To the Editor:
The presence of entrapped megakaryocytes in the capillaries of brain tissues obtained from victims of the COVID-19 pandemic has been recently described (1). This finding has prompted speculation that entrapped megakaryocytes may contribute to COVID-19-associated neurological sequelae, including the so-called “fog” that is seen in a subset of COVID-19 patients (1). Post-COVID neurological sequelae remain poorly defined, but bear at least some resemblance to prior reports of post-sepsis cognitive complications (2). Circulating megakaryocytes themselves were first described over a century ago (3) and have been found in histopathologic sections across a number of organs (3–5). While previously unrecognized in brain tissues, their presence in a variety of tissues and apparent enrichment during different pathophysiologic states is well-described (3–14). Circulating megakaryocytes are most often recognized in the lungs, where they have a well-established role in peripheral thrombopoiesis (6, 7). Perturbations to lung physiology, such as those that are known to occur in acute COVID-19 disease, have been shown to substantially alter megakaryocyte dynamics as well as platelet production (8–14). This intimate connection between megakaryocytes and the lung, along with prior reports of similar cognitive deficits in sepsis (2), raise the possibility that their presence in brain capillaries is not limited to cases of COVID-19, and that they may be seen in other disease states resulting in lung injury and/or systemic inflammation.
We therefore performed a review of autopsy cases from both infectious and non-infectious causes of diffuse alveolar damage (DAD), including COVID-19, in order to examine brain tissue sections for megakaryocytes and assess whether this recent finding was indeed specific to COVID-19. A total of 18 autopsy cases were selected for review of brain histology. These included 5 COVID-19, 5 influenza, 4 non-infectious DAD, and 4 control cases with no report of lung injury. Each case had at least 4 slides of brain tissue for review, and the sections were taken from a variety of anatomic locations. A total of 121 slides were reviewed (33 COVID-19, 43 Influenza, 19 DAD, and 26 Control). Slides were reviewed at 10× magnification in a Z-scanning method to cover the entire tissue section, and each slide was reviewed twice. The number of megakaryocytes per case, as well as the location and number per slide, were tabulated. Clinical demographics, including patient age and sex, the range of platelet count during admission, and admission days were also noted.
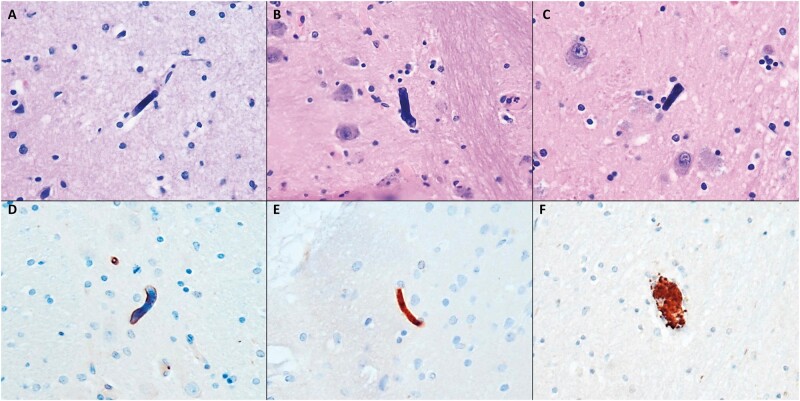
As hypothesized, megakaryocytes were identified in all classes of acute lung injury at essentially the same frequency regardless of cause. Megakaryocytes were seen in 2/5 (40%) cases of COVID-19, 2/5 (40%) cases of influenza, 3/4 (75%) cases of non-infectious DAD, and 0/4 control cases (Fig. 1, Table). Megakaryocytes were found in a more-or-less random distribution, including the frontal cortex, basal ganglia, hippocampus, pons, midbrain, and thalamus. The density of megakaryocytes varied across different cases, with a range of 0–3 per tissue section across all cases. In both a COVID-19 case and an influenza case, 2 megakaryocytes were present within the same high-power field. A case of influenza exhibited the highest density of megakaryocytes with a total of 3 seen in a single tissue section and 6 seen across all of the slides submitted for the case. Megakaryocytes were universally present as naked nuclei entrapped in small capillaries, similar to Nauen et al.’s observations (1) (Fig. 1). CD42b and CD61 immunostains confirmed the morphologic impression of megakaryocytes, and numerous platelet-rich thrombi were seen across the cases assessed by these immunostains (Fig. 1D–F). Platelet counts varied substantially across the assessed patients, but all forms of lung injury exhibited some degree of thrombocytopenia during admission. In all but one of the patients where megakaryocytes were seen, the final platelet count was less than 100 k/µL. There was no apparent association between patient age, sex, or admission length.
FIGURE 1.
(A–C) Representative hematoxylin and eosin images of megakaryocytes identified in brain sections of COVID-19 (A), influenza (B), and non-infectious DAD (C). (D and E) CD42b (D) and CD61 (E) immunostaining highlights entrapped megakaryocytes. (F) Several platelet-rich clots were seen in both CD42b and CD61 immunostains in cases of acute lung injury. All images were taken at 400× magnification.
TABLE.
Summary of Clinical and Experimental Data for the Study
| Case | Age/Sex | Admission Days | Slides | Slides With MK | Megakaryocytes | Regions | PLT Count Range (k/µL) |
|---|---|---|---|---|---|---|---|
| COVID-1 | 23 M | 26 | 4 | NA | 0 | 57–421 (Final: 248) | |
| COVID-2 | 39 M | 5 | 7 | NA | 0 | 107–315 (Final: 124) | |
| COVID-3 | 69 F | 11 | 7 | NA | 0 | 2–80 (Final: 2) | |
| COVID-4 | 57 M | 21 | 6 | 3 | 5 | Frontal cortex, basal ganglia | 21–56 (Final: 56) |
| COVID-5 | 63 F | 5 | 9 | 1 | 1 | Hippocampus | 42–178 (Final: 42) |
| FLU-1 | 84 M | 4 | 7 | NA | 0 | 71–87 (Final: 87) | |
| FLU-2 | 48 F | 3 | 5 | 3 | 6 | Pons, midbrain, hippocampus | 6–187 (Final: 82) |
| FLU-3 | 40 F | 2 | 12 | 1 | 1 | Pons | 23–163 (Final: 163) |
| FLU-4 | 17 M | 1 | 7 | NA | 0 | 70 (only 1 count) | |
| FLU-5 | 48 M | 11 | 12 | NA | 0 | 10–202 (Final: 46) | |
| DAD-1 | 57 M | 2 | 5 | 2 | 2 | Midbrain, frontal cortex | 29–104 (Final: 70) |
| DAD-2 | 65 M | 11 | 5 | NA | 0 | 6–43 (Final: 30) | |
| DAD-3 | 65 M | 3 | 4 | 2 | 2 | Thalamus | 60–206 (Final: 95) |
| DAD-4 | 85 M | >60 | 5 | 1 | 1 | Occipital cortex | 8–325 (Final: 8) |
| Control—HF | 66 F | 5 | 6 | NA | 0 | 206–335 (Final: 206) | |
| Control—Met Ca | 70 M | 2 | 7 | NA | 0 | 112–174 (Final: 126) | |
| Control—HF2 | 63 F | 4 | 6 | NA | 0 | 190–314 (Final: 190) | |
| Control—SCD | 74 M | <1 | 7 | NA | 0 | NA |
COVID, SARS-CoV2-associated disease; FLU, seasonal influenza; DAD, non-infectious diffuse alveolar damage; HF, heart failure; Met Ca, metastatic carcinoma; SCD, sudden cardiac death; NA, not applicable; PLT, platelet; MK, megakaryocytes.
Our brief data expand on the currently limited knowledge regarding the presence of megakaryocytes in the brain microvasculature, and demonstrates the phenomenon of megakaryocytes entrapped in the vasculature of the brain is not limited to COVID-19. The cause and effect of circulating megakaryocytes is still a matter of debate, but since the lung is the principle site of peripheral entrapment it is possible that any insult to lung architecture or physiology could potentially perturb the dynamics of circulating megakaryocytes. One potential explanation for their increased presence in the systemic circulation following lung injury is altered adherence within the pulmonary vasculature, as cardiopulmonary bypass itself has been demonstrated to result in increased arterial megakaryocytes (15). It is also possible that these megakaryocytes are increased as a result of systemic inflammation in order to exert immunomodulatory or repair activities through the platelets they produce (10–13, 16). We cannot exclude or confirm that entrapped megakaryocytes are present in other disease states resulting in systemic inflammation, thromboembolic disease, or in cases of malignancy. It is possible that entrapped megakaryocytes in the brain could contribute to neurological sequelae observed across different diseases including COVID-19, sepsis, and other similar conditions. Platelets are also known to exert numerous effects apart from thrombopoietic functions (16), and despite being recognized in the literature across a variety of organs, the significance of megakaryocytes in peripheral tissues is still largely uncertain and speculative. Further studies are needed in this regard. What was once described as an idle curiosity in tissue sections (4), it is becoming clearer that megakaryocytes and platelets may be involved a spectrum of activities in a variety of locations outside of canonical thinking.
The authors collectively have no relevant financial disclosures.
The authors have no conflicts of interest to declare.
REFERENCES
- 1.Nauen DW, Hooper JE, Stewart CM, et al. Assessing brain capillaries in coronavirus disease. JAMA Neurol 2019;2021:e210225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Annane D, Sharshar T. Cognitive decline after sepsis. Lancet Respir Med 2015;3:61–9 [DOI] [PubMed] [Google Scholar]
- 3.Slater D, Martin J, Trowbridge A. Circulating megakaryocytes. Histopathology 1983;7:136–40 [DOI] [PubMed] [Google Scholar]
- 4.Brill R, Halpern MM. The frequency of megakaryocytes in autopsy sections. Blood 1948;3:286–91 [PubMed] [Google Scholar]
- 5.Pedersen NT. Occurrence of megakaryocytes in various vessels and their retention in the pulmonary capillaries in man. Scand J Haematol 1978;21:369–75 [DOI] [PubMed] [Google Scholar]
- 6.Levine RF, Shoff P, Han ZC, et al. Circulating megakaryocytes and platelet production in the lungs. Prog Clin Biol Res 1990;356:41–52 [PubMed] [Google Scholar]
- 7.Woods MJ, Greaves M, Trowbridge EA. The physiological significance of circulating megakaryocytes. Br J Haematol 1992;80:266–7 [DOI] [PubMed] [Google Scholar]
- 8.Da Xiao W, Yang M, Yang J, et al. Lung damage may induce thrombocytopenia. Platelets 2006;17:347–9 [DOI] [PubMed] [Google Scholar]
- 9.Mandal RV, Mark EJ, Kradin RL. Megakaryocytes and platelet homeostasis in diffuse alveolar damage. Exp Mol Pathol 2007;83:327–31 [DOI] [PubMed] [Google Scholar]
- 10.Hansen M, Pedersen NT. Circulating megakaryocytes in patients with pulmonary inflammation and in patients subjected to cholecystectomy. Scand J Haematol 1979;23:211–6 [DOI] [PubMed] [Google Scholar]
- 11.Couldwell G, Machlus KR. Modulation of megakaryopoiesis and platelet production during inflammation. Thromb Res 2019;179:114–20 [DOI] [PubMed] [Google Scholar]
- 12.Behrens K, Alexander WS. Cytokine control of megakaryopoiesis. Growth Factors 2018;36:89–103 [DOI] [PubMed] [Google Scholar]
- 13.Sulkowski S, Terlikowski S, Sulkowska M. Occlusion of pulmonary vessels by megakaryocytes after treatment with tumour necrosis factor-alpha (TNF-alpha). J Comp Pathol 1999;120:235–45 [DOI] [PubMed] [Google Scholar]
- 14.Dziecioł J, Debek W, Chyczewski L, et al. Megakaryocytes in the acute stage of experimental hemorrhagic shock. Part I. Megakaryocytes circulating in the blood. Rocz Akad Med Bialymst 1995;40:88–93 [PubMed] [Google Scholar]
- 15.Wilde NT, Burgess R, Keenan DJ, et al. The effect of cardiopulmonary bypass on circulating megakaryocytes. Br J Haematol 1997;98:322–7 [DOI] [PubMed] [Google Scholar]
- 16.Kapur R, Semple JW. The nonhemostatic immune functions of platelets. Semin Hematol 2016;53 Suppl 1:S2–6 [DOI] [PubMed] [Google Scholar]