Abstract
Heart failure is a leading cause of readmissions in the United States, although treatment has come along away, palliative care is often not appropriately offered in advanced heart failure. The purpose of this study was to use a large database of national in-patient sample to find out the use of palliative care in acute heart failure admissions. Data from 2002 to 2017 was used for analysis. Simple linear regression was used for trend analysis over the years. Variables that were statistically significant in univariate analysis were used in single-step (entry method) multiple logistic analysis. The use of palliative care was found to be low at 4.1%, although recent trends have shown an increase (from 0.4% in 2002 to 6.2% in 2017). Women (0.3% in 2002 to 6.5% in 2017) and Caucasians (0.6% in 2002 to 6.9% in 2017) had a higher proportion of PC encounters as compared to men (0.5% in 2002 to 5.9% in 2017) and other racial minorities, increasing age (OR, 1.04[CI; 1.03–1.04], p < 0.01), female gender (OR, 1.03[CI; 1.02–1.03], p < 0.01), do not resuscitate status (OR, 10.62[CI; 10.53–10.70], p < 0.01), diabetes mellitus (OR, 1.10[CI; 1.01–1.11], p < 0.01), liver disease (OR, 1.63[CI; 1.60–1.66], p < 0.01), renal failure (OR, 1.40[CI; 1.39–1.41], p < 0.01), acute myocardial infarction (OR, 1.28[CI; 1.27–1.30], p < 0.01), and cardiogenic shock (OR, 2.89[CI; 2.84–2.93], p < 0.01) were associated with higher odds of having PC encounter. In conclusion, the use of palliative care has increased in the United States over the years, however, it is still low as compared to other high-income countries.
Keywords: Palliative care encounters, Acute heart failure, Racial disparities, National inpatient sample
1. Introduction
Heart failure (HF) affects almost 10% of the population above 75 years [1]. HF management has improved over the last three decades since numerous new trials have paved the way for better treatment strategies [1,2]. Patients with HF now live longer and hence, prevalence of HF has increased over the years [3]. Acute HF is the most common cause of readmission in adults over 65 years in high-income countries [4]. The burden of HF on our health system is going to increase going further [4,5]. Traditionally, associated with oncology patients, PC is appropriate for any end stage disease including advance HF. Therefore, in patients with end-stage diseases like advanced HF with limited treatment options, there has been a renewed focus on the quality of life through integrated palliative care (PC) that can address the psychological and physical discomfort of advanced heart failure. PC encounter is the first step towards progression to PC [6[. Previous studies have shown that PC utilization is low despite the increase in population of end stage HF [7,8]. Contemporary data on PC access is still lacking despite a recent increase in advanced HF patients and a renewed focus on PC. Racial and gender disparities in end of life care and hospice access has been previously identified [9], however, to what extent do such disparities exist in HF is not known. No prior studies exist on racial disparities in access to PC in hospital admissions due acute HF. In this study we have focused on recent trends in PC encounters in patients admitted with acute decompensated heart failure to hospitals in united states using a nationally representative data. We have also focused on disparities with respect to gender and race in PC encounters and finally we have looked at association between demographic variables, surrogates for intensive care, co-morbid conditions and PC encounters in patients admitted for acute HF.
2. Methods
2.1. Study data
The national Inpatient Sample (NIS) from 2002 to 2017 was used for data analysis. The NIS is a Federal-State-Industry partnership sponsored by the Agency for Healthcare Research and Quality (AHRQ). The NIS is derived from all States for national estimates of healthcare utilization, costs, and outcome [10]. As NIS is compiled annually; the data can be used for the analysis of trends over time. Our study did not require Institutional Review Board approval or informed consent given the de-identified nature of the NIS database.
2.2. Study design and data selection
NIS data from January 2002 to December 2017 was analyzed using the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) and ICD-10 codes. Patients under 18 years were excluded. Inclusion criteria included patients with acute HF (428.21, 428.31, 428.41 & I50.21, I50.23, I50.31, I50.33, I50.41, I50.43) in any diagnosis code. The use of PC encounter was determined by using all diagnostic field for relevant codes (V66.7 and Z51.5). These diagnostic codes have high specificity (98%) and positive predicted value (98%) in identifying PC encounters [7,11]. Discharge weight provided was used for analysis after 2011 and trend weight provided was used for analysis before 2012.
2.3. Study endpoints
Primary endpoints for study were predictors of palliative encounters and trends in utilization of palliative encounters with emphasis on gender, racial and, ethnic disparities in palliative care encounters.
2.4. Statistical analysis
For univariable analysis, descriptive statistics were presented as frequencies with percentages for categorical variables and as means with standard deviations for continuous variables.
Baseline characteristics were compared using a Pearson chi square test and independent samples t-test for continuous variables. Trend analysis over the years was done. Simple linear regression (linear trend model) was used to predict trends over the years. Pairwise deletion was done to address the missing data in certain variables. Significant missing data was present in race, insurance payee, income and cost (>5%).
Multivariable analysis was done by constructing a binary logistic regression model for predictors of PC encounter using variables in Table 1. All statistical analyses were performed using Statistical Package for Social Science (SPSS) version 26 (IBM Corp.).
Table 1.
Baseline characters of study cohort and predictors of palliative encounter.
| Variable no. (%) | Univariate analysis |
Multiple variable analysis |
||||
|---|---|---|---|---|---|---|
| No palliative encounter (13,322,694) | Palliative encounter (571,310) | p value | Odds ratio | 95% confidence interval | p value | |
| Age (median [IQR]) years | 75(63–84) | 82(73–88) | <0.01 | 1.036 | 1.035–1.037 | <0.01 |
| Age < 65 | 3,567,240(26.8) | 68,530(12.0) | <0.01 | Reference | ||
| 65–84 | 6,746,143(50.6) | 267,196(46.8) | <0.01 | 1.009 | 0.990–1.030 | 0.35 |
| ≥85 | 3,009,311(22.6) | 235,584(41.2) | <0.01 | 1.450 | 1.411–1.490 | <0.01 |
| Died | 464,715(3.5) | 219,143(38.4) | <0.01 | 17.221 | 17.116–17.326 | <0.01 |
| Disposition of surviving patients | ||||||
| Home discharge | 9,084,764(70.7) | 159,712(45.7) | <0.01 | Reference | ||
| Facility discharge | 3,765,692(29.3) | 189,810(54.3) | 1.817 | 1.803–1.831 | <0.01 | |
| Female | 6,651,767(49.9) | 299,437(52.4) | <0.01 | 1.026 | 1.019–1.034 | <0.01 |
| Race | ||||||
| Caucasian | 8,792,353(71.1) | 430,930(79.7) | <0.01 | Reference | ||
| African American | 2,151,685(17.4) | 57,395(10.6) | 0.866 | 0.856–0.877 | <0.01 | |
| Hispanics | 847,020(6.8) | 28,907(5.3) | 0.831 | 0.817–0.844 | <0.01 | |
| Asian or Pacific Islander | 228,121(1.8) | 10,850(2.0) | 0.810 | 0.789–0.832 | <0.01 | |
| Native American | 65,761(0.5) | 1919(0.4) | 0.689 | 0.645–0.735 | <0.01 | |
| Other | 283,452(2.3) | 10,488(1.9) | 1.025 | 1.016–1.033 | <0.01 | |
| Do not resuscitate (DNR) order | 991,369(7.4) | 309,829(54.2) | <0.01 | 10.615 | 10.530–10.700 | <0.01 |
| Admission is weekend | 3,091,450(23.2) | 139,347(24.4) | <0.01 | 0.650 | 0.639–0.662 | <0.01 |
| Elective admission | 911,327(6.9) | 31,488(5.5) | <0.01 | 0.866 | 0.856–0.877 | <0.01 |
| Co-morbidities | ||||||
| Chronic pulmonary disease | 4,890,852(36.7) | 207,981(36.4) | 0.70 | 1.099 | 1.09–1.107 | <0.01 |
| Coagulopathy | 1,009,399(7.6) | 78,703(13.8) | <0.01 | 1.204 | 1.191–1.218 | <0.01 |
| Diabetes (complicated) | 2,196,877(16.5) | 92,679(16.2) | <0.01 | 1.100 | 1.089–1.111 | <0.01 |
| Hypertension | 8,264,006(62.1) | 329,382(57.7) | <0.01 | 0.737 | 0.731–0.742 | <0.01 |
| Hypothyroidism | 2,246,615(16.9) | 111,838(19.6) | <0.01 | 1.022 | 1.013–1.031 | 0.02 |
| Liver disease | 428,701(3.2) | 25,514(4.5) | <0.01 | 1.633 | 1.604–1.663 | <0.01 |
| Lymphoma | 136,976(1.0) | 9798(1.7) | <0.01 | 1.519 | 1.477–1.562 | <0.01 |
| Metastatic cancer | 150,308(1.1) | 22,988(4.0) | <0.01 | 3.931 | 3.859–4.005 | <0.01 |
| Obesity | 2,685,452(20.2) | 70,147(12.3) | <0.01 | 0.790 | 0.781–0.799 | <0.01 |
| Paralysis | 329,038(2.5) | 26,264(4.6) | <0.01 | 1.425 | 1.399–1.452 | <0.01 |
| Solid tumor with no metastasis | 251,126(1.9) | 21,418(3.7) | <0.01 | 1.962 | 1.926–1.999 | <0.01 |
| Pulmonary circulation disorder | 517,120(3.9) | 36,929(6.5) | <0.01 | 0.993 | 0.977–1.010 | 0.44 |
| Peripheral vascular disorders | 1,702,396(12.8) | 80,308(14.1) | <0.01 | 1.028 | 1.017–1.039 | <0.01 |
| Peptic ulcer disease | 38,460(0.3) | 2767(0.5) | <0.01 | 1.143 | 1.084–1.205 | <0.01 |
| Renal failure | 5,279,507(39.6) | 271,324(47.5) | <0.01 | 1.403 | 1.393–1.414 | <0.01 |
| Weight loss | 886,537(6.7) | 97,215(17.0) | <0.01 | 1.759 | 1.741–1.777 | <0.01 |
| Valvular disease | 921,488(6.9) | 67,518(11.8) | <0.01 | 1.056 | 1.043–1.070 | <0.01 |
| Smoking | 1,522,646(11.4) | 37,339(6.5) | <0.01 | 0.968 | 0.954–0.983 | <0.01 |
| Prior stroke | 1,473,340(11.1) | 76,207(13.3) | <0.01 | 1.179 | 1.167–1.192 | <0.01 |
| Prior defib | 1,045,707(7.8) | 41,846(7.3) | <0.01 | 1.483 | 1.463–1.503 | <0.01 |
| Prior pacer | 1,081,096(8.1) | 47,892(8.4) | <0.01 | 0.938 | 0.927–0.950 | <0.01 |
| Prior CABG* | 1,803,817(13.5) | 67,705(11.9) | <0.01 | 0.934 | 0.923–0.945 | <0.01 |
| Acute MI† | 1,568,964(11.8) | 97,489(17.1) | <0.01 | 1.281 | 1.267–1.295 | <0.01 |
| Prior PCI‡ | 1,370,265(10.3) | 45,761(8.0) | <0.01 | 0.927 | 0.915–0.940 | <0.01 |
| Cardiogenic shock | 341,034(2.6) | 55,742(9.8) | <0.01 | 2.887 | 2.836–2.938 | <0.01 |
| Vasopressors use | 119,637(0.9) | 21,771(3.8) | <0.01 | 1.491 | 1.451–1.533 | <0.01 |
| IABP¶ | 123,723(0.9) | 7956(1.4) | <0.01 | 0.509 | 0.486–0.533 | <0.01 |
| Percutaneous VADs§ | 22,845(0.2) | 2736(0.5) | <0.01 | 1.189 | 1.087–1.301 | <0.01 |
| Vent | 911,944(6.8) | 107,815 (18.9) | <0.01 | 1.206 | 1.189–1.223 | <0.01 |
| Primary payee | ||||||
| Medicare | 10,097,397(75.9) | 476,073(83.5) | <0.01 | Reference | ||
| Medicaid | 1,050,480(7.9) | 23,074(4.0) | 1.228 | 1.203–1.253 | <0.01 | |
| Private | 1,565,544(11.8) | 51,269(9.0) | 1.039 | 1.024–1.054 | <0.01 | |
| Self | 349,238(2.6) | 5991(1.1) | 0.901 | 0.866–0.936 | 0.61 | |
| Hospital location | ||||||
| Rural | 1,454,982(10.9) | 40,651(7.1) | <0.01 | Reference | ||
| Urban non-teaching | 4,533,146(34.0) | 165,457(29.0) | 1.298 | 1.278–1.319 | <0.01 | |
| Urban teaching | 7,334,567(55.1) | 365,203(63.9) | 2.003 | 1.973–2.033 | <0.01 | |
| Bed size of the hospital | ||||||
| Small | 2,001,113(15.0) | 79,084(13.8) | <0.01 | Reference | ||
| Medium | 3,663,127(27.5) | 154,280(27.0) | 1.112 | 1.100–1.125 | <0.01 | |
| Large | 7,658,454(57.5) | 337,946(59.2) | 1.210 | 1.197–1.223 | <0.01 | |
| Region | ||||||
| Northeast | 2,829,969(21.2) | 105,860(18.5) | <0.01 | Reference | ||
| Midwest | 3,246,402(24.4) | 147,013(25.7) | 1.535 | 1.518–1.553 | <0.01 | |
| South | 5,183,348(38.9) | 205,756(36.0) | 1.627 | 1.610–1.644 | <0.01 | |
| West | 2,062,976(15.5) | 112,681(19.7) | 1.731 | 1.711–1.753 | <0.01 | |
| Median income | ||||||
| 0–25th | 4,156,918(31.8) | 141,990(25.2) | <0.01 | Reference | ||
| 26–50th | 3,476,886(26.6) | 148,683(26.4) | 1.107 | 1.096–1.119 | <0.01 | |
| 51–75th | 3,027,978(23.2) | 144,314(25.6) | 1.117 | 1.106–1.129 | <0.01 | |
| 76–100th | 2,405,337(18.4) | 127,823(22.7) | 1.123 | 1.111–1.1360 | <0.01 | |
Coronary artery bypass surgery.
Myocardial infarction.
Percutaneous coronary intervention.
Ventricular assist device.
Intra-aortic balloon pump.
3. Results
A total of 13,894,004 discharge encounters were recorded from 2002 to 2017. Out of these, 571,310 (4.1%) had a PC encounter. The median age was 75 years (interquartile range [IQR, 64–84]). The median age for discharges with PC encounters was higher than those without (75 years [IQR, 63–84] vs 82 years [IQR, 73–88]). Discharges with PC encounters had a greater proportion of patients ≥85 (41.2% vs 22.6%). Discharges with PC encounters had higher mortality (38.4% vs 3.5%) though mortality was substantially high even in discharges without PC encounters as well. Demographic and other baseline characters are given in Table 1.
Discharges with PC encounters were more likely to be discharged to a nursing home as compared to those without (54.3% vs 29.3%) and less likely to be discharged home (45.7% vs 70.7%). Do not resuscitate (DNR) status was more often found in discharges with PC encounters as compared to those without one (54.2% vs 7.4%). Most of the comorbidities like anemia, chronic obstructive pulmonary disease (COPD), coagulopathy, pulmonary circulation disorders, renal failure were more common in discharges with a PC encounters as compared to those without a PC encounter.
On multivariable analysis increasing age (OR, 1.036 [95% CI, 1.035–1.037], p < 0.01), female gender (OR, 1.026 [95% CI, 1.019–1.034], p < 0.01), DNR status (OR, 10.615 [95% CI, 10.530–10.700], p < 0.01), COPD (OR, 1.099 [95% CI, 1.09–1.107], p < 0.01), diabetes mellitus(OR, 1.100 [95% CI, 1.089–1.111], p < 0.01), liver disease (OR, 1.633 [95% CI, 1.604–1.663], p < 0.01), renal failure (OR, 1.403 [95% CI, 1.393–1.414], p < 0.01), weight loss (OR, 1.759 [95% CI, 1.741–1.777], p < 0.01) and cardiogenic shock (OR, 2.887 [95% CI, 2.836–2.938], p < 0.01) were associated with higher odds of having PC encounter (Table 1). Similarly, teaching hospital (OR, 2.003 [95% CI, 1.973–2.033], p < 0.01), larger size hospital (OR, 1.210 [95% CI, 1.197–1.223], p < 0.01), West census region (OR, 1.731 [95% CI, 1.711–1.753], p < 0.01) had higher odds of having a PC encounter. African Americans (OR, 0.866 [95% CI, 0.856–0.877], p < 0.01), Hispanics (OR, 0.831 [95% CI, 0.817–0.844], p < 0.01) and Asians (OR, 0.810 [95% CI, 0.789–0.832], p < 0.01) were less likely to have a PC encounter as compared to Caucasians.
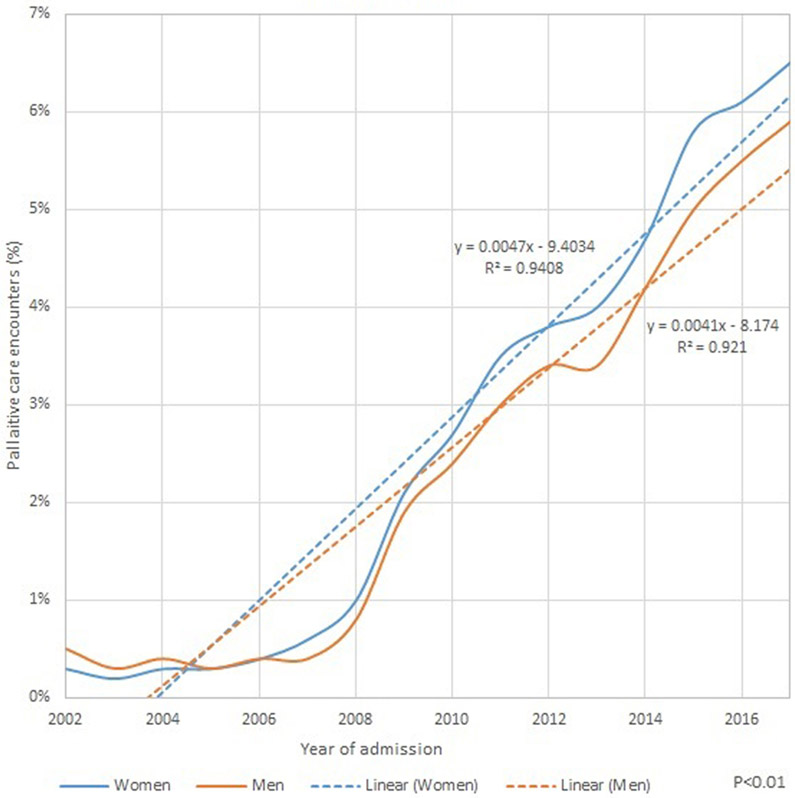
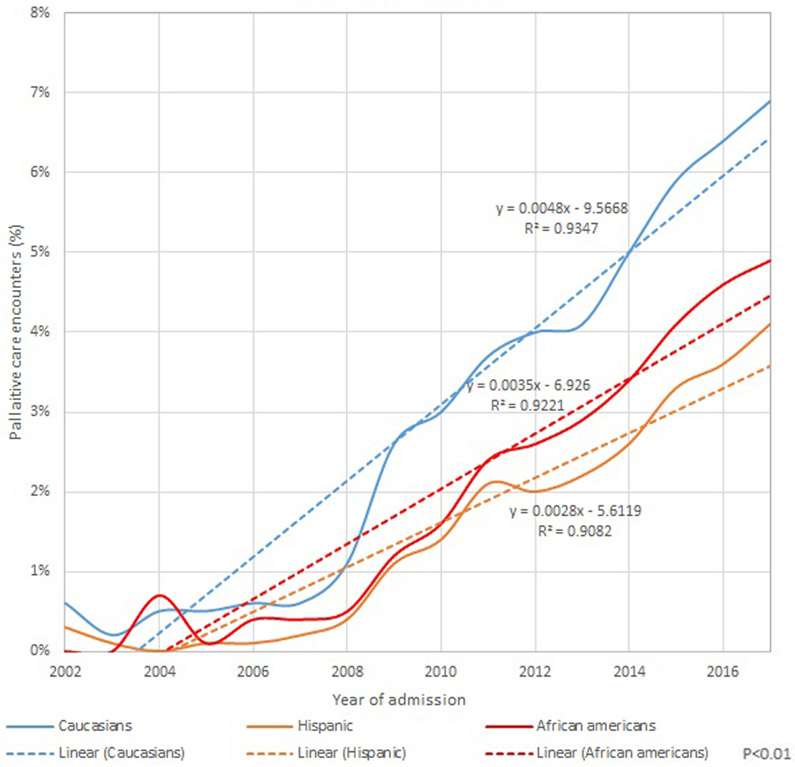
Over the years the use of PC encounters has increased from 0.4% in 2002 to 6.2% in 2017 (P < 0.01) [Fig. 1]. The increase was seen in all races, both men and women. Women (0.3% in 2002 to 6.5% in 2017) and Caucasians (0.6% in 2002 to 6.9% in 2017) had a higher proportion of PC encounters as compared to men and other racial minorities (Fig. 2).
Fig. 1.
Gender trends in palliative care encounters in acute heart failure admissions.
Fig. 2.
Ethnic and racial trends in palliative care encounters in acute heart failure admissions.
4. Discussion
Advanced HF is one of the leading terminal conditions in the United States. This study demonstrates that the use of PC is still very low at around 6.2% in 2017, although there is an increase recent trend (0.4% in 2002). Prevalence was low even for discharge encounters with high comorbidities. Belonging to racial and ethnic minority predict lower odds of having a PC encounter.
HF is the leading cause of readmission in elderly patients [1]. These readmissions have tremendous physical and psychological effects on patients. Acute HF hospitalizations provides a unique opportunity for physicians and the patients to reflect upon their current goals of care. PC availability provides this opportunity to the patient. Previously, Mandawat et al. [7] in a study in Veteran's Affairs Healthcare noticed there was increase in trends in PC encounters. Alqahtani et al. [8] using the same database as ours showed a similar small increase in uptake till 2014. Our cohort extends this till 2017 and shows a rapid increase from 2014 to 2017. This shows that recently there has been better availability of PC services. Only 61.6% of the patients who received PC encounters were discharged alive from the hospital. Patients who end up having a PC encounter had very high inpatient mortality pointing towards terminal condition [12]. Warraich et al. [13] from the HF Medicare patients registry showed a similar low hospice discharge rate, though the trend seems to be increasing. However, overall, the utilization of PC remains low as compared to other high-income countries. Studies outside the United States, especially in Scandinavian countries show a much higher trend of PC and end of life discussions. Pivodic, Lara et al. found Palliative care services offered to 29% of patients in the Netherlands, 39% in Italy, 45% in Spain, and 47% in Belgium [14,15].
There are many reasons for the low utilization of PC including reluctance by patients, families, and clinicians to accept that the patient is in the end-stage of illness [16,17]. Our study also showed that patients with DNR status, elderly, and having multiple comorbidities are more likely to have a PC encounters (Table 1). DNR status patients were ten times more likely to have a PC encounter, this may suggest hesitancy on part of physicians to address the goals of care, until the very end when the care is futile [6,18,19]. This would also explain the very high in-patient mortality rates in patients who end up having a PC encounter and escalation of care before the end of life discussion [20].
Patients' cultural, religious, and/or ethnic backgrounds may also play a role use of hospice services [21]. Ethnic and racial disparities in the use of palliative care are not well understood. Previously, studies have shown greater preference for life-sustaining therapies among African Americans and Hispanics compared to Caucasians [9,22]. While previous research for the reasons behind this are lacking, potential reasons could include organizational barriers like lack of communication skills, language barriers, interpreters, and education [23]. Research is needed to understand the disparities in palliative care.
Going forward, several avenues of improvement exist in the provision of PC encounters to patients with HF exacerbation admitted to the hospitals. Administrative barriers like delay hospice referrals needs to be addressed. Centers for Medicare and Medicaid Services (CMS) is the largest payer for hospice care. To access this end-of-life care benefit, CMS requires certification of a terminal prognosis by a patient's treating physician and a hospice medical director, which itself is limiting factor given the uncertainty in the estimation of survival in most patients [24,25]. Since 2012, several associations such as the American Academy of Hospice and Palliative Medicine, Hospice and Palliative Nurses Association have led the campaign “Choosing Wisely” to initiate greater discussion of hospice care in patients with terminal conditions requiring recurrent admissions and Intensive care [26]. The focus is on quality of life rather than unnecessary aggressive care. The federal government through the “Bipartisan Budget Act of 2018” allowed broader availability of hospice care by allowing physician assistants to provide independent hospice care where needed [27]. Availability of dedicated PC teams, skill enhancement among physicians, residents and specialty HF management teams have shown to improve delivery of PC, further improvements are needed in this area [28-31].
This study uses NIS which has several limitations. The NIS is an administrative claim-based database that uses ICD-9-CM and ICD-10-CM codes for diagnosis and reimbursement that may be subject to error. Validity studies for ICD-9-CM and ICD-10-CM codes are limited. One such study showed sensitivity of 84% (95% CI: 72–92) and specificity was 98% (95% CI: 86–99) for palliative care encounter [11]. NIS collects data on in-patient discharges and each admission is registered as an independent event. Readmissions cannot be tracked. NIS samples are not designed to follow patients longitudinally, so long-term outcomes could not be assessed from the present dataset.
In conclusion, recently there has been an increase trend in PC encounters in heart failure admissions, however, the use of PC is still low. Further prospective interventional studies might provide insight into tools to address low utilization of PC encounters.
Footnotes
Declaration of competing interest
Author have no conflicts to disclose.
Appendix A. Supplementary data
Supplementary data to this article can be found online at https://doi.org/10.1016/j.carrev.2020.08.024.
References
- [1].Metra M, Teerlink JR. Heart failure. Lancet. 2017;390:1981–95. 10.1016/S0140-6736(17)31071-1. [DOI] [PubMed] [Google Scholar]
- [2].Taylor CJ, Ordóñez-Mena JM, Roalfe AK, Lay-Flurrie S, Marshall T, Roalfe AK, et al. Trends in survival after a diagnosis of heart failure in the United Kingdom 2000–2017: population based cohort study. BMJ. 2019;364:1223. 10.1136/bmj.l223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Najafi F Jamrozik K, Dobson AJ. Understanding the “epidemic of heart failure”: a systematic review of trends in determinants of heart failure. Eur J Heart Fail. 2009;11:472–9. 10.1093/eurjhf/hfp029. [DOI] [PubMed] [Google Scholar]
- [4].Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, et al. Heart disease and stroke statistics-2019 update: a report from the American Heart Association. Circulation. 2019;139:e56–528. 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- [5].Heidenreich PA Albert NM, Allen LA Bluemke DA Butler J, Fonarow GC, et al. Forecasting the impact of heart failure in the United States a policy statement from the American Heart Association. Circ Hear Fail. 2013;6:606–19. 10.1161/HHF.0b013e318291329a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Elgendy IY, Elbadawi A Sardar P, Kolte D, Omer MA Mahmoud AN, et al. Palliative care use in patients with acute myocardial infarction. J Am Coll Cardiol. 2020;75:113–7. 10.1016/j.jacc.2019.11.009. [DOI] [PubMed] [Google Scholar]
- [7].Mandawat A Heidenreich PA, Mandawat A, Bhatt DL Trends in palliative care use in veterans with severe heart failure using a large national cohort JAMA Cardiol. 2016;1:617–9. 10.1001/jamacardio.2016.1687. [DOI] [PubMed] [Google Scholar]
- [8].Alqahtani F, Balla S, Almustafa A Sokos G, Alkhouli M. Utilization of palliative care in patients hospitalized with heart failure: a contemporary national perspective. Clin Cardiol. 2019;42:136–42. 10.1002/clc.23119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Barnato AE, Anthony DL, Skinner J, Gallagher PM, Fisher ES. Racial and ethnic differences in preferences for end-of-life treatment. J Gen Intern Med. 2009;24:695–701. 10.1007/s11606-009-0952-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Agency for Healthcare Research and Quality. Overview of the national (nationwide) inpatient sample (NIS). Rockville: AHRQ. [Google Scholar]
- [11].Feder SL, Redeker NS, Jeon S, Schulman-Green D, Womack JA Tate JP, et al. Validation of the ICD-9 diagnostic code for palliative care in patients hospitalized with heart failure within the Veterans Health Administration. Am J Hosp Palliat Med. 2018;35:959–65. 10.1177/1049909117747519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Aslakson RA Randall Curtis J, Nelson JE. The changing role of palliative care in the ICU. Crit Care Med. 2014;42:2418–28. 10.1097/CCM.0000000000000573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Warraich HJ, Xu H, Devore AD, Matsouaka R, Heidenreich PA Bhatt DL, et al. Trends in hospice discharge and relative outcomes among Medicare patients in the get with the guidelines-heart failure registry. JAMA Cardiol. 2018;3:917–26. 10.1001/jamacardio.2018.2678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Pivodic L, Pardon K, Van den Block L, Casteren VV, Miccinesi G, Donker GA et al. Palliative care service use in four European countries: a cross-national retrospective study via representative networks of general practitioners. PLoS One. 2013;8:e84440. 10.1371/journal.pone.0084440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Chambaere K, Vander Stichele R, Mortier F, Cohen J, Deliens L. Recent trends in euthanasia and other end-of-life practices in Belgium. N Engl J Med. 2015;372:1179–81. 10.1056/NEJMc1414527. [DOI] [PubMed] [Google Scholar]
- [16].Autor SH, Storey SL, Ziemba-Davis M. Knowledge of palliative care. J Hosp Palliat Nurs. 2013. 10.1097/njh.0b013e3182930800. [DOI] [Google Scholar]
- [17].Spice R, Lau M, Perez G, Turley N, Turin TC. Hospice care in Calgary: survey of family physicians on their knowledge, experience, and attitudes. Can Fam Physician. 2016;62:e484–94. [PMC free article] [PubMed] [Google Scholar]
- [18].Christakis NA, Lamont EB. Extent and determinants of error in doctors’ prognoses in terminally ill patients: prospective cohort study. Br Med J. 2000;320:469–72. 10.1136/bmj.320.7233.469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Rakoski MO, Volk ML. Palliative care for patients with end-stage liver disease: an overview. Clin Liver Dis. 2015;6:19–21. 10.1002/cld.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Teno JM, Gozalo PL, Bynum JPW, Leland NE, Miller SC, Morden NE, et al. Change in end-of-life care for medicare beneficiaries: site of death, place of care, and health care transitions in 2000, 2005, and 2009. JAMA. 2013;309:470–7. 10.1001/jama.2012.207624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Washington KT, Bickel-Swenson D, Stephens N. Barriers to hospice use among african americans: a systematic review. Heal Soc Work 2008;33:267–74. 10.1093/hsw/33.4.267. [DOI] [PubMed] [Google Scholar]
- [22].Kwak J, Haley WE. Current research findings on end-of-life decision making among racially or ethnically diverse groups. Gerontologist. 2005;45:634–41. 10.1093/geront/45.5.634. [DOI] [PubMed] [Google Scholar]
- [23].Reese DJ, Melton E, Ciaravino K. Programmatic barriers to providing culturally competent end-of-life care. Am J Hosp Palliat Med. 2004;21:357–64. 10.1177/104990910402100510. [DOI] [PubMed] [Google Scholar]
- [24].Keating NL, Landrum MB, Rogers SO, Baum SK, Virnig BA Huskamp HA et al. Physician factors associated with discussions about end-of-life care. Cancer. 2010;116:998–1006. 10.1002/cncr.24761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Fine PG. Hospice underutilization in the U.S.: the misalignment of regulatory policy and clinical reality. J Pain Sympt Manage. 2018. 10.1016/j.jpainsymman.2018.08.005. [DOI] [PubMed] [Google Scholar]
- [26].Choosing Wisely, a ABIM initiative. https://www.choosingwisely.org/our-mission/.
- [27].Two big changes for hospice. https://healthcareprovidersolutions.com/physician-assistants-as-attending-physicians-and-early-hospital-discharges-to-hospice-care/.
- [28].Morrison RS, Meier DE. Palliative care. N Engl J Med. 2004;350:2582–90 +2629 10.1056/NEJMcp035232. [DOI] [PubMed] [Google Scholar]
- [29].Wolf SM, Berlinger N, Jennings B. Forty years of work on end-of-life care-from patients’ rights to systemic reform. N Engl J Med. 2015;372:678–82. 10.1056/NEJMms1410321. [DOI] [PubMed] [Google Scholar]
- [30].Mitchell G, Zhang J, Burridge L, Senior H, Miller E, Young S, et al. Case conferences between general practitioners and specialist teams to plan end of life care of people with end stage heart failure and lung disease: an exploratory pilot study. BMC Palliat Care. 2014;13. 10.1186/1472-684X-13-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Fendler TJ, Swetz KM, Allen LA. Team-based palliative and end-of-life care for heart failure. Heart Fail Clin. 2015;11:479–98. 10.1016/j.hfc.2015.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]