Abstract
Purpose
This study aimed to establish an accurate and easy predictive model for ST-segment elevation myocardial infarction (STEMI) patients with hyperuricemia, using readily available features to estimate intrahospital mortality risk.
Patients and Methods
This was a multicenter retrospective study involving the development of risk prediction models for intrahospital mortality among all STEMI patients with hyperuricemia from Zunyi Medical University Chest Pain Center’s specialized alliance between January 1, 2016 and June 30, 2020. The primary outcome was intrahospital mortality. A total of 48 candidate variables were considered from demographic and clinical data. The least absolute shrinkage and selection operator (LASSO) was used to develop a nomogram. Concordance index values, decision curve analysis, the area under the curve (AUC), and clinical impact curves were examined. In this study, 489 patients with STEMI were included in the training dataset and an additional 209 patients from the 44 chest pain centers were included in the test cohort. B-type natriuretic peptides, α-hydroxybutyrate dehydrogenase (α-HBDH), cystatin C, out-of-hospital cardiac arrest (OHCA), shock index, and neutrophil-to-lymphocyte ratio were associated with intrahospital mortality and included in the nomogram.
Results
The model showed good discrimination power, and the AUC generated to predict survival in the training set was 0.875 (95% confidence interval, 0.825–0.925). In the validation set, the AUC of survival predictions was 0.87 (95% confidence interval, 0.792–0.947). Calibration plots and decision curve analysis showed good model performance in both datasets. A web-based calculator (https://bzxzmu.shinyapps.io/STEMI-with-Hyperuricemia-intrahospital-mortality/) was established based on the nomogram model, which was used to measure the levels of OHCA, neutrophil-to-lymphocyte ratio, shock index, α-HBDH, cystatin C, and B-type natriuretic peptides.
Conclusion
For practical applications, this model may prove clinically useful for personalized therapy management in patients with STEMI with hyperuricemia.
Keywords: hyperuricemia, STEMI, nomogram, mortality
Introduction
Acute myocardial infarction (AMI) covers a wide range of clinical manifestations, including ST-segment elevation myocardial infarction (STEMI) and non-STEMI (NSTEMI), that are associated with high morbidity and mortality rates. STEMI is the most severe type of AMI and has a poor prognosis.1–3 it shows rapid progression and high risk of intrahospital mortality.4–6 Therefore, a simple, easy, and rapid prognostic model would have a huge clinical impact on the prognoses of patients with STEMI. Common risk factors for STEMI include dyslipidemia, hypertension, diabetes mellitus, and a family history of coronary artery disease. In recent years, elevated serum uric acid (UA) levels have become a well-known cardiovascular risk factor.7–12 Although it is still controversial whether UA is an independent predictor of cardiovascular disease, recent retrospective studies have demonstrated that elevated UA levels are an independent predictor of short- and long-term mortality in patients with AMI.13,14 Various prognostic models based on clinical and procedural variables have been established to predict the outcomes of STEMI, such as the Global Registry of Acute Coronary Events (GRACE) and Observatoire Regional Breton sur l’Infarctus (ORBI) scores.15,16 Based on preprocedural factors (typically a combination of clinical and angiographic variables), several prognostic risk scores estimate the individualized risk for adverse outcomes after coronary revascularization.17–19 However, for individualized prognosis prediction, these scores are limited by the categorization of continuous variables, such as age and blood glucose levels, and the risk of delayed scoring until the angiographic variables can be collected and calculated. A nomogram is a graphical display tool that conveniently calculates and interprets predictive results. This device is essential to modern clinical decision-making that is used worldwide in various clinical applications, including cancer treatment, surgery, and other specialities.20–22 However, to date, a nomogram model with adequacy to detect the probability of intrahospital mortality in STEMI patients with hyperuricemia is yet to be developed. Accurate prediction of adverse events after coronary revascularization is essential for preprocedural informed consent and appropriate therapy selection. Considering the number of related risk factors, an accurate prediction tool with early intervention could be the most effective way to treat STEMI patients with hyperuricemia. However, to the best of our knowledge, there is no research on this subject. This study aimed to establish an accurate and easy predictive model for STEMI patients with hyperuricemia, using readily available features to estimate intrahospital mortality risk.
Materials and Methods
Training cohorts were selected from the affiliated hospital of Zunyi Medical University (ZMU), the tertiary medical institution of the Zunyi Cross-Regional Specialized Alliance of Chest Pain Center (ZMUCPC), between January 2016 and June 2020. ZMUCPC is a regional CPC association, including the affiliated hospital of ZMU (tertiary medical institution) and 44 other referral hospitals (secondary medical institutions) across 20 counties in the northern Guizhou Province, that serves 10 million people and was established in May 2017. Validation of the model was performed on a cohort of patients who underwent percutaneous coronary intervention (PCI) for STEMI between June 2017 and June 2020 at these 44 referral hospitals of the ZMUCPC. All patients met the diagnostic criteria of current guidelines for acute STEMI and underwent primary PCI.23 Patients with STEMI who met the following inclusion criteria were included in the study: 1) increase or occurrence of ischemic chest discomfort at rest, 2) elevation of ST-segment ≥ 0.1 mV, 3) elevation of ST-segment in 2 consecutive leads, and 4) elevated levels of cardiac troponin I (≥ 0.03 μg/L) or elevation of cardiac troponin T (≥ 42 ng/L). The exclusion criteria were patients with STEMI who (1) did not undergo primary PCI, (2) were pregnant or lactating, and (3) had allergies to the contrast agent. We also removed variables with > 20% missing data to facilitate and ensure accuracy. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki. Research approval was obtained from the Ethics Committee of ZMU (approval no. KLL[2020]0144). ZMUCPC has a computerized database of all STEMI patients. Medical records pertaining to the demographic characteristics, clinical data, and outcomes were carefully obtained from the computerized database. The requirement for written informed consent from patients was waived because of the study’s retrospective nature. As the data were susceptible to incorrect notation by the researcher; data cleansing and editing, that consisted of removing typographical errors and reviewing data integrity/quality in data reporting, were performed by a second researcher to avoid a flawed model training process. This researcher assessed all clinical endpoints blinded to the outcome of mortality. Additionally, a different researcher assessed the plausibility of the results regarding the outcome of mortality.
A standardized case-report form was used to collect demographic and clinical data, including procedural information. Intrahospital mortality was defined as all-cause mortality during hospitalization. Hyperuricemia was defined as UA levels >7 mg/dL (420 mmol/L) in males and >6 mg/dL (360 mmol/L) in females, as described in previous studies.24 Patients with an estimated glomerular filtration rate (eGFR) <60 mL/min/1.73 m2 for more than three months were defined as having chronic kidney disease (CKD). Delay was defined as and when patient’s first medical contact exceeded 12 hours from symptom onset. Weekend (Saturday and Sunday) or nonweekend exposure (Monday to Friday) was categorized according to the admission calendar. To enrich the dataset, we computed “index” variables, such as shock index (SI), which was defined as the ratio of heart rate and systolic blood pressure, systemic inflammatory response index, systemic inflammatory reaction index, platelet-to-lymphocyte ratio, neutrophil-to-lymphocyte ratio (NLR), and monocyte-to-lymphocyte ratio.
Continuous variables were presented as the medians (interquartile ranges [IQR]) and categorical variables as the numbers (%). Differences in baseline characteristics between groups were analyzed using independent sample t-tests, with Mann–Whitney U-tests used for continuous variables and chi-squared or Fisher’s exact tests used for categorical variables, as appropriate. All statistical analyses were performed using R software (Version 4.0.2; https://www.R-project.org). We used the LASSO approach with the Akaike information criterion (AIC) to select the best predictive features of mortality using the backward selection method that included variables with P<0.05. The characteristic of the nonzero coefficient in the cable regression model was selected, and these risk factors were considered based on odds ratios (ORs) with 95% confidence intervals (CIs) and P-values. A vertical line needs to be delineated to the point raw to assign a point value for significant predictors to use the nomogram, and then it needs to be added to generate a total score and converted into an individual probability of intrahospital mortality. The nomogram was programmed using the ZMU data and externally validated using the test cohort. The discriminative performance was measured by the concordance index (C-index). Calibration was tested using a calibration plot with bootstraps of 1000 resamples, which described the degree of fit between actual and nomogram-predicted mortality. Decision curve analysis (DCA) was conducted to assess the predictive nomogram’s clinical usefulness by quantifying the net benefits at different threshold probabilities. Finally, the clinical impact curve (CIC) was plotted to evaluate the model’s clinical usefulness and applicability with net benefits with the best diagnostic value.
Results
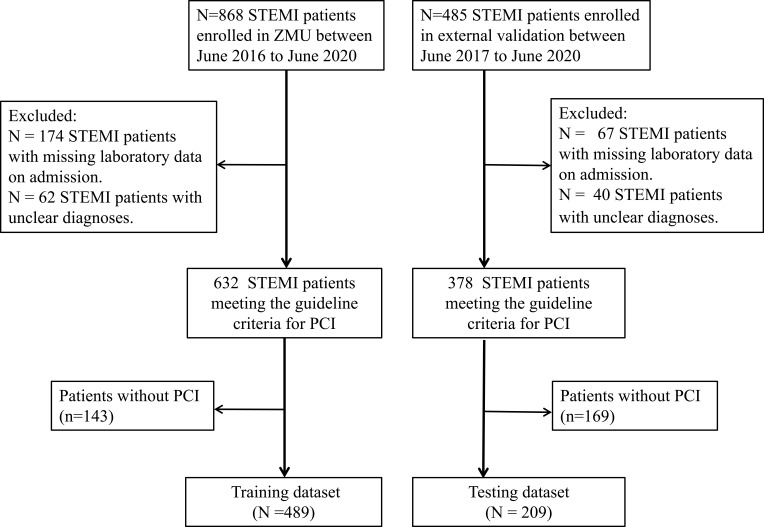
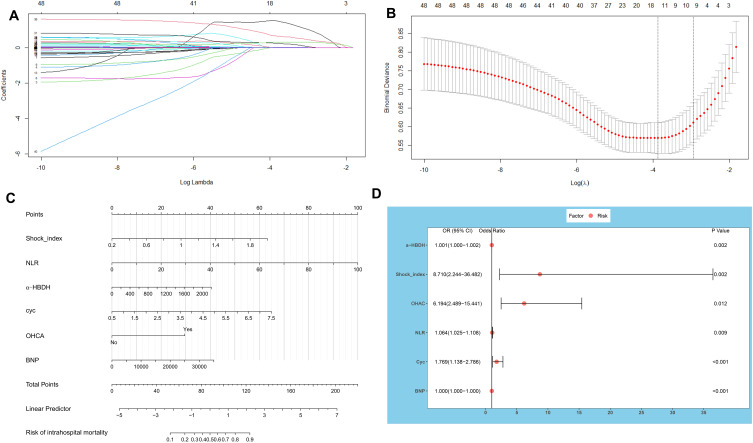
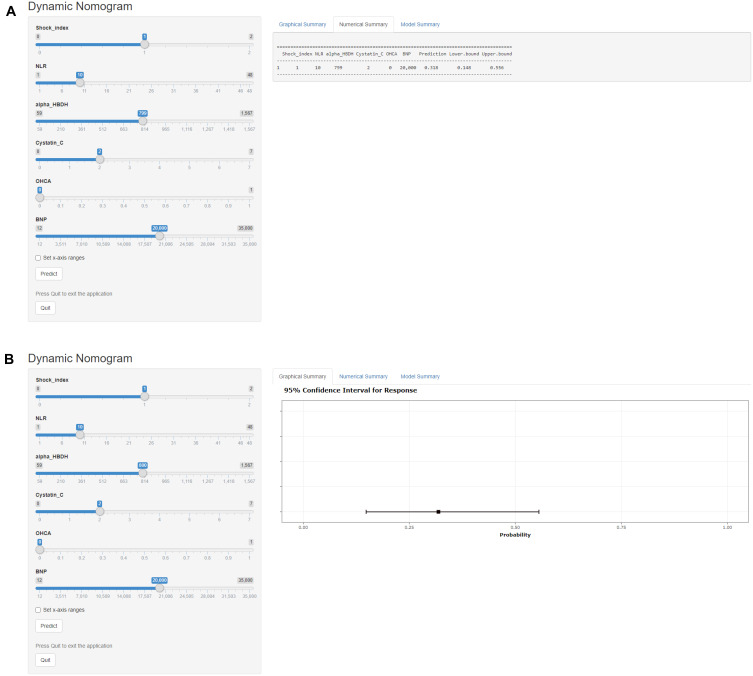
The flow chart of patient inclusion is presented in Figure 1. The baseline characteristics of the training and validation sets are described in Table 1. The training and test cohort included 489 (median age, 64 years; 24.9% female) and 209 (median age, 63 years; 27.2% female) patients, respectively. No difference in intrahospital mortality was detected between the cohorts (14.1% versus 13.8%; P=0.995). According to LASSO analysis, in the training cohort, the SI index, out-of-hospital cardiac arrest (OHCA), neutrophil count, NLR, and α-hydroxybutyrate dehydrogenase (α-HBDH), B-type natriuretic peptides (BNP), LDH, Killip, and cystatin C levels were potential predictors for intrahospital mortality (P<0.01; Table 2, Figure 2A and B). Figure 2C shows the nomogram diagram including six significant predictors. Baseline BNP (OR, 1.000; 95% CI, 1.000–1.000; P<0.001), α-HBDH (OR, 1.001; 95% CI, 1.000–1.002; P=0.012), and cystatin C (OR, 1.769; 95% CI, 1.137–2.786; P=0.009) levels; OHCA (OR, 6.194; 95% CI, 2.489–15.441; P<0.001), SI (OR, 8.71; 95% CI, 2.244–36.482; P=0.002), and NLR (OR, 1.063; 95% CI, 1.025–1.108; P=0.002) were detected by AIC as predictors of intrahospital mortality (Table 3, Figure 2D). To facilitate the clinical application of our findings, we established a model to predict the risk of intrahospital mortality among patients with STEMI with hyperuricemia according to the nomogram (Figure 3). For example, a patient with a circulating cystatin C level of 2 mg/L, BNP level of 20,000 pg/mL, α-HBDH level of 800 U/L, SI of 1, and NLR of 10 would have a total of 91 points (14 points for cystatin C, 24 points for BNP, 15 points for α-HBDH, 28 points for SI, and 10 points for NLR). Intrahospital mortality was approximately 31.9% (95% CI, 14.8–55.6%) among the study cohort.
Figure 1.
Flow chart outlining the patient inclusion process.
Abbreviations: ZMU, The affiliated Hospital of Zunyi Medical University; STEMI, ST-segment elevation myocardial infarction; PCT, percutaneous coronary intervention.
Table 1.
Demographics and Clinical Characteristics of the Training and Test Cohorts
| Variables | Training Cohort (n = 489) | Test Cohort (n = 209) | P-value | |||
|---|---|---|---|---|---|---|
| Demographic characteristics | ||||||
| Sex, n (%) | 0.583 | |||||
| Female | 22 (25) | 57 (27) | ||||
| Male | 367 (75) | 152 (73) | ||||
| Age, y | 64.0 (52.0, 74.0) | 63.0 (53.0, 72.0) | 0.216 | |||
| Smoking, n (%) | 314 (64) | 132 (63) | 0.857 | |||
| Weekend on admission, n (%) | 122 (25) | 69 (33) | 0.036 | |||
| Delay, n (%) | 119 (24) | 50 (24) | 0.984 | |||
| Vascular risk factors | ||||||
| Hypertension, n (%) | 297 (61) | 114 (55) | 0.15 | |||
| Diabetes mellitus, n (%) | 98 (20) | 45 (22) | 0.731 | |||
| Prior-Stroke, n (%) | 30 (6) | 8 (4) | 0.294 | |||
| CKD, n (%) | 107 (22) | 45 (22) | 0.998 | |||
| OHCA, n (%) | 44 (9) | 13 (6) | 0.282 | |||
| GRACE, score | 128.0 (105.0, 154.0) | 122.0 (102.0, 154.0) | 0.363 | |||
| Clinical data | ||||||
| HR, beats/min | 80.0 (73.0, 92.0) | 84.0 (72.0, 94.0) | 0.294 | |||
| SBP, mmHg | 126.0 (108.0, 140.0) | 126.0 (110.0, 141.0) | 0.4 | |||
| DBP, mmHg | 80.00 (72.00, 90.00) | 80.00 (68.00, 90.00) | 0.409 | |||
| Shock index | 0.7 (0.6, 0.8) | 0.6 (0.5, 0.8) | 0.965 | |||
| Killip, n (%) | 0.238 | |||||
| 1 | 369 (75) | 161 (77) | ||||
| 2 | 54 (11) | 16 (8) | ||||
| 3 | 23 (5) | 16 (8) | ||||
| 4 | 43 (9) | 16 (8) | ||||
| Laboratory examinations on admission | ||||||
| WBC, *109/L | 11.4 (8.6, 14.2) | 11.3 (8.6, 14.0) | 0.864 | |||
| Neutrophil count, *109/L | 8.9 (6.3, 11.8) | 9.1 (6.1, 11.5) | 0.898 | |||
| NLR | 6.8 (4.0, 10.7) | 6.3 (3.5, 10.9) | 0.735 | |||
| PLR | 152.4 (105.8, 228.7) | 148.4 (100.5, 218.4) | 0.325 | |||
| MLR | 0.5 (0.3, 0.8) | 0.5 (0.4, 0.8) | 0.28 | |||
| SIRI | 4.5 (2.6, 8.4) | 3.9 (2.5, 7.4) | 0.296 | |||
| SII | 1312.4 (789.4, 2256.4) | 1307.8 (678.1, 2247.2) | 0.545 | |||
| HB, g/L | 136.0 (121.0, 152.0) | 139.0 (120.0, 152.0) | 0.935 | |||
| RBC, *1012/L | 4.5 (3.9, 5.0) | 4.5 (4.0, 5.0) | 0.504 | |||
| PLT, *109/L | 208.0 (165.0, 256.0) | 212.0 (162.0, 248.0) | 0.566 | |||
| ALT, U/L | 31.0 (22.0, 52.0) | 34.0 (23.0, 56.0) | 0.175 | |||
| AST, U/L | 69.0 (36.0, 163.0) | 72.0 (34.0, 173.0) | 0.647 | |||
| GGT, U/L | 42.0 (25.0, 73.0) | 46.0 (29.0, 75.0) | 0.197 | |||
| BUN, mmol/L | 6.7 (5.2, 9.1) | 6.5 (5.2, 9.2) | 0.379 | |||
| Creatinine, umol/L | 99.0 (80.0, 124.0) | 97.0 (77.0, 123.0) | 0.317 | |||
| Uuric acid, umol/L | 472.0 (437.0, 537.0) | 473.0 (436.0, 523.0) | 0.545 | |||
| Cystatin C, mg/L | 1.2 (1.0, 1.5) | 1.1 (0.9, 1.5) | 0.575 | |||
| CK, U/L | 453.0 (184.0, 1352.0) | 501.0 (172.0, 1406.0) | 0.588 | |||
| CKMB, U/L | 49.0 (24.0, 129.0) | 48.0 (25.0, 126.0) | 0.959 | |||
| LDH, U/L | 360.0 (264.0, 609.0) | 390.0 (270.0, 657.0) | 0.287 | |||
| α-HBDH, U/L | 251.0 (171.0, 459.0) | 281.0 (183.0, 502.0) | 0.325 | |||
| CTnT, ng/L | 956.6 (204.5, 3291.0) | 1014.0 (157.0, 3315.0) | 0.767 | |||
| BNP, pg/mL | 1094.0 (265.6, 4087.0) | 1013.0 (228.7, 4497.0) | 0.718 | |||
| Glucose, mmol/L | 6.7 (5.6, 8.7) | 6.7 (5.6, 9.0) | 0.795 | |||
| Myoglobin, ng/mL | 375.7 (102.2, 961.6) | 295.5 (91.7, 723.5) | 0.08 | |||
| Procedural features | ||||||
| LM, n (%) | 6 (1) | 6 (3) | 0.199 | |||
| LAD, n (%) | 149 (30) | 79 (38) | 0.071 | |||
| LCX, n (%) | 53 (11) | 19 (9) | 0.576 | |||
| RCA, n (%) | 118 (24) | 51 (24) | 1 | |||
| Intrahospital complications | ||||||
| Post-Ventricular fibrillation, n (%) | 44 (9) | 16 (8) | 0.666 | |||
| Post-Cardiogenic shock, n (%) | 51 (10) | 19 (9) | 0.688 | |||
| Introhospital Mortality, n (%) | 69 (14) | 29 (13) | 0.995 | |||
| Other | ||||||
| Total hospital duration stay, d | 7.0 (5.0, 10.0) | 6.0 (5.0, 9.0) | 0.136 | |||
Notes: Values are expressed as medians with interquartile ranges for continuous data. Other values are presented as numbers and percentages.
Abbreviations: Shock index, ratio of HR to SBP; SIRI, systemic inflammatory response index; SII, systemic inflammatory reaction index; PLR, ratio of platelets to lymphocytes; NLR, the ratio of neutrophils to lymphocytes; MLR, ratio of monocytes to lymphocytes; OHCA, out-of-hospital cardiac arrest; GRACE, Global Registry of Acute Coronary Events score; α-HBDH, α-Hydroxybutyrate dehydrogenase; BNP, B-type natriuretic peptides.
Table 2.
Comparison of Characteristics of Patients with and without Mortality in the Training Cohort
| Variables | Survival (n=420) | Death (n=69) | P-value |
|---|---|---|---|
| Demographic characteristics | |||
| Sex, n (%) | 0.059 | ||
| Female | 98 (23) | 24 (35) | |
| Male | 322 (77) | 45 (65) | |
| Age, y | 64.0 (51.8, 73.0) | 70.0 (61.0, 77.0) | < 0.001 |
| Smoking, n (%) | 273 (65) | 41 (59) | 0.447 |
| Weekend on admission, n (%) | 108 (26) | 14 (20) | 0.415 |
| Delay, n (%) | 92 (22) | 27 (39) | 0.003 |
| Vascular risk factors | |||
| Hypertension, n (%) | 256 (61) | 41 (59) | 0.914 |
| Diabetes mellitus, n (%) | 83 (20) | 15 (22) | 0.827 |
| Prior-Stroke, n (%) | 26 (6) | 4 (6) | 1 |
| CKD, n (%) | 85 (20) | 22 (32) | 0.044 |
| OHCA, n (%) | 16 (4) | 28 (41) | < 0.001 |
| GRACE, score | 122.0 (102.0, 145.0) | 178.0 (142.0, 213.0) | < 0.001 |
| Clinical data | |||
| HR, beats/min | 79.0 (72.0, 90.0) | 86.0 (76.0, 110.0) | < 0.001 |
| SBP, mmHg | 128.0 (110.0, 142.0) | 109.0 (89.0, 130.0) | < 0.001 |
| DBP, mmHg | 80.00 (68.00, 92.00) | 73.00 (58.00, 85.00) | < 0.001 |
| Shock_index | 0.6 (0.5, 0.7) | 0.8 (0.7, 1.1) | < 0.001 |
| Killip, n (%) | < 0.001 | ||
| 1 | 343 (82) | 26 (38) | |
| 2 | 47 (11) | 7 (10) | |
| 3 | 14 (3) | 9 (13) | |
| 4 | 16 (4) | 27 (39) | |
| Electrocardiographic data | |||
| Inferior_wall, n (%) | 196 (47) | 23 (33) | 0.053 |
| Anterior_wall, n (%) | 205 (49) | 41 (59) | 0.133 |
| Other, n (%) | 13 (3) | 4 (6) | 0.28 |
| Right_ventricular, n (%) | 5 (1) | 1 (1) | 0.601 |
| Laboratory examinations on admission | |||
| WBC, *109/L | 11.2 (8.4, 13.5) | 13.6 (10.0, 18.1) | < 0.001 |
| Neutrophil_count, *109/L | 8.6 (6.2, 11.1) | 11.3 (7.8, 15.1) | < 0.001 |
| NLR | 6.3 (3.9, 9.8) | 9.7 (5.9, 14.8) | < 0.001 |
| PLR | 152.0 (107.8, 223.3) | 155.6 (87.2, 278.2) | 0.93 |
| MLR | 0.5 (0.3, 0.8) | 0.8 (0.4, 1.1) | 0.003 |
| SIRI | 4.2 (2.5, 7.4) | 7.9 (4.1, 14.1) | < 0.001 |
| SII | 1236.8 (778.3, 2094.1) | 2009.1 (1074.2, 2940.4) | 0.005 |
| HB, g/L | 138.00 (122.00, 153.00) | 126.00 (115.00, 147.00) | 0.018 |
| RBC, *1012/L | 4.52 (3.98, 4.98) | 4.17 (3.74, 4.85) | 0.027 |
| PLT, *109/L | 209.5 (167.5, 256.2) | 197.0 (157.0, 254.0) | 0.286 |
| ALT, U/L | 30.0 (22.0, 48.0) | 50.0 (26.0, 129.0) | < 0.001 |
| AST, U/L | 63.0 (35.0, 139.2) | 178.0 (64.0, 399.0) | < 0.001 |
| GGT, U/L | 41.0 (25.8, 69.2) | 55.0 (25.0, 83.0) | 0.403 |
| BUN, mmol/L | 6.4 (5.1, 8.2) | 10.2 (7.7, 13.1) | < 0.001 |
| Creatinine, umol/L | 96.0 (79.0, 116.0) | 135.0 (100.0, 181.0) | < 0.001 |
| Uuric acid, umol/L | 470.0 (436.0, 527.0) | 515.0 (449.0, 601.0) | 0.003 |
| Cystatin C, mg/L | 1.2 (0.9, 1.5) | 1.6 (1.2, 2.2) | < 0.001 |
| CK, U/L | 423.0 (166.5, 1297.8) | 744.0 (303.0, 1639.0) | 0.006 |
| CKMB, U/L | 45.0 (23.0, 118.5) | 86.0 (39.0, 182.0) | 0.002 |
| LDH, U/L | 343.5 (253.0, 523.8) | 655.0 (381.0, 1057.0) | < 0.001 |
| α-HBDH, U/L | 233.5 (166.0, 404.5) | 451.0 (276.0, 739.0) | < 0.001 |
| CTnT, ng/L | 747.1 (175.7, 2914.2) | 2590.0 (1140.0, 5476.0) | < 0.001 |
| BNP, pg/mL | 870.1 (212.3, 2878.5) | 6279.0 (2061.0, 21,400.0) | < 0.001 |
| Glucose, mmol/L | 6.6 (5.6, 8.4) | 7.9 (6.3, 10.6) | < 0.001 |
| Myoglobin, ng/mL | 332.5 (94.4, 893.2) | 677.1 (191.0, 1908.0) | < 0.001 |
| Procedural features | |||
| LM, n (%) | 6 (1) | 0 (0) | 1 |
| LAD, n (%) | 129 (31) | 20 (29) | 0.882 |
| LCX, n (%) | 47 (11) | 6 (9) | 0.683 |
| RCA, n (%) | 102 (24) | 16 (23) | 0.964 |
| Intrahospital complications | |||
| Post-Ventricular fibrillation, n (%) | 19 (5) | 25 (36) | < 0.001 |
| Post-Cardiogenic shock, n (%) | 16 (4) | 35 (51) | < 0.001 |
| Other | |||
| Total hospital duration stay, d | 7.0 (5.0, 10.0) | 2.0 (1.0, 4.0) | < 0.001 |
Notes: Values are expressed as medians with interquartile ranges for continuous data. Other values are presented as numbers and percentages. Shock index ratio of HR to SBP.
Abbreviations: SIRI, systemic inflammatory response index; SII, systemic inflammatory reaction index; PLR, ratio of platelets to lymphocytes; NLR, the ratio of neutrophils to lymphocytes; MLR, ratio of monocytes to lymphocytes; OHCA, out-of-hospital cardiac arrest; GRACE, Global Registry of Acute Coronary Events score; α-HBDH, α-Hydroxybutyrate dehydrogenase; BNP, B-type natriuretic peptides.
Figure 2.
Demographic and clinical feature selection using the LASSO. (A) The minimum criterion of 10-fold cross-validation selects the optimal parameter (λ) in the LASSO model. (B) LASSO coefficient profiles of the 45 features. The coefficient profiles are drawn as a function of log(λ). (C) Intrahospital mortality nomogram. (D) Forest plot of odds ratio (OR) with confidence intervals.
Table 3.
Multivariate Logistic Regression Analysis for the Risk Factors Associated with Mortality in the Training Cohort
| Multivariate Analysis OR(95% CI) | P-value | AIC Adjusted OR(95% CI) | P-value | |
|---|---|---|---|---|
| (Intercept) | 0.001(0.000–0.006) | < 0.001 | 0.002(0.001–0.008) | < 0.001 |
| Shock_index | 8.661(2.07–39.641) | 0.003 | 8.710(2.244–36.482) | 0.002 |
| Neutrophil count | 1.04(0.956–1.131) | 0.352 | ||
| NLR | 1.048(1.001–1.101) | 0.053 | 1.063(1.025–1.108) | 0.002 |
| BUN | 1.032(0.946–1.122) | 0.466 | ||
| LDH | 1.000(0.998–1.001) | 0.901 | ||
| Cystatin C | 1.548(0.892–2.687) | 0.109 | 1.769(1.137–2.786) | 0.009 |
| α-HBDH | 1.000(0.998–1.002) | 0.451 | 1.001(1.000–1.002) | 0.012 |
| OHCA | 3.054(0.460–19.378) | 0.236 | 6.194(2.489–15.441) | < 0.001 |
| Killip1 | Reference | |||
| Killip2 | 1.0193(0.313–2.817) | 0.972 | ||
| Killip3 | 2.344(0.655–7.593) | 0.169 | ||
| Killip4 | 2.334(0.3462–15.158) | 0.376 | ||
| BNP | 1.000(1.000–1.000) | 0.007 | 1.000(1.000–1.000) | < 0.001 |
Figure 3.
Construction of a web-based calculator (https://bzxzmu.shinyapps.io/STEMI-with-Hyperuricemia-intrahospital-mortality/) for predicting intrahospital mortality based on the nomogram model. (A) Web mortality risk calculator. (B) 95% confidence interval of the web mortality rate.
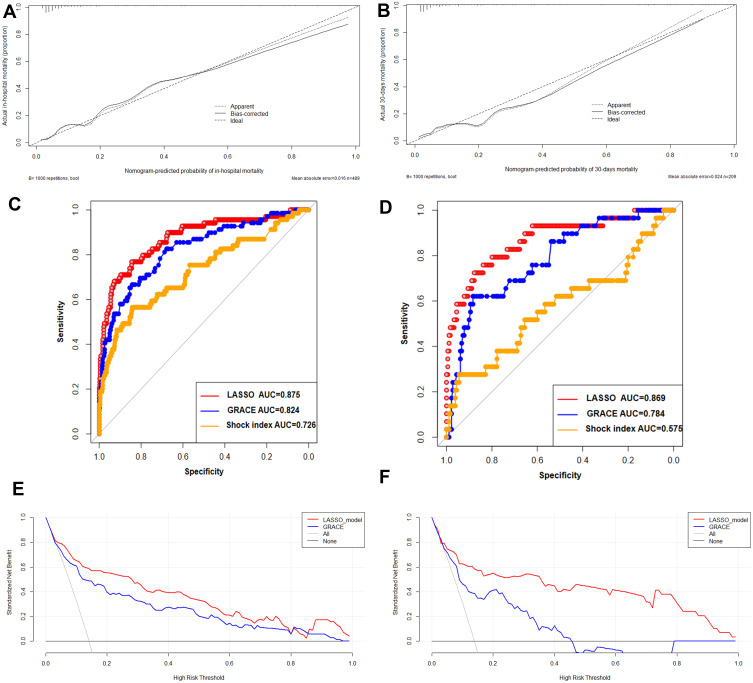
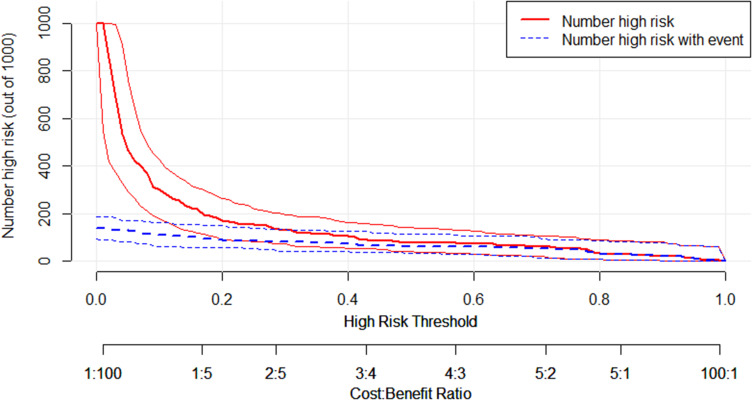
Discrimination of the nomogram was measured by calculating the C-index, which was 0.875 (95% CI, 0.825–0.925), indicating good predictive power in the training cohort (Figure 4A). The C-index of all training and test cohorts was 0.866 by 10-fold cross-validation. The test cohort also confirmed the nomogram’s calibration with a C-index of 0.87 (95% CI, 0.792–0.947; Figure 4B). As a C-index >0.75 is generally considered to indicate reliable discrimination, this nomogram performed well in terms of discrimination and calibration in both the training and test cohorts.25 We further compared the DCA of the new nomogram with the previously published GRACE score. The nomogram’s DCA was superior to that of the GRACE scores in the training and test cohorts (Figure 4C and D). Similar significant associations were also observed in the receiver operating characteristic curves (Figure 4E and F). The DCA demonstrated that when the threshold probabilities ranged between 1.0% and 99.0% and 2.0% and 99% in the training and test cohorts, respectively, the use of nomogram to predict intrahospital mortality versus the strategy of “assuming all” or “assuming no” shows different results for categorizing patients as “at high mortality risk”. For example, if the individual threshold probability of a patient is 30% (the patient would opt for further treatment if his probability of mortality were >30%), the net benefit is 0.44 in the training cohort and 0.43 in the test cohort. The CIC is another type of plot produced based on the decision curve. For this risk model, Figure 5 shows the estimated number who would be declared as high risk for each risk threshold and shows the proportion of cases (true positives). In this example, if a 20% of risk threshold was used, then of the 1000 patients screened, about 180 would be deemed at high risk, about 100 of which would experience mortality. Similar plots have been used in the literature.26
Figure 4.
Calibration plot of the nomogram in the training (A) and test cohorts (B). The dotted line represents the nomogram’s performance, whereas the solid line corrects any bias in the nomogram. The dashed line represents the reference line where an ideal nomogram would lie. Predictive accuracy of the LASSO model, GRACE model, shock index model for intrahospital mortality in the training (C) and test cohorts (D).Decision curve analysis of the nomogram in the training (E) and test cohorts (F). The x-axis indicates the threshold probability. The y-axis measures the net benefit. The gray line displays the net benefit of the strategy of treating all patients. The black line illustrates the net benefit of the strategy of treating no patients. The red line indicates the nomogram. Decision curve analysis is a specific method developed for evaluating the prognostic value of nomogram strategies. The net benefit of using a model to predict intrahospital mortality versus the strategies of “assuming all” or “assuming no” patients would be at high risk is shown for a different decision. The LASSO nomogram model (red) demonstrated an improved net benefit compared with the GRACE model.
Figure 5.
Clinical impact curve for the LASSO nomogram model. The heavy red solid line shows the total number of patients out of 1000 who would be deemed high risk for each risk threshold. The blue dashed line shows how many of those would be true positives cases.
Discussion
Previous studies have confirmed that baseline renal dysfunction and acute kidney injury are strong predictors of in-hospital adverse cardiovascular outcomes after STEMI.27,28 Our study has shown that hyperuricemia on admission was frequently observed in patients with AMI who underwent PCI similar to previous studies.1,8 The nomogram shows that the SI may be the critical individual factor determining intrahospital mortality in STEMI patients with hyperuricemia on admission. UA acts as a direct modulator of inflammation, sub-intimal lipid accumulation, oxidative stress, and tissue injury, contributing to atherosclerosis, plaque composition, and vascular instability.9 UA is strongly associated with cardiovascular disease. This study developed an accurate nomogram based on the baseline SI, NLR, OHCA, and circulating α-HBDH, cystatin C, and BNP levels that can predict the probability of intrahospital mortality for STEMI patients with hyperuricemia. The nomogram’s excellent capacity to discriminate and calibrate the mortality risk was demonstrated in the training cohort and further confirmed through external validation. LASSO regression results in a full shrinkage of a subset of variables, which effectively operates as a form of variable selection. This leads to a more stable model with better predictability, mainly when applied to external datasets.29 Integrating risk factors for clinical data and laboratory measurements on admission into an easy-to-use nomogram facilitates individualized prediction of mortality development in STEMI patients with hyperuricemia via the creation of a risk nomogram.
OHCA is a leading cause of mortality worldwide. The primary cause of OHCA is coronary artery disease, in particular ACS. The survival rate of OHCA patients in Asia is 3.0%.30,31 Urgent coronary angiography and PCI are essential to post-resuscitation care. Inflammatory and oxidative stress play a major role in the pathogenesis of cardiovascular disease. As an easily available inflammatory marker, the role of NLR in cardiovascular disease has been widely studied in the past few years. NLR has been shown to predict short-term mortality in patients with AMI. It has a good correlation with AMI risk prediction models such as GRACE and SYNTAX scores.32 Consistent with previous reports,33–37 NLR, OHCA and cystatin C were significant predictors of mortality in our nomogram. These factors indicate that it is challenging to rescue patients with STEMI who were hypoperfused at the time of admission. Except for other laboratory variables on admission like cystatin C, BNP, α-HBDH, and NLR, SI was shown to be the strongest predictor in the nomogram. Previous studies have used it to predict mortality of AMI and found that an increased SI can predict short-term mortality in patients with STEMI.38–41 Our current research has some strengths. First, the nomogram was developed from a largely homogeneous population of patients with STEMI analyzed using the LASSO approach and achieved improved model performance over traditional regression methods. This method also results in a better final prediction model without sacrificing the interpretability of the relationship between risk factors and the outcome of interest. Second, a high risk of bias will overestimate model efficacy. The risk of bias assessment is an essential step in any prediction model study. Based on the prediction model risk of the bias assessment tool (PROBAST), the risk of bias is low when predictions are made without knowing the outcome status.42
Based on the patients’ clinical and laboratory examinations on admission, the proposed LASSO risk model of intrahospital mortality was constructed to ensure a low ROB. Additionally, there was no risk of delayed calculation caused by waiting for the available procedural results. Despite these strengths, our study had certain limitations. First, as the nature of the study was exploratory, the findings should have been interpreted with caution, as this study excluded several patients because of missing laboratory data. Second, our study focused on STEMI patients with hyperuricemia, and therefore, may not be applicable to all patients with STEMI or NSTEMI. Third, not all possible factors that influence mortality were included among the risk factors studied. For example, lactate was not routinely recorded among our patients and could not be tested as a potential predictor of mortality.
Conclusion
In summary, the nomogram, composed of OHCA, NLR, SI, circulating α-HBDH, cystatin C, and BNP levels, may predict the risk of intrahospital mortality in patients with STEMI with hyperuricemia. Further studies are warranted to validate our findings in other STEMI populations in other regions and countries.
Acknowledgments
We express our gratitude to all patients who participated in this study. We would like to thank Editage (www.editage.cn) for English language editing.
Funding Statement
This research was supported by technological innovation project of Zunyi Science and Technology Bureau(HZ-2021-NO.298). Scientific and technological Innovation Project of Guizhou Provincial Health Commission (gzwkj2021-138).
Abbreviations
SI, Shock index; SIRI, systemic inflammatory response index; SII, systemic inflammatory reaction index; PLR, ratio of platelets to lymphocytes; NLR, the ratio of neutrophils to lymphocytes; MLR, ratio of monocytes to lymphocytes; OHCA, out-of-hospital cardiac arrest; GRACE, Global Registry of Acute Coronary Events score; α-HBDH, α-Hydroxybutyrate dehydrogenase; BNP, B-type natriuretic peptides.
Data Sharing Statement
The datasets are available from the corresponding author upon reasonable request.
Ethical Approval and Informed Consent
The Ethics Committee of the Affiliated Hospital of Zunyi Medical University (approval no KLL[2020]0144) approved the study. All procedures performed in this study involving human participants were in accordance with the Declaration of Helsinki.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Guo W, Yang D, Wu D, et al. Hyperuricemia and long-term mortality in patients with acute myocardial infarction undergoing percutaneous coronary intervention. Ann Transl Med. 2019;7(22):636. doi: 10.21037/atm.2019.10.110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Chung SC, Gedeborg R, Nicholas O, et al. Acute myocardial infarction: a comparison of short-term survival in national outcome registries in Sweden and the UK. Lancet. 2014;383(9925):1305–1312. doi: 10.1016/S0140-6736(13)62070-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sanchis-Gomar F, Perez-Quilis C, Leischik R, Lucia A. Epidemiology of coronary heart disease and acute coronary syndrome. Ann Transl Med. 2016;4(13):256. doi: 10.21037/atm.2016.06.33 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mathias WJ, Tsutsui JM, Tavares BG, et al. Sonothrombolysis in ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention. J Am Coll Cardiol. 2019;73(22):2832–2842. doi: 10.1016/j.jacc.2019.03.006 [DOI] [PubMed] [Google Scholar]
- 5.Schrage B, Ibrahim K, Loehn T, et al. Impella support for acute myocardial infarction complicated by cardiogenic shock. Circulation. 2019;139(10):1249–1258. doi: 10.1161/CIRCULATIONAHA.118.036614 [DOI] [PubMed] [Google Scholar]
- 6.Chapman AR, Shah A, Lee KK, et al. Long-term outcomes in patients with type 2 myocardial infarction and myocardial injury. Circulation. 2018;137(12):1236–1245. doi: 10.1161/CIRCULATIONAHA.117.031806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Srivastava A, Kaze AD, Mcmullan CJ, Isakova T, Waikar SS. Uric acid and the risks of kidney failure and death in individuals with CKD. Am J Kidney Dis. 2018;71(3):362–370. doi: 10.1053/j.ajkd.2017.08.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bai Z, Lu J, Li T, et al. Clinical feature-based machine learning model for 1-year mortality risk prediction of ST-segment elevation myocardial infarction in patients with hyperuricemia: a Retrospective Study. Comput Math Methods Med. 2021;2021:7252280. doi: 10.1155/2021/7252280 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ndrepepa G. Uric acid and cardiovascular disease. Clin Chim Acta. 2018;484:150–163. doi: 10.1016/j.cca.2018.05.046 [DOI] [PubMed] [Google Scholar]
- 10.Lacey B, Herrington WG, Preiss D, Lewington S, Armitage J. The role of emerging risk factors in cardiovascular outcomes. Curr Atheroscler Rep. 2017;19(6):28. doi: 10.1007/s11883-017-0661-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berezin AE. Is serum uric acid a pretty accurate prognostic predictor of ST elevated acute coronary syndrome? Int J Cardiol. 2018;254:49. doi: 10.1016/j.ijcard.2017.05.113 [DOI] [PubMed] [Google Scholar]
- 12.Piepoli MF, Hoes AW, Agewall S, et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: the sixth joint task force of the European society of cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of 10 societies and by invited experts). Int J Behav Med. 2017;24(3):321–419. doi: 10.1007/s12529-016-9583-6 [DOI] [PubMed] [Google Scholar]
- 13.Magnoni M, Berteotti M, Ceriotti F, et al. Serum uric acid on admission predicts in-hospital mortality in patients with acute coronary syndrome. Int J Cardiol. 2017;240:25–29. doi: 10.1016/j.ijcard.2017.04.027 [DOI] [PubMed] [Google Scholar]
- 14.Tscharre M, Herman R, Rohla M, et al. Uric acid is associated with long-term adverse cardiovascular outcomes in patients with acute coronary syndrome undergoing percutaneous coronary intervention. Atherosclerosis. 2018;270:173–179. doi: 10.1016/j.atherosclerosis.2018.02.003 [DOI] [PubMed] [Google Scholar]
- 15.Kao Y-T, Hsieh Y-C, Hsu C-Y, et al. Comparison of the TIMI, GRACE, PAMI and CADILLAC risk scores for prediction of long-term cardiovascular outcomes in Taiwanese diabetic patients with ST-segment elevation myocardial infarction: from the registry of the Taiwan society of cardiology. PLoS One. 2020;15(2):e0229186. doi: 10.1371/journal.pone.0229186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Auffret V, Cottin Y, Leurent G, et al. Predicting the development of in-hospital cardiogenic shock in patients with ST-segment elevation myocardial infarction treated by primary percutaneous coronary intervention: the ORBI risk score. Eur Heart J. 2018;39(22):2090–2102. doi: 10.1093/eurheartj/ehy127 [DOI] [PubMed] [Google Scholar]
- 17.Serruys PW, Morice MC, Kappetein AP, et al. Percutaneous coronary intervention versus coronary-artery bypass grafting for severe coronary artery disease. N Engl J Med. 2009;360(10):961–972. doi: 10.1056/NEJMoa0804626 [DOI] [PubMed] [Google Scholar]
- 18.Yadav M, Palmerini T, Caixeta A, et al. Prediction of coronary risk by SYNTAX and derived scores: synergy between percutaneous coronary intervention with taxus and cardiac surgery. J Am Coll Cardiol. 2013;62(14):1219–1230. doi: 10.1016/j.jacc.2013.06.047 [DOI] [PubMed] [Google Scholar]
- 19.Weintraub WS, Grau-Sepulveda MV, Weiss JM, et al. Prediction of long-term mortality after percutaneous coronary intervention in older adults: results from the national cardiovascular data registry. Circulation. 2012;125(12):1501–1510. doi: 10.1161/CIRCULATIONAHA.111.066969 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kim Y, Margonis GA, Prescott JD, et al. Nomograms to predict recurrence-free and overall survival after curative resection of adrenocortical carcinoma. JAMA Surg. 2016;151(4):365–373. doi: 10.1001/jamasurg.2015.4516 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jehi L, Yardi R, Chagin K, et al. Development and validation of nomograms to provide individualised predictions of seizure outcomes after epilepsy surgery: a retrospective analysis. Lancet Neurol. 2015;14(3):283–290. doi: 10.1016/S1474-4422(14)70325-4 [DOI] [PubMed] [Google Scholar]
- 22.Cappellari M, Mangiafico S, Saia V, et al. IER-SICH nomogram to predict symptomatic intracerebral hemorrhage after thrombectomy for stroke. Stroke. 2019;50(4):909–916. doi: 10.1161/STROKEAHA.118.023316 [DOI] [PubMed] [Google Scholar]
- 23.Ibanez B, James S, Agewall S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–177. doi: 10.1093/eurheartj/ehx393 [DOI] [PubMed] [Google Scholar]
- 24.Guo W, Song F, Chen S, et al. The relationship between hyperuricemia and contrast-induced acute kidney injury undergoing primary percutaneous coronary intervention: secondary analysis protocol for the ATTEMPT RESCIND-1 study. Trials. 2020;21(1):567. doi: 10.1186/s13063-020-04505-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Zhang X, Yuan K, Wang H, et al. Nomogram to predict mortality of endovascular thrombectomy for ischemic stroke despite successful recanalization. J Am Heart Assoc. 2020;9(3):e014899. doi: 10.1161/JAHA.119.014899 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bryant RJ, Sjoberg DD, Vickers AJ, et al. Predicting high-grade cancer at ten-core prostate biopsy using four kallikrein markers measured in blood in the ProtecT study. J Natl Cancer Inst. 2015;107(7):djv095. doi: 10.1093/jnci/djv095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hayiroglu MI, Bozbeyoglu E, Yildirimturk O, Tekkesin AI, Pehlivanoglu S. Effect of acute kidney injury on long-term mortality in patients with ST-segment elevation myocardial infarction complicated by cardiogenic shock who underwent primary percutaneous coronary intervention in a high-volume tertiary center. Turk Kardiyol Dern Ars. 2020;48(1):1–9. doi: 10.5543/tkda.2019.84401 [DOI] [PubMed] [Google Scholar]
- 28.Hayiroglu MI, Canga Y, Yildirimturk O, et al. Clinical characteristics and outcomes of acute coronary syndrome patients with intra-aortic balloon pump inserted in intensive cardiac care unit of a tertiary clinic. Turk Kardiyol Dern Ars. 2018;46(1):10–17. doi: 10.5543/tkda.2017.11126 [DOI] [PubMed] [Google Scholar]
- 29.Goldstein BA, Navar AM, Carter RE. Moving beyond regression techniques in cardiovascular risk prediction: applying machine learning to address analytic challenges. Eur Heart J. 2017;38(23):1805–1814. doi: 10.1093/eurheartj/ehw302 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Myat A, Song KJ, Rea T. Out-of-hospital cardiac arrest: current concepts. Lancet. 2018;391(10124):970–979. doi: 10.1016/S0140-6736(18)30472-0 [DOI] [PubMed] [Google Scholar]
- 31.Hassager C, Nagao K, Hildick-Smith D. Out-of-hospital cardiac arrest: in-hospital intervention strategies. Lancet. 2018;391(10124):989–998. doi: 10.1016/S0140-6736(18)30315-5 [DOI] [PubMed] [Google Scholar]
- 32.Afari ME, Bhat T. Neutrophil to lymphocyte ratio (NLR) and cardiovascular diseases: an update. Expert Rev Cardiovasc Ther. 2016;14(5):573–577. doi: 10.1586/14779072.2016.1154788 [DOI] [PubMed] [Google Scholar]
- 33.Del TS, Basta G, De Caterina AR, et al. Different inflammatory profile in young and elderly STEMI patients undergoing primary percutaneous coronary intervention (PPCI): its influence on no-reflow and mortality. Int J Cardiol. 2019;290:34–39. doi: 10.1016/j.ijcard.2019.05.002 [DOI] [PubMed] [Google Scholar]
- 34.van der Laan SW, Fall T, Soumare A, et al. Cystatin C and cardiovascular disease: a Mendelian Randomization Study. J Am Coll Cardiol. 2016;68(9):934–945. doi: 10.1016/j.jacc.2016.05.092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Luo J, Wang LP, Hu HF, et al. Cystatin C and cardiovascular or all-cause mortality risk in the general population: a meta-analysis. Clin Chim Acta. 2015;450:39–45. doi: 10.1016/j.cca.2015.07.016 [DOI] [PubMed] [Google Scholar]
- 36.Okabe T, Yakushiji T, Kido T, et al. Poor prognosis of heart failure patients with in-hospital worsening renal function and elevated BNP at discharge. ESC Heart Fail. 2020;7(5):2912–2921. doi: 10.1002/ehf2.12901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lee S, Koppensteiner R, Kopp CW, Gremmel T. α-Hydroxybutyrate dehydrogenase is associated with atherothrombotic events following infrainguinal angioplasty and stenting. Sci Rep. 2019;9(1):18200. doi: 10.1038/s41598-019-54899-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Huang B, Yang Y, Zhu J, et al. Usefulness of the admission shock index for predicting short-term outcomes in patients with ST-segment elevation myocardial infarction. Am J Cardiol. 2014;114(9):1315–1321. doi: 10.1016/j.amjcard.2014.07.062 [DOI] [PubMed] [Google Scholar]
- 39.Bilkova D, Motovska Z, Widimsky P, Dvorak J, Lisa L, Budesinsky T. Shock index: a simple clinical parameter for quick mortality risk assessment in acute myocardial infarction. Can J Cardiol. 2011;27(6):739–742. doi: 10.1016/j.cjca.2011.07.008 [DOI] [PubMed] [Google Scholar]
- 40.Spyridopoulos I, Noman A, Ahmed JM, et al. Shock-index as a novel predictor of long-term outcome following primary percutaneous coronary intervention. Eur Heart J Acute Cardiovasc Care. 2015;4(3):270–277. doi: 10.1177/2048872614561480 [DOI] [PubMed] [Google Scholar]
- 41.Supel K, Kacprzak M, Zielinska M, Aalto-Setala K. Shock index and TIMI risk index as valuable prognostic tools in patients with acute coronary syndrome complicated by cardiogenic shock. PLoS One. 2020;15(1):e0227374. doi: 10.1371/journal.pone.0227374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Moons K, Wolff RF, Riley RD, et al. PROBAST: a tool to assess risk of bias and applicability of prediction model studies: explanation and elaboration. Ann Intern Med. 2019;170(1):W1–W33. doi: 10.7326/M18-1377 [DOI] [PubMed] [Google Scholar]