Abstract
Objective
COVID-19 has had unprecedented effects on American families, including increases in depression, anxiety, and irritability for both parents and children. While parents and children influence each other’s psychological functioning during non-disaster times, this effect may be amplified during times of disaster. The current study investigated how COVID-19 influenced covariance of depressive symptoms and irritability in children and their parents.
Methods
Three hundred and ninety-one parents and their 8- to 17-year-old children (Mage = 10.68 years old, 70% male, 86% White) from a large sample of children and parents, primarily from Southeastern Louisiana, completed self-report measures of depression and irritability approximately 6 weeks into the COVID-19 pandemic, as well as providing retrospective reports of their symptoms prior to the pandemic. Actor–partner interdependence models were used to measure the reciprocal effects of parent symptoms on children and vice versa, both before and during the pandemic.
Results
Actor effects in both the depressive symptoms and irritability models suggested that pre-COVID-19 depressive symptoms and irritability were robust predictors of early-COVID-19 depressive symptoms and irritability for both parents and children. Partner effects were also detected in the irritability model, in that parental irritability prior to COVID-19 was associated with decreased child irritability during the pandemic. Both before and during the pandemic, associations between parent and child depressive symptoms and irritability scores were weaker in families evidencing greater dysfunction.
Conclusions
Results suggest that COVID-19-related stress is associated with increases in both parent and child symptomatology, and that family relationships likely influence associations between these symptoms.
Keywords: COVID-19, depression, parenting, stress
Introduction
The novel coronavirus (COVID-19), and its associated restrictions (including stay-at-home orders, social distancing, and other virus-containment procedures), is a stressor much like other natural and human-made disasters. Previous research has documented the behavioral health impact of natural disasters on youth and their families (Liu et al., 2020; Rubens et al., 2018). During these times, youth and their families are affected not only by physical restrictions and limitations placed on residents, but also by fear and uncertainty associated with major disasters. Natural disasters such as hurricanes, floods, and tsunamis are stressors linked to greater likelihood of psychopathology among children and adolescents, including higher rates of depression, substance use, and post-traumatic stress disorders (PTSDs) (Adams et al., 2015; Lai et al., 2015; Orengo-Aguayo et al., 2019). Such negative effects have been demonstrated in studies assessing symptoms both months (Adams et al., 2015; Lai et al., 2015; Orengo-Aguayo et al., 2019; Rubens et al., 2018) and years (Liu et al., 2020; Rubens et al., 2018) after a given disaster.
The COVID-19 pandemic is similar to natural and human-made disasters in its rapid development, extensive disruption, and economic devastation. Pandemics, however, last longer and have uncertain end dates, often involve social isolation and/or limited social contact, and typically have far-reaching effects beyond one community or region. A recent review demonstrated that social isolation procedures, though often necessary for public health, were associated with negative psychological effects such as post-traumatic stress symptoms, confusion, and anger among adults (Brooks et al., 2020). The authors also reported that longer quarantine duration, infection fears, frustration, boredom, inadequate supplies, inadequate information, financial loss, and stigma were each associated with greater risk for and severity of negative psychological outcomes.
Very little of the work on the negative effects of isolation and stay-at-home orders considers impacts on youth. One notable exception is Sprang and Silman (2013), who reported that 30% of youth who had isolated during a health crisis met criteria for PTSD via parent report collected during the 2009 H1N1 pandemic. Youth may experience psychological distress associated with stay-at-home periods for the same reasons as adults: isolation from typical routines (e.g., school, friends, extracurricular activities), uncertainty around the duration of the restrictions, and fears about personal safety and health. However, youth may be additionally vulnerable to psychological distress due to intensified exposure to family members who may also be suffering. Remmerswaal and Muris (2011), for example, reported that children’s fear during the 2009 H1N1 “swine flu” pandemic was significantly associated with parental fear, and this association was partially mediated by parental transmission of threat-related information about the pandemic. Children and adolescents, whose emotional regulation abilities and cognitive functioning capacities are still developing, may take their emotional cues from the adults around them, especially during times of crisis.
COVID-19-related stressors have thus far been associated with increases in depression and loneliness among adolescents (Ellis et al., 2020), as well as increased restlessness, irritability, and nervousness/anxiety among children (Imran et al., 2020; Jiao et al., 2020; Shorer & Leibovich, 2020). Furthermore, parents of minor children reported elevated levels of depression, anxiety, and perceived stress, effects that were amplified by low family harmony and quarantine procedures (Wu et al., 2020). These outcomes may be partially due to increased demands on parents while schools and daycare centers are closed (Marchetti et al., 2020), as higher caregiver burden during COVID-19 was associated with higher rates of caregiver depression and anxiety, as well as more conflict and less closeness to their children during the isolation period (Russell et al., 2020).
During non-disaster times, parents and children exert bidirectional influences on each other’s psychological distress. Parental depression scores predict child depression scores both cross-sectionally and longitudinally (Hughes & Gullone, 2010; Tichovolsky et al., 2018), and reductions in maternal depression are associated with fewer child problem behaviors (Cuijpers et al., 2015; Goodman & Garber, 2017). Conversely, child internalizing symptoms can impact parental depression (Allmann et al., 2016; Hughes & Gullone, 2010; Raposa et al., 2011), and improved child behavior has been associated with decreased parent depression (Neill et al., 2018).
Parent and child psychological dysfunction continue to be associated during times of disaster (Chemtob et al., 2010; Dyb et al., 2011; Remmerswaal & Muris, 2011). Early evidence suggests COVID-19 is no different, with Spinelli et al. (2020) reporting that parental distress was associated with child psychological problems, including emotional symptoms, in response to lockdown procedures in an Italian sample. Mazza et al. (2020) reported similar findings, as well as noting that child psychological symptoms also impacted parental symptoms. Furthermore, some research suggests that these associations may actually be strengthened in the aftermath of disasters (Hausman et al., 2020).
In non-disaster times, family chaos is robustly associated with youth dysfunction (Bakker et al., 2012; Marcynyszyn et al., 2008; Sturge-Apple et al., 2017; Webster-Stratton & Hammond, 1999). Family dysfunction during or immediately following disasters has also been related to higher levels of distress among youth (Bokszczanin, 2008; Wasserstein & La Greca, 1998). COVID-19 stay-at-home periods may have an especially striking effect on dysfunction as families spend more time together, in confined spaces, without non-familial interactions to buffer conflicts (Brooks et al., 2020; Peterman et al., 2020; Usher et al., 2020). However, previous research has neglected to examine how family dysfunction may influence the association between parent and child symptoms during disasters.
Importantly, a significant impediment to disaster research is the inability to gather pre-disaster symptom data on new samples. To address this limitation, previous disaster research has gathered pre-disaster symptom data using retrospective report, while simultaneously collecting information on participants’ current functioning (Grimm et al., 2012; Sharpley & Christie, 2007). Previous research has demonstrated that retrospective reporting of symptoms correlates highly with prospective reporting over a specific period of time (Barrett, 1997), suggesting that participants are likely able to meaningfully distinguish between their functioning at a specific time in the past and current functioning. This may be especially true during significant events with a clear onset point. For example, Sharpley & Christie (2007) reported on individuals diagnosed with breast cancer who were asked to simultaneously report on current depressive and anxious symptoms and symptoms they experienced at the time of their diagnosis (approximately 2 years later). They found consistency in some symptoms over time (i.e., feelings of helplessness and difficulty coping) but meaningful shifts in the presentation of other symptoms (i.e., more somatic anxiety symptoms at the time of diagnosis versus more difficulty managing their worry 2 years later). This technique has also been used in disaster scenarios (Grimm et al., 2012), and specifically with regard to mood symptoms (Sharpley & Christie, 2007). Therefore, although prospective data are the strongest measure of pre-disaster functioning, the onset of isolation procedures during the COVID-19 pandemic may constitute such an event for which participants can clearly delineate how they felt before and after it occurred.
The current study extends prior literature in a few notable ways. First, most research investigating the relation between parent and child symptomatology during disasters relies on parent report of child symptoms, which may be influenced by parental distress (Gartstein et al., 2009; Kroes et al., 2003). Furthermore, most studies examining the impact of disasters on parent and child symptomatology focus on post-traumatic stress and anxious reactions. Outcomes such as depression and irritability may be more relevant to families during the current crisis, as isolation periods may be associated with less acute fear and more chronic uncertainty and boredom.
To address these limitations, the current study investigated the associations between self-reported parent and child depression and irritability, before and approximately 6 weeks into the COVID-19 pandemic. Additionally, we explored family dysfunction during the stay-at-home period as a moderator of the associations between parent and child distress. In line with previous research, we hypothesized that parental depressive symptoms and irritability would be positively associated with child depressive symptoms and irritability, respectively. We further hypothesized cross-lagged effects of parental symptoms on child symptoms, such that increased parental depressive symptoms and irritability prior to COVID-19 would be associated with increased child depressive symptoms and irritability, respectively, at the beginning of the pandemic. We hypothesized that child symptoms would also influence later parent symptoms in the same manner (i.e., child symptoms prior to the pandemic associated with parental symptoms at the beginning of the pandemic). Finally, family dysfunction during the first 6 weeks of isolation procedures was expected to influence the strength of these relationships; due to the exploratory nature of these analyses, however, a direction for this association was not proposed.
Methods
Study Design
The current sample came from an online, cross-sectional survey of families drawn from a convenience sample primarily from New Orleans, Louisiana. Families were recruited via Facebook advertisements, targeted emails to schools and parenting groups, and word-of-mouth. Parents were invited to participate in the online survey if they had a child under the age of 18 and lived in the greater New Orleans area, based on the larger study aims of investigating the relationship between hurricane exposure and COVID-19-related trauma (reported elsewhere). Approximately 10% of families who completed the survey reported living somewhere other than Southeastern Louisiana; due to the more general aims of the current study, however, families who lived outside of the desired area and completed the survey were included in the current analyses.
Participants
Twelve hundred and ninety-six families participated in an online survey of COVID-19 impacts on children and families. Of these, 398 consented for their 8- to 17-year-old child to complete child report surveys; of these, 391 children completed informed assent. The current sample is drawn from these 391 parent–child dyads. Parents who did not allow their children to participate were more likely to be female (χ2(1) = 18.10, p < .001), less likely to identify as Hispanic/Latinx (χ2(1) = 9.64, p < .01), more likely to identify as White (χ2(1) = 7.56, p < .01), more likely to have completed a Bachelor’s degree (χ2(6) = 48.60, p < .001), and self-reported fewer depressive symptoms (t(456) = 5.04, p < .001) and irritability (t(456) = 9.59, p < .001) prior to COVID-19.
The majority of parents reported being fathers (70%), currently married (96%), and having at least some college education (97%). Parents in the sample were, on average, 36.90 years old (SD = 4.71, range = 27–62 years), and primarily White (83%) and non-Hispanic/Latinx (81%). Non-White participants described their race as African American (7.7%), Native American (1.8%), Asian American (1.5%), Pacific Islander (0.5%), Other (0.5%), or declined to note their race (0.5%); totals add up to >100% due to some respondents selecting multiple options.
Children in the current study were, on average, 10.68 years old (SD = 2.28 years) and 70% of the sample was male. Ethnicity of children was as follows: 86% were White, 15.5% were Hispanic/Latinx, 2.4% were African American, 0.2% were Native American, 1.7% were Asian American, 0.3% were Pacific Islander, and 0.5% listed their child’s race as Other; again, totals add up to >100% due to some respondents selecting multiple options.
Procedure
All advertisements and procedures were approved by the investigators’ University institutional review board prior to initiation. Parents completed questionnaires regarding their own symptoms and COVID-19-associated stressors, as well as questionnaires about up to three minor children living with them. Children ages 8–17 years also answered questionnaires about themselves. To avoid nested data, only information on the first child reported on was used in the current analysis. Regarding symptom data (i.e., depressive and irritability measures), parents and children were asked to report on symptoms prior to the pandemic (using an anchor date of February 2020) and within the past 2 weeks (with the exception of the Family Assessment Device [FAD]; see below for additional details). Compensation consisted of an Amazon e-gift card worth $10, $15, or $20 for completing surveys about one, two, or three children, respectively.
Measures
Parent Report
Mood and Feeling Questionnaire, Adult Self-Report, Short Form (MFQ-A). The MFQ-A (Angold et al., 1995) is a 13-item self-report questionnaire designed to assess depressive symptoms in adults. Parents were asked to indicate whether an item was true (=2), sometimes true (=1), or not true for them (=0) at the moment. Item scores are then summed to create a total score, with a score of 12 indicating clinically significant depressive symptoms (Thabrew et al., 2018). For the current study, parents were asked to report on their depressive symptoms both before the stay-at-home period and in the past 2 weeks. Both timepoints had acceptable reliability (Cronbach’s alphas of .83 and .77, respectively).
Brief Irritability Test (BITe). The BITe (Holtzman et al., 2015) is a five-item self-report of irritable mood in adults on a six-point scale, ranging from never (=1) to always (=5). Clinical cutoffs have not been established for the BITe, but a comparable community sample reported an average BITe score of 11.73 (SD = 5.99; Deveney et al., 2019). For the current study, parents were asked to report on their irritability symptoms both before the stay-at-home period and in the past 2 weeks. These scales demonstrated modest reliability, with Cronbach’s alphas of .71 (before COVID-19) and .62 (during COVID-19).
FAD—General Functioning(GF)Subscale. The FAD is a 60-item scale assessing six facets of family functioning including problem-solving, communication, and affective involvement, as well as a GF scale (Epstein et al., 1983). The GF subscale is a 12-item measure within the FAD that assesses overall family functioning. Given that the GF subscale of the FAD measures trait-like features of family functioning that are unlikely to change quickly, parents were instructed to consider their family’s GF rather than functioning before and during COVID-19. Each item was rated on a scale that ranged from strongly agree (=1) to strongly disagree (=4), with the final score being an average of the item scores. Higher scores on the FAD indicate more dysfunction, and scores over 2 suggest difficulties in general family functioning (Miller et al., 1985). The FAD demonstrated modest reliability (Cronbach’s alpha = .68).
Child Report
Mood and Feelings Questionnaire, Child Self-Report, Short Form (MFQ-C). The MFQ-C (Angold et al., 1995) is a 13-item self-report questionnaire designed to assess depressive symptoms in children. Children indicated whether each item was not true (=0), sometimes true (=1), or true (=2). Item scores were summed to create total scores, and scores over 12 indicated clinically significant difficulties with depression (Thabrew et al., 2018). For the current study, children were asked to report on their depressive symptoms both before the stay-at-home period and in the past 2 weeks. Reliability at both timepoints was acceptable, with Cronbach’s alphas of .82 and .78, respectively.
Affective Reactivity Inventory (ARI). The ARI (Stringaris et al., 2012) assesses child’s irritable mood with six summed items (e.g., easily annoyed by others; often loses temper). (A seventh item assessing impairment is not part of the total score.) Each item was rated on a scale from not true (=0) to certainly true (=2); summed scores were compared to a clinical cutoff of 3 (Stringaris et al., 2012). For the current study, children were asked to report on their irritability symptoms both before the stay-at-home period and in the past 2 weeks. Both timepoints of the ARI were demonstrated modest reliability, with Cronbach’s alphas of .69 and .71, respectively.
Data Analysis
First, correlations and t-tests were used to characterize the study sample, and sensitivity analyses were conducted to assess any significant differences between the current subsample and the larger sample from which it was drawn. Parent and child symptom scores, as well as family functioning scores, were also compared to established norms and clinical cutoffs for the respective measures.
To examine the associations between parent and child depression and irritability before and during the COVID-19 pandemic, two latent actor–partner interdependence models (APIMs; Cook & Kenny, 2005) were created using Mplus version 8 (Muthén & Muthén, 2017). APIMs are used to simultaneously model how members of a dyad (in this case, parents and their children) influence one another’s symptoms. Actor effects measure the extent to which an individual’s prior symptoms are associated with their later symptoms (stability), while partner effects measure the effect to which one member of the dyad influences their partner’s symptom profile.
The first APIM modeled the relation between parent and child depression before and during COVID-19. The second APIM modeled parent and child irritability at the same timepoints. For both APIMs, factor scores (rather than raw sum scores from each measure) were created from latent factors in order to minimize measurement error (Klein, 2016) and reduce the number of variables included in each model. Child report items from the MFQ-C, and parent report items from the MFQ-A, were used to indicate the depression latent factors before and during the COVID-19 pandemic, while child and parent irritability factors were indicated by items from the ARI and BITe, respectively. Child age, parent sex, and child sex were included in both models as covariates, as all three are factors that are independently associated with mood and irritability symptoms (Copeland et al., 2015; Kuehner, 2017; Twenge & Nolen-Hoeksema, 2002). Model fit was based on generally accepted standards in the field (i.e., root mean square error of approximation [RMSEA] < .06, standard root mean square residual [SRMR] < .08, comparative fit index [CFI] >.95, and Tucker-Lewis index [TLI] >.95; Hu & Bentler, 1999). Missing data were handled using full information maximum likelihood estimation methods.
Confidence intervals (CIs), calculated with a Fisher’s z′ transformation, were used to determine if correlations between parent and child depressive symptoms and irritability were significantly different before and during the pandemic. If CIs did not overlap, correlations were considered significantly different.
Finally, moderation models in multiple linear regression were used to examine if family functioning moderated the relationship between child and parent depressive symptoms and irritability at either timepoint. Depressive symptoms, irritability, and family functioning were included in the models as latent factors, with child age, parent sex, and child sex included as covariates. The moderation analyses were done using the reports of constructs before COVID-19 and separately for the reports of the constructs during the COVID-19 pandemic. In order to consider differing influences of parents on children and vice versa, models were run twice—once with parent irritability or depressive symptoms as the dependent variable and once with child irritability or depressive symptoms as the dependent variable. The PROCESS macro (Hayes, 2017) was used to probe significant interactions and assess the significance of simple slopes.
Results
Descriptive statistics and associations between study variables are presented in Table I.
Table I.
Descriptive Statistics and Bivariate Correlations Between Symptom and Family Functioning Scores
| Parent variables | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 |
|---|---|---|---|---|---|---|---|---|---|
| 1. Pre-CV depressive symptoms | — | ||||||||
| 2. Early-CV depressive symptoms | .42 | — | |||||||
| 3. Pre-CV irritability symptoms | .66 | .23 | — | ||||||
| 4. Early-CV irritability symptoms | .28 | .53 | .28 | — | |||||
| Child variables | |||||||||
| 5. Pre-CV depressive symptoms | .65 | .23 | .62 | .27 | — | ||||
| 6. Early-CV depressive symptoms | .32 | .55 | .23 | .47 | .49 | — | |||
| 7. Pre-CV irritability symptoms | .50 | .16 | .52 | .22 | .69 | .39 | — | ||
| 8. Early-CV irritability symptoms | .24 | .52 | .21 | .42 | .35 | .69 | .43 | — | |
| Family variables | |||||||||
| 9. Family functioning | .47 | .33 | .36 | .19 | .39 | .27 | .22 | .18 | — |
| Mean (SD) | 10.20 (5.13) | 12.26 (4.93) | 15.91 (4.87) | 17.60 (4.69) | 10.28 (5.57) | 12.02 (5.13) | 5.18 (2.71) | 6.09 (2.71) | 2.32 (0.37) |
Note. Early-CV = early-COVID-19 assessment; Pre-CV = pre-COVID-19 assessment. All correlations p < .001.
For parents, the mean depressive symptom score prior to COVID-19 was 10.20 (SD = 5.13), with 36% of parents scoring above the typical clinical cutpoint of 12 (Thabrew et al., 2018); at the beginning of the pandemic, the mean depressive symptom score was 12.26 (SD = 4.93), with 53% of the sample above the clinical cutoff. A paired sample t-test indicated that this was a significant increase, t(384) = 7.36, p < .001. The mean parental irritability score prior to the pandemic was 15.91 (SD = 4.87); at the beginning of the pandemic, the mean irritability score was 17.60 (SD = 4.69). While clinical cutoffs have not been established for the BITe, these scores were higher than the average seen in a comparable community sample (Deveney et al., 2019). Again, a paired sample t-test indicated a significant increase in irritability symptoms, t(385) = 5.72, p < .001.
For children, the mean depressive symptom score prior to COVID-19 was 10.28 (SD = 5.57), with 40% of children scoring above the typical clinical cutpoint of 12 (Thabrew et al., 2018); at the beginning of the pandemic, the mean depressive symptom score was 12.02 (SD = 5.13), with 52% of the sample above the clinical cutoff. The mean child irritability score prior to COVID-19 was 5.18 (SD = 2.71), with 73% of children scoring above the typical clinical cutpoint of 3 (Stringaris et al., 2012); at the beginning of the pandemic, the mean irritability score was 6.09 (SD = 2.71), with 82% of the sample above the clinical cutoff. The increases in child depressive and irritability scores from pre- to early-COVID were statistically significant, t(361) = 6.07, p < .001 and t(359) = 6.01, p < .001, respectively. Finally, parents reported a mean family functioning score of 2.31 (SD = .37), with 80% of families scoring above the typical cutoff indicating dysfunction.
Calculation of Factor Scores
Factor scores for depressive symptoms, irritability, and family functioning were calculated separately to reduce error and simplify the model. The depressive symptoms factor score model had excellent fit, χ2 = 1,501.341, df = 1,268, p < .001; RMSEA = 0.022, 90% CI [0.017–0.026]; CFI = 0.922; TLI = 0.918; SRMR = 0.049. The irritability and family functioning factor score models also had excellent fits, χ2 = 284.672, df = 246, p < 0.05; RMSEA = 0.020, 90% CI [0.003–0.030]; CFI = 0.965; TLI = 0.960; SRMR = 0.045 and χ2 = 15.056, df = 9, p = 0.089; RMSEA = 0.042, 90% CI [0.000–0.077]; CFI = 0.942; TLI = 0.904; SRMR = 0.035, respectively.
Actor–Partner Interdependence Model Results
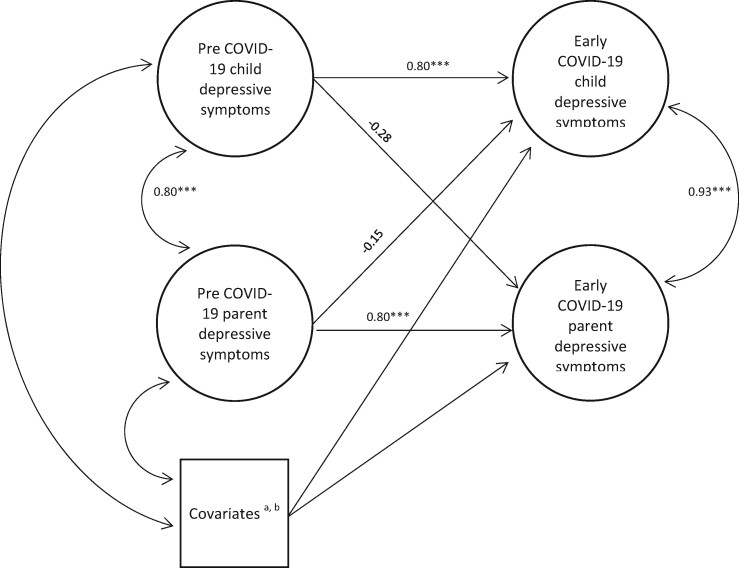
The APIM of child and parent depressive symptoms had excellent fit, χ2 = 1,690.434, df = 1,412, p = 0.000; RMSEA = 0.023, 90% CI [0.018–0.027]; CFI = 0.912; TLI = 0.907; SRMR = 0.049. Regression and correlation coefficients can be seen in Figure 1. Significant actor effects were detected: pre-COVID-19 child depressive symptoms significantly predicted child depressive symptoms during COVID-19 (β = 0.80, p < .001). Similarly, pre-COVID-19 parent depressive symptoms significantly predicted parent depressive symptoms during COVID-19 (β = 0.80, p < .001). Partner effects for the associations between parent and child depressive symptoms were not detected, however. Child age (β = 0.19, p < 0.01) was significantly associated with child depressive symptoms during COVID-19, in that older children reported more depressive symptoms than younger children. There were large, positive correlations between parent and child depressive symptoms before (r = 0.80, 95% CI [0.76–0.83]; p < 0.01) and during (r = 0.93, 95% CI [0.92–0.94]; p < 0.01) the COVID-19 pandemic; the correlation was significantly larger during the pandemic (as indicated by non-overlapping CIs).
Figure 1.
Results of actor–partner interdependence model for parent and child depressive symptoms. aSignificant correlations between covariates and independent variables (IVs): Pre-COVID-19 child depressive symptoms with child sex (β = −0.27, p < 0.001), child age (β = −0.19, p < 0.01), parent sex (β = −0.29, p < 0.001), parent age (β = −0.19, p < 0.01); Pre-COVID-19 parent depressive symptoms with parent age (β = −0.16, p < 0.05), parent sex (β = −0.35, p < 0.001), child sex (β = −0.23, p < 0.01). bSignificant coefficients between covariates and dependent variable (DV): Early-COVID-19 child depressive symptoms and child age (β = 0.19, p < 0.01). ***Coefficient is significant at the 0.001 level (two-tailed). **Coefficient is significant at the 0.01 level (two-tailed). *Coefficient is significant at the 0.05 level (two-tailed).
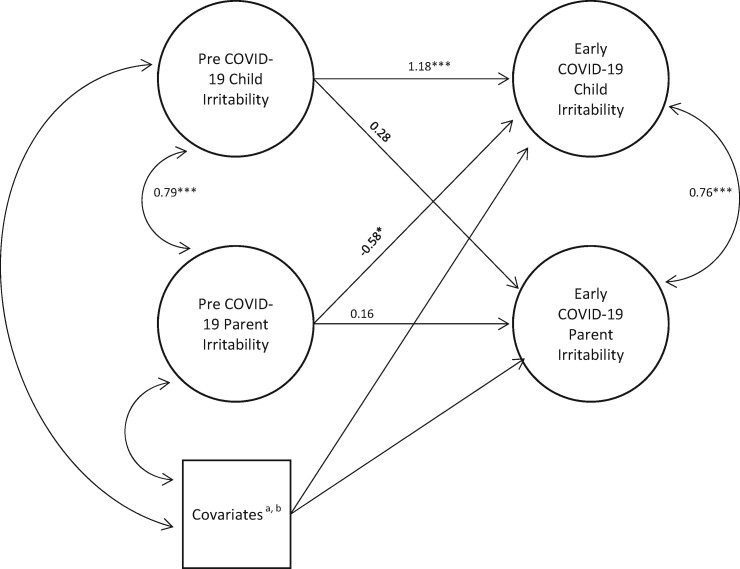
The actor–partner model of child and parent irritability also had excellent fit, χ2 = 371.095, df = 306, p < 0.01; RMSEA = 0.023, 90% CI (0.013–0.031); CFI = 0.947; TLI = 0.940; SRMR = 0.045. Figure 2 shows regression and correlation coefficients. Actor effects emerged for children, as pre-COVID-19 child irritability was associated with greater child irritability during the COVID-19 pandemic (β = 1.18, p < .001). However, pre-COVID-19 parent irritability was not associated with early-COVID-19 parent irritability in the APIM. Additionally, child age was significantly associated with child irritability during COVID-19 (β = 0.23, p < .001), in that older children reported more irritability. None of the independent variables or covariates significantly predicted parent irritability during the pandemic. Regarding partner effects, pre-COVID-19 parent irritability was significantly associated with lower child irritability during the pandemic (β = −0.58, p < .05). Similar to depressive symptom scores, parent and child irritability had large and significant correlations before (r = 0.79, 95% CI [0.75–0.83], p < .01) and during (r = 0.76, 95% CI [0.71–0.80], p < .01) the pandemic. Overlapping CIs, however, suggest that there is not a significant difference in covariance of parent and child irritability between the two timepoints.
Figure 2.
Results of actor–partner interdependence model for parent and child irritability. aSignificant associations between covariates and IVs: Pre-COVID-19 child irritability with child sex (β = −0.18, p < 0.01), child age (β = −0.15, p < 0.05), parent sex (β = −0.22, p < 0.01); Pre-COVID-19 parent irritability with parent sex (β = −0.23, p < 0.01), child sex (β = −0.23, p < 0.001). bSignificant associations between covariates and DV: Early-COVID-19 child irritability and child age (β = 0.23, p < 0.01). ***Coefficient is significant at the 0.001 level (two-tailed). **Coefficient is significant at the 0.01 level (two-tailed). *Coefficient is significant at the 0.05 level (two-tailed).
Moderation Results
Before the COVID-19 pandemic, child depressive symptoms interacted with family functioning to predict parent depressive symptoms (β = −0.26, standard error [SE] = .08, p < 0.001) such that, in families with less dysfunction, child depressive symptoms had a stronger impact on parent depressive symptoms (β = 0.67, SE = 0.03, p < 0.001) than in families reporting more dysfunction (β = 0.51, SE = .04, p < 0.001). Similarly, children’s early-COVID-19 depressive symptom scores interacted with family functioning to predict parents early-COVID-19 depressive symptom scores (β = −0.37, SE = .10, p < 0.001), with a similar pattern of simple slopes (β = 0.71, SE = .02, p < 0.001 and β = 0.48, SE = .05, p < 0.001) for families with low and high levels of dysfunction, respectively.
Family functioning interacted with parent irritability to predict child irritability before COVID-19 (β = −0.10, SE = .04, p < 0.05) such that, in families with less dysfunction, the impact of parent irritability on child irritability was stronger (β = 0.39, SE = .01, p < 0.001) than when parents reported more dysfunction (β = 0.33, SE = .02, p < 0.001). During the COVID-19 pandemic, a similar pattern emerged—namely, parent irritability interacted with family functioning to predict child irritability in the same way (β = −0.18, SE = .03, p < 0.001), with families reporting less dysfunction demonstrating a stronger relationship between parent and child irritability (β = 0.39, SE = .02, p < 0.001) than families with more dysfunction (β = 0.27, SE = .02, p < 0.001).
Discussion
The current study investigated bidirectional associations between parent and child depressive symptoms and irritability before and during the COVID-19 pandemic and stay-at-home period. Previous research has demonstrated that parents and children exert mutual effects on each other’s psychological functioning both within and outside of disaster situations. Our findings largely support this notion and add to the burgeoning literature on the impact of COVID-19 on families, specifically on psychological functioning of children and parents during this unique stressor.
With regard to depressive symptoms before and during the pandemic, APIMs revealed evidence of significant actor effects for both children and parents. This suggests that parents and children both demonstrated similar levels of depressive symptoms at both timepoints, and that earlier depressive symptoms were the best predictor of future symptoms for both members of the dyad. While we did not find evidence of partner effects (e.g., pre-pandemic depressive symptom scores in one member of the dyad did not influence early-pandemic depressive symptom scores in the other member), there was a significant increase in the covariance of depressive symptoms within the dyad across the assessment period. Specifically, parent and child depressive symptom scores were more closely related during the COVID-19 pandemic than they were beforehand. The most likely explanation for this finding is that parents and their minor children are spending more time together, and may be experiencing the same COVID-19-related stressors. While parents and children typically spend large amounts of time together, the impact of this time may be diluted when they are also spending time with friends, coworkers, or other extended family members.
A related explanation introduces the concept of attunement, or synchronized emotional and behavioral responses during dyadic interactions. Previous research has demonstrated that higher levels of emotional and behavioral attunement in parent–child dyads are associated with more optimal emotional functioning in children (Feldman, 2012). While increases in depressive symptomatology ought not be considered optimal emotional functioning, such increases may be normative during times of stress and disaster (Bonanno et al., 2010). Increased covariance in parent and child depressive symptoms, therefore, may be evidence of familial closeness and emotional attunement. This explanation is supported by our moderation findings, which suggest that the impact of child depressive symptoms on parent depressive symptoms was stronger in the presence of less family dysfunction. In families with less dysfunction, children may be able to share and express their stressful experiences of the pandemic more honestly (Carpenter et al., 2017), leading to increased parent–child attunement, while increased family dysfunction may impede such emotional attunement. Additionally, families reporting less dysfunction may have more resources to draw upon in times of stress, including flexible employment, outside assistance from family and friends, or financial stability. Access to such resources may free up cognitive space for parents and allow for increased attention to children’s emotions and symptoms; indeed, previous research suggests that dysfunction and family chaos is associated with decreased parental sensitivity and responsivity (Evans & Wachs, 2010). Increased responsiveness, in turn, may result in greater detection of child symptoms, increased parental concern, and subsequent parent symptoms (Fisak et al., 2012).
When considering irritability, APIM also revealed significant actor effects for children, suggesting that children’s irritability prior to COVID-19 was a strong predictor of their irritability at the beginning of the pandemic. Such actor effects were not found for parents, however, suggesting that parental irritability at the beginning of the pandemic was not significantly influenced by parental irritability prior to the pandemic. It may be that many parents who reported irritability at the beginning of the pandemic were not experiencing an exacerbation of underlying irritability, but rather a new onset of irritability as the result of a stressful situation. Significant partner effects, however, suggested that more parental irritability prior to the pandemic was associated with lower child irritability during the pandemic. Irritability may manifest as relational aggression, including snapping at others due to feeling bothered. Children whose parents have already demonstrated significant irritability prior to the pandemic may attempt to restrain their own irritable emotions, for fear of “setting off” parental anger, especially during the increasingly stressful conditions of social isolation (Gruhn & Compas, 2020). Similar to the depressive symptom findings, higher levels of family dysfunction attenuated the effect of parent irritability on child irritability. Again, this supports the notion that children are detecting instability or chaos in their homes which in turn prevents them from fully expressing their irritability; conversely, parents in more stable families may have more emotional and physical resources to attend to and feel concern about their children’s emotions (Dumas et al., 2005). Relatedly, children from more chaotic families may demonstrate less irritability and depression during disasters simply because they have become accustomed to unpredictable emotional displays from their parents. Future research should investigate the potential mechanisms influencing the relationships between family instability and parent–child symptom concordance.
Child age was significantly associated with both depressive symptoms and irritability at the beginning of the pandemic. While age-related changes in depressive symptoms and irritability are typical (Copeland et al., 2015; Rapee et al., 2019; Twenge & Nolen-Hoeksema, 2002), adolescents may be at particular risk for poor mental health outcomes during the current period of social isolation. Notably, adolescents may be more significantly impacted by restrictions on their activities, as the importance of peer relationships grows as children age (Ellis & Zarbatany, 2017). Furthermore, school closures may have a more significant impact on adolescents’ future academic and occupational prospects than those of younger children, leading to feelings of helplessness and despair (Ellis et al., 2020). Finally, in the absence of outside help, adolescents may be asked to take on more household chores or childcare responsibilities for younger siblings than usual, which could lead to increased feelings of irritability.
The current study had a number of strengths, including contemporaneous assessment of mood symptoms during the COVID-19 stay-at-home period, use of self-report data for both parents and children (avoiding informant bias seen when utilizing parent reports of child symptoms), and the use of APIM to model bidirectional effects within parent–child dyads. There were, however, significant limitations. First, our measures of pre-pandemic and early-pandemic functioning were collected simultaneously, introducing the potential for response bias. Relatedly, it is possible that our APIM model fit may have been inflated due to subsequent high correlations between symptom scores. Despite this, previous research suggests that retrospective reporting of symptoms correlates highly with prospective reporting over a specific period of time (Barrett, 1997). Furthermore, this technique has been used previously in the disaster literature (Grimm et al., 2012) and specifically for the assessment of mood symptoms (Sharpley & Christie, 2007). Second, we did not have a highly diverse sample, with the majority of respondents being highly educated, married, and White. The disproportionate impact of the COVID-19 pandemic on communities of color, including both health and economic disparities, is well-documented (Andrasfay & Goldman, 2021; Cyrus et al., 2020; Gemelas et al., 2021; Millett et al., 2020). Furthermore, the current sample is not representative of the racial and ethnic distribution of the population of New Orleans (e.g., 59.5% Black/African American; United States Census Bureau, 2019). It is possible, therefore, that this sample provides an underrepresentation of the mental health difficulties experienced by children and families during stay-at-home orders, and may limit applicability of our findings to other groups of Americans. Relatedly, fathers were overrepresented in the current sample; while in some ways this can be considered a strength (as fathers are typically underrepresented in developmental research [Phares et al., 2005]), it also suggests that the current sample may not be fully representative of the population as a whole. Third, the percentage of children reporting significant irritability in this sample is high, which may indicate biases in reporting, non-adherence to questionnaire directions, or misunderstanding of the questionnaire items. Fourth, report of family dysfunction was only collected from parents, which prevents us from understanding how children’s perception of family dysfunction may influence their symptoms. Finally, data were collected at the relative beginning of the pandemic, approximately 6 weeks after stay-at-home procedures had been adopted. Assessing parents and children at later points in the pandemic may have yielded different results.
Taken together, our results suggest that the COVID-19 pandemic has been associated with an increase in depressive symptoms and irritability among both children and parents, and that family relationships likely influence these symptoms. Future research should investigate the extent to which increased depressive symptoms and irritability persist beyond the pandemic and stay-at-home periods. It is possible that the current findings reflect a temporary increase in distress as families adjust to a “new normal,” from which most families will ultimately recover (Dvorsky et al., 2020). Other families, however, may demonstrate continued dysfunction and distress. For these families especially, future research should explore intervention strategies that may mitigate the negative effects of medically necessary periods of isolation. Such interventions could include psychoeducation around the impacts of social isolation and disruption of routines, behavioral activation to support healthy and safe behaviors during periods of social isolation, and problem-solving training in order to help families manage conflict effectively while in close quarters. Future research may also investigate the effectiveness of delivering such interventions remotely (via videoconferencing or telephone) or in a self-guided form (e.g., online program or printed materials available in the community) to ensure participant safety during public health emergencies.
Conflicts of interest: None declared.
References
- Adams Z. W., Danielson C. K., Sumner J. A., McCauley J. L., Cohen J. R., Ruggiero K. J. (2015). Comorbidity of PTSD, major depression, and substance use disorder among adolescent victims of the spring 2011 tornadoes in Alabama and Joplin, Missouri. Psychiatry: Interpersonal and Biological Processes, 78(2), 170–185. 10.1080/00332747.2015.1051448 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allmann A. E., Kopala-Sibley D. C., Klein D. N. (2016). Preschoolers' psychopathology and temperament predict mothers' later mood disorders. Journal of Abnormal Child Psychology, 44(3), 421–432. 10.1007/s10802-015-0058-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Andrasfay T., Goldman N. (2021). Reductions in 2020 US life expectancy due to COVID-19 and the disproportionate impact on the Black and Latino populations. Proceedings of the National Academy of Sciences, 118(5), e2014746118. 10.1073/pnas.2014746118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angold A., Costello E. J., Messer S. C., Pickles A., Winder F., Silver D. (1995). The development of a short questionnaire for use in epidemiological studies of depression in children and adolescents. International Journal of Methods in Psychiatric Research, 5, 237–249. [Google Scholar]
- Bakker M. P., Ormel J., Verhulst F. C., Oldehinkel A. J. (2012). Childhood family instability and mental health problems during late adolescence: a test of two mediation models—the TRAILS study. Journal of Clinical Child and Adolescent Psychology, 41(2), 166–176. 10.1080/15374416.2012.651990 [DOI] [PubMed] [Google Scholar]
- Barrett L. F. (1997). The relationships among momentary emotion experiences, personality descriptions, and retrospective ratings of emotion. Personality and Social Psychology Bulletin, 23(10), 1100–1110. 10.1177/01461672972310010 [DOI] [Google Scholar]
- Bokszczanin A. (2008). Parental support, family conflict, and overprotectiveness: predicting PTSD symptom levels of adolescents 28 months after a natural disaster. Anxiety, Stress, and Coping, 21(4), 325–335. 10.1080/10615800801950584 [DOI] [PubMed] [Google Scholar]
- Bonanno G. A., Brewin C. R., Kaniasty K., Greca A. M. L. (2010). Weighing the costs of disaster: consequences, risks, and resilience in individuals, families, and communities. Psychological Science in the Public Interest, 11(1), 1–49. 10.1177/1529100610387086 [DOI] [PubMed] [Google Scholar]
- Brooks S. K., Webster R. K., Smith L. E., Woodland L., Wessely S., Greenberg N., Rubin G. J. (2020). The psychological impact of quarantine and how to reduce it: rapid review of the evidence. The Lancet, 395(10227), 912–920. 10.1016/S0140-6736(20)30460-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carpenter A. L., Elkins R. M., Kerns C., Chou T., Greif Green J., Comer J. S. (2017). Event-related household discussions following the Boston Marathon bombing and associated posttraumatic stress among area youth. Journal of Clinical Child and Adolescent Psychology, 46(3), 331–342. 10.1080/15374416.2015.1063432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chemtob C. M., Nomura Y., Rajendran K., Yehuda R., Schwartz D., Abramovitz R. (2010). Impact of maternal posttraumatic stress disorder and depression following exposure to the September 11 attacks on preschool children's behavior. Child Development, 81(4), 1129–1141. 10.1111/j.1467-8624.2010.01458.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook W. L., Kenny D. A. (2005). The actor-partner interdependence model: a model of bidirectional effects in developmental studies. International Journal of Behavioral Development, 29(2), 101–109. 10.1080/01650250444000405 [DOI] [Google Scholar]
- Copeland W. E., Brotman M. A., Costello E. J. (2015). Normative irritability in youth: developmental findings from the Great Smoky Mountains Study. Journal of the American Academy of Child & Adolescent Psychiatry, 54(8), 635–642. 10.1016/j.jaac.2015.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cuijpers P., Weitz E., Karyotaki E., Garber J., Andersson G. (2015). The effects of psychological treatment of maternal depression on children and parental functioning: a meta-analysis. European Child & Adolescent Psychiatry, 24(2), 237–245. 10.1007/s00787-014-0660-6 [DOI] [PubMed] [Google Scholar]
- Cyrus E., Clarke R., Hadley D., Bursac Z., Trepka M. J., Dévieux J. G., Bagci U., Furr-Holden D., Coudray M., Mariano Y., Kiplagat S., Noel I., Ravelo G., Paley M., Wagner E. F. (2020). The impact of COVID-19 on African American communities in the United States. Health Equity, 4(1), 476–483. 10.1089/heq.2020.0030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deveney C. M., Stoddard J., Evans R. L., Chavez G., Harney M., Wulff R. A. (2019). On defining irritability and its relationship to affective traits and social interpretations. Personality and Individual Differences, 144, 61–67. 10.1016/j.paid.2019.02.031 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dumas J. E., Nissley J., Nordstrom A., Smith E. P., Prinz R. J., Levine D. W. (2005). Home chaos: sociodemographic, parenting, interactional, and child correlates. Journal of Clinical Child and Adolescent Psychology, 34(1), 93–104. 10.1207/s15374424jccp3401_9 [DOI] [PubMed] [Google Scholar]
- Dvorsky M. R., Breaux R., Becker S. P. (2020). Finding ordinary magic in extraordinary times: child and adolescent resilience during the COVID-19 pandemic. European Child & Adolescent Psychiatry, 1–3. Advance online publication. 10.1007/s00787-020-01583-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dyb G., Jensen T. K., Nygaard E. (2011). Children’s and parents’ posttraumatic stress reactions after the 2004 tsunami. Clinical Child Psychology and Psychiatry, 16(4), 621–634. 10.1177/1359104510391048 [DOI] [PubMed] [Google Scholar]
- Ellis W. E., Dumas T. M., Forbes L. M. (2020). Physically isolated but socially connected: psychological adjustment and stress among adolescents during the initial COVID-19 crisis. Canadian Journal of Behavioural Science / Revue Canadienne Des Sciences du Comportement, 52(3), 177–187. 10.1037/cbs0000215 [DOI] [Google Scholar]
- Ellis W. E., Zarbatany L. (2017). Understanding processes of peer clique influence in late childhood and early adolescence. Child Development Perspectives, 11(4), 227–232. 10.1111/cdep.12248 [DOI] [Google Scholar]
- Epstein N. B., Baldwin L. M., Bishop D. S. (1983). The McMaster family assessment device. Journal of Marital and Family Therapy, 9(2), 171–180. 10.1111/j.1752-0606.1983.tb01497.x [DOI] [Google Scholar]
- Evans G. W., Wachs T. D. (Eds.) (2010). Chaos and its influence on children's development: an ecological perspective. American Psychological Association. [Google Scholar]
- Feldman R. (2012). Bio-behavioral synchrony: a model for integrating biological and microsocial behavioral processes in the study of parenting. Parenting, 12(2-3), 154–164. 10.1080/15295192.2012.683342 [DOI] [Google Scholar]
- Fisak B., Holderfield K. G., Douglas-Osborn E., Cartwright-Hatton S. (2012). What do parents worry about? Examination of the construct of parent worry and the relation to parent and child anxiety. Behavioural and Cognitive Psychotherapy, 40(5), 542–557. 10.1017/S1352465812000410 [DOI] [PubMed] [Google Scholar]
- Gartstein M. A., Bridgett D. J., Dishion T. J., Kaufman N. K. (2009). Depressed mood and maternal report of child behavior problems: another look at the depression-distortion hypothesis. Journal of Applied Developmental Psychology, 30(2), 149–160. 10.1016/j.appdev.2008.12.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gemelas J., Davison J., Ing S. (2021). Inequities in employment by race, ethnicity, and sector during COVID-19. Journal of Racial and Ethnic Health Disparities, 1–6. Advance online publication. 10.1007/s40615-021-00963-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goodman S. H., Garber J. (2017). Evidence-based interventions for depressed mothers and their young children. Child Development, 88(2), 368–377. 10.1111/cdev.12732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grimm A., Hulse L., Preiss M., Schmidt S. (2012). Post- and peritraumatic stress in disaster survivors: an explorative study about the influence of individual and event characteristics across different types of disasters. European Journal of Psychotraumatology, 3(1), 7382. 10.3402/ejpt.v3i0.7382 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gruhn M. A., Compas B. E. (2020). Effects of maltreatment on coping and emotion regulation in childhood and adolescence: a meta-analytic review. Child Abuse & Neglect, 103, 104446. 10.1016/j.chiabu.2020.104446 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hausman E. M., Black S. R., Bromet E., Carlson G., Danzig A., Kotov R., Klein D. N. (2020). Reciprocal effects of maternal and child internalizing symptoms before and after a natural disaster. Journal of Family Psychology, 34(7), 836–845. 10.1037/fam0000653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes A. F. (2017). Introduction to mediation, moderation, and conditional process analysis (2nd edn). The Guilford Press. [Google Scholar]
- Holtzman S., O'Connor B. P., Barata P. C., Stewart D. E. (2015). The Brief Irritability Test (BITe): a measure of irritability for use among men and women. Assessment, 22(1), 101–115. 10.1177/1073191114533814 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L. T., Bentler P. M. (1999). Cutoff criteria for fit indexes in covariance structure analysis: conventional criteria versus new alternatives. Structural Equation Modeling: A Multidisciplinary Journal, 6(1), 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Hughes E. K., Gullone E. (2010). Reciprocal relationships between parent and adolescent internalizing symptoms. Journal of Family Psychology, 24(2), 115–124. 10.1037/a0018788 [DOI] [PubMed] [Google Scholar]
- Imran N., Aamer I., Sharif M. I., Bodla Z. H., Naveed S. (2020). Psychological burden of quarantine in children and adolescents: a rapid systematic review and proposed solutions. Pakistan Journal of Medical Sciences, 36(5), 1106–1116. 10.12669/pjms.36.5.3088 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiao W. Y., Wang L. N., Liu J., Fang S. F., Jiao F. Y., Pettoello-Mantovani M., Somekh E. (2020). Behavioral and emotional disorders in children during the COVID-19 epidemic. The Journal of Pediatrics, 221, 264–266.e1. 10.1016/j.jpeds.2020.03.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein R. B. (2016). Specification and identification of confirmatory factor analysis model. In Little T. D. (Ed.), Principals and practice of structural equation modeling (4th edn, pp. 188–225). The Guilford Press. [Google Scholar]
- Kroes G., Veerman J. W., De Bruyn E. E. J. (2003). Bias in parental reports? Maternal psychopathology and the reporting of problem behavior in clinic-referred children. European Journal of Psychological Assessment, 19(3), 195–203. 10.1027/1015-5759.19.3.195 [DOI] [Google Scholar]
- Kuehner C. (2017). Why is depression more common among women than among men? The Lancet Psychiatry, 4(2), 146–158. 10.1016/S2215-0366(16)30263-2 [DOI] [PubMed] [Google Scholar]
- Lai B. S., Kelley M. L., Harrison K. M., Thompson J. E., Self-Brown S. (2015). Posttraumatic stress, anxiety, and depression symptoms among children after Hurricane Katrina: a latent profile analysis. Journal of Child and Family Studies, 24(5), 1262–1270. 10.1007/s10826-014-9934-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu X., Tang B., Zhao F., Xue C., Dong J., Zhang L. (2020). Post-traumatic positive and negative psychological changes experienced by child and adolescent earthquake survivors in remote rural western China: a cross-sectional study six years after the Yushu earthquake. Psychology, Health, & Medicine, 26(2), 184–195. 10.1080/13548506.2020.1738020. [DOI] [PubMed] [Google Scholar]
- Marchetti D., Fontanesi L., Mazza C., Di Giandomenico S., Roma P., Verrocchio M. C. (2020). Parenting-related exhaustion during the Italian COVID-19 lockdown. Journal of Pediatric Psychology, 45(10), 1114–1123. 10.1093/jpepsy/jsaa093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcynyszyn L. A., Evans G. W., Eckenrode J. (2008). Family instability during early and middle adolescence. Journal of Applied Developmental Psychology, 29(5), 380–392. 10.1016/j.appdev.2008.06.001 [DOI] [Google Scholar]
- Mazza C., Ricci E., Marchetti D., Fontanesi L., Giandomenico S., Di, Verrocchio M. C., Roma P. (2020). How personality relates to distress in parents during the COVID-19 lockdown: the mediating role of child’s emotional and behavioral difficulties and the moderating effect of living with other people. International Journal of Environmental Research and Public, 17(17), 6236. 10.3390/ijerph17176236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miller I. W., Epstein N. B., Bishop D. S., Keitner G. I. (1985). The McMaster family assessment device: reliability and validity. Journal of Marital and Family Therapy, 11(4), 345–356. 10.1111/j.1752-0606.1985.tb00028.x [DOI] [Google Scholar]
- Millett G. A., Jones A. T., Benkeser D., Baral S., Mercer L., Beyrer C., Honermann B., Lankiewicz E., Mena L., Crowley J. S., Sherwood J., Sullivan P. S. (2020). Assessing differential impacts of COVID-19 on black communities. Annals of Epidemiology, 47, 37–44. 10.1016/j.annepidem.2020.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L. K., Muthén B. O. (2017). Mplus user’s guide (8th edn). Muthén & Muthén. https://www.statmodel.com/HTML_UG/introV8.htm. [Google Scholar]
- Neill E. L., Weems C. F., Scheeringa M. S. (2018). CBT for child PTSD is associated with reductions in maternal depression: evidence for bidirectional effects. Journal of Clinical Child and Adolescent Psychology, 47(3), 410–420. 10.1080/15374416.2016.1212359 [DOI] [PubMed] [Google Scholar]
- Orengo-Aguayo R., Stewart R. W., de Arellano M. A., Suárez-Kindy J. L., Young J. (2019). Disaster exposure and mental health among Puerto Rican youths after Hurricane Maria. JAMA Network Open, 2(4), e192619. 10.1001/jamanetworkopen.2019.2619 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterman A., Potts A., Donnell, Thompson K., M O., Shah N., Oertelt-Prigione S., Van G., N. (2020). Pandemics and violence against women and children. Center for Global Development, 528, 43. https://www.cgdev.org/publication/pandemics-and-violence-against-women-and-children [Google Scholar]
- PharesV., , LopezE., , FieldsS., , KamboukosD., & , Duhig A. M. (2005). Are fathers involved in pediatric psychology research and treatment?. Journal of Pediatric Psychology, 30(8), 631–643. 10.1093/jpepsy/jsi050 [DOI] [PubMed] [Google Scholar]
- Rapee R. M., Oar E. L., Johnco C. J., Forbes M. K., Fardouly J., Magson N. R., Richardson C. E. (2019). Adolescent development and risk for the onset of social-emotional disorders: a review and conceptual model. Behaviour Research and Therapy, 123, 103501. 10.1016/j.brat.2019.103501 [DOI] [PubMed] [Google Scholar]
- Raposa E. B., Hammen C. L., Brennan P. A. (2011). Effects of child psychopathology on maternal depression: the mediating role of child-related acute and chronic stressors. Journal of Abnormal Child Psychology, 39(8), 1177–1186. 10.1007/s10802-011-9536-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Remmerswaal D., Muris P. (2011). Children's fear reactions to the 2009 swine flu pandemic: the role of threat information as provided by parents. Journal of Anxiety Disorders, 25(3), 444–449. 10.1016/j.janxdis.2010.11.008 [DOI] [PubMed] [Google Scholar]
- Rubens S. L., Felix E. D., Hambrick E. P. (2018). A meta‐analysis of the impact of natural disasters on internalizing and externalizing problems in youth. Journal of Traumatic Stress, 31(3), 332–341. 10.1002/jts.22292 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell B. S., Hutchison M., Tambling R., Tomkunas A. J., Horton A. L. (2020). Initial challenges of caregiving during COVID-19: caregiver burden, mental health, and the parent–child relationship. Child Psychiatry and Human Development, 51(5), 671–682. 10.1007/s10578-020-01037-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sharpley C. F., Christie D. R. (2007). How I was then and how I am now’: current and retrospective self‐reports of anxiety and depression in Australian women with breast cancer. Psycho-Oncology, 16(8), 752–762. 10.1002/pon.1125 [DOI] [PubMed] [Google Scholar]
- Shorer M., Leibovich L. (2020). Young children’s emotional stress reactions during the COVID-19 outbreak and their associations with parental emotion regulation and parental playfulness. Early Child Development and Care, 1–11. Advance online publication. 10.1080/03004430.2020.1806830 [DOI] [Google Scholar]
- Spinelli M., Lionetti F., Pastore M., Fasolo M. (2020). Parents’ stress and children’s psychological problems in families facing the COVID-19 outbreak in Italy. Frontiers in Psychology, 11(July), 1713–1717. 10.3389/fpsyg.2020.01713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sprang G., Silman M. (2013). Posttraumatic stress disorder in parents and youth after health-related disasters. Disaster Medicine and Public Health Preparedness, 7(1), 105–110. 10.1017/dmp.2013.22 [DOI] [PubMed] [Google Scholar]
- Stringaris A., Goodman R., Ferdinando S., Razdan V., Muhrer E., Leibenluft E., Brotman M. A. (2012). The Affective Reactivity Index: a concise irritability scale for clinical and research settings. Journal of Child Psychology and Psychiatry, and Allied Disciplines, 53(11), 1109–1117. 10.1111/j.1469-7610.2012.02561.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sturge-Apple M. L., Davies P. T., Cicchetti D., Hentges R. F., Coe J. L. (2017). Family instability and children's effortful control in the context of poverty: sometimes a bird in the hand is worth two in the bush. Development and Psychopathology, 29(3), 685–696. 10.1017/S0954579416000407 [DOI] [PubMed] [Google Scholar]
- Thabrew H., Stasiak K., Bavin L. M., Frampton C., Merry S. (2018). Validation of the Mood and Feelings Questionnaire (MFQ) and Short Mood and Feelings Questionnaire (SMFQ) in New Zealand help‐seeking adolescents. International Journal of Methods in Psychiatric Research, 27(3), e1610. 10.1002/mpr.1610 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tichovolsky M. H., Griffith S. F., Rolon-Arroyo B., Arnold D. H., Harvey E. A. (2018). A longitudinal study of fathers’ and young children’s depressive symptoms. Journal of Clinical Child and Adolescent Psychology, 47(sup1), S190–S204. 10.1080/15374416.2016.1212357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Twenge J. M., Nolen-Hoeksema S. (2002). Age, gender, race, socioeconomic status, and birth cohort difference on the children's depression inventory: a meta-analysis. Journal of Abnormal Psychology, 111(4), 578–588. 10.1037/0021-843X.111.4.578 [DOI] [PubMed] [Google Scholar]
- United States Census Bureau (2019). QuickFacts: New Orleans, Louisiana. https://www.census.gov/quickfacts/neworleanscitylouisiana.
- Usher K., Bhullar N., Durkin J., Gyamfi N., Jackson D. (2020). Family violence and COVID-19: increased vulnerability and reduced options for support. International Journal of Mental Health Nursing, 29(4), 549–552. 10.1111/inm.12735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasserstein S. B., La Greca A. M. (1998). Hurricane Andrew: parent conflict as a moderator of children's adjustment. Hispanic Journal of Behavioral Sciences, 20(2), 212–224. 10.1177/07399863980202005 [DOI] [Google Scholar]
- Webster-Stratton C., Hammond M. (1999). Marital conflict management skills, parenting style, and early-onset conflict problems: processes and pathways. Journal of Child Psychology and Psychiatry, and Allied Disciplines 40(6), 917–927. 10.1111/1469-7610.00509 [DOI] [PubMed] [Google Scholar]
- Wu M., Xu W., Yao Y., Zhang L., Guo L., Fan J., Chen J. (2020). Mental health status of students’ parents during COVID-19 pandemic and its influence factors. General Psychiatry, 33(4), e100250. 10.1136/gpsych-2020-100250 [DOI] [PMC free article] [PubMed] [Google Scholar]