Abstract
Objectives
The I CARE study (Improving Care After colon canceR treatment in the Netherlands) aims to compare surgeon-led to general practitioner (GP)-led colon cancer survivorship care. Recruitment to the trial took longer than expected. In this descriptive study, recruitment is critically reviewed.
Setting
Patients were recruited from eight Dutch medical centres.
Participants
Patients treated with curative intent for stages I–III colon cancer. Target patient sample size was calculated at 300.
Interventions
Patients were randomised to surgeon-led (usual) versus GP-led care, with or without access to an eHealth application (Oncokompas).
Outcome measures
Baseline characteristics of (non-)participants, reasons for non-participation and strategies to improve recruitment were reviewed.
Results
Out of 1238 eligible patients, 353 patients were included. Of these, 50 patients dropped out shortly after randomisation and before start of the intervention, resulting in a participation rate of 25%. Participants were on average slightly younger (68.1 years vs 69.3 years) and more often male (67% vs 50%) in comparison to non-participants. A total of 806 patients declined participation for reasons most often relating to research (57%), including the wish to remain in specialist care (31%) and too much effort to participate (12%). Some patients mentioned health (9%) and confrontation with the disease (5%) as a reason. In 43 cases, GPs declined participation, often related to the study objective, need for financial compensation and time restraints. The generally low participation rate led to concerns about reaching the target sample size. Methods to overcome recruitment challenges included changes to the original recruitment procedure and the addition of new study centres.
Conclusions
Challenges were faced in the recruitment to a randomised trial on GP-led colon cancer survivorship care. Research on the transition of care requires sufficient time, funding and support base among patients and healthcare professionals. These findings will help inform researchers and policy-makers on the development of future practices.
Trial registration number
NTR4860.
Keywords: primary care, qualitative research, gastrointestinal tumours
Strengths and limitations of this study.
This is one of the first and largest randomised trials on general practitioner (GP) led colon cancer survivorship care.
Recruitment to the trial is critically reviewed by comparing participants to non-participants, exploring patients’ and GPs’ reasons for non-participation and describing methods employed to overcome recruitment challenges.
Insights are provided into the support base of this type of primary-care-based intervention for colon cancer patients and the generalisability of its results.
Additional information on non-participants would have been preferable for the further assessment of selection bias, but data were limited to legal and ethical constrictions.
Background
Worldwide, colon cancer incidence and prevalence are rising.1 2 Growing numbers have led to concerns regarding the long-term sustainability of colon cancer survivorship care in a hospital-based setting. Patient advocates ask for a more tailored approach to survivorship care, including increased attention to psychosocial needs, multimorbidity and rehabilitation aspects of care.3 In most countries, general practitioners (GPs) are involved in the management of needs and symptoms of cancer survivors,4–8 without playing a formal role during survivorship care. Interview studies among patients and GPs showed ambiguous opinions about a greater involvement of the GP.9 10 However, possible benefits of GP-led care were also identified, including a better accessibility of care, improved comprehensiveness (related to the high number of patients with multimorbidity) and continuity of care.9 10 GP-led cancer survivorship care has showed similar results with respect to clinical and patient-reported outcomes in comparison to specialist-led care, though the level of evidence is generally low.11 12 Altogether, these considerations formed the basis for the I CARE study (Improving Care After colon canceR treatment in the Netherlands) in which patients with colon cancer were randomised to survivorship care by a surgeon versus care by a GP, with or without access to an eHealth application Oncokompas.13 Oncokompas is aimed at improving knowledge and self-efficacy of patients.14 At baseline, patients in the GP-led trial arm had better quality of life (QoL) scores compared with the surgeon-led trial arm, suggesting some form of indication or sampling bias.15
Recruiting participants to trials on transition of care can be challenging.16 17 Approximately 60% of trials are not able to recruit the original target sample and the target often has to be revised.18–20 Willingness to participate and treatment preferences can play a substantial role in the recruitment and outcome of randomised trials.21 22 Low inclusion creates a problem when recruiting a sample of the patient population that should be representative of the target population. This in turn can lead to difficulties in the extrapolation of results to the general patient population (generalisability or external validity), which is often the case in medical trials.23 24
Despite considerable effort and resources, the recruitment of patients and GP’s in the I CARE study took longer than expected and needed additional interventions. In this descriptive study, we critically review the recruitment to this GP-led colon cancer survivorship care intervention and try to understand how this may contribute to the support base and generalisability of the trial.
Materials and methods
Study design
The I CARE study is a multicentre randomised controlled trial comparing surgeon-led (usual care) to GP-led survivorship care for colon cancer patients in the Netherlands.13 The primary outcome quality of life (QoL) is measured by the European Organisation for Research and Treatment of Cancer (EORTC) Questionnaires; EORTC QLQ-C30 and CR29 at baseline, 3 months, 6 months, 12 months, 24 months, 36 months, 48 months and 60 months after surgery.25 26 The calculated sample size was set at 300 to detect a clinically meaningful difference of 10 units of change in QoL (superiority design with α 0.05, power 80% and anticipating drop-out of 15%).27 At any point in time, patients were allowed to transfer from the GP back to the surgeon, or able to withdraw from study participation completely.
Participants and recruitment procedure
Prior to the start of recruitment, an opt-out procedure was introduced for GPs in the participating regions. Information about the study and opt-out procedure was sent to the participating hospitals, which was then distributed among the affiliated primary care practices. Patient selection was performed in eight Dutch centres (one academic medical hospital and seven community-based hospitals). Patients who were treated for colon cancer stages I–III with curative intent (including adjuvant chemotherapy) were eligible. Exclusion criteria included hereditary colorectal cancer (eg, Lynch syndrome and familial adenomatous polyposis), rectal cancer, inflammatory bowel disease related cancer and a history of a second primary cancer (within 15 years prior to colon cancer diagnosis). Patients who already participated in other research with conflicting endpoints, who were not able to speak Dutch or English, or who were in need of specialised care after surgical treatment, were also excluded.13 Eligible patients were recruited by treating physicians, or in some cases specialised oncology nurses, either shortly after surgery or after completion of chemotherapy treatment. The treating physician or nurse informed the patient and written informed consent was then obtained by the research team. Subsequently, the GP was contacted and asked whether he or she was willing to participate. If both the patient and GP agreed to participate, the patient was included. Patients who declined were asked to participate in a patients’ preference group in which they would receive the usual care by a surgeon but were asked to fill in the baseline questionnaire. The goal of the preference group was to address possible selection bias during recruitment. The Consolidated Standards of Reporting Trials 2010 guidelines were used for the reporting of the trial flow diagram.28
Randomisation
Using computer-generated variable block randomisation stratified for age (cut-off value: 65 years) and tumour stage (I–III), patients were randomly assigned in a factorial design to surgeon-led or GP-led survivorship care (randomisation step 1), with or without additional access to an eHealth application Oncokompas (randomisation step 2), creating four trial arms in total (ratio: 1:1:1:1). In case a second patient of a participating GP was included, this patient (and all subsequent patients) was automatically randomised to the same survivorship care arm to avoid having patients from the same GP receiving different care. If a patient gave consent for participation, randomisation was done centrally at the Academic Medical Centre in Amsterdam by a research assistant to preclude any conflict of interest.
Data collection and processing
Data were recorded using Castor EDC.29 During the recruitment phase, baseline characteristics (including age, gender, tumour stage and treatment with adjuvant chemotherapy) were collected from hospital electronic medical records for all eligible patients. For patients who agreed to participate (participants) and the preference group, additional information on educational level, employment status, marital stage, comorbidities, cancer diagnosis and QoL were extracted from their records and baseline questionnaires. For patients and GPs who refused to participate (non-participants), no additional patient information was gathered, but attempts were made by the treating physician and research team to determine their reason(s) for refusal. Multiple reasons could be given by one individual. Reasons for refusal were also gathered for the preference group. Reasons were documented electronically in Castor using free text. When possible, reasons for refusal were summarised into categories to enable a narrative synthesis of the results. Categories were identified by two independent researchers using an iterative approach (LAMD and JAMV). Disagreement between the two researchers was resolved by discussion, or by consulting a third party if deemed necessary (HCPMvW and KMvA) until consensus was reached.
Statistics
Descriptive statistics were used for baseline comparisons between (non-)participants; t-tests for comparing means and χ2 test for binary and categorical data. Reasons to refuse participation were analysed separately for patients and GPs. Descriptive statistics were performed post-hoc to assess whether patients who dropped out shortly after randomisation differed from the participants who remained in the study population. As part of an exploratory analysis, QoL scores of the I CARE participants were compared with those of the preference group.
Statistical analyses were conducted using SPSS (V.26). A two-sided p value of less than 0.05 was considered statistically significant.
Results
Between 26 March 2015 and 21 November 2018, a total of 1238 eligible patients were identified and approached for participation (figure 1 shows the trial flow diagram). Since the initial screening and selection was done by the treating healthcare professionals, the number of screened patients could not be determined. Eight hundred and six patients (65%) and 43 GPs (4%) declined participation. Two hundred and two patients participated in the preference group. In 36 cases (3%), there was a failure to reach the patient. A total of 353 patients consented and were randomised for the study. Shortly after randomisation and before the start of the intervention, an additional number of 50 patients dropped out due to the patients’ (n=27) or GPs’ withdrawal of consent (n=23). These patients were not considered as part of the study population nor target sample size, since no additional data or questionnaire was available. Most patients who dropped out early were randomised to care by a GP (38 out of 50, or 76%), resulting in a small difference between the trial arm sizes. As a result, the study population consisted of 303 patients, of which 141 patients received GP-led survivorship care (68 with access to Oncokompas) and 162 surgeon-led care (83 with Oncokompas). The overall participation rate in the trial was 25%.
Figure 1.
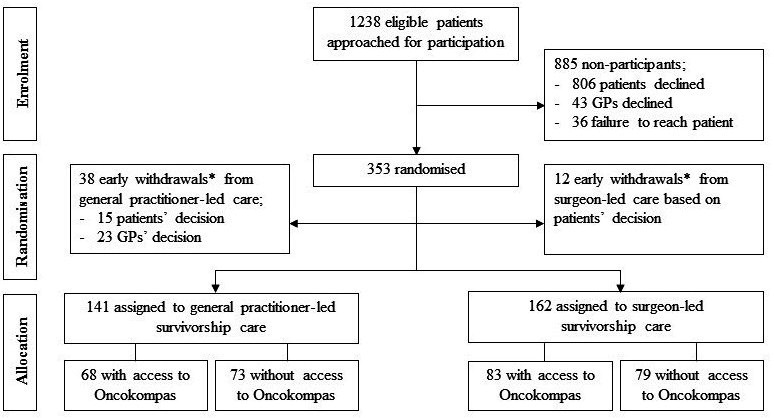
Trial flow diagram. *Participants who withdrew study consent shortly after randomisation. GPs, general practitioners.
Table 1 shows the baseline characteristics of (non-)participants. Participants were on average younger compared with all non-participants (mean: 68.1 years vs 69.3 years, p=0.03) and more often male (67% vs 50%, p<0.001). Participants had slightly more early stage (I–II) colon cancers, but this was not significantly different from non-participants (p=0.07). There were no differences relating to the treatment with adjuvant chemotherapy. Participants most often lived together with their partner or children (75%) and were retired or not actively employed (71%). Colon cancer was diagnosed through population screening in half of the cases. Also half of the cases had limited to no comorbidities. Comorbid conditions most often related to the cardiovascular (60%) and endocrine system (24%). Patients in the preference group showed similar baseline characteristics and comorbid conditions (figure 2). However, preference patients often reported lower QoL scores compared with participants (online supplemental appendix S1). Participants did not differ from patients who dropped out early from the study in age, gender, tumour stage or adjuvant chemotherapy treatment (data not shown).
Table 1.
Characteristics of participants and non-participants
| Participants (N=303) | Non-participants (N=885) | P value* | ||
| Non-participants (683) | Preference (202) | |||
| Age (years, mean, SD) | 68.1 (8.4) | 70.0 (9.7) | 67.2 (8.7) | 0.03 |
| Gender (male, %) | 203 (67.0) | 332 (48.6) | 114 (56.4) | <0.001 |
| Tumour stage† (%) | ||||
| I | 113 (37.3) | 202 (29.6) | 64 (31.7) | 0.07 |
| II | 104 (34.3) | 270 (39.5) | 81 (40.1) | |
| III | 86 (28.4) | 200 (29.3) | 57 (28.2) | |
| Unknown | NA | 11 (1.6) | NA | |
| Adjuvant chemotherapy treatment‡, (%) | 68 (22.4) | 168 (24.6) | 48 (23.8) | 0.42 |
| Unknown | NA | 13 (1.9) | NA | |
| Living situation, together (%) | 227 (74.9) | NA | 150 (74.3) | 0.42 |
| Employment status, active (%) | 89 (29.4) | NA | 45 (22.3) | 0.09 |
| Educational attainment (%) | 0.07 | |||
| Primary or none | 27 (8.9) | NA | 8 (4.0) | |
| Secondary | 68 (22.4) | 60 (29.7) | ||
| Vocational education | 146 (48.2) | 102 (50.5) | ||
| University | 36 (11.9) | 20 (9.9) | ||
| Cancer diagnosis (%) | 0.39 | |||
| Population screening | 152 (50.2) | NA | 98 (48.5) | |
| Clinical course | 151 (49.8) | 104 (51.5) | ||
| Chronic comorbid condition (%) | 0.53 | |||
| 0–1 | 147 (48.5) | NA | 98 (48.5) | |
| >2 | 156 (51.5) | 104 (51.5) | ||
*P values are shown for the comparison between participants (N=303) and all non-participants (N=885).
†Tumour stage was defined using the tumour, node, metastases (TNM) 5 criteria.33
‡Adjuvant chemotherapy treatment.
NA, not applicable.
Figure 2.
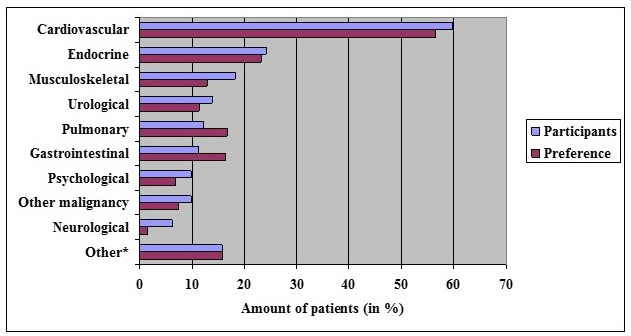
Chronic comorbid conditions. *Other chronic comorbid conditions were reported by less than 5% of the participants and included ear, nose, throat diseases, skin disorders, eye disorders, infectious disorders and blood disorders.
bmjopen-2021-048985supp001.pdf (802.3KB, pdf)
Six hundred and seventy-nine out of 806 patients (84%) provided 745 reasons to decline participation. For 127 patients (16%), the reason for declining participation was unknown. Eighty-nine patients provided more than one reason (table 2).
Table 2.
Reasons for patients to decline participation (N=806 patients)
| Category | n (%) | Subcategory | n (%) |
| Research related | 461 (57) | ||
| Wish to remain in specialist care | 249 (31) | ||
| Too much effort | 95 (12) | ||
| No interest in any research participation | 51 (6) | ||
| Participates in another study | 31 (4) | ||
| Other research related reason* | 35 (4) | ||
| Patient related | 166 (21) | ||
| Health-related reason | 70 (9) | ||
| Confrontation with the disease | 38 (5) | ||
| Age related | 23 (3) | ||
| Other patient-related reason† | 35 (4) | ||
| GP related | 54 (7) | ||
| Bad experience with the GP | 29 (4) | ||
| No relationship with the GP | 25 (3) | ||
| Hospital related | 40 (5) | ||
| Positive previous experience with hospital | 32 (4) | ||
| Other reason to stay in hospital‡ | 8 (1) | ||
| Other reason§ | 24 (3) | ||
| Unknown | 127 (16) |
*Other research related reasons (<5% of the participants) were ‘does not understand the content of the study’, ‘the study is too complicated’, ‘study information is confusing’, ‘privacy related reason’, ‘does not agree with study objective’ and ‘does not agree with recruitment procedure’.
†Other patient related reasons were ‘uncertainty about situation’, ‘illness or recent death of partner’, ‘patient is too busy to participate’, ‘dyslexia’ and ‘staying abroad’.
‡Other hospital related reasons included ‘quick insight in results’, ‘hospital is closer to home’, ‘proximity to surgeon’, ‘too soon after surgery’ and ‘wish of partner’.
§Other reasons were ‘in consultation with specialist or/and general practitioner’, ‘follow-up by general practitioner’ and ‘no follow-up’.
GP, general practitioner.
In most cases, patients declined participation due to research related reasons (461 out of 806 patients, or 57%). Patients often wished to remain in specialist care and did not want to receive survivorship care by a GP (31%). Other patients felt it would be too much effort to participate in the study (12%), especially when it meant filling out repeating questionnaires as part of the study. Some patients had no interest to participate in any type of research (6%) or mentioned that they already participated in another type of research (4%). Few patients thought that the study procedure was too complicated. Two patients disagreed with the recruitment procedure in which the GP was asked at a later point in time. In 21% of cases, reasons related to the patients’ situation were reported. Patients mentioned that their current health status did not allow them to participate (9%). Others did not want to be confronted with the disease (5%) or felt that they were too old to participate (3%). A limited amount of reasons related to the patients’ GP were brought forth (7%). Some patients had a previous bad experience with their GP (4%), while others had no prior relationship with the GP (3%). Some patients had previous positive experiences with hospital-based care (4%) or other reasons to wish to remain in the hospital (1%).
Prior to the start of recruitment, 24 primary care practices in the participating regions decided to opt out through email. Since the information about the study and opt-out procedure was largely distributed through participating hospitals, it was not possible to determine the reach of the information. GPs declined participation in 43 cases (table 3). In 18 cases (42%), the reason to decline was unknown. Eight GPs provided more than one reason. Reasons often related to research, including a disagreement with the study objective (transition of colon cancer survivorship care to the GP), a need for financial compensation and the opinion that too many substitutions were already coming to the general practice. Some GPs mentioned that they were too busy to provide survivorship care and one GP did not feel competent to do so.
Table 3.
Reasons for GPs to decline participation (N=43 general practitioners)
| Category | n (%) | Subcategory | n (%) |
| Research related | 24 (56) | ||
| Disagrees with the study objective | 12 (28) | ||
| Wants financial compensation | 11 (26) | ||
| Too many substitutions coming to the GP | 1 (2) | ||
| GP related | 12 (28) | ||
| Too busy | 11 (26) | ||
| Does not feel competent | 1 (2) | ||
| Unknown | 18 (42) |
GPs, general practitioners.
It was previously outlined to include 12 patients each month, resulting in a planned recruitment period of 25 months. Recruitment, however, lasted up to almost 44 months, requiring a 19-month no-cost extension from the funder. Due to the number of eligible patients and GPs declining participation and concerns about reaching the target sample size, different methods had to be employed to overcome the recruitment challenges:
Recruitment was initially solely executed by the treating healthcare professionals at the outpatient clinic. Due to time constraints during follow-up consultations and some initial reservations among treating physicians and nurses towards transferring care to the GP, study participation was sometimes not discussed in further detail. As it is important that patients are well informed about the study procedure and have been given enough time to consider their decision, it was decided shortly after the start of recruitment that members of the research team would screen the outpatient clinic schedules and call all eligible patients after their follow-up visits to enquire about any questions relating to the study and potential participation. This extra recruitment step was implemented in all participating centres from December 2015 onwards.
Two additional hospitals were approached, of which one approved participation and recruitment started on 8 June 2016. Due to the merging of some participating hospitals, this resulted in the participation of 8 different centres (consisting of 10 hospitals) throughout the remainder of the study period.
Some GPs declined participation out of a principle reason. They argued that financial compensation should be provided when their tasks were expanded (table 3). Therefore, from September 2016 onwards, a small reimbursement was provided from the research budget for survivorship care by the GP.
Since early drop-out of patients primarily took place in the GP-led trial arm (38 out of 50 drop-outs, or 76%), the ratio for surgeon-led versus GP-led survivorship care was changed from 1:1 to 1:2 on 23 February 2017. Stratification based on age and tumour stage was not changed.
Finally, because many patients agreed to take part in the preference group, while saturation of the group was already considered reached, it was decided on 6 March 2018 that patients would no longer be offered to participate in the preference group, and time and resources would be focused on the recruitment of new study participants.
Discussion
Challenges were faced in the recruitment to the I CARE study, a randomised trial on GP-led colon cancer survivorship care, resulting in an extended recruitment period. Recruitment to the study was critically reviewed by comparing participants to non-participants, exploring reasons for non-participation and describing changes made to the original recruitment plan to overcome these recruitment challenges. Participants were often of younger age and male in comparison to non-participants. Patients and GPs declined participation due to their preferences for care, personal situation and time restraints. These results provide us with insights regarding the support base and generalisability of this alternative to hospital-based survivorship care.
Support base
In order for any healthcare intervention to be successful, there needs to be sufficient support among those affected by it. Previous research has shown that eligible individuals are less likely to participate in a trial if they have a strong treatment preference.22 Recruitment to the I CARE study faced a similar problem. The overall participation rate of 25% was generally low, especially in comparison to other Dutch primary care research, in which an overall participation rate of 70% has been reported, though the range in these studies was maximal (0%–100%).18 Two previous trials have been published on GP-led colon cancer survivorship in which the participation rate ranged from 18% to 60%.30 31 These results illustrate that the support base differs depending on the context and setting of the trial. However, these two previous trials provided little to no information on non-participation. This study provides additional evidence by describing baseline characteristics of non-participants and exploring reasons for non-participation. Patients often mentioned a preference for surgeon-led or hospital-based care. Similarly, GPs often declined participation due to a disagreement with the study objective and the amount of extra work. The support base for GP-led colon cancer survivorship care may, therefore, be limited. When considering a structural change from surgeon-led to GP-led care, these challenges and concerns have yet to overcome.
Generalisability
Prior to the start of the study, it was hypothesised that patients might benefit from a more generalist approach to survivorship care with increasing age and comorbidities,13 yet participants in the I CARE study were on average younger than non-participants, and often had limited to no comorbidities. The difficulties experienced in the recruitment of the study may have created an unintended selection of the target population. Participants in the I CARE study seem to be healthier than the average colon cancer patients. Participants often reported better QoL scores and lower symptom burden compared with the preference group, indicating a form of sampling or indication bias, as previously suggested.15 Also stage I tumours were seen relatively often among study participants (37% vs 30%). Since the follow-up programme for stage I tumours is less comprehensive than for stage II and III tumours, the impact, possible benefits and also workload of GP-led survivorship care may differ. The unintended selection of the target population can lead to difficulties in the generalisability of the trial results.
Strengths and limitations
This is one of the first and largest randomised trials on GP-led survivorship care for colon cancer patients. Data on eligible patients and reasons for declining participation have been collected within the grasps of the I CARE study. Additional information on non-participants, including comorbidities, would have been preferable for the further assessment of selection bias, but the data were limited to legal and ethical constrictions. Reasons to decline participation were generally widespread and diverse; therefore, a narrative synthesis was used to allow for the identification of categories. As patients and GPs could decline participation without any further specification, this resulted in a small amount of missing data, especially among GPs. Changes to the original recruitment plan were made on the basis of available evidence, including the introduction of an additional screening of eligible patients and telephone reminder.32 Due to these changes, the recruitment challenges were met and the target sample size was reached.
Recommendations
Based on the findings of this study, some recommendations can be formulated for future trials on cancer survivorship care. In these trials, efforts should be made to collect information on eligible patients, if at all possible, to evaluate the risk of selection bias. This will allow for the better assessment of recruitment and treatment outcomes. The recruitment of new participants by treating physicians and nurses took longer than expected, so a more active role for the research team should be intended from the start of recruitment. Two patients disagreed with the recruitment procedure, informing us that it might be better to contact the GP prior to the patient in future trials. Many patients mentioned the amount of effort as a reason to decline participation. The length and amount of questionnaires should, therefore, be reconsidered when measuring patient-reported outcomes. As some patients thought that the study was too complicated, sufficiently detailed and personalised information should be provided at a timely manner in order to make an informed decision. Other patients declined participation due to their health or other personal reasons, which could be related to the timing of the study. And finally, GPs often mentioned the need for financial compensation, so a reimbursement should be considered for this type of research.
Conclusion
Studies on transition of care to complex settings, such as primary care, are often difficult and require sufficient time, funding and support base. This study has illustrated the recruitment challenges to a GP-led colon cancer survivorship care intervention and how these were addressed. This study provides insights into the support base of this type of intervention and the generalisability of its results. These findings will help inform researchers and policy-makers on the development and implementation of future cancer survivorship care practices. In-depth evaluation of experiences, limitations and recommendations among participants by means of a process evaluation will add to the growing evidence.
Supplementary Material
Acknowledgments
The authors would like to acknowledge and thank all participants, contributing hospitals and their principle investigators.
Footnotes
LAMD and JAMV contributed equally.
Collaborators: M J P M Govaert; F H Beverdam; A A W van Geloven; A B Smits; W A Bemelman; A W H van de Ven; Q A J Eijsbouts.
Contributors: All authors made a substantial contribution to the design and coordination of the I CARE study. LAMD, JAMV, TW, JW, HCPMvW and KMvA are the steering investigators of the study. SCD, MJPMG, FHB, AAWvG, ABS, WAB, AWHvdV and QAJE are the principal investigators at the inclusion sites, and helped and advised the steering investigators during the recruitment. Recruitment was done by LAMD and TW. LAMD, TW and JAMV performed the data extraction and analyses. JW, HCPMvW and KMvA supervised the study. LAMD and JAMV drafted the first manuscript. The manuscript was critically revised and approved by all authors.
Funding: This work was supported by KWF Kankerbestrijding/Stichting Alpe d’HuZes grant number BMA 5954.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Contributor Information
the I CARE study group:
MJPM Govaert, FH Beverdam, AAW van Geloven, AB Smits, WA Bemelman, AWH van de Ven, and QAJ Eijsbouts
Data availability statement
Data are available upon reasonable request. All data relevant to the study are included in the article or uploaded as supplementary information. Data Availability Statement. At the end of study, data can be made available, after anonymization, on request to the corresponding author, taking into account possible national and international legal restrictions.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
The study protocol was approved by the medical ethics committee of the Academic Medical Centre (Amsterdam, the Netherlands) (MEC 2014_332). Since baseline data on non-participants were fully anonymised, no informed consent of non-participants was needed.
References
- 1. Bray F, Ferlay J, Soerjomataram I, et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 2018;68:394–424. 10.3322/caac.21492 [DOI] [PubMed] [Google Scholar]
- 2. Arnold M, Sierra MS, Laversanne M, et al. Global patterns and trends in colorectal cancer incidence and mortality. Gut 2017;66:683–91. 10.1136/gutjnl-2015-310912 [DOI] [PubMed] [Google Scholar]
- 3. Hewitt M, Greenfield S, Stovall E. From cancer patient to cancer survivor: lost in transition. Washington, DC: National Academies Press, 2006. [Google Scholar]
- 4. Khan NF, Watson E, Rose PW. Primary care consultation behaviours of long-term, adult survivors of cancer in the UK. Br J Gen Pract 2011;61:197–9. 10.3399/bjgp11X561195 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fidjeland HL, Vistad I, Gjelstad S, et al. Exploring why patients with cancer consult GPs: a 1-year data extraction. BJGP Open 2019. 10.3399/bjgpopen19X101663. [Epub ahead of print: 01 Oct 2019]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Duineveld LAM, Molthof H, Wieldraaijer T, et al. General practitioners' involvement during survivorship care of colon cancer in the Netherlands: primary health care utilization during survivorship care of colon cancer, a prospective multicentre cohort study. Fam Pract 2019;36:765–70. 10.1093/fampra/cmz028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brandenbarg D, Roorda C, Groenhof F, et al. Primary healthcare use during follow-up after curative treatment for colorectal cancer. Eur J Cancer Care 2017;26:ecc.12581. 10.1111/ecc.12581 [DOI] [PubMed] [Google Scholar]
- 8. Kenzik KM. Health care use during cancer survivorship: review of 5 years of evidence. Cancer 2019;125:673–80. 10.1002/cncr.31852 [DOI] [PubMed] [Google Scholar]
- 9. Duineveld LAM, Wieldraaijer T, Wind J, et al. Primary care-led survivorship care for patients with colon cancer and the use of eHealth: a qualitative study on perspectives of general practitioners. BMJ Open 2016;6:e010777. 10.1136/bmjopen-2015-010777 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Nugteren IC, Duineveld LAM, Wieldraaijer T, et al. Need for general practitioner involvement and eHealth in colon cancer survivorship care: patients' perspectives. Fam Pract 2017;34:473–8. 10.1093/fampra/cmw139 [DOI] [PubMed] [Google Scholar]
- 11. Høeg BL, Bidstrup PE, Karlsen RV, et al. Follow-Up strategies following completion of primary cancer treatment in adult cancer survivors. Cochrane Database Syst Rev 2019;2019:CD012425. 10.1002/14651858.CD012425.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Vos JAM, Wieldraaijer T, van Weert HCPM, et al. Survivorship care for cancer patients in primary versus secondary care: a systematic review. J Cancer Surviv 2021;15:66–76. 10.1007/s11764-020-00911-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Duineveld LAM, Wieldraaijer T, van Asselt KM, et al. Improving care after colon cancer treatment in the Netherlands, personalised care to enhance quality of life (I care study): study protocol for a randomised controlled trial. Trials 2015;16:284. 10.1186/s13063-015-0798-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Matthijs de Wit L, van Uden-Kraan CF, Lissenberg-Witte BI, et al. Adoption and implementation of a web-based self-management application "Oncokompas" in routine cancer care: a national pilot study. Support Care Cancer 2019;27:2911–20. 10.1007/s00520-018-4591-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Vos JAM, Duineveld LAM, Wieldraaijer T, et al. Effect of general practitioner-led versus surgeon-led colon cancer survivorship care, with or without eHealth support, on quality of life (I care): an interim analysis of 1-year results of a randomised, controlled trial. Lancet Oncol 2021;22:1175–87. 10.1016/S1470-2045(21)00273-4 [DOI] [PubMed] [Google Scholar]
- 16. Gilbert F, Denis J-L, Lamothe L, et al. Reforming primary healthcare: from public policy to organizational change. J Health Organ Manag 2015;29:92–110. 10.1108/JHOM-12-2012-0237 [DOI] [PubMed] [Google Scholar]
- 17. Javanparast S, Maddern J, Baum F, et al. Change management in an environment of ongoing primary health care system reform: a case study of Australian primary health care services. Int J Health Plann Manage 2018;33:e76–88. 10.1002/hpm.2413 [DOI] [PubMed] [Google Scholar]
- 18. Walters SJ, Bonacho Dos Anjos Henriques-Cadby I, Bortolami O, et al. Recruitment and retention of participants in randomised controlled trials: a review of trials funded and published by the United Kingdom health technology assessment programme. BMJ Open 2017;7:e015276. 10.1136/bmjopen-2016-015276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sully BGO, Julious SA, Nicholl J. A reinvestigation of recruitment to randomised, controlled, multicenter trials: a review of trials funded by two UK funding agencies. Trials 2013;14:166. 10.1186/1745-6215-14-166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. van der Wouden JC, Blankenstein AH, Huibers MJH, et al. Survey among 78 studies showed that Lasagna's law holds in Dutch primary care research. J Clin Epidemiol 2007;60:819–24. 10.1016/j.jclinepi.2006.11.010 [DOI] [PubMed] [Google Scholar]
- 21. Preference Collaborative Review Group . Patients' preferences within randomised trials: systematic review and patient level meta-analysis. BMJ 2008;337:a1864. 10.1136/bmj.a1864 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. King M, Nazareth I, Lampe F, et al. Impact of participant and physician intervention preferences on randomized trials: a systematic review. JAMA 2005;293:1089–99. 10.1001/jama.293.9.1089 [DOI] [PubMed] [Google Scholar]
- 23. Kennedy-Martin T, Curtis S, Faries D, et al. A literature review on the representativeness of randomized controlled trial samples and implications for the external validity of trial results. Trials 2015;16:495. 10.1186/s13063-015-1023-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Brænd AM, Straand J, Klovning A. Clinical drug trials in general practice: how well are external validity issues reported? BMC Fam Pract 2017;18:113. 10.1186/s12875-017-0680-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Stiggelbout AM, Kunneman M, Baas-Thijssen MCM, et al. The EORTC QLQ-CR29 quality of life questionnaire for colorectal cancer: validation of the Dutch version. Qual Life Res 2016;25:1853–8. 10.1007/s11136-015-1210-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Aaronson NK, Ahmedzai S, Bergman B, et al. The European organization for research and treatment of cancer QLQ-C30: a quality-of-life instrument for use in international clinical trials in oncology. J Natl Cancer Inst 1993;85:365–76. 10.1093/jnci/85.5.365 [DOI] [PubMed] [Google Scholar]
- 27. Osoba D, Rodrigues G, Myles J, et al. Interpreting the significance of changes in health-related quality-of-life scores. J Clin Oncol 1998;16:139–44. 10.1200/JCO.1998.16.1.139 [DOI] [PubMed] [Google Scholar]
- 28. Schulz KF, Altman DG, Moher D, et al. Consort 2010 statement: updated guidelines for reporting parallel group randomised trials. BMJ 2010;340:c332. 10.1136/bmj.c332 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Castor EDC. Castor electronic data capture, 2019. Available: https://castoredc.com [Accessed 27 Aug. 2019].
- 30. Augestad KM, Norum J, Dehof S, et al. Cost-Effectiveness and quality of life in surgeon versus general practitioner-organised colon cancer surveillance: a randomised controlled trial. BMJ Open 2013;3:e002391. 10.1136/bmjopen-2012-002391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wattchow DA, Weller DP, Esterman A, et al. General practice vs surgical-based follow-up for patients with colon cancer: randomised controlled trial. Br J Cancer 2006;94:1116–21. 10.1038/sj.bjc.6603052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Treweek S, Pitkethly M, Cook J, et al. Strategies to improve recruitment to randomised trials. Cochrane Database Syst Rev 2018;2:MR000013. 10.1002/14651858.MR000013.pub6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Sobin LH, Fleming ID. Tnm classification of malignant tumors, fifth edition (1997). Union Internationale Contre Le cancer and the American joint Committee on cancer. Cancer 1997;80:1803–4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-048985supp001.pdf (802.3KB, pdf)
Data Availability Statement
Data are available upon reasonable request. All data relevant to the study are included in the article or uploaded as supplementary information. Data Availability Statement. At the end of study, data can be made available, after anonymization, on request to the corresponding author, taking into account possible national and international legal restrictions.


