Summary
Background
Preterm birth rates have increased significantly worldwide over the past decade. Few epidemiological studies on the incidence of preterm birth and temporal trends are available in China. This study used national monitoring data from China's National Maternal Near Miss Surveillance System (NMNMSS) to estimate the rate of preterm birth and trends between 2012 and 2018 in China and to assess risk factors associated with preterm birth.
Methods
In this observational study, data were sourced from the NMNMSS between Jan 1, 2012, and Dec 31, 2018. Pregnancies with at least one livebirth, with the baby born at 28 weeks of gestation or more or 1000 g or more birthweight were included. We estimated the rates of overall preterm, very preterm (born between 28 and 31 weeks’ gestation), moderate preterm (born between 32 and 33 weeks’ gestation), and late preterm (born between 34 and 36 weeks’ gestation) births in singleton and multiple pregnancies and assessed their trends over time. We used logistic regression analysis to examine the associations between preterm birth and sociodemographic characteristics and obstetric complications, considering the sampling strategy and clustering of births within hospitals. Interrupted time series analysis was used to assess the changes in preterm birth rates during the period of the universal two child policy intervention.
Findings
From Jan 1, 2012, to Dec 31, 2018, 9 645 646 women gave birth to at least one live baby, of whom 665 244 (6·1%) were born preterm. In all pregnancies, the overall preterm birth rate increased from 5·9% in 2012 to 6·4% in 2018 (8·8% increase; annual rate of increase [ARI] 1·3 [95% CI 0·6 to 2·1]). Late preterm births (8·8%; ARI 1·5% [0·9 to 2·2]) and very preterm births (13·3%; ARI 1·8% [0·5 to 3·0]) significantly increased from 2012 to 2018, whereas moderate preterm births did not (3·8%; ARI 0·3% [95% CI –0·9 to 1·5]). In singleton pregnancies, the overall preterm birth rate showed a small but significant 6·4% increase (ARI 1·0% [0·4 to 1·7]) over the 7 year period. In multiple pregnancies, the overall preterm birth rate significantly increased from 46·8% in 2012 to 52·7% in 2018 (12·4% increase; ARI 1·9% [1·2 to 2·6]). Compared with women who gave birth in 2012, those who gave birth in 2018 were more likely to be older (aged ≥35 years; 7·4% in 2012 vs 15·9% in 2018), have multiples (1·6% vs 1·9%), have seven or more antenatal visits (50·2% vs 70·7%), and have antepartum complications and medical disease (17·9% vs 35·1%), but they were less likely to deliver via caesarean section (47·5% vs 45·0%). Compared with the baseline period (January, 2012 to June, 2016), a higher increase in preterm birth was observed after the universal two child policy came into effect in July, 2016 (β=0·034; p=0·03).
Interpretation
An increase in preterm births was noted for both singleton and multiple pregnancies between 2012 and 2018 in China. China's strategic investment in maternal and neonatal health has been crucial for the prevention of preterm birth. Due to rapid changes in sociodemographic and obstetric factors related to preterm birth—particularly within the context of the universal two child policy—such as advanced maternal age at delivery, maternal complications, and multiple pregnancies, greater efforts to reduce the burden of preterm birth are urgently needed.
Funding
National Key R&D Program of China, National Health Commission of the People's Republic of China, China Medical Board, WHO, and UNICEF.
Introduction
Preterm birth, defined as birth before 37 weeks’ gestation, is a global maternal and infant health problem. Approximately 11% of neonates worldwide were born preterm in 2014, and the prevalence of preterm birth varied widely between countries and regions (eg, in the USA 9·6% of babies were preterm and in China 6·9% of babies were preterm).1 An estimated 12 million preterm infants were born in Asia and sub-Saharan Africa, accounting for 81% of the global 15 million live preterm births.1 Complications of preterm birth are the leading cause of death in neonates and children younger than 5 years. Individuals who were born preterm have an increased risk of short-term and long-term morbidities, including respiratory distress syndrome, bronchopulmonary dysplasia, necrotising enterocolitis, neurodevelopmental impairment, chronic lung disease, hypertension, and glucose intolerance.2, 3, 4 Many maternal and fetal characteristics are associated with preterm birth, including maternal sociodemographic, nutritional, psychological, and behavioural characteristics, pregnancy status, and biological and genetic markers. However, the causes of preterm birth are not always understood.5
Research in context.
Evidence before this study
We searched PubMed and the China National Knowledge Infrastructure database for articles published from Jan 1, 2000, to Dec 31, 2019, using the terms “preterm or premature”, “incidence or prevalence”, and “China”, with no language restrictions. We also included the reference lists of selected articles. Only two studies reported the national preterm birth rates in China, but estimates were based on statistical models. 42 studies based on empirical data reported the preterm birth rates only at local or regional levels. Because of the local setting, these studies reported a low number of births. Most studies were cross sectional and hospital based. Two of these studies aimed to estimate national rates of preterm birth in China between 2011 and 2014 and between March 1, 2015, and Dec 31, 2016, but one study only included 89 hospitals in 25 provinces and the other only 63 hospitals in 23 provinces. Both estimates varied substantially because the studies sampled a small number of hospitals and did not cover all provinces in China. We found that very few studies reported preterm birth trends in China over time, particularly within the context of the universal two child policy. Whether the change in China's birth policy increased the risk of preterm birth was unclear.
Added value of this study
We used the largest and most updated dataset from China's National Maternal Near Miss Surveillance System to estimate the rate of preterm birth overall, within three preterm birth groups (very preterm, moderate preterm, and late preterm), and for all pregnancies (singleton and multiple) and all women (primiparous and multiparous) between Jan 1, 2012, and Dec 31, 2018. The study included more than 9 million pregnant women. We observed a significant increase in preterm births for both singleton and multiple pregnancies during the study period. Potential contributors might have included advanced maternal age, maternal complications, multiple pregnancies, and implementation of the universal two child policy. Unexpectedly, a reduction in caesareans and an increase in antenatal visits might have mitigated the increasing trend in preterm births.
Implications of all the available evidence
To our knowledge, this is the first nationally representative study to estimate the preterm birth rate in China, providing the most complete picture to date of trends in the rate of preterm birth and related risk factors since 2012. Preterm birth remains a crucial maternal and infant health issue due to the large number of babies born prematurely every year and an increase in the overall preterm birth rate in China. Although preventing preterm birth remains a challenge, strengthening antenatal care and management for pregnant women can be of great value in reducing the risk of preterm birth. Efforts should include health education and guidance in maternal and newborn care, continued monitoring and management in high-risk pregnant women, and improvements in the quantity and quality of antenatal visits. The most disadvantaged women—namely those with multiple pregnancies, older mothers, and those with obstetric complications—should be closely monitored. Our findings provide essential information regarding the prevention and management of preterm birth for clinical practitioners, public health professionals, and policy makers. This study also has implications for improving the quality and volume of data on preterm birth in other low-income and middle-income countries through standardisation of definitions, more accurate measurement of gestational age, and more thorough reporting of risk factors.
Although intense research efforts have focused on preventing preterm birth, rates of preterm birth have increased in worldwide over the past decade.1, 6 Globally, the preterm birth rate increased from 9·8% in 2010 to 10·6% in 2014.1 In addition to changes in measuring and recording preterm birth, other factors might contribute to the increase in preterm birth rate, such as an increase in the rate of multiple pregnancy associated with the use of assisted reproductive technology, advanced maternal age at childbirth,7, 8 more common use of obstetric interventions (eg, labour induction or caesarean delivery),9 and more prevalent maternal demographic risk factors (eg, advanced maternal age and higher maternal body-mass index).10, 11
Epidemiological studies on the incidence of preterm birth and temporal trends are few in China. Most of the available studies only reported the preterm birth rate at a municipal or provincial level.12, 13 Although several cross-sectional studies have analysed the preterm birth rate at the national level in China, the rates reported in the studies differed greatly due to differences in the sample populations. For example, one study based on the China Labor and Delivery Survey (89 hospitals in 25 provinces) reported that the weighted national rate of preterm birth was 6·7% of livebirths between 2015 and 2016.14 Another study based on the National Neonatal Network (63 tertiary hospitals in 23 provinces) reported a preterm birth rate of 11·0% of singleton livebirths between 2011 and 2014.15 In addition, due to a small number of national monitoring systems, vital statistics, and population-based studies, a modelling study was done by Chawanpaiboon and colleagues.1 This study predicted a preterm birth rate of 6·9% in China.
The Chinese Government implemented a universal two child policy on Oct 29, 2015, which came into effect on births in July, 2016. The change in birth policy might have led to changes in the sociodemographic characteristics of pregnant women, such as increasing the proportion of older pregnant women (≥35 years) and associated pregnancy complications, which might have increased maternal and infant health risk.16 Preterm birth trends in China over time need to be better understood.
China's National Maternal Near Miss Surveillance System (NMNMSS), established in October, 2010, by the National Health Commission of China, was designed to monitor women's health status during pregnancy. In this study, we used high-quality national monitoring data from the NMNMSS to estimate the rate of and recent trends in preterm births in China; additionally, we used the data to assess risk factors associated with preterm birth.
Methods
Study design and participants
In this observational study, we assessed data from China's NMNMSS for livebirths between Jan 1, 2012, and Dec 31, 2018. The NMNMSS includes data from 438 health facilities at the county level or higher across 326 urban districts and rural counties in 30 provinces (Tibet not included) within the National Maternal and Child Mortality Surveillance System. The sampling strategy is described in appendix 2 (p 2).17, 18 Within each sampled district or county, two health facilities with more than 1000 births per year were randomly selected (or one facility if only one was available). To select the hospitals, we first numbered the centres that meet the requirements in each surveillance district or county, then use the random number method to select the hospitals. Because health facilities with the necessary number of births were mostly located in urban areas, large hospitals in urban districts were oversampled; as a result, births in urban areas were over represented in the NMNMSS, particularly in central and west China. This study was approved by the ethics committee of the West China Second University Hospital, Chengdu, China.
The maternal sociodemographic and obstetric information of all pregnant or post-partum women admitted to the obstetric department at each of the included hospitals was prospectively collected from the time of admission to discharge. The doctors responsible for pregnancy care were trained to complete a specially designed data collection form for each pregnant woman according to their medical records. The data included the baby's date of birth, maternal age, education level, marital status, number of antenatal visits, parity, gestational age at delivery, mode of delivery, single or multiple pregnancy, and maternal complications (at any time during hospital admission). The data from each hospital were entered into a web-based reporting system centralised at the National Office for Maternal and Child Health Surveillance of China, Chengdu, China. A deliberate data quality control strategy was implemented in the NMNMSS (appendix 2 p 3).
We restricted our analysis to pregnancies with at least one live birth; the babies had to be born after 28 weeks of gestation or more or have birthweight of 1000 g or more, according to the definition of the perinatal period in China.19
Procedures
In accordance with criteria recommended by WHO, we defined babies as preterm if they were born before 37 weeks’ gestation. Preterm births were categorised as very preterm (born between 28 and 31 weeks), moderate preterm (born between 32 and 33 weeks), and late preterm (born between 34 and 36 weeks).20 In this study, we estimated gestational age on the basis of last menstrual period or an early ultrasound if the date of the last menstrual period is unknown. The selection exposure variables to be analysed was based on factors shown to have a possible association with preterm birth, including sociodemographic characteristics (region, hospital level, maternal education, marital status, maternal age, number of antenatal visits, parity, and type of pregnancy) and obstetric factors (vaginal or caesarean birth and maternal complications).5 We used common definitions according to China's criteria for region (east, central, and west),21 hospital level (levels 1–3; based on the number of beds, categories of clinical departments, number of medical staff members, type and quantity of equipment, and hospital funding),22 and maternal education level (illiterate, primary school, middle school, high school, and college or higher; appendix 2 pp 6–8).17
We classified maternal complications into mutually exclusive categories of obstetric complications, medical diseases, and none of the above. If women had both obstetric complications and medical diseases, they were categorised as part of the obstetric complications group. Antepartum complications included ruptured uterus, placenta previa, abruptio placentae, unspecified antepartum haemorrhage, chronic hypertension, gestational hypertension, pre-eclampsia, eclampsia, HELLP syndrome, or any fetal malpresentation (breech, shoulder, or other). Medical diseases included heart disease, embolism or thrombophlebitis, hepatic disease, severe anaemia (haemoglobin concentration of <70 g/L), renal disease (including urinary tract infection), lung disease (including upper respiratory tract infection), HIV, AIDS, connective tissue disorders, gestational diabetes, and cancer.
Statistical analysis
We calculated the number and rate of preterm births overall and within each preterm group, for all pregnancies, separately for singleton and multiple pregnancies, and for primiparous and multiparous women separately during the study period (Jan 1, 2012, to Dec 31, 2018). We also calculated the number and rate of preterm births overall and within each preterm group separately according to maternal sociodemographic and obstetric characteristics. Preterm birth rate was calculated as the number of liveborn preterm babies divided by the total number of births. Because NMNMSS oversampled large urban hospitals, we weighed the preterm birth rate based on the sampling distribution of the population according to the 2010 census of China, which has been described previously.17
We then examined the associations between maternal sociodemographic and obstetric characteristics and all preterm births and each of the preterm birth groups. We used logistic regression models, which accounted for sampling strategy and clustering of births within hospitals, to identify these associations. Because this was an exploratory analysis, we included all of the aforementioned sociodemographic and obstetric factors known to be associated with preterm birth that had been collected in the NMNMSS in the model. First, crude odds ratios (ORs) with 95% CIs were estimated for each of these factors. Second, we used multivariate logistic regression to estimate the ORs adjusted for potential confounders using two models. Model 1 was adjusted for maternal sociodemographic factors (region, maternal education, maternal age, marital status, antenatal visits, parity, and type of pregnancy [singleton vs multiple]). Model 2 was adjusted for the same factors as model 1 and for obstetric complications. To identify the most robust and stable model, we investigated both multicollinearity and goodness of fit (appendix 2 pp 9–10). We did not adjust for hospital level or mode of delivery, because we deemed both to be reflections of anticipated risk.
To investigate changes in the overall and the preterm groups rates of preterm birth and the proportions of maternal sociodemographic and obstetric characteristics over the study period, we selected factors that were potentially associated with changing trends in preterm birth, including maternal age, antenatal visits, multiple pregnancies, caesarean section, and obstetric complications. To examine whether there was a linear relationship over time, we did a Cochran Armitage test on these temporal trends using the PROC FREQ procedure in SAS (version 9.0). More details on these analyses are available in appendix 2 (pp 3–4).
The universal two child policy was introduced during the study; we hypothesised that this policy change might have been associated with changes in preterm births. We used interrupted time series analysis with ordinary least-squares regression models adjusted for autocorrelation to examine changes in preterm birth rates per month before and after the introduction of the universal two child policy. We defined the date that the universal two child policy took effect as July 1, 2016, 9 months after the announcement of the policy (Oct 29, 2015). Potential confounders included maternal age, antenatal visits, and multiple pregnancies. Statistical analyses were done with SAS and STATA (version 14.2). p values less than 0·05 were considered statistically significant.
Role of the funding source
The funder of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report.
Results
9 676 989 women had at least one live baby between Jan 1, 2012, and Dec 31, 2018. After excluding pregnancies of unknown gestational age, 9 645 646 (99·7%) pregnancies were included in the final analysis (of which 9 474 961 [98·2%] were singletons and 170 547 [1·8%] were multiples; there was no information on the number of fetuses in 138 pregnancies). 665 244 (6·9%) of 9 645 646 women gave birth to a live baby before 37 weeks of gestation was completed, giving a weighted preterm birth rate of 6·1% (birth rate was weighted for the sampling distribution of the population). Of these preterm births, 73 681 (11·1%) were very preterm, 92 551 (13·9%) were moderate preterm, and 499 012 (75·0%) were late preterm. The weighted rate of very preterm births was 0·6%, the rate for moderate preterm births was 0·8%, and it was 4·7% for late preterm births. The weighted rate of singleton pregnancies was 5·4%, whereas it was 49·4% for multiple pregnancies. The weighted rate of overall preterm births in primiparous women was 5·9%, whereas it was 6·3% for multiparous women (table 1).
Table 1.
Preterm births in singleton and multiple pregnancies and in primiparous and multiparous women in China, 2012–18
|
Year |
Change 2012–18 | Annual rate of increase (95% CI)*†‡ | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Total | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | |||
| All pregnancies (n=9 645 646) | ||||||||||
| Very preterm | 73 681 (0·6%) | 9079 (0·6%) | 9461 (0·6%) | 10 755 (0·6%) | 9949 (0·7%) | 11 569 (0·7%) | 11 784 (0·6%) | 11 084 (0·7%) | 13·3% | 1·8% (0·5 to 3·0) |
| Moderate preterm | 92 551 (0·8%) | 12 241 (0·8%) | 12 326 (0·8%) | 13 655 (0·8%) | 12 377 (0·8%) | 14 068 (0·8%) | 14 317 (0.8%) | 13 567 (0·8%) | 3·8% | 0·3% (−0·9 to 1·5) |
| Late preterm | 499 012 (4·7%) | 65 047 (4·5%) | 63 832 (4·5%) | 72 604 (4·5%) | 66 294 (4·6%) | 77 565 (4·7%) | 79 706 (4·8%) | 73 964 (4·9%) | 8·8% | 1·5% (0·9 to 2·2) |
| All preterm | 665 244 (6·1%) | 86 367 (5·9%) | 85 619 (5·9%) | 97 014 (5·9%) | 88 620 (6·1%) | 10 3202 (6·2%) | 10 5807 (6·2%) | 98 615 (6·4%) | 8·8% | 1·3% (0·6 to 2·1) |
| Singleton pregnancies (n=9 474 961)§ | ||||||||||
| Very preterm | 64 058 (0·6%) | 7948 (0·5%) | 8288 (0.6%) | 9270 (0·6%) | 8589 (0·6%) | 10 092 (0·6%) | 10 254 (0·6%) | 9617 (0·6%) | 13·2% | 1·6% (0·4 to 2·9) |
| Moderate preterm | 78 953 (0·7%) | 10 524 (0·7%) | 10 579 (0·7%) | 11 615 (0·7%) | 10 535 (0·7%) | 12 017 (0·7%) | 12 232 (0·7%) | 11 451 (0·7%) | 2·9% | 0 (−1·2 to 1·3) |
| Late preterm | 432 751 (4·1%) | 57 284 (4·1%) | 55 688 (4·0%) | 62 973 (4·0%) | 57 342 (4·1%) | 67 692 (4·2%) | 68 769 (4·2%) | 63 003 (4·3%) | 6·1% | 1·2% (0·5 to 1·8) |
| All preterm | 575 762 (5·4%) | 75 756 (5·3%) | 74 555 (5·3%) | 83 858 (5·3%) | 76 466 (5·4%) | 89 801 (5·5%) | 91 255 (5·5%) | 84 071 (5·7%) | 6·4% | 1·0% (0·4 to 1·7) |
| Multiple pregnancies (n=170 547)§ | ||||||||||
| Very preterm | 9606 (5·1%) | 1127 (4·8%) | 1164 (4·9%) | 1484 (5·3%) | 1360 (5·2%) | 1476 (5·2%) | 1529 (5·1%) | 1466 (5·1%) | 6·0% | 2·5% (1·0 to 4·0) |
| Moderate preterm | 13 588 (7·2%) | 1710 (7·2%) | 1747 (7·2%) | 2038 (7·3%) | 1841 (7·1%) | 2051 (7·4%) | 2085 (7·1%) | 2116 (7·4%) | 3·1% | 1·8% (0·3 to 3·4) |
| Late preterm | 66 245 (37·1%) | 7762 (34·8%) | 8141 (35·5%) | 9629 (36·2%) | 8951 (36·3%) | 9872 (37·2%) | 10 933 (38·9%) | 10 957 (40·1%) | 15·2% | 2·4% (1·6 to 3·2) |
| All preterm | 89 439 (49·4%) | 10 599 (46·8%) | 11052 (47·5%) | 13 151 (48·8%) | 12 152 (48·5%) | 13 399 (49·8%) | 14 547 (51·1%) | 14 539 (52·7%) | 12·4% | 1·9% (1·2 to 2·6) |
| Primiparous women (n=5 440 535)¶ | ||||||||||
| Very preterm | 37 851 (0·6%) | 5295 (0·5%) | 5481 (0·6%) | 5891 (0·6%) | 5243 (0·6%) | 5728 (0·6%) | 5293 (0·6%) | 4920 (0·6%) | 18·5% | 2·9% (1·2 to 4·7) |
| Moderate preterm | 48 866 (0·8%) | 7476 (0·8%) | 7314 (0·8%) | 7770 (0·8%) | 6607 (0·8%) | 7117 (0·8%) | 6529 (0·8%) | 6053 (0·8%) | 5·3% | 0·7% (−1·3 to 2·8) |
| Late preterm | 270 558 (4·5%) | 41 472 (4·4%) | 39 194 (4·4%) | 42 709 (4·4%) | 36 321 (4.6%) | 40 023 (4·6%) | 36 609 (4·7%) | 34 230 (4·8%) | 9·1% | 1·7% (0·9 to 2·4) |
| All preterm | 357 275 (5·9%) | 54 243 (5·7%) | 51 989 (5·7%) | 56 370 (5·7%) | 48 171 (6.0%) | 52 868 (6·0%) | 48 431 (6·1%) | 45 203 (6·2%) | 9·3% | 1·6% (0·7 to 2·6) |
| Multiparous women (n=4 194 100)¶ | ||||||||||
| Very preterm | 35 145 (0·7%) | 3774 (0·7%) | 3973 (0·7%) | 4855 (0·7%) | 4699 (0.7%) | 5837 (0·7%) | 6298 (0·6%) | 5709 (0·7%) | −5·7% | −1·6% (−3·1 to −0·1) |
| Moderate preterm | 430 86 (0·8%) | 4755 (0·9%) | 5005 (0·9%) | 5877 (0·9%) | 5766 (0·8%) | 6943 (0·8%) | 7629 (0.8%) | 7111 (0·8%) | −5·7% | −1·7% (−3·1 to −0·2) |
| Late preterm | 226 805 (4·8%) | 23 515 (4·7%) | 24 618 (4·7%) | 29 868 (4·7%) | 29 955 (4·7%) | 37 523 (4·8%) | 42 648 (4·8%) | 38 678 (4·9%) | 4·4% | 0·6% (−0·2 to 1·5) |
| All preterm | 305 036 (6·3%) | 32 044 (6·3%) | 33 596 (6·3%) | 40 600 (6·3%) | 40 420 (6·3%) | 50 303 (6·3%) | 56 575 (6·2%) | 51 498 (6·4%) | 1·9% | 0·1% (−0·8 to 1·0) |
Data are n (%), unless otherwise stated. % represents the number of liveborn preterm deliveries per 100 deliveries, adjusting for the sampling distribution of the population. Annual rate of increase represents the annual rate change in preterm birth rate from 2012 to 2018. Very preterm babies were born after 28–31 completed weeks' gestation. Moderate preterm babies were born after 32–33 weeks' gestation. Late preterm babies were born after 34–36 weeks' gestation.
Estimated by Poisson regression model with robust standard error.
Adjusted for the sampling distribution of the population.
Adjusted for the clustering of births within hospitals.
The records of 138 (<0·1%) pregnancies did not contain information regarding the number of fetuses.
A total of 11 011 (0·1%) women did not report information on parity.
The overall preterm birth rate increased from 5·9% in 2012 to 6·4% in 2018 (8·8% increase; annual rate of increase [ARI] 1·3% [95% CI 0·6 to 2·1]; table 1). The late preterm (8·8%; ARI 1·5% [0·9 to 2·2]) and very preterm (13·3%; ARI 1·8% [0·5 to 3·0]) subgroups significantly increased in size; the moderate preterm subgroup also increased in size by 3·8%, but the change was not statistically significant (ARI 0·3% [–0·9 to 1·5]; table 1).
Of the singleton pregnancies, the overall preterm birth rate significantly increased (6·4%; ARI 1·0% [CI 0·4–1·7]); the increase was more prominent in the very preterm subgroup than in the late preterm subgroup (table 1). Of the multiple pregnancies, the overall preterm birth rate significantly increased from 46·8% in 2012 to 52·7% in 2018 (12·4%; ARI 1·9% [1·2–2·6]); the increase was more evident in the late preterm subgroup than in the very preterm subgroup (table 1).
In primiparous women, the overall preterm birth rate significantly increased by 9·3% (from 5·7% in 2012 to 6·2% in 2018; ARI 1·6% [0·7–2·6); the greatest increase occurred in the very preterm birth subgroup. However, the overall preterm birth rate remained constant in multiparous women (table 1).
Most women gave birth at a level 2 or level 3 hospital, most had attended school and completed their middle education, and nearly all were married (table 2). High rates of overall preterm birth (more than 7·0%) were reported in women with low education level, single marital status, who were younger than 20 years or older than 35 years, low frequencies of antenatal visits (less than four visits), multiple pregnancies, caesarean sections, and antepartum complications (table 2).
Table 2.
Maternal sociodemographic and obstetric characteristics of all pregnancies according to gestational age in China, 2012–18
| Number of pregnancies (n=9 645 646) |
All preterm |
Very preterm |
Moderate preterm |
Late preterm |
|||||
|---|---|---|---|---|---|---|---|---|---|
| Rate (per 100 deliveries)* | Crude odds ratio (95% CI)*† | Rate (per 100 deliveries)* | Crude odds ratio (95% CI)*† | Rate (per 100 deliveries)* | Crude odds ratio (95% CI)*† | Rate (per 100 deliveries)* | Crude odds ratio (95% CI)*† | ||
| Region | |||||||||
| East | 2 796 175 (29·0%) | 197 604 (6·6%) | 1·19 (0·97–1·45) | 22 596 (0·7%) | 1·24 (0·84–1·82) | 27 129 (0·9%) | 1·20 (0·85–1·68) | 147 879 (5·0%) | 1·18 (1·01–1·38) |
| Central | 3 832 858 (39·7%) | 250 835 (5·7%) | 1 (ref) | 28 303 (0·6%) | 1 (ref) | 35 254 (0·7%) | 1 (ref) | 187 278 (4·3%) | 1 (ref) |
| West | 3 016 613 (31·3%) | 216 805 (6·1%) | 1·08 (0·92–1·27) | 22 782 (0·6%) | 1·01 (0·77–1·33) | 30 168 (0·8%) | 1·08 (0·84–1·38) | 163 855 (4·7%) | 1·09 (0·95–1·25) |
| Hospital level | |||||||||
| Unknown | 487 869 (5·1%) | 26 839 (4·5%) | 1·34 (0·91–1·96) | 2766 (0·4%) | 2·07 (1·19–3·60) | 3847 (0·6%) | 1·97 (1·10–3·52) | 20 226 (3·5%) | 1·22 (0·87–1·71) |
| Level 1 | 592 620 (6·1%) | 20 696 (3·4%) | 1 (ref) | 1255 (0·2%) | 1 (ref) | 1835 (0·3%) | 1 (ref) | 17 606 (2·9%) | 1 (ref) |
| Level 2 | 4 442 131 (46·1%) | 209 790 (4·5%) | 1·33 (1·15–1·53) | 16 599 (0·4%) | 1·66 (1·31–2·10) | 22 227 (0·5%) | 1·53 (1·22–1·92) | 170 964 (3·7%) | 1·28 (1·12–1·47) |
| Level 3 | 4 123 026 (42·7%) | 407 919 (9·6%) | 3·00 (2·53–3·55) | 53 061 (1·3%) | 6·27 (4·72–8·34) | 64 642 (1·5%) | 5·28 (4·05–6·87) | 290 216 (6·9%) | 2·52 (2·17–2·92) |
| Maternal education | |||||||||
| Illiterate | 46 802 (0·5%) | 5548 (10·0%) | 2·03 (1·72–2·40) | 821 (1·4%) | 2·95 (2·38–3·66) | 1034 (1·8%) | 2·94 (2·40–3·61) | 3693 (6·8%) | 1·78 (1·52–2·08) |
| Primary school | 286 364 (3·0%) | 25 939 (7·5%) | 1·50 (1·38–1·62) | 3400 (0·9%) | 1·94 (1·72–2·18) | 4199 (1·1%) | 1·83 (1·65–2·04) | 18 340 (5·5%) | 1·39 (1·29–1·50) |
| Middle school | 304 2496 (31·5%) | 181 315 (5·2%) | 1 (ref) | 18 914 (0·5%) | 1 (ref) | 24 451 (0·6%) | 1 (ref) | 137 950 (4·0%) | 1 (ref) |
| High school | 2 593 856 (26·9%) | 191 210 (6·4%) | 1·26 (1·15–1·37) | 21 539 (0·7%) | 1·39 (1·20–1·62) | 27 182 (0·9%) | 1·37 (1·19–1·56) | 142 489 (4·9%) | 1·22 (1·14–1·32) |
| College or higher | 3 473 549 (36·0%) | 241 097 (6·6%) | 1·30 (1·15–1·45) | 26 280 (0·7%) | 1·45 (1·16–1·82) | 32 364 (0·9%) | 1·38 (1·14–1·67) | 182 453 (5·0%) | 1·26 (1·15–1·39) |
| No data | 202 579 (2·1%) | 20 135 (9·4%) | .. | 2727 (1·3%) | .. | 3321 (1·5%) | .. | 14 087 (6·6%) | .. |
| Marital status | |||||||||
| Married | 9 510 128 (98·6%) | 652 621 (6·1%) | 1 (ref) | 71 926 (0·6%) | 1 (ref) | 90 500 (0·8%) | 1 (ref) | 490 195 (4·6%) | 1 (ref) |
| Single, widowed, or divorced | 133 655 (1·4%) | 12 403 (8·3%) | 1·40 (1·24–1·57) | 1727 (1·1%) | 1·77 (1·45–2·17) | 2024 (1·3%) | 1·64 (1·41–1·90) | 8652 (5·9%) | 1·30 (1·18–1·44) |
| No data | 1863 (<0·1%) | 220 (11·6%) | .. | 28 (1·5%) | .. | 27 (1·4%) | .. | 165 (8·7%) | .. |
| Maternal age (years) | |||||||||
| <20 | 238 885 (2·5%) | 19 632 (7·1%) | 1·39 (1·30–1·48) | 2564 (0·9%) | 1·74 (1·53–1·99) | 3321 (1·1%) | 1·76 (1·57–1·98) | 13 747 (5·1%) | 1·29 (1·22–1·36) |
| 20–24 | 1 852 590 (19·2%) | 109 197 (5·1%) | 0·97 (0·93–1·00) | 11 491 (0·5%) | 0·97 (0·91–1·04) | 15 617 (0·7%) | 1·02 (0·96–1·08) | 82 089 (3·9%) | 0·96 (0·93–0·98) |
| 25–29 | 3 932 312 (40·8%) | 230 965 (5·2%) | 1 (ref) | 23 887 (0·5%) | 1 (ref) | 30 709 (0·7%) | 1 (ref) | 176 369 (4·1%) | 1 (ref) |
| 30–34 | 2 275 671 (23·6%) | 169 005 (6·7%) | 1·30 (1·27–1·33) | 18 761 (0·7%) | 1·41 (1·35–1·46) | 22 969 (0·9%) | 1·35 (1·30–1·39) | 127 275 (5·1%) | 1·28 (1·26–1·30) |
| 35–39 | 872 465 (9·1%) | 84 908 (8·8%) | 1·74 (1·69–1·79) | 10 224 (1·0%) | 2·05 (1·94–2·16) | 12 004 (1·2%) | 1·88 (1·81–1·95) | 62 680 (6·6%) | 1·68 (1·64–1·72) |
| 40–44 | 188 472 (2·0%) | 22 243 (10·7%) | 2·16 (2·08–2·24) | 2694 (1·2%) | 2·51 (2·33–2·69) | 3284 (1·5%) | 2·41 (2·27–2·57) | 16 265 (8·0%) | 2·07 (2·00–2·14) |
| 45–49 | 12 165 (0·1%) | 1681 (12·1%) | 2·49 (2·22–2·79) | 196 (1·3%) | 2·74 (2·29–3·27) | 257 (1·7%) | 2·79 (2·36–3·31) | 1228 (9·1%) | 2·41 (2·12–2·74) |
| No data | 273 086 (2·8%) | 27613 (9·0%) | .. | 3864 (1·2%) | .. | 4390 (1·4%) | .. | 19 359 (6·4%) | .. |
| Antenatal visits | |||||||||
| None | 118 561 (1·2%) | 15 947 (11·3%) | 1·87 (1·45–2·40) | 2787 (1·9%) | 2·84 (2·03–3·97) | 3071 (2·1%) | 2·52 (1·86–3·42) | 10 089 (7·3%) | 1·60 (1·29–2·00) |
| 1–3 | 636 518 (6·6%) | 65 424 (8·8%) | 1·43 (1·27–1·60) | 10 814 (1·4%) | 2·00 (1·71–2·35) | 11 140 (1·4%) | 1·68 (1·45–1·95) | 43 470 (6·0%) | 1·29 (1·17–1·43) |
| 4–6 | 280 6087 (29·1%) | 211 964 (6·4%) | 1 (ref) | 26 209 (0·7%) | 1 (ref) | 31 741 (0·9%) | 1 (ref) | 154 014 (4·8%) | 1 (ref) |
| 7–9 | 2 911 415 (30·2%) | 196 907 (5·9%) | 0·93 (0·85–1·01) | 16 215 (0·5%) | 0·64 (0·55–0·74) | 23 494 (0·7%) | 0·76 (0·67–0·85) | 157 198 (4·8%) | 1·00 (0·92–1·09) |
| ≥10 | 2 898 681 (30·1%) | 138 095 (4·4%) | 0·67 (0·56–0·81) | 12 098 (0·4%) | 0·51 (0·36–0·73) | 16 306 (0·5%) | 0·56 (0·42–0·75) | 109 691 (3·5%) | 0·72 (0·61–0·83) |
| No data | 274 384 (2·8%) | 36 907 (12·5%) | .. | 5558 (1·9%) | .. | 6799 (2·2%) | .. | 24 550 (8·4%) | .. |
| Parity | |||||||||
| Primiparous | 544 0535 (56·4%) | 357 275 (5·9%) | 1 (ref) | 37 851 (0·6%) | 1 (ref) | 48 866 (0·8%) | 1 (ref) | 270 558 (4·5%) | 1 (ref) |
| Multiparous | 4 194 100 (43·5%) | 305 036 (6·3%) | 1·08 (1·03–1·12) | 35 145 (0·7%) | 1·15 (1·06–1·25) | 43 086 (0·8%) | 1·10 (1·01–1·19) | 226 805 (4·8%) | 1·06 (1·03–1·10) |
| No data | 11 011 (0·1%) | 2933 (25·3%) | .. | 685 (5·9%) | .. | 599 (5·2%) | .. | 1649 (14·2%) | .. |
| Type of pregnancy | |||||||||
| Singleton | 9 474 961 (98·2%) | 575 762 (5·4%) | 1 (ref) | 64 058 (0·6%) | 1 (ref) | 78 953 (0·7%) | 1 (ref) | 432 751 (4·1%) | 1 (ref) |
| Multiple | 170 547 (1·8%) | 89 439 (49·4%) | 17·07 (16·09–18·12) | 9606 (5·1%) | 16·79 (15·86–17·78) | 13 588 (7·2%) | 19·35 (18·18–20·59) | 66 245 (37·1%) | 16·73 (15·71–17·81) |
| No data | 138 (<0·1%) | 43 (31·5%) | .. | 17 (12·8%) | .. | 10 (7·4%) | .. | 16 (11·3%) | .. |
| Mode of delivery | |||||||||
| Vaginal | 5 292 002 (54·9%) | 292 507 (5·0%) | 1 (ref) | 38 668 (0·6%) | 1 (ref) | 40 511 (0·7%) | 1 (ref) | 213 328 (3·8%) | 1 (ref) |
| Caesarean | 435 1440 (45·1%) | 372 309 (7·4%) | 1·51 (1·40–1·63) | 34 838 (0·7%) | 1·09 (0·95–1·26) | 51 969 (1·0%) | 1·52 (1·35–1·70) | 285 502 (5·8%) | 1·58 (1·48–1·69) |
| No data | 2204 (<0·1%) | 428 (19·3%) | .. | 175 (8·1%) | .. | 71 (3·3%) | .. | 182 (8·0%) | .. |
| Maternal complications | |||||||||
| Antepartum complications | 1 899 073 (19·7%) | 309 499 (14·6%) | 4·16 (3·92–4·40) | 38 280 (1·7%) | 5·04 (4·54–5·60) | 48 394 (2·2%) | 5·18 (4·68–5·74) | 222 825 (10·8%) | 3·89 (3·71–4·09) |
| Medical disease | 694 116 (7·2%) | 46 862 (6·3%) | 1·63 (1·53–1·74) | 4108 (0·5%) | 1·44 (1·32–1·58) | 5771 (0·8%) | 1·63 (1·48–1·80) | 36 983 (5·0%) | 1·65 (1·56–1·75) |
| None of the above | 7 052 457 (73·1%) | 308 883 (4·0%) | 1 (ref) | 31 293 (0·4%) | 1 (ref) | 38 386 (0·5%) | 1 (ref) | 239 204 (3·1%) | 1 (ref) |
Data are n (%) unless otherwise stated. Very preterm babies were born after 28–31 completed weeks' gestation. Moderate preterm babies were born after 32–33 weeks' gestation. Late preterm babies were born after 34–36 weeks' gestation.
‡Adjusted for the clustering of births within hospitals.
Adjusted for the sampling distribution of the population.
Maternal education, maternal age, marital status, antenatal visits, and multiple pregnancies had significant effects on preterm birth in all groups (table 3). The association between multiple pregnancies and preterm birth was the strongest. In model 2, when compared with singleton pregnancies, multiple pregnancies were about 15·5 times more likely to result in preterm birth in all preterm pregnancies (table 3). Maternal age was the second most important risk factor. Women aged 40–44 years and 45–49 years were approximately 1·8 times more likely to have a preterm birth than women aged 25–29 years, and the risk was similar for all preterm groups (table 3). Mothers who were illiterate were most likely to have a moderate preterm birth and those with college education or higher were more likely to have a very preterm birth (table 3). The risk for preterm birth was also associated with single marital status; the risk was highest in the very preterm subgroup.
Table 3.
Association between maternal sociodemographic and obstetric characteristics and preterm birth according to gestational age in all pregnancies in China, 2012–18
|
Model 1 (adjusted odds ratio)*† |
Model 2 (adjusted odds ratio)*†‡ | |||||||
|---|---|---|---|---|---|---|---|---|
| All preterm | Very preterm | Moderate preterm | Late preterm | All preterm | Very preterm | Moderate preterm | Late preterm | |
| Region | ||||||||
| East | 1·28 (1·07-1·53) | 1·34 (0·93–1·93) | 1·31 (0·96–1·81) | 1·26 (1·10–1·45) | 1·23 (1·02–1·47) | 1·27 (0·88–1·83) | 1·25 (0·91–1·72) | 1·22 (1·06–1·40) |
| Central | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| West | 1·15 (0·99–1·33) | 1·07 (0·82–1·40) | 1·14 (0·90–1·44) | 1·16 (1·02–1·31) | 1·11 (0·96–1·29) | 1·03 (0·78–1·34) | 1·09 (0·86–1·39) | 1·13 (1·00–1·28) |
| Maternal education | ||||||||
| Illiterate | 1·50 (1·27–1·79) | 1·88 (1·49–2·37) | 2·03 (1·64–2·52) | 1·37 (1·17–1·61) | 1·43 (1·22–1·68) | 1·78 (1·43–2·21) | 1·92 (1·57–2·35) | 1·31 (1·13–1·52) |
| Primary school | 1·21 (1·13–1·30) | 1·44 (1·28–1·62) | 1·40 (1·26–1·56) | 1·15 (1·08–1·23) | 1·15 (1·08–1·23) | 1·37 (1·23–1·52) | 1·32 (1·20–1·46) | 1·10 (1·04–1·17) |
| Middle school | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| High school | 1·35 (1·25–1·46) | 1·67 (1·45–1·91) | 1·57 (1·39–1·78) | 1·29 (1·21–1·37) | 1·36 (1·26–1·46) | 1·69 (1·48–1·93) | 1·59 (1·41–1·78) | 1·29 (1·21–1·37) |
| College or higher | 1·56 (1·43–1·71) | 2·19 (1·85–2·61) | 1·93 (1·68–2·23) | 1·45 (1·35–1·56) | 1·53 (1·40–1·68) | 2·16 (1·82–2·56) | 1·90 (1·65–2·18) | 1·42 (1·32–1·53) |
| Marital status | ||||||||
| Married | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Single, widowed, or divorced | 1·30 (1·14–1·49) | 1·49 (1·18–1·88) | 1·38 (1·16–1·64) | 1·26 (1·12–1·42) | 1·28 (1·11–1·48) | 1·46 (1·15–1·87) | 1·35 (1·13–1·63) | 1·24 (1·09–1·41) |
| Maternal age (years) | ||||||||
| <20 | 1·32 (1·25–1·40) | 1·55 (1·39–1·72) | 1·65 (1·50–1·82) | 1·25 (1·19–1·31) | 1·46 (1·38–1·54) | 1·73 (1·56–1·93) | 1·86 (1·68–2·05) | 1·37 (1·30–1·44) |
| 20–24 | 0·98 (0·95–1·00) | 0·96 (0·91–1·02) | 1·03 (0·98–1·08) | 0·97 (0·95–0·99) | 1·02 (0·99–1·05) | 1·02 (0·96–1·08) | 1·09 (1·03–1·14) | 1·01 (0·99–1·04) |
| 25–29 | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| 30–34 | 1·28 (1·25–1·31) | 1·39 (1·33–1·47) | 1·33 (1·28–1·39) | 1·26 (1·24–1·29) | 1·22 (1·19–1·25) | 1·32 (1·25–1·40) | 1·26 (1·20–1·32) | 1·21 (1·18–1·23) |
| 35–39 | 1·75 (1·70–1·81) | 2·05 (1·92–2·20) | 1·88 (1·78–1·98) | 1·70 (1·65–1·75) | 1·55 (1·49–1·61) | 1·79 (1·66–1·92) | 1·63 (1·53–1·74) | 1·51 (1·46–1·55) |
| 40–44 | 2·24 (2·14–2·34) | 2·53 (2·31–2·77) | 2·47 (2·29–2·66) | 2·17 (2·09–2·25) | 1·84 (1·76–1·93) | 2·03 (1·84–2·23) | 1·97 (1·81–2·14) | 1·80 (1·73–1·88) |
| 45–49 | 2·31 (2·11–2·52) | 2·37 (1·96–2·88) | 2·41 (2·04–2·84) | 2·29 (2·07–2·52) | 1·87 (1·71–2·06) | 1·87 (1·55–2·26) | 1·89 (1·59–2·25) | 1·87 (1·69–2·08) |
| Antenatal visits | ||||||||
| None | 1·80 (1·48–2·19) | 2·72 (2·07–3·55) | 2·44 (1·92–3·10) | 1·55 (1·31–1·85) | 1·78 (1·47–2·16) | 2·71 (2·08–3·52) | 2·43 (1·91–3·07) | 1·54 (1·30–1·83) |
| 1–3 | 1·44 (1·30–1·59) | 2·04 (1·77–2·35) | 1·71 (1·49–1·96) | 1·31 (1·20–1·43) | 1·40 (1·27–1·54) | 1·99 (1·73–2·28) | 1·66 (1·46–1·90) | 1·27 (1·17–1·39) |
| 4–6 | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| 7–9 | 0·80 (0·73–0·87) | 0·52 (0·45–0·60) | 0·64 (0·56–0·72) | 0·87 (0·80–0·95) | 0·76 (0·69–0·83) | 0·49 (0·42–0·57) | 0·60 (0·53–0·67) | 0·83 (0·76–0·90) |
| ≥10 | 0·50 (0·43–0·59) | 0·33 (0·24–0·46) | 0·39 (0·30–0·51) | 0·55 (0·48–0·63) | 0·47 (0·40–0·54) | 0·31 (0·23–0·42) | 0·36 (0·28–0·47) | 0·51 (0·45–0·58) |
| Parity | ||||||||
| Primiparous | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Multiparous | 0·96 (0·91–1·00) | 0·97 (0·88–1·07) | 0·97 (0·89–1·06) | 0·95 (0·92–0·99) | 1·07 (1·01–1·13) | 1·10 (0·99–1·23) | 1·10 (0·99–1·22) | 1·05 (1·01–1·10) |
| Type of pregnancy | ||||||||
| Singleton | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Multiple | 17·56 (16·54–18·64) | 17·82 (16·79–18·91) | 20·56 (19·24–21·97) | 17·07 (16·03–18·17) | 15·51 (14·44–16·67) | 15·48 (14·46–16·58) | 17·81 (16·54–19·18) | 15·17 (14·08–16·34) |
| Maternal complications | ||||||||
| Antepartum complications | .. | .. | .. | .. | 3·91 (3·66–4·17) | 4·80 (4·26–5·41) | 4·88 (4·32–5·51) | 3·67 (3·47–3·87) |
| Medical disease | .. | .. | .. | .. | 1·57 (1·47–1·68) | 1·47 (1·31–1·65) | 1·63 (1·44–1·84) | 1·58 (1·49–1·67) |
| None of the above | .. | .. | .. | .. | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
Data are odds ratio (95% CI). Very preterm babies were born after 28–31 completed weeks' gestation. Moderate preterm babies were born after 32–33 weeks' gestation. Late preterm babies were born after 34–36 weeks' gestation.
Adjusted for the sampling distribution of the population.
Adjusted for the clustering of births within hospitals and maternal sociodemographic characteristics (region, maternal education, maternal age, marital status, antenatal visits, parity, and type of pregnancy).
Adjusted for maternal complications.
An increased number of maternal antenatal visits was associated with a lower risk of preterm birth. Compared with women with four to six antenatal visits, women with ten or more visits had a 53% decrease in the risk of preterm birth (adjusted OR 0·47 [95% CI 0·40–0·54]). Women with seven to nine visits had a 24% decrease in the risk of preterm birth (adjusted OR 0·76 [0·69–0·83]; table 3). The magnitude of effect was strongest in the very preterm and moderate preterm subgroups.
After adjusting for maternal sociodemographic characteristics, women with antepartum complications were approximately four times more likely to have a preterm birth than those with no maternal complications (adjusted OR 3·91 [95% CI 3·66–4·17]; table 3), and the risk was highest in the very preterm and moderate preterm subgroups. Women diagnosed with medical diseases were 1·6 times more likely to have a preterm birth (adjusted OR 1·57 [1·47–1·68]), and the risk was highest in the moderate preterm and late preterm subgroups (table 3).
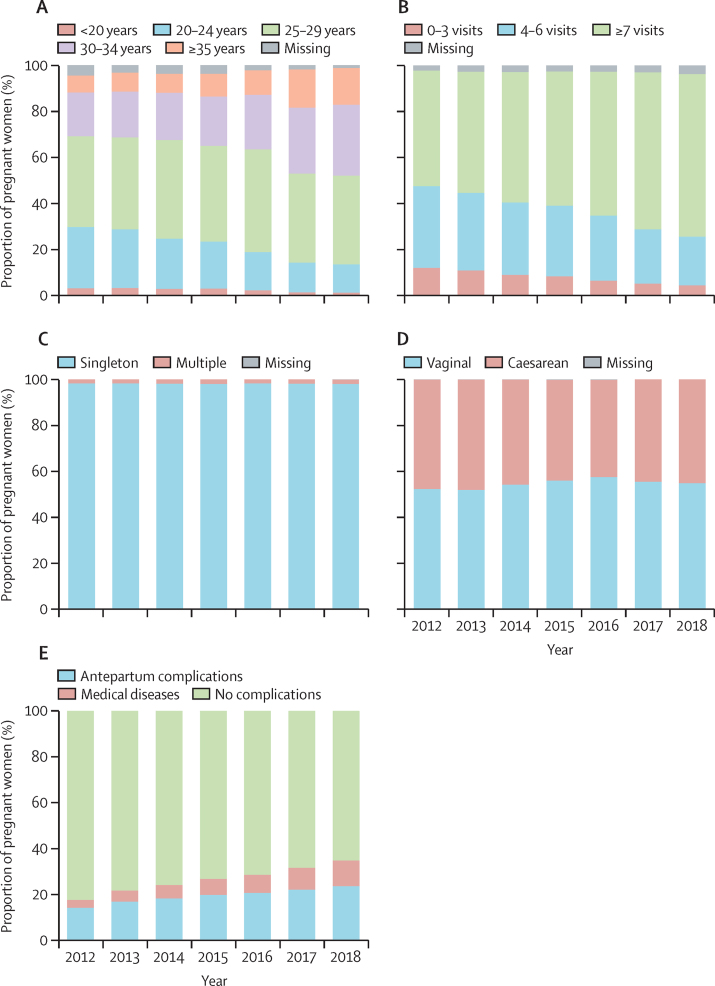
Overall, 1 073 102 (11·1%) of 9 645 646 women gave birth at 35 years of age or older, increasing to more than 15% in 2017 and 2018 (table 2; appendix 2 pp 11–13). More than half (5 810 096 [60·2%] of 9 645 646; table 2) of all women had seven or more antenatal visits. Nearly half (4 351 440 [45·1%] of 9 645 646; table 2) of all births were by caesarean section, and about a quarter (2 593 189 [26·9%] of 9 645 646; table 2) of all women had had a maternal complication. Attending less than four antenatal care visits was more common in women from west China, in multiparous women, and in mothers who were very young (<20 years) or older (≥35 years), single, and those who had not attended school and those who had completed only primary and middle school (appendix 2 p 25). When compared with women who gave birth in 2012, those who gave birth in 2018 were more likely to be 35 years old or older (7·4% in 2012 vs 15·9% in 2018), have a multiple pregnancy (1·6% vs 1·9%), attended seven or more antenatal visits (50·2% vs 70·7%), antepartum complications (14·4% vs 23·8%), and medical diseases (3·5% vs 11·2%), but they were less likely to have a caesarean section (47·5% vs 45·0%; figure 1; appendix 2 pp 11–13). Furthermore, the number of women who attended no to three antenatal visits decreased by 64% from 2012 to 2018, and women who attended four to six antenatal visits decreased by 40% (appendix 2 pp 11–13). Similar changing patterns were noted in primiparous women. Multiparous women who gave birth in 2018 were less likely to have multiples, but they were more likely to have a caesarean (appendix 2 pp 11–13).
Figure 1.
Changes factors associated with preterm birth in all pregnancies in China, 2012–18
Maternal age (A), number of antenatal visits (B), type of pregnancy (C), type of birth (D), and maternal complications (medical disease; eg, heart disease, embolism or thrombophlebitis, hepatic disease, severe anaemia [haemoglobin concentration of <70 g/L], renal disease [including urinary tract infection], lung disease [including upper respiratory tract infection], HIV/AIDS, connective tissue disorders, gestational diabetes, and cancer; E).
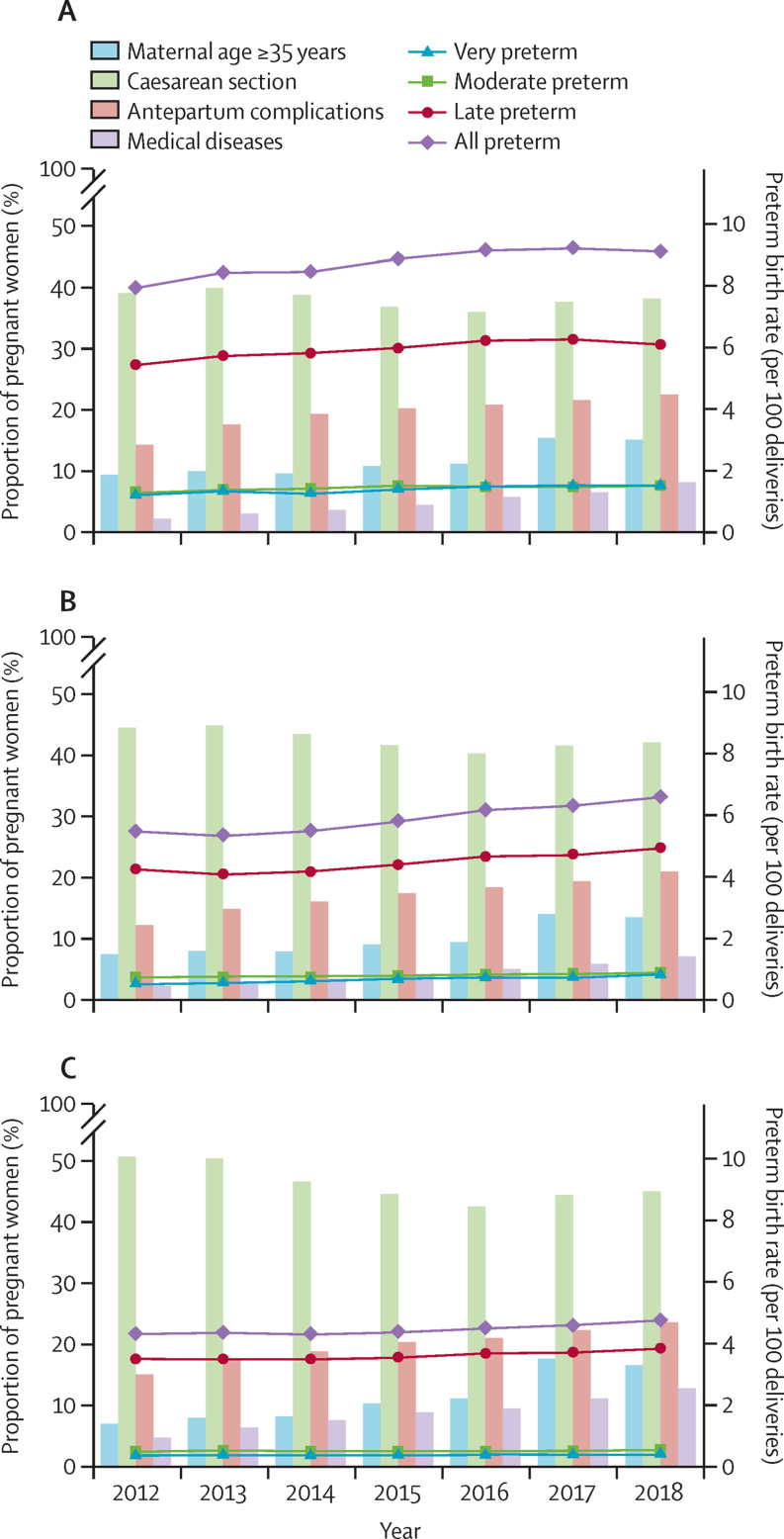
Changes in preterm birth rate and the proportions of women with singleton pregnancies who were 35 years or older, who had had a caesarean, and those with maternal complications varied according to the frequency of antenatal visits during the study period (figure 2; appendix 2 pp 14–19). There were higher increases between 2012 and 2018 in the rates of preterm birth in the very preterm, moderate preterm, and late preterm subgroups in women with 0–3 antenatal visits (26·9% for the very preterm group, 15·4% for the moderate preterm group, and 12.0% for the late preterm group; p<0·0001) and women with 4–6 antenatal visits (54·9% for the very preterm group, 20·8% for the moderate preterm group, and 16·4% for the late preterm group; p<0·0001; appendix 2 pp 14–15). The increases in women who attended seven or more antenatal visits were smaller but still statistically significant (14·7% for the very preterm group, 10·4% for the moderate preterm group, and 10·1% for the late preterm group; p<0·0001; appendix 2 pp 14–15). Over the same study period, the proportions of women with any frequency of antenatal visits who were 35 years old or older had significantly increased (61·4% had no to three antenatal visits, 82·1% had four to six visits, and 138·5% had seven or more visits; p<0·0001; appendix 2 pp 14–15), but the biggest increase was reported in women with seven or more antenatal visits.
Figure 2.
Changes in preterm birth rate, advanced maternal age , and obstetric factors associated with preterm birth according to frequency of antenatal visits in singleton pregnancies in China, 2012–18
(A) No to three antenatal care visits. (B) four to six antenatal care visits. (C) seven or more antenatal care visits. Very preterm births were during 28–31 weeks’ gestation. Moderate preterm were during 32–33 weeks’ gestation. Late preterm were during 34–36 weeks’ gestation. Preterm birth rate was adjusted according to the sampling distribution of the population.
The proportions of women with antepartum complications and those with medical diseases had significant increases, despite the increasing frequency of antenatal visits (appendix 2 pp 14–15). Women with medical diseases were more likely to have seven or more antenatal visits. Women who had a caesarean had significantly decreased, regardless of the frequency of antenatal visits (–2·2% for those who attended no to three antenatal visits, –5·4% for those who attended four to six antenatal visits, and –11·3% for those who attended seven or more antenatal visits; p<0·0001; appendix 2 pp 14–15); the largest decrease was seen in women with seven or more antenatal visits. Similar pattern changes were observed in primiparous and multiparous women with singleton pregnancies. In multiparous women, a decrease in caesarean section rates was only observed with seven or more antenatal visits (appendix 2 pp 16–19).
In women with singleton pregnancies who were between 25 and 29 years and had antepartum complications, there were bigger decreases in the rates of preterm birth in the moderate preterm group (–16·5%; p<0·0001) and late preterm group (–8·1%; p<0·0001), except for the very preterm subgroup (–4·0%; p=0·02) between 2012 and 2018, when a significant decrease in caesarean rates was only observed between 34–36 weeks of gestation (–9·2%, p<0·0001; table 4). By comparison, there was no significant decrease in caesarean rate between 32–33 weeks of gestation (–2·1%, p=0·12), whereas the caesarean rate between 28–31 weeks of gestation increased significantly (9·8%, p=0·02; table 4). Similar findings were observed for women with medical diseases, although the decrease in caesarean rate between 34–36 weeks of gestation was small (–4·7%; p=0·02; table 4). When stratified by primiparous and multiparous, similar patterns were shown between late preterm birth and caesarean section (appendix 2 pp 20–23).
Table 4.
Changes in preterm birth rates and gestational-age-specific caesarean section rates stratified by obstetric complications in singleton pregnancies in women aged 25–29 years in China, 2012–18
|
Year |
Change 2012–18 | p value for trend | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | ||||
| Antepartum complications (n=733 504) | ||||||||||
| Number of births | 70 339 | 81 503 | 10 8380 | 99 864 | 13 1833 | 12 3135 | 11 8450 | 68·4 | .. | |
| Caesarean section rate (per 100 deliveries) | ||||||||||
| 28–31 weeks | 57·0% | 59·3% | 57·6% | 54·4% | 57·3% | 59·0% | 62·6% | 9·8 | 0·02 | |
| 32–33 weeks | 66·2% | 67·3% | 64·8% | 66·0% | 66·2% | 65·7% | 64·8% | −2·1 | 0·12 | |
| 34–36 weeks | 63·7% | 63·9% | 60·1% | 58·3% | 57·0% | 58·0% | 57·8% | −9·2 | <0·0001 | |
| ≥37 weeks | 64·9% | 62·9% | 57·1% | 53·5% | 50·1% | 48·9% | 48·3% | −25·2 | <0·0001 | |
| Preterm birth rate (per 100 deliveries)* | ||||||||||
| Very preterm | 1·3% | 1·3% | 1·2% | 1·2% | 1·2% | 1·1% | 1·2% | −4·0 | 0·05 | |
| Moderate preterm | 1·8% | 1·6% | 1·6% | 1·5% | 1·5% | 1·5% | 1·5% | −16·5 | <0·0001 | |
| Late preterm | 9·1% | 8·5% | 8·5% | 8·3% | 8·5% | 8·3% | 8·3% | −8·1 | <0·0001 | |
| All preterm | 12·1% | 11·4% | 11·3% | 11·0% | 11·1% | 10·9% | 11·0% | −8·9 | <0·0001 | |
| Medical diseases (n=253 933) | ||||||||||
| Number of births | 17 535 | 23 552 | 34 780 | 34 414 | 46 966 | 46 807 | 49 879 | 184·5 | .. | |
| Caesarean section rate (per 100 deliveries) | ||||||||||
| 28–31 weeks | 28·1% | 47·5% | 38·0% | 34·9% | 28·9% | 36·5% | 46·5% | 65·9 | 0·10 | |
| 32–33 weeks | 51·2% | 54·0% | 47·6% | 51·5% | 47·8% | 52·5% | 53·2% | 3·9 | 0·35 | |
| 34–36 weeks | 63·1% | 61·7% | 59·0% | 56·7% | 56·0% | 57·9% | 60·1% | −4·7 | 0·02 | |
| ≥37 weeks | 56·9% | 53·5% | 48·7% | 45·4% | 42·5% | 42·2% | 56·9% | −28·2 | <.0001 | |
| Preterm birth rate (per 100 deliveries)* | ||||||||||
| Very preterm | 0·4% | 0·4% | 0·4% | 0·4% | 0·4% | 0·4% | 0·4% | −20·5 | 0·24 | |
| Moderate preterm | 0·7% | 0·7% | 0·6% | 0·6% | 0·5% | 0·5% | 0·6% | −14·9 | 0·002 | |
| Late preterm | 4·9% | 4·4% | 3·8% | 3·8% | 3·7% | 3·5% | 3·6% | −27·3 | <0·0001 | |
| All preterm | 6·0% | 5·4% | 4·7% | 4·8% | 4·6% | 4·3% | 4·5% | −25·5 | <0·0001 | |
Very preterm babies were born after 28–31 completed weeks' gestation. Moderate preterm babies were born after 32–33 weeks' gestation. Late preterm babies were born after 34–36 weeks' gestation.
Adjusted for the sampling distribution of the population.
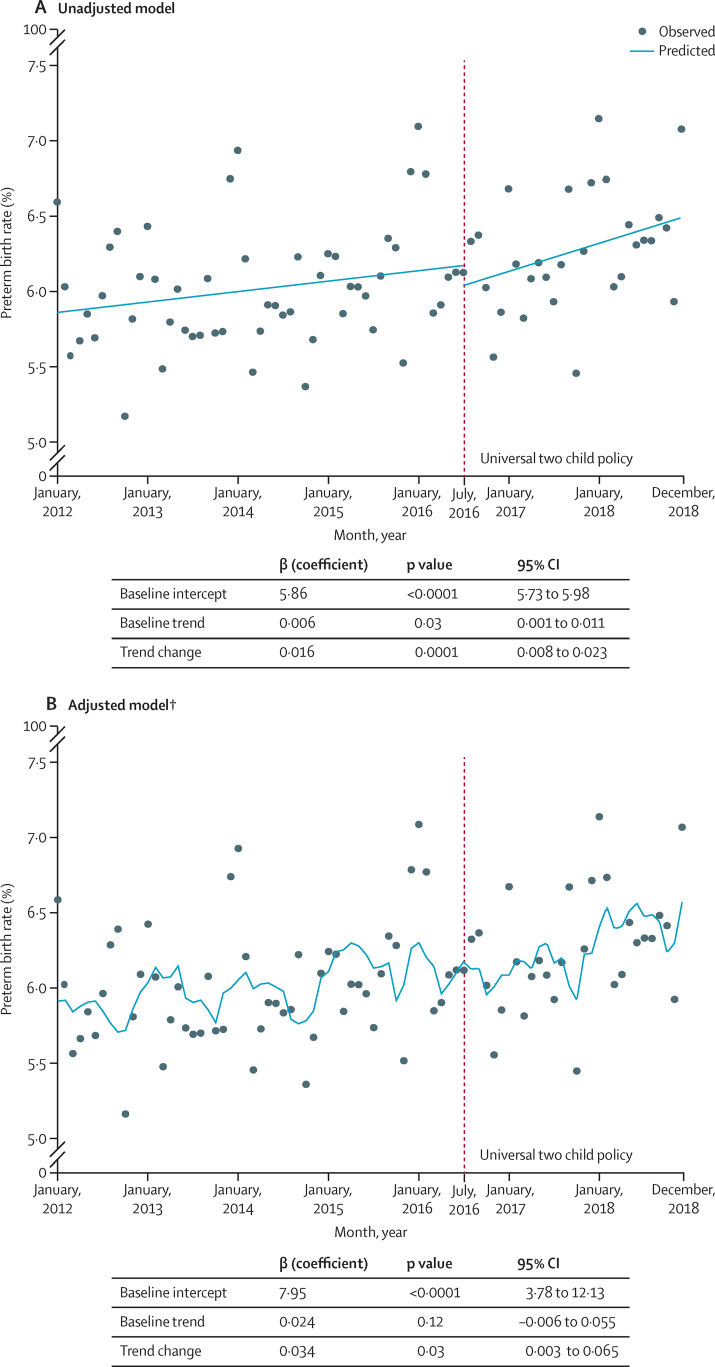
Through interrupted time series analysis, we observed that the preterm birth rate increased slightly before the universal two child policy took effect (between January, 2012 and June, 2016; β=0·006; p=0·03; figure 3); a higher increase was observed during the effective period (β=0·016; p=0·0001). After adjusting for confounding factors, the increasing preterm birth rate during the effective period remained significant (β=0·034; p=0·03; figure 3).
Figure 3.
Estimated change in rate of preterm birth in all pregnancies following the introduction of the universal two child policy based on interrupted time series analysis
(A) Crude change in preterm birth rate. (B) Change in preterm birth rate after adjusting for confounding factors. *The change in preterm birth rate during the effective period (July, 2016, to December, 2018). Baseline January, 2012, to June, 2016. †Model was adjusted for advanced maternal age (≥35 years), antenatal visits, and multiple pregnancies.
Discussion
This is the first in-depth study to describe the rates of liveborn preterm births by gestational age and temporal trends using the largest and most updated dataset in China. We found a slight increase in preterm births for both singleton and multiple pregnancies between 2012 and 2018. These increases were mainly due to an increase in the number of singletons born between 28 and 31 weeks’ gestation (very preterm) and multiples born after 34–36 weeks’ gestation (late preterm). This might have been driven partly by an increase in maternal age at delivery, the proportion of mothers with complications, in the number of multiple pregnancies, and the implementation of the universal two child policy. Nevertheless, a reduction in caesarean sections and an increase in antenatal visits might have mitigated the increasing trend in preterm births.
An accurate estimation of the preterm birth rate depends on the method used to assess gestational age, the definition of fetal viability, and the data collection method. Accurate estimation of preterm birth remains a major challenge, particularly in low-income and middle-income countries. Modelled predictions have often been used as reports of the national preterm birth rate Asian (including China) and African countries, in which data on preterm birth are not available in a national civil registration, vital statistics, or population-representative surveys.1, 6 Our study was based on a large-scale and standardised nationwide monitoring system that was used to directly report the liveborn preterm birth rate in pregnancies from China. Although this system was facility based, we selected different levels of hospitals proportionately across regions; the monitored birth population included approximately 10% of all births annually in China (in which the proportion of hospital delivery was nearly 100%). Our method might provide a representative sample for estimating current preterm birth rates. The rate of overall preterm birth reported in our study (6·1% for all pregnancies) was slightly lower than the rate (6·9% for all livebirths) estimated for China at a national level in a 2014 modelling study;1 our findings were similar to the 2010 live singleton preterm birth rates reported in most European countries, such as France (5·5%), Italy (5·7%), the Netherlands (5·9%), Switzerland (5·2%), and England and Wales (5·6%).23 Our preterm birth rate was lower than that reported in south Asia (>10%),1 north Africa (13·4%),1 and North America (11·2%).1 We also reported the weighted rates of very preterm (0·6%), moderate preterm (0·8%), and late preterm births (4·7%); late preterm births accounted for most (75·0%) preterm births, which is in line with reports from those European countries.24, 25 Our system oversampled high-level referral hospitals in urban areas (in which the preterm birth rate was higher due to a higher proportion of pregnant women at high risk than in low-level hospitals); we weighed the preterm birth rate by the population distribution in urban and rural areas in each region. However, whether this fully adjusted for the oversampling of high-level hospitals remains unclear.
The low preterm birth rate in pregnant women might have benefited from health care reform over the past decade in China. To achieve universal health coverage, China launched a major health care reform plan in 2009 that pledged to provide all citizens with equal access to basic health care with reasonable quality (including basic public health service and basic medical service) and sufficient financial risk protection by 2020.26 The National Basic Public Health Service programme, which includes maternal health management, was implemented in July, 2009, to provide free basic public health services to all urban and rural residents. Strategies for strengthening pregnancy health management—such as pregnancy health education, maternal exercise, nutritional and psychological guidance, maternal and fetal physical examinations and health evaluations, and referral of women at high risk of pregnancy to at least five antenatal visits—might improve maternal and neonatal outcomes. For example, maternal mortality declined from 59 per 100 000 livebirths to 29 per 100 000 livebirths, the mortality rate in children younger than 5 years declined from 36·8 per 1000 livebirths to 9·3 per 1000 livebirths, and neonatal mortality declined from 21·4 per 1000 livebirths to 4·7 per 1000 livebirths between 2000 and 2017.26, 27 The national guidelines on preterm birth clinical practice, issued in 2015, highlighted the definition of women at high risk of preterm birth and prevention strategies, including recommendations for progesterone, and might have contributed to the improvement of maternal and neonatal health status.28
Our findings show that there was a slight increase in preterm births for both singleton and multiple pregnancies from 2012 to 2018 in China. A prominent increase occurred in very preterm singletons and late preterm multiples. By comparison, a study of 19 European countries found that between 1996 and 2008 approximately half of the countries had no change or a decrease in preterm singleton births, whereas most countries reported significant increases for multiple births.29 A study from six high-income countries revealed a favourable trend between 2006 and 2014: late preterm singleton livebirths from the USA and Norway significantly decreased.9 Such a declining trend might have been primarily driven by a significant decrease in spontaneous preterm birth.24, 30
At least three factors might have contributed to this overall rise in preterm birth in China: (1) advanced maternal age is a significant risk factor for preterm birth, as shown by our study. In addition, we found that the overall proportion of older mothers (≥35 years) was as high as 10% (increasing to more than 15% in 2017 and 2018; appendix 2 pp 11–13), which is similar to several reports.16, 30 Furthermore, our findings show an approximately 114% increase in older mothers (appendix 2 pp 11–13), which is similar to that reported in a study of south Australia, in which the preterm birth rate increased by 40% from 1986 to 2014.31 By contrast, a smaller change in older mothers was reported in the USA from 2005 to 2012, where there was a significant decrease in preterm birth.30 (2) 26·9% of women had antepartum complications or medical diseases in the Chinese population, which is similar to the estimates in a Scottish study.25 We found that common complications were gestational diabetes, polyhydramnios or oligohydramnios, and pre-eclampsia. These diseases were associated with an increased risk of preterm birth; however, this effect depends on disease severity.32, 33, 34 In our population, from 2012 to 2018, the proportion of women with antepartum complications increased by 66%; the proportion of women with medical diseases increased from 3·5% in 2012 to 11·2% in 2018. This suggests that both increases might have played a role in increasing preterm birth over the study period. (3) Multiple pregnancies are also an important risk factor for preterm birth. Previous studies have shown that the rise in preterm birth is accompanied by an increase in multiple births.5, 11 The proportion of multiple births increased significantly from 1·6% in 2012 to 1·9% in 2018 in our study (appendix 2 pp 11–13), which might have been due to the increased use of assisted reproduction in China.35
The universal two child policy might have been an important contributor to the increase in preterm births since its implementation on Oct 29, 2015. Evidence that suggests an increase in advanced maternal age and pregnancy complications (risk factors for preterm birth) occurred after implementation of the policy.16, 36, 37 In our study, we observed visible increases in the proportion of mothers older than 35 years, maternal antepartum complications, and medical diseases during the policy-effective period (particularly between 2017 and 2018). Several studies have found that birth-policy changes elevated the risks of some birth outcomes, such as birth defects.16 However, few have focused on the effect of birth-policy changes on preterm births. A study in China showed that there was no association between the policy change and preterm births.36 This might be because the estimate of preterm birth rate in this study (4·2%) was based on a system that has collected data only since January, 2015.36 This system was not nationally representative as a result of incomplete birth reports and because the observation period for preterm births was only 2 years (Jan 1, 2016, to Dec 31, 2017).36
An unexpected but important finding of this study is that the slight increase in preterm births might be partly because of the reduction in caesareans and the increasing frequency of antenatal visits. Both factors mitigated increasing number of preterm births to some extent, but preventing preterm birth remains a global challenge. We found that decreases in preterm birth rates were accompanied by a decrease in caesareans, particularly for births between 34–36 weeks of gestation, which suggests that changes in caesareans might affect the prevalence of preterm birth. This finding can be shown with the results of previous studies, although they are difficult to interpret. One study from the 2005 WHO global survey on maternal and perinatal health reported that rates of preterm delivery increase as rates of caesarean section increase to between 10% and 20% of births in Latin America.38 Another multi-country analysis reported that caesareans and labour induction accounted for an approximately 20% increase in late preterm birth between 1989 and 2004.39 In China, the rate of caesareans was as high as 50% due to an increase in unnecessary use by health-care providers and maternal requests in the early 2000s.40, 41 However, our data and previous studies show that the rate of caesareans in China has significantly decreased over the past decade.18 We speculated that this declining trend would contribute to the decrease in late preterm births and would then offset the overall increase in preterm births. The Chinese Government recommends five or more antenatal visits in rural areas and eight or more in urban areas, depending on differences in health system development. Antenatal care is provided by specialised health-care workers in primary care institutions and hospitals and often includes health education and guidance, maternal and fetal health assessment, routine biochemical testing and necessary special testing, prevention and treatment for obstetric complications, and continued monitoring and management for women at high risk of pregnancy complications (appendix 2 p 24).42 Antenatal care in primary care institutions is free of charge, and uptake is high.43 We found that a high frequency of antenatal visits significantly reduced the risk of preterm birth. The higher the number of antenatal visits, the lower the preterm birth rate. This effect is mainly a result of better access to antenatal care and regular pregnancy management, suggesting that more women should give birth vaginally or be encouraged to deliver after 37 weeks of gestation, even in the presence of obstetric complications. In our study, between 2012 and 2018, a 41% increase was reported in the proportion of women with seven or more antenatal visits, but a 64% decrease was reported in women who attended no to three antenatal care sessions and a 40% decrease in those who attended four to six antenatal sessions (appendix 2 pp 11–13). These changes might also mitigate the overall increase in preterm births. Additionally, low frequencies of antenatal visits were more common in women in west China, in multiparous women, very young (<20 years) or older (≥35 years) mothers, single mothers, and mothers with lower education levels. Although these percentages were low, more attention should be paid to these populations (appendix 2 p 25).
Data in this study were collected from a large and well established national registry, providing a reliable overview of the prevalence of preterm birth in China. Our study is unique in its sample size and representation because it includes the records of more than 900 million births from different facilities and regions (accounting for approximately 10% of all births annually in mainland China). This allowed us to analyse more subtle changes in preterm birth rates at a national level rather than a smaller sample from a single centre or from local areas. Furthermore, comprehensive data quality control strategies were continually done to ensure data validity, including internal and external data quality control and online data check. All variables had between 0% and 2·8% missing data. However, this is an observational study, and causation cannot be established.
Our study had some limitations. First, livebirth in China is defined as the birth of a fetus with signs of life at or after 28 completed weeks of gestation or at birth weight of 1000 g or more, which conforms to WHO's definition.44 The threshold of gestational age for fetal viability used in our study is higher than that of 23–24 weeks used in most high-income countries. Therefore, caution is needed when making international comparisons using our data. According to the published rate of extremely preterm birth (less than 28 weeks) ranged from 0·2% to 0·4% in high-income countries.10, 11, 24, 25 We acknowledge that extending the gestational age cutoff might have increased the overall preterm birth rates, but this magnitude is assumed to be very small due to a very low rate of extremely preterm birth. If extremely preterm birth was included, our overall preterm birth rates might be slightly higher than estimates in most European countries. Second, early pregnancy ultrasound is considered the gold standard for gestational age measurement. However, we assessed gestational age by the last menstrual period, similar to other low-income and middle-income countries in which medical resources are scarce. Previous studies have shown that dating a pregnancy using the date of the last menstrual period might overestimate gestational age by about 2 days (range 0·2–2·8 days) when compared with ultrasound, and the sensitivity and positive predictive value of the last menstrual period in identifying preterm births were relatively high.45, 46, 47 However, in the absence of early ultrasound, the last menstrual period was deemed to be one of the most reliable clinical measures for gestational age. Although this method might underestimate the preterm birth rate, the effect of underestimation is assumed to be relatively small. For example, Yang and colleagues48 found that the preterm birth rate based on the last menstrual period was underestimated by about 1·5% compared with that based on early ultrasound (7·6% for last menstrual period vs 9·1% for ultrasound). Nonetheless, the measurement of gestational age by early ultrasound is recommended. Third, understanding the preterm birth rate by delivery mode (spontaneous vs health-care provider-initiated) is of value for guiding research on causes and determinants and for implementing and monitoring prevention strategies. However, in our study, we were unable to separate spontaneous preterm births from those in which labour was induced because the NMNMSS simply classified the mode of delivery into two subgroups: vaginal or caesarean delivery. Therefore, we were unable to analyse the preterm birth rate as spontaneous versus provider-initiated due to an absence of data. Finally, some important risk factors—such as the use of assisted reproductive technology, a history of preterm birth, interpregnancy interval, nutritional status, and fetal complications—might be associated with preterm birth. However, the NMNMSS was designed to investigate maternal deaths and near misses rather than preterm births, so the potential factors for preterm birth that we collected were incomplete. However, we could not rule out all residual confounding factors; we included all existing covariates in our analysis, considering some variables as a proxy for confounding (eg, region and maternal education). Incomplete adjustment might have affected our reported associations. Future analyses should consider the use of these covariates as they become available.
Preterm birth remains a crucial maternal and infant health issue in China because of the large number of babies born prematurely every year and an increase in the overall preterm birth rate. Moreover, preterm birth is the most common cause of neonatal death.49 From the perspectives of society and family loss, the burden of preterm birth in China is substantial. The Chinese Government's strategic investments in maternal and neonatal health have partly contributed to the prevention of preterm birth. However, because of the rapid changes in sociodemographic and obstetric factors associated with preterm birth—such as advanced maternal age, maternal complications, and multiple pregnancies particularly within the context of the universal two child policy—more efforts to avert the rise in preterm birth are urgently needed, including health education and guidance in maternal and newborn care, continued monitoring and management for pregnant women at a high risk of preterm birth, and improvements in the quantity and quality of antenatal visits. Reducing the burden of preterm birth is needed to achieve Sustainable Development Goal 3—ending preventable deaths in neonates and children younger than 5 years by 2030—and to achieve Health China 2030 targets for reducing mortality in children younger than 5. Our findings could be used to inform policies and programmes to ensure more attention is paid to women at the highest risk: those with multiple pregnancies, older (≥35 years) mothers, those with obstetric complications, and those who attend fewer antenatal visits. Our study also shows that strengthening the data monitoring system not only improves the validity of our estimates, but is also useful for national policy making and international exchange. To better contribute to global preterm birth debates, we should take urgent action, particularly to strengthen the quality and volume of data. This can be achieved by standardising definitions, more accurately measuring for gestational age, and more accurately reporting risk factors. With the newly introduced three child policy, preterm birth rate should continue to be monitored and assessed in China.
Data sharing
The data in our study are not publicly available due to the terms of our contract with the Chinese National Health Commission, but are available from the corresponding authors on reasonable request and with permission of the National Health Commission of China.
Declaration of interests
We declare no competing interests.
Acknowledgments
Acknowledgments
This study was supported by the National Key Research and Development Program of China (grant number 2019YFC1005100), the National Health Commission of China, the China Medical Board (grant number 11-065), WHO (grant number CHN-12-MCN-004888), and UNICEF (grant number 2016EJH016). We would like to thank the facilities and staff of the National Maternal Near Miss Surveillance System for the data collection, reports, and review.
Contributors
KD, JL, JZ, and HL designed the study. KD did the statistical analysis with support from YM and XL. YM, ZL, YW, ML, LD, QL, PC, and YX reviewed the data and did the coding. KD and JL wrote the first draft of the Article. KD, JL, JZ, and HL have full access to all the data in the study. All authors critically interpreted the results and developed the report. All authors reviewed and approved the final version.
Contributor Information
Zheng Liu, Email: hanmin@vip.163.com.
Jun Zhu, Email: zhujun028@163.com.
Supplementary Materials
References
- 1.Chawanpaiboon S, Vogel JP, Moller AB. Global, regional, and national estimates of levels of preterm birth in 2014: a systematic review and modelling analysis. Lancet Glob Health. 2019;7:e37–e46. doi: 10.1016/S2214-109X(18)30451-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Moster D, Lie RT, Markestad T. Long-term medical and social consequences of preterm birth. NEJM. 2008;359:262–273. doi: 10.1056/NEJMoa0706475. [DOI] [PubMed] [Google Scholar]
- 3.Saigal S, Doyle LW. An overview of mortality and sequelae of preterm birth from infancy to adulthood. Lancet. 2008;371:261–269. doi: 10.1016/S0140-6736(08)60136-1. [DOI] [PubMed] [Google Scholar]
- 4.Vogel JP, Chawanpaiboon S, Moller AB, Watananirun K, Bonet M, Lumbiganon P. The global epidemiology of preterm birth. Best Pract Res Clin Obstet Gynaecol. 2018;52:3–12. doi: 10.1016/j.bpobgyn.2018.04.003. [DOI] [PubMed] [Google Scholar]
- 5.Goldenberg RL, Culhane JF, Iams JD, Romero R. Epidemiology and causes of preterm birth. Lancet. 2008;371:75–84. doi: 10.1016/S0140-6736(08)60074-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Blencowe H, Cousens S, Oestergaard MZ. National, regional, and worldwide estimates of preterm birth rates in the year 2010 with time trends since 1990 for selected countries: a systematic analysis and implications. Lancet. 2012;379:2162–2172. doi: 10.1016/S0140-6736(12)60820-4. [DOI] [PubMed] [Google Scholar]
- 7.de Mouzon J, Goossens V, Bhattacharya S. Assisted reproductive technology in Europe, 2007: results generated from European registers by ESHRE. Hum Reprodn. 2012;27:954–966. doi: 10.1093/humrep/des023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Blondel B, Kogan MD, Alexander GR. The impact of the increasing number of multiple births on the rates of preterm birth and low birthweight: an international study. American J Pub Health. 2002;92:1323–1330. doi: 10.2105/ajph.92.8.1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Richards JL, Kramer MS, Deb-Rinker P. Temporal trends in late preterm and early term birth rates in 6 high-income countries in North America and Europe and association with clinician-initiated obstetric interventions. JAMA. 2016;316:410–419. doi: 10.1001/jama.2016.9635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tracy SK, Tracy MB, Dean J, Laws P, Sullivan E. Spontaneous preterm birth of liveborn infants in women at low risk in Australia over 10 years: a population-based study. BJOG. 2007;114:731–735. doi: 10.1111/j.1471-0528.2007.01323.x. [DOI] [PubMed] [Google Scholar]
- 11.Keirse MJ, Hanssens M, Devlieger H. Trends in preterm births in Flanders, Belgium, from 1991 to 2002. Paediatr Perinat Epidemiol. 2009;23:522–532. doi: 10.1111/j.1365-3016.2009.01067.x. [DOI] [PubMed] [Google Scholar]
- 12.Miao H, Li B, Li W. Adverse birth outcomes in Guangdong province, China, 2014-2017: a spatiotemporal analysis of 2.9 million births. BMJ Open. 2019;9 doi: 10.1136/bmjopen-2019-030629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zou L, Wang X, Ruan Y, Li G, Chen Y, Zhang W. Preterm birth and neonatal mortality in China in 2011. Int J Gynaecol Obstet. 2014;127:243–247. doi: 10.1016/j.ijgo.2014.06.018. [DOI] [PubMed] [Google Scholar]
- 14.Chen C, Zhang JW, Xia HW. Preterm birth in China between 2015 and 2016. American J Pub Health. 2019;109:1597–1604. doi: 10.2105/AJPH.2019.305287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhu L, Zhang R, Zhang S. Chinese neonatal birth weight curve for different gestational age. Zhonghua Er Ke Za Zhi. 2015;53:97–103. (in Chinese). [PubMed] [Google Scholar]
- 16.Zhang X, Chen L, Wang X. Changes in maternal age and prevalence of congenital anomalies during the enactment of China's universal two-child policy (2013-2017) in Zhejiang province, China: an observational study. PLoS Med. 2020;17 doi: 10.1371/journal.pmed.1003047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhu J, Liang J, Mu Y. Sociodemographic and obstetric characteristics of stillbirths in China: a census of nearly 4 million health facility births between 2012 and 2014. Lancet Glob Health. 2016;4:e109–e118. doi: 10.1016/S2214-109X(15)00271-5. [DOI] [PubMed] [Google Scholar]
- 18.Liang J, Mu Y, Li X. Relaxation of the one child policy and trends in caesarean section rates and birth outcomes in China between 2012 and 2016: observational study of nearly seven million health facility births. BMJ. 2018;360:k817. doi: 10.1136/bmj.k817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang WY. In: Obstetrics and gynecology. 8th edn. Xie X, Gou WL, editors. People's Health Publishing; Beijing: 2013. Antenatal care; p. 142. (in Chinese). [Google Scholar]
- 20.WHO Recommended definitions, terminology and format for statistical tables related to the perinatal period and use of a new certificate for cause of perinatal deaths. Modifications recommended by FIGO as amended October 14, 1976. Acta Obstet Gynecol Scand. 1977;56:247–253. [PubMed] [Google Scholar]
- 21.National Bureau of Statistics of China National data. 2015. http://data.stats.gov.cn/easyquery.htm?cn=E0103
- 22.Chinese Ministry of Health The measures for the administration of the hospital grade. Ministry of Health, China (in Chinese) 1989. https://baike.baidu.com/item/%E5%8C%BB%E9%99%A2%E5%88%86%E7%BA%A7%E7%AE%A1%E7%90%86%E5%8A%9E%E6%B3%95/420525?fr=aladdin
- 23.Delnord M, Mortensen L, Hindori-Mohangoo AD. International variations in the gestational age distribution of births: an ecological study in 34 high-income countries. Eur J Pub Health. 2018;28:303–309. doi: 10.1093/eurpub/ckx131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schaaf JM, Mol BW, Abu-Hanna A, Ravelli AC. Trends in preterm birth: singleton and multiple pregnancies in the Netherlands, 2000–2007. BJOG. 2011;118:1196–1204. doi: 10.1111/j.1471-0528.2011.03010.x. [DOI] [PubMed] [Google Scholar]
- 25.Norman JE, Morris C, Chalmers J. The effect of changing patterns of obstetric care in Scotland (1980–2004) on rates of preterm birth and its neonatal consequences: perinatal database study. PLoS Med. 2009;6 doi: 10.1371/journal.pmed.1000153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yip WC, Hsiao WC, Chen W, Hu S, Ma J, Maynard A. Early appraisal of China's huge and complex health-care reforms. Lancet. 2012;379:833–842. doi: 10.1016/S0140-6736(11)61880-1. [DOI] [PubMed] [Google Scholar]
- 27.Tao W, Zeng Z, Dang H. Towards universal health coverage: achievements and challenges of 10 years of healthcare reform in China. BMJ Glob Health. 2020;5 doi: 10.1136/bmjgh-2019-002087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Obstetrics Subgroup. Chinese Society of Obstetrics Gynecology. Chinese Medical Association Diagnosis and therapy guideline of preterm birth (2014) Zhonghua Fu Chan Ke Za Zhi. 2014;49:481–485. [PubMed] [Google Scholar]
- 29.Zeitlin J, Szamotulska K, Drewniak N. Preterm birth time trends in Europe: a study of 19 countries. BJOG. 2013;120:1356–1365. doi: 10.1111/1471-0528.12281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Gyamfi-Bannerman C, Ananth CV. Trends in spontaneous and indicated preterm delivery among singleton gestations in the United States, 2005–2012. Obstet Gynecol. 2014;124:1069–1074. doi: 10.1097/AOG.0000000000000546. [DOI] [PubMed] [Google Scholar]
- 31.Verburg PE, Dekker GA, Venugopal K. Long-term trends in singleton preterm birth in south Australia from 1986 to 2014. Obstet Gynecol. 2018;131:79–89. doi: 10.1097/AOG.0000000000002419. [DOI] [PubMed] [Google Scholar]
- 32.Abalos E, Cuesta C, Carroli G. Pre-eclampsia, eclampsia and adverse maternal and perinatal outcomes: a secondary analysis of the World Health Organization Multicountry Survey on Maternal and Newborn Health. BJOG. 2014;121(suppl 1):14–24. doi: 10.1111/1471-0528.12629. [DOI] [PubMed] [Google Scholar]
- 33.Hirst JE, Tran TS, Do MA, Morris JM, Jeffery HE. Consequences of gestational diabetes in an urban hospital in Viet Nam: a prospective cohort study. PLoS Med. 2012;9 doi: 10.1371/journal.pmed.1001272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Passini R, Jr, Cecatti JG, Lajos GJ. Brazilian multicentre study on preterm birth (EMIP): prevalence and factors associated with spontaneous preterm birth. PLoS One. 2014;9 doi: 10.1371/journal.pone.0109069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Wahlberg A. The birth and routinization of IVF in China. Reprod Biomed Soc Online. 2016;2:97–107. doi: 10.1016/j.rbms.2016.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Li HT, Xue M, Hellerstein S. Association of China's universal two child policy with changes in births and birth related health factors: national, descriptive comparative study. BMJ. 2019;366 doi: 10.1136/bmj.l4680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zhang HX, Zhao YY, Wang YQ. Analysis of the characteristics of pregnancy and delivery before and after implementation of the two-child policy. Chin Med J. 2018;131:37–42. doi: 10.4103/0366-6999.221268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Villar J, Valladares E, Wojdyla D. Caesarean delivery rates and pregnancy outcomes: the 2005 WHO global survey on maternal and perinatal health in Latin America. Lancet. 2006;367:1819–1829. doi: 10.1016/S0140-6736(06)68704-7. [DOI] [PubMed] [Google Scholar]
- 39.Chang HH, Larson J, Blencowe H. Preventing preterm births: analysis of trends and potential reductions with interventions in 39 countries with very high human development index. Lancet. 2013;381:223–234. doi: 10.1016/S0140-6736(12)61856-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lumbiganon P, Laopaiboon M, Gulmezoglu AM. Method of delivery and pregnancy outcomes in Asia: the WHO global survey on maternal and perinatal health 2007–08. Lancet. 2010;375:490–499. doi: 10.1016/S0140-6736(09)61870-5. [DOI] [PubMed] [Google Scholar]
- 41.Zhang J, Liu Y, Meikle S, Zheng J, Sun W, Li Z. Cesarean delivery on maternal request in southeast China. Obstet Gynecol. 2008;111:1077–1082. doi: 10.1097/AOG.0b013e31816e349e. [DOI] [PubMed] [Google Scholar]
- 42.Obstetrics group. Obstetrics and Gynecology branch. Chinese Medical Association Guidelines for pre-pregnancy and pregnancy care (2018) Chin J Perinat Med. 2018;21:145–152. (in Chinese). [Google Scholar]
- 43.Meng Q, Xu L, Zhang Y. Trends in access to health services and financial protection in China between 2003 and 2011: a cross-sectional study. Lancet. 2012;379:805–814. doi: 10.1016/S0140-6736(12)60278-5. [DOI] [PubMed] [Google Scholar]
- 44.WHO . World Health Organization; Geneva: 1993. International statistical classification of diseases and related health problems: tenth revision. [PubMed] [Google Scholar]
- 45.Macaulay S, Buchmann EJ, Dunger DB, Norris SA. Reliability and validity of last menstrual period for gestational age estimation in a low-to-middle-income setting. J Obstet Gynaecol. 2019;45:217–225. doi: 10.1111/jog.13801. [DOI] [PubMed] [Google Scholar]
- 46.Hoffman CS, Messer LC, Mendola P, Savitz DA, Herring AH, Hartmann KE. Comparison of gestational age at birth based on last menstrual period and ultrasound during the first trimester. Paediat Perinat Epidemiol. 2008;22:587–596. doi: 10.1111/j.1365-3016.2008.00965.x. [DOI] [PubMed] [Google Scholar]
- 47.Savitz DA, Terry JW, Jr, Dole N, Thorp JM, Jr, Siega-Riz AM, Herring AH. Comparison of pregnancy dating by last menstrual period, ultrasound scanning, and their combination. Am J Obstet Gynecol. 2002;187:1660–1666. doi: 10.1067/mob.2002.127601. [DOI] [PubMed] [Google Scholar]
- 48.Yang H, Kramer MS, Platt RW. How does early ultrasound scan estimation of gestational age lead to higher rates of preterm birth? Am J Obstet Gynecol. 2002;186:433–437. doi: 10.1067/mob.2002.120487. [DOI] [PubMed] [Google Scholar]
- 49.Liu Y, Kang L, He C. Neonatal mortality and leading causes of deaths: a descriptive study in China, 2014-2018. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-042654. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data in our study are not publicly available due to the terms of our contract with the Chinese National Health Commission, but are available from the corresponding authors on reasonable request and with permission of the National Health Commission of China.