Abstract
Cannabidiol (CBD), one of the primary non-euphoric components in the Cannabis sativa L. plant, has undergone clinical development over the last number of years as a therapeutic for patients with Lennox-Gastaut syndrome and Dravet syndromes. This phytocannabinoid demonstrates functional and pharmacological diversity, and research data indicate that CBD is a comparable antioxidant to common antioxidants. This review gathers the latest knowledge regarding the impact of CBD on oxidative signalling, with focus on the proclivity of CBD to regulate antioxidants and control the production of reactive oxygen species. CBD is considered an attractive therapeutic agent for neuroimmune disorders, and a body of literature indicates that CBD can regulate redox function at multiple levels, with a range of downstream effects on cells and tissues. However, pro-oxidant capacity of CBD has also been reported, and hence caution must be applied when considering CBD from a therapeutic standpoint. Such pro- and antioxidant functions of CBD may be cell- and model-dependent and may also be influenced by CBD dose, the duration of CBD treatment and the underlying pathology.
Keywords: Cannabidiol, Cannabinoids, Oxidative signalling, Oxidative stress, Reactive oxygen species
Introduction
Production of reactive oxygen species (ROS) is commonly associated with oxidative stress and its pathological role in inflammatory diseases such as multiple sclerosis (MS), rheumatoid arthritis (RA), atherosclerosis and inflammatory bowel disease (IBD) [1–5]. During infection, immune cells produce ROS via the NADPH oxidase 2 (NOX2) complex as a mechanism to eradicate pathogens [6]. When NOX2-generated ROS production is dysregulated due to mutations in NOX2 complex proteins, this can result in defective phagocyte function characterized by severe and recurrent infections defined as chronic granulomatous disease (CGD) [7]. Moreover, ROS produced in the phagosome to activate proteolytic enzymes can escape the immune cell, thus damaging the surrounding tissue [8]. Despite this, it is clear that a deficiency in ROS production has the proclivity to aggravate disease processes [9]. In addition, leukocytes isolated from individuals with chronic MS produce less superoxide than those with a milder disease [10], and a similar scenario has been identified in Guillain–Barré syndrome (a subtype of acute inflammatory demyelinating polyneuropathy), where evidence suggests that leukocytes produce lower levels of oxygen radicals in the most severe cases of disease [11]. Taken together, these findings support a complex role of ROS in regulating inflammation in disease.
In recent years, cannabinoid molecules, such as cannabidiol (CBD) and Δ9-tetrahydrocannabinol (Δ9-THC), have drawn attention due to their anti-inflammatory, antioxidant and neuroprotective properties [12,13]. The most well-described targets for cannabinoids are their specific receptors, the cannabinoid receptors CB1 and CB2 [14,15], but their pharmacological actions are not solely limited to these receptors. Indeed, cannabinoids are lipophilic and certain cannabinoids have also been shown to target a wide range of receptors, including the peroxisome proliferator-activated receptors (PPARs), the transient receptor potential cation channel subfamily V member 1 (TRPV1), G-protein-coupled receptor 55 (GPR55), the 5-hydroxytryptamine receptor subtype 1A (5-HT1A), glycine α1 and α1β receptors, in addition to ion channels (Ca2+) and enzymes such as the adenosine membrane transporter phospholipase A2, lipoxygenase (LO) and cyclooxygenase-2 (COX-2) [16–22]. Depending both on the cannabinoid structure and cell/tissue targeted, the pharmacological effects of cannabinoids may vary.
Overall, cannabinoids have been shown to possess therapeutic efficacy in several inflammatory and neuronal diseases [23]. Given that the production of ROS is an intrinsic feature of neuroinflammation and peripheral immune responses, this review aims to gather the latest knowledge on the action of cannabinoids on oxidative signalling, with focus on the phytocannabinoid CBD. CBD is selected for review given recent advances in its therapeutic development [24–26].
Oxidative signalling and stress
The production and maintenance of controlled levels of intracellular ROS has a key role in several physiological functions, including the maintainance of redox homeostasis, cell cycle signalling and hormone production [27,28]. When present, ROS can regulate several signalling pathways by reacting with transcription factors and genes, modifying their structure and thus their function. Hence, ROS can modulate gene expression patterns and signalling proteins related to the stress response and cell survival mechanisms [29]. It is when this homeostasis is impaired, by either an overproduction of ROS or inefficient ROS scavenging mechanisms, that oxidative stress ensues, promoting cellular damage, lipid peroxidation, DNA modifications and enzyme inactivation, and when persistent, can ultimately lead to cell death and tissue destruction [30–32]. This rationale has been the basis for the development of several anticancer drugs [33–35].
ROS
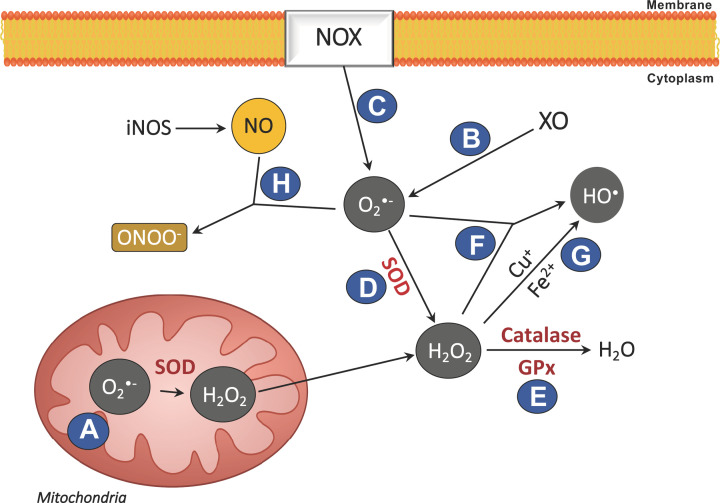
ROS represent a group of unstable oxygen radicals and molecules with strong oxidizing properties. Once formed, ROS are converted to other oxidative species or eliminated by the antioxidant mechanisms of the cell [29,36]. The most common ROS are the superoxide anion (O2•−), hydrogen peroxide (H2O2) and the hydroxyl radical (HO•) [29]. There are three major cellular mechanisms of ROS production as described in Figure 1: (A) ROS are produced via the mitochondrial electron transport chain, in complex I and II; (B) production via the enzymatic reaction catalysed by the enzyme xanthine oxidase (XO); and (C) by NOX as a defence against pathogens [37–39]. To maintain the levels of ROS under control, the enzyme superoxide dismutase (SOD) converts O2•− into H2O2 (D), which is then converted into water, a reaction catalysed by catalase (CAT) and/or glutathione peroxidase (GPx) (E) [40,41]. However, during periods of high ROS generation, H2O2 may cross cell membranes and react with O2•− and metal cations (Fe2+ or Cu+) to form HO• (Fenton and Haber–Weiss reactions) (F, G) [42]. Furthermore, oxygen radicals can also react with nitrogen species, namely nitric oxide (NO) (H). The reaction of O2•− with NO can generate the production of peroxynitrite (ONOO−) (H) [43], a particularly reactive radical that may promote generalized oxidative/nitrosative damage, including DNA fragmentation and lipid degradation.
Figure 1. Modulation of cellular ROS.
The majority of ROS originate from various sources within the cell. Production is via (A) the mitochondrial electron transport chain, (B) the enzymatic reaction catalysed by XO and (C) by NOX. Endogenous antioxidant mechanisms are exerted via (D) SOD conversion of O2•− to H2O2, followed by conversion to water by (E) CAT and/or GPx. When ROS production exceeds the endogenous antioxidant mechanisms capacity, (F and G) H2O2 may react with O2•− to form HO• (Haber–Weiss and Fenton reactions). (H) Oxygen radicals can also react with NO to generate ONOO-.
NOX2 production of ROS
One of the main cellular sources of ROS is the NOX2 complex, which belongs to a family of NADPH oxidases. NOX are transmembrane enzymes involved in the electron transport across biological membranes by oxidizing intracellular NADPH = NADH, while reducing molecular oxygen into O2•− anions [37]. Among the seven NOX members identified to date, NOX2 has the ability to produce an oxidative burst to eliminate pathogens [44]. The NOX2 complex consists in a transmembrane catalytic core, a heterodimer containing gp91phox and the protein p22phox. On the cytosolic side of the membrane, the proteins p47phox, p67phox, p40phox and Rac (a small GTP-binding protein) regulate the complex activity [37,45].
Antigen-presenting cells can produce ROS upon activation via the NOX2 complex [6,46]. Interestingly, gp91phox is also expressed in bone marrow and thymus, contributing to the role of NOX2-derived ROS in B-/T-cell development and maturation [47,48]. Although phagocytes express high levels of the NOX2 complex, components of this complex are also found in nonphagocytic cells, such as cardiomyocytes, endothelial cells and muscle cells [49–51]. In resting cells, the NOX2 complex remains inactive, and upon exposure to certain stimuli, the complex becomes primed or activated [52]. NOX2 priming prepares the complex to produce ROS, initiating a weak oxidative response without eliciting an oxidative burst. This can occur upon stimulation by pro-inflammatory cytokines (e.g. tumour necrosis factor-α [TNF-α] and interleukin [IL]-1β, toll-like receptor [TLR] agonists, e.g. lipopolysaccharide [LPS], flagellin), OONO− and proteases. The priming induces a partial phosphorylation of p47phox that alters its conformation, thus decreasing its autoinhibition and facilitating its translocation and interaction with the NOX2 enzymatic core. This mechanism exerts tight control over NOX2 activation to prevent unintended O2•− release [53,54]. Full activation of the NOX2 complex requires additional stimuli, such as phorbol 12-myristate 13-acetate, a protein kinase C activator and formyl-methionyl-leucyl phenylalanine, which acts via the formylpeptide receptor. Upon activation, NOX2 increases the production of superoxide [55], and therefore, mutations in any of the components of NOX2 dysregulate its activity and thus ROS signalling [7,56].
Antioxidant mechanisms
Cellular antioxidant mechanisms regulate ROS signalling and furthermore prevent/reduce the oxidation of unintended molecules. Antioxidant mechanisms include enzymes such as CAT, SOD, GPx, thioredoxin and peroxiredoxin, in addition to the radical scavengers such as reduced glutathione (GSH) [40,41,57,58]. As mentioned previously, CAT catalyses the conversion of H2O2 to water (Figure 1), and although this enzyme is highly expressed during inflammation, the GPx enzyme has even higher affinity to the H2O2 radical. GPx activity depends on the GSH ability to be oxidized to glutathione disulfide (GSSG) in the presence of NADPH, thus functioning as a proton donor. The GSH pool is afterwards replenished by both its regeneration from GSSG mediated by GSH reductase and de novo synthesis [59,60]. Additionally, dietary antioxidant molecules are also useful at maintaining the level of ROS by directly scavenging ROS, namely tocopherols (vitamin E) and ascorbic acid (vitamin C) [61,62].
More research is still needed to achieve a deeper understanding on the specific roles for each particular oxygen radical. Current methodologies are limited in their ability to measure isolated radicals but rather a group of radicals, making it difficult to differentiate amongst them. What is known today in the field is based on the use and development of various ROS scavengers, enzyme inhibitors and antioxidant enzymes. Moreover, many in vitro studies employ the use of high levels of ROS and thus do not represent the physiological fine-tune modulatory effects of ROS in vivo.
In consideration of antioxidant mechanisms, much data indicate that nuclear factor erythroid 2-related factor-2 (Nrf2), a ubiquitously expressed redox-sensitive transcription factor, is important in initiating the transcription of antioxidant and cytoprotective genes [63]. In the cytoplasm, Nrf2 is bound to its inhibitor Kelch-like ECH-associated protein1 (Keap1), and in response to pro-oxidant stress, oxidative modification of Keap1 dissociates Keap1 from Nrf2, facilitating the nuclear translocation of Nrf2 [64]. Nrf2 binds to antioxidant response elements (AREs) to orchestrate the expression of antioxidant enzymes, including SOD [65], to promote a reduction in ROS. Antioxidants can act by promoting Nrf2 activation [66,67], and deficiencies in Nrf2 factor have been associated with increased inflammation and carcinogenesis [68]. The enzyme heme oxygenase-1 (HO-1) is a key Nrf2 gene target, and a large body of data indicate that HO-1 possesses diverse antioxidant and anti-inflammatory capacity [69]. HO-1 is an enzyme that catalyses the degradation of heme and is induced under conditions of oxidative stress [70]. Importantly, HO-1 has the proclivity to negate the production of ROS [71] and inflammatory mediators [72], making HO-1 inducers potential therapeutic targets in disease [73].
ROS and oxidative signalling
While some studies suggest that oxidative stress plays a critical role in the progression of diseases including cancer, diabetes and CNS disorders [1–5,74], many studies have failed to demonstrate that the therapeutic effects of antioxidants translate to a clinical setting [75]. Indeed, although antioxidants are believed to wield anti-inflammatory effects, their assessment as therapeutics in both human and rodent studies has provided contradictory findings [76–79]. On the contrary, the use of pro-oxidant molecules, such as phytol (NOX2 activator and vitamin E precursor), can improve, or even prevent, ongoing inflammation in animal models [80]. Considering this, the controlled production of ROS is recognized to exert crucial effects in regulating biological functions and cell signalling. This occurs via the rapid generation and removal of ROS within defined cell compartments, thus avoiding sustained signalling and/or oxidative stress [28]. Contrary to previous interpretation, ROS signalling may regulate the inflammatory response.
As previously described, to eliminate invading pathogens, phagocytic cells produce ROS into phagolysosomes following NOX2 activation, and this results in a pH increase within the vesicles, triggering the activation of proteolytic enzymes which in turn destroys the engulfed pathogens/debris [8,81]. Radicals that escape the vesicle membrane into the cytoplasm are rapidly eliminated by the cell antioxidant mechanisms. It is important to note that there are some indications that ROS production can regulate the activation of the NLRP3 inflammasome during inflammation [82,83]. The inflammasome consists in a protein complex that can activate caspase-1 to control the production of IL-1β, a classic pro-inflammatory cytokine [84]. Although ROS may regulate NLRP3 inflammasome activation, it appears to be independent of NOX2 activation. Other known NLRP3 inflammasome activators include innate stimuli (e.g. pathogens and environmental insults) and particulate adjuvants (e.g. alum, silica and urate crystals) [85].
As previously discussed, NO plays a role on oxidative signalling mechanisms [43], in addition to its important role in modulating physiological functions such as neurotransmission, vasodilation and immunomodulation [86]. NO is synthesized on demand and is produced by one of the three known isoforms of nitric oxide synthase (NOS): neuronal NOS (nNOS), inducible NOS (iNOS) and endothelial NOS (eNOS). The nNOS and eNOS isoforms are constitutively present in neuronal and endothelial cells, respectively [86], while iNOS expression is inducible and regulated at the transcriptional level, particularly in inflamed tissues [87]. As mentioned previously, the reaction of O2•− with NO can generate ONOO− [43] (Figure 1), which can contribute to generalized oxidative/nitrosative damage, including DNA fragmentation and lipid degradation.
Oxidative stress ensues when ROS are produced in high quantities without control, and ROS production plays a key role in neuroimmune disorders, resulting in several harmful nonspecific events such as DNA laddering and lipid peroxidation. While some radicals react rapidly and rarely escape the cell membrane (e.g. O2•−), other more stable radicals can cross the cell membrane and diffuse to adjacent tissues (e.g. H2O2) [88]. Moreover, O2•− gives rise to HO• and perhydroxyl (HOO•) radicals [29,89], with data indicating that the HO• radical can inactivate the mitochondrial enzyme pyruvate dehydrogenase [90], depolymerize gastrointestinal mucin [91] and inflict oxidative DNA damage [92]. The HOO• is also highly deleterious, initiating lipid peroxidation [93], disturbing membrane permeability [94] and demonstrating toxicity [95]. Such events may be associated with mutagenesis in chronic intestinal inflammation [96] and in addition to intestinal inflammation, much data link the production of ROS to the pathology of a range of inflammatory diseases such as RA, atherosclerosis, MS and IBD [1–5]. The key role of ROS in physiological processes adds to the complexity of targeting ROS production therapeutically, and the balance between ROS elimination and generation may be key in terms of the management of disease.
Cannabinoids
The introduction of medicinal cannabis, and cannabis-based therapeutics, to mainstream medicine has proved a controversial topic, although medicinal benefits of the Cannabis sativa L. (C. sativa) plant have been recorded for centuries. Indeed, evidence exists for medicinal use of cannabis dating back to the fourth century when used in the treatment of a broad range of ailments [97]. Much public reticence with the introduction of cannabinoids to a medical setting are associated with the recreational use of cannabis, the euphoric effects of the drug and the evidence linking cannabis abuse with psychosis [98]. With the discovery and characterization of many compounds in C. sativa, in addition to an increase in our understanding of cannabinoid pharmacology and toxicology, selective cannabinoid-based therapeutics continue to make advancement in pre-clinical and clinical studies.
To date, a large body of data suggest that cannabinoids have therapeutic properties, alleviating symptoms of several CNS disorders. Indeed, cannabinoids can mitigate inflammation, reduce CNS spasticity, alleviate neuropathic pain, and a body of evidence indicates that cannabinoids provide neuroprotection following injury or inflammation in the CNS [99,100]. The most well-known cannabinoids are the phytocannabinoids synthesized by C. sativa, including THC, a euphoric component of the plant, in addition to CBD, cannabinol (CBN), cannabichromene (CBC) and cannabigerol (CBG), which are considered non-euphoric cannabinoids [101]. Cannabinoids also include a class of lipid messengers known as endogenous cannabinoids (eCBs), with N-arachidonoylethanolamine (anandamide; AEA) and 2-arachidonoyl-glycerol (2-AG) representing the most actively studied eCBs [102]. Both AEA and 2-AG are synthesized on demand in the body to mediate diverse physiological functions via interaction with a range of receptors, particularly the G-protein-coupled receptors (GPCRs), CB1 and CB2 [103]. The system of eCBs and cannabinoid receptors constitutes the eCB system (ECS). In addition, many synthetic agonists, antagonists and inverse agonists for the cannabinoid receptors have been developed and such classes of molecules are under investigation.
Phytocannabinoids
C. sativa is an annual dioecious plant containing a diverse repertoire of botanical cannabinoids commonly known as phytocannabinoids. To date approximately 150 phytocannabinoids have been characterized in the plant [104]. The primary phytocannabinoids are THC and CBD, which represent the most commonly studied phytocannabinoids in experimental and clinical settings, demonstrating a wide range of effects on physiological processes. Other phytocannabinoids currently under investigation include the less well-characterized phytocannabinoids, CBG and CBC. The biosynthetic pathways involved in the generation of the main classes of phytocannabinoids involve the formation of acidic cannabinoids including cannabigerolic acid (CBGA), the precursor of tetrahydrocannabinolic acid (THCA), cannabidiolic acid (CBDA) and cannabichromenic acid (CBCA), which have poor oxidative stability. Following oxidation or decarboxylation, neutral forms of cannabinoids are generated by heating or naturally as the plant ages [105]. Other compounds isolated from C. sativa include a variety of terpenes [106]. Indeed, over 200 terpenes have been identified, including the monoterpenes (limonene, α-pinene and linalool) and sesquiterpenes (β-caryophyllene), which share the same biological precursor with phytocannabinoids. Terpenes produced by the plant are responsible for the plant aroma [107], acting as botanical insecticides and attracting predatory mites [108].
Phytocannabinoids and terpenes accumulate in the secretory cavity of the glandular trichomes in C. sativa [109,110] and are present in the highest quantity on the female flower of the plant. Male plants produce lower levels of phytocannabinoids [111]. Glandular trichomes consist of a sac-like cavity packed with secretory vesicles known as glandular hairs. Glandular trichomes of C. sativa alter morphology and metabolite content during flower maturation, and phytocannabinoids/terpenes are found on the calyx and the underside of anthers of flowers, leaves and bracts [109]. Trichomes rupture due to environmental stress or damage (due to high temperatures and herbivorous consumption), resulting in the release of phytocannabinoids and terpenes as a noxious, sticky liquid on the plant surface.
The ECS
The activity of phytocannabinoids was initially considered to result from their proclivity to fluidise membranes. However, in the early 1990s the cannabinoid receptors CB1 [14] and CB2 [15], the receptors of the ECS, were identified. Both receptors are GPCRs and are responsible for many of the effects of cannabinoids on physiological systems. CB2 is abundantly expressed in immune tissues [112] and is responsible for many immunomodulatory effects, while CB1 expression is predominantly confined to the CNS, with expression also identified in peripheral tissues including the heart, reproductive organs and thymus [112]. Indeed, CB1 is considered one of the most highly expressed GPCRs in the brain [113]. Under normal physiological conditions CB2 exhibits low basal expression in the CNS, with evidence indicating that this receptor is expressed in the brain stem [114] and on hippocampal pyramidal neurons [115]. Importantly, in pathological conditions, data suggest that the expression of the CB2 receptor is up-regulated, particularly on microglial cells [116]. Cannabinoids vary in their affinity for the cannabinoid receptors. Indeed, THC is a partial agonist for both CB1 and CB2 [117], whereas CBD has low affinity for both CB1 and CB2 [117,118].
The discovery of receptors that mediate the cellular action of components of C. sativa was followed by the subsequent identification of the eCBs, AEA [119] and 2-AG [120,121], again in the early 1990s. eCBs vary in their affinities for the cannabinoid receptors; AEA has relatively high affinity for CB1 but little to no affinity for CB2, while 2-AG is an agonist at both CB1 and CB2 [122]. AEA and 2-AG are non-charged, hydrophobic lipid molecules that can act to control neurotransmission [123] and are produced on demand in response to an increase in intracellular Ca2+ [124–126]. Basal concentrations of 2-AG in brain tissue are 170 times greater than AEA [127]. Furthermore, AEA is a member of the family of N-acylethanolamines, other members of which include the eCB-like compounds, palmitoylethanolamide (PEA) and oleolylethanolamide (OEA), both of which possess diverse physiological functions [128–130].
Although CB1 and CB2 are considered classic cannabinoid receptors, much evidence suggests the existence of further receptor targets for cannabinoids, including nuclear PPARs, GPR55 and the TRPV1. Although GPR55 shares a low amino acid sequence homology with both CB1 and CB2, data indicate that GPR55 is a receptor for cannabinoid ligands including AEA, PEA, THC and CBD [16,17,131–135]. TRPV1 is a cationic channel receptor dependent on intrinsic and extrinsic calcium concentrations, and evidence indicates that TRPV1 is a target for CBD, 2-AG and AEA [18,136,137]. This receptor exists largely on sensory neurons and cannabinoid activity through this receptor has shown significant analgesic potential [138]. Several studies have also shown that CBD targets PPAR-γ [13,19,139,140], and it should also be noted that PEA and OEA can exert their effects via PPARs [141–143]. In terms of CBD, further CB1/2-independent cellular targets include serotonin (5-HT) receptors [19,20,144,145] and both μ- and δ-opioid receptors [146].
Synthetic cannabinoids
Multiple synthetic cannabinoid compounds have been developed with the aim to pharmacologically target specific aspects of the ECS and to facilitate the development of cannabinoid therapeutics [147]. Firstly, the compound WIN55,212-2, an aminoalkylindole derivative, with affinity for both cannabinoid receptors, but binding to CB2 with higher affinity, represents one of the most actively studied synthetic cannabinoids [148,149]. Indeed, research on this compound has shown that WIN55,212-2 is an analgesic in rodent models of neuropathic pain [150] and mechanical allodynia [151], while topical administration of WIN55,212-2 was shown to reduce intraocular pressure in patients with glaucoma [152]. HU-210 is another synthetic cannabinoid agonist that has been extensively researched. HU-210 is a high affinity CB1/CB2 receptor agonist [153,154] with agonist activity also at GPR55 [16]. This cannabinoid has been shown to be protective in models of experimental colitis [155] and photoreceptor degeneration [156]. The canabinoid agonist CP55,940 shares biochemical properties with THC, demonstrates high affinity for CB1 and CB2 [157,158] and is also a GPR55 agonist [16]. CP55,940 has been shown to mitigate tumour-evoked hyperalgesia in murine models in a dose-dependent manner [159] and also possesses antioxidant capacity in neutrophils [160]. The JWH family of synthetic cannabinoids have also been shown to be effective agonists of the cannabinoid receptors. Indeed, evidence indicates that JWH-133, a selective CB2 agonist [161], ameliorates spasticity in murine MS [162] and prevents microglial cell activation and inflammation following exposure to β-amyloid [163]. Finally, ACEA is a well described synthetic CB1 agonist and analogue of AEA [164]. ACEA has the proclivity to protect ischemic neurons from oxygen-glucose deprivation/reoxygenation and middle cerebral artery occlusion [165].
Overall, there is a large array of synthetic cannabinoid ligands currently employed in cannabinoid pharmacological research. Such synthetic cannabinoid ligands are useful pharmacological tools that may be used to identify therapeutic avenues in the ECS.
Antioxidant and anti-inflammatory effects of cannabinoids: focus on CBD
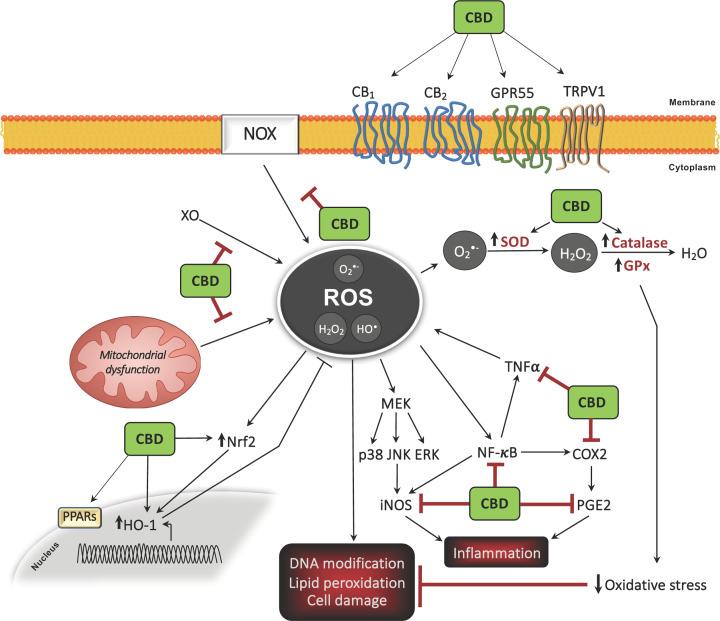
The antioxidative and anti-inflammatory properties of cannabinoids across a variety of tissue types and cellular models have been studied for several decades and are well described [166]. A summary of the antioxidant capacity of CBD is presented in Figure 2. In particular, much evidence has highlighted that CBD, the major non-euphoric phytocannabinoid in C. sativa, has an array of anti-inflammatory effects, with proclivity to modulate oxidative processes in neuropathic and inflammatory models [167]. As discussed previously, CBD can act through cannabinoid receptor-dependent and -independent mechanisms, and demonstrates minimal agonist activity (and very low affinity) for both CB1 and CB2 [117,118]. Furthermore, CB1/2-independent mechanisms of action for CBD have also been identified, including PPAR-γ [13,19,139,140], TRPV1 receptor [18], GPR55 [16], 5-HT receptors [19,20,144,145] and μ-/δ-opioid receptors [146]. Much data suggest that CBD has antioxidant capacity, and CBD has been shown to reduce oxidative metabolism in polymorphonuclear leukocytes [168] and H2O2-treated nucleus pulposus cells [169], and furthemore reduces oxidative stress parameters in aged pancreatic cells [170]. In addition, CBD has the proclivity to improve cell viability following H2O2 treatment [169]. In addition, data from Barichello and colleagues (2012) indicate that CBD reduces host immune responses and exerts an anti-inflammatory effect (reduced cortical TNF-α) in the CNS of rats exposed to intrathecal Streptococcus pneumoniae [171]. This is significant given the key role played by TNF-α in the CNS, particularly in events associated with neuroinflammation, neurodegeneration and neurogenesis [172–174]. Broadly, CBD has an inhibitory effect on TNF-α expression in an array of inflammatory models, which has been recently reviewed by Nicols and Kaplan (2020) [175]. Interestingly, CBD attenuates neural production of ROS following cadmium chloride treatment, in a manner similar to vitamin E (α-tocopheryl acetate) [176], and evidence also suggests that it is more neuroprotectve than ascorbate and α-tocopherol against glutamate toxicity [177]. Owing to its functional and pharmacological diversity, and evidence of is comparable antioxidant capacity to known antioxidants, CBD is an attractive agent for therapeutic immunomodulation and has been studied in conditions including intractable epilepsy [26], Huntington’s disease [178] and schizophrenia [179], amongst others.
Figure 2. Overview of the antioxidant propensity of CBD.
Antioxidant mechanisms of action of CBD
Regulation of antioxidants
A body of research evidence indicates that CBD modifies redox balance by altering the level and activity of antioxidant molecules (Figure 2). Indeed, CBD has been shown to target the regulation of redox-sensitive transcription factors such as Nrf2 in microglia [180], keratinocytes [181] and endothelia [182], which is important given the key role of Nrf2 in initiating the transcription of antioxidant and cytoprotectve genes [63]. Indeed, recent data have shown that CBD can target the expression of Keap1 and Nrf2 in a pulmonary arterty smooth muscles cells, which may contibute to its antioxidant effect in a model of pulmonary arterial hypertension [183]. CBD has also been shown to regulate the expression of the inducible antioxidant enzyme HO-1 in keratinocytes [184], adipose tissue-derived mesenchymal stem cells [185], neuroblastoma cells [186] and smooth muscle [187], which may impact the proclivity of this phytocannabinoid to regulate cellular ROS levels. Indeed, CBD significantly increases HO-1 mRNA and protein expression in human umbilical artery smooth muscle cells in a time- and concentration-dependent manner independent of CB receptors, and this effect was reversed via glutathione precursor N-acetyl cysteine (NAC), indicating the participation of ROS signalling in this process [187]. Similar effects of CBD were determined in human umbilical vein endothelial cells [182]. Data elsewhere indicate that CBD can also regulate the activity of SOD and the enzymatic activity of Cu-, Zn- and Mn-SOD, which metabolize superoxide radicals [181,188]. The vasorelaxant effects of CBD are reduced by a SOD inhibitor, suggesting that CBD acts via SOD to promote its vascular actions [189]. CBD also attenuates hippocampal oxidative damage post-oxygen–glucose-deprivation/reperfusion injury, up-regulating GSH levels and simultaneously increasing SOD1 and GPx activity following injury [190]. In support of this, in vivo administration of CBD attenuates the reduction in reduced/oxidized glutathione ratio (GSH/GSSG) in myocardial tissue of diabetic mice [188], and furthermore prevents GSH depletion in cardiac tissue following doxorubicin cardiotoxicity [191].
Free radical scavenging capacity
A body of data indicates that CBD demonstrates intrinsic free radical scavenging capacity (Figure 2). Indeed, CBD has been shown to ameliorate LPS-induced ROS production in microglia [192]. Furthermore, CBD inhibits mitochondrial superoxide generation in high glucose-stimulated human coronary endothelial cells [193] and reduces mitochondrial ROS generation following hippocampal oxidative damage post-oxygen–glucose-deprivation/reperfusion injury [190]. Neuroprotective effects of CBD have been shown in models of retinal neurotoxicity whereby CBD directly mitigates N-methyl-D-aspartate (NMDA)-mediated oxidative stress by potentially targeting the production of nitrotyrosine, a product of tyrosine nitration [194]. Similarly, oligodendrocyte progenitor cells and keratinocytes are protected from H2O2-induced cell death by CBD, with this phytocannabinoid demonstrating ROS scavenging properties against H2O2-induced ROS in the progenitor cells and keratinocytes [195,196]. CBD was recently shown to exert a similar effect on H2O2-induced ROS in intestinal cell monolayers [197]. Furthermore, data from Branca and colleagues (2019) indicate that CBD attenuates neural ROS production following cadmium chloride exposure in a manner similar to α-tocopheryl acetate [176], and CBD also dose-dependently reduces β-amyloid-induced ROS production in neurons [198]. In parallel, CBD has been shown to ameliorate cisplatin-induced production of renal nitrotyrosine in a model of nephrotoxicity [199] and has also been shown to dose-dependently reduce tert-butyl hydroperoxide-induced ROS production in keratinocytes [184]. In support of this, CBD reduces chemotactic peptide-induced ROS production in polymorphonuclear leukocytes [168] and furthermore in vivo administration of CBD ameliorates the production of ROS, in addition to lipid peroxides, in myocardial tissue of diabetic mice [188]. Finally, recent data from Baeeri and colleagues (2020) indicate that CBD attenuates age-related increases in ROS production in pancreatic islets [170], overall indicating the proclivity of CBD to exert free radical scavenging capacity in response to a multitude of stimuli.
Redox balance
CBD principally affects redox balance via intrinsic mechanisms. Indeed, evidence indiates that CBD interrupts free radical chain reactions, transforming free radicals into more inert molecules via the electrophilic aromatic molecular region and hydroxyl groups of its phenol ring [200]. Using cyclic voltammetry, Hampson et al. (1998) demonstrated that CBD donated electrons at a similar potential to known antioxidants, and using the iron-catalysed ROS production system (Fenton reaction), CBD was shown to prevent hydroperoxide-induced oxidative damage in neurons [177]. Again, using cyclic voltammetry, Hamelink and colleagues (2005) demonstrated that CBD is a comparable antioxidant to the common antioxidants tocopherol and butylated hydroxytoluene [201], with data indicating that CBD can reduce ROS production by chelating transition metal ions involved in the Fenton reaction [202]. Neuroprotective effects of CBD have also been shown following anti-Yo-associated paraneoplastic cerebellar degeneration, where data indicate that CBD minimizes the downgrading of the mitochondrial membrane potential induced by anti-Yo in a manner similar to the ROS scavenger butylated hydroxytoluene, although simultaneously potentiated Yo-induced ROS production [203]. CBD has also been shown to protect hippocampal neurons from energy stress via modulation of glucose consumption by activation of the pentose-phosphate pathway in an oxygen–glucose-deprivation/reperfusion injury model [190].
Indirect antioxidant actions on XO and NOX
In addition to its intrinsic antioxidant function, CBD alters oxidative metabolism through more indirect mechanisms to modulate downstream mediators of oxidative stress (Figure 2). Indeed, Atalay and colleagues (2020) recently demonstrated that CBD attenuates XO activity in keratinocytes exposed to UVB irradiation and H2O2 [204]. CBD has been shown to reduce the expression of the superoxide generators RENOX (NOX4) and NOX1 in a mouse model of cisplatin-induced nephrotoxicity [199], and in a comprehensive study, Rajesh et al. (2010) identified the proclivity of CBD to attenuate diabetes-induced mRNA expression of NADPH oxidase subunits (p22phox, p67phox and gp91phox) in myocardial tissue using a model of diabetic cardiomyopathy [188]. Elsewhere, CBD has been shown to attenuate LPS-induced intracellular NADPH synthesis in microglia [192], and similarly, in vivo administration of CBD reduces the hepatic expression of the NADPH NOX2 isoforms p67phox/gp91phox and nitrosative stress in ethanol-fed mice, while reducing oxidative burst in neutrophils isolated from the livers of ethanol-fed mice [205]. CBD has also been shown to reduce nitrosative stress in cardiac tissue following doxorubicin-induced cardiac injury in rats, promoting a reduction in nuclear factor-κB (NF-κB), Fas ligand, caspase-3 and TNF-α in cardiac tissue following doxorubucin administration [191]. Similarly, CBD attenuates H2O2-induced COX2 and iNOS in nucleus pulposus cells [169], attenuates iNOS expression in the myocarium of diabetic mice [188] and in rats following doxorubicin cardiotoxicity [191], and furthemore attenuates NO expression in paw tissue following sciatic nerve injury and intraplantar injection of complete Freund’s adjuvant [167]. In parallel, Rajesh and colleagues (2007) demonstrated that CBD blunts iNOS expression in high glucose-stimulated human coronary endothelial cells [193], and data elsewhere indicate that CBD inhibits cisplatin-induced renal iNOS in a mouse model of nephrotoxicity [199]. CBD has also been shown to ameliorate plasma levels of prostaglandin E2 (PGE2) in animal models of neuropathic and inflammatory pain, using sciatic nerve constriction and intraplantar injection of complete Freund’s adjuvant, respectively [167]. By lowering ROS levels, CBD therefore protects non-enzymatic antioxidants, preventing their oxidation. Recent evidence also suggests that CBD can ameliorate H2O2-induced IL-1β expression and the expression of other NLRP3 inflammasome-related genes, and this area warrants full investigation [196].
Pro-oxidant effects of CBD
Despite data indicating that CBD promotes antioxidative metabolism in various cells/systems, conflicting data exist regarding the influence of CBD on redox status. The effects of CBD on cell viability [170,181,195,206–210] and proliferation [187,211] are dose-dependent, and this may also be the case with respect to its antioxidant function. Indeed, in terms of ROS production, CBD has been shown to disrupt mitochondrial integrity and also induce ROS production and apoptosis in human CD14+ monocytes in a time-dependent manner [206]. Studies also indicate that CBD elevates intracellular ROS production in several cell systems, including human THP-1 monocytes [207], mouse macrophages [212], breast cancer cells [213] and human glioma cells [214]. Similarly, CBD promotes ROS production to promote apoptosis in leukaemia cells [208], thymocytes [211] and splenocytes [209], and data from Panja and colleagues (2019) indicate that CBD potentiates Yo-induced ROS production in a model of postparaneoplastic cerebellar degeneration treatment [203]. CBD has also been shown to overcome oxaliplatin resistance in human colorectal cancer cells by inducing mitochondrial dysfunction by increasing intracellular ROS and decreasing SOD2 [215]. Data from Gonzalez-Garcia et al. (2017) indicate that CBD induces apoptosis of encephalitogenic cells through oxidative stress induction (increase in ROS) in murine MS [210]. CBD has also been shown to increase the oxygen consumption rate and enhance mitochondrial bioenergetics [190], and at high concentrations can promote COX-2 expression in LPS-treated macrophages [216]. In further support of the pro-oxidant capacity of CBD, it is also important to note that CBD has been shown to increase the expression of the NOX4 and p22phox NAP(P)H oxidases [208], and also enhances the production of the p47 subunit of pro-oxidative NADPH oxidase in endotoxin-treated neutrophils from healthy subjects [217]. Finally, CBD promotes a reduction in GSH in splenocytes [209] and has been shown to deplete GSH in human gliomas [214].
Overall, CBD modulates redox function at multiple levels and a variety of downstream effects are presented in the literature. These pro- and antioxidant functions may be cell- and model-dependent, and may also to be influenced by the dose of CBD delivered, the duration of CBD treatment and the underlying pathology.
Cannabis-based therapeutics
Cannabinoid-based therapeutics are currently approved for a range of symptoms in various disorders; anorexia associated with loss of appetite in acquired immunodeficiency syndrome (AIDS), chemotherapy-associated nausea, spasticity in people with (pw)MS and the treatment of seizures in Lennox-Gastaut and Dravet syndromes. The therapeutics include Epidiolex®, Sativex®, Marinol® and Cesamet®, and such cannabinoid-based therapeutics are used as treatment strategies in those patients where conventional treatments are ineffective.
Of particular relevance to this review, the CBD-based therapeutic in the form of Epidiolex® has recently entered the clinic in the management of epileptic seizures. Epidiolex®, a purified solution of CBD oil formulated for oral administration [24], is a medication approved by the US Food and Drug administration (FDA) and the European Medicines Agency (EMA) for patients with Lennox–Gastaut Syndrome and Dravet syndromes. CBD demonstrates efficacy in reducing convulsive seizure frequency in double-blind placebo-controlled trials [218], and in a prospective open-label study assessing the efficacy of Epidiolex® in patients with treatment resistant epilepsy, Epidiolex® improved the severity and frequency of seizures, and this was sustained for up to 48 weeks of treatment [219]. Devinsky and colleagues (2018) also demonstrated that 10 and 20 mg/kg doses of Epidiolex® (administered as two doses per day over a 14-week period) ameliorated drop seizures in patients with Lennox–Gastaut syndrome, when compared with placebo control cases [25].
In a second cannabis-based therapeutic, CBD is combined with THC as an oromucosal spray (Sativex®), developed to manage spasticity in pwMS [220]. Sativex® can be used as an add-on therapy to ameliorate MS symptoms, with each 100 μl Sativex® actuation delivering 2.5 mg CBD and 2.7 mg THC, in addition to other constituents [221,222]. In terms of effectiveness in ameliorating spasticity, data indicate that the majority of pwMS that administer Sativex® experience an improvement in spasticity score within a 4-week period [223].
Finally, both Marinol® (a pharmaceutical formulation of synthetic THC) and Cesamet® (a synthetic analogue of THC) are FDA approved cannabinoid therapeutics that can be administered orally in tablet form for the managment of chemotherapy-induced nausea/emesis in patients who are refractory to other antiemetics [224,225]. Marinol® is also indicated for anorexia associated with loss of appetite in AIDS patients [225], and data suggest that Cesamet® has efficacy as an analgesic in chronic non-cancer pain [226].
It should be noted that given that adverse effects may be associated with cannabinoids, certain cannabis-based therapeutics are contraindicated in patients with a history of psychotic illness, schizophrenia, substance abuse and also in pregnancy and patients who are breast feeding. Certain cannabis-based therapeutics are also not recommended for use in certain age groups.
Conclusions
It is clear that cannabinoid use in the clinical setting has a wide variety of uses in terms of ameliorating symptoms of neurological disease, such as seizure disorders and MS, and further cannabis-based therapeutics are in the pipeline for a range of disorders. Epidiolex®, a purified solution of CBD, is in the clinic for the management of epileptic seizures. Given the recent advancements in the clinical development of CBD, this review has focussed on the signalling targets for this phytocannabinoid, and in doing so, aimed to outline both the complex role played by ROS in disease processes, in addition to the key role of ROS in regulating biological functions. It is clear that ROS are integral players in neuroinflammation, peripheral immune responses and physiological processes, and herein we have summarized evidence that CBD readily targets oxidative signalling and ROS production. Further research is required to fully understand the interplay of this phytocannabinoid with oxidative signalling. The balance between the ability of CBD to regulate both the generation and elimination of ROS may govern its effectiveness in impacting the symptoms of disease.
Abbreviations
- 2-AG
2-arachidonoyl-glycerol
- 5-HT1A
5-hydroxytryptamine receptor subtype 1A
- AEA
anandamide
- AIDS
acquired immunodeficiency syndrome
- ARE
antioxidant response element
- CAT
catalase
- CBC
cannabichromene
- CBCA
cannabichromenic acid
- CBD
cannabidiol
- CBDA
cannabidiolic acid
- CBG
cannabigerol
- CBGA
cannabigerolic acid
- CBN
cannabinol
- CGD
chronic granulomatous disease
- COX-2
cyclooxygenase-2
- eCB
endocannabinoid
- ECS
eCB system
- EMA
European Medicines Agency
- eNOS
endothelial NOS
- FDA
US Food and Drug administration
- GPCR
G-protein-coupled receptor
- GPR55
G-protein-coupled receptor 55
- GPx
glutathione peroxidase
- GSH
glutathione
- GSSG
glutathione disulfide
- HO-1
heme oxygenase-1
- IBD
inflammatory bowel disease
- IFN
interferon
- IL
interleukin
- iNOS
inducible NOS
- Keap1
kelch-like ECH-associated protein1
- LO
lipoxygenase
- LPS
lipopolysaccharide
- MS
multiple sclerosis
- NAC
N-acetyl cysteine
- NF-κB
nuclear factor-κB
- NMDA
N-methyl-D-aspartate
- nNOS
neuronal NOS
- NO
nitric oxide
- NOS
nitric oxide synthase
- NOX2
NADPH oxidase 2
- Nrf2
nuclear factor erythroid 2-related factor-2
- OEA
oleolylethanolamide
- PEA
palmitoylethanolamide
- PGE2
prostaglandin E2
- PPAR
peroxisome proliferator-activated receptor
- pwMS
people with MS
- RA
rheumatoid arthritis
- ROS
reactive oxygen species
- SOD
superoxide dismutase
- THC
tetrahydrocannabinol
- THCA
tetrahydrocannabinolic acid
- TLR
toll-like receptor
- TNF-α
tumour necrosis factor-α
- TRPV1
transient receptor potential cation channel subfamily V member 1
- XO
xanthine oxidase
Competing Interests
The authors declare that there are no competing interests associated with the manuscript.
Funding
This work is supported by Enterprise Ireland [grant number IP/2018/0740 (to E.J.D.)] and the Provosts PhD Project Awards at Trinity College Dublin (to E.J.D.).
References
- 1.Firuzi O.et al. (2011) Antioxidant therapy: current status and future prospects. Curr. Med. Chem. 18, 3871–3888 10.2174/092986711803414368 [DOI] [PubMed] [Google Scholar]
- 2.Drevet S.et al. (2018) Reactive oxygen species and NADPH oxidase 4 involvement in osteoarthritis. Exp. Gerontol. 111, 107–117 10.1016/j.exger.2018.07.007 [DOI] [PubMed] [Google Scholar]
- 3.Negre-Salvayre A.et al. (2020) Role of reactive oxygen species in atherosclerosis: Lessons from murine genetic models. Free Radic. Biol. Med. 149, 8–22 10.1016/j.freeradbiomed.2019.10.011 [DOI] [PubMed] [Google Scholar]
- 4.Tavassolifar M.J.et al. (2020) The Influence of reactive oxygen species in the immune system and pathogenesis of multiple sclerosis. Autoimmune Dis. 2020, 5793817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Patlevic P.et al. (2016) Reactive oxygen species and antioxidant defense in human gastrointestinal diseases. Integr. Med. Res. 5, 250–258 10.1016/j.imr.2016.07.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kim S.Y.et al. (2017) Pro-inflammatory hepatic macrophages generate ROS through NADPH oxidase 2 via endocytosis of monomeric TLR4-MD2 complex. Nat. Commun. 8, 2247 10.1038/s41467-017-02325-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.O'Neill S.et al. (2015) Genetic disorders coupled to ROS deficiency. Redox Biol. 6, 135–156 10.1016/j.redox.2015.07.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Paiva C.N. and Bozza M.T. (2014) Are reactive oxygen species always detrimental to pathogens? Antioxid. Redox Signal. 20, 1000–1037 10.1089/ars.2013.5447 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dogan S.A.et al. (2018) Perturbed redox signaling exacerbates a mitochondrial myopathy. Cell Metab. 28, 764e5–775e5 10.1016/j.cmet.2018.07.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mossberg N.et al. (2009) Oxygen radical production in leukocytes and disease severity in multiple sclerosis. J. Neuroimmunol. 213, 131–134 10.1016/j.jneuroim.2009.05.013 [DOI] [PubMed] [Google Scholar]
- 11.Mossberg N.et al. (2007) Oxygen radical production and severity of the Guillain–Barre syndrome. J. Neuroimmunol. 192, 186–191 10.1016/j.jneuroim.2007.09.020 [DOI] [PubMed] [Google Scholar]
- 12.Downer E.J. (2011) Cannabinoids and innate immunity: taking a toll on neuroinflammation. Sci. World J. 11, 855–865 10.1100/tsw.2011.84 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Esposito G.et al. (2011) Cannabidiol reduces Abeta-induced neuroinflammation and promotes hippocampal neurogenesis through PPARgamma involvement. PLoS ONE 6, e28668 10.1371/journal.pone.0028668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Matsuda L.A.et al. (1990) Structure of a cannabinoid receptor and functional expression of the cloned cDNA. Nature 346, 561–564 10.1038/346561a0 [DOI] [PubMed] [Google Scholar]
- 15.Munro S., Thomas K.L. and Abu-Shaar M. (1993) Molecular characterization of a peripheral receptor for cannabinoids. Nature 365, 61–65 10.1038/365061a0 [DOI] [PubMed] [Google Scholar]
- 16.Ryberg E.et al. (2007) The orphan receptor GPR55 is a novel cannabinoid receptor. Br. J. Pharmacol. 152, 1092–1101 10.1038/sj.bjp.0707460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pertwee R.G. (2007) GPR55: a new member of the cannabinoid receptor clan? Br. J. Pharmacol. 152, 984–986 10.1038/sj.bjp.0707464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.De Petrocellis L.et al. (2011) Effects of cannabinoids and cannabinoid-enriched Cannabis extracts on TRP channels and endocannabinoid metabolic enzymes. Br. J. Pharmacol. 163, 1479–1494 10.1111/j.1476-5381.2010.01166.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hind W.H., England T.J. and O'Sullivan S.E. (2016) Cannabidiol protects an in vitro model of the blood-brain barrier from oxygen-glucose deprivation via PPARgamma and 5-HT1A receptors. Br. J. Pharmacol. 173, 815–825 10.1111/bph.13368 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Russo E.B.et al. (2005) Agonistic properties of cannabidiol at 5-HT1a receptors. Neurochem. Res. 30, 1037–1043 10.1007/s11064-005-6978-1 [DOI] [PubMed] [Google Scholar]
- 21.Pellati F.et al. (2018) Cannabis sativa L. and nonpsychoactive cannabinoids: their chemistry and role against oxidative stress, inflammation, and cancer. Biomed. Res. Int. 2018, 1691428 10.1155/2018/1691428 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Massi P.et al. (2008) 5-Lipoxygenase and anandamide hydrolase (FAAH) mediate the antitumor activity of cannabidiol, a non-psychoactive cannabinoid. J. Neurochem. 104, 1091–1100 10.1111/j.1471-4159.2007.05073.x [DOI] [PubMed] [Google Scholar]
- 23.Schrot R.J. and Hubbard J.R. (2016) Cannabinoids: medical implications. Ann. Med. 48, 128–141 10.3109/07853890.2016.1145794 [DOI] [PubMed] [Google Scholar]
- 24.Ali S., Scheffer I.E. and Sadleir L.G. (2019) Efficacy of cannabinoids in paediatric epilepsy. Dev. Med. Child Neurol. 61, 13–18 10.1111/dmcn.14087 [DOI] [PubMed] [Google Scholar]
- 25.Devinsky O.et al. (2018) Effect of cannabidiol on drop seizures in the Lennox-Gastaut syndrome. N. Engl. J. Med. 378, 1888–1897 10.1056/NEJMoa1714631 [DOI] [PubMed] [Google Scholar]
- 26.Devinsky O.et al. (2017) Trial of cannabidiol for drug-resistant seizures in the Dravet syndrome. N. Engl. J. Med. 376, 2011–2020 10.1056/NEJMoa1611618 [DOI] [PubMed] [Google Scholar]
- 27.Sena L.A. and Chandel N.S. (2012) Physiological roles of mitochondrial reactive oxygen species. Mol. Cell 48, 158–167 10.1016/j.molcel.2012.09.025 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Zhou Z.et al. (2020) Dancing with reactive oxygen species generation and elimination in nanotheranostics for disease treatment. Adv. Drug Deliv. Rev. 158, 73–90 10.1016/j.addr.2020.06.006 [DOI] [PubMed] [Google Scholar]
- 29.Zorov D.B., Juhaszova M. and Sollott S.J. (2014) Mitochondrial reactive oxygen species (ROS) and ROS-induced ROS release. Physiol. Rev. 94, 909–950 10.1152/physrev.00026.2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.An X.et al. (2019) Increasing the TRPM2 channel expression in human neuroblastoma SH-SY5Y cells augments the susceptibility to ROS-induced cell death. Cells 8, 10.3390/cells8010028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hong S.W.et al. (2011) p34 (SEI-1) inhibits ROS-induced cell death through suppression of ASK1. Cancer Biol. Ther. 12, 421–426 10.4161/cbt.12.5.15972 [DOI] [PubMed] [Google Scholar]
- 32.Schumacker P.T. (2015) Reactive oxygen species in cancer: a dance with the devil. Cancer Cell 27, 156–157 10.1016/j.ccell.2015.01.007 [DOI] [PubMed] [Google Scholar]
- 33.Fan X.et al. (2021) Daphnetin triggers ROS-induced cell death and induces cytoprotective autophagy by modulating the AMPK/Akt/mTOR pathway in ovarian cancer. Phytomedicine 82, 153465 10.1016/j.phymed.2021.153465 [DOI] [PubMed] [Google Scholar]
- 34.Liang H.H.et al. (2018) Heat shock protein 27 influences the anti-cancer effect of curcumin in colon cancer cells through ROS production and autophagy activation. Life Sci. 209, 43–51 10.1016/j.lfs.2018.07.047 [DOI] [PubMed] [Google Scholar]
- 35.Zou P.et al. (2015) ROS generation mediates the anti-cancer effects of WZ35 via activating JNK and ER stress apoptotic pathways in gastric cancer. Oncotarget 6, 5860–5876 10.18632/oncotarget.3333 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Sareila O.et al. (2011) NOX2 complex-derived ROS as immune regulators. Antioxid. Redox Signal. 15, 2197–2208 10.1089/ars.2010.3635 [DOI] [PubMed] [Google Scholar]
- 37.Brandes R.P., Weissmann N. and Schroder K. (2014) Nox family NADPH oxidases: molecular mechanisms of activation. Free Radic. Biol. Med. 76, 208–226 10.1016/j.freeradbiomed.2014.07.046 [DOI] [PubMed] [Google Scholar]
- 38.Quinlan C.L.et al. (2012) Native rates of superoxide production from multiple sites in isolated mitochondria measured using endogenous reporters. Free Radic. Biol. Med. 53, 1807–1817 10.1016/j.freeradbiomed.2012.08.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Vergeade A.et al. (2012) Xanthine oxidase contributes to mitochondrial ROS generation in an experimental model of cocaine-induced diastolic dysfunction. J. Cardiovasc. Pharmacol. 60, 538–543 10.1097/FJC.0b013e318271223c [DOI] [PubMed] [Google Scholar]
- 40.Espinosa-Diez C.et al. (2015) Antioxidant responses and cellular adjustments to oxidative stress. Redox Biol. 6, 183–197 10.1016/j.redox.2015.07.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Murphy M.P. (2009) How mitochondria produce reactive oxygen species. Biochem. J. 417, 1–13 10.1042/BJ20081386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sharpe M.A., Robb S.J. and Clark J.B. (2003) Nitric oxide and Fenton/Haber-Weiss chemistry: nitric oxide is a potent antioxidant at physiological concentrations. J. Neurochem. 87, 386–394 10.1046/j.1471-4159.2003.02001.x [DOI] [PubMed] [Google Scholar]
- 43.Radi R. (2018) Oxygen radicals, nitric oxide, and peroxynitrite: Redox pathways in molecular medicine. Proc. Natl. Acad. Sci. U.S.A. 115, 5839–5848 10.1073/pnas.1804932115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Quinn M.T., Ammons M.C. and Deleo F.R. (2006) The expanding role of NADPH oxidases in health and disease: no longer just agents of death and destruction. Clin. Sci. (Lond.) 111, 1–20 10.1042/CS20060059 [DOI] [PubMed] [Google Scholar]
- 45.Bedard K. and Krause K.H. (2007) The NOX family of ROS-generating NADPH oxidases: physiology and pathophysiology. Physiol. Rev. 87, 245–313 10.1152/physrev.00044.2005 [DOI] [PubMed] [Google Scholar]
- 46.Paardekooper L.M.et al. (2019) Human monocyte-derived dendritic cells produce millimolar concentrations of ROS in phagosomes per second. Front. Immunol. 10, 1216 10.3389/fimmu.2019.01216 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Richards S.M. and Clark E.A. (2009) BCR-induced superoxide negatively regulates B-cell proliferation and T-cell-independent type 2 Ab responses. Eur. J. Immunol. 39, 3395–3403 10.1002/eji.200939587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Belikov A.V., Schraven B. and Simeoni L. (2015) T cells and reactive oxygen species. J. Biomed. Sci. 22, 85 10.1186/s12929-015-0194-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Krijnen P.A.et al. (2003) Increased Nox2 expression in human cardiomyocytes after acute myocardial infarction. J. Clin. Pathol. 56, 194–199 10.1136/jcp.56.3.194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Petry A.et al. (2006) NOX2 and NOX4 mediate proliferative response in endothelial cells. Antioxid. Redox Signal. 8, 1473–1484 10.1089/ars.2006.8.1473 [DOI] [PubMed] [Google Scholar]
- 51.Henriquez-Olguin C.et al. (2019) Cytosolic ROS production by NADPH oxidase 2 regulates muscle glucose uptake during exercise. Nat. Commun. 10, 4623 10.1038/s41467-019-12523-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Grauers Wiktorin H.et al. (2020) NOX2-derived reactive oxygen species in cancer. Oxid. Med. Cell Longev. 2020, 7095902 10.1155/2020/7095902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Panday A.et al. (2015) NADPH oxidases: an overview from structure to innate immunity-associated pathologies. Cell Mol. Immunol. 12, 5–23 10.1038/cmi.2014.89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Rastogi R.et al. (2016) NOX activation by subunit interaction and underlying mechanisms in disease. Front. Cell Neurosci. 10, 301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Judkins C.P.et al. (2010) Direct evidence of a role for Nox2 in superoxide production, reduced nitric oxide bioavailability, and early atherosclerotic plaque formation in ApoE-/- mice. Am. J. Physiol. Heart Circ. Physiol. 298, H24–H32 10.1152/ajpheart.00799.2009 [DOI] [PubMed] [Google Scholar]
- 56.Giardino G.et al. (2017) NADPH oxidase deficiency: a multisystem approach. Oxid. Med. Cell Longev. 2017, 4590127 10.1155/2017/4590127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Hunyadi A. (2019) The mechanism(s) of action of antioxidants: From scavenging reactive oxygen/nitrogen species to redox signaling and the generation of bioactive secondary metabolites. Med. Res. Rev. 39, 2505–2533 10.1002/med.21592 [DOI] [PubMed] [Google Scholar]
- 58.Beyrath J.et al. (2018) KH176 Safeguards Mitochondrial Diseased Cells from Redox Stress-Induced Cell Death by Interacting with the Thioredoxin System/Peroxiredoxin Enzyme Machinery. Sci. Rep. 8, 6577 10.1038/s41598-018-24900-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lubos E., Loscalzo J. and Handy D.E. (2011) Glutathione peroxidase-1 in health and disease: from molecular mechanisms to therapeutic opportunities. Antioxid. Redox Signal. 15, 1957–1997 10.1089/ars.2010.3586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lian G.et al. (2018) Glutathione de novo synthesis but not recycling process coordinates with glutamine catabolism to control redox homeostasis and directs murine T cell differentiation. Elife 7, 1–28 10.7554/eLife.36158 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Niki E. (2014) Role of vitamin E as a lipid-soluble peroxyl radical scavenger: in vitro and in vivo evidence. Free Radic. Biol. Med. 66, 3–12 10.1016/j.freeradbiomed.2013.03.022 [DOI] [PubMed] [Google Scholar]
- 62.Carcamo J.M.et al. (2004) Vitamin C is a kinase inhibitor: dehydroascorbic acid inhibits IkappaBalpha kinase beta. Mol. Cell. Biol. 24, 6645–6652 10.1128/MCB.24.15.6645-6652.2004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Vomund S.et al. (2017) Nrf2, the master regulator of anti-oxidative responses. Int. J. Mol. Sci. 18, 10.3390/ijms18122772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.He X. and Ma Q. (2009) NRF2 cysteine residues are critical for oxidant/electrophile-sensing, Kelch-like ECH-associated protein-1-dependent ubiquitination-proteasomal degradation, and transcription activation. Mol. Pharmacol. 76, 1265–1278 10.1124/mol.109.058453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Dong J., Sulik K.K. and Chen S.Y. (2008) Nrf2-mediated transcriptional induction of antioxidant response in mouse embryos exposed to ethanol in vivo: implications for the prevention of fetal alcohol spectrum disorders. Antioxid. Redox Signal. 10, 2023–2033 10.1089/ars.2007.2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Furue M.et al. (2017) Antioxidants for healthy skin: the emerging role of aryl hydrocarbon receptors and nuclear factor-erythroid 2-related factor-2. Nutrients 9, 10.3390/nu9030223 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Hashimoto-Hachiya A., Tsuji G. and Furue M. (2019) Antioxidants cinnamaldehyde and Galactomyces fermentation filtrate downregulate senescence marker CDKN2A/p16INK4A via NRF2 activation in keratinocytes. J. Dermatol. Sci. 96, 53–56 10.1016/j.jdermsci.2019.09.002 [DOI] [PubMed] [Google Scholar]
- 68.Cheung K.L.et al. (2014) Nrf2 knockout enhances intestinal tumorigenesis in Apc(min/+) mice due to attenuation of anti-oxidative stress pathway while potentiates inflammation. Mol. Carcinog. 53, 77–84 10.1002/mc.21950 [DOI] [PubMed] [Google Scholar]
- 69.Gozzelino R., Jeney V. and Soares M.P. (2010) Mechanisms of cell protection by heme oxygenase-1. Annu. Rev. Pharmacol. Toxicol. 50, 323–354 10.1146/annurev.pharmtox.010909.105600 [DOI] [PubMed] [Google Scholar]
- 70.Keyse S.M. and Tyrrell R.M. (1989) Heme oxygenase is the major 32-kDa stress protein induced in human skin fibroblasts by UVA radiation, hydrogen peroxide, and sodium arsenite. Proc. Natl. Acad. Sci. U.S.A. 86, 99–103 10.1073/pnas.86.1.99 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Seiwert N.et al. (2020) Heme oxygenase 1 protects human colonocytes against ROS formation, oxidative DNA damage and cytotoxicity induced by heme iron, but not inorganic iron. Cell Death Dis. 11, 787 10.1038/s41419-020-02950-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Zhang F.H.et al. (2017) Protective effects of heme oxygenase-1 against severe acute pancreatitis via inhibition of tumor necrosis factor-alpha and augmentation of interleukin-10. BMC Gastroenterol. 17, 100 10.1186/s12876-017-0651-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Campbell N.K., Fitzgerald H.K. and Dunne A. (2021) Regulation of inflammation by the antioxidant haem oxygenase 1. Nat. Rev. Immunol. 21, 411–425 10.1038/s41577-020-00491-x [DOI] [PubMed] [Google Scholar]
- 74.Egea J.et al. (2017) European contribution to the study of ROS: a summary of the findings and prospects for the future from the COST action BM1203 (EU-ROS). Redox Biol. 13, 94–162 10.1016/j.redox.2017.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Ohlow M.J.et al. (2017) Why have clinical trials of antioxidants to prevent neurodegeneration failed? - a cellular investigation of novel phenothiazine-type antioxidants reveals competing objectives for pharmaceutical neuroprotection Pharm. Res. 34, 378–393 10.1007/s11095-016-2068-0 [DOI] [PubMed] [Google Scholar]
- 76.Thal L.J.et al. (2003) Idebenone treatment fails to slow cognitive decline in Alzheimer’s disease. Neurology 61, 1498–1502 10.1212/01.WNL.0000096376.03678.C1 [DOI] [PubMed] [Google Scholar]
- 77.Sakellariou G.K.et al. (2016) Long-term administration of the mitochondria-targeted antioxidant mitoquinone mesylate fails to attenuate age-related oxidative damage or rescue the loss of muscle mass and function associated with aging of skeletal muscle. FASEB J. 30, 3771–3785 10.1096/fj.201600450R [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Fiebiger S.M.et al. (2013) The antioxidant idebenone fails to prevent or attenuate chronic experimental autoimmune encephalomyelitis in the mouse. J. Neuroimmunol. 262, 66–71 10.1016/j.jneuroim.2013.07.002 [DOI] [PubMed] [Google Scholar]
- 79.Pemp B., Kircher K. and Reitner A. (2019) Visual function in chronic Leber’s hereditary optic neuropathy during idebenone treatment initiated 5 to 50 years after onset. Graefes Arch. Clin. Exp. Ophthalmol. 257, 2751–2757 10.1007/s00417-019-04444-6 [DOI] [PubMed] [Google Scholar]
- 80.Carvalho A.M.S.et al. (2020) Phytol, a chlorophyll component, produces antihyperalgesic, anti-inflammatory, and antiarthritic effects: possible NFkappaB pathway involvement and reduced levels of the proinflammatory cytokines TNF-alpha and IL-6. J. Nat. Prod. 83, 1107–1117 10.1021/acs.jnatprod.9b01116 [DOI] [PubMed] [Google Scholar]
- 81.Joshi G.N., Goetjen A.M. and Knecht D.A. (2015) Silica particles cause NADPH oxidase-independent ROS generation and transient phagolysosomal leakage. Mol. Biol. Cell 26, 3150–3164 10.1091/mbc.e15-03-0126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Martinon F. (2010) Signaling by ROS drives inflammasome activation. Eur. J. Immunol. 40, 616–619 10.1002/eji.200940168 [DOI] [PubMed] [Google Scholar]
- 83.Minutoli L.et al. (2016) ROS-mediated NLRP3 inflammasome activation in brain, heart, kidney, and testis ischemia/reperfusion injury. Oxid. Med. Cell Longev. 2016, 2183026 10.1155/2016/2183026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Rathinam V.A. and Fitzgerald K.A. (2016) Inflammasome complexes: emerging mechanisms and effector functions. Cell 165, 792–800 10.1016/j.cell.2016.03.046 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.He Y., Hara H. and Nunez G. (2016) Mechanism and regulation of NLRP3 inflammasome activation. Trends Biochem. Sci 41, 1012–1021 10.1016/j.tibs.2016.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Esplugues J.V. (2002) NO as a signalling molecule in the nervous system. Br. J. Pharmacol. 135, 1079–1095 10.1038/sj.bjp.0704569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Nakazawa H.et al. (2017) iNOS as a driver of inflammation and apoptosis in mouse skeletal muscle after burn injury: possible involvement of Sirt1 S-nitrosylation-mediated acetylation of p65 NF-kappaB and p53. PLoS ONE 12, e0170391 10.1371/journal.pone.0170391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Bienert G.P., Schjoerring J.K. and Jahn T.P. (2006) Membrane transport of hydrogen peroxide. Biochim. Biophys. Acta 1758, 994–1003 10.1016/j.bbamem.2006.02.015 [DOI] [PubMed] [Google Scholar]
- 89.De Grey A.D. (2002) HO2*: the forgotten radical. DNA Cell Biol. 21, 251–257 10.1089/104454902753759672 [DOI] [PubMed] [Google Scholar]
- 90.Bogaert Y.E., Rosenthal R.E. and Fiskum G. (1994) Postischemic inhibition of cerebral cortex pyruvate dehydrogenase. Free Radic. Biol. Med. 16, 811–820 10.1016/0891-5849(94)90197-X [DOI] [PubMed] [Google Scholar]
- 91.Grisham M.B.et al. (1987) Interaction between oxygen radicals and gastric mucin. Am. J. Physiol. 253, G93–G96 10.1152/ajpgi.1987.253.1.G93 [DOI] [PubMed] [Google Scholar]
- 92.Xu D.et al. (2019) Mechanism of unprecedented hydroxyl radical production and site-specific oxidative DNA damage by photoactivation of the classic arylhydroxamic acid carcinogens. Carcinogenesis 40(9), 1153–1163 10.1093/carcin/bgz021 [DOI] [PubMed] [Google Scholar]
- 93.Aikens J. and Dix T.A. (1991) Perhydroxyl radical (HOO.) initiated lipid peroxidation. The role of fatty acid hydroperoxides. J. Biol. Chem. 266, 15091–15098 10.1016/S0021-9258(18)98591-1 [DOI] [PubMed] [Google Scholar]
- 94.Landi L.et al. (1995) Injury of rat thymocytes caused by exogenous peroxyl radicals in vitro. Biochim. Biophys. Acta 1239, 207–212 10.1016/0005-2736(95)00158-Y [DOI] [PubMed] [Google Scholar]
- 95.Chiste R.C.et al. (2014) Carotenoids are effective inhibitors of in vitro hemolysis of human erythrocytes, as determined by a practical and optimized cellular antioxidant assay. J. Food Sci. 79, H1841–H1847 10.1111/1750-3841.12580 [DOI] [PubMed] [Google Scholar]
- 96.Pereira C.et al. (2015) Oxidative stress and DNA damage: implications in inflammatory bowel disease. Inflamm. Bowel Dis. 21, 2403–2417 [DOI] [PubMed] [Google Scholar]
- 97.Zias J.et al. (1993) Early medical use of cannabis. Nature 363, 215 10.1038/363215a0 [DOI] [PubMed] [Google Scholar]
- 98.Radhakrishnan R., Wilkinson S.T. and D'Souza D.C. (2014) Gone to Pot - a review of the association between Cannabis and Psychosis. Front. Psychiatry 5, 54 10.3389/fpsyt.2014.00054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Fitzpatrick J.K. and Downer E.J. (2017) Toll-like receptor signalling as a cannabinoid target in multiple sclerosis. Neuropharmacology 113, 618–626 10.1016/j.neuropharm.2016.04.009 [DOI] [PubMed] [Google Scholar]
- 100.Pereira S.R.et al. (2020) Recent advances in the understanding of the aetiology and therapeutic strategies in burning mouth syndrome: focus on the actions of cannabinoids. Eur. J. Neurosci. 10.1111/ejn.14712 [DOI] [PubMed] [Google Scholar]
- 101.Bonini S.A.et al. (2018) Cannabis sativa: A comprehensive ethnopharmacological review of a medicinal plant with a long history. J. Ethnopharmacol. 227, 300–315 10.1016/j.jep.2018.09.004 [DOI] [PubMed] [Google Scholar]
- 102.Joshi N. and Onaivi E.S. (2019) Endocannabinoid system components: overview and tissue distribution. Adv. Exp. Med. Biol. 1162, 1–12 10.1007/978-3-030-21737-2_1 [DOI] [PubMed] [Google Scholar]
- 103.Di Marzo V. (2009) The endocannabinoid system: its general strategy of action, tools for its pharmacological manipulation and potential therapeutic exploitation. Pharmacol. Res. 60, 77–84 10.1016/j.phrs.2009.02.010 [DOI] [PubMed] [Google Scholar]
- 104.Shahbazi F.et al. (2020) Cannabinoids and cannabinoid receptors: the story so far. iScience 23, 101301 10.1016/j.isci.2020.101301 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Sirikantaramas S.et al. (2005) Tetrahydrocannabinolic acid synthase, the enzyme controlling marijuana psychoactivity, is secreted into the storage cavity of the glandular trichomes. Plant Cell Physiol. 46, 1578–1582 10.1093/pcp/pci166 [DOI] [PubMed] [Google Scholar]
- 106.Downer E.J. (2020) Anti-inflammatory potential of terpenes present in Cannabis sativa L. ACS Chem. Neurosci. 11, 659–662 10.1021/acschemneuro.0c00075 [DOI] [PubMed] [Google Scholar]
- 107.Russo E.B. (2011) Taming THC: potential cannabis synergy and phytocannabinoid-terpenoid entourage effects. Br. J. Pharmacol. 163, 1344–1364 10.1111/j.1476-5381.2011.01238.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.de Boer J.G., Posthumus M.A. and Dicke M. (2004) Identification of volatiles that are used in discrimination between plants infested with prey or nonprey herbivores by a predatory mite. J. Chem. Ecol. 30, 2215–2230 10.1023/B:JOEC.0000048784.79031.5e [DOI] [PubMed] [Google Scholar]
- 109.Happyana N.et al. (2013) Analysis of cannabinoids in laser-microdissected trichomes of medicinal Cannabis sativa using LCMS and cryogenic NMR. Phytochemistry 87, 51–59 10.1016/j.phytochem.2012.11.001 [DOI] [PubMed] [Google Scholar]
- 110.Taura F.et al. (2007) Phytocannabinoids in Cannabis sativa: recent studies on biosynthetic enzymes. Chem. Biodivers. 4, 1649–1663 10.1002/cbdv.200790145 [DOI] [PubMed] [Google Scholar]
- 111.Chandra S.et al. (2017) Cannabis cultivation: methodological issues for obtaining medical-grade product. Epilepsy Behav. 70, 302–312 10.1016/j.yebeh.2016.11.029 [DOI] [PubMed] [Google Scholar]
- 112.Galiegue S.et al. (1995) Expression of central and peripheral cannabinoid receptors in human immune tissues and leukocyte subpopulations. Eur. J. Biochem. 232, 54–61 10.1111/j.1432-1033.1995.tb20780.x [DOI] [PubMed] [Google Scholar]
- 113.Busquets-Garcia A., Bains J. and Marsicano G. (2018) CB(1) receptor signaling in the brain: extracting specificity from ubiquity. Neuropsychopharmacology 43, 4–20 10.1038/npp.2017.206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Van Sickle M.D.et al. (2005) Identification and functional characterization of brainstem cannabinoid CB2 receptors. Science 310, 329–332 10.1126/science.1115740 [DOI] [PubMed] [Google Scholar]
- 115.Stempel A.V.et al. (2016) Cannabinoid type 2 receptors mediate a cell type-specific plasticity in the hippocampus. Neuron 90, 795–809 10.1016/j.neuron.2016.03.034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Ashton J.C.et al. (2007) Cerebral hypoxia-ischemia and middle cerebral artery occlusion induce expression of the cannabinoid CB2 receptor in the brain. Neurosci. Lett. 412, 114–117 10.1016/j.neulet.2006.10.053 [DOI] [PubMed] [Google Scholar]
- 117.Pertwee R.G. (2008) The diverse CB1 and CB2 receptor pharmacology of three plant cannabinoids: delta9-tetrahydrocannabinol, cannabidiol and delta9-tetrahydrocannabivarin. Br. J. Pharmacol. 153, 199–215 10.1038/sj.bjp.0707442 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ibeas Bih C.et al. (2015) Molecular targets of cannabidiol in neurological disorders. Neurotherapeutics 12, 699–730 10.1007/s13311-015-0377-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Devane W.A.et al. (1992) Isolation and structure of a brain constituent that binds to the cannabinoid receptor. Science 258, 1946–1949 10.1126/science.1470919 [DOI] [PubMed] [Google Scholar]
- 120.Mechoulam R.et al. (1995) Identification of an endogenous 2-monoglyceride, present in canine gut, that binds to cannabinoid receptors. Biochem. Pharmacol. 50, 83–90 10.1016/0006-2952(95)00109-D [DOI] [PubMed] [Google Scholar]
- 121.Sugiura T.et al. (1995) 2-Arachidonoylglycerol: a possible endogenous cannabinoid receptor ligand in brain. Biochem. Biophys. Res. Commun. 215, 89–97 10.1006/bbrc.1995.2437 [DOI] [PubMed] [Google Scholar]
- 122.Bedse G., Hill M.N. and Patel S. (2020) 2-arachidonoylglycerol modulation of anxiety and stress adaptation: from grass roots to novel therapeutics. Biol. Psych. 88, 520–530 10.1016/j.biopsych.2020.01.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Alger B.E. (2012) Endocannabinoids at the synapse a decade after the dies mirabilis (29 March 2001): what we still do not know. J. Physiol. 590, 2203–2212 10.1113/jphysiol.2011.220855 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Kano M.et al. (2009) Endocannabinoid-mediated control of synaptic transmission. Physiol. Rev. 89, 309–380 10.1152/physrev.00019.2008 [DOI] [PubMed] [Google Scholar]
- 125.Castillo P.E.et al. (2012) Endocannabinoid signaling and synaptic function. Neuron 76, 70–81 10.1016/j.neuron.2012.09.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Katona I. and Freund T.F. (2008) Endocannabinoid signaling as a synaptic circuit breaker in neurological disease. Nat. Med. 14, 923–930 10.1038/nm.f.1869 [DOI] [PubMed] [Google Scholar]
- 127.Stella N., Schweitzer P. and Piomelli D. (1997) A second endogenous cannabinoid that modulates long-term potentiation. Nature 388, 773–778 10.1038/42015 [DOI] [PubMed] [Google Scholar]
- 128.Karwad M.A.et al. (2017) Oleoylethanolamine and palmitoylethanolamine modulate intestinal permeability in vitro via TRPV1 and PPARalpha. FASEB J. 31, 469–481 10.1096/fj.201500132 [DOI] [PubMed] [Google Scholar]
- 129.Okine B.N.et al. (2016) N-palmitoylethanolamide in the anterior cingulate cortex attenuates inflammatory pain behaviour indirectly via a CB1 receptor-mediated mechanism. Pain 157, 2687–2696 10.1097/j.pain.0000000000000687 [DOI] [PubMed] [Google Scholar]
- 130.Vaia M.et al. (2016) Palmitoylethanolamide reduces inflammation and itch in a mouse model of contact allergic dermatitis. Eur. J. Pharmacol. 791, 669–674 10.1016/j.ejphar.2016.10.005 [DOI] [PubMed] [Google Scholar]
- 131.Kaplan J.S.et al. (2017) Cannabidiol attenuates seizures and social deficits in a mouse model of Dravet syndrome. Proc. Natl. Acad. Sci. U.S.A. 114, 11229–11234 10.1073/pnas.1711351114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Cruz S.L.et al. (2018) Anandamide inhibits FcepsilonRI-dependent degranulation and cytokine synthesis in mast cells through CB2 and GPR55 receptor activation. Possible involvement of CB2-GPR55 heteromers. Int. Immunopharmacol. 64, 298–307 10.1016/j.intimp.2018.09.006 [DOI] [PubMed] [Google Scholar]
- 133.Kolbe M.R.et al. (2021) THC reduces ki67-immunoreactive cells derived from human primary glioblastoma in a GPR55-dependent manner. Cancers (Basel) 13, 10.3390/cancers13051064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Sawzdargo M.et al. (1999) Identification and cloning of three novel human G protein-coupled receptor genes GPR52, PsiGPR53 and GPR55: GPR55 is extensively expressed in human brain. Brain Res. Mol. Brain Res. 64, 193–198 10.1016/S0169-328X(98)00277-0 [DOI] [PubMed] [Google Scholar]
- 135.Kramar C.et al. (2017) Palmitoylethanolamide modulates GPR55 receptor signaling in the ventral hippocampus to regulate mesolimbic dopamine activity, social interaction, and memory processing. Cannabis Cannabinoid Res. 2, 8–20 10.1089/can.2016.0030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Petrosino S.et al. (2016) The anti-inflammatory mediator palmitoylethanolamide enhances the levels of 2-arachidonoyl-glycerol and potentiates its actions at TRPV1 cation channels. Br. J. Pharmacol. 173, 1154–1162 10.1111/bph.13084 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Fonseca B.M., Correia-da-Silva G. and Teixeira N.A. (2018) Cannabinoid-induced cell death in endometrial cancer cells: involvement of TRPV1 receptors in apoptosis. J. Physiol. Biochem. 74, 261–272 10.1007/s13105-018-0611-7 [DOI] [PubMed] [Google Scholar]
- 138.Starkus J.et al. (2019) Diverse TRPV1 responses to cannabinoids. Channels (Austin) 13, 172–191 10.1080/19336950.2019.1619436 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Ramer R.et al. (2013) COX-2 and PPAR-gamma confer cannabidiol-induced apoptosis of human lung cancer cells. Mol. Cancer Ther. 12, 69–82 10.1158/1535-7163.MCT-12-0335 [DOI] [PubMed] [Google Scholar]
- 140.Scuderi C., Steardo L. and Esposito G. (2014) Cannabidiol promotes amyloid precursor protein ubiquitination and reduction of beta amyloid expression in SHSY5YAPP+ cells through PPARgamma involvement. Phytother. Res. 28, 1007–1013 10.1002/ptr.5095 [DOI] [PubMed] [Google Scholar]
- 141.Lo Verme J.et al. (2005) The nuclear receptor peroxisome proliferator-activated receptor-alpha mediates the anti-inflammatory actions of palmitoylethanolamide. Mol. Pharmacol. 67, 15–19 10.1124/mol.104.006353 [DOI] [PubMed] [Google Scholar]
- 142.Fu J.et al. (2003) Oleylethanolamide regulates feeding and body weight through activation of the nuclear receptor PPAR-alpha. Nature 425, 90–93 10.1038/nature01921 [DOI] [PubMed] [Google Scholar]
- 143.LoVerme J.et al. (2005) The search for the palmitoylethanolamide receptor. Life Sci. 77, 1685–1698 10.1016/j.lfs.2005.05.012 [DOI] [PubMed] [Google Scholar]
- 144.Alharris E.et al. (2019) Role of miRNA in the regulation of cannabidiol-mediated apoptosis in neuroblastoma cells. Oncotarget 10, 45–59 10.18632/oncotarget.26534 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Ledgerwood C.J.et al. (2011) Cannabidiol inhibits synaptic transmission in rat hippocampal cultures and slices via multiple receptor pathways. Br. J. Pharmacol. 162, 286–294 10.1111/j.1476-5381.2010.01015.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Kathmann M.et al. (2006) Cannabidiol is an allosteric modulator at mu- and delta-opioid receptors. Naunyn Schmiedebergs Arch. Pharmacol. 372, 354–361 10.1007/s00210-006-0033-x [DOI] [PubMed] [Google Scholar]
- 147.Chung E.Y.et al. (2021) Pharmacology and adverse effects of new psychoactive substances: synthetic cannabinoid receptor agonists. Arch. Pharm. Res. 44, 402–413 10.1007/s12272-021-01326-6 [DOI] [PubMed] [Google Scholar]
- 148.Showalter V.M.et al. (1996) Evaluation of binding in a transfected cell line expressing a peripheral cannabinoid receptor (CB2): identification of cannabinoid receptor subtype selective ligands. J. Pharmacol. Exp. Ther. 278, 989–999 [PubMed] [Google Scholar]
- 149.Felder C.C.et al. (1995) Comparison of the pharmacology and signal transduction of the human cannabinoid CB1 and CB2 receptors. Mol. Pharmacol. 48, 443–450 [PubMed] [Google Scholar]
- 150.Meng I.D.et al. (1998) An analgesia circuit activated by cannabinoids. Nature 395, 381–383 10.1038/26481 [DOI] [PubMed] [Google Scholar]
- 151.Ulugol A.et al. (2004) The effect of WIN 55,212-2, a cannabinoid agonist, on tactile allodynia in diabetic rats. Neurosci. Lett. 371, 167–170 10.1016/j.neulet.2004.08.061 [DOI] [PubMed] [Google Scholar]
- 152.Porcella A.et al. (2001) The synthetic cannabinoid WIN55212-2 decreases the intraocular pressure in human glaucoma resistant to conventional therapies. Eur. J. Neurosci. 13, 409–412 10.1046/j.0953-816X.2000.01401.x [DOI] [PubMed] [Google Scholar]
- 153.Slipetz D.M.et al. (1995) Activation of the human peripheral cannabinoid receptor results in inhibition of adenylyl cyclase. Mol. Pharmacol. 48, 352–361 [PubMed] [Google Scholar]
- 154.Howlett A.C.et al. (1990) Stereochemical effects of 11-OH-delta 8-tetrahydrocannabinol-dimethylheptyl to inhibit adenylate cyclase and bind to the cannabinoid receptor. Neuropharmacology 29, 161–165 10.1016/0028-3908(90)90056-W [DOI] [PubMed] [Google Scholar]
- 155.Lin S.et al. (2017) The Anti-Inflammatory Effect and Intestinal Barrier Protection of HU210 Differentially Depend on TLR4 Signaling in Dextran Sulfate Sodium-Induced Murine Colitis. Dig. Dis. Sci. 62, 372–386 10.1007/s10620-016-4404-y [DOI] [PubMed] [Google Scholar]
- 156.Lax P.et al. (2014) Neuroprotective effects of the cannabinoid agonist HU210 on retinal degeneration. Exp. Eye Res. 120, 175–185 10.1016/j.exer.2014.01.019 [DOI] [PubMed] [Google Scholar]
- 157.Wiley J.L.et al. (1995) Discriminative stimulus effects of CP 55,940 and structurally dissimilar cannabinoids in rats. Neuropharmacology 34, 669–676 10.1016/0028-3908(95)00027-4 [DOI] [PubMed] [Google Scholar]
- 158.Griffin G.et al. (1998) Evaluation of cannabinoid receptor agonists and antagonists using the guanosine-5'-O-(3-[35S]thio)-triphosphate binding assay in rat cerebellar membranes. J. Pharmacol. Exp. Ther. 285, 553–560 [PubMed] [Google Scholar]
- 159.Hamamoto D.T., Giridharagopalan S. and Simone D.A. (2007) Acute and chronic administration of the cannabinoid receptor agonist CP 55,940 attenuates tumor-evoked hyperalgesia. Eur. J. Pharmacol. 558, 73–87 10.1016/j.ejphar.2006.11.062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 160.Kraft B., Wintersberger W. and Kress H.G. (2004) Cannabinoid receptor-independent suppression of the superoxide generation of human neutrophils (PMN) by CP55 940, but not by anandamide. Life Sci. 75, 969–977 10.1016/j.lfs.2004.02.007 [DOI] [PubMed] [Google Scholar]
- 161.Correa F.et al. (2005) Activation of cannabinoid CB2 receptor negatively regulates IL-12p40 production in murine macrophages: role of IL-10 and ERK1/2 kinase signaling. Br. J. Pharmacol. 145, 441–448 10.1038/sj.bjp.0706215 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Baker D.et al. (2000) Cannabinoids control spasticity and tremor in a multiple sclerosis model. Nature 404, 84–87 10.1038/35003583 [DOI] [PubMed] [Google Scholar]
- 163.Ramirez B.G.et al. (2005) Prevention of Alzheimer's disease pathology by cannabinoids: neuroprotection mediated by blockade of microglial activation. J. Neurosci. 25, 1904–1913 10.1523/JNEUROSCI.4540-04.2005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Hillard C.J.et al. (1999) Synthesis and characterization of potent and selective agonists of the neuronal cannabinoid receptor (CB1). J. Pharmacol. Exp. Ther. 289, 1427–1433 [PubMed] [Google Scholar]
- 165.Yang S.et al. (2020) Cannabinoid CB1 receptor agonist ACEA alleviates brain ischemia/reperfusion injury via CB1-Drp1 pathway. Cell Death Discov. 6, 102 10.1038/s41420-020-00338-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Chiu P.et al. (1975) The influence of delta9-tetrahydrocannabinol, cannabinol and cannabidiol on tissue oxygen consumption. Res. Commun. Chem. Pathol. Pharmacol. 12, 267–286 [PubMed] [Google Scholar]
- 167.Costa B.et al. (2007) The non-psychoactive cannabis constituent cannabidiol is an orally effective therapeutic agent in rat chronic inflammatory and neuropathic pain. Eur. J. Pharmacol. 556, 75–83 10.1016/j.ejphar.2006.11.006 [DOI] [PubMed] [Google Scholar]
- 168.Mabou Tagne A.et al. (2019) A novel standardized Cannabis sativa L. extract and its constituent cannabidiol inhibit human polymorphonuclear leukocyte functions. Int. J. Mol. Sci. 20(8), 1833 10.3390/ijms20081833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Chen J.et al. (2016) Protective effect of cannabidiol on hydrogen peroxideinduced apoptosis, inflammation and oxidative stress in nucleus pulposus cells. Mol. Med. Rep. 14, 2321–2327 10.3892/mmr.2016.5513 [DOI] [PubMed] [Google Scholar]
- 170.Baeeri M.et al. (2020) Cannabinoids as anti-ROS in aged pancreatic islet cells. Life Sci. 256, 117969 10.1016/j.lfs.2020.117969 [DOI] [PubMed] [Google Scholar]
- 171.Barichello T.et al. (2012) Cannabidiol reduces host immune response and prevents cognitive impairments in Wistar rats submitted to pneumococcal meningitis. Eur. J. Pharmacol. 697, 158–164 10.1016/j.ejphar.2012.09.053 [DOI] [PubMed] [Google Scholar]
- 172.Frankola K.A.et al. (2011) Targeting TNF-alpha to elucidate and ameliorate neuroinflammation in neurodegenerative diseases. CNS Neurol. Disord. Drug Targets 10, 391–403 10.2174/187152711794653751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.McCoy M.K.et al. (2011) TNF: a key neuroinflammatory mediator of neurotoxicity and neurodegeneration in models of Parkinson's disease. Adv. Exp. Med. Biol. 691, 539–540 10.1007/978-1-4419-6612-4_56 [DOI] [PubMed] [Google Scholar]
- 174.Guarnieri G.et al. (2020) Tumor necrosis factor alpha influences phenotypic plasticity and promotes epigenetic changes in human basal forebrain cholinergic neuroblasts. Int. J. Mol. Sci. 21(17), 6128 10.3390/ijms21176128 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Nichols J.M. and Kaplan B.L.F. (2020) Immune responses regulated by cannabidiol. Cannabis Cannabinoid Res. 5, 12–31 10.1089/can.2018.0073 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Branca J.J.V.et al. (2019) Cannabidiol protects dopaminergic neuronal cells from cadmium. Int. J. Environ. Res. Public Health 16, 10.3390/ijerph16224420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Hampson A.J.et al. (1998) Cannabidiol and (-)Delta9-tetrahydrocannabinol are neuroprotective antioxidants. Proc. Natl. Acad. Sci. U.S.A. 95, 8268–8273 10.1073/pnas.95.14.8268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Consroe P.et al. (1991) Controlled clinical trial of cannabidiol in Huntington’s disease. Pharmacol. Biochem. Behav. 40, 701–708 10.1016/0091-3057(91)90386-G [DOI] [PubMed] [Google Scholar]
- 179.Leweke F.M.et al. (2012) Cannabidiol enhances anandamide signaling and alleviates psychotic symptoms of schizophrenia. Transl. Psychiatry 2, e94 10.1038/tp.2012.15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Juknat A.et al. (2013) Microarray and pathway analysis reveal distinct mechanisms underlying cannabinoid-mediated modulation of LPS-induced activation of BV-2 microglial cells. PLoS ONE 8, e61462 10.1371/journal.pone.0061462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Jastrzab A., Gegotek A. and Skrzydlewska E. (2019) Cannabidiol regulates the expression of keratinocyte proteins involved in the inflammation process through transcriptional regulation. Cells 8(8), 827 10.3390/cells8080827 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Bockmann S. and Hinz B. (2020) Cannabidiol promotes endothelial cell survival by heme oxygenase-1-mediated autophagy. Cells 9(7), 1703 10.3390/cells9071703 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Lu X.et al. (2021) Cannabidiol attenuates pulmonary arterial hypertension by improving vascular smooth muscle cells mitochondrial function. Theranostics 11, 5267–5278 10.7150/thno.55571 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Casares L.et al. (2020) Cannabidiol induces antioxidant pathways in keratinocytes by targeting BACH1. Redox Biol. 28, 101321 10.1016/j.redox.2019.101321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 185.Bublitz K.et al. (2020) Cannabinoid-induced autophagy and heme oxygenase-1 determine the fate of adipose tissue-derived mesenchymal stem cells under stressful conditions. Cells 9(10), 2298 10.3390/cells9102298 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Duvigneau J.C.et al. (2020) Cannabidiol protects dopaminergic neurons in mesencephalic cultures against the complex i inhibitor rotenone via modulation of heme oxygenase activity and bilirubin. Antioxidants (Basel) 9, 135 10.3390/antiox9020135 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Schwartz M., Bockmann S. and Hinz B. (2018) Up-regulation of heme oxygenase-1 expression and inhibition of disease-associated features by cannabidiol in vascular smooth muscle cells. Oncotarget 9, 34595–34616 10.18632/oncotarget.26191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Rajesh M.et al. (2010) Cannabidiol attenuates cardiac dysfunction, oxidative stress, fibrosis, and inflammatory and cell death signaling pathways in diabetic cardiomyopathy. J. Am. Coll. Cardiol. 56, 2115–2125 10.1016/j.jacc.2010.07.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.O'Sullivan S.E.et al. (2009) Time-dependent vascular actions of cannabidiol in the rat aorta. Eur. J. Pharmacol. 612, 61–68 10.1016/j.ejphar.2009.03.010 [DOI] [PubMed] [Google Scholar]
- 190.Sun S.et al. (2017) Cannabidiol attenuates OGD/R-induced damage by enhancing mitochondrial bioenergetics and modulating glucose metabolism via pentose-phosphate pathway in hippocampal neurons. Redox Biol. 11, 577–585 10.1016/j.redox.2016.12.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Fouad A.A.et al. (2013) Cardioprotective effect of cannabidiol in rats exposed to doxorubicin toxicity. Environ. Toxicol. Pharmacol. 36, 347–357 10.1016/j.etap.2013.04.018 [DOI] [PubMed] [Google Scholar]
- 192.Dos-Santos-Pereira M.et al. (2020) Cannabidiol prevents LPS-induced microglial inflammation by inhibiting ROS/NF-kappaB-dependent signaling and glucose consumption. Glia 68, 561–573 10.1002/glia.23738 [DOI] [PubMed] [Google Scholar]
- 193.Rajesh M.et al. (2007) Cannabidiol attenuates high glucose-induced endothelial cell inflammatory response and barrier disruption. Am. J. Physiol. Heart Circ. Physiol. 293, H610–H619 10.1152/ajpheart.00236.2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.El-Remessy A.B.et al. (2003) Neuroprotective effect of (-)Delta9-tetrahydrocannabinol and cannabidiol in N-methyl-D-aspartate-induced retinal neurotoxicity: involvement of peroxynitrite. Am. J. Pathol. 163, 1997–2008 10.1016/S0002-9440(10)63558-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Mecha M.et al. (2012) Cannabidiol protects oligodendrocyte progenitor cells from inflammation-induced apoptosis by attenuating endoplasmic reticulum stress. Cell Death Dis. 3, e331 10.1038/cddis.2012.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Liu C.et al. (2021) Cannabidiol protects human skin keratinocytes from hydrogen-peroxide-induced oxidative stress via modulation of the caspase-1-il-1beta axis. J. Nat. Prod. 84(5), 1563–1572 10.1021/acs.jnatprod.1c00083 [DOI] [PubMed] [Google Scholar]
- 197.Cocetta V.et al. (2021) Cannabidiol isolated from Cannabis sativa L. protects intestinal barrier from in vitro inflammation and oxidative stress. Front. Pharmacol. 12, 641210 10.3389/fphar.2021.641210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Iuvone T.et al. (2004) Neuroprotective effect of cannabidiol, a non-psychoactive component from Cannabis sativa, on beta-amyloid-induced toxicity in PC12 cells. J. Neurochem. 89, 134–141 10.1111/j.1471-4159.2003.02327.x [DOI] [PubMed] [Google Scholar]
- 199.Pan H.et al. (2009) Cannabidiol attenuates cisplatin-induced nephrotoxicity by decreasing oxidative/nitrosative stress, inflammation, and cell death. J. Pharmacol. Exp. Ther. 328, 708–714 10.1124/jpet.108.147181 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Borges R.S.et al. (2013) Understanding the molecular aspects of tetrahydrocannabinol and cannabidiol as antioxidants. Molecules 18, 12663–12674 10.3390/molecules181012663 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Hamelink C.et al. (2005) Comparison of cannabidiol, antioxidants, and diuretics in reversing binge ethanol-induced neurotoxicity. J. Pharmacol. Exp. Ther. 314, 780–788 10.1124/jpet.105.085779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Atalay S., Jarocka-Karpowicz I. and Skrzydlewska E. (2019) Antioxidative and anti-inflammatory properties of cannabidiol. Antioxidants (Basel) 9, 10.3390/antiox9010021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Panja D., Vedeler C.A. and Schubert M. (2019) Paraneoplastic cerebellar degeneration: Yo antibody alters mitochondrial calcium buffering capacity. Neuropathol. Appl. Neurobiol. 45, 141–156 10.1111/nan.12492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Atalay S.et al. (2020) Cannabidiol protects keratinocyte cell membranes following exposure to UVB and hydrogen peroxide. Redox Biol. 36, 101613 10.1016/j.redox.2020.101613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 205.Wang Y.et al. (2017) Cannabidiol attenuates alcohol-induced liver steatosis, metabolic dysregulation, inflammation and neutrophil-mediated injury. Sci. Rep. 7, 12064 10.1038/s41598-017-10924-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 206.Wu H.Y.et al. (2018) Cannabidiol induced apoptosis in human monocytes through mitochondrial permeability transition pore-mediated ROS production. Free Radic. Biol. Med. 124, 311–318 10.1016/j.freeradbiomed.2018.06.023 [DOI] [PubMed] [Google Scholar]
- 207.Schultze N.et al. (2017) Mitochondrial functions of THP-1 monocytes following the exposure to selected natural compounds. Toxicology 377, 57–63 10.1016/j.tox.2016.12.006 [DOI] [PubMed] [Google Scholar]
- 208.McKallip R.J.et al. (2006) Cannabidiol-induced apoptosis in human leukemia cells: a novel role of cannabidiol in the regulation of p22phox and Nox4 expression. Mol. Pharmacol. 70, 897–908 10.1124/mol.106.023937 [DOI] [PubMed] [Google Scholar]
- 209.Wu H.Y.et al. (2008) Cannabidiol-induced apoptosis in primary lymphocytes is associated with oxidative stress-dependent activation of caspase-8. Toxicol. Appl. Pharmacol. 226, 260–270 10.1016/j.taap.2007.09.012 [DOI] [PubMed] [Google Scholar]
- 210.Gonzalez-Garcia C.et al. (2017) Mechanisms of action of cannabidiol in adoptively transferred experimental autoimmune encephalomyelitis. Exp. Neurol. 298, 57–67 10.1016/j.expneurol.2017.08.017 [DOI] [PubMed] [Google Scholar]
- 211.Lee C.Y.et al. (2008) A comparative study on cannabidiol-induced apoptosis in murine thymocytes and EL-4 thymoma cells. Int. Immunopharmacol. 8, 732–740 10.1016/j.intimp.2008.01.018 [DOI] [PubMed] [Google Scholar]
- 212.Muthumalage T. and Rahman I. (2019) Cannabidiol differentially regulates basal and LPS-induced inflammatory responses in macrophages, lung epithelial cells, and fibroblasts. Toxicol. Appl. Pharmacol. 382, 114713 10.1016/j.taap.2019.114713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 213.de la Harpe A., Beukes N. and Frost C.L. (2021) CBD activation of TRPV1 induces oxidative signaling and subsequent ER stress in breast cancer cell lines. Biotechnol. Appl. Biochem. [DOI] [PubMed] [Google Scholar]
- 214.Massi P.et al. (2006) The non-psychoactive cannabidiol triggers caspase activation and oxidative stress in human glioma cells. Cell. Mol. Life Sci. 63, 2057–2066 10.1007/s00018-006-6156-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Jeong S.et al. (2019) Cannabidiol Overcomes Oxaliplatin Resistance by Enhancing NOS3- and SOD2-Induced Autophagy in Human Colorectal Cancer Cells. Cancers (Basel) 11, 10.3390/cancers11060781 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Yeisley D.J., Arabiyat A.S. and Hahn M.S. (2021) Cannabidiol-Driven Alterations to Inflammatory Protein Landscape of Lipopolysaccharide-Activated Macrophages In Vitro May be Mediated by Autophagy and Oxidative Stress. Cannabis Cannabinoid Res. 10.1089/can.2020.0109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Wojcik P.et al. (2020) Cannabidiol Modifies the Formation of NETs in Neutrophils of Psoriatic Patients. Int. J. Mol. Sci. 21, 10.3390/ijms21186795 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Devinsky O.et al. (2017) Trial of Cannabidiol for Drug-Resistant Seizures in the Dravet Syndrome. N. Engl. J. Med. 376, 2011–2020 10.1056/NEJMoa1611618 [DOI] [PubMed] [Google Scholar]
- 219.Szaflarski J.P.et al. (2018) Cannabidiol improves frequency and severity of seizures and reduces adverse events in an open-label add-on prospective study. Epilepsy Behav. 87, 131–136 10.1016/j.yebeh.2018.07.020 [DOI] [PubMed] [Google Scholar]
- 220.Flachenecker P., Henze T. and Zettl U.K. (2014) Nabiximols (THC/CBD oromucosal spray, Sativex®) in clinical practice–results of a multicenter, non-interventional study (MOVE 2) in patients with multiple sclerosis spasticity. Eur. Neurol. 71, 271–279 10.1159/000357427 [DOI] [PubMed] [Google Scholar]
- 221.Stott C.G.et al. (2013) A phase I study to assess the single and multiple dose pharmacokinetics of THC/CBD oromucosal spray. Eur. J. Clin. Pharmacol. 69, 1135–1147 10.1007/s00228-012-1441-0 [DOI] [PubMed] [Google Scholar]
- 222.Feliu A., Moreno-Martet M., Mecha M., Carrillo-Salinas F.J., Lago E., Fernandez-Ruiz J.et al. (2015) Sativex-like combination of phytocannabinoids as a disease-modifying therapy in a viral model of multiple sclerosis. Br. J. Pharmacol. 172(14), 3579–3595 10.1111/bph.13159 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Patti F.et al. (2016) Efficacy and safety of cannabinoid oromucosal spray for multiple sclerosis spasticity. J. Neurol. Neurosurg. Psychiatry 87, 944–951 10.1136/jnnp-2015-312591 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 224.Zurier R.B. and Burstein S.H. (2016) Cannabinoids, inflammation, and fibrosis. FASEB J. 30, 3682–3689 10.1096/fj.201600646R [DOI] [PubMed] [Google Scholar]
- 225.Badowski M.E. and Yanful P.K. (2018) Dronabinol oral solution in the management of anorexia and weight loss in AIDS and cancer. Therap. Clin. Risk Manag. 14, 643–651 10.2147/TCRM.S126849 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 226.Berlach D.M., Shir Y. and Ware M.A. (2006) Experience with the synthetic cannabinoid nabilone in chronic noncancer pain. Pain Med. 7, 25–29 10.1111/j.1526-4637.2006.00085.x [DOI] [PubMed] [Google Scholar]