Abstract
The ability of SARS-CoV-2 to infect the gastrointestinal tract is well described. Inflammatory bowel diseases (IBD) are believed to represent a disorganised immune response in genetically predisposed individuals, which are triggered by various environmental factors, notably infections. Here we report a case of chronic watery diarrhoea that was triggered by a SARS-CoV-2 infection. The work-up confirmed a new diagnosis of lymphocytic colitis, and the patient responded favourably to a course of oral budesonide. Clinicians should become vigilant to the possibility of triggered IBD in patients with persistent diarrhoea following a SARS-CoV-2 infection.
Keywords: COVID-19, inflammatory bowel disease, gastrointestinal system, infection (gastroenterology)
Background
Lymphocytic colitis, one of the two phenotypes of microscopic colitis, is an inflammatory bowel disease (IBD) characterised by chronic watery diarrhoea. It is usually diagnosed with the histological hallmarks of disease despite a macroscopically normal large bowel.1 The direct involvement of the gastrointestinal (GI) system in SARS-CoV-2 infections is well established, with main symptoms of diarrhoea, loss of taste, nausea, vomiting and abdominal pain.2
The increased risk of IBD following infectious gastroenteritis is well described in literature. Moreover, the observation that the incidence rate of IBD after a documented bacterial gastroenteritis was similar to the incidence rate after episodes of gastroenteritis with negative stool cultures, in which a significant proportion of cases are probably of viral origin, suggests the possibility that both bacterial and viral infections can trigger IBD.3 Only a handful of SARS-CoV-2-triggered IBD cases have been reported. To the best of our knowledge, this is the first case report of a SARS-CoV-2-triggered lymphocytic colitis. This case report aimed to alert healthcare professionals to consider the spectrum of IBD in patients with persistent GI symptoms, notably diarrhoea, after a SARS-CoV-2 infection.
Case presentation
A 62-year-old female patient suffered from COVID-19 in March 2020, which presented with acute onset of cough, severe headache and low-grade fever. Gradual improvement started after 5 days with symptomatic treatment. Watery diarrhoea, up to six bowel movements daily, commenced on the 10th day of the illness and persisted for the following 3 months. This was associated with bloating, urgency and nocturnal motions. She sought medical advice from her primary care physician in a telephone consultation and symptomatic treatment with paracetamol and loperamide was recommended. The symptoms were not severe enough to warrant hospitalisation, and SARS-CoV-2 testing was available only for hospitalised patients at that time. Her medical history was notable for gastro-oesophageal reflux disease, for which she has been using proton pump inhibitors for the past 9 years. She used to occasionally take naproxen; however, she denied taking any non-steroidal anti-inflammatory drugs (NSAIDs) for the past 3 years. Otherwise, she had no significant medical or surgical history, and she had no family history of IBD or cancer.
Investigations
Stool microscopy and cultures were negative for Giardia, Cryptosporidia, Shigella, Escherichia coli, Salmonella and Campylobacter. Full blood count, liver function tests, kidney function tests and C reactive protein were within their normal ranges. Tissue transglutaminase antibody (tTG-IgA) test returned negative and thyroid function tests were within normal range. Noteworthy, her SARS-CoV-2 antibody test resulted positive in September 2020. Considering the patient’s age and clinical presentation, colonoscopy was required regardless of faecal calprotectin level; in turn, faecal calprotectin test was omitted. Immunodeficiency disorders were unlikely, considering her medical history; therefore, HIV testing was not performed.
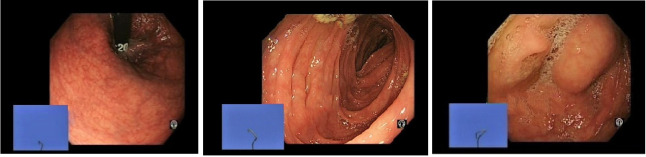
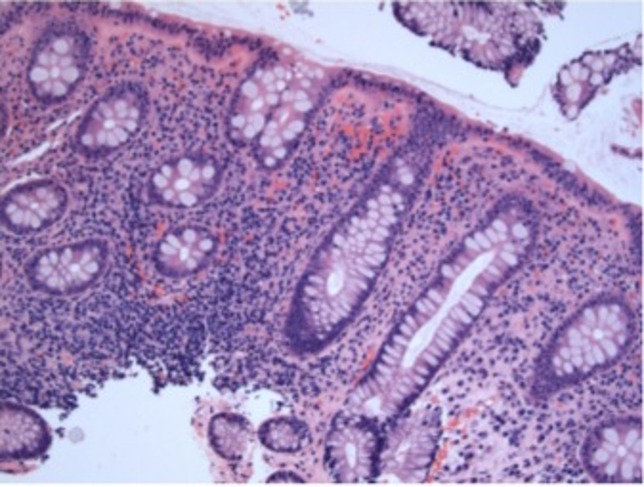
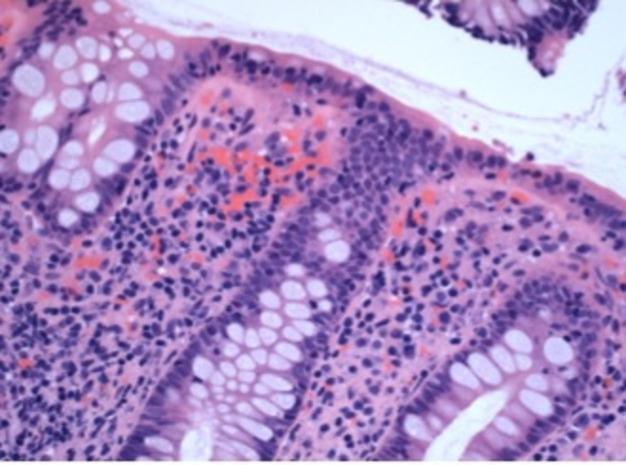
She was referred for colonoscopy in July 2020 with a 3-month history of persistent watery diarrhoea. Colonoscopy was unremarkable apart from few uncomplicated diverticula in the sigmoid colon (figure 1). Biopsies were taken from the ascending and descending colon to rule out microscopic colitis. The histopathological analysis was typical for lymphocytic colitis, showing an increase in chronic inflammatory cell infiltrate in the lamina propria, with lymphocytes extending into the surface epithelium as well as the epithelium lining the crypts. There was no thickening of the subepithelial collagen plate, no granulomas and no significant crypt distortion (figures 2 and 3).
Figure 1.
Unremarkable colonoscopy, apart from a few uncomplicated sigmoid diverticula (from left to right: rectum, sigmoid colon and cecum).
Figure 2.
Histology, increased lamina propria chronic inflammation (H&E, ×200).
Figure 3.
Histology, lymphocytes extending into the epithelium lining the surface and crypts (H&E, ×400).
Differential diagnosis
Based on a combination of the clinical presentation of chronic watery diarrhoea, the normal colonoscopic examination and the typical microscopic findings, she was diagnosed with lymphocytic colitis. Infectious causes of chronic diarrhoea were ruled out by negative stool tests. Coeliac disease was much less likely, considering the negative tTG-IgA test. Hyperthyroidism was excluded by normal thyroid function tests. NSAIDs and other drug-induced diarrhoea were not considered due to lack of compatible history. The histopathological findings argue against a diagnosis of irritable bowel syndrome or collagenous colitis, and the endoscopic findings rule out the diagnosis of ulcerative or Crohn’s colitis.
Treatment
She was prescribed an 8-week course of oral budesonide for induction of remission, in the form of budesonide multimatrix formula (Cortiment) 9 mg/day.
Outcome and follow-up
Symptomatic improvement was noted after 5 days with almost complete resolution of symptoms after 10 days. Clinical remission has been maintained so far. The prompt and sustained clinical response to budesonide provided an additional diagnostic confirmation.
Discussion
We report a case of COVID-19 which presented with the typical clinical features of fever and respiratory symptoms, followed by 3 months of persistent watery diarrhoea. Patients with persistent or recurrent symptoms after a SARS-CoV-2 infection are usually considered for the poorly understood diagnoses of ‘long COVID-19’, ‘chronic COVID-19 syndromes’ or ‘postacute COVID-19 syndrome’.4 In a recently published retrospective study of 117 patients who were admitted with COVID-19, 44% had persistent GI symptoms after discharge. GI sequelae were defined as GI symptoms that presented after discharge but were not present within the month before onset of COVID-19. Seventeen per cent of the study group was suffering from chronic diarrhoea 90 days after discharge. The study suggested the hypoxia-mediated multiorgan damage as a pathogenic mechanism. Furthermore, patients who received nutritional support during hospitalisation were less likely to suffer from long-term GI sequelae.5
Only a few SARS-CoV-2-triggered IBD cases were reported in the literature. Taxonera et al reported a female patient who presented with a SARS-CoV-2 infection in March 2020.6 She presented with a 7-day history of fever, sore throat, myalgia, dyspnoea and watery diarrhoea. Similar to our case, the watery diarrhoea persisted for 3 months after recovery. Stool cultures ruled out common pathogens and colonoscopy showed confluent distal colonic inflammation. The histopathology confirmed a diagnosis of ulcerative colitis, and she achieved a clinical remission with a combination of oral and rectal mesalazine. In another case report,7 a 19-year-old woman was admitted with a history of fever, nausea, vomiting, bloody diarrhoea and loss of taste. A nasopharyngeal swab resulted positive for SARS-CoV-2. A CT scan showed no pneumonia but increased contrast enhancement in the ileum and colon. Ileocolonoscopy showed extensive colitis, and the biopsies showed typical features of ulcerative colitis. Furthermore, SARS-CoV-2 RNA testing in the colonic, ileal and faecal samples was negative. Aydin and Tasdemir reported a 50-year-old male patient who returned 2 weeks after a SARS-CoV-2 infection with bloody diarrhoea. Colonoscopy revealed diffuse ulcerations with granular appearance in the rectum and sigmoid colon. Similarly, pathological examination revealed the typical features of ulcerative colitis, while no specific micro-organism was detected. He responded favourably to mesalazine treatment as well.8
The direct involvement of the GI system in SARS-CoV-2 infections is well studied. In a recent systematic review of 35 studies comprising 6686 patients with COVID-19, the pooled prevalence of all GI symptoms was 15%.9 ACE II receptors and the transmembrane serine protease are found to be highly expressed in GI epithelial cells, from the oesophagus to the rectum, providing a prerequisite for SARS-CoV-2 entrance.10 SARS-CoV-2 viral RNA has been frequently detected in the stool specimens of infected patients,11 and 20% of patients showed prolonged presence of SARS-CoV-2 RNA in faecal samples after the viral testing converted to negative in the respiratory specimens. These findings suggest that SARS-CoV-2 can actively infect and replicate in the GI tract.12 SARS-CoV-2 has also been detected in stool samples from patients without GI symptoms.13 Moreover, GI symptoms could be the first manifestation antedating the respiratory symptoms, and patients suffering from only digestive symptoms without any respiratory symptoms have also been reported.14 Furthermore, SARS-CoV-2 RNA was directly detected in tissue samples from the oesophagus, stomach, duodenum and rectum.15
There are several plausible explanations for the ability of SARS-CoV-2 infection to trigger IBD. The association between infection and autoimmunity, the first leading to the latter by the mechanisms of molecular mimicry, epitope spreading, and bystander or polyclonal activation, is well established.16 In addition to the immunological mechanisms, SARS-CoV-2 has been demonstrated to induce significant changes in the GI microbiome, which persisted even after viral clearance.17
The present case demonstrated a clear temporal relationship between SARS-CoV-2 infection and the onset of lymphocytic colitis. Interestingly, lymphocytic infiltration, the salient feature of lymphocytic colitis, was the predominant feature in biopsies of a patient with COVID-19 who underwent endoscopy because of GI bleeding.18 It is possible to postulate that SARS-CoV-2 infection can initiate an immunological reaction which, in a genetically predisposed individual, can trigger an IBD. Noteworthy, consistently elevated levels of faecal calprotectin have been documented in patients with COVID-19 with persistent diarrhoea even in the absence of faecal SARS-CoV-2 RNA, probably denoting a triggered chronic inflammatory diarrhoea, rather than a persistent viral infection.19 Nevertheless, the lack of SARS-CoV-2 RNA testing of the stool and tissue samples is an important limitation of the present case report.
Learning points.
Lymphocytic colitis could be considered in the differential diagnosis for patients with COVID-19 with persistent diarrhoea.
SARS-CoV-2-triggered lymphocytic colitis could respond favourably to its standard pharmacological therapy (budesonide).
Dysregulated immune response to SARS-CoV-2 infection could be one of the pathogenic mechanisms responsible for the persistent GI symptoms of ‘long COVID-19 syndrome’.
Footnotes
Contributors: Case report conception: MNQ; data acquisition: ION, MNQ and GL; writing the case report: ION; critical review: NS, MNQ and GL.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Obtained.
References
- 1.Boland K, Nguyen GC. Microscopic colitis: a review of collagenous and lymphocytic colitis. Gastroenterol Hepatol 2017;13:671–7. [PMC free article] [PubMed] [Google Scholar]
- 2.Su S, Shen J, Zhu L, et al. Involvement of digestive system in COVID-19: manifestations, pathology, management and challenges. Therap Adv Gastroenterol 2020;13:1756284820934626. 10.1177/1756284820934626 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.García Rodríguez LA, Ruigómez A, Panés J. Acute gastroenteritis is followed by an increased risk of inflammatory bowel disease. Gastroenterology 2006;130:1588–94. 10.1053/j.gastro.2006.02.004 [DOI] [PubMed] [Google Scholar]
- 4.Halpin S, O'Connor R, Sivan M. Long COVID and chronic COVID syndromes. J Med Virol 2021;93:1242–3. 10.1002/jmv.26587 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Weng J, Li Y, Li J, et al. Gastrointestinal sequelae 90 days after discharge for COVID-19. Lancet Gastroenterol Hepatol 2021;6:344–6. 10.1016/S2468-1253(21)00076-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taxonera C, Fisac J, Alba C. Can COVID-19 trigger de novo inflammatory bowel disease? Gastroenterology 2021;160:1029–30. 10.1053/j.gastro.2020.11.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Calabrese E, Zorzi F, Monteleone G, et al. Onset of ulcerative colitis during SARS-CoV-2 infection. Dig Liver Dis 2020;52:1228–9. 10.1016/j.dld.2020.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Aydin M, Tasdemir H. Ulcerative colitis developed in a COVID-19 patient: a case report. Research Square. [Preprint]2020. [Google Scholar]
- 9.Mao R, Qiu Y, He J-S, et al. Manifestations and prognosis of gastrointestinal and liver involvement in patients with COVID-19: a systematic review and meta-analysis. Lancet Gastroenterol Hepatol 2020;5:667–78. 10.1016/S2468-1253(20)30126-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zou X, Chen K, Zou J, et al. Single-Cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection. Front Med 2020;14:185–92. 10.1007/s11684-020-0754-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cheung KS, Hung IFN, Chan PPY, et al. Gastrointestinal manifestations of SARS-CoV-2 infection and virus load in fecal samples from a Hong Kong cohort: systematic review and meta-analysis. Gastroenterology 2020;159:81–95. 10.1053/j.gastro.2020.03.065 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Parasa S, Desai M, Thoguluva Chandrasekar V, et al. Prevalence of gastrointestinal symptoms and fecal viral shedding in patients with coronavirus disease 2019: a systematic review and meta-analysis. JAMA Netw Open 2020;3:e2011335. 10.1001/jamanetworkopen.2020.11335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang W, Xu Y, Gao R, et al. Detection of SARS-CoV-2 in different types of clinical specimens. JAMA 2020;323:1843–4. 10.1001/jama.2020.3786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Luo S, Zhang X, Xu H. Don't Overlook Digestive Symptoms in Patients With 2019 Novel Coronavirus Disease (COVID-19). Clin Gastroenterol Hepatol 2020;18:1636–7. 10.1016/j.cgh.2020.03.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lin L, Jiang X, Zhang Z, et al. Gastrointestinal symptoms of 95 cases with SARS-CoV-2 infection. Gut 2020;69:997–1001. 10.1136/gutjnl-2020-321013 [DOI] [PubMed] [Google Scholar]
- 16.Lidar M, Langevitz P, Shoenfeld Y. The role of infection in inflammatory bowel disease: initiation, exacerbation and protection. Isr Med Assoc J 2009;11:558–63. [PubMed] [Google Scholar]
- 17.Zuo T, Zhang F, Lui GCY, et al. Alterations in gut microbiota of patients with COVID-19 during time of hospitalization. Gastroenterology 2020;159:944–55. 10.1053/j.gastro.2020.05.048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xiao F, Tang M, Zheng X, et al. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology 2020;158:1831–3. 10.1053/j.gastro.2020.02.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Effenberger M, Grabherr F, Mayr L, et al. Faecal calprotectin indicates intestinal inflammation in COVID-19. Gut 2020;69:1543–4. 10.1136/gutjnl-2020-321388 [DOI] [PMC free article] [PubMed] [Google Scholar]