Abstract
Introduction
To evaluate insulin injection knowledge, attitudes, and practices of nurses across China in order to provide reference for the formulation of a national unified standard of insulin injection practice and the targeted implementation of standardized training on insulin injection for nurses.
Methods
We enrolled nurses who worked and injected insulin at grassroot hospitals including community health service centers and township clinics, secondary and tertiary care hospitals across China between July 28, 2019 and August 30, 2019. A nurse insulin injection knowledge, attitude, and practice questionnaire was used to evaluate the knowledge, attitude, and practice level of nurses.
Results
A total of 223,368 nurses were included in the study. The mean knowledge score was 13.70 ± 3.30 and 35.19% had a poor knowledge score. The mean attitude score was 17.18 ± 2.69 for the study nurses; merely 3.15% had a poor attitude score. The mean practice score of the study population was 83.03 ± 8.16 and only 0.88% had a poor practice score. Pearson correlation analysis showed significant correlation between the knowledge score and the attitude score (r = 0.29; P < 0.001), the knowledge score and the practice score (r = 0.27; P < 0.001), and between the attitude score and the practice score (r = 0.56; P < 0.001). A multivariate analysis revealed that nurses with higher knowledge scores were also more likely to have higher attitude scores and practice scores, and nurses with higher attitude scores were also more likely to have higher practice scores.
Conclusion
Chinese nurses have a good attitude and behavior towards insulin injection, while their knowledge of insulin injection is insufficient. It is also revealed that knowledge of insulin injection can directly or indirectly affect insulin injection behavior through attitude, indicating that hospitals should formulate unified insulin injection norms and regularly organize relevant training and assessment so as to improve nurses’ knowledge, attitude, and behavior of insulin injection.
Supplementary Information
The online version contains supplementary material available at 10.1007/s13300-021-01122-x.
Keywords: Knowledge, Attitudes, Practices, Insulin injection
Key Summary Points
| Numerous studies have demonstrated that a sizeable proportion of nurses still lack proper insulin injection knowledge, have not skillfully mastered insulin injection techniques, and should be compliant with insulin injection guidelines. |
| This is the first cross-sectional study of insulin injection knowledge, attitude, and practice among nurses at different healthcare settings across China. |
| The study highlights the need for workplace-based learning and training to further enhance insulin injection-related knowledge, attitude, and practice. |
Introduction
The global prevalence of diabetes has rapidly increased over the past decade [1] and close to 600 million people are predicted to develop diabetes by 2035 globally [2]. Diabetes also poses a major public health burden in China; according to the International Diabetes Federation (IDF) report, China has the highest number of patients with diabetes in the world [3] 2019. Patients with type 1 diabetes (T1DM) are absolutely deficient in insulin and must rely on exogenous insulin supplementation. Insulin treatment is also required for patients with type 2 diabetes (T2DM) with progressive β-cell insufficiency or who are contraindicated for oral antidiabetic medications.
Insulin intensification therapy is often used in hospitalized patients in and outside endocrinology departments. Proper insulin injection knowledge and practices are critical to blood glucose control in both patients with T1DM and patients with T2DM. Many of the issues in insulin injection practices by nurses can be attributed to their inadequate knowledge of proper insulin injection techniques, suggesting the importance of educating the nurses on proper insulin injection techniques and improving their compliance with insulin injection guidelines [4, 5]. Numerous studies have demonstrated that a sizeable proportion of nurses still lack proper insulin injection knowledge, have not skillfully mastered insulin injection techniques, and have not been compliant with insulin injection guidelines [6–10]. However, no cross-sectional study across China has been conducted and no study has been conducted in a primary care setting in China.
In the current cross-sectional, non-interventional nationwide study, we sought to evaluate insulin injection knowledge, attitudes, and practices of nurses and nurse administrators who had performed insulin injection within the preceding year at primary, secondary, and tertiary care hospitals across China using the stratified sampling method.
Methods
Study Population
This cross-sectional, non-interventional multicenter study conducted at multiple centers across China (Appendix I in the supplementary material) enrolled nurses who worked and injected insulin at grassroot hospitals including community health service centers and township clinics, secondary and tertiary care hospitals between July 28, 2019 and August 30, 2019. Nurses who provided at least one insulin injection within the preceding year were eligible. Nurses in training, interns, and nursing students were excluded. Nurses were randomly chosen from 231 grassroot hospitals, 453 secondary care hospitals, and 564 tertiary care hospitals listed on the Chinese government’s official website [11]. Data on gender, age, years worked, professional title, and administrative title were retrieved.
The study protocol ethical approval was granted by the ethics committee of China–Japan Friendship Hospital (No. 2019-68-K47), the leading institution for the study, and local ethics committees and institutional review boards of the participating institutions (Appendix I in the supplementary material). All study subjects provided written informed consent prior to enrollment. The study was conducted in accordance with the Declaration of Helsinki.
Questionnaire
The nurse insulin injection knowledge, attitude, and practice questionnaire asked the participants about their knowledge about insulin, injection technique, and hypoglycemia prevention and treatment, their attitudes regarding importance, standardization, and confidence of insulin injection technique, and their practices in the use of insulin injection devices and injection procedure. The questionnaire was designed on the basis of the Guidelines for Drug Administration Techniques in Diabetes Patients in China 2016 Guidelines on Chinese Diabetes Medication Skills [10] with two rounds of consultation with 17 experts on the China Diabetes Expert Committee and Chinese Nursing Association Nursing Management Committee. The questionnaire was pretested and validated in nurses of three hospitals in China. Construct validity was tested to estimate the validity of our instrument. Cronbach’s α was 0.686 for the nurse insulin injection knowledge domain, 0.785 for the insulin injection attitude domain, and 0.886 for the insulin injection practice domain, indicating excellent internal consistency. In the nurse insulin injection knowledge domain, items 1, 2, 6, 16, and 19–21 were related to mastery of basic knowledge, items 3–5 were related to mastery of insulin storage knowledge, and items 7–15, 17, and 18 related to mastery of insulin injection techniques. Each item had a score of 1 for correct answer and the total score was 21. A total score less than 13 was considered poor, a score ≥ 13 but < 17 was considered satisfactory and a score ≥ 17 was considered good. In the insulin injection attitude domain, items 1–4 were assigned a score 1–5 for the choices given in the order given and items 5 and 6 were not assigned a score. The total score was 20. A total score less than 12 was considered poor, a score ≥ 12 but < 16 was considered satisfactory, and a score ≥ 16 was considered good. In the insulin injection practice domain, items 1–14 and 16–18 were assigned a score 1–5 for the choices given in the order given and item 15 was assigned a score 5–1 for the choices given in the order given. The total score was 90. A total score less than 54 was considered poor, a score ≥ 54 but < 72 was considered satisfactory, and a score ≥ 72 was considered good. The questionnaire was administered between January 1, 2019 and February 28, 2019 via the website portal http://ww.wjx.cn and answered anonymously by participants using laptop computer, mobile phone, and smart devices.
Statistical Analysis
Statistical analysis was carried out using SAS9.3 (The SAS Institute, Cary, NC, USA). Quantitative data were presented as mean ± standard deviation or median (interquartile range, IQR) and compared by Student’s t test or Wilcoxon rank sum test, when appropriate. All categorical data were presented as percentage and compared by chi-square analysis. The correlation among knowledge, altitude, and practices was analyzed using Spearman correlation. In addition, score levels and correlation coefficients were analyzed using the Cochran–Mantel–Haenszel (CMH3) method. Poor knowledge, altitude, and practices were entered into multivariate linear logistic regression analysis as dependent variables and nurse characteristics as independent variables. A P value less than 0.05 in a two-sided test or the OR 95% CI did not cross 1 was considered to indicate a statistically significantly different.
Results
Demographic and Baseline Characteristics of Study Population
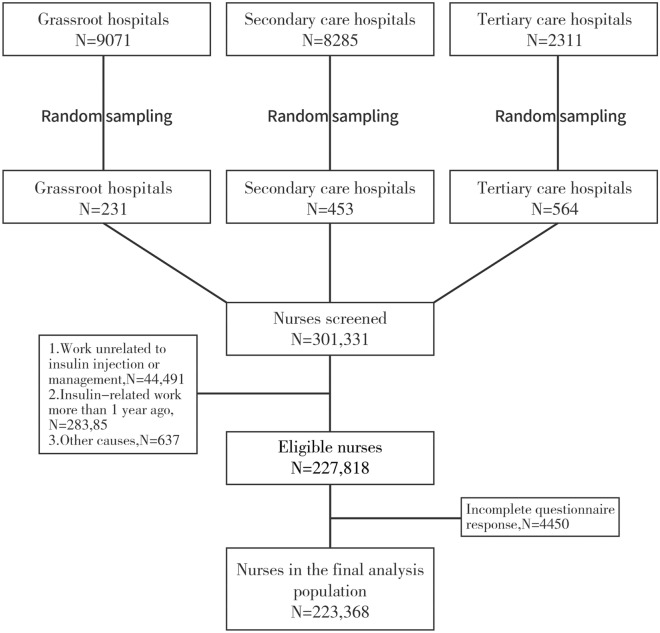
The study flowchart is shown in Fig. 1. We surveyed a total of 301,331 nurses from 1248 hospitals across China during the study period. We excluded 44,491 nurses whose work was unrelated to insulin injection, 28,385 nurses who had not performed insulin injection-related duties within the preceding year, and 637 nurses because of other causes. A total of 227,818 nurses were eligible for the study. After exclusion of 4450 nurses because of incomplete questionnaire response, 223,368 nurses were included in the current cross-sectional study. The demographic and baseline variables of the study nurses are shown in Table 1. They included 60,472 nurses (27.07%), 106,107 (47.50%), and 49,130 (22.0%) nurses-in-charge with a mean age of 30.7 ± 6.4 years and median (Q1, Q3) duration of work experience of 7 years (4, 11). In addition, 25,289 (11.32%) nurses were certified diabetes nurses and 13,912 (6.23%) nurses worked at an endocrinology department. Most nurses (87.89%) came from tertiary care hospitals, 11.40% from secondary care hospitals, and 0.71% from primary care clinics. A total of 155,032 (69.14%) nurses received a bachelor’s degree and 62,432 (27.95%) nurses graduated from junior colleges.
Fig. 1.
Study flowchart
Table 1.
Demographic and baseline characteristics of the study nurses
| Variables | N = 223,368 |
|---|---|
| Female sex, n (%) | 217,199 (97.24) |
| Age, years | |
| Mean (SD) | 30.74 (6.41) |
| Range | 18, 70 |
| < 25 | 31,818 (14.24) |
| 25–30 | 78,481 (35.14) |
| 30–35 | 62,092 (27.80) |
| ≥ 35 | 50,977 (22.82) |
| Education, n (%) | |
| Technical secondary school | 3779 (1.69) |
| Junior college | 62,432 (27.95) |
| Bachelor | 155,032 (69.41) |
| Master or above | 2125 (0.95) |
| Work experience, years | 8.88 |
| Median (Q1, Q3) | 7 (4, 11) |
| < 4 | 52,186 (23.36) |
| 4–7 | 48,352 (21.65) |
| 7–11 | 58,934 (26.38) |
| ≥ 11 | 63,896 (28.61) |
| Levels of nurses, n (%) | |
| Nurse | 60,472 (27.07) |
| Senior nurse | 106,107(47.50) |
| Nurse-in-charge | 49,130 (22.00) |
| Associate chief nurse | 6870 (3.08) |
| Chief nurse | 789 (0.35) |
| Certified diabetes nurse | |
| Yes | 25,289 (11.32) |
| Positions held, n (%) | |
| Head nurse | 15,753 (7.05) |
| Clinical nurse | 206,986 (92.67) |
| Diabetes educator | 629 (0.28) |
| Number of beds at department | |
| Median (Q1, Q3) | 46 (34, 58) |
| < 35 | 57,791 (25.87) |
| 35–45 | 42,132 (18.86) |
| 45–60 | 70,892 (31.74) |
| ≥ 60 | 52,553 (23.53) |
| Hospital setting | |
| Primary care | 1576 (0.71) |
| Secondary care | 25,465 (11.40) |
| Tertiary care | 196,327 (87.89) |
| Department affiliations | |
| ICU | 18,898 (8.46) |
| Pediatrics | 3357 (1.50) |
| Ob/Gyn | 13,264 (5.94) |
| Emergency | 10,503 (4.70) |
| Outpatient | 1432 (0.64) |
| Endocrinology | 13,912 (6.23) |
| Non-endocrinology | 71,368 (31.95) |
| Others | 29,361 (13.14) |
| Surgery | 61,273 (27.43) |
Insulin Injection Knowledge Scores of Nurses
The mean knowledge score of the study population was 13.70 ± 3.30 and 20.91% of the nurses achieved a good knowledge score, 43.90% achieved a satisfactory knowledge score, and 35.19% had a poor knowledge score (Table 2). The mean score of conceptual knowledge mastery was 2.59 ± 0.63, the mean score of procedural knowledge mastery was 7.15 ± 1.97, and the mean factual knowledge mastery score was 2.93 ± 1.19. Less than 50% of the nurses answered seven items correctly in the questionnaire including correct interval between two injections at the same site (16.37%), what type of insulin is Aspart (38.41%), when to inject short-acting insulin (45.71%), injection site management post withdrawal of insulin pen needle (38.93%), mixing method for premixed insulin (43.06%), proper insulin needle disposal after injection (47.97%), and management of hypoglycemia (49.40%) (Table 3).
Table 2.
Overall scores of insulin injection knowledge, attitudes, and practices among nurses
| Variables | |
|---|---|
| Knowledge scores | |
| Mean (SD) | 13.70 (3.30) |
| Range | 1, 21 |
| Score categories, n (%) | |
| Good | 46,697 (20.91) |
| Satisfactory | 98,065 (43.90) |
| Poor | 78,606 (35.19) |
| Mastery of conceptual knowledge | |
| Mean (SD) | 2.59 (0.63) |
| Range | 0, 3 |
| Mastery of procedural knowledge | |
| Mean (SD) | 7.15 (1.97) |
| Range | 0, 11 |
| Mastery of factual knowledge | |
| Mean (SD) | 2.93 (1.19) |
| Range | 0, 5 |
| Attitude scores | |
| Mean (SD) | 17.18 (2.69) |
| Range | 4, 20 |
| Score categories, n (%) | |
| Good | 156,229 (75.25) |
| Satisfactory | 44,837 (21.60) |
| Poor | 6549 (3.15) |
| Practice scores | |
| Mean (SD) | 83.03 (8.16) |
| Range | 21, 90 |
| Score categories, n (%) | |
| Good | 187,791 (90.45) |
| Satisfactory | 17,997 (8.67) |
| Poor | 1827 (0.88) |
Table 3.
Insulin injection knowledge in nurses
| Variables | N (%) |
|---|---|
| 1. What type of insulin is insulin Aspart? | |
| Long-acting insulin | 22,970 (10.28) |
| Short-acting insulin | 97,914 (43.84) |
| Rapid-acting insulin | 85,802 (38.41) |
| Intermediate-acting insulin | 16,682 (7.47) |
| 2. Time of injection of short-acting insulin | |
| After meal | 2439 (1.09) |
| 30 min before meal | 102,097 (45.71) |
| 5–10 min before meal | 62,203 (27.85) |
| Immediately before meal | 56,629 (25.35) |
| 3. Correct storage temperature of unopened insulin | |
| 10–15 °C | 5775 (2.59) |
| 15–30 °C | 6673 (2.99) |
| 2–8 °C | 208,546 (93.36) |
| < 0 °C | 2374 (1.06) |
| 4. How long is insulin placed at room temperature before injection after it is taken out from the refrigerator? | |
| 15 min | 44,747 (20.03) |
| 30 min | 171,131 (76.61) |
| 45 min | 660 (0.30) |
| 60 min | 6830 (3.06) |
| 5. How long can an opened vial of insulin remain at room temperature? | |
| 15 days | 16,906 (7.57) |
| 30 days | 199,378 (89.26) |
| 45 days | 3005 (1.35) |
| 60 days | 4079 (1.83) |
| 6. The safest needle entry length | |
| 4 mm and 6 mm | 186,266 (83.39) |
| 4 mm and 8 mm | 19,252 (8.62) |
| 5 mm and 6 mm | 13,214 (5.92) |
| 5 mm and 8 mm | 4636 (2.08) |
| 7. Which type of skin disinfectant should be used for insulin injection? | |
| Anerdian skin disinfectant | 6171 (2.76) |
| 70–80% ethanol | 210,191 (94.10) |
| Iodophor | 5696 (2.55) |
| Chlorine disinfectant | 1310 (0.59) |
| 8. Appropriate site for insulin injections | |
| Abdomen | 221,417 (99.13) |
| Lateral thigh | 193,877 (86.80) |
| Superolateral buttocks | 169,201 (75.75) |
| Lateral arm | 205,746 (92.11) |
| 9. Rate of absorption of insulin according to injection site (rapid to slow) | |
| Thigh, abdomen, upper arm, buttocks | 3636 (1.63) |
| Abdomen, upper arm, thigh, buttocks | 182,832 (81.85) |
| Abdomen, buttocks, upper arm, thigh | 26,327 (11.79) |
| Upper arm, abdomen, thigh, buttocks | 10,573 (4.73) |
| 10. The minimal distance of injection site from the last injection site | |
| 1 cm | 114,130 (51.10) |
| 2 cm | 67,619 (30.27) |
| 3 cm | 21,268 (9.52) |
| 4 cm | 20,351 (9.11) |
| 11. Interval between two injections at the same site | |
| 1 week | 162,632 (72.81) |
| 2 weeks | 22,449 (10.05) |
| 3 weeks | 1725 (0.77) |
| 4 weeks | 36,562 (16.37) |
| 12. The skin is pinched during insulin injection between | |
| Thumb and ring finger | 7317 (3.28) |
| Thumb and middle finger | 18,167 (8.13) |
| Thumb, middle finger and index finger | 187,046 (83.74) |
| All five fingers | 10,838 (4.85) |
| 13. Entry angle of 4 mm or 5 mm needle | |
| 30° | 19,606 (8.78) |
| 45° | 17,018 (7.62) |
| 60° | 4226 (1.89) |
| 90° | 182,518 (81.71) |
| 14. Entry angle of ≥ 6 mm needle (apart from pinching the skin) | |
| 15° | 17,034 (7.63) |
| 30° | 25,624 (11.47) |
| 45° | 164,302 (73.56) |
| 60° | 16,408 (7.35) |
| 15. How long should the needle stay after insulin pen injection? | |
| 2–3 s | 21,015 (9.41) |
| 6–9 s | 13,495 (6.04) |
| ≥ 10 s | 186,450 (83.47) |
| No | 2408 (1.08) |
| 16. Insulin injection-associated complications | |
| Lipohypertrophy or lipoatrophy | 207,025 (92.68) |
| Infections | 196,579 (88.01) |
| Pain | 197,331 (88.34) |
| Bleeding or congestion | 200,912 (89.95) |
| 17. Proper insulin pen needle disposal method after injection | |
| Recap the needle with a single hand and dispose the needle in the sharp container | 145,972 (65.35) |
| Recap the needle and dispose the needle in the sharp container | 181,819 (81.40) |
| Remove needle using a needle remover or tweezers and dispose the needle in the sharp container | 204,082 (91.37) |
| Recap the needle and leave the needle in the pen | 205,294 (91.91) |
| 18. After withdrawal of insulin pen needle, the injection site should | |
| Be pressed with dry cotton swab | 132,695 (59.41) |
| Be pressed with alcohol cotton swab | 2773 (1.24) |
| Be pressed with fingers | 940 (0.42) |
| Not be pressed | 86,960 (38.93) |
| 19. Incorrect mixing method for insulin | |
| Clear insulin by naked eye does not need to be mixed | 74,857 (33.51) |
| If insulin is not fully mixed, mixing can be repeated | 13,752 (6.16) |
| Insulin pen fill is rolled horizontally between hands ten times and then flipped up and down ten times in 10 s | 38,569 (17.27) |
| When mixing intermediate-acting insulin and short-acting insulin, intermediate-acting insulin should be taken followed by short-acting insulin | 96,190 (43.06) |
| 20. Wrong statement on insulin syringe | |
| U-100 insulin syringe is only suitable for using 100 U/mL insulin | 24,338 (10.90) |
| U-40 insulin syringe should not be used for taking insulin from insulin pen fill for injection | 53,935 (24.15) |
| U-40 insulin syringe can be used for taking insulin from the insulin pen fill | 123,913 (55.47) |
| U-40 insulin syringe is only suitable for 40 U/mL insulin | 21,182 (9.48) |
| 21. Which one of the following is wrong in managing hypoglycemia? | |
| When hypoglycemia is suspected, plasma glucose is immediately tested to ascertain diagnosis. If plasma glucose cannot be measured, treat the patient as having hypoglycemia | 70,562 (31.59) |
| 5% or 10% glucose can be given intravenously in conscious patients | 110,337 (49.40) |
| 15–20 g candy (glucose preferred) can be given orally in conscious patients | 12,133 (5.43) |
| 20 mL 50% glucose can be given by intravenous injection in conscious patients | 30,336 (13.58) |
Correct answer is in italics
Insulin Injection Attitude Scores
In addition, the mean attitude score was 17.18 ± 2.69 for the study nurses; 75.25% nurses achieved a good attitude score, another 21.60% achieved a satisfactory attitude score, and merely 3.15% had a poor attitude score (Table 2). Most nurses considered that insulin injection technique was very important (75.43%) or rather important (17.76%) for plasma glucose control and the majority of the nurses felt that they could inject insulin very properly (41.35%) or rather properly (36.0%) (Table 4). In addition, 46.44% of the nurses were very concerned or rather concerned (29.06%) about the feeling of patients with diabetes receiving insulin injection. Furthermore, 53.24% of the nurses were very concerned or rather concerned (24.39%) about needle reuse by patients with diabetes. Moreover, 42.77% of the nurses felt very confident or rather confident (32.36%) that they could educate patients about insulin injection and 41.73% of the nurses very much wanted or rather wanted (25.55%) to receive formal training on insulin injection.
Table 4.
Insulin injection attitudes among nurses
| Variables | N (%) |
|---|---|
| 1. Do you think that insulin injection technique is important for plasma glucose control? | |
| Not at all | 1332 (0.64) |
| A little bit | 4484 (2.16) |
| Somewhat | 8323 (4.01) |
| Rather | 36,878 (17.76) |
| Very | 156,598 (75.43) |
| 2. Do you think that you can inject insulin properly? | |
| Not at all | 1309 (0.63) |
| A little bit | 7568 (3.65) |
| Somewhat | 38,146 (18.37) |
| Rather | 74,734 (36.00) |
| Very | 85,858 (41.35) |
| 3. How concerned are you about the feeling of diabetic patients at the time of insulin injection? | |
| Not at all | 1076 (0.52) |
| A little bit | 9562 (4.61) |
| Somewhat | 40,233 (19.38) |
| Rather | 60,328 (29.06) |
| Very | 96,416 (46.44) |
| 4. How concerned are you about needle reuse by diabetic patients? | |
| Not at all | 3935 (1.90) |
| A little bit | 9485 (4.57) |
| Somewhat | 33,022 (15.91) |
| Rather | 50,638 (24.39) |
| Very | 110,535 (53.24) |
| 5. Are you confident that you can teach diabetic patients to correctly inject insulin? | |
| Not at all | 1418 (0.68) |
| A little bit | 8915 (4.29) |
| Somewhat | 41,298 (19.89) |
| Rather | 67,193 (32.36) |
| Very | 88,791 (42.77) |
| 6. Do you want to receive formal training on insulin injection? | |
| Not at all | 2611 (1.26) |
| A little bit | 15,461 (7.45) |
| Somewhat | 49,868 (24.02) |
| Rather | 53,043 (25.55) |
| Very | 86,632 (41.73) |
Insulin Injection Practice Scores
The mean practice score of the study population was 83.03 ± 8.16. Most nurses (90.45%) achieved a good practice score, 8.67% had a satisfactory practice score, and only 0.88% had a poor practice score (Table 2). Most nurses always (74.55%) or often (18.66%) washed their hands before injection and 58.86% of the nurses always or often (22.30%) left the unopened vial or insulin pen fill at room temperature for at least 30 min (Table 5). Most nurses always (81.76%) or often (13.80%) verified name, clarity, expiration date, and remaining volume of insulin in the insulin pen fill before injection and 82.34% of the nurses always or often (12.87%) fully mixed premixed insulin before injection while 78.98% of the nurses always or often (12.10%) pushed out air bubbles before injection. In addition, 67.22% of the nurses always or often (19.77%) asked about the site of last injection and 67.38% of the nurses always or often (19.97%) asked about tenderness of the injection site while 73.01% of the nurses always or often (12.62%) used new needles in each injection and 69.51% of the nurses always or often (21.54%) shifted the injection site during each injection. Furthermore, 71.40% of the nurses always or often (15.96%) recapped or removed the needle using the tweezers or needle remover and placed the needle and syringe in a safe container after injection. Additionally, 87.96% of the nurses always or often (9.2%) asked about meal preparation when giving mealtime insulin while 80.51% of the nurses always or often (14.72%) paid attention to plasma glucose levels in patients with diabetes.
Table 5.
Survey of insulin injection practices among nurses
| Variables | N (%) |
|---|---|
| 1. Wash hand before injection | |
| Never | 679 (0.33) |
| Occasionally | 3711 (1.79) |
| Sometimes | 9695 (4.67) |
| Often | 38,745 (18.66) |
| Always | 154,785 (74.55) |
| 2. Unopened vial of insulin or insulin pen fill is left at room temperature for 30 min after being taken out from the refrigerator | |
| Never | 5292 (2.55) |
| Occasionally | 9746 (4.69) |
| Sometimes | 24,078 (11.60) |
| Often | 46,298 (22.30) |
| Always | 122,201 (58.86) |
| 3. Name, character, expiration date, and remaining volume of insulin in the insulin pen fill is checked before injection | |
| Never | 706 (0.34) |
| Occasionally | 2237 (1.08) |
| Sometimes | 6284 (3.03) |
| Often | 28,646 (13.80) |
| Always | 169,742 (81.76) |
| 4. Full mixing is done before injection of premixed insulin | |
| Never | 1277 (0.62) |
| Occasionally | 2174 (1.05) |
| Sometimes | 6485 (3.12) |
| Often | 26,720 (12.87) |
| Always | 170,959 (82.34) |
| 5. Push out air bubbles in the insulin pen or syringe before injecting insulin | |
| Never | 4837 (2.33) |
| Occasionally | 4290 (2.07) |
| Sometimes | 9408 (4.53) |
| Often | 25,112 (12.10) |
| Always | 163,968 (78.98) |
| 6. The volume button in the insulin pen is set to the right dose before use | |
| Never | 1485 (0.72) |
| Occasionally | 1232 (0.59) |
| Sometimes | 2863 (1.38) |
| Often | 13,927 (6.71) |
| Always | 188,108 (90.60) |
| 7. Ask about meal preparation when giving mealtime insulin | |
| Never | 506 (0.24) |
| Occasionally | 1260 (0.61) |
| Sometimes | 4137 (1.99) |
| Often | 19,100 (9.20) |
| Always | 182,612 (87.96) |
| 8. Pay attention to plasma glucose levels in patients | |
| Never | 437 (0.21) |
| Occasionally | 1682 (0.81) |
| Sometimes | 7786 (3.75) |
| Often | 30,556 (14.72) |
| Always | 167,154 (80.51) |
| 9. Ask about site of last injection | |
| Never | 1619 (0.78) |
| Occasionally | 5529 (2.66) |
| Sometimes | 19,854 (9.56) |
| Often | 41,046 (19.77) |
| Always | 139,567 (67.22) |
| 10. Ask about injection site tenderness prior to injection | |
| Never | 1304 (0.63) |
| Occasionally | 5099 (2.46) |
| Sometimes | 19,869 (9.57) |
| Often | 41,452 (19.97) |
| Always | 139,891 (67.38) |
| 11. Injection site is shifted during each injection | |
| Never | 1003 (0.48) |
| Occasionally | 3226 (1.55) |
| Sometimes | 14,359 (6.92) |
| Often | 44,717 (21.54) |
| Always | 144,310 (69.51) |
| 12. Prior to injection, injection site is carefully examined for skin induration or swelling | |
| Never | 3220 (1.55) |
| Occasionally | 6425 (3.09) |
| Sometimes | 20,880 (10.06) |
| Often | 44,260 (21.32) |
| Always | 132,830 (63.98) |
| 13. The injection site is disinfected and becomes dry before injection | |
| Never | 512 (0.25) |
| Occasionally | 1747 (0.84) |
| Sometimes | 7048 (3.39) |
| Often | 35,151 (16.93) |
| Always | 163,157 (78.59) |
| 14. Skin pinching technique or entry at an angle of 45° is done when using ≥ 6 mm insulin pen or syringe | |
| Never | 2874 (1.38) |
| Occasionally | 3399 (1.64) |
| Sometimes | 14,080 (6.78) |
| Often | 46,653 (22.47) |
| Always | 140,609 (67.73) |
| 15. Insulin is injected despite injection site skin induration or swelling | |
| Never | 167,131 (80.50) |
| Occasionally | 8956 (4.31) |
| Sometimes | 2914 (1.40) |
| Often | 4703 (2.27) |
| Always | 23,911 (11.52) |
| 16. New needle is used each time insulin is injected | |
| Never | 1394 (0.67) |
| Occasionally | 8535 (4.11) |
| Sometimes | 19,905 (9.59) |
| Often | 26,208 (12.62) |
| Always | 151,573 (73.01) |
| 17. Needle remains subcutaneously for at least 10 s after insulin is injected | |
| Never | 1574 (0.76) |
| Occasionally | 2242 (1.08) |
| Sometimes | 6159 (2.97) |
| Often | 22,287 (10.73) |
| Always | 175,353 (84.46) |
| 18. After insulin is injected, the needle is recapped or is removed using tweezers or needle remover and the needle and syringe are placed in a safe container | |
| Never | 5773 (2.78) |
| Occasionally | 6313 (3.04) |
| Sometimes | 14,148 (6.81) |
| Often | 33,138 (15.96) |
| Always | 148,243 (71.40) |
Correlation Among Insulin Injection Knowledge, Attitude, and Practice Scores Among Nurses
We analyzed the correlation among insulin injection knowledge, attitude, and practice scores among nurses. Pearson correlation analysis showed significant correlation between the knowledge score and the attitude score (r = 0.29; P < 0.001) and between the knowledge score and the practice score (r = 0.27; P < 0.001) (Table 6 and Supplementary Tables 1 and 2). Furthermore, the attitude score exhibited significant correlation with the practice score (r = 0.56; P < 0.001). These findings were further confirmed by our Spearman correlation analysis. Our multivariate analysis additionally revealed that nurses with higher knowledge scores were also more likely to have higher attitude scores and practice scores (Table 7) and nurses with higher attitude scores were also more likely to have higher practice scores.
Table 6.
Correlation among insulin injection knowledge, attitude, and practice scores among nurses
| Pearson correlation coefficient, N = 207,615 | Spearman correlation coefficient, N = 207,615 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| Variables | Correlation value | Knowledge score | Attitude score | Practice score | Variables | Correlation value | Knowledge score | Attitude score | Practice score |
| Knowledge score | r | 1 | 0.29 | 0.27 | Knowledge score | r | 1 | 0.26 | 0.24 |
| p | < 0.0001 | < .0.0001 | p | < 0.0001 | < 0.0001 | ||||
| Attitude score | r | 0.29 | 1 | 0.57 | Attitude score | r | 0.26 | 1 | 0.54 |
| p | < 0.0001 | < 0.0001 | p | < 0.0001 | < 0.0001 | ||||
| Practice score | r | 0.27 | 0.7 | 1 | Practice score | r | 0.24 | 0.54 | 1 |
| p | < .0.0001 | < 0.0001 | p | < 0.0001 | < 0.0001 | ||||
Table 7.
Multivariate logistic regression analysis for risk factors of poor insulin injection knowledge, attitude, and practice scores among nurse
| Variables | Knowledge score | Attitude score | Practice score | |||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Gender | ||||||
| Male vs. female | 1.625 | 1.541, 1.714 | 1.021 | 0.963, 1.082 | 1.420 | 1.307, 1.542 |
| Age, years | ||||||
| < 25 vs. ≥ 35 | 0.734 | 0.692, 0.778 | 1.046 | 0.979, 1.118 | 1.064 | 0.959, 1.180 |
| 25–30 vs. ≥ 35 | 0.930 | 0.886, 0.975 | 1.024 | 0.969, 1.082 | 1.122 | 1.029, 1.223 |
| 30–35 vs. ≥ 35 | 1.015 | 0.978, 1.054 | 1.116 | 1.067, 1.168 | 1.243 | 1.157, 1.334 |
| Education | ||||||
| Technical secondary school vs. master or above | 1.889 | 1.682, 2.120 | 0.920 | 0.793, 1.067 | 0.695 | 0.562, 0.859 |
| Junior college vs. master or above | 1.350 | 1.226, 1.486 | 0.834 | 0.733, 0.948 | 0.599 | 0.500, 0.718 |
| Bachelor vs. master or above | 1.078 | 0.981, 1.185 | 0.830 | 0.731, 0.943 | 0.637 | 0.533, 0.760 |
| Levels of nurse | ||||||
| Nurse vs. chief nurse | 1.708 | 1.467, 1.988 | 0.889 | 0.670, 1.179 | 1.301 | 0.794, 2.132 |
| Senior nurse vs. chief nurse | 1.174 | 1.011, 1.364 | 0.905 | 0.683, 1.200 | 1.476 | 0.902, 2.416 |
| Nurse-in-charge vs. chief nurse | 0.815 | 0.703, 0.946 | 0.920 | 0.694, 1.220 | 1.596 | 0.974, 2.615 |
| Associate chief nurse vs. chief nurse | 0.784 | 0.672, 0.915 | 0.719 | 0.527, 0.980 | 1.220 | 0.710, 2.099 |
| Certified diabetes nurse | ||||||
| No vs. yes | 0.735 | 0.715, 0.756 | 1.136 | 1.098, 1.175 | 0.934 | 0.887, 0.983 |
| Positions held | ||||||
| Head nurse vs. diabetes educator | 3.256 | 2.635, 4.023 | ||||
| Clinical nurse vs. diabetes educator | 1.659 | 1.346, 2.044 | 1.392 | 1.070, 1.811 | 0.840 | 0.583, 1.209 |
| Number of beds | ||||||
| < 35 vs. ≥ 60 | 1.016 | 0.988, 1.045 | 0.933 | 0.903, 0.965 | 0.874 | 0.830, 0.921 |
| 35–45 vs. ≥ 60 | 0.935 | 0.910, 0.961 | 0.901 | 0.873, 0.931 | 0.931 | 0.885, 0.978 |
| 45–60 vs. ≥ 60 | 0.959 | 0.936, 0.982 | 0.938 | 0.913, 0.965 | 0.970 | 0.929, 1.012 |
| Duration of employment, years | ||||||
| < 4 vs. ≥ 11 | 0.840 | 0.798, 0.884 | 1.504 | 1.419, 1.595 | 1.363 | 1.246, 1.492 |
| 4–7 vs. ≥ 11 | 0.958 | 0.916, 1.002 | 1.330 | 1.263, 1.401 | 1.363 | 1.259, 1.475 |
| 7–11 vs. ≥ 11 | 1.024 | 0.988, 1.062 | 1.237 | 1.186, 1.290 | 1.247 | 1.168, 1.331 |
| Healthcare setting | ||||||
| Secondary vs. primary | 1.304 | 1.165, 1.459 | 0.889 | 0.777, 1.016 | 1.129 | 0.903, 1.410 |
| Tertiary vs. primary | 1.218 | 1.091, 1.360 | 0.827 | 0.725, 0.943 | 1.122 | 0.902, 1.396 |
| Departments | ||||||
| ICU vs. surgery | 1.059 | 1.018, 1.101 | 1.327 | 1.270, 1.387 | 0.988 | 0.922, 1.059 |
| Pediatrics vs. surgery | 0.946 | 0.880, 1.018 | 1.176 | 1.077, 1.283 | 0.613 | 0.523, 0.719 |
| Obstetrics vs. surgery | 0.959 | 0.922, 0.998 | 1.070 | 1.022, 1.120 | 0.772 | 0.714, 0.834 |
| Emergency vs. surgery | 1.171 | 1.119, 1.225 | 1.400 | 1.332, 1.473 | 1.001 | 0.926, 1.082 |
| Outpatient department vs. surgery | 1.133 | 1.015, 1.265 | 0.978 | 0.825, 1.159 | 1.009 | 0.769, 1.325 |
| Endocrinology vs. surgery | 0.305 | 0.290, 0.320 | 0.442 | 0.416, 0.470 | 0.725 | 0.658, 0.799 |
| Internal medicine excluding endocrinology vs. surgery | 0.866 | 0.847, 0.886 | 0.990 | 0.964, 1.017 | 1.068 | 1.025, 1.112 |
| Others vs. surgery | 1.044 | 1.013, 1.075 | 1.002 | 0.968, 1.038 | 1.027 | 0.973, 1.084 |
| Knowledge scores | ||||||
| Good vs. poor | – | – | 0.272 | 0.263, 0.281 | 0.351 | 0.331, 0.372 |
| Satisfactory vs. poor | – | – | 0.530 | 0.518, 0.542 | 0.586 | 0.566, 0.607 |
| Attitude scores | ||||||
| Good vs. poor | – | – | – | – | 0.049 | 0.046, 0.051 |
| Satisfactory vs. poor | – | – | – | – | 0.338 | 0.320, 0.357 |
Our multivariate analysis further showed that male gender was a significant risk for lower knowledge score (OR 1.625; 95% CI 1.541, 1.714) and attitude score (OR 1.021, 95% CI 0.963, 1.082) (Table 7). Age < 25 years was associated with a higher knowledge score versus age ≥ 35 years (OR 0.734; 95% CI 0.692, 0.778) while age between 30 and 35 years was a significant risk for lower attitude score (OR 1.116; 95% CI 1.067, 1.168) and practice score versus age ≥ 35 years (OR 1.243; 95% CI 1.157, 1.334). In addition, nurses with lower educational levels were in general more likely to have a poor knowledge score but were more likely to have a higher attitude score and a higher practice score. Furthermore, nurses with a shorter work history were more likely to have a poor attitude score and a poor practice score than nurses with a longer work history. Nurses at lower professional ranks were less likely to have a poor attitude score compared with higher level nurses and nurses were more likely to have a poor knowledge score compared to chief nurses (OR 1.708; 95% CI 1.467, 1.988). Furthermore, clinical nurses were more likely than diabetes educators to have a lower knowledge score (OR 1.659; 95% CI 1.346, 2.044) and a lower attitude score (OR 1.392; 95% CI 1.070, 1.811). Moreover, non-certified diabetes nurses were less likely to have a poor knowledge score (OR 0.735; 95% CI 0.715, 0.756) but more likely to have a poor attitude score compared to certified diabetes specialist nurses (OR 1.136; 95% CI 1.098, 1.175). Compared to nurses in the primary care setting, nurses in the secondary care setting were more likely to have a poor knowledge score (OR 1.304; 95% CI 1.165, 1.459), but they (OR 0.889; 95% CI 0.777, 1.016) and nurses in tertiary care setting (OR 0.827; 95% CI 0.725, 0.943) were less likely to have a lower attitude score. Compared to nurses from endocrinology department, nurses from non-endocrinology departments were more likely to have a poor knowledge, attitude, and practice score. Emergency nurses had the lowest knowledge and practice scores while ICU nurses had lower attitude and practice scores.
Discussion
Our study revealed some deficiencies in insulin injection knowledge, attitudes, and practices, which was similar to the previous studies [11–17]. The study showed that only 64.81% of the nurses achieved a good or satisfactory knowledge score, which was in line with 66.2% of nurses at a tertiary care hospital in Hunan province, but lower than 83.5% of nurses at another tertiary care hospital in Guangdong province, suggesting that the insulin injection knowledge levels of nurses may differ across regions in China. In addition, we found that nurses at secondary care hospitals had the lowest overall score, indicating that secondary care nurses may be a weak link in insulin injection management. This could be due to the point-to-point coupling of primary care clinics and tertiary care hospitals in China. Nurses in the primary care setting had the highest overall score which may be because community hospital nurses carry out the job of chronic disease management and nurses have more opportunities to educate patients with diabetes on injection. Moreover, most (93.77%) of the nurses in this study were from non-endocrinology departments. The result showed that diabetes educators had higher overall score than other types of nurses, indicating that training on insulin injection knowledge should focus more on non-diabetes clinic nurses.
It has been shown that nurses showed deficiencies in diabetes and diabetes care knowledge [18]. Our study further revealed that approximately one-third of the nurses surveyed had a poor insulin injection knowledge score and the deficits were particularly acute in injection site management and insulin needle disposal and hypoglycemia management. Our study revealed that approximately two in ten nurses (22.37%) did not show much concern about needle reuse by diabetic patients. A survey of 380 patients with diabetes from 20 centers in China showed that the rate of single needle reuse was high in patients with diabetes and needle reuse significantly correlated with lipohypertrophy (r = 0.426, P = 0.000) [19]. Song et al. also showed that Chinese patients with diabetes had a higher needle reuse rate than patients in other countries (78% vs. 48%) [20]. It remains to be investigated whether greater nurse concern about needle reuse by patients with DM lowers the rate of single needle reuse in patients with DM. These issues are important barriers for effective and safe management of insulin injection. We speculate that the poor knowledge scores are due to inadequate training and not being up to date about current guidelines on diabetes. Dai et al. found that only 56.87% nurses at tertiary care institutions knew about the most recent guideline for insulin injection in patients with diabetes [21], highlighting the need for workplace-based learning and training based on the latest guidelines to further enhance insulin injection-related knowledge, attitude, and practice.
The current study showed that 96.85% of nurses achieved a good or satisfactory attitude score, indicating an overall positive attitude among nurses in China. Considering the relatively low knowledge scores of the nurses, it remains possible that the nurses may overestimate their attitudes and practices in self-evaluation. However, this is speculative given the subjective nature of the current questionnaire in the study and that no real-world practices were assessed, and no skill tests were performed. In addition, approximately one-quarter of the nurses were inadequate in confidence in proper injection, concern for the feeling of patients with diabetes, repetitive use of insulin needles, and confidence in instructing insulin injection. Approximately two in three (67.28%) nurses felt that they need training on insulin injection. Furthermore, we found that a quarter of the nurses were not fully confident about teaching diabetic patients about correct insulin injection techniques. As mastery of insulin injection knowledge and insulin injection techniques is essential for nurses to administer insulin correctly and to educate patients adequately, our findings highlight the importance of improving nurses’ insulin injection knowledge and practice and the need for patient education. In addition, patient education regarding correct and safe insulin injection practices may also be improved with increased insulin injection knowledge by nurses as patients with diabetes have a deficit in insulin injection technique [22, 23].
Theofanidis found that nurses had a poor compliance rate of insulin injection practices and 42.7% of the nurses did not check for air bubbles in the syringe and 89.1% of the nurses did not check the injection site for appropriateness or other possible complications [11]. In our study, approximately 90% of the nurses always or often check for air bubbles in the syringe before injection and about 85% of them carefully examined the insulin injection site before injection, indicating that nurses in China have better rates of good insulin injection practice.
The study further found significant correlation among knowledge, attitude, and practice scores of the nurses, suggesting that both knowledge and attitudes influence practices, emphasizing the importance of mastery of knowledge of proper insulin injection. To improve the levels of knowledge and attitudes that influence practices among non-endocrinology nurses, endocrinology nurses and diabetes liaison nurses could play a bigger role. A hospital diabetes management group should be established to promote standardized insulin injection procedures and centralized training and examination so that insulin injection can be provided at the same standard at different departments and across different institutions.
This is the first cross-sectional study of insulin injection knowledge, attitude, and practice among nurses at different healthcare settings across China. It uncovers certain areas of deficiencies in nurses’ knowledge and practices like lack of knowledge that can be addressed to improve nurses’ practices and thus diabetes care. However, this study has some limitations. One is that the assessment was done by the nurses themselves, which may raise the question about the objectivity of the nurses’ answers. In addition, the injection techniques skills probed in the questionnaire were not verified in real-world practice. Another limitation is that we did not analyze the results of the study by healthcare settings. The study surveyed nurses from the primary, secondary, and tertiary care settings. The primary care setting has a very high proportion of chronic patients including patients with diabetes. As a result, these nurses may put more emphasis on learning insulin injection knowledge and skills, which may affect their insulin injection knowledge, attitudes, and practice scores. We will further carry out analysis of performance of nurses in these areas in the future to see how nurses from different healthcare settings differ in insulin injection knowledge, attitudes, and practice scores and provide recommendations on improving their insulin injection knowledge, attitudes, and practice abilities through continuing education and standardized training.
Conclusions
Less than two-thirds of the nurses surveyed achieved a good or satisfactory knowledge score while more than 95% of them achieved a good or satisfactory attitude or practice score. Our study highlights the need for workplace-based learning and training to further enhance insulin injection-related knowledge, attitude, and practice.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
Thanks to all the experts and staff who participated in the project. Thanks to Chinese Nursing Association and Becton Dickinson (BD) for their contribution.
Author’s Contributions
Xinjuan Wu and Fang Zhao contributed to the study conception and design. All authors collected the data and performed the data analysis. All authors contributed to the interpretation of the data and the completion of figures and tables. All authors contributed to the drafting of the article and final approval of the submitted version.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Disclosures
Xinjuan Wu, Fang Zhao, Mingxia Zhang, Li Yuan, Yining Zheng, Jin Huang, Yangxi Li and Caihong Li declare that they have nothing to disclose.
Funding
This study and journal’s Rapid Service Fee was funded by BD. No healthcare professional received payment for participating in the study, and no payments were given to any author for the publication of this article.
Compliance with Ethics Guidelines
The study protocol ethical approval was granted by the ethics committee of China–Japan Friendship Hospital (No. 2019-68-K47). All procedures performed in studies involving human participants were in accordance with the Helsinki Declaration of 1964, and its later amendments. All study subjects provided written informed consent prior to enrollment.
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Footnotes
Xinjuan Wu and Fang Zhao contributed equally to this work.
References
- 1.NCD Risk Factor Collaboration (NCD-RisC) Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 44 million participants. Lancet. 2016;387(10027):1513–1530. doi: 10.1016/S0140-6736(16)00618-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guariguata L, Whiting DR, Hambleton I, Beagley J, Linnenkamp U, Shaw JE. Global estimates of diabetes prevalence for 2013 and projections for 2035. Diabetes Res Clin Pract. 2014;103(2):137–149. doi: 10.1016/j.diabres.2013.11.002. [DOI] [PubMed] [Google Scholar]
- 3.IDF Diabetes Atlas. 9th Edition. 2019. https://www.d-net.idf.org/upload/resources/material/20200302_133351_IDFATLAS9e-final-web.pdf [DOI] [PubMed]
- 4.Frid AH, Hirsch LJ, Menchior AR, Morel DR, Strauss KW. Worldwide injection technique questionnaire study: population parameters and injection practices. Mayo Clin Proc. 2016;91(9):1212–1223. doi: 10.1016/j.mayocp.2016.06.011. [DOI] [PubMed] [Google Scholar]
- 5.Frid AH, Hirsch LJ, Menchior AR, Morel DR, Strauss KW. Worldwide injection technique questionnaire study: population parameters and injection practices. Mayo Clin Proc. 2016;91(9):1224–1230. doi: 10.1016/j.mayocp.2016.06.012. [DOI] [PubMed] [Google Scholar]
- 6.Prieto-Sanchez LM. Hyperglycemia in-hospital management. Ther Adv Endocrinol Metab. 2011;2(1):3–7. doi: 10.1177/2042018810397083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Misnikova IV, Gubkina VA, Lakeeva TS, Dreval AV. A randomized controlled trial to assess the impact of proper insulin injection technique training on glycemic control. Diabetes Ther. 2017;8(6):1309–1318. doi: 10.1007/s13300-017-0315-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grassi G, Scuntero P, Trepiccioni R, Marubbi F, Strauss K. Optimizing insulin injection technique and its effect on blood glucose control. J Clin Transl Endocrinol. 2014;1(4):145–150. doi: 10.1016/j.jcte.2014.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Frid AH, Kreugel G, Grassi G, et al. New insulin delivery recommendations. Mayo Clin Proc. 2016;91(9):1231–1255. doi: 10.1016/j.mayocp.2016.06.010. [DOI] [PubMed] [Google Scholar]
- 10.Chinese Diabetes Society. Chinese diabetes drug delivery guideline (2016). Chinese J Diabetes Mellitus. 2017;9(2):79–105. 10.3760/cma.j.issn.1674-5809.2017.02.005. http://rs.yiigle.com/CN115791201702/945763.htm.
- 11.Theofanidis D. In-hospital administration of insulin by nurses in northern Greece: an observational study. Diabetes Spectr. 2017;30(3):175–181. doi: 10.2337/ds16-0001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Robb A, Reid B, Laird EA. Insulin knowledge and practice: a survey of district nurses in Northern Ireland. Br J Community Nurs. 2017;22(3):138–145. doi: 10.12968/bjcn.2017.22.3.138. [DOI] [PubMed] [Google Scholar]
- 13.Derr RL, Sivanandy MS, Bronich-Hall L, Rodriguez A. Insulin-related knowledge among health care professionals in internal medicine. Diabetes Spectr. 2007;20(3):177–185. doi: 10.2337/diaspect.20.3.177. [DOI] [Google Scholar]
- 14.Mushta AM. Study of insulin injection technique amongst the nursing staff. Pak J Med Sci. 2006;22(3):310–312. [Google Scholar]
- 15.Yacoub MI, Demeh WM, Darawad MW, Barr JL, Saleh AM, Saleh MY. An assessment of diabetes-related knowledge among registered nurses working in hospitals in Jordan. Int Nurs Rev. 2014;61(2):255–262. doi: 10.1111/inr.12090. [DOI] [PubMed] [Google Scholar]
- 16.Adhikari S, Poudel RS, Rajbanshi L, Shrestha S. Assessment of insulin injection practice of nurses working in a tertiary healthcare center of Nepal. Nurs Res Pract. 2018;2018:9375067. doi: 10.1155/2018/9375067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wei SF, Xu P, Li YP, Wang P, Si DQ. Analysis of hidden dangers of non-endocrine insulin use and countermeasures. Nurs Pract Res. 2012;9(5):90–91. [Google Scholar]
- 18.Alotaibi A, Al-Ganmi A, Gholizadeh L, Perry L. Diabetes knowledge of nurses in different countries: an integrative review. Nurse Educ Today. 2016;39:32–49. doi: 10.1016/j.nedt.2016.01.017. [DOI] [PubMed] [Google Scholar]
- 19.Ji J, Lou Q. Insulin pen injection technique survey in patients with type 2 diabetes in mainland China in 2010. Curr Med Res Opin. 2014;30(6):1087–1093. doi: 10.1185/03007995.2014.895711. [DOI] [PubMed] [Google Scholar]
- 20.Song Z, Guo X, Ji L, Huang X, Hirsch LJ, Strauss KW. Insulin injection technique in China compared with the rest of the world. Diabetes Ther. 2018;9(6):2357–2368. doi: 10.1007/s13300-018-0525-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dai M, Liang H, Huang J. Investigation of insulin injection knowledge, belief and practice among clinical nurses from grade three general hospitals. J Nurs Sci. 2019;34(24):60–63. [Google Scholar]
- 22.Gentile S, Strollo F, Guarino G, Giancaterini A, Ames PRJ, Speese K, Guida P, Strauss K, on behalf of the AMDOSDI Italian Injection Technique Study Group Factors hindering correct identification of unapparent lipohypertrophy. J Diab Metab Dis Contr. 2016;3:00065. [Google Scholar]
- 23.Gentile S, Guarino G, Giancaterini A, Guida P, Strollo F, AMD-OSDI Italian Injection Technique Study Group A suitable palpation technique allows to identify skin lipohypertrophic lesions in insulin treated people with diabetes. Springerplus. 2016;5:563. doi: 10.1186/s40064-016-1978-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.