Accepted
Background
In early 2020, Ecuador reported one of the highest surges of per capita deaths across the globe.
Methods
We collected a comprehensive dataset containing individual death records between 2015 and 2020, from the Ecuadorian National Institute of Statistics and Census and the Ecuadorian Ministry of Government. We computed the number of excess deaths across time, geographical locations and demographic groups using Poisson regression methods.
Results
Between 1 January and 23 September 2020, the number of excess deaths in Ecuador was 36 402 [95% confidence interval (CI): 35 762–36 827] or 208 per 100 000 people, which is 171% of the expected deaths in that period in a typical year. Only 20% of the excess deaths are attributable to confirmed COVID-19 deaths. Strikingly, in provinces that were most affected by COVID-19 such as Guayas and Santa Elena, the all-cause deaths are more than double the expected number of deaths that would have occurred in a normal year. The extent of excess deaths in men is higher than in women, and the number of excess deaths increases with age. Indigenous populations had the highest level of excess deaths among all ethnic groups.
Conclusions
Overall, the exceptionally high level of excess deaths in Ecuador highlights the enormous burden and heterogeneous impact of COVID-19 on mortality, especially in older age groups and Indigenous populations in Ecuador, which was not fully revealed by COVID-19 death counts. Together with the limited testing in Ecuador, our results suggest that the majority of the excess deaths were likely to be undocumented COVID-19 deaths.
Keywords: Excess deaths, Ecuador, COVID-19
Key Messages.
Between 1 January and 23 September, 2020, the number of excess deaths in Ecuador was 208 per 100 000 people, which is 171% of the expected deaths in that period in a typical year.
Only 20% of the excess deaths are attributable to confirmed COVID-19 deaths.
The extent of excess deaths in men is higher than in women, and the number of excess deaths increases with age.
Indigenous populations had the highest level of excess deaths among all ethnic groups.
Strict non-pharmaceutical interventions in April 2020 likely prevented further heavy burden on mortality.
Introduction
The coronavirus disease 2019 (COVID-19) pandemic has caused high morbidity and mortality across the globe. The total number of confirmed COVID-19 deaths is approximately 1.8 million by the end of 2020.1 However, this number only partially reflects the total burden of COVID-19 on mortality, because it does not include undocumented COVID-19 deaths or other causes of deaths due to societal disruptions. A more accurate measure of the burden of COVID-19 on mortality is therefore the excess deaths,2,3 i.e. the number of all-cause deaths exceeding the expected number of deaths in a typical year without COVID-19. This measure is especially relevant for countries where testing capacity is limited, such as Ecuador,4 which may lead to substantial under-reporting of COVID-19 cases and deaths.
Excess deaths in 2020 have been formally estimated previously for many high-income countries with high COVID-19 cases, including the USA,5–8 England and Wales,9 Italy,10,11 and middle-income countries such as Brazil.12 The numbers of all-cause deaths range between 120% and 131% of expected deaths in these countries, i.e. between 20% and 31% of excess deaths, highlighting the heavy burden of COVID-19 spread directly on mortality, despite differences in demographics, social mixing patterns and health care systems. In these countries, a major fraction of excess deaths (between 67% to 80%) are attributable to COVID-19 deaths,5,8,9,11 suggesting that the majority of excess deaths are caused directly by COVID-19 infections. In contrast, Ecuador reported a relatively small number of COVID-19 deaths13; however, a surprisingly large number of excess deaths was reported in the Our World in Data online database,13 in a newspaper during early COVID-19 outbreak in April 202014 and more recently in a study.15 This raises the questions about how the excess deaths vary temporally, spatially and demographically and how they are related to COVID-19 spread in Ecuador.
Here, by analysing a rich dataset containing death records from Ecuador during 2015–20, we provide a comprehensive analysis of the spatial, temporal and demographic patterns of excess all-cause deaths in Ecuador between 1 January and 23 September, 2020. We show that the extent of excess deaths in Ecuador is several folds higher than in many countries severely affected by COVID-19. In addition, we found that the spatial, temporal and demographic pattern of excess deaths reveal a much more severe early burden of COVID-19 in Ecuador and a more complex spaciotemporal distribution of COVID-19 deaths than is apparent in the official death reports.
Methods
Ethics committee approval was obtained from the Ecuadorian Ministry of Public Health. The analysis by Los Alamos National Laboratory team was approved by that institution’s IRB.
Data
Death records from 2015–19 for all-cause mortality were obtained from the Ecuadorian National Institute of Statistics and Census. The records include age, sex and ethnicity of the deceased, place of death registration, residence and the International Classification of Disease (ICD) code for the cause of death. The Ecuadorian Ministry of Government provided death records from 1 January to 26 September 2020, containing sex, age and registration and residence location by parish, canton and province, but without the cause of death. We report estimates during the study period from 1 January to 23 September 2020. There are 24 provinces in Ecuador. We ignore the three smaller ‘Not Delimited Areas’ located along various provinces' borders. We use the 2020 population estimates from the INEC (the Ecuadorian National Institute of Statistics and Census).
Individual records of COVID-19 incidence, deaths and testing for Ecuador were obtained from the Ecuadorian Ministry of Public Health. All records were aggregated at the weekly level and binned by sex, age group and province.
Statistical methodology
To estimate the expected number of deaths in the absence of COVID-19, we fitted a Poisson regression to the binned weekly death counts from 2015 to 2019. The regression predicts the number of weekly deaths as a function of the week of the year, to account for annual variations, the province and deceased demographics (sex and age group). Since the 2020 death records have ethnicity up to 30 July, we fitted a second model adding ethnicity as a covariate. We defined the excess death factor (EDF) as the ratio of 2020 observed deaths over the expected deaths. See Supplementary Materials, available as Supplementary data at IJE online, for details of the statistical model and the calculation of 95% confidence intervals for the number of deaths. Our model did not incorporate reporting delay in death records; this is because Ecuador has strict regulations concerning the filing of death reports, which leads to minimal delays in reporting (see Supplementary Materials). We estimated that under normal circumstances, the delay in death reporting is negligible, i.e. reporting rate is >90% on average after 1 week of deaths (Supplementary Figure S1, available as Supplementary data at IJE online).
Results
Excess deaths at the country level
We first predicted the expected number of all-cause deaths between 1 January and 23 September 2020 using a Poisson regression model fitted to deaths data collected between 2015 and 2019 (Supplementary Figure S2, available as Supplementary data at IJE online, and Methods and Supplementary Materials, available as Supplementary data at IJE online). We estimated that the expected number of all-cause deaths up to 23 September, 2020 is 51 360 [95% confidence interval (CI): 50 935–52 000]. The number of reported total all-cause deaths during this period is 87 762, leading to the number of excess deaths of 36 402, i.e. 71% higher than expected (Table 1). This is in stark contrast to the percentages estimated for the USA (20% of excess deaths),5,8 England and Wales (31%)9 and Brazil (22%),12 and similar to the estimate for Mexico (61%).16 Normalized by the population size of Ecuador in 2020 [i.e. 17 468 736 according to the INEC (the Ecuadorian National Institute of Statistics and Census)], the number of total all-cause deaths is 502 per 100 000 people. The number of excess deaths is 208 per 100 000 people, i.e. almost 3-fold higher than the estimate for the USA (72 per 100 000 people).5
Table 1.
Mortality and estimated excess deaths between 1 January and 23 September, 2020
| Jurisdiction | Expected deaths | Observed deaths | Excess death | EDFa | Mortality per 100 000 | COVID-19 deaths | Excess deaths attributed to COVID-19 deaths % |
|---|---|---|---|---|---|---|---|
| (95% CI) | (95% CI) | ||||||
| Ecuador | 51 360 | 87 762 | 36 402 | 1.71 | 502 | 7410 | 20 |
| (51 162–51 557) | (36 205–36 600) | ||||||
| Azuay | 2844 (2809–2879) | 3582 | 738 (703–773) | 1.26 | 406 | 177 | 24 |
| Bolivar | 596 (579–613) | 816 | 220 (203–237) | 1.37 | 389 | 47 | 21 |
| Cañar | 778 (759–797) | 1061 | 283 (264–302) | 1.37 | 377 | 61 | 22 |
| Carchi | 497 (483–512) | 674 | 177 (162–191) | 1.36 | 361 | 79 | 45 |
| Chimborazo | 1710 (1682–1739) | 2556 | 846 (817–874) | 1.50 | 488 | 288 | 34 |
| Cotopaxi | 1251 (1226–1277) | 1840 | 589 (563–614) | 1.47 | 376 | 213 | 36 |
| El Oro | 2088 (2056–2120) | 3800 | 1712 | 1.82 | 531 | 399 | 23 |
| (1680–1744) | |||||||
| Esmeraldas | 1153 (1129–1176) | 1625 | 472 (449–496) | 1.41 | 252 | 186 | 39 |
| Galapagos | 34 (30–38) | 35 | 1 (−3–5) | 1.02 | 106 | 0 | 0 |
| Guayas | 14 882 | 31 154 | 16 272 | 2.09 | 710 | 1689 | 10 |
| (14 785–14 977) | (16 177–16 369) | ||||||
| Imbabura | 1414 (1388–1441) | 1930 | 516 (489–542) | 1.36 | 405 | 118 | 23 |
| Loja | 1688 (1660–1717) | 2093 | 405 (376–433) | 1.24 | 402 | 198 | 49 |
| Los Rios | 2548 (2514–2583) | 3842 | 1294 | 1.51 | 417 | 344 | 27 |
| (1259–1328) | |||||||
| Manabi | 4660 (4597–4725) | 7671 | 3011 | 1.65 | 491 | 877 | 29 |
| (2946–3074) | |||||||
| Morona Santiago | 347 (335–360) | 453 | 106 (93–118) | 1.30 | 230 | 15 | 14 |
| Napo | 262 (251–273) | 406 | 144 (133–155) | 1.55 | 304 | 75 | 52 |
| Orellana | 284 (272–295) | 409 | 125 (114–137) | 1.44 | 254 | 42 | 34 |
| Pastaza | 217 (206–228) | 310 | 93 (82–104) | 1.43 | 271 | 52 | 56 |
| Pichincha | 9137 (9064–9212) | 14 614 | 5477 | 1.60 | 453 | 1402 | 26 |
| (5402–5550) | |||||||
| Santa Elena | 934 (914–954) | 2398 | 1464 | 2.57 | 598 | 365 | 25 |
| (1444–1484) | |||||||
| Santo Domingo de Los Tsachilas | 1457 (1431–1483) | 2419 | 962 (936–988) | 1.66 | 527 | 407 | 42 |
| Sucumbios | 430 (416–444) | 684 | 254 (240–268) | 1.59 | 297 | 88 | 35 |
| Tungurahua | 1973 (1941–2004) | 3117 | 1144 | 1.58 | 528 | 248 | 22 |
| (1113–1176) | |||||||
| Zamora Chinchipe | 176 (167–185) | 273 | 97 (88–106) | 1.55 | 227 | 40 | 41 |
EDF: excess death factor. It is defined as the ratio between the number of observed deaths over the number of predicted deaths without COVID-19 .
Up to 23 September 2020, there were 7410 officially reported COVID-19 deaths in Ecuador, which only account for 20% of the total all-cause excess deaths (36 402). This is a much lower percentage than those reported in countries such as the USA (67%)5,8 and England and Wales (87%).9
Time series of the total all-cause deaths suggest that the number of reported deaths started to become higher than expected in mid-March 2020, shortly after the first COVID-19 case was confirmed in Ecuador on 29 February 2020 (Figure 1). There exist two waves of excess deaths, i.e. a first major wave between late March and April and a second minor wave between July and early August (Figure 1). The first wave started in the week of 11–17 March. The number of excess deaths increased extremely rapidly and reached the highest level, i.e. 33 per 100 000 people per week (or a total of 7133 deaths per week; see Supplementary Figure S3, available as Supplementary data at IJE online) in the first week of April. Remarkably, this is over five times the number of expected deaths per week (Supplementary Figure S3). The number of weekly excess deaths declined afterwards to approximately 5 per 100 000 people per week (Supplementary Figure S3). This rapid decline coincides with the period of strict lockdown implemented by the Ecuador government.17
Figure 1.
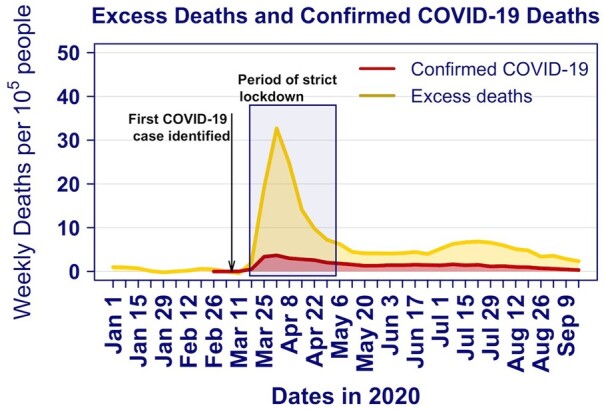
Time series for excess deaths (yellow; lighter colour) and documented COVID-19 deaths (red; darker colour) per 100 000 people in Ecuador. The period of strict national lockdown by the Ecuador government (shaded area) is taken from the Oxford COVID-19 Government Response Tracker17
The second wave occurred in July and early August, a period after strict lockdowns were gradually phased out. The number of weekly per capita deaths ranges between 5 and 8 per 100 000 people or total weekly deaths between 2200 and 2500 (Figure 1; and Supplementary Figure S3). These numbers are between 170% and 190% of the expected number of deaths.
Excess deaths by sex and age and ethnicity
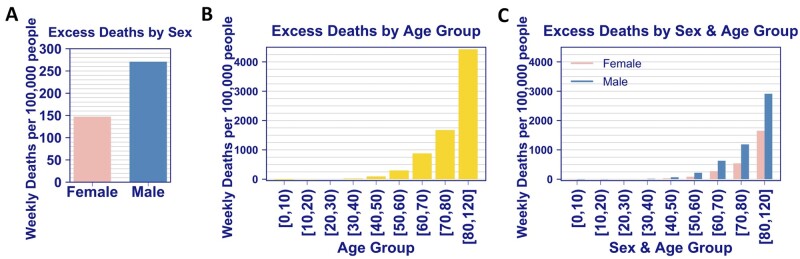
We estimate that over the entire observational period, excess deaths were higher in men than women, i.e. 271 and 147 excess deaths per 100 000 people for men and women, respectively (Figure 2A). The observed deaths in men were 183% of expected levels, compared to 156% for women (Supplementary Figure S4A, available as Supplementary data at IJE online). Deaths were significantly elevated for all age groups greater than 40 years old, with the number exponentially increasing with age group (Figure 2B). Across all age groups greater than 40 years old, more men died than women (Figure 2C). Interestingly, we found that the numbers of deaths were 27% and 22% lower than expected for age groups between 0 and 9 years and between 10 and 19 years, respectively (Supplementary Figure S4B). A slight decrease of mortality in children has been observed in England.18 One possible explanation is that the social distancing and restrictions during the pandemic may be protective for children from accidental death.
Figure 2.
Excess deaths per 100 000 people by sex (A), by age group (B) and by sex and age group (C) in Ecuador. The numbers of excess deaths are normalized by the population size in each group
The sex and age characteristics in excess deaths are in line with the demographic characteristics of the risk of COVID-19 mortality.19 The fact that the number of reported COVID-19 deaths only account for 20% of the total all-cause deaths suggests that a large fraction of COVID-19 deaths are undocumented, as a result of lack of COVID-19 testing.4 To corroborate this hypothesis, we obtained COVID-19 testing and diagnoses data from the Ministry of Public Health (Methods), and calculated the weekly testing positivity rate, i.e. the number of COVID-19 cases over the total number of tests administered. The overall testing positivity rates in Ecuador using data up to 23 September are exceptionally high, i.e. 35%. In particular, during the period between 18 March and 8 April when highest excess deaths and COVID-19 deaths are observed, the test positivity rates are as high as 37–47% (Supplementary Figure S5, available as Supplementary data at IJE online). These rates are in stark contrast to the test positivity rate reported in other countries.13 Therefore, the exceptionally high test positivity rates in Ecuador are consistent with the hypothesis that the majority of excess deaths in Ecuador were caused directly by COVID-19 infection, but were not documented as COVID-19 deaths as a result of limited testing capacity.
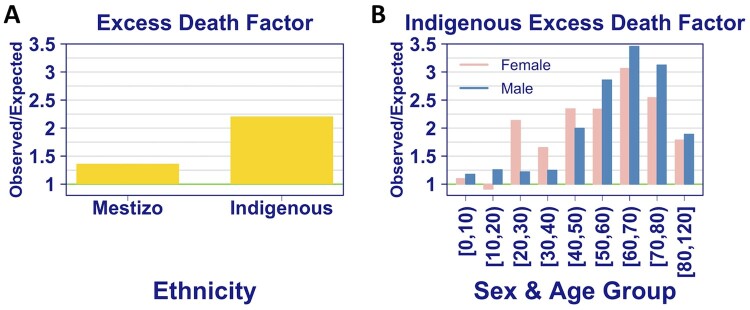
We next analysed the excess deaths by ethnic groups in Ecuador, and found that the excess death factor for the Indigenous group is 2.2, i.e. excess deaths are 220% of the expected deaths, compared with just 136% for the predominant ethnic group in Ecuador, i.e. the Mestizo group (Figure 3A). The distribution of excess deaths by sex and age group for the Indigenous population is similar to that for the general population, except that excess death factors for women in the age groups 20–30, 30–40 and 40–50 years are larger than those for men by 75%, 32% and 17%, respectively (Figure 3B). Ethnicity for death registrations is self-reported with typically 5% not being reported, but 24% were not reported in 2020. Even if all unreported ethnic data were not Indigenous, our results would show that the Indigenous group is much more disproportionally affected by COVID-19 than the confirmed death counts suggest.
Figure 3.
The excess death factor, i.e. the number of all-cause deaths over the number of expected deaths, by ethnicity (A) and by sex and age for the Indigenous group (B). Estimates for ethnic groups other than Mestizo and Indigenous are not shown because of the uncertain and changing definition of these groups between 2015 and 2020
Spatial and temporal pattern of excess deaths at the provincial level
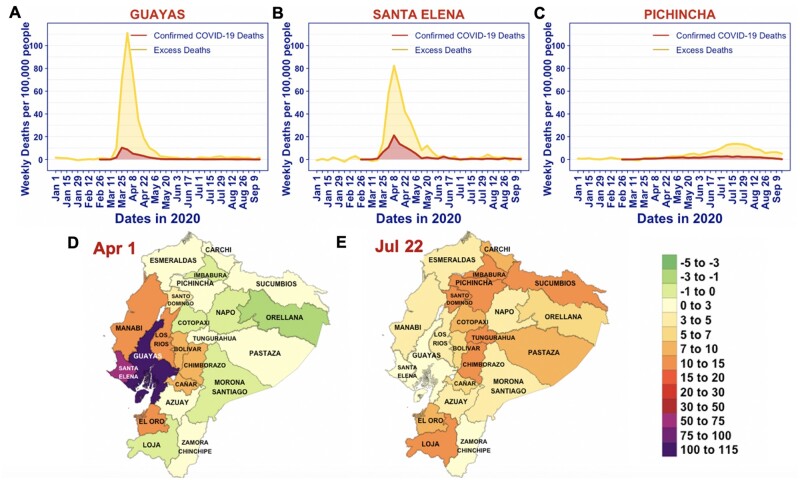
Next, we examined the excess deaths at the provincial level. The highest total excess deaths occurred in Guayas and Pichincha, comprising 29% and 18% of the excess deaths in Ecuador, respectively (Table 1). Note that the two provinces also reported the highest numbers of COVID-19 deaths (Table 1). When the number of deaths is normalized by the population size in each province, Guayas and Santa Elena had the highest per capita deaths, at 710 and 598 per 100 000 people, respectively (Table 1). Remarkably, the estimated excess death factors, i.e. the number of observed deaths over the number of expected deaths for Guayas, Pichincha and Santa Elena, are 2.1, 1.6 and 2.6, respectively (Table 1). These exceptionally high levels of excess deaths rate emphasize the enormous burden of COVID-19 spread on mortality.
There is a strong spatial and temporal pattern in the magnitude and timing of excess deaths, which is mostly consistent with the COVID-19 spread (as measured by COVID-19 deaths). In Guayas and Santa Elena, most excess deaths occurred during late March and mid-May 2020, with the highest numbers of weekly all-cause deaths and documented COVID-19 deaths occurring during the 2 weeks between 1 and 14 April (Figure 4), leading to the first wave of all-cause deaths in Ecuador as seen in Figure 1. During this period, the test positivity rates in these provinces are extremely high (40–80%; see Supplementary Figure S5). Again, this highlights the burden of COVID-19 spread on the limited testing and health care capacity in Ecuador, and the notion that it is likely that a large fraction of COVID-19 deaths was not diagnosed or documented. The high burden of mortality is also apparent in provinces neighbouring Guayas and Santa Elena, such as Los Rios, Manabí, Bolivar, Chimborazo, Cañar and El Oro (Figure 4D;Supplementary Figures S6 and S7, available as Supplementary data at IJE online).
Figure 4.
The spatial and temporal patterns of excess deaths in 2020 in Ecuador. (A–C) Time series for excess deaths (yellow; lighter colour) and documented COVID-19 deaths (red; darker colour) per 100 000 people in Guayas, Santa Elena and Pichincha. (D and E) Provincial maps of Ecuador showing the number of excess deaths per 100 000 people (colour) during the weeks of 1–7 April (panel D) and 22–28 July 2020 (panel E )
In July and August, Pichincha, where the capital city Quito is located, became the COVID-19 epicentre during the second wave of excess deaths (Figure 4C and E). Several other provinces close to Pichincha also saw excess deaths peaking during this period. Again, the geographical and temporal trends in the excess deaths follow the spatial and temporal spread of COVID-19, as indicated by reported COVID-19 deaths (Supplementary Figures S6 and S7, available as Supplementary data at IJE online).
Discussion
We observed a very high level of total all-cause deaths, 87 762 in total or 502 per 100 000 people, between 1 January and 23 September 2020 in Ecuador. Analysing death records during 2015 and 2020, we estimated the number of excess deaths to be 36 402 or 208 per 100 000 people; that is, deaths were 171% of their expected value during the study period. We found substantial heterogeneity in the spatial and temporal patterns in excess deaths. Guayas and Santa Elena had the most per capita excess deaths, most of which occurred during early COVID-19 outbreak in April 2020.
The high level of mortality, i.e. excess deaths of 208 per 100 000 people, highlights the enormous burden of COVID-19 on mortality in Ecuador. First, compared with estimates for other countries that have been heavily affected by COVID-19, such as the USA, England and Wales and Brazil, the level of excess deaths in Ecuador is approximately 2.9- and 2.3-fold of the estimate in the USA and in England and Wales, respectively.5,9 It is comparable to the excess deaths estimated for Mexico.16 Second, we compared the level of excess deaths with excess deaths estimated for previous pandemics. It is much higher than estimates of mortality for the 2009 influenza pandemic.20 During the 1918–20 influenza pandemic, the number of excess deaths is estimated to be between 200 to 4400 per 100 000 people across 27 countries.21 Therefore, the level of excess deaths in Ecuador is at the low end of estimates of excess death on the 1918–20 influenza pandemic. Similar results are found in analyses for Mexico16 and New York City.22
A distinguishing feature of excess deaths in Ecuador as compared with other countries, such as the USA and England and Wales,5,8,9 is that COVID-19 deaths (7410 in total up to 23 September 2020) only account for a small fraction, i.e. 20%, of all-cause excess deaths. Excess deaths can be caused directly by COVID-19 infection or indirectly as a result of COVID-19 related disruptions in society.2,3 We do not have data on the causes of deaths in 2020, and thus are unable to assess the major cause of the large number of excess deaths not attributable to COVID-19 deaths. However, results of our analyses as listed below strongly suggest that the true number of COVID-19 deaths is under-reported and a majority of excess deaths are likely to be caused directly by COVID-19, as seen in other countries.8–12 First, the spatial and temporal patterns of excess deaths follow closely the spatial and temporal patterns of COVID-19 outbreaks in Ecuador as suggested by the COVID-19 deaths counts. Second, more men died than women, and the excess deaths become apparent for age groups greater than 40 years old: the number of excess deaths increases dramatically with increases in age. These demographic characteristics of mortality are consistent with the risk of COVID-19 mortality19 and are very similar to the demographics in excess deaths found in countries such as England and Wales9 and Italy,11 where the majority of excess deaths were attributable to COVID-19 deaths. Third, we found that the test positivity rate in Ecuador is extremely high over the period of COVID-19 outbreak, indicating the very low testing capacity in Ecuador.4 Therefore, it is likely that a lot of COVID-19 infections, as well as deaths, were not detected or documented. Overall, irrespective of the cause of the excess deaths, our analysis demonstrates the enormous burden of COVID-19 on mortality in Ecuador which was not revealed by the numbers of COVID-19 cases and deaths previously.
Non-pharmaceutical interventions played important roles in suppressing SARS-CoV-2 transmission and preventing deaths.23 We found that in two provinces that had the most per capita excess deaths, i.e. Guayas and Santa Elena, the numbers of excess deaths decreased rapidly after the highest excess deaths occurred in the week of 1–8 April. This rapid decline coincides with the strict social distancing measures implemented during 17 March to 4 May 2020 by the Ecuador government. These measures include a national lockdown, border closure, suspension of travel and strict confinement of citizens with a curfew.17 Therefore, it is likely that the non-pharmaceutical interventions led to reduced COVID-19 transmission and effectively averted the extremely rapid increases in deaths, as shown for COVID-19 outbreaks in other countries.23 Given the exponential growth nature of the outbreak in the absence of intervention efforts,24–26 we reason that COVID-19 may have caused even more mortality than the observed high level if strict social distancing measures had been delayed or not been implemented at all. Thus, our results strongly suggest the importance of social distancing efforts in preventing deaths, and the potential devastating consequence in mortality if the strict non-pharmaceutical interventions, especially during early COVID-19 outbreak, were not implemented.
We estimated the excess deaths using death registration records collected between 1 January and 26 September 2020 in Ecuador. There are limitations in our estimates. First, the delay in death reporting was not taken into account. Updated summary death count statistics at the end of February 2021 reveal that during our study period, an additional 2309 deaths were added to the 87 762 deaths that we originally observed, suggesting an under-reporting of 2.6% due to reporting delays. At the time of publication, it was not possible to adjust our estimates of excess death using the updated death data due to a lack of associated metadata. Nonetheless, this result suggests that our estimation may be a slight underestimate in the order of a few percent. Second, death registration in Ecuador may be incomplete, as pointed out by Peralta et al.27 If the completeness of death registration remained constant over the period of the data we used for analysis, i.e. 2015–20, our estimation would be accurate; however, if the completeness was lower in certain years, for example in 2020 due to the disruption in societal activities because of COVID-19, we would underestimate the true total excess deaths in 2020. Likewise, differential incompleteness in the death registration records could produce some bias in the comparisons between geographical and ethnic groups. Further work estimating the completeness of data over 2015–20 would provide a more accurate assessment of the extent of excess deaths and improve the utility of the Ecuadorian death registry as a public health research tool.
Funding
The work is partially funded by the Laboratory Directed Research and Development (LDRD) Rapid Response Program through the Center for Nonlinear Studies at Los Alamos National Laboratory, and LDRD grants 20200699ER and 20210709ER. R.K. and S.P. would like to acknowledge funding from DARPA (HR0011938513), the Center for Nonlinear Studies. E.R.S. was funded through an NIH grant (R01AI135946). L.C. and N.H. would also like to acknowledge the US Department of Energy Office of Science through the National Virtual Biotechnology Laboratory, a consortium of national laboratories (Argonne, Los Alamos, Oak Ridge and Sandia) focused on responding to COVID-19, with funding provided by the Coronavirus CARES Act. The funding source had no role in the design of the study, execution, analyses, interpretation of the data or decision to publish.
Author contributions
Conceptualization: L.C., I.T., E.R.S., N.H. and R.K.; data acquisition: I.T.; methodology and formal analysis: L.C., E.R.S., R.M., N.O., S.P. and N.H.; funding acquisition: L.C. and R.K.; underlying data validation: L.C., I.T. and N.H.; visualization and writing: L.C. and R.K.
Data availability
The data underlying this article cannot be shared publicly due to Ecuador government regulations that the Ecuadorian Ministry of Public Health must approve the research protocol to release reusable COVID-19 datasets. Vital statistics may be available upon request to the Ecuadorian Civil Registry and will be publicly available through the Institute of Statistics and Census according to its statistics calendar. The data may be shared on reasonable request to the corresponding authors.
Conflict of interest
None declared.
Supplementary data
Supplementary data are available at IJE online.
Supplementary Material
References
- 1.WHO. WHO Coronavirus Disease (COVID-19) Dashboard. 2020. https://covid19.who.int (31 May 2021, date last accessed).
- 2. Kiang MV, Irizarry RA, Buckee CO, Balsari S.. Every body counts: measuring mortality from the COVID-19 pandemic. Ann Intern Med 2020;173:1004–1007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Leon DA, Shkolnikov VM, Smeeth L, Magnus P, Pechholdová M, Jarvis CI.. COVID-19: a need for real-time monitoring of weekly excess deaths. Lancet 2020;395:e81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Torres I, Sacoto F.. Localising an asset-based COVID-19 response in Ecuador. Lancet 2020;395:1339. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Woolf SH, Chapman DA, Sabo RT, Weinberger DM, Hill L, Taylor DDH.. Excess deaths from COVID-19 and other causes, March-July 2020. JAMA 2020;324:1562–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Weinberger DM, Chen J, Cohen T. et al. Estimation of excess deaths associated with the COVID-19 pandemic in the United States, March to May 2020. JAMA Intern Med 2020;180:1336–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bilinski A, Emanuel EJ.. COVID-19 and excess all-cause mortality in the US and 18 comparison countries. JAMA 2020;324:2100–2102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rossen LM, Branum AM, Ahmad FB, Sutton P, Anderson RN.. Excess deaths associated with COVID-19, by age and race and ethnicity - United States, January 26-October 3, 2020. MMWR Morb Mortal Wkly Rep 2020;69:1522–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Aburto JM, Kashyap R, Scholey J. et al. Estimating the burden of the COVID-19 pandemic on mortality, life expectancy and lifespan inequality in England and Wales: a population-level analysis. J Epidemiol Community Health 2021;75:735–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Michelozzi P, de'Donato F, Scortichini M. et al. Temporal dynamics in total excess mortality and COVID-19 deaths in Italian cities. BMC Public Health 2020;20:1238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Scortichini M, Schneider Dos Santos R, De' Donato F. et al. Excess mortality during the COVID-19 outbreak in Italy: a two-stage interrupted time-series analysis. Int J Epidemiol 2021;49:1909–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Carvalho TA, Boschiero MN, Marson FAL.. COVID-19 in Brazil: 150,000 deaths and the Brazilian underreporting. Diagn Microbiol Infect Dis 2021;99:115258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.ourworldindata.org. Coronavirus Pandemic (COVID-19). 2020. https://ourworldindata.org/coronavirus (31 May 2021, date last accessed).
- 14. Cabrera JML, Kurmanaev A. Ecuador’s death toll during outbreak is among the worst in the world. New York Times 23 April 2020.
- 15. Cevallos-Valdiviezo H, Vergara-Montesdeoca A, Zambrano-Zambrano G.. Measuring the impact of the COVID-19 outbreak in Ecuador using preliminary estimates of excess mortality. Int J Infect Dis 2021;104:297–99. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Dahal S, Banda JM, Bento AI, Mizumoto K, Chowell G.. Characterizing all-cause excess mortality patterns during COVID-19 pandemic in Mexico. BMC Infect Dis 2021;21:432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Hale T, Angrist N, Goldszmidt R. et al. A global panel database of pandemic policies (Oxford COVID-19 Government Response Tracker). Nat Hum Behav 2021;5:529–38. [DOI] [PubMed] [Google Scholar]
- 18. Ladhani SN, Amin-Chowdhury Z, Davies HG. et al. COVID-19 in children: analysis of the first pandemic peak in England. Arch Dis Child 2020;105:1180–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Verity R, Okell LC, Dorigatti I. et al. Estimates of the severity of coronavirus disease 2019: a model-based analysis. Lancet Infect Dis 2020;20:669–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Simonsen L, Spreeuwenberg P, Lustig R. et al. ; GLaMOR Collaborating Teams. Global mortality estimates for the 2009 Influenza Pandemic from the GLaMOR project: a modeling study. PLoS Med 2013;10:e1001558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Murray CJ, Lopez AD, Chin B, Feehan D, Hill KH.. Estimation of potential global pandemic influenza mortality on the basis of vital registry data from the 1918-20 pandemic: a quantitative analysis. Lancet 2006;368:2211–18. [DOI] [PubMed] [Google Scholar]
- 22. Faust JS, Lin Z, Del Rio C.. Comparison of estimated excess deaths in New York City during the COVID-19 and 1918 influenza pandemics. JAMA Netw Open 2020;3:e2017527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Flaxman S, Mishra S, Gandy A. et al. ; Imperial College COVID-19 Response Team. Estimating the effects of non-pharmaceutical interventions on COVID-19 in Europe. Nature 2020;584:257–61. [DOI] [PubMed] [Google Scholar]
- 24. Ke R, Romero-Severson EO, Sanche S, Hengartner N.. Estimating the reproductive number R0 of SARS-CoV-2 in the United States and eight European countries and implications for vaccination. J Theor Biol 2021;517:110621. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Romero-Severson EO, Hengartner N, Meadors G, Ke R.. Change in global transmission rates of COVID-19 through May 6 2020. PLoS One 2020;15:e0236776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Sanche S, Lin YT, Xu C, Romero-Severson E, Hengartner N, Ke R.. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis 2020;26:1470–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Peralta A, Benach J, Borrell C. et al. Evaluation of the mortality registry in Ecuador (2001-2013) - social and geographical inequalities in completeness and quality. Popul Health Metr 2019;17:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article cannot be shared publicly due to Ecuador government regulations that the Ecuadorian Ministry of Public Health must approve the research protocol to release reusable COVID-19 datasets. Vital statistics may be available upon request to the Ecuadorian Civil Registry and will be publicly available through the Institute of Statistics and Census according to its statistics calendar. The data may be shared on reasonable request to the corresponding authors.