Abstract
Background
Since coronavirus disease 2019 (COVID-19) outbreak, its terrible infectiousness has caused great panic, anxiety and poor sleep quality to the vulnerable adolescent populations.
Methods
This cross-sectional online survey recruited 10 569 Chinese junior and senior high school adolescents during 31 January to 9 February 2020. Basic socio-demographic information, Pittsburgh Sleep Quality Index (PSQI), Self-rating Anxiety Scale (SAS) and Fear of negative evaluation (FNE) were included in the survey. The χ2 and logistic regression analyses were used to identify factors correlated with poor sleep quality.
Results
The prevalence of poor sleep quality was 18.6% in the Chinese adolescent population. The average score of PSQI was 3.39 (SD = 2.64), which was significantly correlated with scores for anxiety (r = 0.50, p < 0.01), and FNE (r = 0.36, p < 0.01). Adjusted logistic regression indicated that gender (females) and education (senior high school) were associated with poor sleep quality, while living in Hubei Province and time spent on the COVID-19 information were inversely associated with poor sleep quality. Having a family member or friend infected/suspected and spending time on electronics were associated with higher odds of having poor sleep quality. Adolescents with anxiety were 8 times, and those with FNE were three times more likely than ones without anxiety or FNE to have poor sleep quality. In addition, the number of meals, exercise time and diet quality were also significantly associated with sleep quality. (p < 0.05).
Conclusions
Poor sleep quality was common during the COVID-19 pandemic in Chinese adolescents. Understanding several factors associated with the poor sleep quality will offer some important insights into determining potential interventions to improve sleep quality during the COVID-19 pandemic.
Keywords: COVID-19, prevalence, poor sleep quality, risk factors, adolescents
INTRODUCTION
Adolescence is a critical period of transition in the life span, which is characterized by tremendous changes and growth [1]. Sleep is indispensable for the growth and development of adolescents and it is also necessary for maintaining their physical and psychological health [1]. According to the previous studies, prevalence of poor sleep quality in adolescents ranged from 3.4% to 40% in various countries [2, 3]. While, the prevalence of poor sleep quality in Chinese adolescent ranged from 3.4% to 25.7% [4, 5] before the COVID-19 pandemic. Compared with Chinese adolescents with good sleep quality, those with poor sleep quality were more likely to be girls, city residence, victims of bullying, with unstable personality, senior grades, with high academic pressure, lonely, anxious and depressed [4, 5]. The sleep theme of adolescents with poor sleep includes difficulties falling asleep, restless sleep, mid-sleep awakening for several times and waking up too early [1–5].
Adolescents, who are going through an immature psychological developing period, are easily affected by external adverse factors, especially the public health emergencies [6, 7]. The emergence of COVID-19 pandemic has exacerbated anxiety globally [7]. Recent studies have shown an increased prevalence of mental health disorders; such as anxiety, depression and post-traumatic stress symptoms with the rapid spread of and lock down caused by COVID-19 [8–10]. Among the various emergency measures taken to limit the COVID-19 outbreak, the temporary closure of schools and keeping the students at home, rendered lifestyle changes such as stopping the usual daily activities and spending more time on electronics [11]. Such lifestyle changes may bear risk to the adolescent physical and psychological health by hindering peer relationships and depriving opportunities for stress regulation [11]. However, since the morbidity and mortality of COVID-19 infection were lower in adolescents than in adults [12], the previous studies primarily focused on the mental and sleep outcomes associated with COVID-19 among the adult population [13], especially the health care medical staff [14], with insufficient attention on the adolescents’ sleep quality [6, 7]. Therefore, it is necessary to timely evaluate adolescents’ sleep quality and the related factors induced by the pandemic.
This study seeks to evaluate the prevalence and influencing factors of poor sleep quality among adolescents in junior and senior high schools during the COVID-19 pandemic, which could be helpful to screen the poor sleep quality among adolescents and explore potential interventions in the current or future pandemics.
METHODS
Data collection and participants
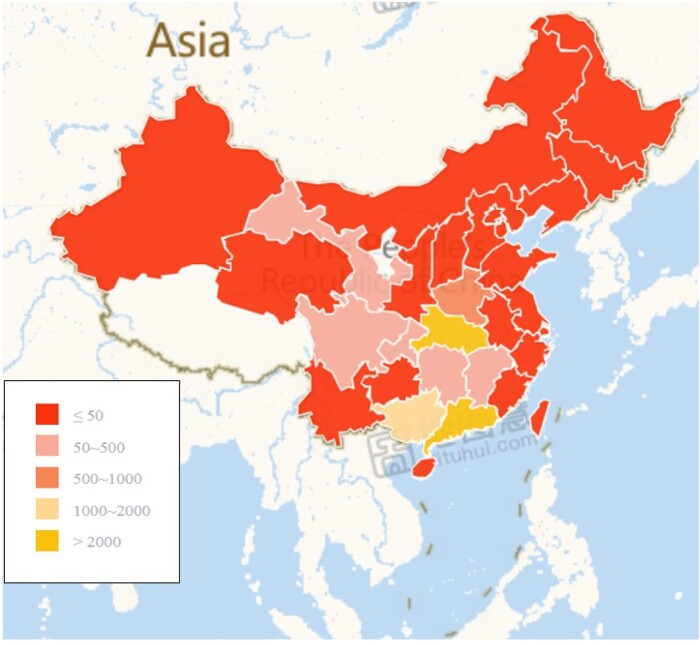
By the convenience sampling method, an online cross-sectional survey that recruited 10 569 participants from 32 provinces of China was conducted through the WenJuanxing platform, a large ecommerce and information service platform that provides online health products and services in China (https://www.wjx.cn/). The detailed geographic distribution of participants is shown in Fig. 1. The inclusion criteria for this study were as follow: (i) age between 12 and 20 years, (ii) adolescents in junior or senior high schools and (iii) volunteered to participate in the survey.
FIG. 1.
The detailed geographic distribution of participants.
The online questionnaire was designed to collect basic socio-demographic information, Pittsburgh Sleep Quality Index (PSQI), Self-rating Anxiety Scale (SAS) and Fear of negative evaluation (FNE) questionnaire from 31 January to 9 February 2020. All adolescents provided informed consent. Participants had received explanation before signing the consent to participate and the analysis was entirely anonymous. This study was conducted anonymously and approved by the Ethics Committee of School of Medicine, Wuhan University of Science and Technology.
INSTRUMENTS
Sleep quality
The sleep quality was assessed using the PSQI [15]. The PSQI scale is categorized into seven dimensions: (i) subjective sleep quality; (ii) sleep latency; (iii) sleep duration; (iv) habitual sleep efficiency; (v) sleep disturbances; (vi) use of sleeping medication and (vii) daytime dysfunction. Each dimension was graded on an integer score from 0 to 3, and accordingly, the PSQI score ranged from 0 to 21. Higher scores represented poorer sleep quality, and a PSQI total score > 5 defined the poor sleep quality group [6, 7, 15]. The reliability and validity of the Chinese version of PSQI were verified in previous studies in China and the Cronbach’s alpha for this scale was 0.842 [16].
Anxiety
The SAS was wildly used to assess anxiety [17]. The SAS consists of 20 self-report items on anxiety and all items are rated on a 4-point Likert scale from 1 (never) to 4 (always). A standardized scoring algorithm was used to define symptoms of anxiety, and the total score ranged from 20 to 80. Higher scores indicated higher risk of anxiety. Anxiety symptoms were defined when the total SAS score was ≥50 [18]. The reliability and validity of the Chinese version of the SAS was verified and the correlation between test and retest within a 2-week period was 0.85 [19].
Fear of negative evaluation
The adolescents’ levels of FNE were assessed by the Brief FNE Scale [20]. The BFNE is a 12-item self-reported questionnaire that assesses fear and distress related to negative evaluation from others, including eight obverse-scored items and four reverse-scored items. A 5-point Likert scale ranging from 1 (not at all a characteristic of me) to 5 (extremely a characteristic of me) was used to rate each item. High FNE was defined when the total BFNE score was >30 [21]. The BFNE demonstrated adequate internal consistency in the current sample, and the Cronbach’s alpha coefficient of the total scale was 0.813.
Statistical analysis
The Statistical Package of Social Science (SPSS 25.0) was used for data analyses. Continuous variables were presented as mean [standard deviations (SDs)] and categorical variables were presented as frequencies (percentages). For the purpose of our study, the number of confirmed COVID-19 cases in the adolescent’s city was divided into none, ≤50, 51–100 and >100. Family members or friends infected/suspected were classified as none, confirmed and suspected. The time spent using electronics every day (h/d) was classified into five groups: <1, 1–4, 5–8, 9–12 and >12. The time spent on COVID-19 information per day was grouped into <0.5, 0.5–1 and >1 h/d. The number of meals every day, self-reported diet quality and exercise time every day were divided into three levels: decreasing, unchanged and increasing. The χ2 test was used to compare the distributions of the characteristic variables between adolescents in the good with poor sleep quality groups. According to the findings of the previous studies and the established associations between sleep quality and a wide range of the collected variables [1, 2], univariate analyses were conducted to assess the associations between each of age, gender, education, being a single child, living in Hubei province, home quarantine, number of confirmed COVID-19 cases in the adolescents’ city, having a family member or a friend infected/suspected, time spent on electronics per day, time spent on COVID-19 information per day, number of meals and exercise time, self-reported eating quality, anxiety level and FNE with poor sleep quality in our sample. Variables that showed significant associations with poor sleep quality in the univariate analyses were tested in multivariable-adjusted logistic regression models. Moreover, we conducted a stratified analysis by the level of education (junior high school versus senior high school) to explore potential differences in the influence of factors associated with sleep quality during COVID-19 outbreak among younger and older adolescents. Odds ratios (ORs) and 95% confidence intervals (95% CIs) were obtained from the logistic regression models. All statistical tests were two-tailed and values of p < 0.05 were regarded as statistically significant.
RESULTS
Demographic characteristics
The socio-demographic characteristics of the recruited Chinese adolescents according to binary categories of sleep quality are shown in Table 1. None of the 10 569 recruited adolescents reported symptoms of COVID-19. The number of respondents in Hubei (the epidemic area) and other regions (including Guangdong, Guangxi and other 29 regions) were 4402 (41.7) and 6167 (58.3%), respectively. The mean age of the recruited adolescents was 15.94 ± 1.45, and 50.3% were males. During the COVID-19 pandemic, 18.6% of adolescents had a poor sleep quality (PSQI >5). There were significant differences in all the studied factors between adolescents with and without poor sleep quality (p < 0.05).
TABLE 1.
Distributions of socio-demographic characteristics according to the reported sleep quality
| Variables | Total | Good sleep quality | Poor sleep quality n = 1966 | p value |
|---|---|---|---|---|
| (n = 10 569) | n = 8603 (81.4%) | (18.6%) | ||
| Age (years) | <0.001 | |||
| <16 | 3464 (32.8) | 2937 (84.8) | 527 (15.2) | |
| ≥16 | 7105 (67.2) | 5666 (79.6) | 1439 (20.3) | |
| Gender | <0.001 | |||
| Male | 5319 (50.3) | 4460 (83.9) | 859 (16.1) | |
| Female | 5250 (49.7) | 4143 (78.9) | 1105 (21.1) | |
| Education | <0.001 | |||
| Junior high school | 2110 (20.0) | 1865 (88.4) | 245 (11.6) | |
| Senior high school | 8459 (80.0) | 6738 (79.7) | 1721 (20.3) | |
| Single child | 0.060 | |||
| No | 5168 (48.9) | 4169 (80.7) | 999 (19.3) | |
| Yes | 5401 (51.1) | 4434 (82.1) | 967 (17.9) | |
| Living in Hubei Province | <0.001 | |||
| No | 6167 (58.3) | 4916 (79.7) | 1251 (20.3) | |
| Yes | 4402 (41.7) | 3687 (83.8) | 715 (16.2) | |
| Quarantinea | 0.155 | |||
| No | 5319 (50.3) | 4358 (81.9) | 961 (18.1) | |
| Yes | 5250 (49.7) | 4245 (80.9) | 1005 (19.1) | |
| Number of COVID-19 cases in your city | <0.001 | |||
| None | 649 (6.1) | 566 (87.2) | 83 (12.8) | |
| ≤50 | 4567 (43.2) | 3677 (80.5) | 890 (19.5) | |
| 51–100 | 1732 (16.4) | 1405 (81.1) | 327 (18.9) | |
| >100 | 2441 (23.1) | 1969 (80.7) | 472 (19.3) | |
| Do not know the number of patients | 1180 (11.2) | 986 (83.6) | 194 (16.4) | |
| Family member or friend infected/ suspectedb infected | <0.001 | |||
| None | 8797 (83.2) | 7280 (82.8) | 1517 (17.2) | |
| Confirmed | 1178 (11.1) | 889 (75.5) | 289 (24.5) | |
| Suspected | 594 (5.6) | 434 (73.1) | 160 (26.9) | |
| Time spent using electronics (h/d) | <0.001 | |||
| <1 | 637 (6.0) | 589 (92.5) | 48 (7.5) | |
| 1–4 | 4212 (39.9) | 3622 (86.0) | 590 (14.0) | |
| 5–8 | 3518 (33.3) | 2850 (81.0) | 668 (19.0) | |
| 9–12 | 1578 (14.9) | 1127 (71.4) | 451 (28.6) | |
| >12 | 624 (5.9) | 415 (66.5) | 209 (33.5) | |
| Time spent on COVID-19 information (h/day) | 0.004 | |||
| <0.5 | 5032 (47.6) | 4030 (80.1) | 1002 (19.9) | |
| 0.5–1 | 4653 (44.0) | 3849 (82.7) | 804 (17.3) | |
| >1 | 884 (8.4) | 724 (81.9) | 160 (18.1) | |
| Number of meals every day | <0.001 | |||
| Decreasing | 956 (9.0) | 642 (67.2) | 314 (32.8) | |
| Unchanged | 9405 (89.0) | 7826 (83.2) | 1579 (16.8) | |
| Increasing | 208 (2.0) | 135 (64.9) | 73 (35.1) | |
| Eating quality | <0.001 | |||
| Decreasing | 1185 (11.2) | 750 (63.3) | 435 (36.7) | |
| Unchanged | 8762 (82.9) | 7354 (83.9) | 1408 (16.1) | |
| Increasing | 622 (5.9) | 499 (80.2) | 123 (19.8) | |
| Exercise time every day | <0.001 | |||
| Decreasing | 5830 (55.2) | 4522 (77.6) | 1308 (22.4) | |
| Unchanged | 3934 (37.2) | 3382 (86.0) | 552 (14.0) | |
| Increasing | 805 (7.6) | 699 (86.8) | 106 (13.2) | |
| Anxiety | <0.001 | |||
| No | 9855 (93.2) | 8367 (84.9) | 1488 (15.1) | |
| Yes | 714 (6.8) | 236 (33.1) | 478 (66.9) | |
| FNE | <0.001 | |||
| No | 2960 (28.0) | 2704 (91.4) | 256 (8.6) | |
| Yes | 7609 (72.0) | 5899 (77.5) | 1710 (22.5) |
Adolescents in junior and senior high school were forced to be quarantined at home to prevent further spread of COVID-19.
The suspected cases need to meet at least one of the epidemiological history features and two clinical manifestations or three clinical manifestations items if without a clear epidemiological history. The confirmed cases were defined as suspected case with pathogenic or serological evidence.
p value < 0.05 was statistically significant and calculated by the χ2 test and T-test.
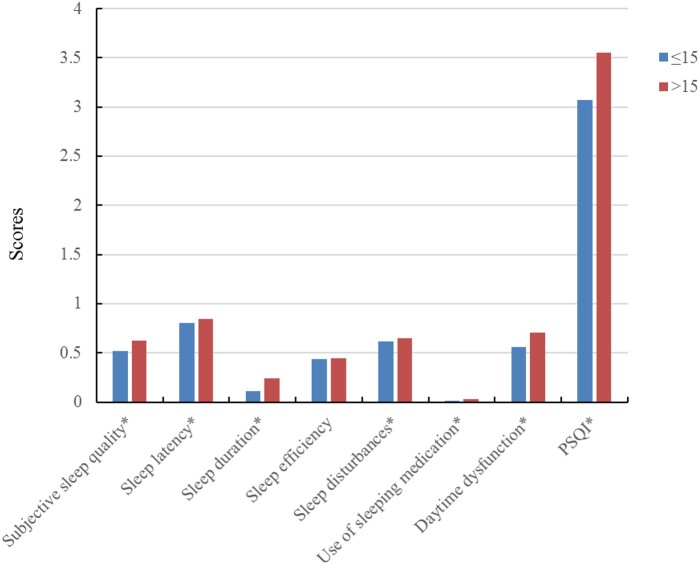
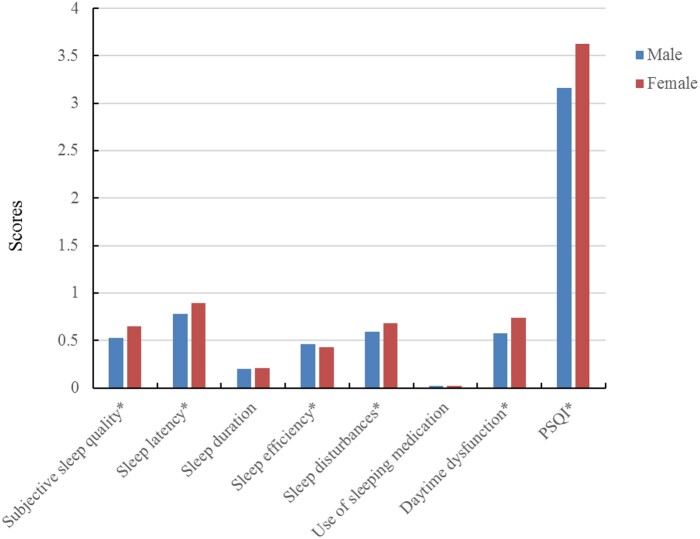
Correlations
The mean, SD and Pearson correlation coefficients of the sleep quality-related variables are shown in Table 2. The PSQI total score was significantly correlated with the scores for anxiety (r = 0.50, p < 0.01) and FNE (r = 0.36, p < 0.01). Sleep latency was the highest PSQI domain score, and the use of sleeping medication was the lowest PSQI domain score. The mean score of the PSQI was 3.39, and the detailed seven domains’ scores of sleep quality divided by age and gender are reported in Figs 2 and 3. Adolescents aged 16 years or more reported worse sleep quality, except for the sleep efficiency, compared with adolescents under 16 years. Furthermore, about the gender difference on sleep quality, females reported better performance at sleep efficiency, but worse performance at sleep quality, sleep latency, sleep disturbance, daytime dysfunction and total PSQI scores than males.
TABLE 2.
Pearson correlation analysis according to sleep quality
| Mean | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Subjective sleep quality | 0.59 | 1 | |||||||||
| Sleep latency | 0.83 | 0.50** | 1 | ||||||||
| Sleep duration | 0.20 | 0.20** | 0.11** | 1 | |||||||
| Sleep efficiency | 0.45 | 0.12** | 0.15** | 0.29** | 1 | ||||||
| Sleep disturbance | 0.64 | 0.41** | 0.34** | 0.11** | 0.08** | 1 | |||||
| Use of sleeping medication | 0.02 | 0.15** | 0.10** | 0.06** | 0.04** | 0.14** | 1 | ||||
| Daytime dysfunction | 0.66 | 0.48** | 0.32** | 0.23** | 0.03** | 0.40** | 0.13** | 1 | |||
| FNE | 36.19 | 0.30** | 0.22** | 0.12** | 0.02* | 0.27** | 0.07** | 0.37** | 1 | ||
| Anxiety | 37.30 | 0.41** | 0.31** | 0.17** | 0.15** | 0.34** | 0.17** | 0.41** | 0.30** | 1 | |
| PSQI | 3.39 | 0.74** | 0.70** | 0.44** | 0.45** | 0.61** | 0.25** | 0.69** | 0.36** | 0.50** | 1 |
p < 0.05.
p < 0.01.
FIG. 2.
The domain score of sleep quality by age. *Significant difference over different age groups (p value < 0.05).
FIG. 3.
The domain score of sleep quality by gender. *Significant difference over different gender groups (p value < 0.05).
Related factors of poor sleep quality
The independent factors of poor sleep quality are shown in Table 3. During the COVID-19 pandemic, the univariate analyses showed that being a single child and being forced to homestay during the COVID-19 pandemic were not associated with the sleep quality. Whereas, older adolescents’ age, female gender, senior high education, increasing number of COVID-19 cases in the city, having a suspected or infected family member of COVID-19, the increasing daily hours spent using electronics, having anxiety and FNE were positively associated with poor sleep quality. On the other hand, living in Hubei province, the increasing daily hours spent following or searching for COVID-19 information, unchanged number of daily meals, unchanged or increased eating quality and unchanged or increased daily exercise time were inversely associated with poor sleep quality. In the multivariable-adjusted models, being a female, as well as a senior school student, were both associated with higher risk of poor sleep quality (OR : 1.228, 95% CI: 1.153–1.435 and OR : 1.533, 95% CI: 1.237–1.902). Living in Hubei Province was negatively correlated with poor sleep quality (OR: 0.826, 95% CI: 0.723–0.944). Adolescents with family member or friend infected or suspected to be infected with the new virus were more likely to have poor sleep quality (OR: 1.327, 95% CI: 1.124–1.566 for confirmed infection and 1.454; 95% CI: 1.176–1.796 for suspected infection). The OR of having poor sleep quality increased with time spent on electronics in a dose–response pattern reaching an (OR: 3.08, 95% CI: 2.492–5.223 for >12 vs. <1 h/d). Time spent on COVID-19 information per day was inversely associated with the poor sleep quality (OR: 0.774, 95% CI: 0.627–0.957 for >1 h/d vs. <0.5 h/d). In reference to adolescents with decreased diet quality, those who kept their diet quality unchanged and those who increased it, during the pandemic, had ORs (95% CIs) for poor sleep quality = 0.541 (0.463–0.632) and 0.523 (0.401–0.682), respectively. In addition, the higher category of the dichotomized anxiety score (OR: 8.269, 95% CI: 6.883–9.935) and the FNE (OR: 2.834, 95% CI: 2.341–3.430) were significantly associated with the odds of having poor sleep quality.
TABLE 3.
Univariate and adjusted logistic regression analysis of factors influencing the poor sleep quality
| Variables | Univariate OR (95% CI) | p value | Adjusted ORa (95% CI) | p value |
|---|---|---|---|---|
| Age (years) | ||||
| <16 | 1.00 | 1.00 | ||
| ≥16 | 1.415 (1.269–1.579) | <0.001 | 1.002 (0.861–1.165) | 0.983 |
| Gender | ||||
| Male | 1.00 | 1.00 | ||
| Female | 1.387 (1.257–1.531) | <0.001 | 1.286 (1.153–1.435) | <0.001 |
| Education | ||||
| Junior high school | 1.00 | 1.00 | ||
| Senior high school | 1.944 (1.685–2.244) | <0.001 | 1.533 (1.237–1.902) | <0.001 |
| Single child | ||||
| No | 1 | 1.00 | ||
| Yes | 0.910 (0.825–1.004) | 0.060 | 0.912 (0.814–1.022) | 0.114 |
| Living in Hubei Province | ||||
| No | 1.00 | 1.00 | ||
| Yes | 0.762 (0.689–0.843) | <0.001 | 0.826 (0.723–0.944) | 0.005 |
| Quarantine | ||||
| No | 1.00 | |||
| Yes | 1.074 (0.973–1.184) | 0.155 | 0.981 (0.881–1.094) | 0.734 |
| Number of COVID-19 cases in your city | ||||
| None | 1.00 | 1.00 | ||
| ≤50 | 1.651 (1.296–2.102) | <0.001 | 1.226 (0.944–1.591) | 0.126 |
| 51–100 | 1.587 (1.224–2.058) | <0.001 | 1.205 (0.909–1.596) | 0.195 |
| >100 | 1.635 (1.271–2.102) | <0.001 | 1.284 (0.971–1.698) | 0.080 |
| Family member or friend infected/suspected | ||||
| None | 1.00 | 1.00 | ||
| Confirmed | 1.560 (1.351–1.801) | <0.001 | 1.327 (1.124–1.566) | 0.001 |
| Suspected | 1.769 (1.464–2.138) | <0.001 | 1.454 (1.176–1.796) | 0.001 |
| Time spent using electronics (h/d) | ||||
| <1 | 1.00 | 1.00 | ||
| 1–4 | 1.999 (1.471–2.717) | <0.001 | 1.899 (1.367–2.639) | <0.001 |
| 5–8 | 2.876 (2.118–3.906) | <0.001 | 2.417 (1.738–3.361) | <0.001 |
| 9–12 | 4.911 (3.588–6.721) | <0.001 | 3.490 (2.484–4.903) | <0.001 |
| >12 | 6.180 (4.408–8.664) | <0.001 | 3.608 (2.492–5.223) | <0.001 |
| Time spent on COVID-19 information (h/d) | ||||
| <0.5 | 1.00 | 1.00 | ||
| 0.5–1 | 0.840 (0.758–0.931) | 0.001 | 0.887 (0.792–0.994) | 0.039 |
| >1 | 0.889 (0.739–1.069) | 0.211 | 0.774 (0.627–0.957) | 0.018 |
| Number of meals every day | ||||
| Decreasing | 1.00 | 1.00 | ||
| Unchanged | 0.413 (0.357–0.477) | <0.001 | 0.653 (0.549–0.776) | <0.001 |
| Increasing | 1.106 (0.807–1.515) | 0.532 | 1.308 (0.904–1.893) | 0.155 |
| Eating quality | ||||
| Decreasing | 1.00 | 1.00 | ||
| Unchanged | 0.330 (0.290–0.376) | <0.001 | 0.541 (0.463–0.632) | <0.001 |
| Increasing | 0.250 (0.338–0.536) | <0.001 | 0.523 (0.401–0.682) | <0.001 |
| Exercise time every day | ||||
| Decreasing | 1.00 | 1.00 | ||
| Unchanged | 0.564 (0.506–0.629) | <0.001 | 0.773 (0.685–0.873) | <0.001 |
| Increasing | 0.524 (0.424–0.490) | <0.001 | 0.792 (0.626–1.002) | 0.052 |
| Anxiety | ||||
| No | 1.00 | 1.00 | ||
| Yes | 11.389 (9.653–13.437) | <0.001 | 8.269 (6.883–9.935) | <0.001 |
| FNE | ||||
| No | 1.00 | 1.00 | ||
| Yes | 3.062 (2.664–3.518) | <0.001 | 2.834 (2.341–3.430) | <0.001 |
OR, Odds ratio; CI, confidence interval.
Adjusted ORs were derived from a logistic regression model included the significant factors in univariate analyses where p values <0.05 indicated statistical significance.
Related factors of sleep quality stratified by education
Factors which associated with poor sleep quality among Chinese adolescents varied by the education level as shown in Table 4. Among senior high school students, all the studied factors, except for the number of COVID-19 cases in the city were associated with poor sleep quality. While among Junior high school students, the number of COVID-19 cases in the city besides female gender, suspected COVID-19 in family members or friends and diet-related factors were associated with poor sleep quality. Anxiety and FNE were associated with poor sleep quality in both levels of education.
TABLE 4.
Stratified analyses of factors influencing the poor sleep quality by education level
| Variables | Junior high school |
Senior high school |
||
|---|---|---|---|---|
| Univariate OR (95% CI) | p value | Adjusted ORa (95% CI) | p value | |
| Gender | ||||
| Male | 1.00 | 1.00 | ||
| Female | 1.501 (1.110–2.031) | <0.001 | 1.225 (1.087–1.381) | 0.001 |
| Single child | ||||
| No | 1.00 | 1.00 | ||
| Yes | 1.058 (0.774–1.446) | 0.724 | 0.889 (0.785–1.007) | 0.065 |
| Living in Hubei Province | ||||
| No | 1.00 | 1.00 | ||
| Yes | 1.037 (0.665–1.618) | 0.871 | 0.851 (0.737–0.982) | 0.027 |
| Quarantine | ||||
| No | 1.00 | 1.00 | ||
| Yes | 0.946 (0.702–1.274) | 0.713 | 0.975 (0.866–1.097) | 0.674 |
| Number of COVID-19 cases in your city | ||||
| None | 1.00 | 1.00 | ||
| ≤50 | 3.515 (1.144–10.796) | 0.028 | 1.064 (0.793–1.427) | 0.679 |
| 51–100 | 4.322 (1.304–14.327) | 0.017 | 1.153 (0.854–1.556) | 0.353 |
| >100 | 2.941 (0.974–8.879) | 0.056 | 1.071 (0.781,1.467) | 0.671 |
| Family member or friend infected/suspected | ||||
| None | 1.00 | 1.00 | ||
| Confirmed | 1.301 (0.879–1.926) | 0.188 | 1.295 (1.073–1.564) | 0.007 |
| Suspected | 1.675 (1.007–2.787) | 0.047 | 1.374 (1.084–1.741) | 0.009 |
| Time spent using electronics (h/d) | ||||
| <1 | 1.00 | 1.00 | ||
| 1–4 | 1.506 (0.823–2.755) | 0.184 | 2.092 (1.400–3.128) | <0.001 |
| 5–8 | 1.533 (0.816–2.879) | 0.184 | 2.656 (1.778–3.966) | <0.001 |
| 9–12 | 1.767 (0.854–3.659) | 0.125 | 3.782 (2.512–5.695) | <0.001 |
| >12 | 1.071 (0.393–2.920) | 0.893 | 3.623 (2.339–5.610) | <0.001 |
| Time spent on COVID-19 information (h/d) | ||||
| <0.5 | 1.00 | 1.00 | ||
| 0.5–1 | 0.929 (0.672–1.284) | 0.655 | 0.905 (0.800–1.024) | 0.113 |
| >1 | 1.157 (0.721–1.856) | 0.546 | 0.747 (0.586–0.952) | 0.018 |
| Number of meals every day | ||||
| Decreasing | 1.00 | 1.00 | ||
| Unchanged | 0.441 (0.293–0.665) | <0.001 | 0.740 (0.609–0.900) | 0.000 |
| Increasing | 1.407 (0.583–3.393) | 0.447 | 1.314 (0.868–1.988) | 0.193 |
| Diet quality | ||||
| Decreasing | 1.00 | 1.00 | ||
| Unchanged | 0.653 (0.424–1.004) | 0.052 | 0.541 (0.456–0.641) | <0.001 |
| Increasing | 0.932 (0.473–1.835) | 0.838 | 0.482 (0.359–0.648) | <0.001 |
| Exercise time every day | ||||
| Decreasing | 1.00 | 1.00 | ||
| Unchanged | 0.901 (0.644–1.262) | 0.545 | 0.773 (0.678–0.881) | <0.001 |
| Increasing | 0.723 (0.449–1.163) | 0.181 | 0.790 (0.598–1.044) | 0.098 |
| Anxiety | ||||
| No | 1.00 | 1.00 | ||
| Yes | 8.373 (5.082–13.796) | <0.001 | 6.854 (5.598–8.390) | <0.001 |
| FNE | ||||
| No | 1.00 | 1.00 | ||
| Yes | 1.075 (1.054–1095) | <0.001 | 1.064 (1.056–1.072) | <0.001 |
OR, Odds ratio; CI, confidence interval.
Adjusted ORs were derived from a logistic regression model included the significant factors in univariate analyses where p values <0.05 indicated statistical significance.
DISCUSSIONS
The prevalence of poor sleep quality among Chinese adolescents in junior and senior high schools during the COVID-19 pandemic period was 18.6%, and the overall average score of PSQI was 3.39. Factors that were positively associated with poor sleep quality included older age, female gender, senior high education, having an infected/suspected family member or a friend, time spent using electronics every day, anxiety and FNE; while living in Hubei province, time spent on COVID-19 information, improving diet and increasing daily exercise time were inversely associated with poor sleep quality. Our findings provided a data support for an accurate understanding about the Chinese adolescents’ sleep quality during COVID-19 outbreak.
Factors associated with poor sleep quality
Females were more likely to have poor sleep quality than males during the COVID-19 outbreak, which was consistent with findings of an earlier study [6]. Anxiety and FNE scores were strongly correlated with scores of the seven dimensions of PSQI in our study (subjective sleep quality, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbances, use of sleeping medication and daytime dysfunction) indicating an association between sleep quality and mental health issues [2, 22]. Recent studies have suggested that the public level of anxiety-related symptoms increased when a major infectious disease occurred such as in SARS [23] and COVID-19 [24]. As sleep quality is sensitive to psychological status, and with the prevalent symptoms of anxiety and depression during the COVID-19 pandemic [25], many people had suffered from poor sleep quality [6, 7, 24]. The current study showed that adolescents in junior and senior high schools with anxiety and FNE had approximately eight and three times, respectively, poor sleep quality rate compared with those without anxiety and FNE (p < 0.05).
In addition, adolescents with a family member or a friend infected or suspected to be infected with COVID-19 were more likely to develop poor sleep quality. The presence of nearby infected relatives or friends could have led to experience more anxiety and negative emotions, which can affect the sleep quality of the young individuals of the family [24, 26]. The COVID-19 has disrupted the normal learning and living conditions of the adolescent students and affected their sleep quality. Due to the outbreak of COVID-19, a large number of students had to apply social distancing or forced to isolate at home. This has led to more spare time to use various electronic devices and to stay awake later than usual. Staying awake for late or midnight time could change the circadian rhythm and slow the homeostatic sleep drive accumulation, which may lead to the decline of sleep quality in those adolescents [27].
Factors associated with good sleep quality
The average time spent focusing on the COVID-19 outbreak news was found inversely associated with poor sleep quality. This result may be explained by the fact that the time of monitoring COVID-19 news could have provided the adolescents by the necessary information; such as facts, inflection data and government measures which could have reduced their fears and anxiety and led to the better quality of sleep [28]. It is somewhat surprising that adolescents living in Hubei province, where the first COVID-19 case was detected, showed a better sleep quality than adolescents in other provinces. This could be attributed to the adequate medical resources and online psychological counselling services provided by the Chinese government to the Hubei residents [29, 30]. The results of study showed an interesting phenomenon that adolescents were more likely to get a good sleep when their physical activity levels improved or did change during the pandemic. Therefore, we recommend governments to encourage young individuals to practice more indoor exercise during epidemics. In our study, more than 80% of adolescents have not changed the number of daily meals or their diet quality. Adolescents who did not change their frequency of eating or decreased the quality of their diet were more likely to get a good sleep. A growing body of evidence also supports the idea that properly controlled diets can have an impact on circadian rhythms and sleep [31, 32].
Stratified analysis by the education level
Age was positively associated with poor sleep quality in our sample of Chinese adolescents, which could be reflecting the effect of the stage of education. Of note, 20.3% of senior high school students, compared with 11.6% junior high school students, had a poor sleep quality during the COVID-19 pandemic. All the studied factors showed strong associations with poor sleep quality among senior rather than junior high school students. Senior high school students have heavier academic burdens, and being not able to attend school regularly with the potentiality to face the university entrance exam during the COVID-19 outbreak may have resulted in more anxiety and worries about their chances of getting into college, which could be triggers for decreased sleep quality [6, 7, 9, 11].
Strengths and limitations
This cross-sectional study has provided a comprehensive insight into factors associated with sleep quality of junior and senior high school adolescents during the COVID-19 pandemic in China. We used validated scales to assess the dependent and independent variables under the study. Moreover, we provided stratified analyses by the education level to assess the potential impact of the stage of education on the adolescents’ sleep pattern response to varied factors during the COVID-19 pandemic.
The study limitations include the difficulty to deduce causal associations between the outcome and exposure variables because of the cross-sectional nature of this study. However, some factors such as anxiety, FNE and increasing time spent using electronics showed consistent strong associations in the adjusted and stratified models which suggest a potential cause–effect association. To further explore the temporal relationship between the outcome and exposure variables, we are considering to conduct a case–control study whenever the data are available. Second, the prevalence of poor sleep quality may be over-or under-estimated, and the indicated levels of sleep quality may not always be consistent with the evaluations of mental health professionals, since the study was conducted by self-reports from only one source. Third, due to the impact of COVID-19 pandemic, we conducted the survey of this study by online questionnaire rather than face-to-face investigation, which may bear certain deviation in the response population, especially with the use of convenience sampling. This was obvious for the differences in the age strata proportions; adolescents aged ≥16 accounted for a relatively large proportion, and age matching should be carried out in future studies. Therefore, the findings of the study should be cautiously applied to sleep problems among national adolescents.
CONCLUSIONS
During the COVID-19 pandemic, poor sleep quality was prevalent in junior and senior high school adolescents in China. A variety of demographic and geopolitical factors detected to influence the adolescents’ sleep quality. Sleep support is important for managing the COVID-19 emergency and improving sleep quality, and even is helpful to protect the adolescents’ physical health. Therefore, more attention should be paid to sleep quality among adolescents and be ensured that they get enough rest and sleep time. Also, in order to protect the adolescents’ mental and physical health, more interventions in reducing COVID-19-caused anxiety and promoting healthy sleep habits are recommended.
ACKNOWLEDGEMENTS
The authors thank all people who helped in the data collection through the Wenjuanxing platform (https://www.wjx.cn/). The authors thank all the participants for their time and efforts. The authors thank our colleagues from Osaka University Center of Medical Data Science, Advanced Clinical Epidemiology Investigator’s Research Project for providing their insight and expertise for our research.
FUNDING
This study was supported by the National Social Science Fund of China in 2015 [grant number: 15BSH057].
DATA AVAILABILITY
The data that support the findings of this study are available upon request, Prof. Bing Xiang (397126318@qq.com).
REFERENCES
- 1.Kaur H, Bhoday HS.. Changing adolescent sleep patterns: factors affecting them and the related problems. J Assoc Physicians India 2017;65:73–7. [PubMed] [Google Scholar]
- 2.Gomes GC, Passos MHPD, Silva HA, et al. Sleep quality and its association with psychological symptoms in adolescent athletes. Rev Paul Pediatr 2017;35:316–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Şimşek Y, Tekgül N.. Sleep quality in adolescents in relation to age and sleep related habitual and environmental factors. J Paediatr Res 2019;6:307–13. [Google Scholar]
- 4.Xu Z, Su H, Zou Y, et al. Sleep quality of Chinese adolescents: distribution and its associated factors. J Paediatr Child Health 2012;48:138–45. [DOI] [PubMed] [Google Scholar]
- 5.Zhou Y, Guo L, Lu CY, et al. Bullying as a risk for poor sleep quality among high school students in China. PLoS One 2015;10:e0121602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhou SJ, Wang LL, Yang R, et al. Sleep problems among Chinese adolescents and young adults during the coronavirus-2019 pandemic. Sleep Med 2020;74:39–47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Filho G, Genta PR.. COVID-19 pandemic impact on sleep habits, chronotype and health-related quality of life among high school students: a longitudinal study. J Clin Sleep Med 2021. (Epub ahead of print, 5 March 2021). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ahmed MZ, Ahmed O, Aibao Z, et al. Epidemic of COVID-19 in China and associated psychological problems. Asian J Psychiatr 2020;51:102092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cao W, Fang Z, Hou G, et al. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res 2020;287:112934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wang Y, Di Y, Ye J, et al. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol Health Med 2021;26:13–22. [DOI] [PubMed] [Google Scholar]
- 11.Isumi A, Doi S, Yamaoka Y, et al. Do suicide rates in children and adolescents change during school closure in Japan? The acute effect of the first wave of COVID-19 pandemic on child and adolescent mental health. Child Abuse Negl 2020;110:104680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wang F, Cao J, Yu Y, et al. Epidemiological characteristics of patients with severe COVID-19 infection in Wuhan, China: evidence from a retrospective observational study. Int J Epidemiol 2021;49:1940–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yang Y, Zhu JF, Yang SY, et al. Prevalence and associated factors of poor sleep quality among Chinese returning workers during the COVID-19 pandemic. Sleep Med 2020;73:47–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wang LQ, Zhang M, Liu GM, et al. Psychological impact of coronavirus disease (2019) (COVID-19) epidemic on medical staff in different posts in China: a multicenter study. J Psychiatr Res 2020;129:198–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Buysse DJ, Reynolds CF 3rd, Monk TH, et al. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 1989;28:193–213. [DOI] [PubMed] [Google Scholar]
- 16.Liu XC, Tang MQ, Hu L, et al. Reliability and validity of the Pittsburgh sleep quality index. Chin J Psychiat 1996;29:103e7. [Google Scholar]
- 17.Zung WW.A rating instrument for anxiety disorders. Psychosomatics 1971;12:371–9. [DOI] [PubMed] [Google Scholar]
- 18.Liu CY, Yang YZ, Zhang XM, et al. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: a cross-sectional survey. Epidemiol Infect 2020;148:e98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liu XC, Oda S, Peng X, et al. Life events and anxiety in Chinese medical students. Soc Psychiatry Psychiatr Epidemiol 1997;32:63–7. [DOI] [PubMed] [Google Scholar]
- 20.Leary MR.A brief version of the fear of negative evaluation scale. Pers Soc Psychol Bull 1983;9:371–5. [Google Scholar]
- 21.Yuke LI, Zhiqiang YAO.. Influence of college students’ fear of negative evaluation on social anxiety: moderating effect of self-concept clarity. Health Res 2020;40:288–92. [Google Scholar]
- 22.Zhang WJ, Yan C, Shum D, et al. Responses to academic stress mediate the association between sleep difficulties and depressive/anxiety symptoms in Chinese adolescents. J Affect Disord 2020;263:89–98. [DOI] [PubMed] [Google Scholar]
- 23.Su TP, Lien TC, Yang CY, et al. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: a prospective and periodic assessment study in Taiwan. J Psychiatr Res 2007;41:119–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Huang Y, Zhao N.. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatry Res 2020;288:112954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Wang C, Pan R, Wan X, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID19) epidemic among the general population in China. Int J Environ Res Publ Health 2020;17:1729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Qianwei LIU, Guozhen ZHAO, Bo JI, et al. Analysis of the influence of the psychology changes of fear induced by the COVID-19 epidemic on the body. World J Acupunct Moxibustion 2020;6:7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Jenni OG, Carskadon MA.. Sleep behavior and sleep regulation from infancy through adolescence: normative aspects. Sleep Med Clin 2007;2:321–9. [Google Scholar]
- 28.Wang XL, Gao LY, Miu QF.. et al. Perceived uncertainty stress and its predictors among residents in China during the COVID-19 pandemic. Psychol Health Med 2021;1–15. [DOI] [PubMed] [Google Scholar]
- 29.Entire nation mobilizes to help Wuhan. Beijing: National Health Commission of the People’s Republic of China. 2020. http://en.nhc.gov.cn/2020-02/27/c_77008.htm (19 October 2020, date last accessed).
- 30.Hu S, He B, shi C.. Practical Handbook of Psychological Intervention Related to Coronavirus Disease 2019. China: Zhejiang University Press, 2020. [Google Scholar]
- 31.Paoli A, Tinsley G, Bianco A, et al. The influence of meal frequency and timing on health in humans: the role of fasting. Nutrients 2019;11:719. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Berendsen M, Boss M, Smits M, et al. Chrono-nutrition and diet quality in adolescents with delayed sleep–wake phase disorder. Nutrients 2020;12:539. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available upon request, Prof. Bing Xiang (397126318@qq.com).