Abstract
Objective
The Asian American population in the U.S. comprises various, ethnically diverse subgroups. Traditionally, this population has been studied as a single, aggregated group, potentially masking differences in risk among subgroups. Analyses using disaggregated data can help better characterize the health needs of different Asian subpopulations and inform targeted, effective public health interventions. We assessed the prevalence of cardiovascular disease (CVD) risk factors and atherosclerotic CVD (ASCVD) and their associations with socioeconomic factors among Chinese, Asian Indian, Filipino and Other Asian subjects, compared with non-Hispanic White (NHW) subjects in the U.S.
Methods
: Cross-sectional study using data from 298,286 adults from the National Health Interview Survey (NHIS) from 2007 to 2018. We utilized chi-squared tests to compare characteristics across subgroups. Weighted proportions and unadjusted and adjusted logistic regression models were utilized to examine the associations between Asian subgroups, self-reported CVD risk factors and self-reported ASCVD, as well as between socioeconomic factors within each Asian subgroup.
Results
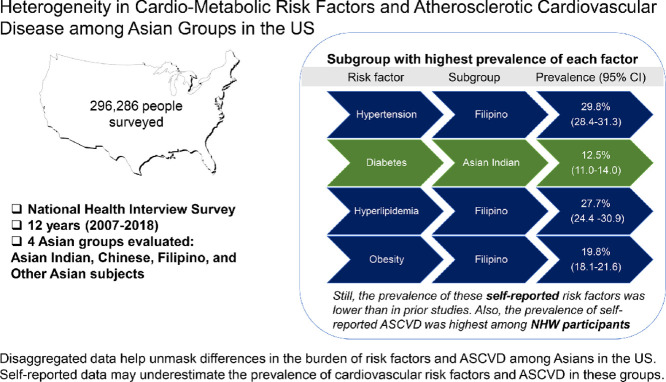
: Asian Indian subjects had the highest prevalence of diabetes (12.5%), while Filipino subjects had the highest prevalence of hyperlipidemia (27.7%), hypertension (29.8%) and obesity (19.8%). Despite this, the prevalence of self-reported ASCVD was lower in all Asian groups compared with NHWs. Chinese subjects had the lowest odds of having each of the CVD risk factors assessed.
Conclusion
: We found considerable heterogeneity in the distribution of risk factors as well as ASCVD among Asian subgroups in the US. Compared with health system or community-based reports, the prevalence of risk factors and ASCVD may be underestimated in some Asian NHIS subgroups. There is an urgent need for efforts to improve recruitment of Asian participants of heterogeneous socioeconomic backgrounds in national surveys, as well as to perform a thorough assessment of risk factors and disease in this population, not relying solely on self-report.
Keywords: Asian American, atherosclerotic cardiovascular disease, Filipino, Indian, ASCVD
Abbreviations: AHA, American Heart Association; ASCVD, atherosclerotic cardiovascular disease; CHD, coronary heart disease; CI, confidence interval; CVD, cardiovascular disease; NHIS, National Health Interview Survey; NHW, Non-Hispanic White; OR, odds ratio; US, United States
Graphical abstract
1. Introduction
The Asian population in the United States (US) is projected to reach nearly 34 million by 2050 [1, 2]. The population consists of many ethnically diverse subgroups with differences in cardiovascular disease (CVD) burden and risk factors. The 6 largest Asian subgroups – Asian Indians, Chinese, Filipinos, Japanese, Koreans, and Vietnamese – constitute nearly 84% of the Asian population in the US [3].
Prior studies have noted a higher prevalence and mortality from ischemic heart disease among Asian Indian and Filipino subjects, when compared with Non-Hispanic White (NHW) individuals [1, [4], [5], [6], [7], [8]]. However, national level data on CVD risk factors among individual ethnic subgroups have been limited due to the aggregation of Asian data in surveys [4, 5, 7, 9, 10]. Previous studies using data from the National Health Interview Survey (NHIS) noted significant heterogeneity in CVD risk between the different Asian subgroups [11, 12], however, these studies examined a small sample of Asian subjects in the US. Inadequate sampling of Asian American subgroups can lead to unreliable and invalid estimates, thereby inaccurately capturing key differences in disease prevalence [13]. A more recent study using NHIS data did not find an increased prevalence of multi-morbidity in Asian Indian and Chinese subjects compared to NHW individuals. However, the study did not assess individual risk factors or ASCVD prevalence [14].
Further, only a few studies have investigated the role of sociodemographic factors on atherosclerotic CVD (ASCVD) prevalence across individual subgroups, and yielded mixed results. The Filipino American Epidemiological Study (FACES) study, for example, did not find an association between education and income, and chronic physical health conditions [15, 16] whereas the National Latino and Asian American Study (NLAAS) study found that higher education levels and income were associated with a higher odds of having “good health” by the Self Rated Physical Health Scale [17]. The Mediators of Atherosclerosis in South Asians Living in America (MASALA) study generated important information on this topic in Asian Indian subjects. They found that Asian Indian immigrants who faced discrimination ate more unhealthy food and had a higher prevalence of depression [18, 19]. They also noted that Asian Indian subjects with a longer duration of stay in the US had higher levels of CVD risk factors and coronary artery calcium [20, 21].
We aimed to build on the findings of these studies by evaluating the effect of traditional- and migration-specific risk factors on cardiovascular health in a large, nationally representative dataset. In order to obtain a sufficiently large population for analyses, we used 12 years worth of data from the NHIS to study the prevalence of ASCVD, CVD risk factors, and their association with specific social determinants of health among different Asian subgroups in the US.
2. Methods
2.1. Setting
We utilized data from the NHIS (2007 to 2018), a cross-sectional household interview survey conducted annually by the National Center for Health Statistics under the auspices of the Centers for Disease Control and Prevention [22]. The NHIS collects standardized information on race, ethnicity, sex, primary language and, disability status, and is an important source of information on health disparities within the country. It is also offered in different languages, thereby increasing the accessibility to non- English speakers. The sample design, a multistage area probability sampling, adjusts for nonresponse, and further allows for national representativeness [23]. The survey consists of four core questionnaires: the household composition, the family core, the sample adult core, and the sample child core. The household section collects basic demographic and relationship information about all persons in the household. The family core collects data on basic sociodemographic characteristics, indicators of health status, activity limitations, injuries, insurance coverage, and access to and utilization of health services [24]. From each family, one sample child and one sample adult are randomly selected to gather further information. In this study, we used the sample adult file with supplementation of variables from other cores. Because of the de-identified nature and public availability of the NHIS, this study was considered exempt from the Institutional Review Board of Houston Methodist Hospital [25].
2.2. Study population
The analytical sample of this study included 298,286 adults aged 18 years and older, from the NHIS adult sample. Race/ethnicity was collected via self-report and for the purposes of this study, we studied only individuals that reported belonging to the following race/ethnicity subgroups: NHW (n = 276,986), Asian Indian (n = 4170), Chinese (n = 4455), and Filipino (n = 4944), and Other Asian (7731, including Korean, Vietnamese, Japanese, and other Asian subgroups). This methodology has previously been used to assess ethnic disparities in the NHIS [11].
2.3. CVD risk factors and ASCVD
Individual CVD risk factors were ascertained by self-report (hypertension, diabetes, high cholesterol, current smoker, obesity [body mass index (BMI) calculated by self-reported height and weight], and/or insufficient physical activity [based on whether individuals participated in <150 min per week of moderate-intensity aerobic physical activity, <75 min per week of vigorous-intensity aerobic physical activity, or a total combination of ≤150 min per week of moderate/vigorous-intensity aerobic physical activity]). Obesity was defined as a BMI ≥ 30 kg/m2. Coronary heart disease (CHD) status was also ascertained via self-report, and included a diagnosis of myocardial infarction, angina, or other CHD. ASCVD was ascertained based on a history of CHD and/or stroke.
2.4. Other relevant variables
Covariates in this study included age, sex, family income, education, insurance status, nativity, years in the US, English proficiency, and number of chronic co-morbidities. The following covariates were categorical and were modeled as follows: age (< 65 years and ≥ 65 years), sex (male or female), family income (defined as the ratio of income to the federal poverty level [FPL]: those < 200% of the FPL were classified as “low-income,” and those ≥ 200% of the FPL were classified as “middle/high-income”), education (high school/GED or less than high school, and some college or higher), insurance status (public, private, or uninsured), nativity (US- vs non-US born), years in the US, and English proficiency by self report (very well/well and not well/not at all). Self-reported chronic co-morbidities included emphysema, chronic obstructive pulmonary disease (COPD), asthma, gastrointestinal ulcer, cancer (any), arthritis (including rheumatoid arthritis, gout, fibromyalgia, systemic lupus erythematosus), and any kind of liver condition. These were aggregated and categorized as having 0, 1 or ≥ 2 co-morbidities.
2.5. Statistical analysis
The NHIS uses complex sampling techniques to select the sample. After adjusting for nonresponse, age, sex, and race/ethnicity (based on the population estimates produced by the 2000 and 2010 US Census Bureau [for years 2007 to 2011, and 2012 to 2018, respectively]), final person-level weights were created, which can then be used to provide national estimates. We described the prevalence of ASCVD and CVD risk factors as weighted proportions. Rao-Scott Chi squared tests were used to compare general characteristics, as well as the prevalence of CVD risk factors and ASCVD among the prespecified subgroups. Univariate and multivariable logistic regression models were utilized to examine the associations between individual CVD risk factors, and ASCVD within race/ethnicity. Explanatory variables included age, sex, family income, education, insurance status, nativity, years in US (if non-US born), English proficiency, region and chronic comorbidities. Variance estimation for the entire pooled cohort was obtained from the Integrated Public Use Microdata Series (http://www.ipums.org) [26]. All analyses were carried out using Stata®, version 16 (StataCorp, LP, College Station, Texas, USA), and were survey-specific, taking into consideration the NHIS complex survey design.
3. Results
3.1. Demographics of Asians in NHIS
The general characteristics of NHW and the four Asian subgroups are shown in Table 1. Overall, Asian subjects accounted for 6.4% of the surveyed population in NHIS, representing 13.1 million individuals during the study period, translating to the following subgroup distribution: Asian Indian (2.86 million), Chinese (2.66 million), Filipino (3.06 million) and Other Asian subjects (4.49 million). The individual, unweighted sample sizes categorized by year are shown in eTable 1. Asian Indian, Chinese, and Filipino subjects had a higher percentage of people with some college or higher level of completed education when compared with NHW. Filipino subjects also had the highest percentage of being US-born (35.4%), living in the US for ≥ 10 years if non-US born (79.6%), and had a high percentage of people proficient in English (93.9%). Whereas, Asian Indian subjects had a higher prevalence of non-US born persons who had lived in the US for < 10 years (38.2%).
Table 1.
General characteristics among Asian subgroups and NHW in the United States, from the National Health Interview Survey, 2007–18.
| White | Asian Indian | Chinese | Filipino | Other Asian | |
| Sample (N) | 276,986 | 4170 | 4455 | 4944 | 7731 |
| Weighted sample, (weighted %) | 189,804,561 (93.6) | 2865,239 (1.4) | 2659,035 (1.3) | 3058,291 (1.5) | 4487,141 (2.2) |
| Age Category, n (weighted %) | |||||
| < 65 years | 209,333 (80.5) | 3824 (92.0) | 3673 (85.5) | 3907 (83.4) | 6178 (85.3) |
| ≥ 65 years | 67,653 (19.5) | 346 (8.0) | 782 (14.5) | 1037 (16.6) | 1553 (14.7) |
| Sex, n (weighted %) | |||||
| Male | 125,966 (48.8) | 2300 (52.3) | 2031 (45.6) | 2107 (44.8) | 3488 (46.6) |
| Female | 151,020 (51.2) | 1870 (47.7) | 2424 (54.4) | 2837 (55.2) | 4243 (53.4) |
| Family Income, n (weighted %) | |||||
| Middle/High-income | 166,836 (71.8) | 2868 (79.7) | 2542 (69.2) | 3082 (75.3) | 4275 (64.9) |
| Low-income | 83,894 (28.2) | 926 (20.3) | 1427 (30.8) | 1342 (24.7) | 2651 (35.1) |
| Education, n (weighted %) | |||||
| Some College or Higher | 164,724 (60.5) | 3584 (84.5) | 3327 (75.1) | 3425 (72.3) | 5046 (66.8) |
| HS/GED or Less than HS | 111,071 (39.5) | 564 (15.5) | 1090 (24.9) | 1483 (27.7) | 2606 (33.2) |
| Insurance Status, n (weighted %) | |||||
| Public | 137,653 (56.4) | 3173 (76.6) | 2837 (66.7) | 2714 (62.4) | 4089 (58.5) |
| Private | 95,249 (29.6) | 542 (13.8) | 1079 (23.5) | 1414 (25.5) | 2270 (26.5) |
| White | Asian Indian | Chinese | Filipino | Other Asian | |
| Uninsured | 38,540 (14.0) | 390 (9.6) | 445 (9.9) | 627 (12.1) | 1155 (15.0) |
| Nativity, n (weighted %) | |||||
| US born | 235,178 (85.9) | 388 (8.4) | 962 (21.9) | 1800 (35.4) | 2343 (26.5) |
| Non-US born | 41,693 (14.1) | 3775 (91.6) | 3488 (78.1) | 3137 (64.6) | 5384 (73.5) |
| Years in US (if Non-US born), (weighted%) | |||||
| < 10 years | 7804 (19.6) | 1685 (38.2) | 1130 (28.1) | 640 (20.4) | 1302 (22.5) |
| ≥ 10 years | 33,292 (80.4) | 2061 (61.8) | 2308 (71.9) | 2459 (79.6) | 4036 (77.5) |
| English Proficiency, n (weighted %) | |||||
| Very well/Well | 130,040 (94.7) | 1940 (93.2) | 1574 (76.4) | 2170 (93.9) | 2743 (78.6) |
| Not well/Not at all | 7097 (5.3) | 116 (6.8) | 480 (23.6) | 152 (6.1) | 697 (21.4) |
| Region, n (weighted %) | |||||
| Northeast | 46,621 (17.9) | 985 (26.1) | 1075 (27.1) | 571 (13.2) | 1015 (15.1) |
| Midwest | 66,081 (24.7) | 778 (18.2) | 499 (10.5) | 449 (9.3) | 917 (12.8) |
| South | 92,486 (34.3) | 1294 (30.6) | 655 (14.7) | 927 (19.7) | 1587 (22.8) |
| West | 71,798 (23.1) | 1113 (25.1) | 2226 (47.6) | 2997 (57.8) | 4212 (49.3) |
| Hypertension, n (weighted %) | 89,349 (29.6) | 647 (17.1) | 889 (18.6) | 1648 (32.0) | 1915 (22.2) |
| Diabetes Mellitus, n (weighted %) | 26,627 (8.8) | 327 (8.9) | 215 (4.3) | 536 (10.7) | 640 (8.3) |
| High Cholesterol*, n (weighted %) | 7832 (28.5) | 106 (26.8) | 86 (19.1) | 133 (29.9) | 189 (26.1) |
| Smoke, n (weighted %) | 49,330 (17.8) | 255 (4.9) | 282 (5.9) | 632 (12.0) | 1001 (12.3) |
| White | Asian Indian | Chinese | Filipino | Other Asian | |
| Insufficient physical activity, n (weighted %) | 139,940 (50.2) | 1966 (48.6) | 2200 (50.8) | 2516 (51.6) | 4019 (53.1) |
| Obesity, n (weighted %) | 86,615 (31.1) | 482 (12.9) | 363 (7.8) | 980 (19.9) | 892 (12.1) |
| ASCVD, n (weighted %) | 26,735 (8.5) | 144 (3.3) | 169 (3.1) | 335 (6.3) | 415 (4.5) |
| Comorbidities, n (weighted %) | |||||
| 0 | 95,506 (57.6) | 2188 (81.2) | 2105 (77.4) | 1977 (64.3) | 3312 (74.7) |
| 1 | 50,162 (27.4) | 393 (15.2) | 477 (16.9) | 793 (26.2) | 940 (18.8) |
| ≥ 2 | 30,388 (15.1) | 96 (3.6) | 146 (5.6) | 314 (9.5) | 371 (6.5) |
Abbreviations: HS, high school; GED, general education development; US, United States.
P values < 0.001 for all categories except Insufficient physical activity (p value 0.003).
Comorbidities include emphysema, chronic obstructive pulmonary disease (COPD), asthma, gastrointestinal ulcer, cancer (any), arthritis (including rheumatoid arthritis, gout, fibromyalgia, systemic lupus erythematosus), and any kind of liver condition.
3.2. Prevalence of self-reported cardiovascular risk factors
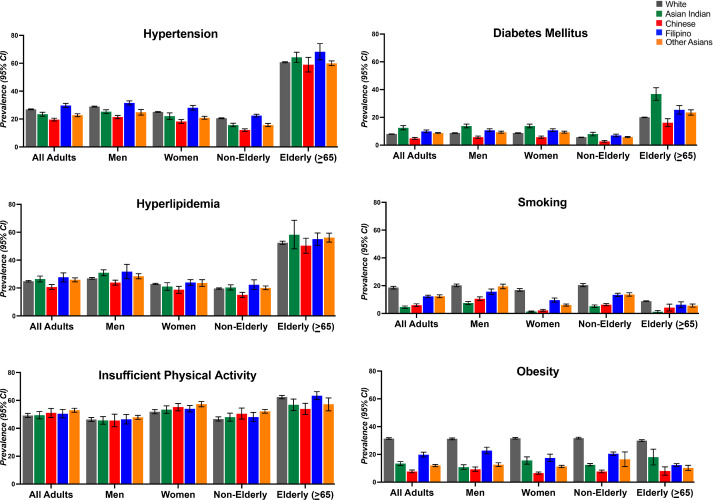
The age-adjusted prevalence of CVD risk factors among different ethnic subgroups is shown in Fig. 1. Among all Asian subgroups, Filipino subjects had the highest prevalence of hypertension (29.8%, 95% CI 28.4, 31.3), obesity (19.8%, 95% CI 18.1, 21.6), and hyperlipidemia (27.7%, 95% CI 24.4, 30.9) while Asian Indian subjects had the highest prevalence of diabetes (12.5%, 95% CI 11.0, 14.0). Across all Asian subgroups, men had a higher prevalence of hypertension, diabetes, hyperlipidemia, and smoking and women reported lower physical activity than men. Uniformly, adults >= 65 years of age had a higher prevalence of all CVD risk factors (hypertension, diabetes mellitus, high cholesterol, and insufficient physical activity), irrespective of race/ethnicity.
Fig. 1.
Central Illustration. Title: Age-adjusted distribution of cardiovascular risk factors in the National Health Interview Survey, 2007–18.
Abbreviations: CI = Confidence interval
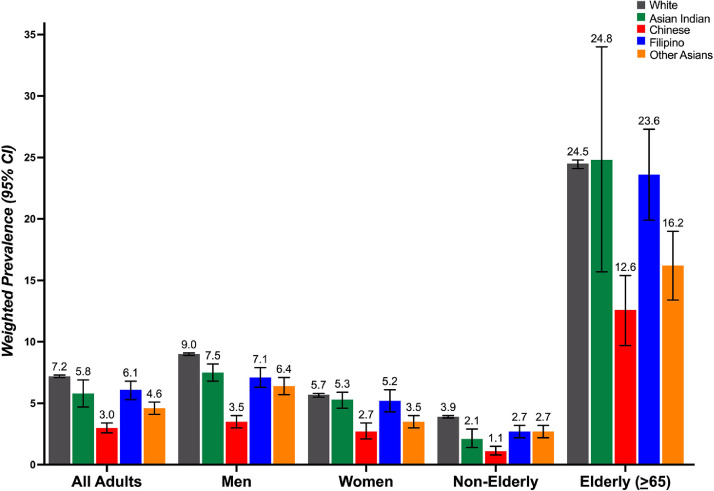
3.3. Prevalence of self-reported ASCVD
The age-adjusted prevalence of ASCVD, CHD, and stroke were highest among NHW compared with all Asian subgroups (Fig. 2, eTable 1 and eFigure1). Among the Asian subgroups, the prevalence of ASCVD in all adults was highest for Filipino subjects (6.1%, 95% CI 5.3, 6.8) followed by Asian Indian subjects (5.8%, 95% CI 4.7, 6.9) (Fig. 2). When stratified by sex and age, Asian Indian men; 7.5% (6.8, 8.2), Asian Indian women; 5.3% (4.6, 5.9), non-elderly Filipino subjects; 2.7% (2.2, 3.2), and elderly Asian Indian subjects; 24.8% (15.7, 34.0) had the highest prevalence of ASCVD in their respective categories (eTable 1). Chinese subjects had the lowest prevalence of ASCVD across all subgroups.
Fig. 2.
Title: Prevalence of age adjusted atherosclerotic cardiovascular disease in the National Health Interview Survey, 2007–18. Abbreviations: CI, Confidence interval.
3.4. Association between Asian subgroups and CVD risk factors and ASCVD
Logistic regression models examining the association between CVD risk factors and ASCVD in Asian subgroups are presented in Tables 1 and eTable 2. In our adjusted analyses, compared with NHW individuals, Filipino subjects had 1.82 (95% CI 1.65, 2.01) higher odds of reporting hypertension, 1.79 (95% CI 1.40, 2.30) higher odds of reporting diabetes, and 1.34 (95% CI 1.21, 1.47) higher odds of reporting insufficient physical activity. Asian Indian subjects had 1.71 (95% CI 1.47, 1.99) higher odds of reporting diabetes but had 46% lower odds of reporting current smoking (odds ratio [OR] 0.54, 95% CI 0.44, 0.66). Chinese subjects had lower odds of diabetes, when compared with NHW. All Asian subgroups had significantly lower odds of obesity when compared to NHW (Table 1).
Table 2.
Associations between Asian subgroups and odds of prevalent cardiovascular risk factors, compared to non-Hispanic Whites, from the National Health Interview Survey, 2007–18.
| Asian Indian | Chinese | Filipino | Other Asian | |
| Hypertension | ||||
| Model 1 | 0.49 (0.45, 0.53) | 0.54 (0.51, 0.58) | 1.12 (1.02, 1.23) | 0.68 (0.64, 0.72) |
| Model 2 | 0.59 (0.54, 0.64) | 0.57 (0.53, 0.61) | 1.21 (1.09, 1.34) | 0.72 (0.68, 0.77) |
| Model 3 | 1.07 (0.89, 1.30) | 0.88 (0.77, 1.00) | 1.82 (1.65, 2.01) | 1.11 (1.01, 1.23) |
| Diabetes Mellitus | ||||
| Model 1 | 1.00 (0.89, 1.13) | 0.46 (0.40, 0.54) | 1.23 (1.07, 1.42) | 0.93 (0.88, 0.99) |
| Model 2 | 1.23 (1.09, 1.39) | 0.50 (0.43, 0.59) | 1.32 (1.14, 1.53) | 1.02 (0.96, 1.08) |
| Model 3 | 1.71 (1.47, 1.99) | 0.64 (0.51, 0.81) | 1.79 (1.40, 2.30) | 1.24 (1.09, 1.41) |
| Smoking | ||||
| Model 1 | 0.24 (0.21, 0.27) | 0.29 (0.24, 0.35) | 0.63 (0.59, 0.67) | 0.65 (0.59, 0.70) |
| Model 2 | 0.22 (0.19, 0.24) | 0.28 (0.23, 0.34) | 0.62 (0.58, 0.66) | 0.62 (0.57, 0.68) |
| Model 3 | 0.54 (0.44, 0.66) | 0.71 (0.49, 1.04) | 1.05 (0.88, 1.25) | 1.23 (1.07, 1.43) |
| Obesity | ||||
| Model 1 | 0.33 (0.30, 0.36) | 0.19 (0.16, 0.22) | 0.55 (0.49, 0.62) | 0.30 (0.28, 0.33) |
| Model 2 | 0.32 (0.30, 0.35) | 0.19 (0.16, 0.22) | 0.55 (0.49, 0.61) | 0.30 (0.28, 0.33) |
| Model 3 | 0.46 (0.41, 0.52) | 0.22 (0.19, 0.26) | 0.72 (0.62, 0.83) | 0.38 (0.33, 0.43) |
| Insufficient physical activity | ||||
| Model 1 | 0.94 (0.88, 1.00) | 1.02 (0.92, 1.14) | 1.06 (0.94, 1.19) | 1.12 (1.08, 1.16) |
| Model 2 | 1.02 (0.95, 1.08) | 1.05 (0.94, 1.17) | 1.07 (0.95, 1.20) | 1.15 (1.11, 1.20) |
| Model 3 | 1.12 (1.00, 1.25) | 1.08 (0.96, 1.21) | 1.34 (1.21, 1.47) | 1.24 (1.14, 1.36) |
Results presented as odds ratios and 95% confidence intervals.
Note: 'Other Asians' includes Korean, Vietnamese, Japanese, and other Asian subgroups.
Reference = Non-Hispanic Whites.
Model 1 = Unadjusted.
Model 2 = Adjusted for age and sex.
Model 3 = Model 2 + Sociodemographic factors*.
*Family income, education, insurance status, nativity, years in US, English proficiency and region.
We further examined the association between Asian subgroups and CVD risk factors exclusively among Asian subjects using Asian Indian subjects as our reference group (eTable 4). In adjusted analysis, Filipino subjects were found to a have 1.70 (95% CI 1.27, 2.27) higher odds of hypertension compared with Asian Indian subjects. Moreover, Filipino subjects had a 1.34 (95% CI 1.16, 1.55) higher odds of reporting insufficient physical activity, and all Asian subgroups reported higher odds of current smoking when compared with Asian Indian subjects. Conversely, Chinese subjects had lower odds of reporting hypertension, diabetes, and obesity when compared with Asian Indian subjects.
When analyzing the association between prevalent ASCVD and race/ethnicity, we found that all Asian subgroups had lower odds for ASCVD when compared to NHW (Table 1). However, once we adjusted for age, sex, sociodemographic factors, comorbidities, and CVD risk factors (Table 1), we found no statistically significant difference in the odds of ASCVD between Asian subgroups and NHW respondents. Predictors of ASCVD for Asian subgroups and NHW are shown in eTable 3.
Table 3.
Associations between Asian subgroups and odds of prevalent ASCVD, compared to non-Hispanic Whites, from the National Health Interview Survey, 2007–18.
| Asian Indian | Chinese | Filipino | Other Asian | |
| Model 1 | 0.36 (0.32, 0.42) | 0.35 (0.30, 0.40) | 0.73 (0.64, 0.83) | 0.51 (0.44, 0.60) |
| Model 2 | 0.49 (0.44, 0.55) | 0.38 (0.33, 0.44) | 0.79 (0.70, 0.90) | 0.57 (0.50, 0.66) |
| Model 3 | 1.04 (0.82, 1.31) | 0.77 (0.59, 1.01) | 1.39 (1.06, 1.81) | 0.94 (0.75, 1.19) |
| Model 4 | 1.07 (0.84, 1.35) | 0.81 (0.61, 1.07) | 1.20 (0.93, 1.55) | 0.85 (0.68, 1.06) |
Results presented as odds ratios and 95% confidence intervals.
Note: 'Other Asians' includes Korean, Vietnamese, Japanese, and other Asian subgroups.
Reference = Non-Hispanic Whites.
Model 1 = Unadjusted.
Model 2 = Adjusted for age and sex.
Model 3 = Model 2 + Socio-demographic factors*.
Model 4 = Model 3 + Cardiovascular risk factors (hypertension, diabetes, obesity, high cholesterol, insufficient physical activity and tobacco use.
4. Discussion
In this nationally representative sample of US adults from 2007 to 2018, we found considerable heterogeneity in the distribution of cardiovascular risk factors among Asian Americans. Given the abundance of prior literature that aggregated diverse Asian subgroups into a single group, we believe our analysis provides robust and more nuanced estimates on associations between sociodemographic characteristics and CVD risk factors and ASCVD across Asian subgroups.
Filipino individuals constitute the third largest Asian subgroup in the US [27]. In our analysis, they had a high prevalence of hypertension, comparable to that of NHW. This is congruent with prior reports in this subgroup [11, [28], [29], [30], [31]]. The prevalence, however, was lower than reports where blood pressure was measured in participants. For example, a clinic-based report in California and a community screening-based report from New York City, both reported a >50% prevalence of hypertension in their population, as opposed to only 30% prevalence identified by self-report in this analysis [31, 32]. Our estimate was similar to prior reports using NHIS data (self-report), suggesting that hypertension remains a largely undetected risk factor in Filipino subjects [11]. Similarly, the University of California San Diego Filipino Health Study found that 71% of CVD cases in Filipina women were previously undiagnosed [33].
The excess risk of hypertension and diabetes in the Filipino population may be related to differences in metabolism, independent of body mass index [34]. However, a significant proportion of risk is influenced by health behaviors with high rates of smoking, stress, high alcohol consumption, and a high sodium diet being reported in this population [35]. These behaviors are in turn influenced by cultural factors such as acculturation and social support, but also socioeconomic factors like health insurance coverage [36]. Many studies, including ours, have found that Filipino individuals follow lower than recommended levels of physical activity, a well-known contributor to both diabetes and hypertension [11, 37]. They also have been found to have poor disease management with suboptimal medical adherence, and a limited knowledge of disease processes [30, [38], [39], [40]]. Community interventions that aim to improve risk factor detection, awareness, and encourage healthy behavior have the potential to improve disease self-management in this population.
Among Asian Indian subjects, the rates of diabetes were the highest across all subgroups, with a prevalence of 12–14%, similar to the CDC national diabetes report [41]. However, it was markedly lower than the 23% prevalence reported from the National Health and Nutrition Examination Survey (NHANES), and the 26% prevalence reported in a recent health system-based report from California. Both these studies measured blood glucose levels and hemoglobin A1c [42] [43]. This would suggest that many diabetics are indeed unaware of their disease status, a finding that was also noted among Asian subjects in NHANES [42]. Our estimated prevalence of ASCVD in Asian Indian subjects was also lower (5.8%) than previously described using other sources of data, such as electronic health records, with rates up to 8.3% being reported in this group [44], [45], [46]. In contrast with various prior studies, we also did not find Asian Indians to have a higher prevalence of ASCVD compared with NHW adults [43]. It is possible that self-reporting underestimates ASCVD prevalence due to poor access to health care and consequent under-diagnosis in migrant communities [47] [48].
Importantly, in Asian Indians, besides potential under-detection of cardiovascular risk factors and ASCVD, it should also be noted that multiple studies, including INTERHEART as well as recent research in Europe, suggest that Asian Indians may be a lower-risk South Asian subgroup compared with Pakistanis and Bangladeshis [49] [50] [51]. Unfortunately, disaggregated data for Pakistanis and Bangladeshis is currently not available in NHIS. Dedicated studies in these two large, rapidly growing groups in the U.S. are needed to better understand their burden of cardiovascular disease, risk factors, and upstream cultural and socioeconomic factors potentially leading to an excess ASCVD risk in these groups. An upcoming expansion of the MASALA study will recruit additional 600 Bangladeshi and 550 Pakistani participants from the New York and Chicago between years 2021 and 2024, and will be well poised to fill prevailing knowledge gaps in these groups in the U.S.
The “healthy immigrant effect” has been proposed as reason for immigrants being healthier than their local counterparts at the time of migration [52]. However, immigrants often lose this advantage with an increasing number of years of residence in the US [21]. Various sociodemographic factors have been identified as potentially contributing to this effect. Our study examined some of these factors. We identified poor English proficiency, low income, and low educational attainment to be predictive of increased ASCVD risk in the total population. Indeed, a lack of access to health care is a key determinant of risk factor burden and health outcomes in the general population. This may be particularly true for immigrants, most notably in first-generation immigrants. Language barriers, difficulty navigating an unfamiliar healthcare system, and concerns regarding the cost of care add to the burden of obtaining CVD preventive care [53].
Finally, we also aimed to provide an estimate of the association between ethnicity and outcomes independent of traditional and sociodemographic risk factors. We found that differences between some Asian subgroups, particularly for Filipinos, remained strong and statistically significant after adjusting for demographics and a variety of socioeconomic variables. Although residual confounding by poorly or un-measured socioeconomic characteristics is a possibility, this finding suggests that other factors, such as culture, may play a role in the observed differences between groups. Further research is needed to understand the upstream mechanisms of these differences across Asian subgroups.
4.1. Study limitations
As described above, underestimation of risk factors and ASCVD among Asian immigrant subgroups is a potentially important limitation of analyses using national surveys. By using self-reported disease alone, the data obtained are dependent upon adequate access to care for diagnosis, as well as adequate health literacy, hence creating inherent selection and information biases [54, 55]. The cross-sectional nature of these data also precludes examination of changes in disease incidence and prevents assessments of premature CVD deaths, which may be a large issue particularly in subgroups affected by a high burden of premature ASCVD events, such as Asian Indians. Another limitation of cross-sectional studies is that causality cannot be established from the data. These issues from national surveys are particularly noteworthy given that they are often used to describe health statistics among at-risk subgroups, inform public health interventions, and make decisions on health resource allocation. An underestimation of ASCVD risk and/or prevalence may lead to a insufficient preventive efforts in Asian groups. As demonstrated in the recent NHANES analysis, there is a need for a thorough evaluation of risk factors in individual Asian subgroups using measurements other than self-reported data [42]. Further, using a BMI cut-off of ≥ 30 kg/m2 to define obesity likely underestimated the prevalence of obesity in Asian American subjects. Despite this potential for underestimation, some signals were particularly clear from our study. For example, the increased prevalence of hypertension in Filipino subjects and diabetes in Asian Indian subjects have been noted consistently and should be used to further develop tailored public health interventions targeting these subgroups.
To achieve a sufficiently large number of Asian NHIS participants in the analysis, we had to pool 12 years of survey data. We also did not have sufficient sample size to independently study other high risk subgroups like Bangladeshi subjects [56]. This highlights the issue of underrepresentation of Asian subgroups in national surveys and the need to resolve this moving forward. There are multiple barriers to Asian participation in clinical and epidemiological research: lack of access, distrust of physicians and medical research, and issues of language and racial discrimination. [57]. Our findings also highlight the pitfalls of using aggregated data for Asian subjects in national surveys and epidemiological studies, an approach that assumes within-group homogeneity among Asians.
5. Conclusion
Asian Americans represent a heterogeneous group with varying risk factor profiles, and preventive interventions need to account for such differences. Disaggregated data from national surveys can help characterize these differences in risk; however, self-reported data may markedly underestimate risk in some Asian subgroups.
Declaration of Conflicts of Interest
Dr. Nasir is on the advisory board of Amgen, Novartis, Medicines Company, and his research is partly supported by the Jerold B. Katz Academy of Translational Research. Dr. Virani's research is supported by the Department of Veterans Affairs, World Heart Federation, and Tahir and Jooma Family, and receives honoraria from the American College of Cardiology as Associate Editor for Innovations (acc.org). No other conflicts of interest relevant to the content of this manuscript were reported by the authors.
Author contributions
PS, MS, MC-A and KN participated in the conception, planning, design, and interpretation of the data, and on the drafting of the manuscript. PS and MS prepared the figures. GG and JV-E interpreted the data, conducted statistical analysis and participated in drafting the manuscript. AK, SV, BH, RM, TY, HZ and ZJ participated in the interpretation of the data and revised the manuscript critically for important intellectual content. PS, MS and KN are responsible for the overall content as guarantors.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ajpc.2021.100219.
Appendix. Supplementary materials
References
- 1.Jose P.O., Frank A.T.H., Kapphahn K.I. Cardiovascular disease mortality in Asian Americans. J Am Coll Cardiol. 2014;64(23):2486–2494. doi: 10.1016/j.jacc.2014.08.048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Passel J.S., Cohn D. Pew Research Center Washington; DC: 2008. US population projections, 2005-2050. [Google Scholar]
- 3.Bureau. USC: Selected Population Profile in the United States . American Community Survey 1-year estimates; 2010. Asian alone by selected groups. [Google Scholar]
- 4.Palaniappan L., Wang Y., Fortmann S.P. Coronary heart disease mortality for six ethnic groups in California, 1990–2000. Ann Epidemiol. 2004;14(7):499–506. doi: 10.1016/j.annepidem.2003.12.001. [DOI] [PubMed] [Google Scholar]
- 5.Wild S.H., Laws A., Fortmann S.P., Varady A.N., Byrne C.D. Mortality from coronary heart disease and stroke for six ethnic groups in California, 1985 to 1990. Ann Epidemiol. 1995;5(6):432–439. doi: 10.1016/1047-2797(95)00058-5. [DOI] [PubMed] [Google Scholar]
- 6.Marmot M.G., Syme S.L., Kagan A., Kato H., Cohen J.B., Belsky J. Epidemiologic studies of coronary heart disease and stroke in Japanese men living in Japan, Hawaii and California: prevalence of coronary and hypertensive heart disease and associated risk factors. Am J Epidemiol. 1975;102(6):514–525. doi: 10.1093/oxfordjournals.aje.a112189. [DOI] [PubMed] [Google Scholar]
- 7.Fang J., Madhavan S., Alderman M.H. Cardiovascular mortality of Chinese in New York City. J Urban Health. 1999;76(1):51–61. doi: 10.1007/BF02344461. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Volgman A.S., Palaniappan L.S., Aggarwal N.T. Atherosclerotic cardiovascular disease in South Asians in the United States: epidemiology, risk factors, and treatments: a scientific statement from the American Heart Association. Circulation. 2018;138(1):e1–e34. doi: 10.1161/CIR.0000000000000580. [DOI] [PubMed] [Google Scholar]
- 9.Hastings K.G., Jose P.O., Kapphahn K.I. Leading causes of death among Asian American subgroups (2003–2011) PLoS ONE. 2015;10(4) doi: 10.1371/journal.pone.0124341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Benfante R. Studies of cardiovascular disease and cause-specific mortality trends in Japanese-American men living in Hawaii and risk factor comparisons with other Japanese populations in the Pacific region: a review. Hum. Biol. 1992:791–805. [PubMed] [Google Scholar]
- 11.Ye J., Rust G., Baltrus P., Daniels E. Cardiovascular risk factors among Asian Americans: results from a National Health Survey. Ann Epidemiol. 2009;19(10):718–723. doi: 10.1016/j.annepidem.2009.03.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barnes P.M., Adams P.F., Powell-Griner E. Health characteristics of the Asian adult population: united States, 2004–2006. Adv Data. 2008;394(394):1–22. [PubMed] [Google Scholar]
- 13.Holland A.T., Palaniappan L.P. Problems with the collection and interpretation of Asian-American health data: omission, aggregation, and extrapolation. Ann Epidemiol. 2012;22(6):397–405. doi: 10.1016/j.annepidem.2012.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhang Y., Misra R., Sambamoorthi U. Prevalence of Multimorbidity among Asian Indian, Chinese, and Non-Hispanic White Adults in the United States. Int J Environ Res Public Health. 2020;17(9):3336. doi: 10.3390/ijerph17093336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.De Castro A.B., Gee G.C., Takeuchi D.T. Job-related stress and chronic health conditions among Filipino immigrants. J Immigrant Minority Health. 2008;10(6):551–558. doi: 10.1007/s10903-008-9138-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.De Castro A.B., Gee G.C., Takeuchi D.T. Workplace discrimination and health among Filipinos in the United States. Am J Public Health. 2008;98(3):520–526. doi: 10.2105/AJPH.2007.110163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.De Castro A.B., Gee G.C., Takeuchi D.T. Examining alternative measures of social disadvantage among Asian Americans: the relevance of economic opportunity, subjective social status, and financial strain for health. J Immigrant Minority Health. 2010;12(5):659–671. doi: 10.1007/s10903-009-9258-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Nadimpalli S., Keita A., Wang J. Are experiences of discrimination related to poorer dietary intakes among South Asians in the MASALA study? J Nutr Educ Behav. 2017;49(10):872–876. doi: 10.1016/j.jneb.2017.07.013. e871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Needham B.L., Mukherjee B., Bagchi P. Acculturation strategies and symptoms of depression: the Mediators of Atherosclerosis in South Asians Living in America (MASALA) Study. J Immigrant Minority Health. 2018;20(4):792–798. doi: 10.1007/s10903-017-0635-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Talegawkar S.A., Kandula N.R., Gadgil M.D., Desai D., Kanaya A.M. Dietary intakes among South Asian adults differ by length of residence in the USA. Public Health Nutr. 2016;19(2):348–355. doi: 10.1017/S1368980015001512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kanaya A.M., Ewing S.K., Vittinghoff E. Acculturation and Subclinical Atherosclerosis among US South Asians: findings from the MASALA study. J Clin Exp Res Cardiol. 2014;1(1) [PMC free article] [PubMed] [Google Scholar]
- 22.About NHIS [https://http://www.cdc.gov/nchs/nhis/about_nhis.htm] 2021
- 23.Lawton J., Ahmad N., Hanna L., Douglas M., Hallowell N. ‘I can't do any serious exercise’: barriers to physical activity amongst people of Pakistani and Indian origin with Type 2 diabetes. Health Educ Res. 2006;21(1):43–54. doi: 10.1093/her/cyh042. [DOI] [PubMed] [Google Scholar]
- 24.NHIS Data, Questionnaires and Related Documentation [https://http://www.cdc.gov/nchs/nhis/data-questionnaires-documentation.htm]
- 25.Bhopal R., Unwin N., White M. Heterogeneity of coronary heart disease risk factors in Indian, Pakistani, Bangladeshi, and European origin populations: cross sectional study. BMJ. 1999;319(7204):215–220. doi: 10.1136/bmj.319.7204.215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Blewett L., Rivera Drew J., Griffin R., King M., Williams K. University of Minnesota; Minneapolis: 2016. IPUMS health surveys: national health interview survey, version 6.2. in. [Google Scholar]
- 27.Bureau U.S.C. United States Census Bureau; Washington (DC): 2017. American community survey (ACS): data releases in. [Google Scholar]
- 28.Klatsky A.L., Tekawa I.S., Armstrong M.A. Cardiovascular risk factors among Asian Americans. Public Health Rep. 1996;111(Suppl 2):62. [PMC free article] [PubMed] [Google Scholar]
- 29.Angel A., Armstrong M.A., Klatsky A.L. Blood pressure among Asian-Americans living in northern California. Am J Cardiol. 1989;64(3):237–240. doi: 10.1016/0002-9149(89)90468-2. [DOI] [PubMed] [Google Scholar]
- 30.Stavig G.R., Igra A., Leonard A.R. Hypertension and related health issues among Asians and Pacific Islanders in California. Public Health Rep. 1988;103(1):28. [PMC free article] [PubMed] [Google Scholar]
- 31.Ursua R.A., Islam N.S., Aguilar D.E. Predictors of hypertension among Filipino immigrants in the Northeast US. J Community Health. 2013;38(5):847–855. doi: 10.1007/s10900-013-9689-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zhao B., Jose P.O., Pu J. Racial/ethnic differences in hypertension prevalence, treatment, and control for outpatients in northern California 2010–2012. Am J Hypertens. 2015;28(5):631–639. doi: 10.1093/ajh/hpu189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Magno C.P., Araneta M.R., Macera C.A., Anderson G.W. Cardiovascular disease prevalence, associated risk factors, and plasma adiponectin levels among Filipino American women. Ethn Dis. 2008;18(4):458–463. [PubMed] [Google Scholar]
- 34.Araneta M.R. Engaging the ASEAN Diaspora: type 2 Diabetes Prevalence, Pathophysiology, and Unique Risk Factors among Filipino Migrants in the United States. J ASEAN Feder Endocrine Soc. 2019;34(2):127–133. doi: 10.15605/jafes.034.02.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Abesamis C.J., Fruh S., Hall H., Lemley T., Zlomke K.R. Cardiovascular health of Filipinos in the United States: a review of the literature. J Transcult Nursing. 2016;27(5):518–528. doi: 10.1177/1043659615597040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lo C.C., Yang P.Q., Cheng T.C. Ash-Houchen W. Explaining Health Outcomes of Asian Immigrants: does Ethnicity Matter? J Racial Ethn Health Disparities. 2020;7(3):446–457. doi: 10.1007/s40615-019-00673-x. [DOI] [PubMed] [Google Scholar]
- 37.Uchima O., Wu Y.Y., Browne C., Braun K.L. Peer Reviewed: disparities in Diabetes Prevalence Among Native Hawaiians/Other Pacific Islanders and Asians in Hawai ‘i. Prev Chronic Dis. 2019;16 doi: 10.5888/pcd16.180187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Grandinetti A., Chang H.K., Theriault A., Mor J. Metabolic syndrome in a multiethnic population in rural Hawaii. Ethn Dis. 2005;15(2):233–237. [PubMed] [Google Scholar]
- 39.Smith Jr S.C., Clark L.T., Cooper R.S. Discovering the full spectrum of cardiovascular disease: minority Health Summit 2003: report of the Obesity, Metabolic Syndrome, and Hypertension Writing Group. Circulation. 2005;111(10):e134–e139. doi: 10.1161/01.CIR.0000157743.54710.04. [DOI] [PubMed] [Google Scholar]
- 40.Taira D.A., Gelber R.P., Davis J., Gronley K., Chung R.S., Seto T.B. Antihypertensive adherence and drug class among Asian Pacific Americans. Ethnicity Health. 2007;12(3):265–281. doi: 10.1080/13557850701234955. [DOI] [PubMed] [Google Scholar]
- 41.Centers for Disease Control and Prevention. Centers for Disease Control and Prevention, US Department of Health and Human Services; Atlanta, GA: 2020. National diabetes statistics report, 2020. [Google Scholar]
- 42.Cheng Y.J., Kanaya A.M., Araneta M.R.G. Prevalence of diabetes by race and ethnicity in the United States, 2011-2016. JAMA. 2019;322(24):2389–2398. doi: 10.1001/jama.2019.19365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pursnani S., Merchant M. South Asian ethnicity as a risk factor for coronary heart disease. Atherosclerosis. 2020:126–130. doi: 10.1016/j.atherosclerosis.2020.10.007. [DOI] [PubMed] [Google Scholar]
- 44.Gordon N.P., Lin T.Y., Rau J., Lo J.C. Aggregation of Asian-American subgroups masks meaningful differences in health and health risks among Asian ethnicities: an electronic health record based cohort study. BMC Public Health. 2019;19(1):1551. doi: 10.1186/s12889-019-7683-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Enas E.A., Garg A., Davidson M.A., Nair V.M., Huet B.A., Yusuf S. Coronary heart disease and its risk factors in first-generation immigrant Asian Indians to the United States of America. Indian Heart J. 1996;48(4):343–353. [PubMed] [Google Scholar]
- 46.Holland A.T., Wong E.C., Lauderdale D.S., Palaniappan L.P. Spectrum of cardiovascular diseases in Asian-American racial/ethnic subgroups. Ann Epidemiol. 2011;21(8):608–614. doi: 10.1016/j.annepidem.2011.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Narayan K.M.V., Aviles-Santa L., Oza-Frank R. Report of a National Heart, Lung, and Blood Institute Workshop: heterogeneity in cardiometabolic risk in Asian Americans in the US: opportunities for research. J. Am. Coll. Cardiol. 2010;55(10):966–973. doi: 10.1016/j.jacc.2009.07.075. [DOI] [PubMed] [Google Scholar]
- 48.Palaniappan L.P., Araneta M.R.G., Assimes T.L. Call to action: cardiovascular disease in Asian Americans: a science advisory from the American Heart Association. Circulation. 2010;122(12):1242–1252. doi: 10.1161/CIR.0b013e3181f22af4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Joshi P., Islam S., Pais P. Risk factors for early myocardial infarction in South Asians compared with individuals in other countries. JAMA. 2007;297(3):286–294. doi: 10.1001/jama.297.3.286. [DOI] [PubMed] [Google Scholar]
- 50.Satish P., Vela E., Bilal U. Burden of cardiovascular risk factors and disease in five Asian groups in Catalonia: a disaggregated, population-based analysis of 121 000 first-generation Asian immigrants. Eur J Prev Cardiol. 2021 doi: 10.1093/eurjpc/zwab074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Hippisley-Cox J., Coupland C. Development and validation of risk prediction equations to estimate survival in patients with colorectal cancer: cohort study. BMJ. 2017:357. doi: 10.1136/bmj.j2497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Koya D.L., Egede L.E. Association between length of residence and cardiovascular disease risk factors among an ethnically diverse group of United States immigrants. J Gen Intern Med. 2007;22(6):841–846. doi: 10.1007/s11606-007-0163-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Cainzos-Achirica M., Nasir K. Suboptimal management of cardiovascular risk factors among Non-US-citizen immigrants: time to build a healthier immigrant Workforce in the United States. In.: Circulation: Cardiovascuar Qual Outcomes; 2020 doi: 10.1161/CIRCOUTCOMES.120.006498. [DOI] [PubMed] [Google Scholar]
- 54.Weisskopf M.G., Sparrow D., Hu H., Power M.C. Biased exposure–health effect estimates from selection in cohort studies: are environmental studies at particular risk? Environ Health Perspect. 2015;123(11):1113–1122. doi: 10.1289/ehp.1408888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Chaix B., Billaudeau N., Thomas F. Neighborhood effects on health: correcting bias from neighborhood effects on participation. Epidemiology. 2011:18–26. doi: 10.1097/EDE.0b013e3181fd2961. [DOI] [PubMed] [Google Scholar]
- 56.Vasudev R., Shah P., Patel J. Should Bangladeshi race be considered as an independent risk factor for multi vessel coronary artery disease? Vasc Health Risk Manag. 2020;16:143. doi: 10.2147/VHRM.S233303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Albert M.A. Inflammatory biomarkers, race/ethnicity and cardiovascular disease. Nutr. Rev. 2007;65(suppl_3):S234–S238. doi: 10.1111/j.1753-4887.2007.tb00369.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.