Abstract
Objectives
In December 2020, CDC launched the Pharmacy Partnership for Long-Term Care Program to facilitate COVID-19 vaccination of residents and staff in long-term care facilities (LTCFs), including assisted living (AL) and other residential care (RC) communities. We aimed to assess vaccine uptake in these communities and identify characteristics that might impact uptake.
Design
Cross-sectional study.
Setting and Participants
AL/RC communities in the Pharmacy Partnership for Long-Term Care Program that had ≥1 on-site vaccination clinic during December 18, 2020–April 21, 2021.
Methods
We estimated uptake using the cumulative number of doses of COVID-19 vaccine administered and normalizing by the number of AL/RC community beds. We estimated the percentage of residents vaccinated in 3 states using AL census counts. We linked community vaccine administration data with county-level social vulnerability index (SVI) measures to calculate median vaccine uptake by SVI tertile.
Results
In AL communities, a median of 67 residents [interquartile range (IQR): 48-90] and 32 staff members (IQR: 15-60) per 100 beds received a first dose of COVID-19 vaccine at the first on-site clinic; in RC, a median of 8 residents (IQR: 5-10) and 5 staff members (IQR: 2-12) per 10 beds received a first dose. Among 3 states with available AL resident census data, median resident first-dose uptake at the first clinic was 93% (IQR: 85-108) in Connecticut, 85% in Georgia (IQR: 70-102), and 78% (IQR: 56-91) in Tennessee. Among both residents and staff, cumulative first-dose vaccine uptake increased with increasing social vulnerability related to housing type and transportation.
Conclusions and Implications
COVID-19 vaccination of residents and staff in LTCFs is a public health priority. On-site clinics may help to increase vaccine uptake, particularly when transportation may be a barrier. Ensuring steady access to COVID-19 vaccine in LTCFs following the conclusion of the Pharmacy Partnership is critical to maintaining high vaccination coverage among residents and staff.
Keywords: COVID-19, vaccination, vaccination coverage, long-term care
Following the US Food and Drug Administration's Emergency Use Authorizations of the first vaccines for prevention of coronavirus disease 2019 (COVID-19), the Advisory Committee on Immunization Practices recommended that residents and staff members of long-term care facilities (LTCFs) be prioritized in the first phase of COVID-19 vaccine allocation.1 As congregate settings, LTCFs pose increased risk for transmission of SARS-CoV-2, the virus that causes COVID-19,2 and residents are also at increased risk for severe COVID-19 illness due to older age or underlying health conditions.3 LTCFs include skilled nursing facilities (SNFs) and other nursing homes, assisted living (AL) and other residential care (RC) communities, and residential facilities for persons with intellectual and developmental disabilities. AL/RC communities provide assistance with activities of daily living (eg, bathing and toileting) and may also provide some health care services (eg, management and administration of medications) in a residential setting; these communities represent approximately 44% of US LTCFs.4 Data from October 2020 indicated that 22% of AL/RC communities with available data reported at least 1 case of COVID-19 among residents or staff members, and that COVID-19–associated mortality among the resident population was significantly higher than that among the general population (21% vs 3%).5
To facilitate COVID-19 vaccination of residents and staff members in LTCFs, CDC launched the Pharmacy Partnership for Long-Term Care Program in December 2020.6 This program, a public-private partnership with 3 pharmacies (CVS, Managed Health Care Associates, and Walgreens), conducted on-site visits to enrolled LTCFs to provide end-to-end management of the COVID-19 vaccination process, including appropriate storage, handling, and transport of vaccines, vaccine administration, and fulfillment of reporting requirements. More than 62,000 LTCFs across 49 states enrolled in the program and received on-site vaccinations for residents and staff members. Early estimates from the first month of the program indicated that a median of 78% of residents and 38% of staff members in SNFs received at least a first dose of COVID-19 vaccine.7 Complementing these results, we aimed to assess vaccine uptake in AL/RC communities participating in the program and identify community and county characteristics that might impact uptake. Specifically, we assessed the association between uptake and county-level social vulnerability, which has been shown to impact COVID-19 vaccine uptake in LTCFs8 and broader population settings.9, 10, 11
Methods
Participating pharmacies reported LTCF-level aggregate COVID-19 vaccine administration data to CDC through a web-based data platform. This analysis included AL/RC communities that had at least 1 on-site vaccination clinic run by a participating pharmacy from December 18, 2020 (date of first on-site clinic), through April 21, 2021 (date of clinic completion for >99% enrolled communities; data as of April 28, 2021). Communities were classified as AL or RC based on self-identification during program signup. Pfizer-BioNTech COVID-19 vaccine and Moderna COVID-19 vaccine were administered through the program; both products required a 2-dose series for completion. Pharmacies generally conducted 3 on-site clinics at each community for administration of first and second vaccine doses; clinics were scheduled approximately 21-28 days apart depending on vaccine product. Smaller communities may have received only 2 clinics if all residents and staff members were vaccinated and a third clinic was not deemed necessary.
To estimate uptake, we calculated the cumulative number of first and second doses of vaccine administered to residents and staff members at each clinic and normalized by the reported total bed capacity per community (presented as number vaccinated per 100 reported beds for AL communities and per 10 reported beds for RC communities to account for differences in average community size; Supplementary Tables 1-2). Additionally, we estimated the percentage of residents who received a first dose of COVID-19 vaccine in AL communities in 3 states (Connecticut,12 Georgia,13 and Tennessee14) that reported resident census counts (number of occupied beds) in publicly available COVID-19 reports obtained via systematic website searches5 during February 2-4, 2021. AL census counts were not available for additional states; RC census counts were available only for a small number of communities and were not included because of insufficient sample size. We linked community-level vaccination data from these states to AL census data using standardized values of community name and address. We calculated the estimated first-dose uptake per 100 residents by dividing the number of first doses of COVID-19 vaccine administered by the reported census count. Estimated first-dose uptake exceeded 100% if reported doses administered were greater than resident census counts.
We linked AL/RC communities with county-level social vulnerability index (SVI) measures.15 SVI is based on county rankings of 15 census measures associated with social determinants of health and is summarized in 4 themes: (1) socioeconomic status, (2) household composition and disability status, (3) racial or ethnic minority status and language, and (4) housing type and transportation. A higher SVI score indicates higher social vulnerability. For communities without a reported Federal Information Processing Standards (FIPS) code (used for identification of US counties), the address zip code was mapped to the corresponding county FIPS code in the US Department of Housing and Urban Development–US Postal Service zip Code Crosswalk.16 When multiple counties mapped to a single zip code, we chose the county with the highest proportion of residential and business addresses. Counties were classified into tertiles for each of the 4 SVI themes. We calculated the median vaccine first-dose uptake among residents and staff members of AL/RC communities by SVI tertile.
All analyses were performed using SAS statistical software (version 9.4; SAS Institute, Cary, NC) and R (version 4.0.2, R Core Team, Vienna, Austria). This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy.∗
Results
As of April 21, 2021, 18,980 AL communities and 16,874 RC communities conducted COVID-19 vaccination clinics through the Pharmacy Partnership for Long Term Care Program. In total, 765,792 residents and 513,293 staff members in AL communities and 222,987 residents and 213,146 staff in RC communities received at least 1 COVID-19 vaccine dose. The median bed size was 35 [interquartile range (IQR): 10-77] among participating AL communities and 6 (IQR: 4-6) among RC communities.
In AL communities, a median of 67 residents (IQR: 48-90) and 32 staff members (IQR: 15-60) per 100 beds received a first dose of vaccine at the first on-site clinic; in RC communities, a median of 8 residents (IQR: 5-10) and 5 staff members (IQR: 2-12) per 10 beds received a first dose (Table 1 ). Cumulatively as of April 21, 2021, a median of 75 residents (IQR: 54-100) and 47 staff members (IQR: 24-85) per 100 beds in AL communities received a first dose of vaccine, and 66 residents (IQR: 45-88) and 37 staff members (IQR: 17-70) per 100 beds received a second dose. In RC communities, a median of 9 residents (IQR: 7-13) and 8 staff members (IQR: 3-18) per 10 beds received a first dose of vaccine, and 8 residents (IQR: 5-10) and 7 staff members (IQR: 2-14) per 10 beds received a second dose.
Table 1.
COVID-19 Vaccine Uptake in Assisted Living and Residential Care Communities∗—Pharmacy Partnership for Long-Term Care Program, December 2020–April 2021
| Assisted Living: Cumulative Vaccine Uptake, Median (IQR) per 100 Beds† (n = 18,980) |
Residential Care: Cumulative Vaccine Uptake, Median (IQR) per 10 Beds† (n = 16,874) |
|
|---|---|---|
| Residents | ||
| First dose | ||
| Clinic 1 | 67 (48-90) | 8 (5-10) |
| Clinic 2 | 75 (54-100) | 9 (7-12) |
| Clinic 3‡ | 75 (54-100) | 9 (7-13) |
| Second dose | ||
| Clinic 1 | 0 (0-0) | 0 (0-0) |
| Clinic 2 | 60 (40-82) | 7 (4-10) |
| Clinic 3‡ | 66 (45-88) | 8 (5-10) |
| Staff members | ||
| First dose | ||
| Clinic 1 | 32 (15-60) | 5 (2-12) |
| Clinic 2 | 44 (23-81) | 8 (3-17) |
| Clinic 3‡ | 47 (24-85) | 8 (3-18) |
| Second dose | ||
| Clinic 1 | 0 (0-0) | 0 (0-0) |
| Clinic 2 | 28 (12-56) | 5 (1-10) |
| Clinic 3‡ | 37 (17-70) | 7 (2-14) |
Communities self-identified as assisted living (AL) or other residential care (RC) for this analysis. Classification and characteristics of AL and RC communities can differ by state; however, RC communities are generally smaller than AL communities. Additionally, AL communities might offer various levels of on-site nursing or medical care whereas RC communities might not; the care offered is less extensive than what is offered in a skilled nursing facility or nursing home.
Uptake is presented as number vaccinated per 100 reported beds for AL communities and per 10 reported beds for RC communities to account for differences in community size; median bed size was 35 (interquartile range [IQR]: 10-77) in AL and 6 (IQR: 4-6) in RC.
Smaller communities may not have conducted third clinics if all residents and staff members were vaccinated in the first 2 clinics. Third clinics were conducted in 15,025 (79%) AL communities and 9881 (59%) RC communities as of April 21, 2021.
Resident census data were available for 89 of 118 (75%) participating AL communities in Connecticut, 192 of 330 (58%) in Georgia, and 232 of 289 (80%) in Tennessee (Table 2 ). The median percentage of beds occupied was 68% (IQR: 55-81) in Connecticut, 58% (IQR: 48-69) in Georgia, and 70% (IQR: 58-84) in Tennessee. This resulted in an estimated median resident first-dose uptake of 93% (IQR: 85-108) in Connecticut, 85% in Georgia (IQR: 70-102), and 78% (IQR: 56-91) in Tennessee at the first on-site clinic. Cumulatively as of April 21, 2021, first-dose uptake increased to 106% (IQR: 97-131) in Connecticut, 98% in Georgia (IQR: 84-120), and 88% (IQR: 66-100) in Tennessee.
Table 2.
First-Dose COVID-19 Vaccine Uptake Among Residents, by Bed Capacity and Resident Occupancy, in Assisted Living Communities—Pharmacy Partnership for Long-Term Care Program, December 2020-April 2021
| Variable | CT |
GA |
TN |
|||
|---|---|---|---|---|---|---|
| Unlinked,∗ Median (IQR) (n = 29) |
Linked,∗ Median (IQR) (n = 89) |
Unlinked, Median (IQR) (n = 138) |
Linked, Median (IQR) (n = 192) |
Unlinked, Median (IQR) (n = 57) |
Linked, Median (IQR) (n = 232) |
|
| Occupancy-to-capacity ratio† | 68 (55-81) | 58 (48-69) | 70 (58-84) | |||
| Clinic 1 | ||||||
| Uptake per 100 beds‡ | 55 (41-63) | 68 (55-83) | 51 (31-71) | 49 (36-63) | 54 (42-67) | 53 (40-71) |
| Uptake per 100 residents (%) | 93 (85-108) | 85 (70-102) | 78 (56-91) | |||
| Clinic 2 | ||||||
| Uptake§ per 100 beds | 65 (48-78) | 75 (60-92) | 60 (37-79) | 57 (43-75) | 57 (44-72) | 59 (45-75) |
| Uptake§ per 100 residents (%) | 103 (95-119) | 97 (82-117) | 88 (64-100) | |||
| Clinic 3 | ||||||
| Uptake§ per 100 beds | 65 (52-80) | 77 (61-96) | 61 (38-83) | 59 (44-76) | 57 (44-73) | 59 (46-76) |
| Uptake§ per 100 residents (%) | 106 (97-131) | 98 (84-120) | 88 (66-100) | |||
“Unlinked” indicates communities not matched to publicly available resident census data; “linked” indicates communities matched to resident census data. Uptake per 100 residents was calculated only for linked communities. Census data were available for AL communities in 3 states; RC census data were available only for a small number of facilities and are not presented.
Occupancy-to-capacity ratio was calculated as resident census (dated January 27–February 2, 2021) divided by total number of reported beds.
First-dose uptake per 100 beds was calculated as number of first doses of COVID-19 vaccine administered normalized per 100 reported beds (total bed capacity). First-dose uptake per 100 residents was calculated as number of first doses of COVID-19 vaccine administered normalized per 100 residents in census counts (occupied beds).
Uptake for clinics 2 and 3 is cumulative vaccine uptake inclusive of previous clinics.
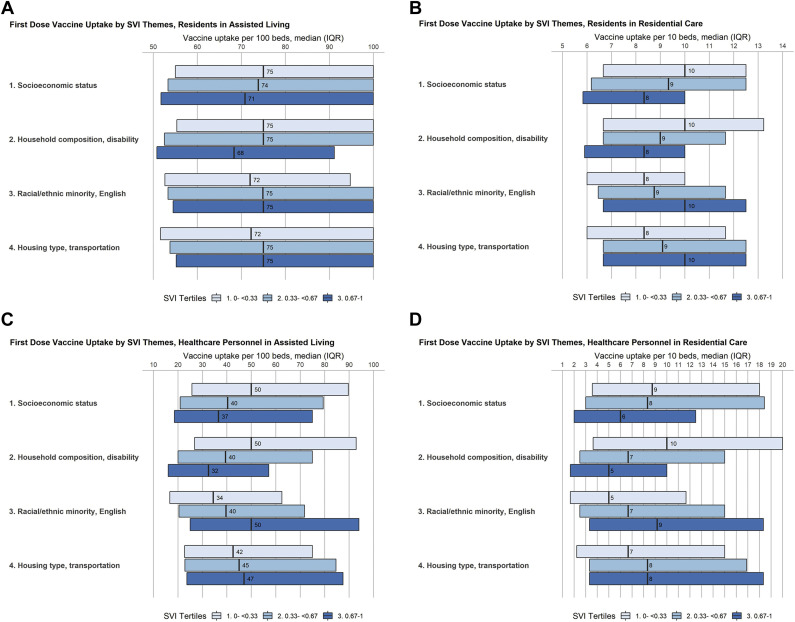
Among the 35,854 participating AL/RC communities, 34,934 (97%) were linked to county-level SVI data. For both residents and staff members, cumulative first-dose vaccine uptake decreased with increasing social vulnerability related to socioeconomic status (SVI theme 1) and household composition and disability status (SVI theme 2) (Figure 1 ). However, uptake increased with increasing social vulnerability related to racial orethnic minority status and language (SVI theme 3) and housing type and transportation (SVI theme 4).
Fig. 1.
First-dose COVID-19 vaccine uptake,∗ by social vulnerability index (SVI) theme† and tertile,‡ among residents and staff members of assisted living (A and B) and other residential care (C and D) communities—Pharmacy Partnership for Long-Term Care Program, December 2020–April 2021. ∗Includes cumulative first-dose vaccine uptake as of April 21, 2021. †SVI ranks counties according to 15 social factors (indicators): (1) percentage of persons with incomes below poverty threshold, (2) percentage of civilian population (aged ≥16 years) that is unemployed, (3) per capita income, (4) percentage of persons aged ≥25 years with no high school diploma, (5) percentage of persons aged ≥65 years, (6) percentage of persons aged ≤17 years, (7) percentage of civilian noninstitutionalized population with a disability, (8) percentage of single-parent households with children aged <18 years, (9) percentage of persons who are racial/ethnic minorities (all persons except non-Hispanic White), (10) percentage of persons aged ≥5 years who speak English “less than well,” (11) percentage of housing structures with ≥10 units (multiunit housing), (12) percentage of housing structures that are mobile homes, (13) percentage households with more persons than rooms (crowding), (14) percentage of households with no vehicle available, and (15) percentage of persons in group quarters. Estimates are created using 2014-2018 (5-year) data from the American Community Survey. The 15 indicators are categorized into 4 themes: (1) socioeconomic status (indicators 1-4), (2) household composition and disability (indicators 5-8), (3) racial/ethnic minority status and language English (indicators 9 and 10), and (4) housing type and transportation (indicators 11-15). Additional details are available at https://www.atsdr.cdc.gov/placeandhealth/svi/documentation/SVI_documentation_2018.html. ‡Higher tertile indicates increased social vulnerability.
Discussion
Early data have indicated that COVID-19 vaccination is effective in reducing the risk for SARS-CoV-2 infection among LTCF residents17; thus, targeted COVID-19 vaccination campaigns, as conducted through the Pharmacy Partnership for Long-Term Care Program, are critical to interrupting virus transmission and decreasing COVID-19–associated morbidity and mortality in LTCFs. Through the Pharmacy Partnership, more than 1.7 million residents and staff members in AL/RC communities received on-site COVID-19 vaccination. First-dose vaccine uptake among both residents and staff increased with subsequent on-site clinics, which could result from doses administered to individuals who were not present at the first clinic (eg, new resident admissions or staff not working during clinic dates) or decreasing vaccine hesitancy over time.
Across 3 states with available resident census data, an estimated median of 78% to 93% of residents were vaccinated at the first on-site clinic in AL communities. These results are consistent with prior analyses indicating that a median of 78% of residents were vaccinated in SNFs during the first month of the program.7 With subsequent clinics, median first-dose uptake among residents in AL communities in these states increased to 88% to 106%. Uptake above 100% likely resulted from new admissions and discharges of residents in these communities; because Pharmacy Partnership data were reported in aggregate at the community level and resident census data were obtained at a single point in time, we could not account or adjust for resident turnover. Other systems to monitor weekly COVID-19 vaccination coverage in long-term care settings, such as the National Healthcare Safety Network (NHSN) LTCF component, can fill this gap following the conclusion of the Pharmacy Partnership program.18 As of June 13, 2021, SNFs are required to report weekly resident and staff COVID-19 vaccination coverage to NHSN.19 Similar vaccination reporting policies for other LTCF settings, including AL/RC communities, could facilitate comprehensive monitoring and evaluation of COVID-19 coverage.
Consistent with our findings, prior analyses of COVID-19 vaccination coverage among the general population by county of residence identified lower vaccination coverage in counties with higher social vulnerability related to socioeconomic status (including income, employment status, and education level) and household composition/disability (including age, single-parent household status, and disability status) but higher vaccination coverage in counties with higher social vulnerability related to racial or ethnic minority status and limited English language fluency.10 Prior analyses examining receipt of COVID-19 vaccine specifically among adults ≥65 years of age also found lower first-dose vaccination coverage associated with social vulnerabilities including poverty, Internet access, and living alone, though no relationship with race or ethnicity.11 Notably, our findings indicated higher uptake associated with social vulnerabilities related to housing type and transportation (including multiunit and mobile home housing, crowding, lack of vehicle availability, and prevalence of institutionalized group quarters), whereas this was not identified among the general population.10 Providing on-site access to vaccination at place of residence or work may help to mitigate access barriers posed by transportation issues, and individuals with these social vulnerabilities may be more likely to seek vaccination through a vaccine delivery program such as the Pharmacy Partnership. With appropriate planning, promotion, and delivery, on-site vaccination programs such as workforce vaccination programs,20 off-site community clinics,21 or mobile clinics22 might similarly increase vaccine uptake across different settings.
These findings are subject to several notable limitations. Firstly, definitions of AL/RC communities vary across jurisdictions, and there may have been misclassification of LTCF types reported to CDC. Resident census data were only available for 3 states and did not include all AL communities within these states; estimated percentage uptake may not be nationally generalizable. We were unable to assess the percentage of staff vaccinated as staffing ratios (number of staff members employed per resident or total bed capacity) vary widely across AL/RC communities.23 In 2014, the national ratio of total nurse and aide staffing hours worked per resident in residential care communities was 2.84 hours per resident per day; state-level estimates ranged from 1.66 to 4.90, indicating wide variability.24 Furthermore, our estimates may underestimate staff member vaccine uptake as we only captured staff vaccinated through the Pharmacy Partnership program and could not account for staff working at multiple communities, intentional staggering of staff vaccination, or staff vaccinated at other locations (eg, at a retail pharmacy). As previously described, we could not account for new resident admissions or discharges at AL/RC communities. Finally, we used county-level estimates of social vulnerability; these factors may vary within large counties, and the characteristics of community locations may not reflect those of residents and staff members admitted from or residing in other localities.
Conclusions and Implications
COVID-19 vaccination of residents and staff members in LTCFs continues to be a public health priority. Though the on-site component of the Pharmacy Partnership for Long-Term Care Program concluded in May 2021, ensuring steady access to vaccine in AL/RC communities and other LTCFs is critical to maintaining high vaccination coverage as new individuals enter the facilities or wish to be vaccinated.6 Additionally, efforts to make vaccine available and accessible to LTCFs and other congregate housing communities with high social vulnerability are critical; delivery strategies such as the on-site clinic model used through the Pharmacy Partnership may help to mitigate access issues related to transportation. Finally, continued, systematic data collection in LTCFs and other high-risk settings is critical to assessing vaccination coverage and impact on COVID-19 disease burden.
Acknowledgments
We thank pharmacy partners from CVS Pharmacy, Managed Health Care Associates, Inc, and Walgreens; residents and staff members in enrolled facilities; state, local, and territorial health departments; Smita Chavan, Sam Cincotta, Nicole Coffin, Rachael Cook, Michelle Hughes, Song Lavalais, Lakshmi Malapati, Adria Mathis, Lauren Moccia, Nadine Shehab, Chelsea Slyker, Nimalie Stone, Kirsten Yates, CDC COVID-19 Response Team; Saahil Madge, Palantir Technologies; Curt Nelson, US Army; and Courtney Bishnoi, David Gifford, Urvi Patel, Lindsay Schwartz, American Health Care Association/National Center for Assisted Living.
Footnotes
The authors declare no conflicts of interest. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
See eg, 45 CFR part 46, 21 CFR part 56; 42 USC §241(d); 5 USC §552a; 44 USC §3501 et seq.
Appendix
Supplementary Table 1.
Facility Characteristics, Clinic Scheduling, and COVID-19 Vaccine First Doses Administered, by State, Among Assisted Living Communities—Pharmacy Partnership for Long-Term Care Program, December 2020–April 2021
| Assisted Living (AL) Communities | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| State/Jurisdiction | No. of Participating AL Communities | No. of Beds |
Clinic 1 Dates |
Total First Doses Administered From Clinic 1 to Clinic 3 |
Median Vaccinated per 100 Beds |
|||||
| Total Across State | Median per AL | Earliest | Latest | Rollout Duration, d | Residents | Staff | Residents | Staff | ||
| AK | 360 | 2228 | 5 | 12/30/2020 | 3/10/2021 | 70 | 2154 | 1701 | 80 | 60 |
| AL | 182 | 8167 | 35 | 1/7/2021 | 3/5/2021 | 57 | 7616 | 4927 | 72 | 38 |
| AR | 37 | 2642 | 70 | 12/29/2020 | 1/19/2021 | 21 | 1877 | 788 | 68 | 25 |
| AZ | 648 | 26,394 | 10 | 1/15/2021 | 3/25/2021 | 69 | 21,935 | 10,465 | 78 | 40 |
| CA | 1103 | 70,158 | 40 | 1/2/2021 | 3/4/2021 | 61 | 46,299 | 37,182 | 70 | 64 |
| CO | 604 | 25,010 | 16 | 12/31/2020 | 2/2/2021 | 33 | 21,532 | 22,375 | 75 | 57 |
| CT | 120 | 12,424 | 96 | 12/21/2020 | 2/5/2021 | 46 | 10,054 | 8447 | 74 | 58 |
| DC | 7 | 604 | 65 | 1/4/2021 | 1/16/2021 | 12 | 930 | 521 | 150 | 88 |
| DE | 30 | 2166 | 63 | 1/5/2021 | 2/5/2021 | 31 | 2158 | 1412 | 70 | 52 |
| FL | 1787 | 81,845 | 14 | 12/22/2020 | 2/12/2021 | 52 | 68,851 | 37,586 | 82 | 46 |
| GA | 330 | 24,131 | 70 | 1/6/2021 | 3/4/2021 | 57 | 15,824 | 8805 | 60 | 30 |
| HI | 17 | 2057 | 104 | 1/2/2021 | 1/28/2021 | 26 | 1952 | 1866 | 85 | 87 |
| IA | 260 | 14,886 | 48 | 12/28/2020 | 2/12/2021 | 46 | 10,841 | 6005 | 62 | 33 |
| ID | 139 | 6921 | 36 | 12/29/2020 | 2/15/2021 | 48 | 4994 | 2570 | 71 | 31 |
| IL | 557 | 37,400 | 60 | 12/29/2020 | 2/24/2021 | 57 | 31,389 | 21,378 | 75 | 44 |
| IN | 250 | 20,737 | 66 | 12/29/2020 | 2/15/2021 | 48 | 14,466 | 5343 | 65 | 24 |
| KS | 193 | 8998 | 36 | 12/28/2020 | 2/5/2021 | 39 | 8224 | 4658 | 76 | 42 |
| KY | 206 | 11,470 | 50 | 12/21/2020 | 2/3/2021 | 44 | 10,122 | 6090 | 80 | 44 |
| LA | 116 | 7472 | 60 | 12/29/2020 | 2/23/2021 | 56 | 4566 | 2509 | 65 | 28 |
| MA | 259 | 19,880 | 78 | 1/2/2021 | 2/9/2021 | 38 | 17,785 | 16,597 | 80 | 78 |
| MD | 769 | 17,961 | 8 | 1/6/2021 | 3/24/2021 | 77 | 17,116 | 12,709 | 88 | 60 |
| ME | 90 | 3910 | 23 | 1/4/2021 | 2/12/2021 | 39 | 4500 | 2170 | 88 | 63 |
| MI | 707 | 28,879 | 20 | 1/4/2021 | 3/16/2021 | 71 | 23,801 | 13,349 | 74 | 35 |
| MN | 711 | 40,063 | 44 | 1/4/2021 | 2/18/2021 | 45 | 32,258 | 24,790 | 76 | 56 |
| MO | 278 | 16,738 | 52 | 1/2/2021 | 2/21/2021 | 50 | 13,475 | 6647 | 66 | 31 |
| MS | 147 | 6469 | 34 | 1/6/2021 | 2/7/2021 | 32 | 4741 | 1984 | 73 | 27 |
| MT | 133 | 5297 | 18 | 12/31/2020 | 2/12/2021 | 43 | 4471 | 3914 | 79 | 45 |
| NC | 428 | 26,729 | 60 | 12/28/2020 | 3/20/2021 | 82 | 21,219 | 10,997 | 69 | 33 |
| ND | 32 | 1644 | 42 | 12/30/2020 | 1/28/2021 | 29 | 1243 | 798 | 78 | 32 |
| NE | 128 | 7408 | 46 | 12/28/2020 | 2/15/2021 | 49 | 5545 | 3466 | 71 | 43 |
| NH | 59 | 3493 | 56 | 1/6/2021 | 2/5/2021 | 30 | 3040 | 2633 | 79 | 66 |
| NJ | 263 | 25,862 | 97 | 1/2/2021 | 3/10/2021 | 67 | 18,725 | 15,632 | 66 | 48 |
| NM | 175 | 4049 | 15 | 12/30/2020 | 2/11/2021 | 43 | 3594 | 3053 | 75 | 67 |
| NV | 291 | 7893 | 10 | 12/31/2020 | 2/25/2021 | 56 | 6307 | 4186 | 80 | 60 |
| NY | 411 | 38,560 | 79 | 12/30/2020 | 2/17/2021 | 49 | 26,444 | 20,015 | 68 | 41 |
| OH | 537 | 47,625 | 76 | 12/18/2020 | 2/12/2021 | 56 | 31,848 | 20,535 | 61 | 34 |
| OK | 133 | 8616 | 58 | 1/8/2021 | 2/4/2021 | 27 | 5564 | 4144 | 62 | 35 |
| OR | 312 | 19,276 | 51 | 12/21/2020 | 2/18/2021 | 59 | 14,927 | 10,084 | 75 | 48 |
| PA | 559 | 41,641 | 66 | 12/29/2020 | 2/26/2021 | 59 | 31,711 | 23,077 | 66 | 45 |
| PR | 901 | 18,535 | 16 | 1/4/2021 | 3/10/2021 | 65 | 16,541 | 12,881 | 90 | 67 |
| RI | 62 | 4824 | 67 | 12/31/2020 | 2/18/2021 | 49 | 3415 | 2342 | 73 | 46 |
| SC | 299 | 16,184 | 48 | 12/28/2020 | 2/19/2021 | 53 | 13,331 | 6305 | 74 | 33 |
| SD | 60 | 2394 | 29 | 12/28/2020 | 1/21/2021 | 24 | 2262 | 520 | 74 | 8 |
| TN | 278 | 19,377 | 60 | 1/5/2021 | 3/2/2021 | 56 | 12,667 | 7841 | 59 | 34 |
| TX | 1250 | 67,418 | 42 | 12/28/2020 | 3/2/2021 | 64 | 55,122 | 41,833 | 77 | 50 |
| UT | 147 | 9282 | 55 | 1/2/2021 | 2/17/2021 | 46 | 6622 | 5301 | 66 | 52 |
| VA | 377 | 28,839 | 72 | 12/30/2020 | 2/15/2021 | 47 | 24,958 | 17,185 | 70 | 49 |
| VT | 49 | 2092 | 35 | 12/30/2020 | 2/3/2021 | 35 | 1780 | 1425 | 81 | 68 |
| WA | 366 | 28,650 | 64 | 12/30/2020 | 2/16/2021 | 48 | 25,402 | 15,396 | 79 | 46 |
| WI | 1802 | 31,169 | 7 | 1/10/2021 | 4/6/2021 | 86 | 28,627 | 16,543 | 81 | 50 |
| WY | 21 | 1456 | 61 | 1/6/2021 | 1/27/2021 | 21 | 967 | 313 | 66 | 22 |
Supplementary Table 2.
Facility Characteristics, Clinic Scheduling, and COVID-19 Vaccine First Doses Administered, by State, Among Other Residential Care Communities—Pharmacy Partnership for Long-Term Care Program, December 2020–April 2021
| Residential Care (RC) Communities | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| State/Jurisdiction | No. of Participating RC Communities | No. of Beds |
Clinic 1 Dates |
Total First Doses Administered From Clinic 1 to Clinic 3 |
Median Vaccinated per 10 Beds |
|||||
| Total Across State | Median per RC | Earliest | Latest | Rollout Duration, d | Residents | Staff | Residents | Staff | ||
| AK | 6 | 21 | 4 | 1/11/2021 | 2/10/2021 | 30 | 15 | 11 | 7 | 2 |
| AL | 7 | 497 | 62 | 1/15/2021 | 2/5/2021 | 21 | 343 | 84 | 7 | 1 |
| AR | 7 | 344 | 60 | 12/30/2020 | 1/15/2021 | 16 | 229 | 33 | 7 | 1 |
| AZ | 113 | 1312 | 3 | 1/16/2021 | 2/10/2021 | 25 | 1213 | 839 | 10 | 7 |
| CA | 5318 | 96,505 | 6 | 12/28/2020 | 4/8/2021 | 101 | 66,814 | 76,509 | 8 | 10 |
| CO | 29 | 373 | 6 | 1/6/2021 | 1/28/2021 | 22 | 224 | 466 | 8 | 15 |
| CT | 191 | 4442 | 6 | 1/4/2021 | 2/17/2021 | 44 | 4460 | 3226 | 10 | 6 |
| DE | 34 | 804 | 4 | 1/10/2021 | 2/8/2021 | 29 | 593 | 424 | 11 | 7 |
| FL | 312 | 4927 | 6 | 1/11/2021 | 2/17/2021 | 37 | 4849 | 3390 | 9 | 7 |
| GA | 113 | 1437 | 4 | 1/11/2021 | 3/4/2021 | 52 | 1335 | 760 | 10 | 7 |
| HI | 8 | 151 | 19 | 12/28/2020 | 1/30/2021 | 33 | 157 | 145 | 7 | 9 |
| IA | 241 | 1626 | 4 | 1/5/2021 | 2/13/2021 | 39 | 2904 | 2350 | 12 | 8 |
| ID | 5 | 358 | 50 | 1/14/2021 | 1/30/2021 | 16 | 210 | 76 | 6 | 1 |
| IL | 123 | 6286 | 10 | 12/29/2020 | 2/24/2021 | 57 | 4774 | 3181 | 9 | 5 |
| IN | 61 | 4804 | 80 | 1/12/2021 | 2/18/2021 | 37 | 3554 | 1064 | 7 | 1 |
| KS | 83 | 3290 | 9 | 12/30/2020 | 2/9/2021 | 41 | 2603 | 1662 | 8 | 6 |
| KY | 14 | 653 | 49 | 12/23/2020 | 2/12/2021 | 51 | 718 | 497 | 9 | 6 |
| LA | 35 | 1066 | 18 | 1/7/2021 | 2/6/2021 | 30 | 934 | 598 | 8 | 9 |
| MA | 1309 | 11,865 | 5 | 1/2/2021 | 3/15/2021 | 72 | 13,275 | 19,896 | 10 | 14 |
| MD | 494 | 5872 | 5 | 1/20/2021 | 3/24/2021 | 63 | 12,009 | 10,135 | 15 | 12 |
| ME | 124 | 742 | 4 | 12/30/2020 | 2/22/2021 | 54 | 1179 | 1670 | 10 | 20 |
| MI | 2484 | 37,344 | 6 | 1/4/2021 | 4/21/2021 | 107 | 27,359 | 16,157 | 8 | 5 |
| MN | 412 | 2815 | 4 | 1/9/2021 | 3/19/2021 | 69 | 2577 | 3154 | 10 | 10 |
| MO | 213 | 5437 | 12 | 12/29/2020 | 2/23/2021 | 56 | 4061 | 2579 | 7 | 3 |
| MS | 22 | 229 | 4 | 1/12/2021 | 2/5/2021 | 24 | 214 | 83 | 10 | 5 |
| NC | 303 | 6913 | 6 | 12/28/2020 | 2/26/2021 | 60 | 6284 | 3621 | 8 | 7 |
| ND | 9 | 362 | 42 | 12/31/2020 | 1/14/2021 | 14 | 383 | 176 | 7 | 3 |
| NE | 1 | 162 | — | 1/17/2021 | — | — | 73 | 45 | 5 | 3 |
| NH | 22 | 802 | 15 | 1/6/2021 | 2/2/2021 | 27 | 689 | 748 | 9 | 14 |
| NJ | 368 | 4593 | 4 | 1/4/2021 | 3/6/2021 | 61 | 5442 | 8580 | 10 | 13 |
| NM | 60 | 727 | 4 | 1/5/2021 | 1/22/2021 | 17 | 1097 | 1500 | 10 | 10 |
| NV | 37 | 719 | 9 | 12/30/2020 | 2/12/2021 | 44 | 535 | 463 | 9 | 7 |
| NY | 386 | 7123 | 8 | 1/11/2021 | 2/26/2021 | 46 | 7364 | 7545 | 10 | 10 |
| OH | 302 | 3208 | 3 | 12/26/2020 | 2/20/2021 | 56 | 2333 | 1387 | 10 | 3 |
| OK | 7 | 502 | 43 | 1/16/2021 | 2/5/2021 | 20 | 461 | 122 | 6 | 2 |
| OR | 493 | 3886 | 5 | 12/26/2020 | 2/19/2021 | 55 | 3850 | 3944 | 9 | 8 |
| PA | 646 | 7321 | 3 | 1/1/2021 | 2/24/2021 | 54 | 7524 | 10,429 | 10 | 15 |
| RI | 61 | 5161 | 25 | 1/18/2021 | 2/14/2021 | 27 | 3214 | 1089 | 8 | 3 |
| SC | 119 | 1283 | 4 | 12/29/2020 | 2/19/2021 | 52 | 1330 | 722 | 10 | 8 |
| SD | 3 | 56 | 12 | 1/8/2021 | 1/19/2021 | 11 | 44 | 42 | 6 | 7 |
| TN | 40 | 1605 | 6 | 1/7/2021 | 2/2/2021 | 26 | 1494 | 459 | 9 | 3 |
| TX | 169 | 1587 | 4 | 12/28/2020 | 3/18/2021 | 80 | 2477 | 1447 | 10 | 3 |
| UT | 72 | 1786 | 5 | 12/28/2020 | 2/10/2021 | 44 | 2071 | 2599 | 13 | 17 |
| VA | 337 | 3256 | 4 | 1/10/2021 | 3/12/2021 | 61 | 3423 | 3838 | 10 | 9 |
| VT | 71 | 1473 | 12 | 12/23/2020 | 2/12/2021 | 51 | 991 | 1130 | 8 | 6 |
| WA | 1045 | 10,313 | 6 | 1/1/2021 | 3/9/2021 | 67 | 8752 | 10,762 | 8 | 7 |
| WI | 564 | 6791 | 4 | 1/14/2021 | 3/16/2021 | 61 | 6469 | 3399 | 8 | 4 |
| WY | 1 | 99 | — | 1/22/2021 | — | — | 84 | 110 | 9 | 11 |
References
- 1.Dooling K., McClung N., Chamberland M. The Advisory Committee on Immunization Practices' interim recommendation for allocating initial supplies of COVID-19 vaccine - United States, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1857–1859. doi: 10.15585/mmwr.mm6949e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Centers for Medicare & Medicaid Services COVID-19 nursing home data. 2020. https://data.cms.gov/stories/s/COVID-19-Nursing-Home-Data/bkwz-xpvg Available at: [PubMed]
- 3.CDC COVID-19 Response Team Severe outcomes among patients with coronavirus disease 2019 (COVID-19) - United States, February 12-March 16, 2020. MMWR Morb Mortal Wkly Rep. 2020;69:343–346. doi: 10.15585/mmwr.mm6912e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Harris-Kojetin L., Sengupta M., Lendon J. Long-term care providers and services users in the United States: Data from the National Study of Long-Term Care Providers, 2015-2016. Vital Health Stat. 2019;3 i–vii;1–78. [PubMed] [Google Scholar]
- 5.Yi S.H., See I., Kent A.G. Characterization of COVID-19 in assisted living facilities - 39 states, October 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1730–1735. doi: 10.15585/mmwr.mm6946a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention Understanding the Pharmacy Partnership for Long-Term Care Program. 2020. https://www.cdc.gov/vaccines/covid-19/long-term-care/pharmacy-partnerships.html Available at:
- 7.Gharpure R., Guo A., Bishnoi C.K. Early COVID-19 first-dose vaccination coverage among residents and staff members of skilled nursing facilities participating in the Pharmacy Partnership for Long-Term Care Program - United States, December 2020-January 2021. MMWR Morb Mortal Wkly Rep. 2021;70:178–182. doi: 10.15585/mmwr.mm7005e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lee J.T., Althomsons S.P., Wu H. Disparities in COVID-19 vaccination coverage among health care personnel working in long-term care facilities, by job category, National Healthcare Safety Network - United States, March 2021. MMWR Morb Mortal Wkly Rep. 2021;70:1036–1039. doi: 10.15585/mmwr.mm7030a2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hughes M.M., Wang A., Grossman M.K. County-level COVID-19 vaccination coverage and social vulnerability - United States, December 14, 2020-March 1, 2021. MMWR Morb Mortal Wkly Rep. 2021;70:431–436. doi: 10.15585/mmwr.mm7012e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barry V., Dasgupta S., Weller D.L. Patterns in COVID-19 vaccination coverage, by social vulnerability and urbanicity - United States, December 14, 2020-May 1, 2021. MMWR Morb Mortal Wkly Rep. 2021;70:818–824. doi: 10.15585/mmwr.mm7022e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Whiteman A., Wang A., McCain K. Demographic and social factors associated with COVID-19 vaccination initiation among adults aged ≥65 years - United States, December 14, 2020-April 10, 2021. MMWR Morb Mortal Wkly Rep. 2021;70:725–730. doi: 10.15585/mmwr.mm7019e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Connecticut COVID-19 Response Nursing homes and assisted living facilities data. 2021. https://portal.ct.gov/-/media/Coronavirus/Nursing-Homes-and-Assisted-Living-Facilities-Data/20210128-Assisted-Living-Facilities-with-COVID-19.pdf Available at:
- 13.Georgia Department of Community Health Long-term care facility COVID-19 report. 2021. https://dch.georgia.gov/ Available at:
- 14.Tennessee Department of Health Long term care facility data. 2021. https://www.tn.gov/health/cedep/ncov/data/clusters-in-long-term-care-facilities.html Available at:
- 15.Centers for Disease Control and Prevention/Agency for Toxic Substances and Disease Registry/Geospatial Research, Analysis, and Services Program. CDC/ATSDR Social Vulnerability Index, 2018 Database, US. https://www.atsdr.cdc.gov/placeandhealth/svi/data_documentation_download.html Available at:
- 16.US Department of Housing and Urban Development HUD USPS ZIP code crosswalk files. 2021. https://www.huduser.gov/portal/datasets/usps_crosswalk.html Available at:
- 17.Britton A., Jacobs Slifka K.M., Edens C. Effectiveness of the Pfizer-BioNTech COVID-19 vaccine among residents of two skilled nursing facilities experiencing COVID-19 outbreaks - Connecticut, December 2020-February 2021. MMWR Morb Mortal Wkly Rep. 2021;70:396–401. doi: 10.15585/mmwr.mm7011e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Geller A.I., Budnitz D.S., Dubendris H. Surveillance of COVID-19 vaccination in US nursing homes, December 2020-April 2021. medRxiv. 2021 doi: 10.1177/00333549211066168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Centers for Medicare & Medicaid Services Medicare and Medicaid Programs; COVID-19 vaccine requirements for long-term care (LTC) facilities and intermediate care facilities for individuals with intellectual disabilities (ICFs-IID) residents, clients, and staff. US Department of Health and Human Services. 2021:26306–26336. [Google Scholar]
- 20.National Institute of Environmental Health Sciences Key elements of a model workplace safety and health COVID-19 vaccination program. 2021. https://tools.niehs.nih.gov/wetp/public/hasl_get_blob.cfm?ID=12621 Available at:
- 21.Centers for Disease Control and Prevention Workplace Vaccination Program. 2021. https://www.cdc.gov/coronavirus/2019-ncov/vaccines/recommendations/essentialworker/workplace-vaccination-program.html Available at:
- 22.Centers for Disease Control and Prevention Mobile vaccination resources. 2021. https://www.cdc.gov/vaccines/covid-19/planning/mobile.html Available at:
- 23.Carder P.C., O'Keefe J., O'Keefe C. RTI Press; Research Triangle Park, NC: 2016. State Regulatory Provisions for Residential Care Settings: An Overview of Staffing Requirements. [Google Scholar]
- 24.Rome V., Harris-Kojetin L.D. Variation in residential care community nurse and aide staffing levels: United States, 2014. Natl Health Stat Report. 2016;91:1–11. [PubMed] [Google Scholar]