Abstract
Background and aims
Fibrosis progression is the most important prognostic factor, and insulin resistance is one of the main mechanisms associated with fibrosis progression in patients with nonalcoholic fatty liver disease (NAFLD). We evaluate the association between baseline insulin resistance and future fibrosis progression in patients with NAFLD without diabetes.
Approach and results
This retrospective longitudinal study with 8-year follow-up period included 32,606 (men, 83%) participants aged >20 years (average age, 38.0 years) without diabetes at baseline who completed at least two comprehensive health checkups from January 1, 2010 to December 31, 2018. NAFLD was diagnosed based on ultrasonography. The homeostasis model assessment of insulin resistance (HOMA-IR) was used to evaluate baseline insulin resistance. Fibrosis progression was assessed using the aspartate aminotransferase to platelet ratio index (APRI). The advanced liver fibrosis with an APRI value above the intermediate fibrosis probability (≥0.5) developed in a total of 2,897 participants during 136,108 person-years. 114 participants progressed to a high fibrosis probability stage (APRI >1.5) during 141,064 person-years. Using the lowest baseline HOMA-IR quartile group (Q1) as a reference, the multivariate-adjusted hazard ratio (HR) for development of advanced liver fibrosis (APRI ≥0.5) in the highest baseline HOMA-IR quartile group (Q4) was 1.95 (95% confidence interval [CI] 1.74–2.19; Model 4). And the HR for development of advanced liver fibrosis with high fibrosis probability was 1.95 (95% CI 1.10–3.46; Model 4). The positive association was maintained throughout the entire follow-up period. The baseline HOMA-IR model was superior to the baseline body mass index (BMI) model in predicting the progression of fibrosis probability.
Conclusions
In this longitudinal study, we found that the degree of baseline insulin resistance, assessed by HOMA-IR values, was positively associated with future fibrosis progression in patients with NAFLD without diabetes.
Introduction
Nonalcoholic fatty liver disease (NAFLD) is the most common liver-related disease worldwide and is increasing in proportion to the growing population with obesity and metabolic syndrome [1]. NAFLD can be diagnosed when steatosis of hepatocytes exceeds 5% histologically, and other secondary factors, such as alcohol, should be excluded [2]. The worldwide prevalence of NAFLD is estimated to be approximately 25% [3]. NAFLD is associated with increased mortality due to cardiovascular disease [4] and liver disease itself. The stage and progression of fibrosis are the most important factors in predicting the prognosis of patients with NAFLD [5].
Unfortunately, approximately 20% of patients with NAFLD progress to nonalcoholic steatohepatitis (NASH) and fibrosis, and approximately 20% of patients with NASH progress to cirrhosis [6]. Given that there is currently no established medical treatment for biopsy-proven NASH and liver fibrosis other than lifestyle modification, it is very important to prevent progression in the early stages of NAFLD [2, 7]. From this point of view, finding a simple and reliable metabolic factor capable of predicting the progression of fibrosis in patients with NAFLD is a major concern for clinicians.
NAFLD is regarded as a disease in which metabolic syndrome affects the liver [8] and has been significantly associated with abdominal obesity as well as types 1 and 2 diabetes [9–11]. The core pathophysiology leading to NASH, fibrosis, and cirrhosis, as well as the development of steatosis, is thought to be insulin resistance (IR) [12–14]. The homeostasis model assessment of IR (HOMA-IR) is an easy and useful method of evaluating IR and beta cell function [15, 16]. To date, liver biopsy is the diagnostic gold standard for liver fibrosis in patients with NAFLD that best reflects histological changes in the liver [7]. However, biopsy has limitations such as cost, difficulty in interpretation, and risk of mortality [17]. In particular, it is practically impossible to apply biopsy as a routine in studies based on a large cohort involving a relatively healthy general population. In addition to imaging techniques such as elastography, scoring panels using biomarkers can be applied to predict or diagnose advanced fibrosis in clinical settings [18].
In patients with NAFLD proven by biopsy, regardless of diabetes, the baseline HOMA-IR can be an independent predictor of fibrosis progression [19, 20], and the HOMA-IR at the time of diagnosis was associated with the stage of fibrosis [21–23]. Only 1 study reported the association between baseline HOMA-IR and the risk of fibrosis progression in patients with NAFLD as evaluated using a non-invasive scoring index regardless of the presence of diabetes; however, the main focus of the study was weight change, not HOMA-IR [24]. In this study, we performed a longitudinal study to evaluate the association between baseline HOMA-IR and the incidence of advanced liver fibrosis as evaluated by aspartate aminotransferase to platelet ratio index (APRI), in a large cohort of relatively young and middle-aged Korean adults with NAFLD without diabetes.
Patients and methods
Study participants
This was a retrospective cohort study of adults aged >20 years who completed at least 2 comprehensive health checkups at the Total Healthcare Center of Kangbuk Samsung Hospital in Seoul and Suwon, South Korea, from January 1, 2010 to December 31, 2018.
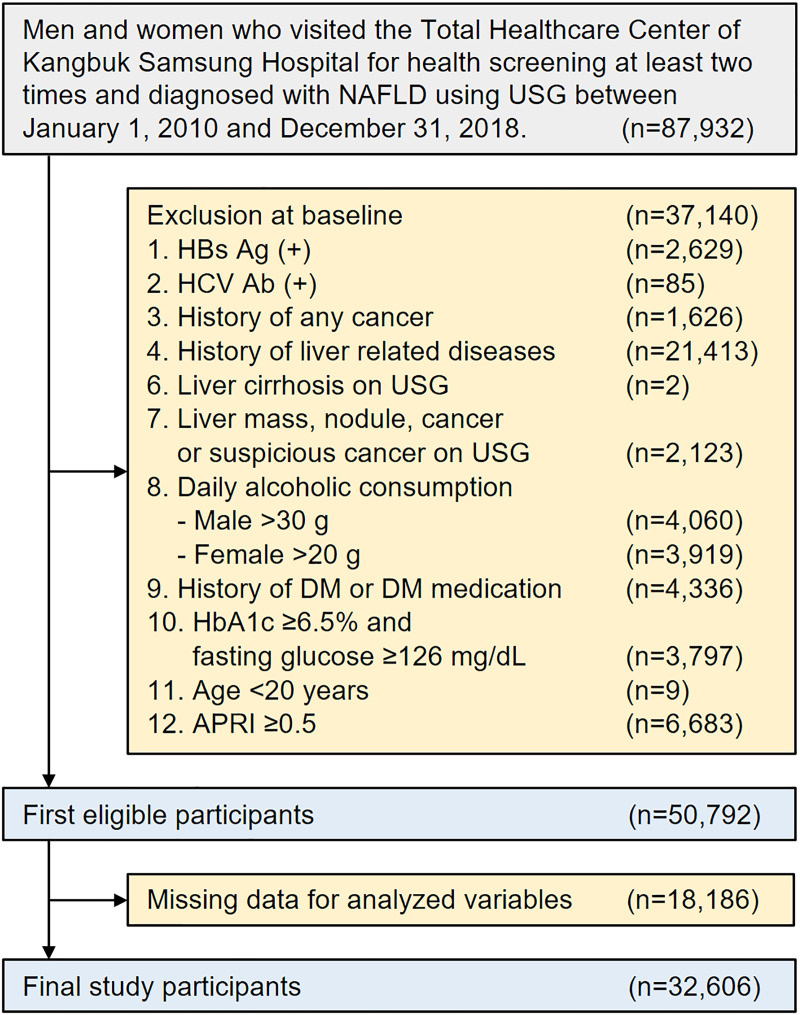
Among subjects who visited our center ≥2 times during the observation period, 87,932 participants diagnosed with NAFLD using abdominal ultrasonography (USG) were selected; 37,140 participants were excluded for the following reasons at baseline: positive findings for serologic markers of hepatitis B (n = 2,629) or hepatitis C infection (n = 85); history of cancer (n = 1,626); history of other liver disease including cirrhosis (n = 21,413); liver cirrhosis on abdominal USG (n = 2); liver mass, nodule, cancer, or suspicious cancer lesions on abdominal USG (n = 2,123); daily alcohol intake of ≥30 g/day for men (n = 4,060) or ≥20 g/day for women (n = 3,919); history of diabetes or use of antidiabetic medications (n = 4,336); hemoglobin A1c (HbA1c) levels ≥6.5% and fasting glucose levels ≥126 mg/dL (n = 3,797) [25]; age <20 years (n = 9); aspartate transaminase to platelet ratio index (APRI) ≥0.5 (n = 6,683); and missing data on blood pressure, BMI, waist circumference, HbA1c, high-sensitivity C-reactive protein (hs-CRP), high-density lipoprotein (HDL) cholesterol, low-density lipoprotein (LDL) cholesterol, or triglyceride (n = 18,186). The final sample size for our study was 32,606 (27,089 men, 83.08%) (Fig 1). This study was approved by the Institutional Review Board of Kangbuk Samsung Hospital (KBSMC 202006110001), which waived the requirement for informed consent because we retrospectively accessed data from a de-identified database.
Fig 1. Flow chart of study participants.
Abbreviations: NAFLD, nonalcoholic fatty liver disease; USG, ultrasonography; DM, diabetes mellitus; APRI, aspartate aminotransferase-to-platelet ratio index.
Anthropometric and laboratory measurements
Medical history, alcohol consumption, smoking status, and exercise status were acquired using a self-administered questionnaire. The questionnaire was based on the 4th National Health and Nutrition Survey [26] and Korean version of the International Physical Activity Questionnaire short form [27]. Alcohol intake was determined based on the average number of drinks per week, and current smoking status was based on the response “yes” or “no.” Regular exercise was defined as moderate- or high-intensity exercise performed >3 times per week. For body weight measurements, the subjects wore a thin gown, and BMI was calculated by dividing body weight (kg) by the squared height (m2). Blood pressure (BP) was measured in both arms at an interval of ≥1 min in a sitting position using a standard sphygmomanometer in a stable state after sufficient rest, and the higher of the 2 values was recorded. If the systolic blood pressure (SBP) or diastolic blood pressure (DBP) exceeded 140 mmHg or 90 mmHg, respectively, the measurement was repeated after 5 min, and the results were averaged. All blood samples were collected from patients after an overnight fast of ≥12 h. To assess fasting blood glucose and insulin levels, the hexokinase method (Modular D2400; Hitachi, Tokyo, Japan) and electrochemiluminescence immunoassay method were used (Modular E170; Hitachi), respectively. The enzymatic colorimetric method was used to measure total cholesterol and triglyceride levels. HDL cholesterol levels were measured using a selective inhibition method, and LDL cholesterol levels were measured using a homogeneous enzymatic colorimetric test. An immunoturbidimetric assay (Cobra Integra 800 automatic analyzer; Roche Diagnostics, Basel, Switzerland) was used to measure HbA1c levels. Aspartate transaminase (AST) and alanine aminotransferase levels were measured using Bayer Reagent Packs on an automated chemistry analyzer (Advia 1650 Autoanalyzer; Bayer Diagnostics, Leverkusen, Germany), and a nephelometric assay (BNII nephelometer; Dade Behring, Deerfield, IL, USA) was used to measure hs-CRP levels. To determine IR, we used the HOMA-IR formula: HOMA-IR = (fasting insulin [μIU/mL] × fasting blood glucose [mg/dL] /405) [15].
Evaluation of NAFLD and liver fibrosis
Fatty liver was examined using abdominal USG (Logic Q700 MR; GE, Milwaukee, WI, USA) and diagnosed based on USG images showing evidence of hepatic steatosis, such as higher echogenicity compared with the kidney or spleen, attenuation of the ultrasound wave, loss of definition of the diaphragm, vessel wall brightness, and poor delineation of the intrahepatic architecture [28, 29]. We defined NAFLD as fatty liver without any other cause of hepatic steatosis [7].
To assess the degree of liver fibrosis in participants with NAFLD, the APRI was applied [30], where APRI = ([AST/upper limit of normal]/platelet [109/L]) × 100. The cutoff values for fibrosis probability estimation based on APRI category were as follows: <0.5, low fibrosis probability; 0.5–1.5, intermediate fibrosis probability; and >1.5, high fibrosis probability; we defined advanced liver fibrosis in NAFLD as when a participant had an APRI value above the intermediate fibrosis probability (≥0.5) [31].
Statistics
The development of advanced liver fibrosis was the primary endpoint in this study. A parametric proportional hazards model adjusted for multivariate using 95% confidence interval (CI), controlling the interval censored events, was applied to analyze the association between baseline HOMA-IR and the incidence for the development of advanced liver fibrosis [32]. For the estimation of baseline log cumulative hazards, restricted cubic splines were used. Multivariate models have been adjusted using confounding variables associated with NAFLD. To control the effects of new-onset diabetes and HOMA-IR change, we further adjusted for time-varying development of diabetes and HOMA-IR changes during the follow-up period. (Model 4).
We also performed predefined subgroup analyses by age (<45, ≥50 years), sex, BMI (<25, ≥25 kg/m2), exercise status (<3 times/week, ≥3 times/week), current alcohol consumption (defined as daily alcohol consumption above the median value: 12 g/day for men and 2 g/day for women), and dyslipidemia (defined as LDL cholesterol ≥130 mg/dL, total cholesterol ≥200 mg/dL, triglyceride ≥150 mg/dL, and HDL <40 mg/dL in men and <50 mg/dL in women; or current use of antidyslipidemic drugs).
To quantitatively evaluate the relative power of baseline HOMA-IR and BMI values in predicting advanced liver fibrosis, the continuous variables were standardized and classified into quartiles, and hazard ratios (HRs) were also calculated. Moreover, the Akaike information criterion (AIC) calculation was performed to compare the probability of the development of advanced liver fibrosis between baseline HOMA-IR and BMI values.
Values in the tables of this study are expressed as means±SDs, numbers (%), or medians (interquartile ranges). All reported 2-tailed p-values of <0.05 were considered statistically significant. All statistical analyses were performed using STATA version 16.1 (StataCorp, College Station, TX, USA).
Results
General characteristics of study participants
Most of the 32,606 study participants were relatively young men (mean age 38.0 ± SD 7.7 years, male 83%). The mean BMI gradually increased from the quartile group with the lowest baseline HOMA-IR (group Q1) to the group with the highest baseline HOMA-IR (group Q4), and the proportion of obese individuals in group Q4 was more than twice that in group Q1 (80.2% vs. 39.5%). As baseline HOMA-IR quartile increased, the levels of baseline metabolic parameters and lifestyle conditions associated with increased IR or NAFLD progression were increasingly unfavorable except for smoking status (Table 1) [2, 4, 7]. Participants who developed advanced liver fibrosis (APRI ≥0.5) had more adverse levels of baseline metabolic parameters associated with increased IR or NAFLD progression than those who did not (S1 Table).
Table 1. Baseline characteristics of participants by HOMA-IR quartile at baseline.
| Characteristics | Overall | Baseline HOMA-IR quartile (range) | p | |||
|---|---|---|---|---|---|---|
| Q1 (0.07–1.13) | Q2 (1.14–1.65) | Q3 (1.66–2.35) | Q4 (2.36–26.15) | |||
| Number of participants | 32,606 | 8,109 | 8,165 | 8,141 | 8,191 | |
| Male, n (%) | 27,089 (83.1) | 6,907 (85.2) | 6,952 (85.1) | 6,877 (84.5) | 6,353 (77.6) | <0.001 |
| Age (years) | 38.0±7.7 | 39.3±8.0 | 38.5±7.8 | 37.6±7.5 | 36.5±7.3 | <0.001 |
| BMI (kg/m2) | 26.0±3.0 | 24.5±2.3 | 25.5±2.5 | 26.2±2.7 | 27.9±3.4 | <0.001 |
| Obesitya, n (%) | 19,662 (60.3) | 3,204 (39.5) | 4,544 (55.7) | 5,343 (65.6) | 6,571 (80.2) | <0.001 |
| WC (cm) | 89.1±7.8 | 85.5±6.5 | 87.9±6.8 | 89.8±7.0 | 93.4±8.5 | <0.001 |
| FBG (mg/dL) | 95.49±9 | 90.5±7.7 | 94.4±7.7 | 96.72±8.0 | 100.4±9.4 | <0.001 |
| Hemoglobin A1c (%) | 5.6±0.3 | 5.6±0.3 | 5.6±0.3 | 5.6±0.3 | 5.7±0.3 | <0.001 |
| SBP (mmHg) | 115.8±12.1 | 113.1±11.7 | 115.1±11.8 | 116.2±11.8 | 118.9±12.4 | <0.001 |
| Antihypertensive medications, n (%) | 1,827 (5.6) | 351 (4.3) | 412 (5.1) | 455 (5.6) | 609 (7.4) | <0.001 |
| Hypertension, n (%) | 3,637 (11.2) | 663 (8.2) | 811 (9.9) | 913 (11.2) | 1,250 (15.3) | <0.001 |
| AST (U/L) | 23 (19–28) | 22 (19–27) | 22 (19–27) | 23 (19–28) | 24 (19–30) | <0.001 |
| ALT (U/L) | 28 (20–40) | 24 (18–33) | 27 (19–37) | 29 (21–41) | 34 (23–49) | <0.001 |
| Platelets (×103/mm3) | 255.6±49.8 | 249.00±47.6 | 253.5±48.9 | 255.9±49.1 | 264.2±52.3 | <0.001 |
| Albumin (g/dL) | 4.7 (4.5–4.9) | 4.7 (4.5–4.9) | 4.7 (4.5–4.9) | 4.7 (4.5–4.9) | 4.7 (4.5–4.9) | <0.001 |
| Total cholesterol (mg/dL) | 205.1±34.6 | 202.9±34.3 | 204.9±33.9 | 205.6±34.6 | 207.2±35.6 | <0.001 |
| Triglyceride (mg/dL) | 132 (95–185) | 104 (77–144) | 127 (93–173) | 140 (103–192) | 161 (118–224) | <0.001 |
| LDL (mg/dL) | 134.2±31.3 | 131.9±31.6 | 133.9±30.7 | 134.8±31.0 | 135.9±31.9 | <0.001 |
| HDL (mg/dL) | 49.5±11.3 | 52.7±12.1 | 50.1±11.4 | 48.7±10.7 | 46.5±10.1 | <0.001 |
| Antidyslipidemic medication, n (%) | 740 (2.27) | 146 (1.8) | 182 (2.23) | 191 (2.35) | 221 (2.7) | 0.002 |
| Dyslipidemia, n (%) | 4,717 (14.5) | 975 (12.0) | 1,056 (12.9) | 1,273 (15.6) | 1,413 (17.3) | <0.001 |
| hs-CRP (mg/dL) | 0.14±0.32 | 0.12±0.29 | 0.13±0.29 | 0.14±0.33 | 0.18±0.37 | <0.001 |
| Current alcohol useb, n (%) | 15,459 (47.4) | 3,790 (46.7) | 3,866 (47.4) | 3,861 (47.4) | 3,942 (48.1) | 0.367 |
| Male | 12,786 (47.2) | 3,186 (46.1) | 3,284 (47.2) | 3,253 (47.3) | 3,063 (48.2) | |
| Female | 2,673 (48.5) | 604 (50.3) | 582 (48.0) | 608 (48.1) | 879 (47.8) | |
| Smoking status, n (%) | <0.001 | |||||
| Never | 11,881 (36.4) | 2,666 (32.9) | 2,861 (35.0) | 2,987 (36.7) | 3,367 (41.1) | |
| Ex | 10,024 (30.7) | 2,680 (33.1) | 2,514 (30.8) | 2,504 (30.8) | 2,326 (28.4) | |
| Current | 9,660 (29.6) | 2,449 (30.2) | 2,535 (31.1) | 2,399 (29.5) | 2,277 (27.8) | |
| Regular exercise, n (%) | <0.001 | |||||
| ≥3 times/week | 3,581 (11.0) | 1,097 (13.5) | 908 (11.1) | 827 (10.2) | 749 (9.1) | |
| <3 times/week | 28,723 (88.1) | 6,921 (85.4) | 7,185 (88.0) | 7,238 (88.9) | 7,379 (90.1) | |
| APRI | 0.25±0.08 | 0.25±0.08 | 0.25±0.08 | 0.25±0.08 | 0.26±0.09 | <0.001 |
Abbreviations: BMI, body mass index; WC, waist circumference; FBG, fasting blood glucose; SBP, systolic blood pressure; AST, aspartate aminotransferase; ALT, alanine aminotransferase; LDL, low-density lipoprotein; HDL, high-density lipoprotein; hs-CRP, high-sensitivity C-reactive protein; APRI, aspartate aminotransferase-to-platelet ratio index.
aObesity was defined as a BMI ≥25 kg/m2.
bParticipants with daily alcohol consumption above the median value (11 g/day for men and 2 g/day for women)
Relationship between the baseline HOMA-IR and the development of advanced liver fibrosis
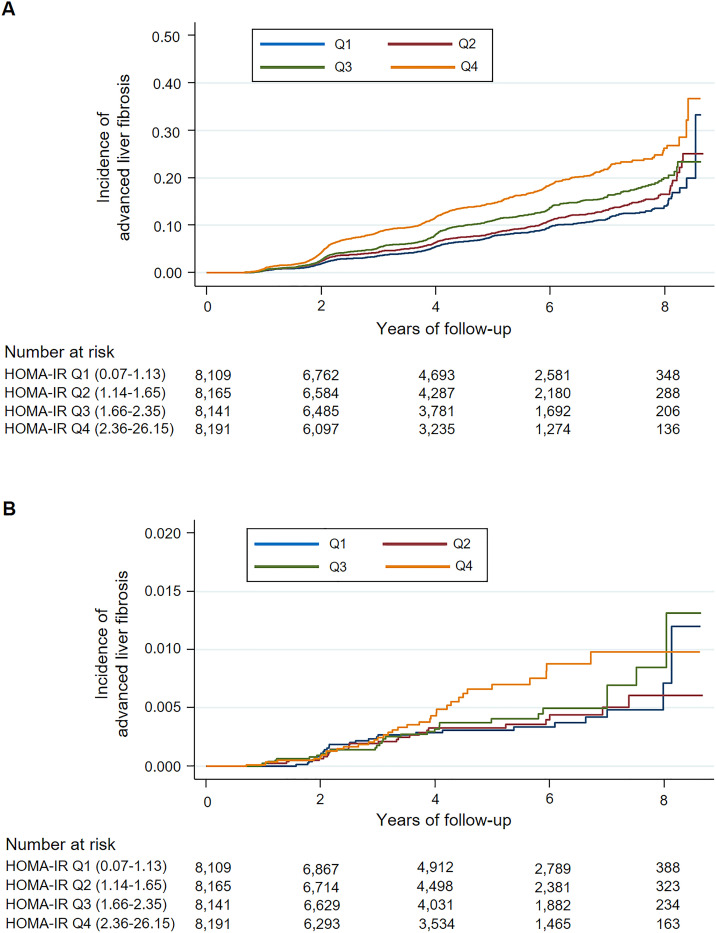
In Table 2, advanced liver fibrosis (APRI ≥0.5) developed in a total of 2,897 participants during 136,108 person-years (median follow-up, 3.97 years). In all models, as the baseline HOMA-IR increased, the HR tended to increase. The HR for advanced liver fibrosis in group Q4 relative to group Q1 was 2.18 (95% CI 1.96–2.42) in Model 1. However, the HR decreased to 1.95 (95% CI 1.74–2.19; Model 4) after adjusting for confounding variables mentioned above. The cumulative incidence of advanced liver fibrosis with an intermediate or high probability linearly increased in all quartile groups from the 2nd year of follow-up. Subsequently, the positive association between baseline HOMA-IR and the incidence of advanced liver fibrosis was maintained throughout the entire follow-up period (Fig 2A).
Table 2. Hazard ratios for the development of advanced liver fibrosis by HOMA-IR quartile at baseline.
| HOMA-IR quartile | No.a | Cases | IR (per 104 PY) | Model 1 HR (95% CI) | Model 2 HR (95% CI) | Model 3 HR (95% CI) | Model 4 HR (95% CI) |
|---|---|---|---|---|---|---|---|
| Above the intermediate fibrosis probability (APRI ≥0.5) | |||||||
| Total | 32,606 | 2,897 | 212.8 (205.2–220.7) | ||||
| Q1 (0.07–1.13) | 8,109 | 596 | 159.4 (147.1–172.7) | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) |
| Q2 (1.14–1.65) | 8,165 | 651 | 183.4 (169.9–198.1) | 1.18 (1.06–1.32) | 1.15 (1.03–1.28) | 1.10 (0.98–1.23) | 1.14 (1.02–1.28) |
| Q3 (1.66–2.35) | 8,141 | 724 | 219.5 (204.1–236.1) | 1.48 (1.32–1.65) | 1.41 (1.27–1.58) | 1.30 (1.16–1.46) | 1.40 (1.25–1.57) |
| Q4 (2.36–26.15) | 8,191 | 926 | 305.8 (286.8–326.2) | 2.18 (1.96–2.42) | 2.00 (1.80–2.23) | 1.71 (1.52–1.92) | 1.95 (1.74–2.19) |
| p-value | <0.001 | <0.001 | <0.001 | <0.001 | |||
| With high fibrosis probability (APRI >1.5) | |||||||
| Total | 32,606 | 114 | 8.0 (6.7–9.7) | ||||
| Q1 (0.07–1.13) | 8,109 | 26 | 6.7 (4.5–9.9) | 1 (reference) | 1 (reference) | 1 (reference) | 1 (reference) |
| Q2 (1.14–1.65) | 8,165 | 25 | 6.8 (4.6–10.1) | 1.02 (0.59–1.77) | 1.03 (0.59–1.78) | 0.95 (0.54–1.69) | 0.99 (0.56–1.76) |
| Q3 (1.66–2.35) | 8,141 | 28 | 8.1 (5.6–11.8) | 1.25 (0.73–2.14) | 1.26 (0.74–2.17) | 1.25 (0.72–2.18) | 1.34 (0.77–2.34) |
| Q4 (2.36–26.15) | 8,191 | 35 | 11.0 (7.9–15.3) | 1.73 (1.03–2.92) | 1.76 (1.03–3.00) | 1.70 (0.96–3.01) | 1.95 (1.10–3.46) |
| p-value | 0.027 | 0.028 | 0.044 | 0.014 | |||
Model 1 adjusted for age, sex, and year of examination. Model 2 was additionally adjusted for SBP, antihypertensive medications, regular exercise, current alcohol consumption, and smoking status. Model 3 was additionally adjusted for BMI, waist circumference, HbA1c, hs-CRP, LDL cholesterol, HDL cholesterol, triglyceride, and lipid-lowering medications. Model 4, additionally adjusted for time-varying development of diabetes and HOMA-IR change during the follow-up period.
Abbreviations: HOMA-IR, homeostasis model assessment of insulin resistance; IR, incidence rate; PY, person-years; HR, hazard ratio; APRI, aspartate aminotransferase-to-platelet ratio index; SBP, systolic blood pressure; BMI, body mass index; HbA1c, hemoglobin A1c; hs-CRP, high-sensitivity C-reactive protein; LDL, low-density lipoprotein; HDL, high-density lipoprotein.
a Number of participants.
Fig 2. Cumulative incidence of advanced liver fibrosis by HOMA-IR quartile at baseline.
(A) Above the intermediate fibrosis probability (APRI ≥0.5), (B) With high fibrosis probability (APRI >1.5). Abbreviations: HOMA-IR, homeostatic model assessment of insulin resistance; APRI, aspartate aminotransferase-to-platelet ratio index.
However, only 114 participants developed advanced liver fibrosis with high probability (APRI >1.5) during 141,064 person-years (median follow-up, 4.06 years) (Table 2). When compared with group Q1 as a reference, the HR for advanced liver fibrosis with high fibrosis probability in group Q4 was 1.73 (95% CI 1.03–2.92) in Model 1. This value was nearly maintained in Models 2 and 3, but slightly increased to 1.95 (95% CI 1.10–3.46) in Model 4. As shown in Fig 2B, the overall tendency in the cumulative incidence of advanced liver fibrosis with high probability was similar to that of Fig 2A. However, meaningful differences in the incidence of advanced liver fibrosis between quartile groups began to appear from the 4th year of follow-up relatively.
The optimal cut-off value of baseline HOMA-IR as a surrogate marker for predicting the development of advanced liver fibrosis was 1.68 (sensitivity 56.2%, specificity 51.5%, positive predictive value 10.2%, and negative predictive value 92.3%), which was obtained using Youden’s J index and area under the receiver operating characteristic (ROC) curve (AUC 0.553, 95% CI; 0.541–0.564) (S1 Fig) [33].
Subgroup analysis
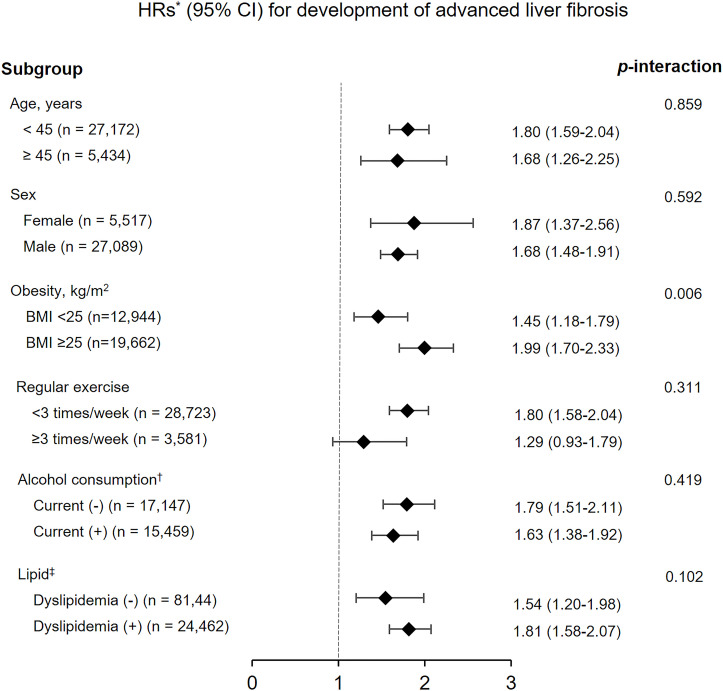
In all subgroup analyses, the HRs for development of advanced liver fibrosis with an APRI value of ≥0.5 also tended to increase as the baseline HOMA-IR quartile increased. All p-values for interaction were >0.05, except obesity (p-interaction = 0.006) (Fig 3). In the analysis of advanced liver fibrosis with high probability, all p-values for interaction were >0.05, and group Q4 was associated with an increased incidence of advanced liver fibrosis except in participants who exercised regularly (≥3 times/week) (S2 Table).
Fig 3. Subgroup analyses of hazard ratios for the development of advanced liver fibrosis (APRI value of ≥0.5) in participants belonging to the highest baseline HOMA-IR quartile (Q4) compared with those belonging to the lowest baseline HOMA-IR quartile (Q1).
*Adjusted for age, sex, year of examination, SBP, antihypertensive medications, regular exercise, current alcohol consumption, smoking status, BMI, waist circumference, HbA1c, hs-CRP, LDL cholesterol, HDL cholesterol, triglyceride, and use of antidyslipidemic drugs. † Current alcohol consumption defined as daily alcohol consumption above the median value (12 g/day for men, 2 g/day for women). ‡ Dyslipidemia was defined as total cholesterol ≥200 mg/dL, triglyceride levels ≥150 mg/dL, LDL cholesterol levels ≥130 mg/dL, HDL cholesterol levels <40 mg/dL in men and <50 mg/dL in women, or use of antidyslipidemic drugs. Abbreviations: HOMA-IR, homeostasis model assessment of insulin resistance; SBP, systolic blood pressure; BMI, body mass index; HbA1c, hemoglobin A1c; hs-CRP, high-sensitivity C-reactive protein; LDL, low-density lipoprotein; HDL, high-density lipoprotein; HR, hazard ratio; CI, confidence interval.
Comparison of baseline HOMA-IR and baseline BMI values with respect to the prediction of fibrosis probability progression
S3 Table demonstrates the comparison between standardized quartiles of baseline HOMA-IR and standardized quartiles of baseline BMI with respect to the risk of advanced liver fibrosis in patients with NAFLD without diabetes. There was no significant difference in quantitative influence; the increase in HR per 1 SD of baseline HOMA-IR values was 1.13 (95% CI 1.10–1.15), and the increase in HR per 1 SD of baseline BMI values was 1.16 (95% CI 1.08–1.25). In the predictive validity analysis for the development of advanced liver fibrosis with an APRI value of ≥0.5, the baseline HOMA-IR model showed a smaller AIC value than the baseline BMI model (54,387 vs. 54,449.29). For the analysis of advanced liver fibrosis with high fibrosis probability (APRI >1.5), the baseline BMI model was not statistically significant.
Discussion
In this longitudinal cohort study of 32,606 young and middle-aged adult participants, we found that higher quartiles of baseline HOMA-IR, i.e., higher insulin resistance, were associated with higher risk of fibrosis progression as evaluated by APRI value in participants with NAFLD without diabetes. In addition, this positive association remained constant throughout the follow-up period. This suggests that insulin resistance at the time of NAFLD diagnosis may be a key factor in future fibrosis progression. This tendency was maintained in all models adjusted for risk factors associated with the development of NAFLD or fibrosis progression and remained even when we eliminated the effect of diabetes that developed after baseline. The results were also consistent in predefined subgroup analysis.
NAFLD is a broad-spectrum disease that can simultaneously or separately show steatosis, NASH, fibrosis, and cirrhosis [34]. In addition to IR, activation of inflammation due to an adverse lifestyle such as a high-calorie diet, genetic factors associated with family history, oxidative stress, and lipotoxicity are the underlying mechanisms of the pathogenesis of NAFLD and progressive fibrosis. IR interferes with the anti-lipolytic effect of insulin and increases free fatty acids (FFA). These excess FFA enter the liver and accumulate. Moreover, increased insulin levels promote triglyceride (TG) synthesis in hepatocytes. In this process, very low density lipoprotein production is activated and increased TG is also a source of FFA. This steatosis is associated with oxidative stress, lipid peroxidation, and increased secretion of inflammatory markers. FFA also stimulate the production of cytokines and chemokines by activating Toll-like receptors (TLRs) and inflammasomes. In the fibrosis of NAFLD, Kupffer cells, recruited macrophages and stellate cells are key regulators activated by cytokines, chemokines, and oxidative stress [35, 36]. In these processes, hepatic mitochondrial dysfunction and triacylglycerol accumulation are included [37], and IR, lipotoxicity, and inflammation influence each other to form a vicious cycle and at the same time to further promote fibrosis progression in patients with NAFLD [38].
A prospective study of patients with NAFLD demonstrated that baseline HOMA-IR, which reflects an estimate of baseline IR, is an independent risk factor for advanced fibrosis [19]. In 2 studies on the progression of fibrosis in patients with NAFLD based on serial biopsies at intervals of ≥1 year, a tendency to have higher baseline HOMA-IR was confirmed in patients with fibrosis progression (5.8±5.1 SD vs. 3.9±2.5 SD, p = 0.09) [20]. Increased IR was also shown to play a key role in the progression of simple steatosis to steatohepatitis with fibrosis [39]. In a prospective cohort study analyzing the association between weight change and the risk of fibrosis progression as evaluated by APRI values in 40,700 Korean adults with NAFLD, the baseline HOMA-IR value was a risk factor for fibrosis progression [24]. Interestingly, in that study, the influence of weight change on fibrosis progression depended on baseline HOMA-IR value, i.e., it was greater in patients with HOMA-IR <2.5. Recently, in a retrospective study using histological verification in patients with NAFLD, the HOMA-IR value at the time of evaluation was closely associated with the degree of liver fibrosis at the same time in patients with NAFLD regardless of the presence of diabetes [21–23].
Obesity, one of the most important phenotypes of patients with metabolic syndrome, is also closely associated with the aggravation of IR and development of NAFLD; obesity and NAFLD share many common pathophysiological mechanisms [35, 40]. Increases in waist circumference and visceral-subcutaneous abdominal fat ratio have been reported to be associated with the development of NAFLD and advanced liver fibrosis [41, 42]. A prospective Korean cohort study showed that weight gain and baseline obesity were associated with APRI progression in patients with NAFLD [24]. These findings are consistent with the results of our study. In our study, the HRs for the development of advanced liver fibrosis above the intermediate fibrosis risk according to baseline HOMA-IR quartile were affected by baseline obesity status (p for interaction = 0.006). In other words, the presence or absence of obesity influenced the association between baseline HOMA-IR value and the risk of advanced liver fibrosis, and the positive association was more pronounced in participants with obesity (BMI ≥25 kg/m2). Therefore, we performed a comparative analysis of quantitative power and prediction quality for the development of advanced liver fibrosis, defined as an APRI value of ≥0.5, between standardized baseline HOMA-IR values and standardized baseline BMI values. Interestingly, based on the AIC calculation, the baseline HOMA-IR model was superior to the baseline BMI model in predicting the advanced liver fibrosis as evaluated by the APRI. However, the quantitative increase in HR per 1 SD was similar in both models.
Despite these statistically significant results, there are some limitations to the interpretation. First, in the diagnosis of NAFLD and fibrosis stage, histological evaluation was not performed, which is a practical limitation of large-scale cohort studies due to the low clinical utility of biopsies in the general population [17]. Despite some of its disadvantages, USG has a relatively high accuracy in diagnosing NAFLD [43]. In addition, the scoring systems, such as NFS and FIB-4, using metabolic variables for predicting the fibrosis progression of NAFLD provide convenience and efficiency in large-scale cohort studies and provide clinically acceptable positive and negative predictive values [7, 44]. However, NFS includes age and BMI as components. And FIB-4 also includes age as a component. In longitudinal studies like ours, age itself can influence outcomes [24]. To exclude the effect of BMI, BMI along with age was included as an adjustment factor. However, if NFS is applied, age and BMI cannot be included as adjustment factors. In addition, NFS cannot be applied in analysis to compare baseline HOMA-IR and baseline BMI. We performed the same analysis based on NFS and FIB-4, and found no statistical significance (No data was provided). APRI could be used as a useful diagnostic tool in the evaluation of fibrosis in patients with NAFLD in a longitudinal study [24, 31, 45]. Nevertheless, in our longitudinal study, baseline HOMA-IR is not a tool to directly diagnose liver fibrosis, and we chronologically analyzed the association between baseline HOMA-IR and incidence of future advanced liver fibrosis indirectly assessed by APRI progression. So, the baseline HOMA-IR cut-off value obtained using AUC requires caution in applying and interpreting the diagnosis of advanced liver fibrosis due to the limitation of applying the APRI ≥0.5 criterion. Second, among the data used in the analysis of our study, the lifestyle, medications, and past medical history, other than laboratory test and measurement data, completely depend on information provided by the participants without any other verification procedure. Third, the effects of drugs and dietary supplements other than antidiabetic, anti-dyslipidemia, and antihypertensive agents were not excluded. Finally, most study participants were relatively young white-collar Korean workers, and the majority of them were men (83%). Sex, race, and age are factors that influence the development and progression of NAFLD [46, 47]. Although age and sex were adjusted for in the analysis of HRs and cumulative incidence of advanced liver fibrosis, the results of our study have limited generalizability. Nonetheless, our study has clinical implications as a highly sophisticated longitudinal study that assessed the progression of fibrosis probability using a non-invasive scoring system according to the baseline HOMA-IR value in participants with NAFLD without diabetes based on a large cohort data.
In conclusion, this study demonstrated that baseline IR assessed using HOMA-IR in patients with NAFLD without diabetes was associated with the future development of advanced liver fibrosis, i.e., the higher the baseline HOMA-IR, the higher the incidence of fibrosis probability progression.
Supporting information
(DOCX)
(DOCX)
(DOCX)
(TIF)
Acknowledgments
The authors acknowledge the efforts of the Department of R&D Management at Kangbuk Samsung Hospital, Korea, for editing the figures and tables.
Abbreviations
- IR
insulin resistance
- NAFLD
non-alcoholic fatty liver disease
- NASH
nonalcoholic steatohepatitis
- HOMA–IR
homeostasis model assessment of insulin resistance
- APRI
AST to platelet ratio index
- BMI
body mass index
- SBP
systolic blood pressure
- DBP
diastolic blood pressure
- AST
aspartate transaminase
- hs-CRP
high-sensitivity C-reactive protein
- HDL
high-density lipoprotein
- LDL
low-density lipoprotein
- HR
hazard ratio
- SD
standard deviation
- AUC
area under the receiver operating characteristic curve
Data Availability
Data are available from the Kangbuk Samsung Health Study whose authors may be contacted through the corresponding author. Unfortunately, the data are not available to be shared publicly as we do not have IRB permission for distributing publicly the data (because public availability would compromise patient confidentiality or participant privacy). The IRB No. of our Study: KBSMC2020-05-019. For additional information, please visit the Kangbuk Samusng Health Study at http://kscs.kbsmc.co.kr/ or contact Gayoung Lim (gayoung.lim@samsung.com).
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Araujo AR, Rosso N, Bedogni G, Tiribelli C, Bellentani S. Global epidemiology of non-alcoholic fatty liver disease/non-alcoholic steatohepatitis: What we need in the future. Liver Int. 2018; 38Suppl 1: 47–51. doi: 10.1111/liv.13643 [DOI] [PubMed] [Google Scholar]
- 2.European Association for the Study of the Liver (EASL), European Association for the Study of Diabetes (EASD), European Association for the Study of Obesity (EASO). EASL-EASD-EASO Clinical Practice Guidelines for the management of non-alcoholic fatty liver disease. J Hepatol. 2016; 64: 1388–1402. doi: 10.1016/j.jhep.2015.11.004 [DOI] [PubMed] [Google Scholar]
- 3.Younossi ZM, Koenig AB, Abdelatif D, Fazel Y, Henry L, Wymer M. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016; 64: 73–84. doi: 10.1002/hep.28431 [DOI] [PubMed] [Google Scholar]
- 4.Adams LA, Anstee QM, Tilg H, Targher G. Non-alcoholic fatty liver disease and its relationship with cardiovascular disease and other extrahepatic diseases. Gut. 2017; 66: 1138–1153. doi: 10.1136/gutjnl-2017-313884 [DOI] [PubMed] [Google Scholar]
- 5.Ekstedt M, Hagstrom H, Nasr P, Fredrikson M, Stal P, Kechagias S, et al. Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology. 2015; 61: 1547–1554. doi: 10.1002/hep.27368 [DOI] [PubMed] [Google Scholar]
- 6.Sheka AC, Adeyi O, Thompson J, Hameed B, Crawford PA, Ikramuddin S. Nonalcoholic Steatohepatitis: A Review. JAMA. 2020; 323: 1175–1183. doi: 10.1001/jama.2020.2298 [DOI] [PubMed] [Google Scholar]
- 7.Chalasani N, Younossi Z, Lavine JE, Charlton M, Cusi K, Rinella M, et al. The diagnosis and management of nonalcoholic fatty liver disease: Practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2018; 67: 328–357. doi: 10.1002/hep.29367 [DOI] [PubMed] [Google Scholar]
- 8.Marchesini G, Bugianesi E, Forlani G, Cerrelli F, Lenzi M, Manini R, et al. Nonalcoholic fatty liver, steatohepatitis, and the metabolic syndrome. Hepatology. 2003; 37: 917–923. doi: 10.1053/jhep.2003.50161 [DOI] [PubMed] [Google Scholar]
- 9.Targher G, Bertolini L, Padovani R, Rodella S, Zoppini G, Pichiri I, et al. Prevalence of non-alcoholic fatty liver disease and its association with cardiovascular disease in patients with type 1 diabetes. J Hepatol. 2010; 53: 713–718. doi: 10.1016/j.jhep.2010.04.030 [DOI] [PubMed] [Google Scholar]
- 10.Targher G, Bertolini L, Padovani R, Rodella S, Tessari R, Zenari L, et al. Prevalence of nonalcoholic fatty liver disease and its association with cardiovascular disease among type 2 diabetic patients. Diabetes Care. 2007; 30: 1212–1218. doi: 10.2337/dc06-2247 [DOI] [PubMed] [Google Scholar]
- 11.van der Poorten D, Milner KL, Hui J, Hodge A, Trenell MI, Kench JG, et al. Visceral fat: a key mediator of steatohepatitis in metabolic liver disease. Hepatology. 2008; 48: 449–457. doi: 10.1002/hep.22350 [DOI] [PubMed] [Google Scholar]
- 12.Utzschneider KM, Kahn SE. Review: The role of insulin resistance in nonalcoholic fatty liver disease. J Clin Endocrinol Metab. 2006; 91: 4753–4761. doi: 10.1210/jc.2006-0587 [DOI] [PubMed] [Google Scholar]
- 13.Rhee EJ, Lee WY, Cho YK, Kim BI, Sung KC. Hyperinsulinemia and the development of nonalcoholic Fatty liver disease in nondiabetic adults. Am J Med. 2011; 124: 69–76. doi: 10.1016/j.amjmed.2010.08.012 [DOI] [PubMed] [Google Scholar]
- 14.Angulo P, Machado MV, Diehl AM. Fibrosis in nonalcoholic Fatty liver disease: mechanisms and clinical implications. Semin Liver Dis. 2015; 35: 132–145. doi: 10.1055/s-0035-1550065 [DOI] [PubMed] [Google Scholar]
- 15.Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985; 28: 412–419. doi: 10.1007/BF00280883 [DOI] [PubMed] [Google Scholar]
- 16.Haffner SM, Miettinen H, Stern MP. The homeostasis model in the San Antonio Heart Study. Diabetes Care. 1997; 20: 1087–1092. doi: 10.2337/diacare.20.7.1087 [DOI] [PubMed] [Google Scholar]
- 17.Sumida Y, Nakajima A, Itoh Y. Limitations of liver biopsy and non-invasive diagnostic tests for the diagnosis of nonalcoholic fatty liver disease/nonalcoholic steatohepatitis. World J Gastroenterol. 2014; 20: 475–485. doi: 10.3748/wjg.v20.i2.475 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Xiao G, Zhu S, Xiao X, Yan L, Yang J, Wu G. Comparison of laboratory tests, ultrasound, or magnetic resonance elastography to detect fibrosis in patients with nonalcoholic fatty liver disease: A meta-analysis. Hepatology. 2017; 66: 1486–1501. doi: 10.1002/hep.29302 [DOI] [PubMed] [Google Scholar]
- 19.Sorrentino P, Terracciano L, D’Angelo S, Ferbo U, Bracigliano A, Vecchione R. Predicting fibrosis worsening in obese patients with NASH through parenchymal fibronectin, HOMA-IR, and hypertension. Am J Gastroenterol. 2010; 105: 336–344. doi: 10.1038/ajg.2009.587 [DOI] [PubMed] [Google Scholar]
- 20.Pais R, Charlotte F, Fedchuk L, Bedossa P, Lebray P, Poynard T, et al. A systematic review of follow-up biopsies reveals disease progression in patients with non-alcoholic fatty liver. J Hepatol. 2013; 59: 550–556. doi: 10.1016/j.jhep.2013.04.027 [DOI] [PubMed] [Google Scholar]
- 21.Gomez de la Cuesta S, Aller de la Fuente R, Tafur Sanchez C, Izaola O, Garcia Sanchez C, Mora N, et al. Analytical, anthropometric and dietary factors associated with the development of fibrosis in patients with nonalcoholic fatty liver disease. Rev Esp Enferm Dig. 2018; 110: 292–298. doi: 10.17235/reed.2018.5118/2017 [DOI] [PubMed] [Google Scholar]
- 22.Fujii H, Imajo K, Yoneda M, Nakahara T, Hyogo H, Takahashi H, et al. HOMA-IR: An independent predictor of advanced liver fibrosis in nondiabetic non-alcoholic fatty liver disease. J Gastroenterol Hepatol. 2019; 34: 1390–1395. doi: 10.1111/jgh.14595 [DOI] [PubMed] [Google Scholar]
- 23.Aller R, Siguenza R, Pina M, Laserna C, Antolin B, Burgueno B, et al. Insulin resistance is related with liver fibrosis in type 2 diabetic patients with non-alcoholic fatty liver disease proven biopsy and Mediterranean diet pattern as a protective factor. Endocrine. 2020; 68: 557–563. doi: 10.1007/s12020-020-02268-7 [DOI] [PubMed] [Google Scholar]
- 24.Kim Y, Chang Y, Cho YK, Ahn J, Shin H, Ryu S. Obesity and Weight Gain Are Associated With Progression of Fibrosis in Patients With Nonalcoholic Fatty Liver Disease. Clin Gastroenterol Hepatol. 2019; 17: 543–550 e542. doi: 10.1016/j.cgh.2018.07.006 [DOI] [PubMed] [Google Scholar]
- 25.American Diabetes A. 2. Classification and Diagnosis of Diabetes: Standards of Medical Care in Diabetes-2021. Diabetes Care. 2021; 44: S15–S33. doi: 10.2337/dc21-S002 [DOI] [PubMed] [Google Scholar]
- 26.Yoon YS, Oh SW, Baik HW, Park HS, Kim WY. Alcohol consumption and the metabolic syndrome in Korean adults: the 1998 Korean National Health and Nutrition Examination Survey. Am J Clin Nutr. 2004; 80: 217–224. doi: 10.1093/ajcn/80.1.217 [DOI] [PubMed] [Google Scholar]
- 27.Chun MY. Validity and reliability of korean version of international physical activity questionnaire short form in the elderly. Korean J Fam Med. 2012; 33: 144–151. doi: 10.4082/kjfm.2012.33.3.144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hamer OW, Aguirre DA, Casola G, Lavine JE, Woenckhaus M, Sirlin CB. Fatty liver: imaging patterns and pitfalls. Radiographics. 2006; 26: 1637–1653. doi: 10.1148/rg.266065004 [DOI] [PubMed] [Google Scholar]
- 29.Mathiesen UL, Franzen LE, Aselius H, Resjo M, Jacobsson L, Foberg U, et al. Increased liver echogenicity at ultrasound examination reflects degree of steatosis but not of fibrosis in asymptomatic patients with mild/moderate abnormalities of liver transaminases. Dig Liver Dis. 2002; 34: 516–522. doi: 10.1016/s1590-8658(02)80111-6 [DOI] [PubMed] [Google Scholar]
- 30.Wai CT, Greenson JK, Fontana RJ, Kalbfleisch JD, Marrero JA, Conjeevaram HS, et al. A simple noninvasive index can predict both significant fibrosis and cirrhosis in patients with chronic hepatitis C. Hepatology. 2003; 38: 518–526. doi: 10.1053/jhep.2003.50346 [DOI] [PubMed] [Google Scholar]
- 31.Salomone F, Micek A, Godos J. Simple Scores of Fibrosis and Mortality in Patients with NAFLD: A Systematic Review with Meta-Analysis. J Clin Med. 2018; 7. doi: 10.3390/jcm7080219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Royston P, Parmar MK. Flexible parametric proportional-hazards and proportional-odds models for censored survival data, with application to prognostic modelling and estimation of treatment effects. Stat Med. 2002; 21: 2175–2197. doi: 10.1002/sim.1203 [DOI] [PubMed] [Google Scholar]
- 33.Hajian-Tilaki K. The choice of methods in determining the optimal cut-off value for quantitative diagnostic test evaluation. Stat Methods Med Res. 2018; 27: 2374–2383. doi: 10.1177/0962280216680383 [DOI] [PubMed] [Google Scholar]
- 34.Anstee QM, Targher G, Day CP. Progression of NAFLD to diabetes mellitus, cardiovascular disease or cirrhosis. Nat Rev Gastroenterol Hepatol. 2013; 10: 330–344. doi: 10.1038/nrgastro.2013.41 [DOI] [PubMed] [Google Scholar]
- 35.Gaggini M, Morelli M, Buzzigoli E, DeFronzo RA, Bugianesi E, Gastaldelli A. Non-alcoholic fatty liver disease (NAFLD) and its connection with insulin resistance, dyslipidemia, atherosclerosis and coronary heart disease. Nutrients. 2013; 5: 1544–1560. doi: 10.3390/nu5051544 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Brunt EM, Wong VW, Nobili V, Day CP, Sookoian S, Maher JJ, et al. Nonalcoholic fatty liver disease. Nat Rev Dis Primers. 2015; 1: 15080. doi: 10.1038/nrdp.2015.80 [DOI] [PubMed] [Google Scholar]
- 37.Koliaki C, Szendroedi J, Kaul K, Jelenik T, Nowotny P, Jankowiak F, et al. Adaptation of hepatic mitochondrial function in humans with non-alcoholic fatty liver is lost in steatohepatitis. Cell Metab. 2015; 21: 739–746. doi: 10.1016/j.cmet.2015.04.004 [DOI] [PubMed] [Google Scholar]
- 38.Chen Z, Yu R, Xiong Y, Du F, Zhu S. A vicious circle between insulin resistance and inflammation in nonalcoholic fatty liver disease. Lipids Health Dis. 2017; 16: 203. doi: 10.1186/s12944-017-0572-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.McPherson S, Hardy T, Henderson E, Burt AD, Day CP, Anstee QM. Evidence of NAFLD progression from steatosis to fibrosing-steatohepatitis using paired biopsies: implications for prognosis and clinical management. J Hepatol. 2015; 62: 1148–1155. doi: 10.1016/j.jhep.2014.11.034 [DOI] [PubMed] [Google Scholar]
- 40.Bedogni G, Miglioli L, Masutti F, Tiribelli C, Marchesini G, Bellentani S. Prevalence of and risk factors for nonalcoholic fatty liver disease: the Dionysos nutrition and liver study. Hepatology. 2005; 42: 44–52. doi: 10.1002/hep.20734 [DOI] [PubMed] [Google Scholar]
- 41.Yun KE, Nam GE, Lim J, Park HS, Chang Y, Jung HS, et al. Waist Gain Is Associated with a Higher Incidence of Nonalcoholic Fatty Liver Disease in Korean Adults: A Cohort Study. PLoS One. 2016; 11: e0158710. doi: 10.1371/journal.pone.0158710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Jung CH, Rhee EJ, Kwon H, Chang Y, Ryu S, Lee WY. Visceral-to-Subcutaneous Abdominal Fat Ratio Is Associated with Nonalcoholic Fatty Liver Disease and Liver Fibrosis. Endocrinol Metab (Seoul). 2020; 35: 165–176. doi: 10.3803/EnM.2020.35.1.165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hernaez R, Lazo M, Bonekamp S, Kamel I, Brancati FL, Guallar E, et al. Diagnostic accuracy and reliability of ultrasonography for the detection of fatty liver: a meta-analysis. Hepatology. 2011; 54: 1082–1090. doi: 10.1002/hep.24452 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.McPherson S, Stewart SF, Henderson E, Burt AD, Day CP. Simple non-invasive fibrosis scoring systems can reliably exclude advanced fibrosis in patients with non-alcoholic fatty liver disease. Gut. 2010; 59: 1265–1269. doi: 10.1136/gut.2010.216077 [DOI] [PubMed] [Google Scholar]
- 45.Sookoian S, Pirola CJ. Systematic review with meta-analysis: the significance of histological disease severity in lean patients with nonalcoholic fatty liver disease. Aliment Pharmacol Ther. 2018; 47: 16–25. doi: 10.1111/apt.14401 [DOI] [PubMed] [Google Scholar]
- 46.Vernon G, Baranova A, Younossi ZM. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther. 2011; 34: 274–285. doi: 10.1111/j.1365-2036.2011.04724.x [DOI] [PubMed] [Google Scholar]
- 47.Pan JJ, Fallon MB. Gender and racial differences in nonalcoholic fatty liver disease. World J Hepatol. 2014; 6: 274–283. doi: 10.4254/wjh.v6.i5.274 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX)
(DOCX)
(DOCX)
(TIF)
Data Availability Statement
Data are available from the Kangbuk Samsung Health Study whose authors may be contacted through the corresponding author. Unfortunately, the data are not available to be shared publicly as we do not have IRB permission for distributing publicly the data (because public availability would compromise patient confidentiality or participant privacy). The IRB No. of our Study: KBSMC2020-05-019. For additional information, please visit the Kangbuk Samusng Health Study at http://kscs.kbsmc.co.kr/ or contact Gayoung Lim (gayoung.lim@samsung.com).