Highlights
-
•
Investigation of social determinants and atrial fibrillation (AF) is limited.
-
•
We measured income, education, and hospitalizations in a cohort (n = 339) with AF.
-
•
Social determinants were related to hospitalization events over median 2.6-years.
-
•
Addressing social determinants of health may reduce adverse events in AF.
Keywords: Atrial fibrillation, Hospitalization, Risk, Education, Income
Abstract
Objective
Social determinants contribute to adverse outcomes in cardiovascular and non-cardiovascular conditions. However, their investigation in atrial fibrillation (AF) remains limited. We examined the associations between annual income and educational attainment with risk of hospitalization in individuals with AF receiving care in a regional health care system. We hypothesized that individuals with lower income and lower education would have an increased risk of hospitalization.
Methods
We enrolled a cohort of individuals with prevalent AF from an ambulatory setting. We related annual income (≤$19,999/year; $20,000–49,000/year; $50,000–99,999/year; ≥$100,000/year) and educational attainment (high school/vocational; some college; Bachelor's; graduate) to hospitalization events in multivariable-adjusted Cox proportional hazards models, using the Andersen-Gill model to account for the potential of participants to have multiple events.
Results
In 339 individuals with AF (age 72.3 ± 10.1 years; 43% women) followed for median 2.6 years (range 0–3.4 years), we observed 417 hospitalization events. We identified an association between both income and educational attainment and hospitalization risk. In multivariable-adjusted analyses which included educational attainment individuals in the lowest annual income category (≤19,999/year) had 2.0-fold greater hospitalization risk than those in the highest (≥100,000/year; 95% Confidence Interval [CI] 1.08–4.09; p = 0.03). In multivariable-adjusted analyses without adjustment for income, those in the lowest educational attainment category (high school/vocational) had a 2-fold increased risk of hospitalization relative to the highest (graduate-level; 95% CI 1.12–3.54, p = 0.02). However, this association between education and events was attenuated with further adjustment for income (95% CI 0.97–3.15, p = 0.06).
Conclusions
We identified relationships between income and education and prospective risk of hospitalization risk in AF. Our findings support the consideration of social determinants in evaluating and treating socioeconomically disadvantaged individuals with AF to reduce hospitalization risk.
Graphical abstract
1. Introduction
Atrial fibrillation (AF) is a common cardiac arrhythmia, often associated with both cardiovascular and non-cardiovascular complications. The rising prevalence of AF contributes to the severe social and financial burdens associated with the condition that include increasing rates of hospitalizations and subsequent health care expenditures [[1], [2], [3], [4]]. Social determinants of health are pertinent to AF, given their potential to challenge health care access, complicate adherence, and increase the risk of associated health outcomes. Social determinants of health have been widely studied in cardiovascular disease, with studies showing consistent associations between income and educational attainment, and health outcomes [5,6]. Low income has been related to increased risk of developing AF and subsequent adverse outcomes such as myocardial infarction and heart failure [7,8]. Conversely, higher educational attainment has been associated with reduced cardiovascular disease such as myocardial infarction, heart failure, and cerebrovascular disease [6,9]. A recent comprehensive meta-analysis identified educational attainment as having predominantly beneficial effects on health across numerous health outcomes, including cardiovascular risk factors and disease [10].
In contrast, there has been limited investigation into how income and educational attainment affect health outcomes in individuals with AF [11]. We investigated the association between annual income and educational attainment with risk of hospitalization in a cohort with prevalent AF. Unplanned hospitalization is common in individuals with AF, and has a high toll on patient well-being. Furthermore, unplanned hospitalizations, cardiovascular or non-cardiovascular, may be financially destabilizing, especially for individuals with limited expendable income. As such, hospitalization may result in unmeasured adversity to socially disadvantaged patients. We hypothesized that individuals with lower income and lower educational attainment would experience increased hospitalization risk than those with higher income and educational attainment.
2. Methods
We prospectively enrolled individuals receiving care for AF at the University of Pittsburgh Medical Center (UPMC), a large regional healthcare system in Pittsburgh, Pennsylvania. We identified eligible participants from the electronic health record and by direct contact at ambulatory visits, referral by a physician or other care provider, and self-referral via a web-based clinical research portal. Eligibility criteria for the study included age ≥18 years, a documented history of non-valvular AF and a CHA2DS2-VASc (congestive heart failure, hypertension, age, diabetes, stroke/transient ischemic attack, valvular disease [history of myocardial infarction, peripheral vascular disease, or aortic atherosclerotic disease], and sex category) score ≥2 [12].
Participants must have been prescribed oral anticoagulants for ischemic stroke prevention of AF. The rationale for this criterion was that such patients are distinguished as receiving active treatment for AF. Participants were required to speak adequate English to provide informed consent and participate in this research protocol. Exclusion criteria were AF secondary to non-cardiac issues as determined from chart review, a history of ischemic and hemorrhagic stroke, having been diagnosed with AF within 30 days of cardiothoracic surgery, or an inability to pass a three-item screening instrument to assess orientation. From 2016 to 2018, we approached 486 individuals at clinical visits as a convenience cohort and invited them to participate. A final cohort of 339 individuals enrolled in the study. Those individuals not enrolled either declined participation or were not approached as part of a clinical visit.
Demographics, including age, sex, and race were self-reported. Body mass index was obtained from the medical record. Clinical history, such as a history of congestive heart failure, hypertension, diabetes, stroke/transient ischemic attack, and valvular disease, were obtained from a combination of self-report and review of the medical records [13,14]. Cigarette smoking status was ascertained by self-report and classified as current, former, or never.
We ascertained annual household income by self-report and categorized income as less than $19,999, $20,000–$49,000, $50,000–$99,999, or greater than $100,000 per year. Educational attainment was categorized as the highest level of education completed among high school or vocational degree, some college, Bachelor's degree, or graduate degree. We elected to assess both income and education because of their separate and unique contributions to health outcomes.
In the current study, hospitalization refers to all-cause hospitalization. Hospitalization was ascertained by review of the UPMC longitudinal electronic health record with events defined by hospital admission for at least 24 continuous hours. Elective procedures were distinguished from hospitalizations and not considered as hospitalization events. Individual follow-up extended from the date of study enrollment to the last date of contact with UPMC as documented in the electronic health record through March 16, 2020, or date of death as identified by the electronic health record. During the study period, all hospitalization events were ascertained, thereby recording more than 1 event per participant.
We summarized continuous variables by their distributions (mean±standard deviation) and categorical variables by their frequency (n,%). We compared characteristics across the four different income categories (<$19,999, $20,000–$49,999, $50,000–$99,999, and >$100,000) and the four categories of educational attainment (high school/vocational, some college, Bachelor's, graduate) using the Chi-square test for categorical variables and analysis of variance for continuous variables. We adhered to guidance from prior studies that have suggested not combining income and education to retain their separate effects [15,16]. Hence we elected in the current analysis to examine income and education as independent variables to assess their respective associations with hospitalizations.
We graphically represent the number of hospitalizations per patient over time using the mean cumulative function. We assessed for risk of hospitalization in multivariable-adjusted Andersen-Gill, employing income and education as our independent variable. Models consisted of: Model 1, comprising of age, sex, and race; Model 2, included model 1 covariates and body mass index, heart failure, hypertension, diabetes, vascular disease, and smoking status; and (3) Model 3, included model 2 covariates and co-adjustment for either income or education, alternatively, depending on the independent variable. We used the Andersen-Gill model to account for the potential of participants to have multiple hospitalization events. This model treats each hospitalization as a separate “time to event” outcome and accounts for the correlation of recurrent hospitalizations within the same individual participant with a robust sandwich variance estimator [17,18]. In contrast, the standard Cox proportional hazards model considers only the first event for each cohort member.
Written informed consent was obtained from each participant in this study. The study was approved by the University of Pittsburgh IRB. All statistical analyses were conducted using SAS version 9.4 software (SAS Institute, Cary, North Carolina).
3. Results
A total of 339 participants (age 72.3 ± 10.1 years; 42.5% women; and 94.4% white) participated in this study (Table 1). Among the participants, approximately 46% achieved a Bachelor's or graduate education level. A high proportion of participants had an annual income ≥$50,000 (47.5%). Heart failure was more common among participants with <$50,000 annual income (45.9%) and those with high school/vocational education (42.7%) than participants with a higher income and higher educational attainment Supplementary Table 1A and B All other covariates, including hypertension, stroke/transient ischemic attack, diabetes, and vascular disease, did not significantly differ by educational attainment or income as summarized by Supplementary Table 1A and B
Table 1.
Characteristics of study participants.
| Characteristic | All Participants n = 339 |
|---|---|
| Age | 72.3 ± 10.1 |
| Female Sex | 144 (42.5%) |
| White Race | 320 (94.4%) |
| Body mass index (m/kg2) | 31.2 ± 7.2 |
| Smoking History | |
| Never | 169 (49.9%) |
| Former | 152 (44.8%) |
| Current | 18 (5.3%) |
| Heart Failure (Any) | 111 (32.7%) |
| Preserved | 61 (18.0%) |
| Reduced | 44 (13.0%) |
| Not Specified | 6 (1.8%) |
| Hypertension | 243 (71.7%) |
| Diabetes | 82 (24.2%) |
| Vascular Disease | 82 (24.2%) |
| Education | |
| High school/Vocational | 117 (34.5%) |
| Some College | 67 (19.8%) |
| Bachelor's | 79 (23.3%) |
| Graduate | 76 (22.4%) |
| Income | |
| <$19,999 | 35 (10.3%) |
| $20,000–49,999 | 100 (29.5%) |
| $50,000–99,999 | 97 (28.6%) |
| >$100,000 | 64 (18.9%) |
| Refused/No Answer | 43 (12.7%) |
Continuous variables presented as mean±standard deviation, and categorical variables as number (percentage).
Table 2 presents the incidence of hospitalization by annual income and educational attainment. We noted a progressive decrease in the incidence of hospitalization with increasing income category. Participants with <$19,999 annual income (860 hospitalizations per 1000 person-years) had a higher incidence of hospitalization than those with >$100,000 annual income (320 hospitalizations per 1000 person-years). Similarly, higher education was associated with a reduction in hospitalization rates. Of note, there was not a clear trend for individuals with some college and a Bachelor's education. Notably, individuals with a Bachelor's had a higher incidence rate of hospitalization (480 hospitalizations per 1000 person-years) than those with some college education (460 hospitalizations per 1000 person-years). Those with a high school education consistently had a higher incidence of hospitalization (640 hospitalizations per 1000 person-years) than participants with a graduate education (240 hospitalizations per 1000 person-years).
Table 2.
Incidence of hospitalization events by annual income and educational attainment.
| Number of Participants | Hospitalization Events | Person-Time At risk (years) | Incidence Rate (Events/person-year) | |
|---|---|---|---|---|
| Annual Income | ||||
| <$19,999 | 35 | 78 | 90.3 | 0.86 |
| $20,000–49,999 | 100 | 129 | 254.8 | 0.51 |
| $50,000–99,999 | 97 | 108 | 258.1 | 0.42 |
| >$100,000 | 64 | 51 | 157.8 | 0.32 |
| Refused/no answer | 43 | 51 | 108.9 | 0.47 |
| Educational Attainment | ||||
| High school/Vocational | 117 | 193 | 299.6 | 0.64 |
| Some College | 67 | 81 | 177.8 | 0.46 |
| Bachelors | 79 | 96 | 200.0 | 0.48 |
| Graduate | 76 | 47 | 192.6 | 0.24 |
Incidence Rate reported as the number of hospitalizations per person-year at risk.
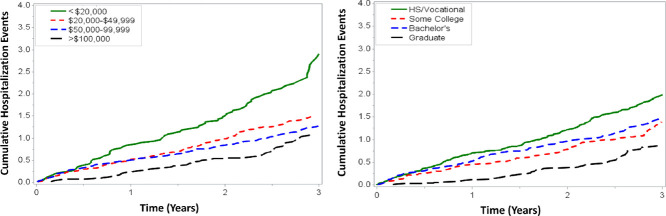
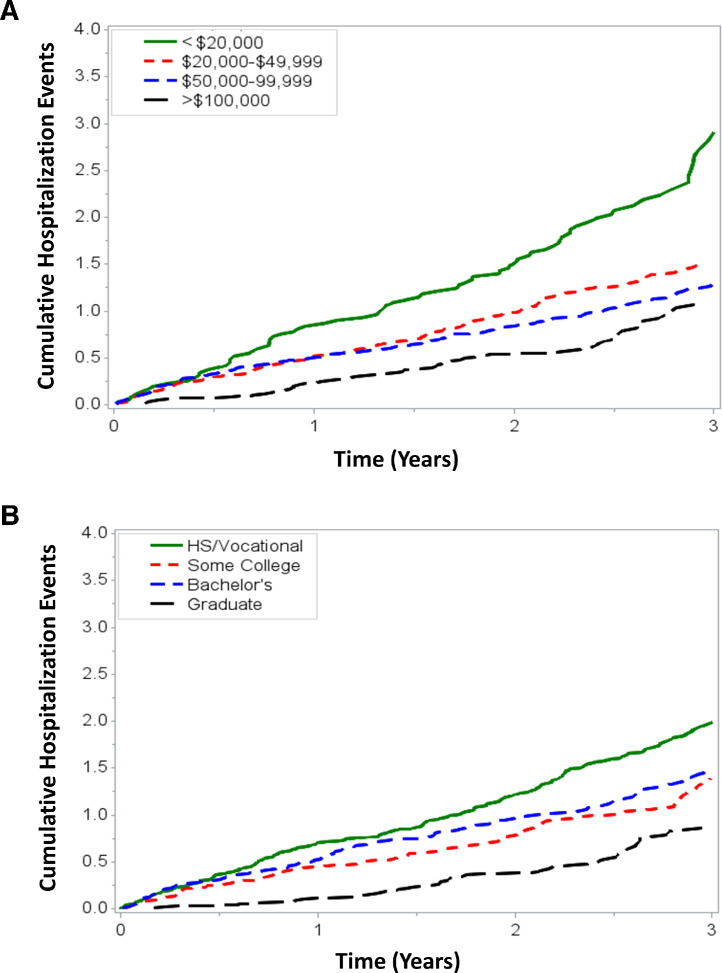
Fig. 1A demonstrates the graded association between annual income and hospitalizations across the study period. Individuals with the lowest income had a greater number of hospitalization events than those in the higher income categories. Fig. 1B shows that participants with lower educational attainment likewise had a higher likelihood of hospitalization.
Fig. 1.
The figures show the mean cumulative function of hospitalization events after enrollment by annual income and educational attainment. Fig. 1A demonstrates a graded association between income and hospitalization rate, such that individuals with a lower category of annual income have increased hospitalization events. Fig. 1B demonstrates that individuals with lower education have progressively increased hospitalization events across education categories.
Table 3 summarizes the associations between income and education with the risk of hospitalization in multivariable-adjusted models. In model 3, participants with an annual income of less than $19,999 had 2-fold higher hospitalization risk (HR 2.11, 95% CI 1.08–4.09; p = 0.03) than participants with an annual income ≥$100,000. In model 2 (adjusted for comorbidities), individuals with a high school/vocational education also had twice the hospitalization risk than those with graduate-level education (HR 1.99, 95% CI 1.12–3.54, p = 0.02). With the inclusion of annual income (Model 3), the association of high school relative to graduate-level educational attainment was attenuated (HR 1.75, 95% CI 0.97–3.15, p = 0.06). Individuals who had achieved a Bachelor's degree had increased risk of hospitalization compared to the graduate-level referent in multivariable-adjustment (HR 1.80, 95% CI 1.00–3.22), attenuated with additional adjustment for income (HR 1.65, 95% CI 0.90–3.03). Likewise, participants with some college had increased risk with adjustment for age, sex, and race (HR 1.95, 95% CI 1.03–3.66, p = 0.04) compared with the graduate-level referent that was attenuated with further multivariable adjustment.
Table 3.
Associations of annual income and educational attainment with hospitalization risk in individuals with AF.
| Model 1 | Model 2 | Model 3 | ||||
|---|---|---|---|---|---|---|
| HR (95% CI) | P-Value | HR (95% CI) | P-Value | HR (95% CI) | P-Value | |
| Annual income | ||||||
| ≥$100,000 (Referent) | – | – | – | |||
| $50,000–99,999 | 1.25 (0.66, 2.37) | 0.49 | 1.19 (0.64, 2.20) | 0.57 | 1.05 (0.56, 1.96) | 0.87 |
| $20,000–49,999 | 1.45 (0.78, 2.70) | 0.24 | 1.37 (0.72, 2.56) | 0.33 | 1.16 (0.60, 2.22) | 0.66 |
| <$19,999 | 2.83 (1.42, 5.63) | 0.003 | 2.53 (1.32, 4.83) | 0.01 | 2.11 (1.08, 4.09) | 0.03 |
| Refused/No Answer | 1.24 (0.63, 2.41) | 0.53 | 1.27 (0.68, 2.34) | 0.45 | 1.11 (0.59, 2.08) | 0.74 |
| Educational attainment | ||||||
| Graduate (Referent) | – | – | – | |||
| Bachelor's | 1.95 (1.06, 3.59) | 0.03 | 1.80 (1.00, 3.22) | 0.05 | 1.65 (0.90, 3.03) | 0.10 |
| Some College | 1.95 (1.03, 3.66) | 0.04 | 1.68 (0.89, 3.18) | 0.11 | 1.50 (0.78, 2.84) | 0.22 |
| High school/Vocational | 2.51 (1.40, 4.49) | 0.002 | 1.99 (1.12, 3.54) | 0.02 | 1.75 (0.97, 3.15) | 0.06 |
Model 1 adjusted for age, sex, race.
Model 2 adjusted for Model 1 components plus body mass index, heart failure, hypertension, diabetes, vascular disease, and smoking status.
Model 3 adjusted for Model 2 components plus either income or education.
4. Discussion
In this moderate-sized cohort of individuals with AF, we observed associations between annual income and educational attainment with hospitalization risk. We observed a graded and persistent association whereby lower income was associated with an increased risk of hospitalization. Our findings describing the association of educational attainment in hospitalization among individuals with AF are similar but were no longer significant when we included adjustment for annual income. Our results are consistent with studies analyzing the effects of income and education on health outcomes in other chronic diseases [19,20].
The association between income and clinical outcomes has had limited study in AF. Utilizing a health claims dataset, one study found an increased risk of adverse cardiovascular outcomes (specifically, heart failure and myocardial infarction) among patients with AF and lower household income [7]. In a large Danish nationwide registry-based cohort of 150,544 individuals, those with the lowest socioeconomic status, based on equivalized income, were more often diagnosed with AF-complications such as strokes and heart failure [11].
Multiple mechanisms may explain the relation between income and adverse clinical outcomes, such as hospitalization events. First, intermediate risk factors for AF and cardiovascular adversity are likely relevant. A broad array of income-related social determinants may influence hospitalization risk, including access to treatment, transportation, family support, neighborhood health, medication adherence, and nutritional choices [[21], [22], [23]]. Second, individuals with lower-income are more likely to have limited insurance. The lack of access to care contributes to lower-income individuals’ inability to obtain timely preventive care and delay hospitalizations [5,24]. For example, individuals with private insurance or Medicare are more likely to be offered extensive treatments for AF, such as catheter ablation or newer anticoagulants, than uninsured individuals to reduce AF-related symptoms and complications [25,26]. Third, individuals of a lower income may have an increased likelihood of challenges to medication adherence due to co-pay costs, pharmacy access, inconsistent patient-provider relationships, and insurance lapses, all of which may result in increased hospitalization rates [27,28].
Study of how educational attainment contributes to outcomes in AF remains limited. Education has been examined in chronic conditions such as cardiovascular disease, with lower educational attainment being associated with a higher prevalence of cardiovascular risk factors and events [[29], [30], [31]]. Multiple pathways may explain the relation of educational attainment and clinical adversity, such as the hospitalization rates observed in the current study.
The major mediating processes can be grouped into four categories: employment, health behaviors, health literacy, and access to care. Foremost, education leads to greater employment potential and higher income, allowing individuals to accumulate wealth that may result in health-related benefits [32]. Our study identified an association between education and hospitalization risk, which was no longer significant after adjusting for income. Our finding suggests that income largely accounts for the relation of education to clinical events.
Second, health behaviors are an essential mediator of health outcomes, and adults with lower educational attainment are more likely to engage in behaviors that exacerbate risk, such as smoke, have an unhealthy diet, and lack exercise [21,33]. Third, education is directly proportional to health literacy, with higher education resulting in a better understanding of chronic health conditions, increased adherence to medications, decreased hospitalization, and decreased mortality [[34], [35], [36]]. Furthermore, individuals with higher educational attainment have been shown as more likely to define AF and stroke accurately than those with a high school or vocational degree [13]. Fourth, access to health care has a role in explaining health inequities by education. Individuals with lower educational attainment have lower household income, less access to health insurance, healthy food, and transportation, all associated with health care access hardship [22].
Our findings are particularly noteworthy as individuals with a lower income and educational attainment are more likely to suffer from cardiovascular disease, including AF, coronary artery disease, and stroke [15]. The associated increased risk for hospitalization among socioeconomically disadvantaged individuals suggests targeted intervention opportunities to ameliorate health outcomes to address and reduce disparities. Despite widespread efforts to address disparities in cardiovascular disease care, gaps across income levels remain wide. Disparities in income, household wealth, homeownership, and educational attainment have widened, and with such increases, we can likewise expect increased hospitalizations as further evidence of disparities in individuals with AF [37,38]. The current study demonstrates the impact that social determinants of health on clinical adversity among individuals with AF.
More research is needed to target interventions for high- patients, thereby addressing disparities. Targeted rehabilitation programs, including group education and physical training for patients with AF, significantly diminished the risk of mortality and cardiovascular hospitalizations [39,40]. These structured care programs have enhanced patient outcomes among patients with AF Reinforced, targeted, in-person education can improve quality of life, symptoms improvement, and medication adherence [41]. Such approaches merit implementation in socioeconomically disadvantaged patients with AF.
AF-related hospitalization has increased for the past decade [42]. AF is a complex disease, such that patients must clearly understand the arrhythmia, its treatment and management, and maintain long-term adherence to therapies [43]. In clinical practice, the use of income and education levels may identify increased risk for adversity and prompt interventions among patients with AF [44]. A multidisciplinary team-based approach in clinical settings has been associated with improved outcomes, such as reduced mortality, hospitalizations, and more cost-effective care [45,46].
Recent professional society statements advocate equitable care but do not include more substantive approaches to identify, accommodate, and address social determinants of health [47]. Our study indicates the substantive contribution of income and education towards adverse outcomes and their role as social determinants, and the vital importance of bringing tailored approaches for socially socioeconomically disadvantaged patients into guideline-based care.
The current study has several strengths. First, we utilized a moderate-sized cohort within an extensive regional healthcare system, thereby enhancing the selected covariates' complete characterization. Second, the individual analyses of income and education allowed us to identify individuals with a diversity of annual income and educational attainment. Third, the use of the Andersen-Gill model facilitated our ability to examine repeated hospitalization events and thereby accommodate for recurrent events in the cohort.
We would like to recognize important limitations to our analysis. First, we appreciate multiple selection biases for participation in this cohort. Participants were recruited at selected ambulatory sites belonging to a regional health care system. We consider this factor as reducing the generalizability of our findings, particularly as individuals receiving care at such sites had health insurance and access to specialty care. We expect the challenges faced by individuals with limited income and education are broadly generalizable beyond our geographic region. Additionally, the exclusion of non-English speakers reduces the generalizability of our findings. Individuals with language barriers may experience impaired access to medical treatments and specialized care. We note as well that no individuals were excluded for being non-English speakers, however. Finally, we required that individuals had been prescribed oral anticoagulation as treatment for AF. While such a distinction indicates active treatment for AF, it does not allow us to examine risk of hospitalization in those who do not have access to such treatment. Second, a substantive portion of our cohort had a higher-income and a graduate-level education, both of which exceed that of the U.S. population [48,49], also limiting our study's generalizability. Third, both income and educational attainment were self-reported, which may have introduced recall or unmeasured biases. Additionally, individuals may have had a higher net worth or additional resources than their reported household income, not captured by our ascertainment of annual household income. Fourth, we cannot account for the effects of AF or other comorbid conditions on individuals' earning capacity and resulting annual income. Fifth, our analysis did not account for multiple residual confounding sources that may mediate hospitalization risks, such as access to additional resources to enhance health, self-care, and medication adherence.
5. Conclusion
In conclusion, we found an association between annual income and educational attainment and hospitalization in a cohort with prevalent AF. Our findings suggest that both income and education merit consideration in the complex management of AF. The development of evidence-based strategies is essential to ameliorate adversity in individuals with AF.
CRediT authorship contribution statement
Tarryn Tertulien: Writing – review & editing. Yimin Chen: Writing – review & editing. Andrew D. Althouse: Writing – review & editing, Software, Formal analysis, Investigation, Resources, Data curation. Utibe R. Essien: Writing – review & editing. Amber Johnson: Writing – review & editing, Investigation. Jared W. Magnani: Conceptualization, Methodology, Investigation, Resources, Writing – original draft, Funding acquisition.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgments
Not applicable.
Funding
This work was supported by NIH/NHLBI grants R33HL144669 and R01HL143010.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.ajpc.2021.100201.
Appendix. Supplementary materials
References
- 1.Virani S.S., Alonso A., Benjamin E.J. Heart disease and stroke statistics-2020 update: a report from the American Heart Association. Circulation. 2020;141:e139–e596. doi: 10.1161/CIR.0000000000000757. [DOI] [PubMed] [Google Scholar]
- 2.Delaney J.A., Yin X., Fontes J.D. Hospital and clinical care costs associated with atrial fibrillation for medicare beneficiaries in the cardiovascular health study and the framingham heart study. SAGE Open Med. 2018;6 doi: 10.1177/2050312118759444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Freeman J.V., Wang Y., Akar J., Desai N., Krumholz H. National trends in atrial fibrillation hospitalization, readmission, and mortality for medicare beneficiaries, 1999–2013. Circulation. 2017;135:1227–1239. doi: 10.1161/CIRCULATIONAHA.116.022388. [DOI] [PubMed] [Google Scholar]
- 4.Krishnamurthi N., Francis J., Fihn S.D., Meyer C.S., Whooley M.A. Leading causes of cardiovascular hospitalization in 8.45 million US veterans. PLoS ONE. 2018;13 doi: 10.1371/journal.pone.0193996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Marmot M., Friel S., Bell R., Houweling T.A., Taylor S., CoSDo Health. Closing the gap in a generation: health equity through action on the social determinants of health. The lancet. 2008;372:1661–1669. doi: 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- 6.Havranek E.P., Mujahid M.S., Barr D.A. Social determinants of risk and outcomes for cardiovascular disease: a scientific statement from the American Heart Association. Circulation. 2015;132:873–898. doi: 10.1161/CIR.0000000000000228. [DOI] [PubMed] [Google Scholar]
- 7.Martinez-Garcia M., Salinas-Ortega M., Estrada-Arriaga I., Hernandez-Lemus E., Garcia-Herrera R., Vallejo M. A systematic approach to analyze the social determinants of cardiovascular disease. PLoS ONE. 2018;13 doi: 10.1371/journal.pone.0190960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.LaRosa A.R., Claxton J., O'Neal W.T. Association of household income and adverse outcomes in patients with atrial fibrillation. Heart. 2020;106:1679–1685. doi: 10.1136/heartjnl-2019-316065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hamad R., Nguyen T.T., Bhattacharya J., Glymour M.M., Rehkopf D.H. Educational attainment and cardiovascular disease in the United States: a quasi-experimental instrumental variables analysis. PLoS Med. 2019;16 doi: 10.1371/journal.pmed.1002834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hamad R., Elser H., Tran D.C., Rehkopf D.H., Goodman S.N. How and why studies disagree about the effects of education on health: a systematic review and meta-analysis of studies of compulsory schooling laws. Soc Sci Med. 2018;212:168–178. doi: 10.1016/j.socscimed.2018.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hagengaard L., Andersen M.P., Polcwiartek C., J.M. Larsen, M.L. Larsen, R.K. Skals, S.M. Hansen, S. Riahi, G. Gislason, C. Torp-Pedersen. Socioeconomic differences in outcomes after hospital admission for atrial fibrillation or flutter. Eur Heart J Qual Care Clin Outcomes. 2019;7(3):295–303. doi: 10.1093/ehjqcco/qcz053. [DOI] [PubMed] [Google Scholar]
- 12.Lip G.Y., Nieuwlaat R., Pisters R., Lane D.A., Crijns H.J. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137:263–272. doi: 10.1378/chest.09-1584. [DOI] [PubMed] [Google Scholar]
- 13.LaRosa A.R., Pusateri A.M., Althouse A.D., Mathier A.S., Essien U.R., Magnani J.W. Mind the gap: deficits in fundamental disease-specific knowledge in atrial fibrillation. Int J Cardiol. 2019;292:272–276. doi: 10.1016/j.ijcard.2019.06.037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gisi B., Althouse A.D., Mathier A.S. The unmeasured burden: contribution of depression and psychological stress to patient-reported outcomes in atrial fibrillation. Int J Cardiol. 2020;302:75–80. doi: 10.1016/j.ijcard.2019.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Khaing W., Vallibhakara S.A., Attia J., McEvoy M., Thakkinstian A. Effects of education and income on cardiovascular outcomes: a systematic review and meta-analysis. Eur J Prev Cardiol. 2017;24:1032–1042. doi: 10.1177/2047487317705916. [DOI] [PubMed] [Google Scholar]
- 16.Braveman P.A., Cubbin C., Egerter S. Socioeconomic status in health research: one size does not fit all. JAMA. 2005;294:2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- 17.Amorim L.D., Cai J. Modelling recurrent events: a tutorial for analysis in epidemiology. Int J Epidemiol. 2015;44:324–333. doi: 10.1093/ije/dyu222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Andersen P.K., Gill R.D. Cox's regression model for counting processes: a large sample study. Ann Stat. 1982:1100–1120. [Google Scholar]
- 19.Ziaeian B., Kominski G.F., Ong M.K., Mays V.M., Brook R.H., Fonarow G.C. National differences in trends for heart failure hospitalizations by sex and race/ethnicity. Circ Cardiovasc Qual Outcomes. 2017;10(7):e003552. doi: 10.1161/CIRCOUTCOMES.116.003552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yusuf S., Joseph P., Rangarajan S. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet. 2020;395:795–808. doi: 10.1016/S0140-6736(19)32008-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mellis A.M., Athamneh L.N., Stein J.S., Sze Y.Y., Epstein L.H., Bickel W.K. Less is more: negative income shock increases immediate preference in cross commodity discounting and food demand. Appetite. 2018;129:155–161. doi: 10.1016/j.appet.2018.06.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Charkhchi P., Fazeli Dehkordy S., Carlos R.C. Housing and food insecurity, care access, and health status among the chronically Ill: an analysis of the behavioral risk factor surveillance system. J Gen Intern Med. 2018;33:644–650. doi: 10.1007/s11606-017-4255-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Drewnowski A., Specter S.E. Poverty and obesity: the role of energy density and energy costs. Am J Clin Nutr. 2004;79:6–16. doi: 10.1093/ajcn/79.1.6. [DOI] [PubMed] [Google Scholar]
- 24.Holahan J. The 2007-09 recession and health insurance coverage. Health Aff (Millwood) 2011;30:145–152. doi: 10.1377/hlthaff.2010.1003. [DOI] [PubMed] [Google Scholar]
- 25.Patel N., Deshmukh A., Thakkar B. Gender, race, and health insurance status in patients undergoing catheter ablation for atrial fibrillation. Am J Cardiol. 2016;117:1117–1126. doi: 10.1016/j.amjcard.2016.01.040. [DOI] [PubMed] [Google Scholar]
- 26.Essien U.R., Holmes D.N., Jackson L.R. Association of race/ethnicity with oral anticoagulant use in patients with atrial fibrillation: findings from the outcomes registry for better informed treatment of atrial fibrillation II. JAMA Cardiol. 2018;3:1174–1182. doi: 10.1001/jamacardio.2018.3945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhang J.X., Lee J.U., Meltzer D.O. Risk factors for cost-related medication non-adherence among older patients with diabetes. World J Diabetes. 2014;5:945–950. doi: 10.4239/wjd.v5.i6.945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harrison E. The cost of not taking our medicine: the complex causes and effects of low medication adherence. Am J Account Care. 2018;12:e11–e13. [Google Scholar]
- 29.Kaplan G.A., Keil J.E. Socioeconomic factors and cardiovascular disease: a review of the literature. Circulation. 1993;88:1973–1998. doi: 10.1161/01.cir.88.4.1973. [DOI] [PubMed] [Google Scholar]
- 30.Mensah G.A., Mokdad A.H., Ford E.S., Greenlund K.J., Croft J.B. State of disparities in cardiovascular health in the United States. Circulation. 2005;111:1233–1241. doi: 10.1161/01.CIR.0000158136.76824.04. [DOI] [PubMed] [Google Scholar]
- 31.Gleason K.T., Himmelfarb C.R.D., Ford D.E. Association of sex, age and education level with patient reported outcomes in atrial fibrillation. BMC Cardiovasc Disord. 2019;19:85. doi: 10.1186/s12872-019-1059-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Mirowsky J., Ross C.E. Transaction Publishers; 2003. Education, social status, and health. [Google Scholar]
- 33.Shaw B.A., Agahi N., Krause N. Are changes in financial strain associated with changes in alcohol use and smoking among older adults? J Stud Alcohol Drugs. 2011;72(6):917–925. doi: 10.15288/jsad.2011.72.917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gazmararian J.A., Williams M.V., Peel J., Baker D.W. Health literacy and knowledge of chronic disease. Patient Educ Couns. 2003;51:267–275. doi: 10.1016/s0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- 35.Magnani J.W., Paasche-Orlow M.K., Parreiras Martins M.A., Lin W., Edgar B., Aronis K.N. Health literacy and atrial fibrillation: relevance and future directions for patient-centred care. Eur Cardiol Rev. 2017;12(1):52–57. doi: 10.15420/ecr.2017:2:2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.O'Neal W.T., Efird J.T., Judd S.E. Impact of awareness and patterns of nonhospitalized atrial fibrillation on the risk of mortality: the reasons for geographic and racial differences in stroke (REGARDS) study. Clin Cardiol. 2016;39:103–110. doi: 10.1002/clc.22501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Beckman AH, J., Nasir K., Desai N., Spatz E. Trends in Cardiovascular Health of US adults by income, 2005-2014. JAMA Cardiol. 2017;2:814–816. doi: 10.1001/jamacardio.2017.1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bor J., Cohen G.H., Galea S. Population health in an era of rising income inequality: USA, 1980–2015. Lancet. 2017;389:1475–1490. doi: 10.1016/S0140-6736(17)30571-8. [DOI] [PubMed] [Google Scholar]
- 39.Joensen A.M., Dinesen P.T., Svendsen L.T. Effect of patient education and physical training on quality of life and physical exercise capacity in patients with paroxysmal or persistent atrial fibrillation: a randomized study. J Rehabil Med. 2019;51:442–450. doi: 10.2340/16501977-2551. [DOI] [PubMed] [Google Scholar]
- 40.Younis A., Shaviv E., Nof E. The role and outcome of cardiac rehabilitation program in patients with atrial fibrillation. Clin Cardiol. 2018;41:1170–1176. doi: 10.1002/clc.23001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Desteghe L., Engelhard L., Vijgen J. Effect of reinforced, targeted in-person education using the Jessa Atrial fibrillation knowledge questionnaire in patients with atrial fibrillation: a randomized controlled trial. Eur J Cardiovasc Nurs. 2019;18:194–203. doi: 10.1177/1474515118804353. [DOI] [PubMed] [Google Scholar]
- 42.Freeman J.V., Wang Y., Akar J., Desai N., Krumholz H. National trends in atrial fibrillation hospitalization, readmission, and mortality for medicare beneficiaries, 1999-2013. Circulation. 2017;135:1227–1239. doi: 10.1161/CIRCULATIONAHA.116.022388. [DOI] [PubMed] [Google Scholar]
- 43.Kirchhof P., Benussi S., Kotecha D. 2016 ESC Guidelines for the management of atrial fibrillation developed in collaboration with EACTS. Eur J Cardiothorac Surg. 2016;50:e1–e88. doi: 10.1093/ejcts/ezw313. [DOI] [PubMed] [Google Scholar]
- 44.Roger V.L. Medicine and society: social determinants of health and cardiovascular disease. Eur Heart J. 2020;41(11):1179–1181. doi: 10.1093/eurheartj/ehaa134. [DOI] [PubMed] [Google Scholar]
- 45.Gallagher C., Elliott A.D., Wong C.X. Integrated care in atrial fibrillation: a systematic review and meta-analysis. Heart. 2017;103:1947–1953. doi: 10.1136/heartjnl-2016-310952. [DOI] [PubMed] [Google Scholar]
- 46.Hendriks J., Tomini F., van Asselt T., Crijns H., Vrijhoef H. Cost-effectiveness of a specialized atrial fibrillation clinic vs. usual care in patients with atrial fibrillation. Europace. 2013;15:1128–1135. doi: 10.1093/europace/eut055. [DOI] [PubMed] [Google Scholar]
- 47.Piccini J.P., Allred J., Bunch T.J. Rationale, considerations, and goals for atrial fibrillation centers of excellence: a Heart Rhythm Society perspective. Heart Rhythm. 2020;17:1804–1832. doi: 10.1016/j.hrthm.2020.04.033. [DOI] [PubMed] [Google Scholar]
- 48.Semega J., Kollar M., E.A. Shrider, J.F. Creamer. U.S. Government Publishing Office; Washington, DC: 2020. U.S. Census Bureau, Current Population Reports, P60-270, Income and Poverty in the United States: 2019. [Google Scholar]
- 49.Ryan C.L., Siebens J. US Census Bureau; 2012. Educational attainment in the united states: 2009. population characteristics. current population reports. P20-566. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.