1. Introduction
On May 12, 2021, the governor of Ohio announced the Vax-a-Million COVID-19 Lottery (lottery) with five $1 million prizes for adults and five full scholarships for those ages 12–17 years to encourage Ohioans to receive the COVID-19 vaccine (total cost approximately $5.6 million) [1]. The lottery was a response to the declining rate of COVID-19 vaccinations among all Ohioans, in particular those in low-income counties. Evidence suggests COVID-19 vaccination rates are much lower in counties with household income less than $60,000 and lower educational attainments [2]. Two recent studies using data from the Centers for Disease Control and Prevention (CDC) found conflicting results regarding the effectiveness of the lottery [3,4]. We sought to clarify the conflicting lottery results using data directly from the state of Ohio and assess if low-income Ohioans were more likely to receive the COVID-19 vaccine as a consequence of the lottery.
2. Methods
The Ohio Department of Health COVID-19 Vaccination Dashboard was queried for all initial COVID-19 vaccinations administered by county and date from January 1 to June 30, 2021 [1]. Population, age, gender, proportion Black, and income data by county were obtained from the United States Census Bureau's American Community Survey [5]. Low-income counties were those in the bottom 25th percentile of median household income (22 of Ohio's 88 counties).
The expected number of COVID-19 vaccinations started were estimated with a trend line using a regression model with the COVID-19 vaccination data from May 12–28, 2021, was excluded. This was the period of increased COVID-19 vaccinations before reverting back to prevailing trends. The observed number of COVID-19 vaccinations, those reported by the Ohio Department of Health, was subtracted from the expected number of COVID-19 vaccinations, those estimated by our model after excluding the period of May 12–28, 2021, to determine the total number of COVID-19 vaccinations as a consequence of the lottery.
The second aim was addressed with a difference-in-difference (DiD) estimation to measure the change in the number of COVID-19 vaccinations in low-income counties while controlling for overall trends in the state of Ohio. The DiD controlled for age, population, and percent of population Black and Female.
All analyses were conducted using SPSS v27 (IBM Corporation Armonk, NY). The study was a retrospective analysis of de-identified data and deemed exempt from institutional review board review.
3. Results
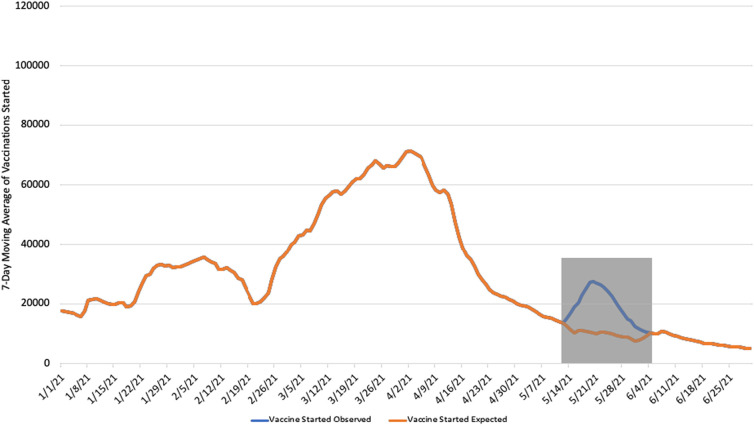
An estimated additional 213,288 individuals started their COVID-19 vaccination (Fig. 1 ) from May 12 to June 25, 2021, with the substantial majority occurring between May 13–28, 2021. During this time period, 104,386 newly eligible 12–15-year-olds received their first dose, resulting in net increase of 108,902 adult COVID-19 vaccinations [6]. The lottery, at a cost of approximately $5.6 million, cost the state approximately $52 per additional COVID-19 vaccination started.
Fig. 1.
COVID-19 Vaccines Started per Day: January 1 to June 25, 2021.
The 7-day moving average is displayed to remove the day-to-day variation in the number of vaccines started. The gray box represents the area in which the Observed and Expected number of vaccines started diverged as a result of the lottery program. 213,288 additional vaccinations started were observed during this period. Data from Ohio Department of Health COVID-19 Dashboard.
The DiD estimate for average number of COVID-19 vaccines started per day per low income county was 140.44 (95% confidence interval [CI] 133.37–147.89) pre-lottery and 165.92 (95% CI 147.80–186.26) post-lottery announcement. This increase of 25.48 COVID-19 vaccinations per low income county per day (95% CI 14.43–38.37; p 0.025) was statistically significant.
For comparison, a DiD model was performed for high income counties, those in the top 25 percentile (22 out of 88 counties). The results indicated a decrease of 19.24 COVID-19 vaccinations per high income county per day though the results were not statistically significant (95% CI 2.91–32.89; p 0.320).
4. Discussion
Our results confirm that the Ohio lottery was associated with an increase in COVID-19 vaccinations. Importantly, the increase was among Ohio's lower-income counties corresponding with a population who was less likely to receive the COVID-19 vaccine at the time of the lottery. Conversely, we did not see a corresponding increase in the number of COVID-19 vaccinations in high-income counties, possibly due to those individuals being more likely to have received the COVID-19 vaccine when first eligible [2]. Based on Ohio's published COVID-19 incidence, hospitalization, and mortality rate, 46 COVID-19 infections, 4 hospitalizations, and one death may have been avoided as a result of the lottery [1].
In contrast to Walkey et al. (2021), our results indicated that the Ohio lottery was associated with increased COVID-19 vaccinations in the adult population [3]. Further, despite using a different data source and statistical method, our results were very similar to the findings of Neil and Sehgal (2021). They estimated 114,553 additional adult COVID-19 vaccinations compared to our results of 108,902 [4]. These findings must be viewed in the context of limitations common to observational studies. Second, the publicly available data was limited to county level data and was augmented from the US Census rather than individual level data.
Our study in context with other published evidence suggested Ohio's lottery drove additional people to receive the COVID-19 vaccination. Whether or not lotteries are an effective incentive strategy for COVID-19 vaccinations depends on the additional benefits relative to the cost. Further research is necessary to examine the cost-effectiveness relative to other COVID-19 vaccination promotion programs to assess value.
Author contributions
All authors contributed to all aspects of the study.
Financial support
The authors did not receive any financial support for this study.
Data availability
Data will be made available upon reasonable request.
Conflicts of interest
The authors report no conflicts of interest with respect to this study.
References
- 1.Ohio Department of Health COVID-19 dashboard. 2021. https://www.bibguru.com/g/ama-websites-citation/ Published. (Accessed June 25, 2021)
- 2.Khubchandani J., Sharma S., Price J.H., Wiblishauser M.J., Sharma M., Webb F.J. COVID-19 vaccination hesitancy in the United States: A rapid national assessment. J Community Health. 2021;46(2):270–277. doi: 10.1007/s10900-020-00958-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Walkey A.J., Law A., Bosch N.A. Lottery-based incentive in Ohio and COVID-19 vaccination rates. JAMA. 2021 doi: 10.1001/jama.2021.11048. Published online July 02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Neil K.R., Sehgal A.B. Impact of Vax-A-Million lottery on COVID-19 vaccination rates in Ohio. Am J Med. 2021 doi: 10.1016/j.amjmed.2021.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.US Census Bureau American Community Survey (ACS) 2020. https://www.census.gov/programs-surveys/acs Published. (Accessed on May 25, 2021)
- 6.Ohio Governor'’s Office Ohio Governor Mike DeWine Week in Review – May 28, 2021. 2021. http://olc.org/wp-content/uploads/2021/06/Gov-DeWine-Week-in-Review-Ending-May-28.pdf (Accessed on July 20, 2021)
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Data will be made available upon reasonable request.