Brugada syndrome (BrS) is a hereditary cardiac disease predisposing to sudden cardiac death in patients with structurally normal heart. Fever has been reported not only to unmask the type 1 Brugada electrocardiogram (ECG) pattern1 but also to trigger ventricular arrhythmias.2 In the Survey on Arrhythmic Events in Brugada Syndrome (SABRUS) registry, the fever-related arrhythmic events (AEs) are the first manifestation of the disease in the majority of BrS patients and frequently occur in asymptomatic patients without spontaneous type 1 ECG pattern; moreover, the 77% of children and 27% of adults with fever-induced AEs presented SCN5A pathogenic variants.3 Sodium channel function seems either less expressed or rapidly inactivated at higher temperatures, thus sensitizing patients to develop life-threatening arrhythmias, as also confirmed by further studies.4
COVID-19 clinical presentation is characterized by fever in about 92.8% of adults and 43.9% of children.5
Moreover, beyond the acute respiratory distress, severe cardiac complications, such as myocarditis, heart failure, and arrhythmias may complicate the clinical course of the disease.4 Due to these reasons, patients with either structural heart diseases or primary arrhythmia syndromes disclose a higher risk of COVID-19 related mortality.6 Thus, a rapid diagnosis, isolation, and intensive clinical management is crucial for BrS patients with COVID-19.7 Even if BrS patients share the COVID-19 infection risk of the whole population, based on the increased fever-induced arrhythmic risk, they should be considered belonging to frail category for the COVID-19 vaccination program.
Brugada syndrome patients with spontaneous pattern are burdened by an increased risk of fever-related AEs compared to those with drug-induced pattern (0.5–0.8%/year vs. 0–0.35%/year); moreover, BrS children (<16 years of both genders) exhibit a considerable risk of AEs, up to 67% of fever-induced AEs occurred in 5 years old or younger children, while AEs are rare in the elderly BrS patients (>70 years).3 No data are actually available on the fever response to antipyretic drugs among BrS population.
COVID-19 vaccines approved by the European Medicines Agency (EMA) include two different platforms: mRNA (Comirnaty—BioNTech/Pfizer, COVID-19 Vaccine Moderna) and adenoviral vectored (COVID-19 Vaccine Janssen, Vaxzevria—AstraZeneca). All of them are burdened by several side effects, particularly fever. Though, data on fever onset, which usually occurs within the first 2 days, are biased by antipyretic medications use (Comirnaty—BioNTech/Pfizer 1st dose 28% and 2nd dose 45%; Janssen 26.7% in patients aged 18–59 and 10% aged >60 years; no data available for Moderna and Vaxzevria—AstraZeneca).8–11
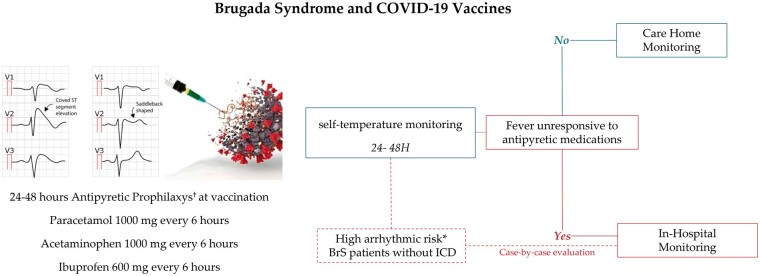
In our opinion, BrS patients should be managed at hospital vaccination centres so that adequate management proportionate to their arrhythmic risk could be guaranteed, allowing greater safety and avoiding delays in vaccinations (Figure 1).
Figure 1.
Covid19 vaccination management for BrS patients. †dosage adjustment according to age, weight, kidney and liver function. *history of ventricular arrhythmias and/or spontaneous type 1 ECG pattern with history of arrhythmic syncope.
We suggest for all BrS patients a prophylaxis with paracetamol 1000 mg every 6 h, acetaminophen 1000 mg every 6 h, ibuprofen 600 mg every 6 h, or other antipyretics, with dosage adjustment according to age, weight, kidney, and liver function, within the first 24–48 h, in order to reduce the risk of fever onset. Moreover, they should perform a daily fever self-monitoring. In case of fever unresponsive to antipyretic medications, BrS patients should be monitored at the emergency department till fever resolves, especially when they show an increased arrhythmic risk for the younger age, the spontaneous type 1 ECG pattern and/or SCN5A pathogenic variant.
Brugada syndrome patients with high arrhythmic risk for the history of ventricular arrhythmias or spontaneous type 1 ECG pattern with a history of arrhythmic syncope may be considered for hospitalization following the COVID-19 vaccination, even without fever occurrence, especially if they are not implantable cardiac defibrillator recipients. However, in this latter subgroup, a case-by-case evaluation should be performed also considering the patients’ age and how previously responded to vaccination and fever. In conclusion, we do believe that the achievement of herd immunity may protect this special population as well.
Conflict of interest: none declared.
The opinions expressed in this article are not necessarily those of the Editors of Europace or of the European Society of Cardiology.
References
- 1.Adler A, Topaz G, Heller K, Zeltser D, Ohayon T, Rozovski U. et al. Fever-induced Brugada pattern: how common is it and what does it mean? Heart Rhythm 2013;10:1375–82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Amin AS, Meregalli PG, Bardai A, Wilde AA, Tan HL.. Fever increases the risk for cardiac arrest in the Brugada syndrome. Ann Intern Med 2008;149:216–8. [DOI] [PubMed] [Google Scholar]
- 3.Michowitz Y, Milman A, Sarquella-Brugada G, Andorin A, Champagne J, Postema PG. et al. Fever-related arrhythmic events in the multicenter Survey on Arrhythmic Events in Brugada Syndrome. Heart Rhythm 2018;15:1394–401. [DOI] [PubMed] [Google Scholar]
- 4.Dendramis G, Brugada P.. Intensive care and anesthetic management of patients with Brugada syndrome and COVID-19 infection. Pacing Clin Electrophysiol 2020;43:1184–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rodriguez-Morales AJ, Cardona-Ospina JA, Gutiérrez-Ocampo E, Villamizar-Peña R, Holguin-Rivera Y, Escalera-Antezana JP, et al. ; Latin American Network of Coronavirus Disease 2019-COVID-19 Research (LANCOVID-19). Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis 2020;34:101623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wu CI, Postema PG, Arbelo E, Behr ER, Bezzina CR, Napolitano C. et al. SARS-CoV-2, COVID-19, and inherited arrhythmia syndromes. Heart Rhythm 2020;17:1456–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Russo V, Bottino R, Carbone A, Rago A, Papa AA, Golino P. et al. COVID-19 and heart: from clinical features to pharmacological implications. J Clin Med 2020;9:1944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Polack FP, Thomas SJ, Kitchin N, Absalon J, Gurtman A, Lockhart S, et al. ; C4591001 Clinical Trial Group. Safety and efficacy of the BNT162b2 mRNA Covid-19 vaccine. N Engl J Med 2020;383:2603–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baden LR, El Sahly HM, Essink B, Kotloff K, Frey S, Novak R. et al. Efficacy and safety of the mRNA-1273 SARS-CoV-2 vaccine. N Engl J Med 2021;384:403–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sadoff J, Gray G, Vandebosch A, Cárdenas V, Shukarev G, Grinsztejn B. et al. Safety and efficacy of single-dose Ad26.COV2.S vaccine against Covid-19. N Engl J Med 2021;384:2187–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ramasamy MN, Minassian AM, Ewer KJ, Flaxman AL, Folegatti PM, Owens DR. et al. Safety and immunogenicity of ChAdOx1 nCoV-19 vaccine administered in a prime-boost regimen in young and old adults (COV002): a single-blind, randomised, controlled, phase 2/3 trial. Lancet 2021;396:1979–93. [DOI] [PMC free article] [PubMed] [Google Scholar]