Abstract
Background
We aimed to investigate the determinants of Health-related quality of life (HRQOL) in Iranian patients with celiac disease (CD) using the structural equation modeling (SEM).
Methods
In the present cross-sectional study, a total of 170 adult patients with CD were recruited. The information regarding adherence to diet, symptom severity, and HRQOL were collected using the celiac disease adherence test (CDAT), gastrointestinal symptom rating scale (GSRS), and SF-36 questionnaire respectively. Association between various studied variables and HRQOL was assessed using SEM. The standardized regression weights were used to assess total, direct and indirect effects. The model fit indices were used to assess the “goodness of fit” between the hypothesized models.
Results
The mean age of participants was 37.57 ± 9.59 years. The results of SEM indicated that the overall fit of our model was acceptable. Adherence to the diet, GSRS score, occupation, and education level was significantly related to PCS of SF-36; and adherence to the diet, GSRS score, and education level were significantly correlated with MCS of SF-36. The analysis of indirect associations indicated that only adherence to diet indirectly via GSRS score was significantly associated with PCS and MCS of SF-36.
Conclusion
In adult patients with celiac disease, HRQOL was associated with age, education, adherence to GFD, and GSRS score. Additionally, occupation and disease duration were associated with HRQOL only in women and men respectively.
Keywords: Coeliac disease, Quality of life, Structural equation modeling
Background
Celiac disease (CD) is a common disorder that is caused by autoimmunity to the gluten protein. It affects about 0.7 to 1% of the population worldwide [1] and its prevalence in Iran is about 2% [2]. Eliminating Gluten-containing foods and products is the only effective and safe treatment [3]. Considering the chronic nature of this disease and since lifelong adherence to gluten-free diet (GFD) is demanding and costly, the quality of life of these patients is affected.
Different demographic, disease related and treatment–related factors can affect the quality of life in patients with celiac disease. One of the important factors is adherence to GFD. In various studies in children and adults, it has been shown that adherence to a gluten-free diet (GFD) had a positive effect on improving symptoms and health-related quality of life (HRQOL) in patients with celiac disease [4–6]. However, considering the limitations of this diet, it can also negatively affect the quality of life. In addition to the treatment effect, other determinant factors were also reported that affect the quality of life in these patients. These factors including demographic factors such as education level, employment status; and disease-related factors such as the presence of comorbidities and disease duration, and presence of symptoms [7, 8]. For example, in a study in Spain, it has been shown that age, gender, and GFD duration were factors that independently associated with HRQOL in Spain [9]. In addition, previous studies have indicated that symptom severity also affects the quality of life in celiac patients. For instance, Usai et al. indicated that there was a negative association between the number of symptoms and comorbidities and HRQOL in patients with celiac disease [10].
To the best of our knowledge, no study in Iran has assessed the determinant factors that affect the HRQOL in Iranian celiac patients. Moreover, most of the previous studies in patients with celiac disease have only reported the direct correlation between different factors and HRQOL. By means of this method, only the direct association of various variables on the outcome can be assessed. However, the exploration of indirect effects could offer new findings in the relationship between different demographic and disease-related factors and HRQOL in patients with celiac disease. So, in the present study, we used structural equation modeling that enables analysis of the interrelationship of independent variables and their direct and indirect associations through other variables. Considering that the HRQOL is affected by different variables, defining its determinants through this technique is beneficial.
Therefore, for the first time, we employed the structural equation modeling (SEM) technique for investigating the determinants of HRQOL in Iranian patients with celiac disease. In the current investigation, we analyzed the relationship between different demographic and disease-related factors and HRQOL in patients with celiac disease; and applied the SEM technique to determine the effect of these variables on HRQOL in a hypostatized model.
Materials and methods
In the present cross-sectional study, the adult patients were selected randomly from the East-Azerbaijan celiac disease registry database. In this registry, the patients were registered if they have a positive serology test confirmed by compatible duodenal histological findings. The patients were included in the present study if they aged more than 18 years old, and were on GFD for at least 6 months.
The sample size for the present study was calculated based on the Bentler recommendation [11] with a minimum of ten observations per estimated parameters. So, we needed a sample size of 90 participants at least. In the present study, a total of 170 participants was recruited.
The Ethics Committee of Tabriz University of medical sciences (IR.TBZMED.REC.1399.904) approved the study and all participants gave written informed consent.
Variables
The information regarding demographic characteristics including age, education level, employment status, marital status was obtained by an expert researcher using a questionnaire.
Medical records were used to gather information regarding comorbidities such as diabetes mellitus, cancers, chronic kidney diseases, chronic liver diseases, autoimmune diseases, inflammatory diseases, and psychological disorders.
Adherence to diet was assessed using the celiac disease adherence test (CDAT) questionnaire [12]. This questionnaire assesses the level of adherence to gluten-free diet using seven questions on the five Likert scale and the total score ranged between seven and 35. We considered a CDAT score of < 13 as good adherence, 13–17 as moderate adherence, and > 17 as poor adherence to GFD [13]. This questionnaire was previously translated to Persian, and its validity was confirmed in the previous study [12].
The severity of gastrointestinal symptoms was assessed by the Persian version of the gastrointestinal symptom rating scale (GSRS) questionnaire [14]. This questionnaire includes fifteen questions on a seven-point Likert scale and higher scores indicate more severe symptoms. The questionnaire assesses five domains including diarrhea, constipation, abdominal pain, reflux, and indigestion.
The HRQOL was assessed using the SF-36 questionnaire. This questionnaire is a 36-item questionnaire that assesses physical [Physical Component Summary (PCS)) and psychological (Mental Component Summary (MCS)] health with a higher score indicating better health. This questionnaire was previously translated to Persian, and its validity was confirmed [15].
Statistical analysis
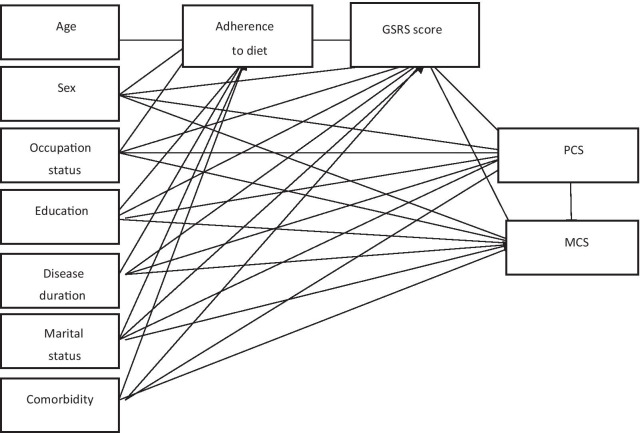
All analysis was performed using STATA-16. The normality of data distribution was assessed using the Kolmogorov–Smirnov test. The continuous variables were presented as mean ± SD and the categorical variable was presented as frequency (%). An independent t-test and chi-square were used to compare the continuous variables and nominal and categorical variables between males and females respectively. Association between sociodemographic factors, disease-related factors, and quality of life was assessed using structural equation modeling (SEM). As can be seen in the conceptual model (Fig. 1), adherence to diet and GSRS score were considered mediators. The standardized regression weights were used to assess the total, direct and indirect effects of variables on the HRQOL. The model fit was assessed to determine the “goodness of fit” between the hypothesized model and the data by use of several methods including the ratio of chi-square to the degree of freedom, root-mean-squared error of approximation (RMSEA), comparative fit index (CFI); and standardized root mean squared residual (SRMR). The acceptable values were Chi-square/DF < 5, RMSEA < 0.08, CFI > 0.9, SRMR < 0.08. A p value less than 0.05 was considered significant.
Fig. 1.
Hypothesized structural models
Results
In the present study, 170 patients with celiac disease with a mean age of 37.57 ± 9.59 were studied. Of them, 103 (60.58%) were female, and 119 (70%) were married. The mean disease duration was 4.52 ± 3.36 years. There were statistically significant differences between males and females regarding marital status, employment status, mean PCS and MCS, and CDAT scores (Table 1).
Table 1.
Baseline demographic and clinical characteristics of patients with celiac disease
| Variable | Total (n = 170) | Male (n = 67) | Female (n = 103) | p value |
|---|---|---|---|---|
| Age (years) | 37.57 ± 9.59 | 36.12 ± 10.44 | 38.9 ± 9.04 | 0.19 |
| Education status n (%) | ||||
| ≤ Diploma | 97 (57.05) | 33 (49.2) | 64 (62.1) | 0.07 |
| College | 73 (42.9) | 34 (50.7) | 39 (37.8) | |
| Marital status n (%) | ||||
| Single | 51 (30.0) | 28 (41.7) | 23 (22.3) | 0.004 |
| Married | 119 (70.0) | 39 (58.2) | 80 (77.6) | |
| Employed | 83 (48.8) | 50 (74.6) | 33 (32.03) | < 0.001 |
| Disease duration (year) | 4.52 ± 3.36 | 4.28 ± 3.66 | 4.65 ± 3.19 | 0.54 |
| Family history of CD, n (%) | 13 (7.6) | 6 (8.9) | 7 (6.7) | 0.79 |
| CDAT score | 15.55 ± 4.04 | 14.29 ± 3.59 | 16.26 ± 4.13 | 0.005 |
| Adherence to diet | 40 (23.5) | 22 (32.8) | 18 (17.4) | 0.10 |
| Presence of comorbidities, n (%) | 51 (30) | 21 (31.9) | 30 (29.1) | 0.41 |
| GSRS score | 30.18 ± 20.54 | 27.70 ± 19.96 | 31.59 ± 20.85 | 0.30 |
| PCS | 235.26 ± 92.88 | 266.27 ± 87.54 | 217.71 ± 91.70 | 0.004 |
| MCS | 218.01 ± 87.84 | 240.81 ± 90.57 | 205.10 ± 84.09 | 0.02 |
GSRS, Gastrointestinal Symptom Rating Scale; PCS, physical component summary; MCS, mental component summary; CDAT, celiac disease adherence test
Structural equation modeling
In the present study, the overall fit of our model was acceptable (RMSEA [95% CI] 0.00 [0.00, 0.10]; Chi-square:2.24; DF: 4, Chi-square/df: 0.56; CF:1; and SRMR:0.02).
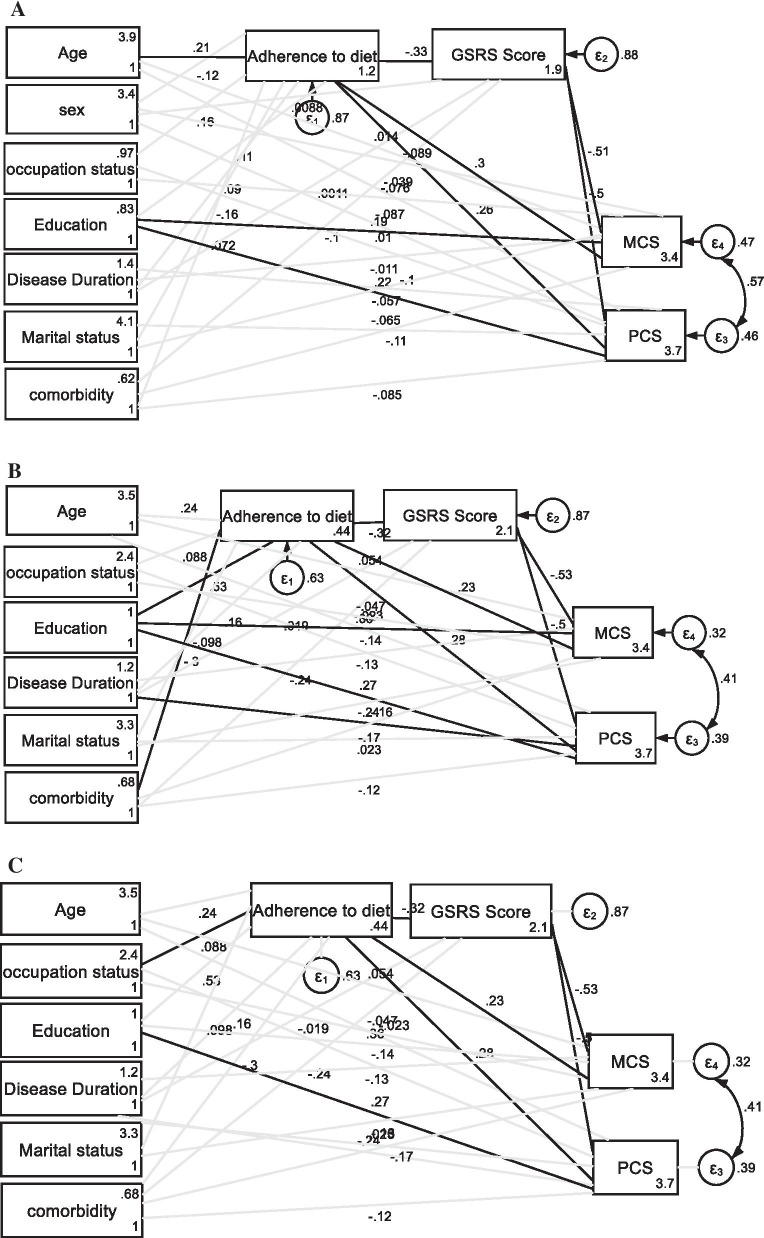
As presented in Table 2, the result of SEM analysis indicated that adherence to the diet, GSRS score, occupation, and education level were significantly related to PCS of SF-36; and adherence to the diet, GSRS score, and education level were significantly correlated to MCS of SF-36. The analysis of indirect association indicated that only adherence to diet indirectly via GSRS score was significantly associated with PCS and MCS of SF-36 (Fig. 2a).
Table 2.
Total, direct and indirect effects of independent variables on dependent variables
| Variables | SF-36 domains | Effect | Age SPC | Sex | Occupation | Education level | Marital status | Disease duration | Comorbidity | Adherence to diet | GSRS |
|---|---|---|---|---|---|---|---|---|---|---|---|
| SPC | SPC | SPC | SPC | SPC | SPC | SPC | SPC | SPC | |||
| Total | PCS | Total | 0.47 | − 26.94 | 14.42* | 50.62* | − 28.76 | − 1.73 | − 13.37 | 52.43* | − 2.27* |
| Direct | − 0.37 | − 16.78 | 1.85 | 41.86* | − 13.98 | − 2.75 | − 17.58 | 31.85* | − 2.27* | ||
| Indirect | 0.85 | − 10.15 | 12.57 | 8.76 | − 14.78 | 1.02 | 4.21 | 20.57* | |||
| MCS | Total | 1.02 | − 26.67 | − 0.17 | 42.41* | − 27.15 | 0.80 | − 18.65 | 54.95* | − 2.18* | |
| Direct | 0.13 | − 16.10 | − 13.35 | 33.23 | − 11.65 | − 0.27 | − 22.17 | 35.15* | − 2.18* | ||
| Indirect | 0.89 | − 10.57 | 13.17 | 9.18 | − 15.49 | 1.07 | 3.51 | 19.79* | |||
| Males | PCS | Total | 0.67 | − 24.34 | 87.45 | − 3.60 | − 3.82 | − 25.29 | 55.49 | − 2.20 | |
| Direct | − 0.19 | − 33.76 | 46.87 | 4.02 | − 5.67 | − 22.96 | 35.18 | − 2.20 | |||
| Indirect | 0.87 | 9.41 | 40.58 | − 7.62 | 1.84 | − 2.33 | 20.30 | ||||
| MCS | Total | 1.27 | − 3.08 | 103.104 | − 35.78 | − 1.47 | − 31.34 | 51.69 | − 2.39 | ||
| Direct | 0.46 | − 11.86 | 12.03 | − 28.68 | − 3.22 | − 32.80 | 29.61 | − 2.39 | |||
| Indirect | 0.81 | 8.77 | 37.80 | − 7.10 | 1.75 | 1.25 | 22.07 | ||||
| Females | PCS | Total | − 0.06 | 43.95 | 18.72 | − 39.38 | − 0.44 | 2.91 | 55.49 | − 2.45 | |
| Direct | − 0.87 | 18.25 | 33.84 | − 23.50 | 0.29 | − 1.64 | 25.31 | − 2.45 | |||
| Indirect | 0.80 | 25.70 | − 15.11 | − 15.88 | − 0.73 | 4.56 | 23.25 | ||||
| MCS | Total | 0.66 | 30.04 | − 3.27 | − 16.72 | 0.93 | − 1.78 | 49.16 | − 2.14 | ||
| Direct | − 0.15 | 4.01 | 12.03 | − 0.64 | 1.56 | − 6.21 | 28.78 | − 2.14 | |||
| Indirect | 0.81 | 26.02 | − 15.30 | − 16.10 | − 0.62 | 4.43 | 20.38 |
GSRS, Gastrointestinal Symptom Rating Scale; PCS, physical component summary; MCS, mental component summary; CDAT, celiac disease adherence test; SPC, standardized path coefficient
*Indicates significant correlation
Fig. 2.
Final structural models after testing the association between socio-demographic and clinical factors and quality of life in total population (a), males (b), and females (c). Black lines indicate significant associations and gray lines indicate insignificant association
We also analyzed the association between independent variables and PCS and MCS in males and females separately (Fig. 2b, c). As can be seen, in males, adherence to the diet, GSRS score, disease duration, and education level were directly related to PCS of SF-36; and adherence to diet and GSRS score were directly related to MCS of SF-36. The analysis of the indirect association indicated that education level and adherence to diet were also indirectly related to the PCS and MCS of SF-36.
In females, CDAT, GSRS, and education level were directly associated with PCS of SF-36; and adherence to diet and GSRS score were significantly associated with MCS of SF-36. The analysis of the indirect effect revealed that occupation and adherence to diet were significantly associated with PCS and MCS score of SF-36 (Fig. 2c).
Discussion
In the present study the result indicated that in the whole population, adherence to the diet, GSRS score, occupation, and education level was directly associated with PCS and MCS of SF-36. Previously, a meta-analysis study on 436 patients with celiac disease, showed that dietary adherence to GFD was significantly associated with both SF-36 MCS and SF-36 PCS [4]. The direct association of dietary adherence with quality of life may partly be due to reductions in depression. Previous studies indicated that GFD had a significant positive effect on depression in patients with celiac disease [16, 17]. In the present study, we also showed that in addition to the direct association, adherence to the diet was indirectly associated with PCS and MCS of SF-36 via GSRS score. Previously, it has been shown that complete adherence to the GFD may be associated with mucosal healing, which resulted in improvement of symptoms [18].
In the present study, we also showed that education level had a direct association with both components of quality of life. Moreover, in males, it was indirectly associated with the quality of life. Previous studies also showed a significant association between education level and HRQOL [19]. It has been indicated that education allows for the development of cognitive skills related to personal care [20]. Moreover, a low level of education intensifies the complications of chronic diseases because of a lack of knowledge [21]. It has been indicated that the education level is related to the higher socioeconomic status [22]. In a previous study, it has been shown that income level has a significant association with health-seeking behavior and access to health care [23], which are correlated with a higher quality of life. In addition to the direct association, education level was indirectly associated with quality of life via an effect on adherence to the diet. Previous studies in celiac disease and other diseases indicated that a high level of education has a positive association with adherence to dietary recommendations [24]. A higher education level was correlated with better adherence to the diet via higher household income and also better self‐perceived knowledge of the GFD.
We found that in males, disease duration had a negative direct association with PCS of SF-36. This finding was similar to the result of the study in Spain [9]. In other chronic diseases such as diabetes similar finding was reported [25]. In the present study, 84.6% of patients had a disease duration of more than one year. We postulated that since strict compliance to GFD may be difficult and costly, the disease may cause significant limitations and impairment of patients’ lifestyles in the long term.
In females, occupation status had a direct positive association with both domains of quality of life. Previous studies in the women population also showed a similar result in different health conditions [26–30]. In women who are working, the social well-being and functional well-being may be higher. This may be related to the greater social support available from coworkers and friends in the workplace and having a sense of normalcy due to their ability to work [31]. Besides, GFD treatment is costly [32–34]. So, employment could have a direct economic effect on preparing gluten-free foods.
This study had the following limitations. The data for this study was obtained cross-sectionally, and the causality could not be inferred. The data about the quality of life was obtained using a general questionnaire, not diseases specific questionnaire. However, this questionnaire was valid and used in many previous studies to assess the quality of life in celiac patients [4, 6, 35]. We just assessed the association between demographic and disease characteristics and quality of life in the East Azerbaijan population. Moreover, the included population is rather young. These issues may normally restrict the generalization of the results. However, the mean age was almost similar to the mean age (35.08 ± 16.78 years) of all patients who were registered in the East Azerbaijan celiac disease registry system. In addition, in the subgroup analysis, the number of male participants was rather low that may limit the power of analysis in this subgroup. However, some studies recommended at least five participants per variable [36]. Based on this recommendation, the number of males was not very low in the present study.
Conclusion
The result of SEM indicated that in adult patients with celiac disease, HRQOL was affected by age, education level, adherence to GFD, and GSRS score. Additionally, occupation and disease duration were associated with HRQOL only in women and men respectively. This structural model provides beneficial information for planning future health promotion programs in celiac patients. Moreover, considering the nature of determinants of QoL in celiac patients, the level of adherence to GFD can be studied in future interventional studies.
Acknowledgements
The authors would like to thank all patients with celiac disease who participated in this study.
Authors' contributions
Conception and design: ZN; acquisition of data: MSh, ZN; data analysis: LN, MAJ, ZN, MAF; Data interpretation: ZN, MFD, MAJ, LN; drafting the manuscript: ZN, LN; revising manuscript critically: ZN, MAJ, MFD, LN, MS; given final approval of the version to be published: ZN, LN, MAJ, MSh, MAF; Agreed to be accountable for all aspects of the work: ZN, LN, MSh, MAJ, MAF. All authors read and approved the final manuscript.
Funding
This study was funded by the Liver and Gastrointestinal Diseases Research Center, Tabriz University of Medical Sciences, Tabriz, Iran [Grant Number: 66570]. The funder had no role in the study design, data collection, analysis, decision to publish, or preparation of the manuscript.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to the institution's policy, but are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to partcipate
The Ethics Committee of Tabriz University of medical sciences (IR.TBZMED.REC.1399.904) approved the study and all participants gave written informed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Singh P, Arora A, Strand TA, Leffler DA, Catassi C, Green PH, Kelly CP, Ahuja V, Makharia GK. Global prevalence of celiac disease: systematic review and meta-analysis. Clin Gastroenterol Hepatol. 2018;16:823–836. doi: 10.1016/j.cgh.2017.06.037. [DOI] [PubMed] [Google Scholar]
- 2.Mohammadibakhsh R, Sohrabi R, Salemi M, Mirghaed MT, Behzadifar M. Celiac disease in Iran: a systematic review and meta-analysis. Electron Phys. 2017;9:3883. doi: 10.19082/3883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Caio G, Volta U, Sapone A, Leffler DA, De Giorgio R, Catassi C, Fasano A. Celiac disease: a comprehensive current review. BMC Med. 2019;17:1–20. doi: 10.1186/s12916-019-1380-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burger JP, de Brouwer B, IntHout J, Wahab PJ, Tummers M, Drenth JP. Systematic review with meta-analysis: Dietary adherence influences normalization of health-related quality of life in coeliac disease. Clin Nutr. 2017;36:399–406. doi: 10.1016/j.clnu.2016.04.021. [DOI] [PubMed] [Google Scholar]
- 5.Nikniaz Z, Farhangi MA, Hosseinifard H, Nikniaz L. Does a gluten-free diet increase body mass index and lipid profile in celiac patients? A systematic review and meta-analysis. Mediterr J Nutr Metab. 2019;12:341–352. doi: 10.3233/MNM-190314. [DOI] [Google Scholar]
- 6.Nikniaz Z, Farhangi MA, Nikniaz L. Systematic review with meta-analysis of the health-related quality of life in children with celiac disease. J Pediatr Gastroenterol Nutr. 2020;70:468–477. doi: 10.1097/MPG.0000000000002604. [DOI] [PubMed] [Google Scholar]
- 7.Casellas F, Rodrigo L, Vivancos JL, Riestra S, Pantiga C, Baudet J, Junquera F, Diví VP, Abadia C, Papo M. Factors that impact health-related quality of life in adults with celiac disease: a multicenter study. World J Gastroenterol: WJG. 2008;14:46. doi: 10.3748/wjg.14.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Norström F, Lindholm L, Sandström O, Nordyke K, Ivarsson A. Delay to celiac disease diagnosis and its implications for health-related quality of life. BMC Gastroenterol. 2011;11:1–8. doi: 10.1186/1471-230X-11-118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rodríguez-Almagro J, Hernández-Martínez A, Lucendo AJ, Casellas F, Solano-Ruiz MC, Siles-González J. Health-related quality of life and determinant factors in celiac disease: a population-based analysis of adult patients in Spain. Rev Esp Enferm Dig. 2016;108:181–189. doi: 10.17235/reed.2016.4094/2015. [DOI] [PubMed] [Google Scholar]
- 10.Usai P, Minerba L, Marini B, Cossu R, Spada S, Carpiniello B, Cuomo R, Boy M. Case control study on health-related quality of life in adult coeliac disease. Dig Liver Dis. 2002;34:547–552. doi: 10.1016/S1590-8658(02)80087-1. [DOI] [PubMed] [Google Scholar]
- 11.Bentler PM, Chou C-P. Practical issues in structural modeling. Sociol Methods Res. 1987;16:78–117. doi: 10.1177/0049124187016001004. [DOI] [Google Scholar]
- 12.Nikniaz Z, Jafarabadi MA, Ghaffarifar S, Saeedi Z, Namvar ZA, Shirmohammadi M. Psychometric properties of the Persian version of the celiac disease adherence test questionnaire. BMC Gastroenterol. 2020;20:1–6. doi: 10.1186/s12876-020-01396-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Leffler DA, Dennis M, Edwards George JB, Jamma S, Magge S, Cook EF, Schuppan D, Kelly CP. A simple validated gluten-free diet adherence survey for adults with celiac disease. Clin Gastroenterol Hepatol. 2009;7(530–536):536.e531–532. doi: 10.1016/j.cgh.2008.12.032. [DOI] [PubMed] [Google Scholar]
- 14.Mazaheri M, SadatKhoshouei M. Comparison between psychometric characteristics of persian version of the gastrointestinal symptoms rating scale in functional gastrointestinal disorders and normal groups. Govaresh. 2012;17:18–24. [Google Scholar]
- 15.Montazeri A, Goshtasebi A, Vahdaninia M, Gandek B. The Short Form Health Survey (SF-36): translation and validation study of the Iranian version. Qual Life Res. 2005;14:875–882. doi: 10.1007/s11136-004-1014-5. [DOI] [PubMed] [Google Scholar]
- 16.Sainsbury K, Mullan B, Sharpe L. Reduced quality of life in coeliac disease is more strongly associated with depression than gastrointestinal symptoms. J Psychosom Res. 2013;75:135–141. doi: 10.1016/j.jpsychores.2013.05.011. [DOI] [PubMed] [Google Scholar]
- 17.Simsek S, Baysoy G, Gencoglan S, Uluca U. Effects of gluten-free diet on quality of life and depression in children with celiac disease. J Pediatr Gastroenterol Nutr. 2015;61:303–306. doi: 10.1097/MPG.0000000000000799. [DOI] [PubMed] [Google Scholar]
- 18.Lebwohl B, Ludvigsson JF. mucosal healing and adherence to the gluten-free diet in coeliac disease. Hoboken: Wiley; 2014. [DOI] [PubMed] [Google Scholar]
- 19.Gil-Lacruz M, Gil-Lacruz AI, Gracia-Pérez ML. Health-related quality of life in young people: the importance of education. Health Qual Life Outcomes. 2020;18:1–13. doi: 10.1186/s12955-020-01446-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Burton-Jeangros C, Cullati S, Sacker A, Blane D. A life course perspective on health trajectories and transitions. Berlin: Springer; 2015. [PubMed] [Google Scholar]
- 21.Gazmararian JA, Williams MV, Peel J, Baker DW. Health literacy and knowledge of chronic disease. Patient Educ Couns. 2003;51:267–275. doi: 10.1016/S0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- 22.Everson SA, Maty SC, Lynch JW, Kaplan GA. Epidemiologic evidence for the relation between socioeconomic status and depression, obesity, and diabetes. J Psychosom Res. 2002;53:891–895. doi: 10.1016/S0022-3999(02)00303-3. [DOI] [PubMed] [Google Scholar]
- 23.Mehra S, Leffler DA, Pallav K, Tariq S, Shah S, Green PH, Hansen J, Dennis M, Kelly CP. Socioeconomic status influences celiac disease diagnosis. Gastroenterology. 2011;140:S438. doi: 10.1016/S0016-5085(11)61796-4. [DOI] [Google Scholar]
- 24.Ayele AA, Emiru YK, Tiruneh SA, Ayele BA, Gebremariam AD, Tegegn HG. Level of adherence to dietary recommendations and barriers among type 2 diabetic patients: a cross-sectional study in an Ethiopian hospital. Clin Diabetes Endocrinol. 2018;4:1–7. doi: 10.1186/s40842-018-0070-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Martino G, Catalano A, Bellone F, Russo GT, Vicario CM, Lasco A, Quattropani MC, Morabito N. As time goes by: anxiety negatively affects the perceived quality of life in patients with type 2 diabetes of long duration. Front Psychol. 2019;10:1779. doi: 10.3389/fpsyg.2019.01779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Adelmann PK, Antonucci TC, Crohan SE, Coleman LM. A causal analysis of employment and health in midlife women. Women Health. 1990;16:5–20. doi: 10.1300/J013v16n01_02. [DOI] [PubMed] [Google Scholar]
- 27.Bartley M, Sacker A, Clarke P. Employment status, employment conditions, and limiting illness: prospective evidence from the British household panel survey 1991–2001. J Epidemiol Community Health. 2004;58:501–506. doi: 10.1136/jech.2003.009878. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Minton JW, Pickett KE, Dorling D. Health, employment, and economic change, 1973–2009: repeated cross sectional study. BMJ. 2012;344:e2316. doi: 10.1136/bmj.e2316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ross CE, Mirowsky J. Does employment affect health? J Health Soc Behav. 1995;36:230–243. doi: 10.2307/2137340. [DOI] [PubMed] [Google Scholar]
- 30.Zhan Y, Wang M, Liu S, Shultz KS. Bridge employment and retirees’ health: a longitudinal investigation. J Occup Health Psychol. 2009;14:374. doi: 10.1037/a0015285. [DOI] [PubMed] [Google Scholar]
- 31.Timperi AW, Ergas IJ, Rehkopf DH, Roh JM, Kwan ML, Kushi LH. Employment status and quality of life in recently diagnosed breast cancer survivors. Psychooncology. 2013;22:1411–1420. doi: 10.1002/pon.3157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lambert K, Ficken C. Cost and affordability of a nutritionally balanced gluten-free diet: Is following a gluten-free diet affordable? Nutr Diet. 2016;73:36–42. doi: 10.1111/1747-0080.12171. [DOI] [Google Scholar]
- 33.Lee AR, Wolf RL, Lebwohl B, Ciaccio EJ, Green PH. Persistent economic burden of the gluten free diet. Nutrients. 2019;11:399. doi: 10.3390/nu11020399. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Singh J, Whelan K. Limited availability and higher cost of gluten-free foods. J Hum Nutr Diet. 2011;24:479–486. doi: 10.1111/j.1365-277X.2011.01160.x. [DOI] [PubMed] [Google Scholar]
- 35.Nikniaz Z, Jafarabadi MA, Ghaffarifar S, Ravand Z, Namvar ZA, Shirmohammadi M. The Persian Translation and validation of the celiac disease quality of life questionnaire (CDQOL) Health Qual Life Outcomes. 2021;19:1–7. doi: 10.1186/s12955-021-01694-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schumacker RE, Lomax RG. A beginner's guide to structural equation modeling. London: Psychology Press; 2004. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due to the institution's policy, but are available from the corresponding author upon reasonable request.