To the Editors,
Recently, we have read with interest the article intitled “tongue nodule as primary manifestation of american cutaneous leishmaniasis in an immunocompetent patient” [1], which describes an unusual case of lingual leishmaniasis affecting a 57-year-old man. After incisional biopsy, microscopy showed a dense chronic inflammatory reaction with macrophages containing scarce round-shaped leishmania-like intracytoplasmic inclusions, suggesting the diagnosis of leishmaniasis. Histochemical analysis (Grocott methenamine silver stain [GMS], periodic acid-Schiff [PAS] stain) was not reported. DNA extraction was performed from paraffin-embedded tissue, and subjected to PCR assays with Leishmania-specifc PCR primers, which confirmed the diagnosis of leishmaniasis.
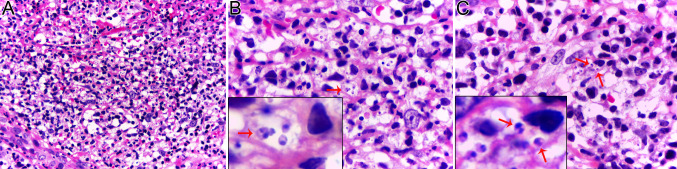
Here, we would like to contribute with an additional case of leishmaniasis, which affected the buccal mucosa of a 65-year-old man. The medical history was noncontributory, including the absence of insect bite report, skin lesion and systemic disease. After incisional biopsy, an exuberant chronic granulomatous inflammation was observed, in which numerous macrophages with clear cytoplasm contained round-shaped intracellular inclusions. The main histopathological differential diagnoses were histoplasmosis and leishmaniasis. However, PAS and GMS stains were negative, excluding histoplasmosis. A detailed microscopic study revealed several amastigotes containing the diagnostic kinetoplast (Fig. 1). Similar with the case reported by Botelho et al. (2020) [1], the PCR assays confirmed the diagnosis of leishmaniasis. The patient was referred to infectious disease service. Currently, he is well, with no alterations in the lesional area.
Fig. 1.
Histopathological findings of oral leishmaniasis. An exuberant granulomatous inflammatory response was observed, showing numerous macrophages containing round-shaped leishmania-like intracytoplasmic inclusions (a × 40). In high-power view, notice several round-shaped intracytoplasmic inclusions exhibiting the diagnostic kinetoplast (arrows) (b and c × 100, oil immersion lens). The areas indicated by the arrows (b and c) are shown in detail in the respective inset. The inset shows (arrow) typical kinetoplast
Leishmaniasis with exclusive involvement of the oral mucosa has been reported [2]. This clinical presentation is very rare. However, some studies indicate that during an early phase of Leishmania braziliensis infection, the parasite spreads to distant sites, before the appearance of cutaneous lesions [2], which can explain the clinical presentation of the current case.
The kinetoplast is a diagnostic structure of the Kinetoplastida order, which encompasses the Trypanosomatidae family. This family comprises species of several genera, including Angomonas, Strigomonas, Crithidia, Leishmania, Trypanosoma, among others. The kinetoplast is a specialized region of the mitochondria harboring the most complex and unusual mitochondrial DNA [3]. The kinetoplast DNA (kDNA) represents approximately 30% of the total cellular DNA [3].
An interesting study of mucosal leishmaniasis [4] reported that the diagnostic kinetoplast of amastigotes are rarely identifiable in histopathological slides. Similarly, the kinetoplast of trypanosomal amastigotes of Chagas disease are difficult to see in histopathological sections [5]. However, if identified, it becomes an important microscopic finding with diagnostic impact, such as observed in the current case. Relevantly, the amastigotes of leishmaniasis and Chagas disease are identical in morphology, being differentiated by cellular location. Leishmania usually concentrates within macrophages, whereas Trypanosoma cruzi has a predilection for myocyte fiber. Moreover, oral involvement by Chagas diasease is extremely rare, a clinical finding that aids in the differential diagnosis.
Such as above commented, the diagnosis of histoplasmosis was initially considered as a strong possibility in the current case. However, PAS and GMS stain were negative, with PCR assays confirming the diagnosis of leishmaniasis. In addition to PCR assays, the immunohistochemistry, using Leishmania specific monoclonal antibodies, is also another important tool that supports the diagnosis of lesihmaniasis with high sensitivity and specificity [2]. Furthermore, it is important to mention that Histoplasma shows lack of kinetoplast, similar to that observed with Toxoplasma [5]. In addition, unlike histoplasmosis, oral involvement by toxoplasmosis is rare, and GMS stain positivity excludes the diagnosis of toxoplasmosis.
In our experience, the Giemsa and Toluidine blue stains often show equivocal results, when assessing histopathological sections of suspected leishmaniasis cases.
In summary, the current case shows that the detection of kinetoplast in intracytoplasmic round-shaped inclusions inside macrophages, when assessing histopathological sections of paraffin-embedded tissue, strongly assists in the diagnosis of leishmaniasis.
Compliance with Ethical Standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical Approval
This article does not contain any studies with human participants or animals performed by any of the authors.
Informed Consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Botelho MCB, Ferreira LL, Fikaris S, Prado-Ribeiro AC, Soubhia AMP, Biasoli ER, Miyahara GI, Bernabé DG. Tongue Nodule as Primary Manifestation of American Cutaneous Leishmaniasis in an Immunocompetent Patient. Head Neck Pathol. 2020 Dec 28. [Online ahead of print]. [DOI] [PMC free article] [PubMed]
- 2.Almeida TF, da Silveira EM, Dos Santos CR, León JE, Mesquita AT. Exclusive primary lesion of oral leishmaniasis with immunohistochemical diagnosis. Head Neck Pathol. 2016;10:533–537. doi: 10.1007/s12105-016-0732-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cavalcanti DP, de Souza W. Thekinetoplast of trypanosomatids: from early studies of electron microscopy to recent advances in atomic force microscopy. Scanning. 2018;2018(19):9603051. doi: 10.1155/2018/9603051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Daneshbod Y, Oryan A, Davarmanesh M, Shirian S, Negahban S, Aledavood A, Davarpanah MA, Soleimanpoor H, Daneshbod K. Clinical, histopathologic, and cytologic diagnosis of mucosal leishmaniasis and literature review. Arch Pathol Lab Med. 2011;135:478–482. doi: 10.5858/2010-0069-OA.1. [DOI] [PubMed] [Google Scholar]
- 5.Sharma N, Melamed M. Diagnosis of leishmania. Arch Pathol Lab Med. 2012;136:353. doi: 10.5858/arpa.2011-0450-LE. [DOI] [PubMed] [Google Scholar]