and managed with intravenous immunoglobulin, intravenous hydrocortisone, and enoxaparin.
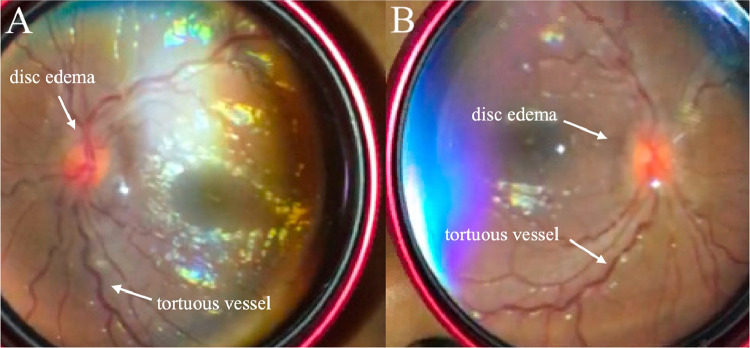
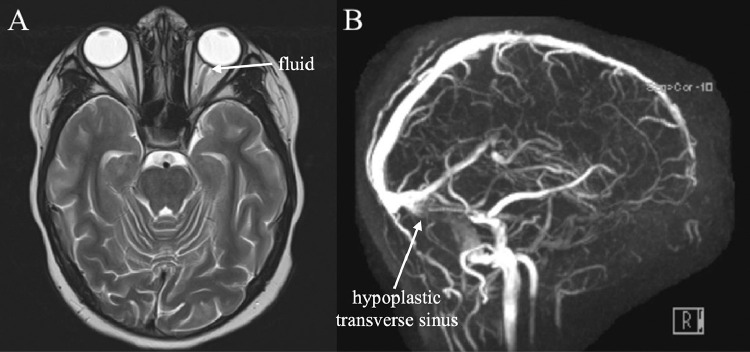
One week into admission, the patient complained of intermittent episodes of headache accompanied by bilateral blurred vision and binocular diplopia. On ophthalmologic examination, his best-corrected near visual acuity was 20/20-2 OD and 20/20 OS. Colour vision on Ishihara testing and intraocular pressures were normal. There was no afferent pupillary defect. Slit-lamp examination of the anterior segment was normal. Fundus examination revealed bilateral grade II–III papilledema (Fig. 1 ) with elevation of the optic nerve heads and peripapillary retinal nerve fibre layer and tortuosity of the retinal vasculature. Extraocular motility examination demonstrated a right esotropia of 15 prism diopters and a –0.5 abduction deficit of the right eye consistent with a right abducens nerve palsy, likely secondary to increased intracranial pressure. Magnetic resonance imaging and magnetic resonance venogram of the head were negative for dural venous sinus thrombosis, though a suspected congenitally hypoplastic left transverse venous sinus was noted (Fig. 2 ). A lumbar puncture was not performed because the patient’s clinical symptoms were improving and his concurrent intravenous immunoglobulin therapy might confound the cell count, IgG index, and opening pressure results. The patient’s blurry vision and diplopia resolved during his hospital course, so observation was recommended. He was discharged 12 days after admission with continuing treatment on acetaminophen, clopidogrel, Aspirin, and lisinopril.
Fig. 1.
Fundoscopic examination of (A) right eye and (B) left eye. Optic discs show swelling consistent with bilateral grade II–III papilledema, in addition to elevation of the optic nerve heads and peripapillary retinal nerve fibre layer and retinal vessel tortuosity.
Fig. 2.
Magnetic resonance imaging (A) and magnetic resonance venography (B). (A) Fluid along optic nerve sheath suggests increased intracranial pressure correlating with the patient’s papilledema. (B) Transverse sinus appears hypoplastic without dural venous sinus thrombosis.
Outpatient ophthalmology follow-up at 1.5 months revealed a best-corrected distance visual acuity of 20/25 OD and 20/20 OS with complete resolution of the bilateral papilledema and right abducens nerve palsy. The patient denied any further episodes of diplopia after discharge. He is scheduled to return in 6 months for follow-up.
In this report, we describe a pediatric patient presenting with bilateral optic nerve edema and a concurrent right abducens nerve palsy related to increased intracranial pressure in the setting of COVID-19-associated Kawasaki-like inflammation, MIS-C. Whereas previous studies have focused on the more anterior ocular manifestations of COVID-19 in adults4 and children,5 this case demonstrates neurologic complications of COVID-19-associated MIS-C. This case is, to the best of our knowledge, only the third reported with elevated intracranial pressure and papilledema with abducens nerve palsy1 , 2 and the first to include fundus images.
Though the precise etiology of the increased intracranial pressure remains unclear, it is likely to be a contributing factor to the ocular and neurologic deficits observed in this MIS-C patient. Lumbar puncture was not attained and elevated opening pressure could not be confirmed because of the confounding impact of the patient’s immunoglobulin therapy and the resolution of his symptoms. However, the patient’s constellation of papilledema, abducens nerve palsy, and headaches is consistent with literature reports of elevated intracranial pressure in patients with MIS-C.
Familiarity with MIS-C ocular presentations can better inform patient care as the COVID-19 pandemic continues to spread at an alarming pace among the pediatric population. Awareness of the ocular and neurologic manifestations of MIS-C is important in recognizing the syndrome quickly, and neurologic complaints of visual disturbances, headache, and ocular movement abnormality should raise suspicion for increased intracranial pressure and possible MIS-C. In patients with these symptoms, a dilated fundus examination may be of benefit.
Acknowledgments
Acknowledgement
The authors acknowledge Adam Baim for the optic disc photos.
Supported by
This work was supported by an unrestricted grant to the Department of Ophthalmology and Visual Sciences at Washington University in St. Louis from research to prevent blindness.
Footnotes and Disclosure
The authors have no proprietary or commercial interest in any materials discussed in this correspondence.
References
- 1.Baccarella A, Linder A, Spencer R, et al. Increased intracranial pressure in the setting of multisystem inflammatory syndrome in children, associated with COVID-19. Pediatr Neurol. 2021;115:48–49. doi: 10.1016/j.pediatrneurol.2020.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Becker AE, Chiotos K, McGuire JL, Bruins BB, Alcamo AM. Intracranial hypertension in multisystem inflammatory syndrome in children. J Pediatr. 2021;233:263–267. doi: 10.1016/j.jpeds.2021.02.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jones VG, Mills M, Suarez D, et al. COVID-19 and Kawasaki disease: novel virus and novel case. Hosp Pediatr. 2020;10:537–540. doi: 10.1542/hpeds.2020-0123. [DOI] [PubMed] [Google Scholar]
- 4.Wu P, Duan F, Luo C, et al. Characteristics of ocular findings of patients with coronavirus disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol. 2020;138:575–578. doi: 10.1001/jamaophthalmol.2020.1291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ma N, Li P, Wang X, et al. Ocular manifestations and clinical characteristics of children with laboratory-confirmed COVID-19 in Wuhan, China. JAMA Ophthalmol. 2020;138:1079–1086. doi: 10.1001/jamaophthalmol.2020.3690. [DOI] [PMC free article] [PubMed] [Google Scholar]