Abstract
Objective
To synthesise the published literature on practitioner, patient and carer views and experiences of shared medical appointments (SMAs) for the management of long-term conditions in primary care.
Design
Systematic review of qualitative primary studies.
Methods
A systematic search was conducted using MEDLINE (Ovid), PsycINFO (Ovid), CINAHL (EBSCOhost), Web of Science, Social Science Premium Collection (Proquest) and Scopus (SciVerse) from database starting dates to June 2019. Practitioner, patient and carer perspectives were coded separately. Deductive coding using a framework approach was followed by thematic analysis and narrative synthesis. Quality assessment was conducted using the Critical Appraisal Skills Programme for qualitative studies.
Results
We identified 18 unique studies that reported practitioner (n=11), patient (n=14) and/or carer perspectivs(n=3). Practitioners reported benefits of SMAs including scope for comprehensive patient-led care, peer support, less repetition and improved efficiency compared with 1:1 care. Barriers included administrative challenges and resistance from patients and colleagues, largely due to uncertainties and unclear expectations. Skilled facilitators, tailoring of SMAs to patient groups, leadership support and teamwork were reported to be important for successful delivery. Patients’ reported experiences were largely positive with the SMAs considered a supportive environment in which to share and learn about self-care, though the need for good facilitation was recognised. Reports of carer experience were limited but included improved communication between carer and patient.
Conclusion
There is insufficient evidence to indicate whether views and experiences vary between staff, medical condition and/or patient characteristics. Participant experiences may be subject to reporting bias. Policies and guidance regarding best practice need to be developed with consideration given to resource requirements. Further research is needed to capture views about wider and co-occurring conditions, to hear from those without SMA experience and to understand which groups of patients and practitioners should be brought together in an SMA for best effect.
PROSPERO registration number
CRD42019141893.
Keywords: general medicine (see internal medicine), health services administration & management, primary care, qualitative research
Strengths and limitations of this study.
Focus on qualitative evidence provides rich insights into barriers to implementation of shared medical appointments (SMAs) in primary care from the perspectives of practitioners, patients and carers.
Robust search strategy, based on previous high-quality reviews, refined to allow us to better identify qualitative research.
The thematic synthesis approach has enabled the identification of analytical themes that offer a new interpretation of practitioner and patient experiences of SMAs beyond earlier reviews.
Rapidly evolving area of practice and publications and the most recent evidence may be missing.
Grey literature was excluded from the synthesis
Introduction
Over 15 million people in England are living with one or more long-term conditions.1 Such multimorbidity is more prevalent in those over 65 years and in socioeconomically deprived areas.2 3 Long-term conditions require ongoing disease management and care, which consume a significant amount of healthcare service delivery time.4 Models of care that support patient self-management (or self-care) are at the centre of government policies worldwide,5 including NHS plans.6 7 Shared medical appointments (SMAs) or group consultations have been promoted as a new way of delivering primary care to simultaneously improve patient self-management and resource use efficiency.8 9
SMAs typically involve a group of patients with the same long-term condition(s) meeting with one or more healthcare practitioners. In contrast to group education programmes, the SMA usually replaces a 1:1 appointment and may include physical examinations, medication adjustments or other clinical interventions.8 10 It has been theorised that SMAs may improve patient self-efficacy by enabling participants to witness the consultation experiences of others and to observe disease management strategies of peers who act as realistic role models for their own self-care.4 10 While there is some evidence that SMAs can support self-management of long-term conditions,4 it is important to understand the feasibility and acceptability of implementing SMAs from the perspectives of primary healthcare practitioners, patients and carers to ascertain if this model of care can meet their needs and reduce health inequalities.
It has been reported that practitioners enjoy SMAs, citing benefits including development of team relationships, learning from patients and more variety in work.4 10 Patients attending SMAs have also reported feelings of socialisation or normalisation of a condition, increased trust with healthcare practitioners and enhanced knowledge.4 11 However, a small number of studies have reported patient concerns, including confidentiality and being unclear about the purpose of a session.4 Providers have reported concerns around insufficient clinician and group facilitation training for SMAs and the need for suitable premises.4 11 12 Earlier reviews have focused on secondary care,4 which is typically disease-specific with time-limited follow-up after specialist treatment.11 In contrast, primary care has an emphasis on ongoing disease management, often including multiple conditions, and care continuity. Hence, this systematic review of qualitative research aimed to provide an in-depth insight into the experiences and perceptions of SMAs for the management of long-term conditions in primary care, including identifying barriers and facilitators regarding implementation.
Review research questions:
What are patient and practitioner views and experiences of SMAs in primary care?
Do these views and experiences vary by long-term condition and/or other patient/ practitioner characteristics?
What does the literature tell us about potential barriers and facilitators to the delivery and uptake of SMAs in primary care?
Methods
A systematic review and narrative synthesis of qualitative studies was conducted.
Search strategy and selection criteria
We searched MEDLINE (Ovid), PsycINFO (Ovid), CINAHL (EBSCOhost), Web of Science, Social Science Premium Collection (Proquest) and Scopus (SciVerse) from database start dates to June 2019. A combination of keywords and Medical Subject Headings to locate relevant qualitative studies were used (see online supplemental file 1). Database searches were supplemented by forward and backward citation searches of the included papers.
bmjopen-2020-046842supp001.pdf (56.4KB, pdf)
Primary qualitative studies were included that (1) explored the views of primary healthcare practitioners, staff, patients or carers that had been involved in the delivery of or attended SMAs within primary care; (2) met our criteria to be classed as an SMA (group appointments that were intended to replace standard 1:1 appointments in general practice, were delivered by primary care practitioners, and included clinical advice and management as well as peer learning and support); and (3) had a patient population with at least one long-term condition. For studies in which participants delivered/attended SMAs for both long-term conditions and non-long-term conditions, only data relating the former were extracted and synthesised. Papers were excluded if (1) the group session did not include an individual assessment/examination/consultation with a primary healthcare professional; (2) papers reported survey data only; and (3) it was not possible to differenciate between data collected from participants attending SMAs for long-term conditions those attending SMAs for non-long-term conditions (eg, antenatal care).
The title and abstracts of retrieved citations were double-screened, and where there were discrepancies, screeners met to reach agreement. All studies at the full-text stage were similarly double-screened with any uncertainties resolved by discussion with a third member of the review team.
Quality assessment
Methodological quality of eligible studies was assessed by two independent reviewers using the Critical Appraisal Skills Programme (CASP) checklist for qualitative studies.13 This was done to assess conduct (validity and robustness), transparency, content and utility of findings. Studies were not excluded on the basis of this appraisal, as limited reporting is not necessarily indicative of low-quality research and risks the exclusion of appropriate studies.14 The strengths and limitations of each included study were considered during the analysis to ensure that findings from unreliable studies did not unduly influence our results.15
Data extraction and synthesis
Key characteristics of the included studies and study participants were recorded using a data extraction form, with the extracted data double-checked by another team member. Full-text papers were then imported into NVivo V.12. A framework based on themes previously identified by reviews4 10 was used to deductively code participant quotes and authors’ interpretations in the Results and Discussion sections of the studies. All data were coded by one reviewer then checked by a second. Data reflecting the views of practitioner, patients and carers were analysed separately.
Data excerpts were compared and contrasted, and descriptive themes were formed by merging codes and grouping them around existing themes4 and emerging themes. This included condensing the existing themes into related/discordant subthemes which were subsequently translated into higher-level themes to better answer the research questions. Texts were reread and data recoded according to newly structured thematic framework through an iterative process to ensure these themes best reflected the data. Data excerpts were then examined to look for similarities and differences in the perspectives of practitioners or patients by characteristics (eg, gender and age).
The Enhancing Transparency in Reporting the Synthesis of Qualitative Research checklist was used for reporting this review (see online supplemental material).
bmjopen-2020-046842supp002.pdf (81.8KB, pdf)
Patient and public involvement (PPI)
The proposed programme of SMA research was presented to a PPI panel who provided their views and opinions about what potential barriers and facilitators to attending an SMA might be from a patient perspective, thus providing insights into potential findings of the review. Our affiliated PPI group read and commented on the draft of this article and have identified several patient community groups through which to share a lay summary of the research findings.
Results
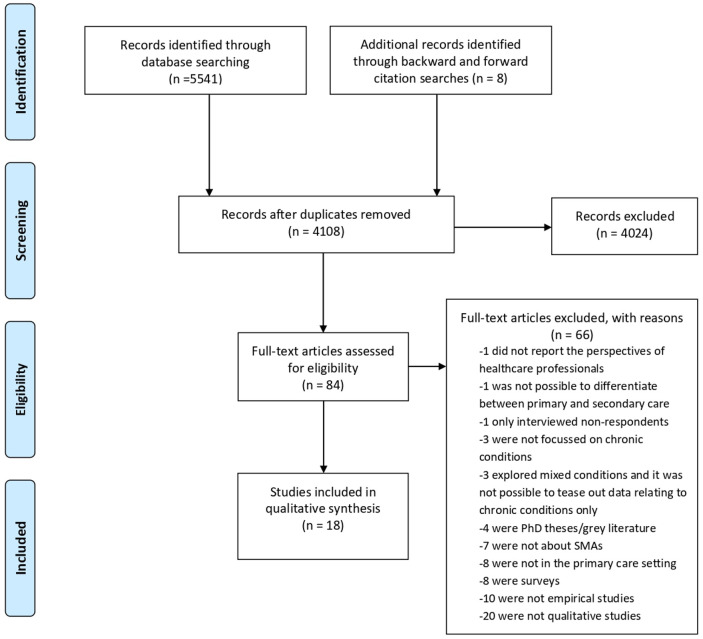
Figure 1 outlines the screening and selection process resulting in the inclusion of 18 studies in the final synthesis.
Figure 1.
Flow diagram of review search. Our search resulted in the retrieval of 84 papers for full-text review. Of these, 66 were ineligible for inclusion. Three additional studies were identified following forward and backward citation searches. This resulted in the inclusion of 18 studies in the final synthesis. SMA, shared medical appointment.
Quality appraisal
Quality of the included studies was generally high; most papers met the majority of the CASP checklist criteria (online supplemental file 2). Weaknesses commonly related to lack of information about participant recruitment16–22 and researcher reflexivity, which was missing in all but two studies.23 24
bmjopen-2020-046842supp003.pdf (75.1KB, pdf)
Overview of included studies
Studies were published between 2004 and 2018 and are summarised in table 1. Studies report the views and experiences of a total of 262 practitioners, 306 patients and 39 carers. The majority of studies were from North America; two were from Australia. Only two studies looked at the views of those healthcare professionals who were not delivering SMAs22 25; the rest of the studies reported the views of individuals with experience of having delivered/attended SMAs. One study26 involved video SMAs; all others were face to face. One study focused on an SMA for children.16
Table 1.
Overview of studies and participant characteristics
| First author and date | Country | Methodology and data collection method | Participants: practitioners | Participants: patients | Participants: carers | |||||||||
| N, job | Age range (years) | %Female | Ethnicity | N | Age (years) | %Female | Ethnicity | N | Age | %Female | Ethnicity | |||
| Arney et al 201823 | USA | Qualitative: interviews | 35 (11 behavioural health staff, 18 AHPs and 6 admin) | 35–64 | 80 | Varied: 83% White | 0 | N/A | N/A | N/A | 0 | N/A | N/A | N/A |
| Bauer et al 201716 | USA | Qualitative: interviews and verbal feedback session | 9 (5 paediatricians, 3 AHPs and 1 NP) | NR | NR | 100% White | 41 | 6–14 | 24 | Varied: 32% Black, 34% Hispanic/Latino, 18%White | 34 | 53%<40 years, 23% ≥40 years | 97 | Varied: 33% Black, 47% Hispanic/Latino, 20% White |
| Cornelio-Flores et al 201817 | USA | Mixed methods: focus groups and interviews | 0 | N/A | N/A | N/A | 11 | Mean 51.6 | 89 | 100% Hispanic | 0 | N/A | N/A | N/A |
| Drake et al 201818 | USA | Mixed methods: focus groups and interviews | 6 (physician, nurse, AHP and admin) | NR | NR | NR | 8 | NR* | NR* | NR* | 0 | N/A | N/A | N/A |
| Egger et al 201519 | Australia | Mixed methods: interviews | 8 GPs | NR | NR | NR | NR* | NR* | NR* | NR* | 0 | N/A | N/A | N/A |
| Housden et al 201625 | Canada | Qualitative: interviews | 7 NPs | NR | 86 | NR | 0 | N/A | N/A | N/A | 0 | N/A | N/A | N/A |
| Housden et al 201727 | Canada | Qualitative: interviews and observations | 12 NPs | NR | NR | NR | 12 | 40–79 | 58 | Varied: 83% Euro-Canadian | 0 | N/A | N/A | N/A |
| Kowalski et al 201828 | USA | Qualitative: interviews | 28 (physicians, nurses, AHPs, facilitators and researchers) | NR | NR | NR | 0 | N/A | N/A | N/A | 0 | N/A | N/A | N/A |
| Lavoie et al 201329† | Canada | Qualitative: interviews | 34 (10 physicians, 7 NPs, 2 nurses, 4 admin, 11 AHPs) | NR | NR | NR | 29 | Mean 62 | 66 | Varied: 55% White, 45% Aboriginal | 0 | N/A | N/A | N/A |
| Miller et al 200433 | USA | Mixed methods: interviews | 0 | N/A | N/A | N/A | 26 | NR* | NR* | NR* | 0 | N/A | N/A | N/A |
| Siple et al 201520 | USA | Qualitative: focus groups | 0 | N/A | N/A | N/A | 18 | 30–80 | 6 | NR | 3 | NR | 100 | NR |
| Stevens et al 201421 | Australia | Qualitative: focus groups | 46 (GP, nurse, AHP and admin | NR | 67 | NR | 49 | 30–70 | 43 | Varied: 90%Non-Indigenous | 0 | N/A | N/A | N/A |
| Stowell et al 201522 | USA | Mixed methods: interviews | 13 medical students | NR | NR | NR | 4 | NR* | NR* | NR* | 0 | N/A | N/A | N/A |
| Stults et al 201632 | USA | Qualitative: focus groups | 0 | N/A | N/A | N/A | 30 | 52–93 | 33 | Varied: 87% White, 7% Hispanic/Latino, 3% Asian/Pacific Islander | 0 | N/A | N/A | N/A |
| Thompson et al 201424 | Canada | Qualitative: semistructured interviews | 0 | N/A | N/A | N/A | 9 | 46–62 | 0 | Varied: ‘predominantly’ White | 0 | N/A | N/A | N/A |
| Tokuda et al 201626 | USA | Mixed methods: focus groups and interviews | 2, NP and AHP | NR | NR | NR | 15 | NR* | NR* | NR* | 2 | NR | NR | NR |
| Thompson-Lastad 201830 | USA | Ethnography: ethnographic observations, interviews conducted in English and Spanish |
28 (13 doctors, 1 NP, 5 AHPs and 8 admin) | NR | 79 | Varied: 54% White | 25 | Mean 58 | 72 | Varied: 60% Black/African–American | 0 | N/A | N/A | N/A |
| Wong et al 201531† | Canada | Qualitative: interviews | 34 (10 physicians, 7 NP, 2 nurses, 4 admin and 11 AHPs) | NR | NR | NR | 29 | Mean 62 | 66 | Varied: 55% White, 45% Aboriginal | 0 | N/A | N/A | N/A |
Admin denotes administrators including healthcare/programme managers and primary care/group visit coordinators. Carers included parents/guardians, wives and social support.
AHPs include pharmacists, dieticians, psychologists, social workers, substance abuse counsellors and nutritionists.
*Data given for shared medical appointment attendees but not separately for study participants.
†Same study participants, different data analysis.
AHP, allied health professional; GP, general practitioner; N/A, not applicable; NP, nurse practitioner; NR, not recorded.
The healthcare practitioner views most commonly reported were general practitioners (GPs), family physicians, practice nurses and nurse practitioners (NPs).16 18 19 21 24 25 27–31 Fewer studies captured the views of healthcare managers, programme/research coordinators and administrators.18 21 23 28–31
The SMAs varied in terms of content, duration, numbers of attendees and frequency of sessions. The majority of studies focused on single-condition SMAs (n=12); three reported on both single-condition and mixed-condition SMAs29 31 32; two reported on mixed-condition SMAs only27 33; and one gave no details.25 ‘Mixed-condition’ SMAs were for patients with one or more of a number of different conditions and thus included those with one condition and those with multimorbidity. Studies of SMAs for diabetes were most common (n=15). A summary of the SMAs is given in table 2.
Table 2.
Characteristics of SMAs delivered in reviewed studies
| First author and date | Description of SMAs | ||||||
| Duration (min) | Attendees (n) | Sessions (n) | Frequency | Long-term condition(s) on which SMA(s) focused | Attendees | Setting | |
| Arney et al 201823 | NR | 5–7 | 4 | NR | Diabetes (type 1) | Veterans | Hospital and community |
| Bauer et al 201716 | 60–75 | NR | 5 | Monthly | ADHD | School age children | Academic centre and community |
| Cornelio-Flores et al 201817 | NR | NR | 9 | Weekly | Chronic pain | Adults, Spanish-speaking Latino population, average age 51.6 years, 89% Female | Hospital and community |
| Drake et al 201818 | 120 | NR | 8 | Monthly | Diabetes (type 2) | Adults, varied ethnicity (74% Black/African–American), average age 55.1, 72% Female | Medical home providing primary care services |
| Egger et al 201519* | 90 | 3–15 | 3 | Monthly | Multiple single-condition SMAs: diabetes (type 2), chronic pain, weight loss and general long-term conditions | Adults, 5% Aboriginal/Torres Strait Islander, aged between 24 years and 86 years | Health centres |
| Housden et al 201625 | N/A | N/A | N/A | N/A | N/A | N/A | N/A |
| Housden et al 201727 | N/A | N/A | N/A | N/A | Healthy living and nutrition-focused mixed SMA for patients with diabetes, obesity, heart disease and/or arthritis | Adults including individuals with concurrent disorders, refugees, those with addiction or other mental health conditions, young adults, women and individuals from First Nations | Community and primary care |
| Kowalski et al 201828 | 120 | 8–10 | NR | NR | Diabetes | Veterans | Veterans Affairs health systems |
| Lavoie et al 201329† | Average 90 | 12–20 | NR | NR | Single-condition SMAs for chronic pain or diabetes and mixed SMAs for multimorbidities, including diabetes, hypertension and arthritis | Adults, living in rural communities | Primary healthcare services |
| Miller et al 200433 | 90 (+30 1:1) | 7 | 6 | Monthly | Mixed SMAs for one or mixed morbidity, including cardiovascular disease, diabetes and osteoarthritis | Adults, varied ethnicity (71% Hispanic/Latino), aged 40–64 years (mean 50), 100% Female | Community health centres |
| Siple et al 201520 | NR | NR | 4 | NR | Diabetes (type 2) | Veterans | Veteran Association Healthcare System |
| Stevens et al 201421 | NR | NR | NR | NR | Diabetes or pre-diabetes (type 2) | Adults with diabetes or pre-diabetes | Regional medical centres |
| Stowell et al 201522 | NR | NR | NR | NR | Diabetes | Adults with type 2 diabetes | Not specified |
| Stults et al 201632* | NR | NR | NR | NR | Single-condition SMAs: (1) pre-diabetes management; (2) type 2 diabetes management; (3) successful ageing that covered issues of concern for seniors (memory, falls and depression); (4) mind–body management; and (5) men’s physicals |
Not specified | Primary care practices |
| Thompson et al 201424 | NR | NR | 24 | Monthly | Diabetes (or at risk of) | Not specified | Community health centre that serves marginalised and vulnerable patients |
| Thompson-Lastad 201830 | 60–120 | NR | NR | Weekly | Single-condition SMAs: hypertension, mental health condition, chronic back pain, pre-diabetes and diabetes*† | Low-income adults | Community health centres |
| Tokuda et al 201626 | 120 | 3–5 | 6 | Weekly–bimonthly | Diabetes for >10 years | Adults, varied ethnicity (55% Asian/Pacific Islander) mean age 60.4 years, 0%Female | Video-SMA to community-based outpatient clinic |
| Wong et al 201531† | 60–90 | 9–15 | NR | Weekly–quarterly | Single-condition SMAs for chronic pain or diabetes and mixed SMAs for mixed diagnosis, including diabetes, hypertension and arthritis | Adults living in rural communities | Community and primary care |
*Study includes SMAs run for non-chronic health conditions. Data extracted for long-term conditions.
†Same study, two papers.
NR, not recorded; SMA, shared medical appointment.
Narrative synthesis
Tables 3 and 4 present the findings of the analysis of practitioner and patient perspectives, respectively. Each table outlines examples of codes that were used to group the data into subthemes, which were subsequently translated into higher-level themes. Practitioner themes were ‘advantages and benefits’, ‘barriers and challenges’ and ‘implementation success and sustainability’.
Table 3.
Views and experiences of practitioners and staff
| Themes | Subthemes | Exemplar codes | Exemplar quotes and data |
| Advantages and benefits | Comprehensive patient-led care | Multidisciplinary care, patient-led, increase patient understanding, increase practitioner understanding | ‘…one person’s worried about hyperglycemia and another person’s worried about nocturia, and another person’s worried about their vision you get information that can be both preventative and curative all in the same visit’. NP25 |
| Peer support and accountability | Normalise condition, offer support, share experiences, encourage accountability, increase motivation | ‘The biggest part is just that they [the patients] get to kind of feed off of each other and they talk about what works and what doesn’t… I think that the fact that they can help teach each other is most important’. Dietician23 | |
| Efficiency and lower cost | More efficient, less repetition, improved access, costs | [The SMAs] kind of a win all around because when you increase your productivity you increase access for patients, your waiting times go down…we’re better able to meet evidence-based guidelines because there’s a team taking care of patients rather than a single provider’. Provider 131 | |
| Barriers and challenges to adoption and implementation | Patient resistance and suitability | Accustomed to 1:1 appointment, not for all patients, attached to physician, confidentiality | ‘Definitely the top barrier will be convincing the patients to show up. We invite an average of 10 people and we usually have between 4 and 7 who come and continue to show up. I think patient buy-in is definitely a barrier’. Primary care physician28 |
| Role adjustment and uncertainties | Colleague resistance, self-efficacy/new skills, power relationships, managing peer interaction | ‘I’ve got to tell you, it’s a hard sell with physicians. Even now, I don’t have a champion for the diabetes SMA. They see it as extra work. They don’t see the added value. It troubles me a lot that it’s so hard to get the docs involved’. Nurse28 | |
| Administrative and resource challenges | Coordinating schedules, patient reminders, funding and billing, lack of space/rooms, staff shortage, busy staff | Author interpretation: NPs described how physical space, administrative time, and buy-in were major barriers to the diffusion of Group Medical Visits. Many NPs described the challenges of lacking regular office space or having limited administrative time, which required them to engage in clinical organization during personal or unpaid time.25 | |
| Implementation success and sustainability | Skilled facilitator | Facilitator—important, group management | Author interpretation: The role of the facilitator was thought to be crucial to the successful operation of the group, and selection and training for the facilitator was seen as crucial to success.21 |
| Tailored to patient groups | Patient background, disease stage | ‘…critical that we (the video-SMA providers) were sensitive and expressed a value for diversity; that we were conscious of the dynamics inherent to the participant’s cultures especially in the group interaction and demonstrated that we (the video-SMA providers) had knowledge regarding these differences and were willing to adapt our service delivery’. Provider26 | |
| Leadership, teamwork and communication | Leadership, teamwork, communication, collegiality | ‘It cannot be one person because the key word is ‘sustainability.’ If that person ever leaves or something ever happens, everything falls apart’. Administrator18 ‘I think speaking to the importance of research and teamwork, getting people together for the betterment of patient care and the collegial approach to doing the kind of thing that brings people from different disciplines together, particularly nursing and the primary care providers. I think that’s where we’ve got to wear that cap to get the right people engaging and working together’. Administrator and primary care physician23 |
NP, nurse practitioner.
Table 4.
Views and experiences of patients and carers
| Themes | Subthemes | Exemplar codes | Exemplar quotes and data |
| Benefits of SMAs | Peer support | Feeling supported, reassurance | ‘I wasn’t the only one who had ADHD. It’s like there’s more people to know how it feels… I really don’t talk to anybody about my stuff I have to go through, so it was fun to tell people about it’. Patient with ADHD16 |
| Vicarious learning and collective problem solving | Surrogate questioning and answers, listening and discussion, learning from peers’ experience | ‘I didn’t even want to go on the medication. To me it was no you know. But hearing it from her [another group member] how it worked for her, I decided to try it. And I’m glad I have, because it has helped me control it’. Patient with diabetes24 | |
| Motivation for self-management | Learn self-management strategies, improved self-management, accountability | ‘… you come out of the group feeling much more self-confident … you’ve got your batteries recharged and you can really go till the next group … it’s more motivating … you want to do more yourself and rely less on others … but then you always realize there’s others out there to help you if needed’. Patient31 | |
| Safe environment to share | Inviting and comfortable atmosphere, honesty, anonymity in group, enjoyment, more time | ‘I just noticed that, listening to the other people, they brought up some things that may have related to me that I felt were my weaknesses or things that I did that I wouldn’t wanna disclose because I might feel a bit of shame or embarrassment, but after hearing other people be open and honest, I think it gives me—or just allows you to be more honest yourself because you’ve already heard other people expose themselves or be honest. Male, approximately 60 years old, type 2 diabetes SMA32 | |
| Barriers to SMA attendance and success | Cultural barriers | Dislike group work, confidentiality and privacy concerns, can’t relate to others, dislike divided time and attention, lacking motivation/ interest in health, sessions too long | Author interpretation: One male stated he was ‘too busy’ to be sitting around in a doctor’s surgery for 90 minutes, although agreed that the total time taken for a consultation, with waiting time, etc, may equal this.21 Author interpretation: While some initially thought sharing information in the group situation was a problem, a concern over privacy tended to drop away after talking about this. ‘I suppose you don’t have to disclose what you don’t want to’. Female21 |
| Physical barriers | Accessibility of venue, transportation costs | ‘I’m on a fixed income, I’m a retiree, and sometimes it gets a little expensive when you’re charting out what you can spend each month … maybe if they could throw a little something in each month, like maybe $10 for transportation or something. Don’t you think that would help?’ Patient with diabetes18 |
Advantages and benefits
Comprehensive patient-led care
Practitioners viewed the care delivered via SMA to be more comprehensive25 29 31 and better suited to supporting self-management than 1:1 appointments.18 Longer appointment times enabled a range of issues and concerns to be covered in the one session18 22 25 and provided the opportunity for patients and practitioners to develop a care plan together.18 29 31 Practitioners reflected that the group sessions had improved their own practice as they were able to gain further insights into patient circumstances, their conditions and the challenges to self-management that patients face in their daily lives.16 25 27–29 Practitioners believed the presence of multiple clinicians with complementary expertise in the SMAs enabled more holistic care.23
Peer support and accountability
Practitioners valued the peer support afforded to patients by group appointments,19 23 28 30 31 believing patients benefitted from listening to the experiences of their peers and from hearing responses to other participants’ questions.22 This, in turn, helped them to understand their condition better and how best to manage it.19 23 Practitioners said patients were able to relate to each other, which helped to normalise their conditions16 and provide confidence in self-management.17 Some clinicians explained there was ‘cathartic value’ or ‘therapeutic effect’ from patients sharing with others in the group their personal story of disease management.16 21 29 The group format also enabled collective problem solving with clinicians and peers.31 Two studies also reported that practitioners believed that patients felt accountable to other group members, which increased their motivation to reach their self-set goals.28 29 However, a clinician in another study reported that the peer-to-peer support element of the SMA ‘didn’t work very well’ when two patients were paired together who were both ‘non-compliant’ and ‘didn’t give off the best information’.28
Efficiency and lower cost
Clinicians reported that they found the sessions enjoyable and made their work less repetitive,21 22 28 less rushed and more relaxed.21 GPs and other managerial staff perceived SMAs to be more time efficient and cost-effective than usual 1:1 appointments19 28 31 and improved patient access to healthcare.28 31 The multidisciplinary nature enabled them to get ‘a lot of work done’23 and meet evidence-based guidelines.31 However, nursing staff did not report time and cost efficiencies; rather they described the additional time and resources involved in setting up the SMAs.
Barriers and challenges to adoption and implementation
Patient resistance and suitability
NPs without SMA experience had concerns about recruitment and attendance, as patients were ‘historically’ and ‘culturally’ accustomed to receiving 1:1 care.25 They also expressed concerns over the appropriateness of group sessions for some patient population groups, particularly those with ‘concurrent disorders’ that ‘can’t keep to the timeline or sit long enough’.25 Lack of motivation to improve health21 and reluctance to share information in a group setting were perceived reasons why patients may not attend SMAs. Concerns about the ability to maintain patient confidentiality during the group session were raised but ‘lessened when it was explained that this is dealt with through a signed confidentiality agreement’.21 22
Practitioners with SMA experience reported that the top barrier to implementing SMAs was ‘convincing the patients to show up’.28 Patients were reported to be reluctant to take part in a group because they did not want to disclose medical history and health complaints to peers,23 and in one case, this was thought to contribute to SMAs being a short-lived and unsuccessful innovation.27 Some providers described how they spent time identifying patients they thought might be ‘willing to attend’ and did not invite those whom they felt were ‘less suited’ to SMAs, such as those who were hard of hearing, who had limited English speaking skills or who were uncomfortable in a group.31
Role adjustment and uncertainties
NPs experienced difficulties encouraging other staff within the practice to ‘buy in’ and support the SMAs,23 28 reporting it being a ‘hard sell’ to doctors who perceived them as ‘extra work’.28 There was uncertainty and hesitancy among practitioners about SMAs, what was expected of them. Some practitioners reported how SMAs changed the dynamics between patients and provider, with practitioners tending to step back or keep quiet and allow patients to explore and discuss and problem solve between themselves,29 30 but to intervene if misinformation was shared.30 A clinician with no previous experience of group care was initially concerned, recognising that different skills were needed for SMAs. Yet, with minimal coaching, she was ‘surprised at how easy’ it was to sit back, observe and listen rather than having the burden of needing to ‘always know the answers’.16 One study27 reported that there were changes in the power dynamics between professionals particularly between NPs and GPs, as the former often take the lead in delivery of SMAs. One NP reported being irritated when the physician had minimal input during the SMA yet ‘billed for the ten people that were in the group even though the NP had done all of the work, teaching, counselling and the prescriptions’.25
Administrative and resource challenges
The most commonly cited challenge to implementing SMAs was the large number of administrative tasks involved in setting them up,16 19 21–23 25 28 31 with clinicians reporting they can be particularly burdensome for ‘non-medical staff’.22 This included the coordination of schedules for multidisciplinary teamwork,16 21–23 28 access to the technological systems and support staff required to organise SMAs,25 26 identification of participants suitable for SMAs,28 31 difficulties in reminding patients of appointment times, and the preparation of clinical notes and documentation for each SMA. In the context of the US healthcare system, providers also expressed concerns over funding and billing for SMAs,16 18 19 22 27 28 31 with insurance reimbursement issues perceived as a barrier to providing SMAs. Lack of physical space to hold the SMAs was reported as key limitation16 23 27 28 31 as well as insufficient staff to support the adoption, implementation and maintenance of SMAs,16 23 28 with some clinicians giving competing demands on their time as a key challenge to implementation.23 28
Implementation success and sustainability
Skilled facilitator
Practitioners deemed the role of a facilitator to be crucial to the success of SMAs.19 21 28 30 31 They had an important role in making the atmosphere in the group session relaxed and conducive to sharing.31 However, not all clinicians were equipped with group facilitation skills, as one dietician reported having difficulties in managing patients in the group who were ‘overbearing’ and ‘offensive’ rather than supportive of other group members.28 Nurses reported that clinicians who could be flexible and were ‘willing to take a back seat’ were most suited to the SMA model of working.28
Tailored to patient groups
Several SMA studies were designed to target specific patient groups, for example, veterans with low health literacy23 and underserved Spanish speakers.17 Practitioners reported having spent time identifying and designing the SMAs for these specific groups31 and the need to be sensitive to the cultural diversity of group participants.26 For disease-specific SMAs, clinicians acknowledged it was important to take into account the disease stage of the SMA participant, as patients with more disease experience may ‘more adequately influence’ those with less experience.21 Most studies in this review did not describe the process by which patients were selected and invited to attend. An NP believed that the SMAs they tried to implement were unsuccessful because they were not organised and designed in a person-centred way; rather the incentive for the practice was ‘to see a bunch of people all at once and sign off’.25
Leadership, teamwork and communication
Two studies described the importance of having leadership support in order to adopt and implement the innovation23 28 to ensure sufficient time and resources were allocated to the SMAs. A team-based approach and effective communication between members, healthcare practitioners and practice staff were reported to be important for effective implementation, maintenance and sustainability.18 The delivery of care by multidisciplinary teams was also considered a key strength of group appointments.23
Patient and carer view and experiences
A number of subthemes emerged from the patient and carers’ perspectives within overarching themes of ‘benefits of SMAs’ and ‘barriers to SMA attendance and success’ (see table 4).
Benefits of SMAs
Peer support
Most patients described feeling supported by others in the group,16 19 21 22 27–29 feeling that ‘they were not the only one’ with their condition and enjoyed having a safe environment in which to share their experiences and feelings.16 Carers valued the group sessions reporting the additional support they received from being able to share with others in their situation.16
Vicarious learning and collective problem solving
Patients described learning more about their condition, disease progression and treatment options by listening to the lived experiences of others and observing and engaging with other individuals at different stages of their disease.17 27 Being able to ask multiple questions and hearing answers to questions they had not thought to ask were very beneficial.19 25 27 They more readily absorbed/listened more closely to health-related information from peers than from the clinician20 24 30 because they knew they had experienced it themselves. Hearing the experiences of others helped overcome feelings of isolation and provided patients with reassurance in their ability to self-manage.19 Support for SMAs was particularly strong from those with previous health-related group experience.21 Conversely, however, it was reported that some patients did not want to attend any further SMAs because they did not want to talk about their health concerns or listen to other people’s concerns in a group.31
Motivation for self-management
Patients reported feeling more motivated to self-manage their condition(s)17 18 20 and accountable to others in the group to adhere to medication26 and achieve goals that they set themselves.18 28 29 32 Veterans reported that they were using less medication following the group session and were better able to self-manage their condition.20 Similarly, carers reported that their children had learnt skills to manage their ADHD better.16
Safe environment to share
Some patients reported feeling anxious prior to attending SMAs and ashamed of how they had been controlling their condition. However, once they had attended the SMA, they found the session a safe environment in which to share and face their fears, and they had developed greater trust in their health practitioner.29 32 Another study reported that some patients felt the group environment was more relaxed and enjoyable than one-to-one appointments, as ‘there is a certain level of anonymity in a group setting’.29 It was widely reported that patients were satisfied with the care they received during the group sessions.16 19 22 24 26 29 32
Barriers to SMA attendance and success
Some studies reported that patients expressed dislike or lack of interest in group appointments.19 23 Some patients also expressed reservations about sharing personal information and about confidentiality prior to attending,19 21 23 33 especially in smaller communities21; however, this was not a concern after attending the group session.19 In the study of video SMAs,26 some patients reported negative experiences including that the SMA was too big (even though there were only four to six patients per SMA), and there was poor control of group dynamics, but this might have been specific to the remote delivery. It was recognised that a skilled facilitator improved enjoyment and engagement,24 and how providers communicate and interact with patients during the appointment can affect their experience.20 Others found it difficult to relate to other group members33 or did not want to talk about their issues, nor hear other patients’ issues in a group.31 Some patients reported they would have liked more individual time with the clinician26 33 or to have seen their own doctor.21 32 Barriers to attendance included scheduling conflicts with other commitments18 and transportation or parking issues.28
Discussion
This systematic review has identified a detailed literature, primarily from North America, that provides rich accounts of practitioners involved in the delivery SMAs. While most studies included patient perspectives, the richness of the supporting data varied between studies and overall was lower compared with practitioner perspectives. The patient quotes reported to support author interpretation were short and few in some studies, and often demographic information was missing, limiting the readers’ ability to judge the transferability of the findings. There was notably less comparable evidence examining carer perspectives. The experiences of some minority ethnic and indigenous groups were represented, thus offering insights into the acceptability of SMAs for these patient groups. The systematic search and selection measures enabled the identification and synthesis of data, which have brought to light several additional challenges to implementation.
Most practitioners and patients with experience of SMAs regarded them positively and reported several advantages compared with one-to-one appointments. GPs and NPs with SMA experience reported that they enjoyed the sessions, with several reporting they helped overcome the repetition fatigue often associated with traditional consultations. Practitioners also perceived SMAs could be a more efficient and effective way of delivering care. Most patients valued the provision of peer support and reported that being able to share and learn from each other helped improve their self-confidence and provided motivation to reach their goals. However, this experience was not shared by all patients, with some reporting that they were unable to relate to others in their group or that they felt others in the group talked too much. This highlights the need for effective facilitation and careful patient selection in order for SMAs to be successful.
Some practitioners reported difficulties in recruiting patients and garnering support for the delivery of SMAs from other practice colleagues. Notable barriers to SMA implementation included insufficient staff, time and resources to set up and run SMAs. Practitioners were concerned that patients would be reluctant to participate in a group appointment due to low motivation, confidentiality concerns and preference for 1:1 appointments. Some patients also expressed reservations about the group setting due to confidentiality concerns and desire for more time to discuss individual needs.
The positive experiences and perceived benefits of SMAs reported by practitioners and patients in this review corroborate those reported previously,4 10 which suggests SMAs may offer advantages in primary care similar to those in other healthcare settings. However, studies included in this review may be subject to reporting bias due to a focus on attendees rather than those who declined SMAs.4 10 11 Staff and facility inadequacies, patient participation and attendance, group dynamic incompatibilities and cost–benefit concerns have been listed as barriers to implementation previously.9 11 Our review of qualitative evidence provides additional, deeper insights into barriers linked to organisational culture. We found practitioner reports of difficulties in gaining support from colleagues in the wider practice, including managerial staff, some of whom expressed negative attitudes towards SMAs. Furthermore, SMAs involving multidisciplinary teams appear to challenge the traditional hierarchal role of practitioners in primary care, which leads to improved collegiality in some cases and frustration in others. This suggests that clear guidance and expectations around SMAs may not have been effectively communicated within practices. Our review has also highlighted that SMAs appear to be most successful when practitioners have designed and prepared SMAs for particular patient groups, and this work is reported to be resource and time intensive. Practitioners report mixed views about the efficiency of SMAs compared with 1:1 appointments in light of the time and resources to set them up, which requires further exploration.
Limitations
Although the quality of included studies was generally good, most of the healthcare professionals were GPs and NPs, which may limit the generalisability of our findings to other healthcare professionals in primary care such as pharmacists, physiotherapists and dieticians, etc. Few studies provided rich detailed accounts of patient and carers; thus, insights offered from the literature are limited. While PPI members were involved throughout this review, we did not involve nor conduct member checking with practitioners. This would have helped to strengthen the credibility of the review findings. Given that many of the patients were recruited immediately after the SMAs, it is possible that patients with negative SMA experiences or those who declined to participate may be missed; therefore, the sample may be biased.4 10 11 Similarly, only two studies included the perspectives of practitioners not implementing SMAs; therefore, other perceived barriers may not have been captured. Furthermore, the lack of researcher reflexivity reported in the studies highlighted a potential source of bias; those involved in developing or delivering SMAs could have influenced participants’ responses. This may help explain the discrepancy between providers telling researchers that patients were hesitant to attend SMAs, while the latter reported a great deal of enthusiasm. As most studies are from North America, it is unclear whether some barriers, such as payment/insurance reimbursement concerns, are applicable in other global healthcare systems. Limited and inconsistent reporting of study participant demographic information limited our understanding as to whether patient experiences and perspectives differ by long-term condition or other personal characteristics. None of the studies reported differences in patient perspectives based on gender, age ethnicity or cultural group. Similarly, the amount of detail reported about the SMA itself in terms of format, staffing, duration and mode of delivery was limited. It is possible that this underpins some of the differences in experiences of patients and practitioners reported in the studies. In addition, it is unclear whether patient willingness to attend SMAs is sustainable over time due to limited study period and follow-ups.
Most studies in this review reported SMAs designed to support patients with diabetes. Only a limited number of studies reported on other long-term conditions, yet the perceived benefits and experiences reported in mixed-condition studies were similar and do not appear to be condition-specific. Furthermore, only five studies explicitly stated that some SMA participants had multimorbidity. Thus, there was insufficient information reported to understand the acceptability of attending group appointments with individuals who have different combinations of conditions. Further exploration of the use and experience of SMAs for patients with multimorbidity is needed.
Conclusion
Practitioner, patient and carer experiences of SMAs delivered in primary care have generally been positive, with benefits to both practice and patients reported. However, there is not enough evidence to show if views and experiences vary by staff involved, medical condition and/or patient characteristics. Further research is needed to better understand which groups of patients and practitioners should be brought together in an SMA for best effect. Whether SMAs for single conditions adequately meet the care needs of patients with multimorbidity also needs further exploration. This will help to inform guidance for practitioners on how best to identify and recruit patients to SMAs, rather than identifying and inviting patients based on personal judgements, which could have implications for health inequalities. Having identified a number of barriers and facilitators, we found that policies and guidance need to be developed and effectively communicated across and within practices on how best to implement and evaluate SMAs in practice. This, in turn, may help to improve staff expectations and overcome the hesitancy regarding SMA approaches. Additional resources may be needed to deliver SMAs such as additional administrative support, further training, compatible IT systems and physical space; a needs assessment may be required at practice level. The views of healthcare practitioners not currently delivering SMAs are required to ensure all barriers have been comprehensively explored. This is important to fully understand what interventions might be necessary to support the widespread adoption and implementation of SMAs in primary care. In addition, given the increased use of video consultations due to the outbreak of COVID-19, further exploration as to the acceptability and feasibility of SMAs delivered via videoconference is warranted.
Supplementary Material
Acknowledgments
We thank the PRU BehSci Public Patient Involvement group and Jan Lecouturier for providing comments on the manuscript prior to submission. Professor Kaner is supported via an NIHR Senior Investigator award.
Footnotes
Contributors: EK, KJ and HM designed the study. MYT and KJ undertook the searches. FG, MYT, KJ, OO, EK and AOD carried out the screening. FG, MYT, KJ and HM carried out the data extraction and analysis. All authors contributed to the interpretation. FG wrote the manuscript that all authors contributed to and approved.
Funding: This paper is independent research commissioned and funded by the NIHR PRU in Behavioural Science (award: PR-PRU-1217-20501) and Research Capability Funding from North East Commissioning Support (award: N/A).
Disclaimer: The views expressed in this publication are those of the authors and not necessarily those of the NHS, the National Institute for Health Research, the Department of Health and Social Care or its arm's length bodies, and other government departments. The funders had no role in the design of the study, collection, analysis or interpretation of data, or in the writing of the manuscript.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information. As this study is a systematic review, all data reported has been previously published and is in the public domain.
Ethics statements
Patient consent for publication
Not required.
References
- 1.Department of Health . Long term conditions compendium of information. Third Edition, 2012. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/216528/dh_134486.pdf [Google Scholar]
- 2.Kingston A, Robinson L, Booth H, et al. Projections of multi-morbidity in the older population in England to 2035: estimates from the population ageing and care simulation (PACSim) model. Age Ageing 2018;47:374–80. 10.1093/ageing/afx201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barnett K, Mercer SW, Norbury M, et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 2012;380:37–43. 10.1016/S0140-6736(12)60240-2 [DOI] [PubMed] [Google Scholar]
- 4.Booth A, Cantrell A, Preston L, et al. What is the evidence for the effectiveness, appropriateness and feasibility of group clinics for patients with chronic conditions? A systematic review. Health Serv Deliv Res 2015;3:1–194. 10.3310/hsdr03460 [DOI] [PubMed] [Google Scholar]
- 5.Department of Health and Social Care . Advancing our health: prevention in the 2020s, 2019. Available: https://www.gov.uk/government/consultations/advancing-our-health-prevention-in-the-2020s/advancing-our-health-prevention-in-the-2020s-consultation-document [Accessed 29 Oct 2020].
- 6.Coulter A, Roberts S, Dixon A. Delivering better services for people with long-term conditions. King’s Fund, 2013: 1–28. https://www.kingsfund.org.uk/sites/default/files/field/field_publication_file/delivering-better-services-for-people-with-long-term-conditions.pdf [Google Scholar]
- 7.NHS England . The NHS long term plan 2019.
- 8.Clay H, Stern R. Making time in general practice, 2015. Available: https://www.primarycarefoundation.co.uk/images/PrimaryCareFoundation/Downloading_Reports/PCF_Press_Releases/Making-Time-in_General_Practice_FULL_REPORT_28_10_15.pdf
- 9.Jones T, Darzi A, Egger G, et al. Process and systems: a systems approach to embedding group consultations in the NHS. Future Healthc J 2019;6:8–16. 10.7861/futurehosp.6-1-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kirsh SR, Aron DC, Johnson KD, et al. A realist review of shared medical appointments: how, for whom, and under what circumstances do they work? BMC Health Serv Res 2017;17:113. 10.1186/s12913-017-2064-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wadsworth KH, Archibald TG, Payne AE, et al. Shared medical appointments and patient-centered experience: a mixed-methods systematic review. BMC Fam Pract 2019;20:97. 10.1186/s12875-019-0972-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Jones KR, Kaewluang N, Lekhak N. Group visits for chronic illness management: implementation challenges and recommendations. Nurs Econ 2014;32:118–47. [PubMed] [Google Scholar]
- 13.Critical Appraisal Skills Programme . Casp checklist: 10 questions to help you make sense of a qualitative research, 2018. Available: https://casp-uk.net/casp-tools-checklists/ [Accessed 29 Oct 2020].
- 14.Saini M, Shlonsky A. Systematic synthesis of qualitative research. pocket guides to social work research methods. New York: Oxford University Press, 2012. [Google Scholar]
- 15.Thomas J, Harden A. Methods for the thematic synthesis of qualitative research in systematic reviews. BMC Med Res Methodol 2008;8:1–10. 10.1186/1471-2288-8-45 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bauer NS, Azer N, Sullivan PD, et al. Acceptability of group visits for attention-deficit hyperactivity disorder in pediatric clinics. J Dev Behav Pediatr 2017;38:565–72. 10.1097/DBP.0000000000000492 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cornelio-Flores O, Lestoquoy AS, Abdallah S, et al. The Latino integrative medical group visit as a model for pain reduction in underserved Spanish speakers. J Altern Complement Med 2018;24:125–31. 10.1089/acm.2017.0132 [DOI] [PubMed] [Google Scholar]
- 18.Drake C, Meade C, Hull SK, et al. Integration of personalized health planning and shared medical appointments for patients with type 2 diabetes mellitus. South Med J 2018;111:674–82. 10.14423/SMJ.0000000000000892 [DOI] [PubMed] [Google Scholar]
- 19.Egger G, Dixon J, Meldrum H, et al. Patients' and providers' satisfaction with shared medical appointments. Aust Fam Physician 2015;44:674–9. [PubMed] [Google Scholar]
- 20.Siple J, Harris EA, Morey JM, et al. Experiences of veterans with diabetes from shared medical appointments. Fed Pract 2015;32:40–5. [PMC free article] [PubMed] [Google Scholar]
- 21.Stevens J, Cole M-A, Binns A, et al. A user assessment of the potential for shared medical appointments in Australia. Aust Fam Physician 2014;43:804–7. [PubMed] [Google Scholar]
- 22.Stowell SA, Miller SC, Fonseca V, et al. Continuing medical education for promoting shared medical visits in diabetes care: table 1. Clin Diabetes 2015;33:28–31. 10.2337/diaclin.33.1.28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Arney J, Thurman K, Jones L, et al. Qualitative findings on building a partnered approach to implementation of a group-based diabetes intervention in Va primary care. BMJ Open 2018;8:e018093–9. 10.1136/bmjopen-2017-018093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Thompson C, Meeuwisse I, Dahlke R, et al. Group medical visits in primary care for patients with diabetes and low socioeconomic status: users' perspectives and lessons for practitioners. Can J Diabetes 2014;38:198–204. 10.1016/j.jcjd.2014.03.012 [DOI] [PubMed] [Google Scholar]
- 25.Housden L, Wong ST, Browne AJ, et al. Complexities of introducing group medical visits with nurse practitioners in British Columbia. Policy Polit Nurs Pract 2016;17:198–207. 10.1177/1527154416675224 [DOI] [PubMed] [Google Scholar]
- 26.Tokuda L, Lorenzo L, Theriault A, et al. The utilization of video-conference shared medical appointments in rural diabetes care. Int J Med Inform 2016;93:34–41. 10.1016/j.ijmedinf.2016.05.007 [DOI] [PubMed] [Google Scholar]
- 27.Housden L, Browne AJ, Wong ST, et al. Attending to power differentials: how NP-led group medical visits can influence the management of chronic conditions. Health Expect 2017;20:862–70. 10.1111/hex.12525 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kowalski CP, Veeser M, Heisler M. Formative evaluation and adaptation of pre-and early implementation of diabetes shared medical appointments to maximize sustainability and adoption. BMC Fam Pract 2018;19:1–23. 10.1186/s12875-018-0797-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lavoie JG, Wong ST, Chongo M, et al. Group medical visits can deliver on patient-centred care objectives: results from a qualitative study. BMC Health Serv Res 2013;13:155. 10.1186/1472-6963-13-155 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Thompson-Lastad A. Group medical visits as participatory care in community health centers. Qual Health Res 2018;28:1065–76. 10.1177/1049732318759528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wong ST, Browne A, Lavoie J, et al. Incorporating group medical visits into primary healthcare: are there benefits? Healthc Policy 2015;11:27–42. 10.12927/hcpol.2016.24449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Stults CD, McCuistion MH, Frosch DL, et al. Shared medical appointments: a promising innovation to improve patient engagement and ease the primary care provider shortage. Popul Health Manag 2016;19:11–16. 10.1089/pop.2015.0008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Miller D, Zantop V, Hammer H, et al. Group medical visits for low-income women with chronic disease: a feasibility study. J Womens Health 2004;13:217–25. 10.1089/154099904322966209 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-046842supp001.pdf (56.4KB, pdf)
bmjopen-2020-046842supp002.pdf (81.8KB, pdf)
bmjopen-2020-046842supp003.pdf (75.1KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information. As this study is a systematic review, all data reported has been previously published and is in the public domain.