Abstract
Background:
Few studies have investigated how adverse childhood experiences are associated with substance use patterns during young adulthood, a crucial developmental period.
Objective:
The objective of this study was to extend current knowledge on the association between adverse childhood experiences and patterns of substance use among young adults. We also sought to understand how current mental health status and biological sex influences these patterns.
Participants and setting:
The current study utilized wave 8 – wave 11 data of a longitudinal cohort study (N = 2,880).
Methods:
We used latent transition analysis (LTA) to understand stability and transition patterns of substance use across participants who reported adverse childhood experiences (ACEs+) versus those who did not (ACEs−). Latent class regression was used to assess contemporaneous effects of mental health and sex on classes over time.
Results:
Both groups had similar patterns of substance use emerge at each timepoint: High All; Binge, Tobacco, Cannabis; and Steady/increasing binge drinking. ACEs+ had a higher proportion of youth in the High All class and much higher stability in this class, compared to the ACEs− group. Those in the ACES+ group were less likely to transition out of a riskier class. Mental health and sex showed differential effects across ACEs groups.
Conclusion:
Results point to increased risk of polysubstance use, including opioids and prescription medications, among those who reported adverse childhood events. Future work may explore protective, malleable, factors that may confer reduced risk of long-term polysubstance use.
Keywords: Childhood Trauma, PTSD, Longitudinal, Adolescent, Victimization
Introduction
In the United States an alarming number of youths experience some form of adverse childhood experience (e.g., physical abuse, sexual abuse, emotional abuse, or neglect). Recent, nationally representative, data indicate that 61% of youth (prior to the age of 18) reported experiencing at least one form of direct violence in the past year (which includes any violence exposure such as adverse childhood experiences, assault, violent crime, witnessing violence etc.), with nearly 41% reporting more than one event (Finkelhor et al., 2015). Specifically, among adolescents ages 14–17, nearly 13% report some form of sexual abuse, 18% report some form of physical abuse (i.e., experiences from an older adult or friend), 24% report emotional abuse, 18.5% report neglect, with 38% reporting any maltreatment (i.e., physical abuse, emotional abuse, and neglect by a caregiver; Finkelhor, Ormrod, & Turner, 2007; Finkelhor et al., 2015). Many youth experience long-term negative consequences of early childhood adversity, including greater alcohol use, marijuana use, and illicit drug use compared to those who have not experienced these events (Davis et al., 2019; Davis, Ingram, Merrin, & Espelage, 2018; Davis, Dumas, Janssen, & Dworkin, 2019.; Ford, Grasso, Hawke, & Chapman, 2013; Turner, Finkelhor, & Ormrod, 2010). Few studies, however, have investigated how experiences of these early adversities may influence long-term substance use patterns during young adulthood (ages 18–25). This is important for two reasons. First, prior epidemiological work indicates that young adults have the highest prevalence rate of binge drinking (36.9%), marijuana (34.8%), tobacco (25.9%), and illicit drug use, such as opioids and pain relievers (10%), compared to adolescents and older adults (SAMHSA, 2019). Second, the majority of studies assessing effects of adverse childhood experiences on young adult substance use are cross-sectional in nature, limiting our knowledge on longitudinal patterns of substance use during a developmental period when substance use escalates.
Broadly, seminal work on toxic stress theory (Shonkoff & Garner, 2012; McEwen & McEwen, 2017) and the cumulative risk model (Felitti et al., 1998) proposes that experiences of stress –defined as events such as early childhood adversity– can be a catalyst for changes in behavior and physiology. According to toxic stress theory and developmental traumatology theory (De Bellis, 2001), from a physiological perspective, the most disruptive form of stress response is a result of frequent and prolonged activation of the body’s stress response system (e.g., Hypothalamic pituitary adrenocortical axis; HPA). The prolonged activation of the HPA axis results in increased levels of the stress hormones, such as cortisol, and can result in the blunting of the stress response, which has been shown to influence long-term physiological and behavioral problems (Arborelius, Owens, Plotsky, & Nemeroff, 1999; Connell, Pittenger, & Lang, 2018). Others have noted that the cumulative risk model can be used to understand how experiences of trauma can influence long-term outcomes, such as substance use. Cumulative risk perspectives posit that various risks, ranging from traumatic events and victimization to adverse interpersonal relationship histories, often co-occur and can accumulate, leading to a variety of undesirable or negative outcomes (Adam et al., 2011; Putnam, Harris, & Putnam, 2013). Support for these theoretical arguments, in regards to adverse events, has been relatively robust. For example, in an early cross-sectional study of adolescents, Moran, Vuchinich, & Hall (2004) noted that all maltreatment types (e.g., emotional, sexual, and physical abuse by a caregiver) were related to greater odds of alcohol, tobacco, and illicit drug use. Further examination indicated that physical and sexual abuse had a greater magnitude of effect compared to emotional abuse. Other large cross-sectional studies have also noted relatively strong (range of odds ratios 1.3 – 4.7) associations between child maltreatment and all substance use disorders (e.g., alcohol, marijuana, heroin, amphetamines, cocaine, and sedatives; Afifi, A Henriksen, Asmundson, & Sareen, 2012). The few longitudinal studies that have been conducted also show evidence of an association with adverse childhood experiences and substance use over time. For example, Yoon et al. (2020) reported that experiences of child maltreatment (defined as adverse experiences from a caregiver) were associated with increased alcohol and marijuana use throughout early and late adolescence. Others have noted that youth who experience adverse events and endorse post traumatic stress symptoms are more likely to transition to higher risk drinking groups over the course of four years than youth who had not experienced a traumatic event (De Bellis et al., 2020). Though less frequent, several recent studies have also noted associations between experiences of child maltreatment and substance use problems in young adulthood. For example, in one longitudinal study, exposure to child maltreatment (via government agency reports) was associated with greater odds of lifetime cannabis use, daily cannabis use, and cannabis dependence diagnosis during young adulthood (Mills, Kisely, Alati, Strathearn, & Najman, 2017).
When attempting to understand patterns of substance use over time, most studies involve adolescent samples where certain theories such as the gateway hypothesis and the common liability model are pitted against each other (Van Leeuwen et al., 2011; Zych, Rodríguez-Ruiz, Marín-López, & Llorent, 2020). Utilizing the gateway hypothesis to understand patterns of substance use among young adults makes little sense given most young adults have already initiated use. However, the common liability model suggests that the use of alcohol and other drugs can be attributed to the influence of a common liability, which can include genetic vulnerability, family liability (i.e., prior familial substance use problems), as well as individual vulnerability such as adverse childhood experiences (Agrawal, Neale, Prescott, & Kendler, 2004; McLaughlin et al., 2010; Vanyukov et al., 2012). Given that most young adults’ substance use is relatively established (Tucker, Ellickson, Orlando, Martino, & Klein, 2005), the common liability model is useful as no order in the sequence of substance use is expected. The common liability model also supports prior research noting that young adults who report heavy substance use tend toward polysubstance use, and also have higher rates of comorbidity (i.e., experiencing depression or other mental health disorder). Thus, this framework allows us the flexibility to understand patterns of substance use among young adults in the context of experiences of early childhood adversity.
Recent person-center methods have been used to characterize patterns of substance use over time, and provide support for the common liability model. However, the majority of this work is with adolescent populations. For example, Choi et al. (2018) identified three classes of substance use over each of the three years of data from ages 16 – 18. These included mild alcohol use, alcohol and moderate cannabis use, and polysubstance use (e.g., use of alcohol, cannabis, and other drugs). Using a person-centered method known as Latent Transition Analysis (LTA) results suggested that adolescents, in general, remained stable in their classes over time. However, when they did transition from time point to time point, it was typically to a more severe substance use class. In one of the only studies to investigate patterns of substance use in relation to child maltreatment, Shin, (2012) also identified a three-class model across two time points (moderate alcohol and cannabis use, high alcohol/cannabis use & moderate illicit drug use, heavy polysubstance use). Overall, over 90% of the sample were considered “movers” (i.e., they transitioned from their initial class at time 1 to a different class at time 2), with the most common transition moving from a less severe class to a more severe class. Interestingly, when assessing patterns by maltreatment status, results indicated the majority of adolescents who reported some form of child maltreatment (69%) were in the heavy polysubstance use class at time 1 (compared to 14% of adolescents in the non-maltreatment group), and the stability within the polysubstance class was 0.92 (compared to 0.72), indicating fewer adolescents who reported maltreatment moved out of the heavy polysubstance use class.
Few studies have attempted to characterize variations and patterns of substance use among a young adult sample who report adverse childhood experiences. This is unfortunate as young adulthood is a developmental period associated with the highest prevalence of substance use, mental health problems, and developmental change (Roberts & Davis, 2016; SAMHSA, 2019; Sussman & Arnett, 2014). Furthermore, few studies have explored how important demographic and common risk factors, such as self-reported sex and mental health problems (i.e., depression and anxiety) as well as more global risk factors such as experiences of adverse childhood events, may influence stability and change in substance use patterns over time. We extend the seminal work in this area with adolescent samples (Shin, 2012) by investigating transition and stability patterns of substance use among young adults over four years, and assess how experiences of early childhood adversity is associated with these patterns. In line with the common liability model and prior work with adolescent populations, we hypothesized that a larger proportion of youth reporting adverse childhood experiences would be classified into higher severity substance use classes compared to individuals who do not report adverse childhood experiences. Further, in line with prior work and the cumulative risk model, we hypothesized that youth reporting adverse experiences would have higher stability patterns in more severe substance use classes over time compared to those who have not had these experiences. We did not have any a priori hypotheses about transition patterns given the relative stability of substance use during young adulthood, and allowed this component to be a more exploratory aspect of the study. Finally, in terms of demographic and common risk factors (i.e., sex, depression, anxiety), we also allowed this to be an exploratory aim given that few studies that have investigated how these factors may influence patterns of substance use in the context of adverse childhood experiences for young adults.
Methods
Procedures
Participants are from two cohorts of students in 6th and 7th grade in 2008 who were initially recruited from 16 middle schools in Southern California as part of a substance use prevention program that occurred in 2008–2009 (D’Amico et al., 2012). All participants received parental consent, and then assented to the study. Procedures were approved by the RAND IRB. Cohorts were followed annually across 11 waves through 2019. Participants completed waves 1 through 5 during physical education. Adolescents transitioned to over 200 high schools following wave 5, and were re-contacted and re-consented to complete annual web-based surveys. Participants were paid $50 for completing each web-based survey. Participants who did not complete a particular wave of data collection remained eligible to complete subsequent waves. They did not “dropout” of the study once they missed a wave; rather, we fielded the full sample every wave so all participants could participate in each individual survey. The current study focuses on data during young adulthood, using waves 8–11 (N = 2,880).
Participants
Table 1 provides information on demographic characteristics as well as participants substance use and experiences of adverse events. We also note variation across our ACEs grouping. On average, at wave 8, participants were 18.3 years old (SD = 0.78), wave 9 was 19.4 (SD = 0.76), wave 10 was 20.7 (SD = 0.70), and at wave 11 participants were 21.5 years old (SD = 0.78) with slightly over half of the sample identifying as female (1,582; 53.7%). Just under half (46%) of the sample reported past year alcohol use, with 30.6% reporting cannabis use, 25.2% tobacco/nicotine use, 6% prescription drug misuse, and 3.7% opioid misuse. Finally, 25% of participants (n = 745) reported experiencing at least one adverse childhood event.
Table 1.
Wave 8 information from project CHOICE on demographic characteristics as well as participants substance use and experiences of adverse event
| Variable | Full sample | ACEs+ | ACEs− | t-value or chi-square |
|---|---|---|---|---|
| M(SD) or n (%) | M(SD) or n (%) | M(SD) or n (%) | ||
| N = 2,526 | N = 745 | N = 1,781 | ||
| Age | 18.33 (0.781) | 18.3 (0.74) | 18.3 (0.77) | −0.60 (2190), p = 0.55 |
| Female | 1,582 (53.7%) | 456 (61.2%) | 936 (52.6%) | 17.7 (1), p < .001 |
| Race/Ethnicity n (%) | ||||
| White | 603 (20.5%) | 142 (19.1%) | 375 (21.1%) | 1.23 (1), p = 0.25 |
| Black | 66 (2.2%) | 19 (2.6%) | 33 (1.9%) | 1.26 (1), p = 0.26 |
| Hispanic | 1,348 (45.8%) | 364 (48.9%) | 800 (44.9%) | 3.42 (1), p = 0.07 |
| Asian | 587 (19.9%) | 145 (19.5%) | 367 (20.6%) | 0.43 (1), p = 0.51 |
| Other | 340 (11.5%) | |||
| Mothers Education n (%) | ||||
| High school or less | 858 (29.2%) | 247 (33.2%) | 486 (27.3%) | 8.77 (1), p < .001 |
| Substance Use, Past Year n (%) | ||||
| Alcohol | 1,355 (46%) | 418 (63.0%) | 756 (49.7%) | 32.7 (1), p < .001 |
| Binge drinking | 957 (32.5%) | 285 (42.9%) | 534 (35.1%) | 12.0 (1), p < .001 |
| Marijuana | 900 (30.6%) | 273 (41.1%) | 487 (32.0%) | 16.7 (1), p < .001 |
| Tobacco/Nicotine | 743 (25.2%) | 221 (33.2%) | 400 (26.2%) | 11.2 (1), p < .001 |
| Non-opioid Prescription Drug Misuse | 177 (6.0%) | 71 (10.7%) | 79 (5.2%) | 21.9 (1), p < .001 |
| Opioid Misuse | 109 (3.7%) | 35 (5.3%) | 46 (3.0%) | 6.52 (1),p < .001 |
| Any Adverse Childhood Experiences n (%) | 745 (25.3%) | − | − | − |
| Average ACEs score | 0.51 (0.91) | 1.71 (0.90) | − | − |
| Mental Health, Past Two Weeks | ||||
| Depression | 4.76 (5.13) | 6.87 (6.01) | 3.94 (4.48) | 12.6 (2182), p <.001 |
| Anxiety | 4.10 (5.04) | 6.19 (6.01) | 3.26 (4.32) | 12.9 (2182), p <.001 |
Note: t-values and chi-square tests assess differences at wave 8 between ACES+ and ACES− participants.
Measures
Background covariates.
Participants reported age, sex (female vs. male), race/ethnicity [non-Hispanic white (reference), non-Hispanic black, Hispanic, Asian, and Other/Multiracial], mother’s education (indicator of family socioeconomic status; 1= “did not finish high school” to 4= “graduated from college”). We also controlled for intervention status, which occurred in 2008, and effects were no longer significant after wave 3.
Substance Use.
Participants were asked separate questions about how many times in the past year they had used five different substances: alcohol, tobacco/nicotine, cannabis, prescription medications (i.e., Adderall, sedatives) to get high, and opioids, including an item on heroin use, and an item about prescription narcotic medications to get high such as Vicodin, codeine, OxyContin, and Percocet. For alcohol use, we focused on binge/heavy drinking as participants were over 21; thus, participants reported the number of times they had drank 5 or more drinks in a row in a couple of hours. Each participant rated the number of times in the past year on a scale from 1=none to 6=more than 20 times for each substance. At wave 11, most participants who reported heroin use also reported prescription opioid misuse (96% at wave 8 and 83% at wave 11), and both items were highly skewed at the upper end of the response scale. Other items such as prescription medications were also highly skewed. Thus, we derived dichotomous indicators of any past year use for alcohol use, marijuana use, tobacco/nicotine use, prescription medication misuse, and heroin/prescription opioid misuse.
Adverse Childhood Experiences.
Using items derived from the Adverse Childhood Experiences Scale (ACES; Felitti et al., 1998), each participant answered six questions regarding their experiences prior to their 18th birthday (during wave 11 when participants were, on average, 21.5 years old). Items covered emotional abuse (i.e., Did a parent or other adult say hurtful or insulting things to you like calling you names, or wished you had never been born, or you felt that someone in your family hated you?), physical abuse (i.e., Did a parent or other adult in the household often or very often push, grab, slap, or throw something at you, or ever hit you so hard that you had marks or were injured?), sexual abuse (i.e., Did an adult or person at least 5 years older than you ever touch or fondle you or have you touch their body in a sexual way, or attempt or actually have oral, anal, or vaginal intercourse with you?), and witnessing parental violence (i.e., Were any of your parents or step-parents often or very often pushed, grabbed, slapped, or had something thrown at them, or kicked, bitten, hit with a fist, or hit with something hard). Each participant answered “yes” or “no” to each item. For the current study, given we were interested in any adverse experiences during childhood, we created a single dichotomous variable that indicated whether each participant experienced any adverse events (ACEs+) or no adverse advents (ACEs−).
Mental Health.
Two mental health measures assessed symptoms in the past two weeks across all waves. Each participant responded on a scale from 0 = not at all to 3 = nearly every day. The Patient Health Questionnaire (Kroenke et al., 2009; PHQ-8; α = 0.91) – 8 item assessed eight symptoms of depression such as feeling down, depressed, or hopeless and having little interest or pleasure in doing things. The Generalized Anxiety Disorder questionnaire (Spitzer, Kroenke, Williams, & Löwe, 2006; GAD-7; α = 0.94) assessed seven symptoms of anxiety such as feeling nervous, anxious, or on edge and not being able to stop or control worrying. Scores were summed for both depression and anxiety to create a total score.
Analytic Plan
To understand both stability and change in substance use patterns over time, we used latent transition mixture modeling (Nylund-Gibson, Grimm, Quirk, & Furlong, 2014). Latent Transition Analysis involves latent class variables across multiple waves. To model changes in latent classes from wave to wave, we regressed, for example, the latent class variable at Time 2 on the previous latent class variable at Time 1. Thus, given our four waves of data, we estimated three latent class regressions to understand stability and transition patterns over time. This procedure quantifies change as a matrix of transition probabilities between two consecutive time points, and is used to assess the probability of transitioning between different emergent latent class. This framework allows us to assess the extent to which membership in a particular substance use class at Time 1 is associated with the probability of transitioning, for example, to a lower or higher-risk pattern of substance use at Time 2. It also allows for examination of how factors such as demographic characteristics or mental health symptoms influence these transition probabilities, as described in more detail below. In this study, we use Latent Class Analysis to model heterogeneity in substance use from wave 8 (average age = 18) to wave 11 (average age = 21.5). Mplus (Muthen & Muthen, 1998–2017) was used for all analyses.
Latent Class Analysis: Class Enumeration
The number of substance use classes were estimated at each time point, separately for those with (ACEs+) and without (ACEs−) any adverse childhood experiences. A series of models were estimated with one to five classes. As with all mixture models, model fit was assessed with several indicators, such that better model fit was indicated by: lower values of the sample size adjusted Bayesian Information Criteria, and non-significant values for the Vuong-Lo-Mendell-Rubin Likelihood Ratio test, Lo-Mendell-Rubin adjusted likelihood ratio test, and bootstrapped likelihood ratio test (Nylund, Asparouhov, & Muthén, 2007).
Latent Transition Analysis: Methods and Moderation Analyses
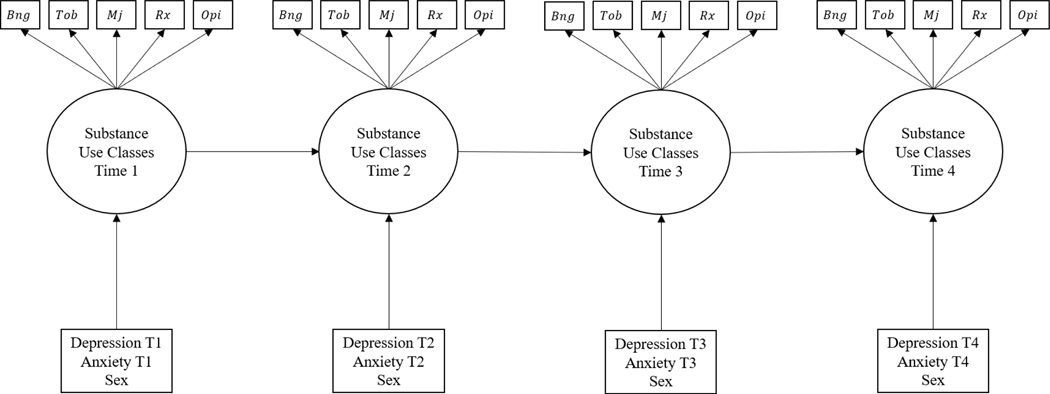
To assess latent transition probabilities (i.e., stability and transition patterns), the latent class variable from earlier waves (i.e., Time 1) assessing heterogeneity in substance use were regressed on the emergent latent class variable at the next time point (i.e., Time 2; see figure 1 for theoretical model). Specifically, emergent classes at Time 1 were regressed onto emergent classes at Time 2, emergent classes at Time 2 were regressed onto emergent classes at Time 3, and emergent classes at Time 3 were regressed onto emergent classes at Time 4. This process was done for participants with (ACEs+) and without (ACEs−) any adverse childhood experiences. In order to understand how mental health (e.g., depression and anxiety) and self-reported sex influenced class membership over time across these two groups, we estimated a series of latent class regressions (a form of multinomial logistic regression) where contemporaneous time varying (mental health) and time invariant (sex) covariates were introduced as predictors of class membership.
Figure 1.
Conceptual model addressing latent class transition model for substance use with time varying and time invariant covariates.
Missing data
Retention rates were high from waves 8–9 (89%), waves 9–10 (90%), and waves 10–11 (92%). Substance use at wave 10 did not significantly predict retention at wave 11, similar to previous waves (D’amico et al., 2020; D’Amico, Rodriguez, Tucker, Pedersen, & Shih, 2018); however, compared to those who did not complete wave 11, retained participants were slightly more likely to be female (94% vs. 91%) and tended to be slightly younger at wave 10 (mean=20.6 years vs. 20.9 years). Missing data are handled using maximum likelihood in Mplus. Here, individuals contribute data at any time point where data are available, without being removed for missing data. Due to missing data on some variables, our final analytic sample size was 2,526.
Results
Substance use class enumeration across adverse childhood experience groups
A series of Latent Class Analysis models were fit to the substance use data across the groups that did (ACEs+) and did not (ACEs−) any adverse childhood experiences. For both the ACEs+ and ACEs− groups, models were estimated from one to five classes at each time point. Model fit statistics for each time point can be found in the supplementary materials. In short, a three-class model fit the data best at each time point and across both the ACEs+ and ACEs− groups. The non-significant fit statistics values (Vuong-Lo-Mendell-Rubin Likelihood Ratio test, Lo-Mendell-Rubin adjusted likelihood ratio test, and bootstrapped likelihood ratio test) for the four-class solution indicated that a three-class solution fit the data best. Further, the adjusted Bayesian information criteria values increased when estimating a four-class solution, indicating that the three-class solution fit the data best.
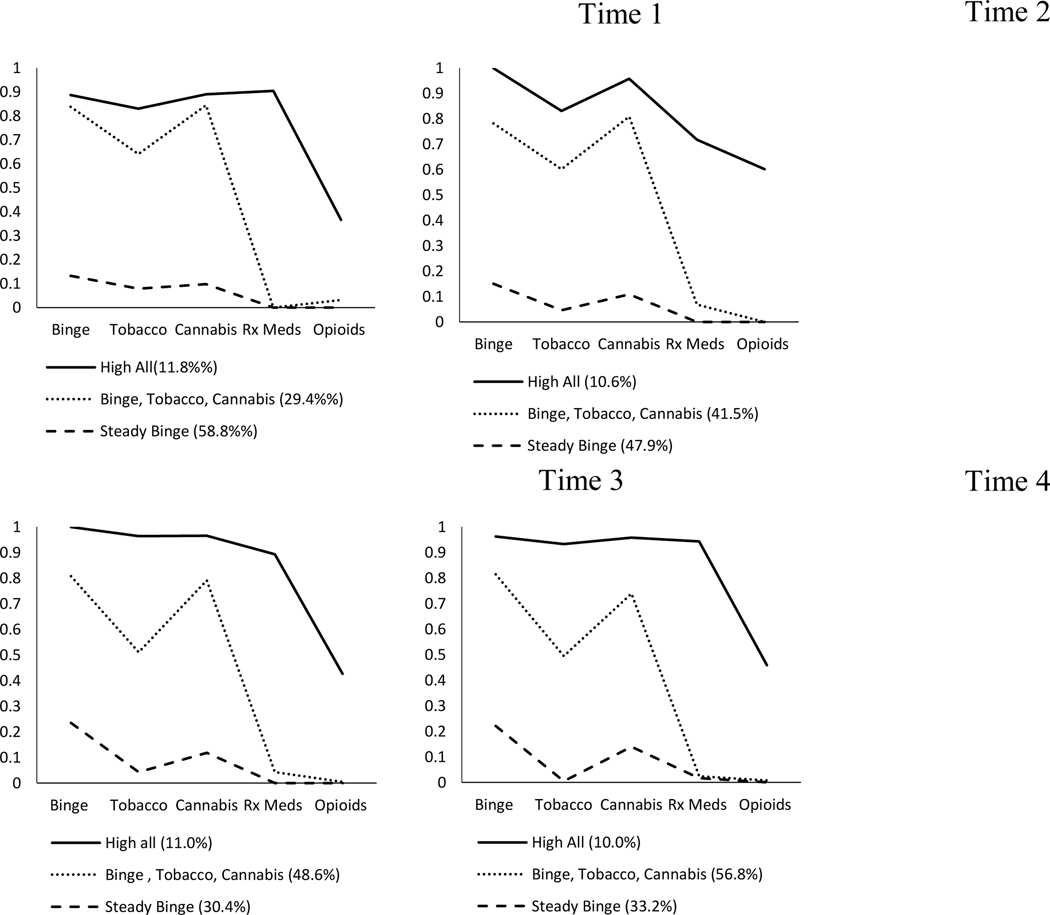
Figure 2 presents item probability plots at each time point for ACES+. Across all four time points, a High All class (10.0% – 12.0%) emerged representing participants endorsing all substances, including relatively high endorsement of opioid use and prescription drug use. A second class emerged labeled Binge, Tobacco, Cannabis (39.4%- 56.8%) representing participants endorsing high rates of binge drinking, tobacco, and cannabis, but low probability of prescription medications and opioids. Finally, the third class to emerged was a Steady Binge Drinking class (30.4% - 47.9%) representing participants endorsing moderate levels of binge drinking, but no other substances.
Figure 2.
Emergent latent classes over time for the ACEs+ group.
Note: Rx meds = non-opioid prescription medication misuse; opioids = heroin and/or prescription opioid medication misuse
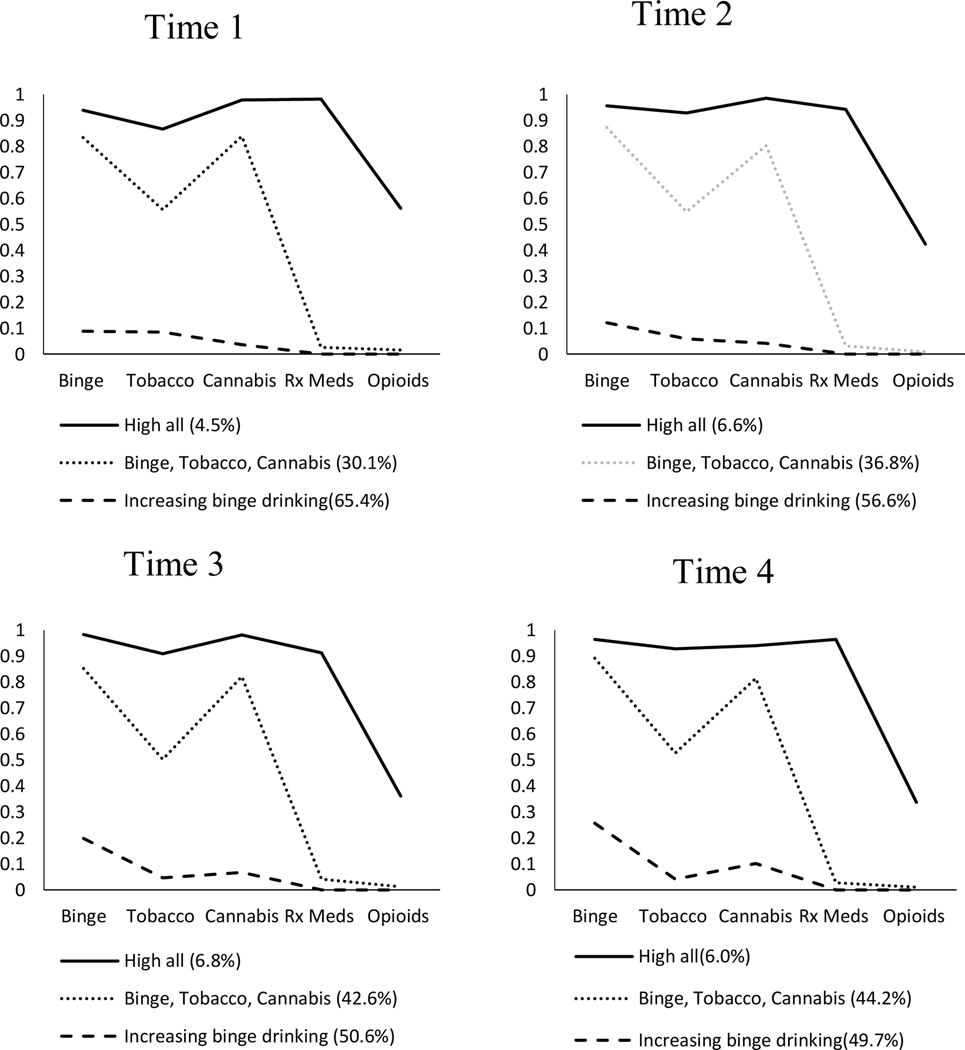
Figure 3 presents item probability plots for the ACEs− group. Similar patterns emerged across all four time points, including a High All class (4.5% - 6.8%). This class represented individuals who endorsed high rates of all substances at each time point. Similarly, a class represented by primarily Binge, Tobacco, and Cannabis use (30.1% - 44.2%) emerged across all time points. Interestingly, in contrast to the Steady Binge Drinking class that emerged for the ACEs+ group, the last class to emerge for the ACEs− group was an Increasing Binge Drinking class (49.7% - 65.4%) that started out endorsing very low probability of all substances (including binge drinking), but increased binge drinking over time
Figure 3.
Emergent latent classes over time for the ACEs− group.
Note: Rx meds = non-opioid prescription medication misuse; opioids = heroin and/or prescription opioid medication misuse
Adverse childhood experiences and transition patterns
Following initial class enumeration process, the next step included cross-group analysis of stability and transitions between classes over the four time points. Results of the latent transition models can be found in Table 2a (ACEs+) and 2b (ACEs−). Several interesting patterns emerged between groups. The ACEs+ group started with a larger proportion of participants in the High All class (11.8% vs. 4.5%) compared to the ACES− group, and maintained a larger proportion of participants at each time point. Further, the stability of participants in the High All class among those in the ACEs+ group was higher over time (Time 1: 0.67; Time 2: 0.80; Time 3: 0.72) compared to the High All stability of participants in the ACEs− group (Time 1: 0.64; Time 2: 0.62; Time 3: 0.61). We found the opposite pattern for the Steady Binge Drinking (ACEs+) and the Increasing Binge Drinking (ACEs−) classes. Here, the stability remained higher for those in the ACEs− group (Time 1: 0.84; Time 2: 0.84; Time 3: 0.92) compared to those in the ACEs+ group (Time 1: 0.78; Time 2: 0.82; Time 3: 0.82). This indicates that, compared to participants who did not report adverse childhood experiences, more participants in the ACEs+ group moved into a more severe substance use classification over time (i.e., High All; Binge, Tobacco, Cannabis), with fewer participants staying in the lowest risk class (i.e., Steady Binge Drinking).
Table 2a.
Conditional latent transition probability estimates for ACEs+ group
| Time 2 | |||
|---|---|---|---|
|
| |||
| Time 1 | High All (10.6%) | Binge, Tobacco, Cannabis (41.5%) | Steady Binge (47.9%) |
|
| |||
| High All (11.8%) | 0.672 | 0.277 | 0.051 |
| Binge, Tobacco, Cannabis (29.4%) | 0.057 | 0.942 | 0.001 |
| Steady Binge (58.8%) | 0.009 | 0.214 | 0.777 |
|
| |||
| Time 3 | |||
|
| |||
| Time 2 | High All (11.0%) | Binge, Tobacco, Cannabis (48.6%) | Steady Binge (30.4%) |
|
| |||
| High All (10.6%) | 0.799 | 0.201 | 0 |
| Binge, Tobacco, Cannabis (41.5%) | 0.079 | 0.084 | 0.057 |
| Steady Binge (47.9%) | 0.006 | 0.017 | 0.82 |
|
| |||
| Time 4 | |||
|
| |||
| Time 3 | High All (10.0%) | Binge, Tobacco, Cannabis (56.8%) | Steady Binge (33.21%) |
|
| |||
| High All (11.0%) | 0.722 | 0.226 | 0.052 |
| Binge, Tobacco, Cannabis (48.6%) | 0.079 | 0.864 | 0.057 |
| Steady Binge (30.4%) | 0.006 | 0.174 | 0.82 |
Note: Diagonal (bold) estimates represent stability patterns over time. Off-diagonal estimates represent Transition patterns over time.
Table 2b.
Conditional latent transition probability estimates for ACEs− group
| Time 2 | |||
|---|---|---|---|
| Time 1 | High All (6.6%) | Binge, Tobacco, Cannabis (36.8%) | Increasing Binge (56.6%) |
|
| |||
| High All (4.5%) | 0.64 | 0.29 | 0.068 |
| Binge, Tobacco, Cannabis (30.1%) | 0.11 | 0.845 | 0.042 |
| Increasing Binge (65.4%) | 0.008 | 0.148 | 0.844 |
|
| |||
| Time 3 | |||
| Time 2 | High All (6.8%) | Binge, Tobacco, Cannabis (42.6%) | Increasing Binge (50.6%) |
|
| |||
| High All (6.6%) | 0.625 | 0.31 | 0.066 |
| Binge, Tobacco, Cannabis (36.8%) | 0.069 | 0.836 | 0.095 |
| Increasing Binge (56.6%) | 0.002 | 0.154 | 0.844 |
|
| |||
| Time 4 | |||
| Time 3 | High All (6.0%) | Binge, Tobacco, Cannabis (44.2%) | Increasing Binge (49.7%) |
|
| |||
| High All (6.8%) | 0.607 | 0.355 | 0.038 |
| Binge, Tobacco, Cannabis (42.6%) | 0.038 | 0.923 | 0.039 |
| Increasing Binge (50.6%) | 0.008 | 0.007 | 0.915 |
Note: Diagonal (bold) estimates represent stability patterns over time. Off-diagonal estimates represent Transition patterns over time.
Mental health and sex as predictors of class membership overtime
In a final step, we introduced contemporaneous time varying (i.e., depression and anxiety) and time invariant (i.e., self-reported sex) covariates into our model to predict class membership. When fitting these models, we used model-fit criteria (i.e., reductions in negative two log likelihood ratio tests) to determine whether constraining effects of our predictors to be equal over time, within class, was a more parsimonious model than allowing effects to vary. Across all classes and predictors, model testing revealed that constrained effects did not result in significantly worse model fit. Table 3 presents results across both groups. Self-reported sex did not significantly predict greater odds of class membership over time for participants in the ACEs+ group. However, females were less likely to be in the High All class at each time point for the ACEs− group. In terms of our mental health covariates, individuals reporting more depressive and anxiety symptoms had greater odds of being in the High All and the Binge, Tobacco, Cannabis classes for youth in the ACEs− group. However, greater depression and anxiety symptoms only resulted in greater risk of membership in the High All class, over time, for participants in the ACEs+ group.
Table 3.
Effect of sex, depression, and anxiety on class membership over time
| ACEs+ Group OR [95%CI] | |||
|---|---|---|---|
| Effect | High All | Binge, Tobacco, Cannabis | Steady Binge |
|
| |||
| Female (vs. male) | 0.77 [0.50, 1.31] | 0.86 [0.66, 1.12] | REF |
| Depression | 1.05 [1.01, 1.09] | 1.01 [0.98, 1.03] | REF |
| Anxiety | 1.05 [1.01, 1.08] | 1.01 [0.98, 1.03] | REF |
|
| |||
| ACEs− group OR [95%CI] | |||
| Effect | High All | Binge, Tobacco, Cannabis | Increasing Binge |
|
| |||
| Female (vs. male) | 0.52 [0.37, 0.73] | 0.89 [0.75, 1.06] | REF |
| Depression | 1.08 [1.05, 1.11] | 1.04 [1.01, 1.06] | REF |
| Anxiety | 1.08 [1.04, 1.11] | 1.03 [1.00, 1.05] | REF |
Note: OR = odds ratio. Effects were constrained to be equal over time – within each class. Reductions
In negative 2 log likelihood were used to determine if constrained (versus freely estimated)
Effects did not result in significantly worse model fit. Results indicated that all effects could be constrained over time, within class, without introducing worse model fit. Sex (female = 1, male = 0).
Discussion
Adverse childhood experiences, such as physical abuse, emotional abuse, and sexual abuse can contribute to long-term psychological and behavioral health problems. In particular, prior cross-sectional work has indicated that adolescents who experience some form of early childhood adversity report earlier age of onset for alcohol and drug use, increased binge drinking, regular alcohol use, as well as increased prevalence of substance use disorders (Hamburger, Leeb, & Swahn, 2008; Hussey, Chang, & Kotch, 2006; Shin, Edwards, & Heeren, 2009). Most studies assessing the effects of adverse childhood experiences on behavioral health trends have been with adolescents, and examine cross-sectional associations. Given that substance use and mental health problems peak during emerging young adulthood (ages 18–25) (Sussman & Arnett, 2014), it is important to understand how adverse childhood experiences may contribute to substance use during this crucial developmental time period (Ballard et al., 2015). However, few studies have attempted to understand how adverse childhood experiences influence patterns and change in substance use throughout young adulthood or how mental health and demographic variables influence these patterns.
The first goal of this study was to examine whether different classes of substance use might emerge for young people who experienced early childhood adversity compared to those who did not. From a basic descriptive perspective, the emergent classes looked quite similar for these two groups. In both cases, there was a class characterized by use of all substances; a class that primarily reported binge drinking, tobacco, and cannabis use; and a class that primarily only reported low to moderate binge drinking. However, while the structure of the classes was nearly identical across the two groups, there were some nuanced differences. For example, the classes identified as binge drinking only were characterized by steady, moderate use over time for those who experienced adverse childhood experiences, but those who did not experience childhood trauma showed a slow increase in their binge drinking. While prior work notes binge drinking tends to increase during young adulthood (SAMHSA, 2019), young adults in the ACEs+ group reported greater binge drinking early on, indicating earlier development of problematic alcohol use behaviors and, potentially, long term problems. Another notable difference involves the High All class, which had consistently higher rates of opioid use for those who experienced childhood adversity compared to those who did not. This is important to note, with over 40,000 opioid-related deaths reported in 2017 and an annual domestic economic burden of nearly $80 billion in costs including treatment, loss of productivity, and criminal justice involvement (Florence, Zhou, Luo, & Xu, 2016), future research may wish to focus on long-term effects of ACEs on aspects of opioid misuse as it may shed light on important prevention mechanisms. Overall, these results point to subtle, yet important within-class differences that suggest a greater risk for problematic substance use among young people who have experienced childhood trauma.
The second goal of this study was to examine differences in the proportion of youth assigned to each class, by whether or not they experienced childhood adversity. Consistent with our hypothesis, a larger proportion of ACEs+ youth were classified into higher severity substance use classes compared to ACEs− youth. For example, across any given time point young people who had reported experiencing early childhood adversity were more likely to be in the High All class, compared to individuals who had not experienced childhood adversity. Conversely, young adults who did not report experiencing childhood adversity were more likely to be in the increasing binge drinking class. In fact, this difference (between ACEs+ and ACEs− across the class characterized by binge drinking) reached a 14% differential at the last time point. These results are consistent with prior research indicating, for example, that young adults who have experienced high levels of sexual assault or violence exposure (i.e., witnessing violence, close friend dies, close to someone who was assaulted), and young adults who have experienced some type of childhood trauma (e.g., sexual, physical, or emotional abuse), tend to be at higher risk for alcohol and drug use disorders compared to those not experiencing childhood trauma (Ballard et al., 2015).
This study extends prior work on childhood adversity and substance use by examining how stability and transitions in substance use over time during emerging young adulthood might differ depending on a young person’s history of childhood adversity. While prior work notes that adolescence is a time of autonomy and change, more recently, theorists and empirical data indicate that young adulthood may, in fact, be more suited for this distinction (Arnett & Tanner, 2006; Davis, Dumas, & Roberts, 2018; Davis, Dumas, Briley, & Sussman, 2018; Roberts & Davis, 2016). For example, prior theory notes that young adulthood is a time when individuals delay traditional adult roles (e.g., marriage, buying a home), engage in identity exploration (e.g., move away from home), and engage in experimentation (e.g., relationships, greater drug experimentation; Davis et al., 2018; Sussman & Arnett, 2014). Consistent with our hypothesis, young adults reporting adverse childhood experiences exhibited higher stability patterns in more severe substance use classes over time compared to those who did not have these adverse experiences. They were more likely to remain in the High All class, and less likely to stay in the class characterized by binge drinking only. This is consistent with developmental traumatology theory (De Bellis, 2001) which suggests that traumatic experiences early in life result in dysregulated stress response systems, which can lead to more severe disorders such as Post traumatic stress disorder, failures of self-regulation, and greater incidence of impulsive behaviors (e.g., problematic substance use). In fact, this was shown in a recent study, such that youth who had experienced a traumatic event and reported post traumatic stress symptoms, were more likely to transition to higher risk drinking groups over a four-year period (De Bellis et al., 2020). Our results extend the theory of developmental traumatology, suggesting that young adults in the ACEs+ group who reported polysubstance use (i.e., endorsing use of all or multiple substances) were less likely to transition out of a higher risk pattern of substance use over time, compared to those in the ACEs− group. Our results echo prior work assessing effects of childhood adversity on substance use stability and transition patterns among adolescents. For example, Shin (2012) reported stability of 0.92 among adolescents reporting poly-substance use who had a history of early childhood adversity with nearly none of these youth transitioning into a lower risk class. Others have reported similar stability patterns for polysubstance use among adolescent populations, also noting sex and age differences (Choi, Lu, Schulte, & Temple, 2018; Evans, Kim, & Hagquist, 2020).
The final goal of this study was to examine whether, and how, mental health symptoms and biological sex might influence class membership over time for young adults with and without experiences of childhood adversity. In the ACEs+ group, greater mental health symptoms were associated with greater odds of being in the High All class, whereas sex was not associated with class membership. In the ACEs− group, greater mental health symptoms were associated with a greater odds of being in the High All and the Binge, Tobacco, and Cannabis classes, and women were less likely to be in the High All class. One of the more important results of this study is that there were no differences in class membership across men and women for the ACEs+ group. While some work contradicts this, our results indicate that high risk substance use, in the context of adverse childhood experiences, may not vary by someone’s sex. In the case of mental health, the toxic stress and cumulative risk model of childhood adversity provides a useful framework for interpreting and understanding our results. Early work has noted that experiences of toxic stress are related to changes in learning, behavior, and physiology that can have effects throughout adulthood (Shonkoff & Garner, 2012). In these models, different developmental outcomes (e.g., delinquency, physiological distress) are regarded as “maladaptive” (vs. “adaptive”), meaning that individuals who experience high levels of adverse childhood experiences are at greater risk of developing abnormally and exhibit behavioral problems that may be detrimental to themselves and others (Ellis et al.,2012). These models operate under the assumption that once individuals surpass an optimal level of responsivity to social stressors (e.g., adverse childhood experiences), their system is overloaded. This overload can emerge as dysregulated stress response systems, which has been associated with long term psychological (Burke, Davis, Otte, & Mohr, 2005; Schulenberg, Sameroff, & Cicchetti, 2004) and behavioral health problems (e.g., substance use; Adinoff, Junghanns, Kiefer, & Krishnan-Sarin, 2005). This model is further supported by our results as they indicate that mental health symptoms are associated with greater odds of being in the poly-substance use class among those in the ACEs+ group over time. Thus, from a theoretical perspective, it seems that both adverse childhood experiences and mental health difficulties may contribute to the strong stability patterns found among the ACEs+ group. Based on prior research discussed above, it appears that similar patterns have emerged among adolescent populations, which may lend some insight into long-term effects of adverse childhood experiences on patterns of substance use from adolescence to young adulthood.
Clinical Implications
The current study, while not focused on a clinical sample, can lend support to improved clinical care coordination. Individuals with histories of adverse childhood experiences, sexual violence, or witnessing interpersonal violence from early childhood onward make up the majority of clients served in the public mental health and substance use treatment systems. While many providers likely include comprehensive interviews that include in-depth assessment of past traumatic experiences, it is likely that, unless individuals meet a certain threshold (e.g., endorsing enough symptoms for a PTSD diagnosis), trauma will not be included as a main priority. Our results, while preliminary, note that individuals who endorse at least one adverse childhood experience are susceptible to long-term substance use problems, and have a much lower probability of moving out of high-risk use classifications. Though there are barriers that may prevent trauma informed care for those meeting subclinical thresholds (i.e., insurance requirements, state Medicare policies), it may be time to re-think how we treat and screen individuals entering the substance use or mental health service sector given mounting evidence that any form of trauma invites a myriad of negative problems. Our results also point to added difficulties when multi-morbid disorders (e.g., depression, anxiety) are considered. Thus, in addition to rethinking our treatment protocols for trauma informed care, our results point to a need for an inclusive system for young adults entering care. Clearly, treatment should be comprehensive and open the door for young adults to receive evidence-based treatments for all challenges they are experiencing.
Limitations and Conclusions
This study is not without limitations. First, the current study used self-report of adverse childhood experiences and substance use. Thus, this study may be subject to recall bias as well as common variance issues. Second, our study did not assess effects across different types of early childhood adversity. Although the data exist to assess this, there are two issues that do not allow us to analyze the data this way: sample size and convergence. Attempting to split our sample into three groups (emotional abuse, physical abuse, sexual abuse) presents issues around sample size. Mixture models typically require relatively large sample sizes, thus slicing the data into three small samples presents convergence issues when attempting to extract classes of substance use. Future research, with suitable sample sizes, may wish to explore stability and transition patterns across specific childhood trauma types. Further, our study may not generalize to all young adults given our sample had few individuals who identified as African American, and our sample has a larger proportion who are currently attending higher education. In addition, we only had information on receipt of treatment at wave 11, which would limit our ability to determine if transition patterns are due, in part, to treatment receipt. Future research may wish to assess how substance use transition patterns function across health care service receipt. Finally, our study does not infer causality. While our study does utilize longitudinal data, all results are simply associations with self-reported early childhood adversity. Despite limitations, this is the first study to explore how adverse childhood experiences is associated with stability and transition patterns of substance use during young adulthood. Most work in this area is with adolescent populations, ignoring young adults who report the highest substance use and mental health problems. Our results point to increased risk of polysubstance use, including opioids and prescription medications, among young adults who report experiencing adverse childhood events. Future work could explore protective, malleable, factors that may confer reduced risk of long-term polysubstance use in order to be implemented in prevention and intervention efforts.
Supplementary Material
Highlights.
ACEs is associated with greater stability in high risk substance use classes
Experiences of ACEs is associated with less likelihood of transitioning out of high-risk substance use classes
Class makeup is differentially associated with sex and mental health over time
Acknowledgements:
Data collection efforts and work on this paper were supported by three grants from the National Institute on Alcohol Abuse and Alcoholism (R01AA016577, R01AA020883, and R01AA025848), as well as supplemental funds provided by the National Institutes of Health HEAL Initiative, awarded to Elizabeth D’Amico.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adam EK, Chyu L, Hoyt LT, Doane LD, Boisjoly J, Duncan GJ, … McDade TW (2011). Adverse adolescent relationship histories and young adult health: Cumulative effects of loneliness, low parental support, relationship instability, intimate partner violence, and loss. Journal of Adolescent Health, 49(3), 278–286. 10.1016/j.jadohealth.2010.12.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Adinoff B, Junghanns K, Kiefer F, & Krishnan‐Sarin S. (2005). Suppression of the HPA Axis Stress‐Response: Implications for Relapse. Alcoholism: Clinical and Experimental Research, 29(7), 1351–1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Afifi TO, A Henriksen C, Asmundson GJG, & Sareen J. (2012). Childhood maltreatment and substance use disorders among men and women in a nationally representative sample. Canadian Journal of Psychiatry, 57(11), 677–686. 10.1177/070674371205701105 [DOI] [PubMed] [Google Scholar]
- Agrawal A, Neale MC, Prescott CA, & Kendler KS (2004). Cannabis and Other Illicit Drugs: Comorbid Use and Abuse/Dependence in Males and Females. Behavior Genetics, 34(3), 217–228. 10.1023/B:BEGE.0000017868.07829.45 [DOI] [PubMed] [Google Scholar]
- Arborelius L, Owens MJ, Plotsky PM, & Nemeroff CB (1999). The role of corticotropin-releasing factor in depression and anxiety disorders. The Journal of Endocrinology, 160(1), 1–12. [DOI] [PubMed] [Google Scholar]
- Arnett JJ, & Tanner JL (2006). Emerging adulthood: Understanding the new way of coming of age. Emerging adults in America: Coming of age in the 21st century. Washington, DC: American Psychological Association. [Google Scholar]
- Ballard ED, Van Eck K, Musci RJ, Hart SR, Storr CL, Breslau N, & Wilcox HC (2015). Latent classes of childhood trauma exposure predict the development of behavioral health outcomes in adolescence and young adulthood. Psychological Medicine, 45(15), 3305–3316. 10.1017/S0033291715001300 [DOI] [PubMed] [Google Scholar]
- Burke H, Davis M, Otte C, & Mohr D. (2005). Depression and cortisol responses to psychological stress: a meta-analysis. Psychoneuroendocrinology, 30(9), 846–856. [DOI] [PubMed] [Google Scholar]
- Choi HJ, Lu Y, Schulte M, & Temple JR (2018). Adolescent substance use: Latent class and transition analysis. Addictive Behaviors, 77, 160–165. 10.1016/j.addbeh.2017.09.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Connell CM, Pittenger SL, & Lang JM (2018). Patterns of Trauma Exposure in Childhood and Adolescence and Their Associations With Behavioral Well-Being. Journal of Traumatic Stress. 10.1002/jts.22315 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’amico EJ, Rodriguez A, Tucker JS, Dunbar MS, Pedersen ER, Shih RA, … Seelam R. (2020). Early and Late Adolescent Factors that Predict Co-use of Cannabis with Alcohol and Tobacco in Young Adulthood. Prevention Science. 10.1007/s11121-020-01086-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Rodriguez A, Tucker JS, Pedersen ER, & Shih RA (2018). Planting the seed for marijuana use: Changes in exposure to medical marijuana advertising and subsequent adolescent marijuana use, cognitions, and consequences over seven years. Drug and Alcohol Dependence, 188, 385–391. 10.1016/J.DRUGALCDEP.2018.03.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- D’Amico EJ, Tucker JS, Miles JNV, Zhou AJ, Shih RA, & Green HD (2012). Preventing Alcohol Use with a Voluntary After-School Program for Middle School Students: Results from a Cluster Randomized Controlled Trial of CHOICE. Prevention Science, 13(4), 415–425. 10.1007/s11121-011-0269-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis JP, Dworkin ER, Helton J, Prindle J, Patel S, Dumas TMTM, & Miller S. (2019). Extending Poly-Victimization Theory: Differential Effects of Adolescents’ Experiences of Victimization on Substance Use Disorder Diagnoses Upon Treatment Entry. Child Abuse & Neglect, 89, 165–177. 10.1016/J.CHIABU.2019.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis JP, Dumas TMTM, & Roberts BWBW (2018). Adverse Childhood Experiences and Development in Emerging Adulthood. Emerging Adulthood, 6(4). 10.1177/2167696817725608 [DOI] [Google Scholar]
- Davis JP, Dumas TM, Briley DA, & Sussman S. (2018). A meta-analysis of the association between substance use and emerging adult development using the IDEA scale. American Journal on Addictions, 27(3). 10.1111/ajad.12707 [DOI] [PubMed] [Google Scholar]
- Davis JP, Ingram KM, Merrin GJ, & Espelage DL (2018). Exposure to parental and community violence and the relationship to bullying perpetration and victimization among early adolescents: A parallel process growth mixture latent transition analysis. Scandinavian Journal of Psychology. 10.1111/sjop.12493 [DOI] [PubMed] [Google Scholar]
- Davis JP, Janssen T, Dworkin ER, Dumas TM, Goldbach J, & Monterosso J. (2020). Influences of victimization and comorbid conditions on substance use disorder outcomes in justice-involved youth: A discrete time survival mixture analysis. Development and psychopathology, 32(3), 1045–1058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Bellis MD (2002). Developmental traumatology: a contributory mechanism for alcohol and substance use disorders. Psychoneuroendocrinology, 27(1–2), 155–170. [DOI] [PubMed] [Google Scholar]
- De Bellis MD, Nooner KB, Brumback T, Clark DB, Tapert SF, & Brown SA (2020). Posttraumatic Stress Symptoms Predict Transition to Future Adolescent and Young Adult Moderate to Heavy Drinking in the NCANDA Sample. Current Addiction Reports, 7(2), 99–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans BE, Kim Y, & Hagquist C. (2020). A latent class analysis of changes in adolescent substance use between 1988 and 2011 in Sweden: associations with sex and psychosomatic problems. Addiction, 115(10), 1932–1941. 10.1111/add.15040 [DOI] [PubMed] [Google Scholar]
- Felitti VJ, Anda RF, Nordenberg D, Williamson DF, Spitz AM, Edwards V, … Marks JS (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The Adverse Childhood Experiences (ACE) Study. American Journal of Preventive Medicine, 14(4), 245–258. [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Ormrod RK, & Turner HA (2007). Poly-victimization: A neglected component in child victimization. Child Abuse & Neglect, 31(1), 7–26. 10.1016/j.chiabu.2006.06.008 [DOI] [PubMed] [Google Scholar]
- Finkelhor D, Turner HA, Shattuck A, Hamby SL, R G, JM L, … R C. (2015). Prevalence of Childhood Exposure to Violence, Crime, and Abuse. JAMA Pediatrics, 169(8), 746. 10.1001/jamapediatrics.2015.0676 [DOI] [PubMed] [Google Scholar]
- Florence CS, Zhou C, Luo F, & Xu L. (2016). The economic burden of prescription opioid overdose, abuse, and dependence in the United States, 2013. Medical Care, 54(10), 901–906. 10.1097/MLR.0000000000000625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford JD, Grasso DJ, Hawke J, & Chapman JF (2013). Poly-victimization among juvenile justice-involved youths. Child Abuse & Neglect, 37(10), 788–800. 10.1016/j.chiabu.2013.01.005 [DOI] [PubMed] [Google Scholar]
- Hamburger ME, Leeb RT, & Swahn MH (2008). Childhood maltreatment and early alcohol use among high-risk adolescents. Journal of Studies on Alcohol and Drugs, 69(2), 291–295. 10.15288/jsad.2008.69.291 [DOI] [PubMed] [Google Scholar]
- Hussey JM, Chang JJ, & Kotch JB (2006). Child maltreatment in the United States: Prevalence, risk factors, and adolescent health consequences. Pediatrics, 118(3), 933–942. 10.1542/peds.2005-2452 [DOI] [PubMed] [Google Scholar]
- Shin S Hyucksun. (2012). A Longitudinal Examination of the Relationships between Childhood Maltreatment and Patterns of Adolescent Substance Use among High-Risk Adolescents. The American Journal on Addictions, 21(5), 453–461. 10.1111/j.1521-0391.2012.00255.x [DOI] [PubMed] [Google Scholar]
- Kroenke K, Strine TW, Spitzer RL, Williams JBW, Berry JT, & Mokdad AH (2009). The PHQ-8 as a measure of current depression in the general population. Journal of Affective Disorders, 114(1–3), 163–173. 10.1016/J.JAD.2008.06.026 [DOI] [PubMed] [Google Scholar]
- McEwen CA, & McEwen BS (2017). Social structure, adversity, toxic stress, and intergenerational poverty: An early childhood model. Annual Review of Sociology, 43, 445–472. [Google Scholar]
- McLaughlin KA, Conron KJ, Koenen KC, Gilman SE, Arata CM, Langhinrichsen-Rohling J, … Wyatt GE (2010). Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: a test of the stress sensitization hypothesis in a population-based sample of adults. Psychological Medicine, 40(10), 1647–1658. 10.1017/S0033291709992121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mills R, Kisely S, Alati R, Strathearn L, & Najman JM (2017). Child maltreatment and cannabis use in young adulthood: a birth cohort study. Addiction, 112(3), 494–501. 10.1111/add.13634 [DOI] [PubMed] [Google Scholar]
- Muthén LK and Muthén BO (1998–2017). Mplus User’s Guide. Eighth Edition. Los Angeles, CA: Muthén & Muthén [Google Scholar]
- Moran PB, Vuchinich S, & Hall NK (2004). Associations between types of maltreatment and substance use during adolescence. Child Abuse and Neglect, 28(5), 565–574. 10.1016/j.chiabu.2003.12.002 [DOI] [PubMed] [Google Scholar]
- Nylund-Gibson K, Grimm R, Quirk M, & Furlong M. (2014). A Latent Transition Mixture Model Using the Three-Step Specification. Structural Equation Modeling: A Multidisciplinary Journal, 21(3), 439–454. 10.1080/10705511.2014.915375 [DOI] [Google Scholar]
- Nylund KL, Asparouhov T, & Muthén BO (2007). Deciding on the Number of Classes in Latent Class Analysis and Growth Mixture Modeling: A Monte Carlo Simulation Study. Structural Equation Modeling: A Multidisciplinary Journal, 14(4), 535–569. 10.1080/10705510701575396 [DOI] [Google Scholar]
- Putnam KT, Harris WW, & Putnam FW (2013). Synergistic childhood adversities and complex adult psychopathology. Journal of Traumatic Stress, 26(4), 435–442. 10.1002/jts.21833 [DOI] [PubMed] [Google Scholar]
- Roberts BWWB, & Davis JJPP (2016). Young Adulthood Is the Crucible of Personality Development. Emerging Adulthood, 4(5), 318–326. 10.1177/2167696816653052 [DOI] [Google Scholar]
- SAMHSA. (2019). Key substance use and mental health indicators in the United States: Results from the 2016 National Survey on Drug Use and Health (HHS Publication No. PEP19–5068, NSDUH Series H-54). Rockville, MD, MD. [Google Scholar]
- Schulenberg JE, Sameroff AJ, & Cicchetti D. (2004). The transition to adulthood as a critical juncture in the course of psychopathology and mental health. Development and Psychopathology, 16(04), 799–806. 10.1017/S0954579404040015 [DOI] [PubMed] [Google Scholar]
- Shin SH, Edwards EM, & Heeren T. (2009). Child abuse and neglect: Relations to adolescent binge drinking in the national longitudinal study of Adolescent Health (AddHealth) Study. Addictive Behaviors, 34(3), 277–280. 10.1016/j.addbeh.2008.10.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shonkoff JP, & Garner AS (2012). The lifelong effects of early childhood adversity and toxic stress. Pediatrics, 129(1), e232–46. 10.1542/peds.2011-2663 [doi] [DOI] [PubMed] [Google Scholar]
- Shonkoff JP, Boyce WT, & McEwen BS (2009). Neuroscience, molecular biology, and the childhood roots of health disparities: building a new framework for health promotion and disease prevention. Jama, 301(21), 2252–2259. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JBW, & Löwe B. (2006). A Brief Measure for Assessing Generalized Anxiety Disorder. Archives of Internal Medicine, 166(10), 1092. 10.1001/archinte.166.10.1092 [DOI] [PubMed] [Google Scholar]
- Sussman S, & Arnett JJ (2014). Emerging Adulthood: Developmental Period Facilitative of the Addictions. Evaluation & the Health Professions, 37(2), 147–155. https://doi.org/0163278714521812 [pii] [DOI] [PubMed] [Google Scholar]
- Tucker JS, Ellickson PL, Orlando M, Martino SC, & Klein DJ (2005). Substance use Trajectories from Early Adolescence to Emerging Adulthood: A Comparison of Smoking, Binge Drinking, and Marijuana use. Journal of Drug Issues, 35(2), 307–332. 10.1177/002204260503500205 [DOI] [Google Scholar]
- Turner HA, Finkelhor D, & Ormrod R. (2010). Poly-Victimization in a National Sample of Children and Youth. American Journal of Preventive Medicine, 38(3), 323–330. 10.1016/j.amepre.2009.11.012 [DOI] [PubMed] [Google Scholar]
- Van Leeuwen AP, Verhulst FC, Reijneveld SA, Vollebergh WAM, Ormel J, & Huizink AC (2011). Can the gateway hypothesis, the common liability model and/or, the route of administration model predict initiation of cannabis use during adolescence? A survival analysisthe TRAILS study. Journal of Adolescent Health, 48(1), 73–78. 10.1016/j.jadohealth.2010.05.008 [DOI] [PubMed] [Google Scholar]
- Vanyukov MM, Tarter RE, Kirillova GP, Kirisci L, Reynolds MD, Kreek MJ, … Ridenour TA (2012, June 1). Common liability to addiction and “gateway hypothesis”: Theoretical, empirical and evolutionary perspective. Drug and Alcohol Dependence. Elsevier 10.1016/j.drugalcdep.2011.12.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon S, Shi Y, Yoon D, Pei F, Schoppe-Sullivan S, & Snyder SM (2020). Child Maltreatment, Fathers, and Adolescent Alcohol and Marijuana Use Trajectories. Substance Use & Misuse, 55(5), 721–733. 10.1080/10826084.2019.1701033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zych I, Rodríguez-Ruiz J, Marín-López I, & Llorent VJ (2020). Longitudinal stability and change in adolescent substance use: A latent transition analysis. Children and Youth Services Review, 112, 104933. 10.1016/j.childyouth.2020.104933 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.