Abstract
Infection with severe acute respiratory syndrome coronavirus-2 (SARS-CoV-2) or seasonal influenza may lead to respiratory failure requiring intubation and mechanical ventilation. The pathophysiology of this respiratory failure is attributed to local immune dysregulation, but how the immune response to viral infection in the lower airways of the human lung differs between individuals with respiratory failure and those without is not well understood. We used quantitative multi-parameter flow cytometry and multiplex cytokine assays to evaluate matched blood and bronchoalveolar lavage (BAL) samples from control human subjects, subjects with symptomatic seasonal influenza who did not have respiratory failure and subjects with severe seasonal influenza or SARS-CoV-2 infection with respiratory failure. We find that severe cases are associated with an influx of non-classical monocytes, activated T cells, and plasmablast B cells into the lower airways. Cytokine concentrations were not elevated in the lower airways of moderate influenza patients compared to controls; however, twenty-eight of thirty-five measured cytokines were significantly elevated in severe influenza, severe SARS-CoV-2 infection or both. We noted the largest elevations in IL-6, IP-10, MCP-1, and IL-8. IL-1 family cytokines and RANTES were higher in severe influenza infection than severe SARS-CoV-2 infection. Interestingly, only the concentration of IP-10 correlated between blood and BAL during severe infection. Our results demonstrate inflammatory immune dysregulation in the lower airways during severe viral pneumonia that is distinct from lower airway responses seen in human patients with symptomatic, but not severe, illness and suggest that measurement of blood IP-10 concentration may predict this unique dysregulation.
Introduction
Infection with both seasonal influenza and severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), which causes coronavirus disease 2019 (COVID-19), are associated with substantial morbidity and mortality (1–5). Manifestations of both diseases range from asymptomatic infection (4, 6) to severe illness leading to acute respiratory failure. Current treatment of severe COVID-19 and severe influenza is primarily supportive with the administration of oxygen and mechanical ventilation when necessary (7–9). There is a more limited role for antiviral therapies during severe disease (10, 11) likely due to ongoing immunopathology that is less dependent on high viral replication during the later stage of illness at which respiratory failure develops. Indeed, recent evidence (12, 13) suggests a mortality benefit in a subset of severely ill COVID-19 patients administered high-dose corticosteroids. Despite this advance, mortality in severe influenza- and COVID-19-associated respiratory failure remains high and the absolute risk reduction for mortality in steroid-treated, mechanically-ventilated COVID-19 patients is somewhat low at approximately 8%−12% (12, 13) suggesting only a subset of severe COVID-19 patients respond to anti-inflammatory treatment.
A complete understanding of the immunologic response in the human lung during severe SARS-CoV-2 and influenza infection is essential to determine the ideal management of these patients, including determining who may benefit from anti-inflammatory medications such as steroids. Unfortunately, only a small number of studies have evaluated lower airway responses in human subjects with severe influenza (14) or COVID-19 (15–18) and very few evaluate individuals with acute symptomatic viral infection who do not have severe disease requiring mechanical ventilation. Numerous studies have shown that subjects with severe influenza and COVID-19 have elevated levels of proinflammatory cytokines in the blood (3, 19, 20). For this reason, there has been significant interest in modulating the immune system to blunt the effects of proinflammatory cytokines during severe COVID-19 (21, 22). However, our previous analysis of plasma samples from subjects with COVID-19 and influenza found a relatively low incidence of dysregulated blood cytokine expression among COVID-19 patients (23) despite generally modest increases in the concentration of circulating cytokines in patients with increasingly severe COVID-19. Other investigators have also reported lower concentrations of inflammatory cytokines in the blood of COVID-19 patients when compared to other groups of critically ill patients (24, 25). Identifying individuals with elevated and dysregulated cytokine expression in the bronchoalveolar space rather than the blood may help to more precisely stratify those at increased risk of severe respiratory failure or death. The bronchoalveolar space serves as a small window into the broader immune response in the lung. Unfortunately, sampling the bronchoalveolar space is complex. The identification of blood markers that correlate with excessive lung inflammation would be helpful. Such markers would allow the physician to target steroids and other novel immunosuppressive therapies to virus-infected individuals with documented severe inflammation in the lung, avoid side-effects in individuals without hyperinflammatory respiratory failure, and potentially increase response rates to targeted anti-inflammatory therapies that have so far proven ineffective in clinical trials (26–28).
To further understand the lower airway mucosal immune response to severe influenza and SARS-CoV-2 infection, we analyzed plasma and bronchoalveolar lavage samples from subjects with severe influenza and COVID-19 and compared them to samples collected with identical methods from healthy controls and subjects with moderate symptomatic influenza infection that did not have respiratory failure or require hospitalization.
Materials and Methods
Study design
This is a prospective observational cohort study of subjects with viral respiratory illness who presented to Barnes Jewish Hospital in Saint Louis, Missouri, USA. COVID-19 patients were enrolled between May 8th and December 17th 2020 after a positive clinical test for SARS-CoV-2. We also report findings from a subset of healthy control subjects and influenza-infected subjects enrolled in the ongoing prospective observational EDFLU cohort study (29) who underwent sampling of blood and bronchoalveolar lavage (BAL) fluid. Subjects with influenza were enrolled in the 2018–2019 and the 2019–2020 influenza seasons.
For subjects with severe COVID-19 or influenza, BAL fluid was obtained via bronchoscopy that was performed for a clinical reason, most frequently to evaluate for bacterial co-infection, at the discretion of the patient’s treating physician. The BAL samples analyzed in this study were excess material collected during that clinical bronchoscopy with BAL procedure. For severe influenza and severe COVID-19 bronchoscopy procedures, the BAL was collected most frequently by wedging the bronchoscope within the right middle lobe bronchus. One severe influenza patient had collection performed in the left lower lobe for clinical purposes. Each clinical procedure involved instilling 100 mL of sterile saline and collecting all returned fluid. The majority of each sample was sent to the clinical laboratory for analysis, but approximately 10–15 mL of the BAL sample was provided to a member of the study team present for the procedure and kept on ice until samples were processed in the laboratory.
For EDFLU subjects with moderate illness and control subjects, samples were obtained during a scheduled elective outpatient research bronchoscopy. Briefly, following subject consent and safety screening with blood coagulation studies and a screening chest x-ray, outpatient subjects received intravenous conscious sedation along with application of lidocaine to the upper airway and vocal cords as the bronchoscope was passed into the airways. A brief visual inspection of the airways was performed to select an appropriate location for BAL collection; however, all outpatient research BAL samples were collected in the right middle lobe bronchus. BAL samples were collected by the instillation of 100 mL to 150 mL of sterile saline and collection of all returned lavage fluid.
Informed consent was obtained from all subjects or their legally authorized representatives. The Institutional Review Board at Washington University in Saint Louis approved these studies (approval numbers 2018-08-115, 2019-10-011, 2020-03-085 and 2020-06-151).
We obtained matched blood and BAL samples from two severe influenza subjects, MC-68 and MC-77, during the 2018-2019 influenza season as a part of an ongoing prospective observational cohort study at the National Institute of Respiratory Diseases Ismael Cosío Villegas in Mexico City, Mexico. This study was approved by the National Institute of Respiratory Diseases Institutional Review Board (approval number B28-16).
Cytokine Quantification
Blood was collected into EDTA-anticoagulated tubes and plasma was frozen at −80°C until analysis. BAL samples were kept on ice and prepared within 4 hours of collection. BAL samples were centrifuged at 300 × g for 15 minutes at 4°C and the collected supernatant was frozen at −80°C.
Plasma and BAL samples were analyzed using a human magnetic cytokine panel providing parallel measurement of 35 cytokines and chemokines (Thermo Fisher Scientific). The assay was performed according to the manufacturer’s instructions with the following modification: the samples were fixed with 100 μL of 1% paraformaldehyde at room temperature for 60 minutes on a shaker at 700 RPM and washed once before the final resuspension. The samples were analyzed on a Luminex FLEXMAP 3D instrument.
Multi-parameter flow cytometry
Absolute cell counts in BAL were determined by flow cytometry with Precision Count Beads (BioLegend) by staining 100 μL of BAL fluid with pre-titrated amounts of CD45 FITC (clone HI30), CD14 PerCP-Cy5.5 (clone M5E2), CD3 PE-Cy7 (clone UCHT1), CD8 BV421 (clone RPA-T8), CD4 APC-Cy7 (clone OKT4) and CD19 APC (clone HIB19). 1 mL of FACS Lysing Solution (BD Biosciences) was added to each sample. 100 μL of Precision Count Beads were added immediately prior to flow cytometry to allow quantification of absolute volume analyzed on the cytometer.
In a separate experiment, fresh BAL cells were analyzed using a panel of antibodies directed against the following antigens: CD3 FITC (clone UCHT1), CD4 APC-Cy7 (clone OKT4), CD8 BV421 (clone RPA-T8), CD14 APC (clone M5E2), CD16 BV570 (clone 3G8), CD19 BV750 (clone HIB19), CD20 Pacific Blue (clone 2H7), CD38 PE-Cy7 (clone HIT2), CD45 Alexa Fluor 532 (clone HI30), CD56 PE/Dazzle 594 (clone HCD56), and HLA-DR BV605 (clone L243). 500,000–1,000,000 fresh BAL cells were stained in BD Brilliant Buffer (BD Biosciences) with Zombie NIR Fixable Viability Marker (BioLegend). Samples were run on a Cytek Aurora spectral flow cytometer using SpectroFlo software (version 2, Cytek) before final analysis in FlowJo software (version 10, BD Biosciences).
Analysis
Absolute cell counts were calculated by measuring the frequencies of each subset in terms of percent of total CD45+ cells or other subsets with known concentration from the Precision Count Bead experiment. Absolute cell count comparisons were made using Kruskal-Wallis ANOVA with Dunn’s post-test.
Individual cytokine concentrations were compared using Kruskal-Wallis ANOVA with Dunn’s post-test. Plasma and BAL correlations were performed with simple linear regression. We utilized a Bonferroni-corrected P value of 0.0015 to adjust for the 35 comparisons.
For the cytokine clustering analysis, cytokine values were processed in R (v4.0.2) and rescaled from 0 to 1 based on the maximum protein level measured for each cytokine. Data was then clustered and visualized using the pheatmap (v1.0.12) R package using Euclidean distances for both row and column clustering.
Plasma IP-10 concentrations measured in a large cohort of COVID-19 patients had been previously reported (23). For the analysis here, we separated the cohort into the groups from the earlier report - uninfected controls and individuals who were intubated or died from COVID-19. We then performed additional chart review to classify all other COVID-19 subjects who did not require intubation or die into groups based upon the presence or absence of organ dysfunction. Those with organ dysfunction had one or more of the following: 1) respiratory failure with a new or increasing oxygen requirement caused by COVID-19, 2) acute kidney injury defined by elevated creatinine requiring hospitalization, 3) cardiac dysfunction classified by a new elevation of troponin in the blood, 4) hypotension, or 5) acute delirium that the medical record documented was due to COVID-19. All Kruskal-Wallis ANOVA tests, linear regression analyses and receiver operating curve analyses were performed in Prism software, version 9 (GraphPad Software).
Results
Demographic and clinical characteristics of human subjects
We prospectively enrolled 17 subjects with severe viral pneumonia who experienced respiratory failure requiring intubation and mechanical ventilation (Table I). Our cohort included 13 individuals with severe COVID-19 and 4 individuals with severe influenza. We also prospectively enrolled 7 individuals who presented for medical attention with moderate symptomatic acute influenza infection that did not require hospitalization (Table I). These individuals returned to the research clinic for an outpatient bronchoscopy with bronchoalveolar lavage (BAL). We further recruited two healthy individuals who had not experienced an influenza-like illness in the 60 days prior to enrollment for outpatient bronchoscopy with BAL. Two of the seven moderate influenza subjects (1920B004 and 1920B005) returned to the clinic more than 45 days after the start of their illness and more than 30 days after the initial bronchoscopy procedure for repeat bronchoscopy with BAL sampling, allowing us to analyze linked samples from these same individuals to make comparisons between their long-term recovery phase (control samples) and their acute symptomatic phase.
Table I –
Cohort demographics
| Subject ID#1 | Age | Sex | Infection status2 | Days after symptom onset for blood/BAL collection3 | VFD4 | Died?5 | CLD?6 | CHF?7 | IS?8 | DM?9 | ESRD?10 |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1819B001 | 28 | F | Control | N/A | 28 | N | N | N | N | N | N |
| 1920B002 | 29 | M | Control | N/A | 28 | N | N | N | N | N | N |
| 1819B004 | 40 | F | Moderate Flu - IAV | D18 | 28 | N | N | N | N | N | N |
| 1819B007 | 27 | M | Moderate Flu - IAV | D9 | 28 | N | N | N | N | N | N |
| 1920B004 | 29 | F | Moderate Flu - IBV | D13, D48 | 28 | N | N | N | N | N | N |
| 1920B005 | 23 | F | Moderate Flu - IBV | D14, D59 | 28 | N | N | N | N | N | N |
| 1920B007 | 28 | F | Moderate Flu - IBV | D20 | 28 | N | N | N | N | N | N |
| 1920B008 | 31 | M | Moderate Flu - IAV | D14 | 28 | N | N | N | N | N | N |
| 1920B013 | 41 | M | Moderate Flu - IBV | D14 | 28 | N | N | N | N | N | N |
| 1920B011 | 26 | F | Severe Flu - IBV | D7 | 18 | N | Y | N | N | Y | N |
| 1920B014 | 50 | M | Severe Flu - IAV | D8 | 0 | N | N | N | N | N | N |
| MC-68 | 46 | M | Severe Flu - IAV | D8 | 0 | Y | Y | N | N | Y | N |
| MC-77 | 43 | F | Severe Flu - IAV | D7 | 8 | N | N | N | N | N | N |
| 350–174 | 74 | M | Severe COVID-19 | D10 | 0 | N | N | N | Y11 | Y | N |
| 350–428 | 59 | F | Severe COVID-19 | D11, D25 | 0 | N | Y | N | N | Y | N |
| 350–441 | 79 | M | Severe COVID-19 | D11 | 0 | Y | N | N | N | Y | N |
| 350–472 | 67 | M | Severe COVID-19 | D10 | 0 | Y | N | N | N | Y | N |
| C2 | 78 | F | Severe COVID-19 | D9 | 0 | Y | N | N | Y12 | N | N |
| C3 | 62 | M | Severe COVID-19 | D14 | 0 | Y | N | N | N | Y | N |
| C7 | 61 | F | Severe COVID-19 | D17 | 0 | Y | Y | N | N | Y | Y |
| C9 | 72 | F | Severe COVID-19 | D32 | 14 | N | Y | N | Y13 | N | N |
| C11 | 60 | F | Severe COVID-19 | D14 | 0 | Y | N | N | Y14 | Y | N |
| C12 | 53 | M | Severe COVID-19 | D11 | 0 | N | N | N | N | N | N |
| C14 | 74 | F | Severe COVID-19 | D14 | 0 | Y | N | N | N | Y | N |
| C15 | 66 | F | Severe COVID-19 | D6 | 0 | N | Y | N | N | Y | N |
| C16 | 73 | F | Severe COVID-19 | D13 | 0 | Y | N | N | Y15 | Y | N |
Footnotes:
Assigned study subject identification number;
Subject severity classification grouping and infecting virus: Control – healthy individuals who did not exhibit an influenza-like illness for at least 60 days prior to outpatient bronchoscopy and bronchoalveolar lavage (BAL) procedure; Moderate Flu – IAV/IBV – healthy individuals with symptomatic influenza A (IAV) or influenza B (IBV) virus infection that did not require hospitalization prior to outpatient bronchoscopy and BAL procedure; Severe Flu – IAV/IBV – individuals with severe IAV or IBV virus infection who were intubated for acute respiratory failure and BAL sampling was performed as a part of standard clinical care; Severe COVID-19 – individuals with severe COVID-19 who were intubated for acute respiratory failure and BAL sampling was performed as part of standard clinical care;
The number of days following the onset of symptoms of viral respiratory illness before each BAL sample was collected;
Ventilator Free Days – 28 days minus the number of days the subject required mechanical ventilation in the intensive care unit; individuals who expired on mechanical ventilation are set at 0;
Yes (Y) or No (N) that patient died during the index hospitalization;
Subject had a history of CLD (Chronic Lung Disease) of any type including asthma or COPD prior to infection;
Subject had a history of CHF (Congestive Heart Failure) prior to infection;
Subject had a history of IS (Immunosuppression) prior to infection;
Subject had a history of DM (Diabetes Mellitus) prior to infection;
Subject had a history of ESRD (End Stage Renal Disease) requiring dialysis prior to infection;
Subject 350–174 had a history of autoimmune disease and was on prednisone;
Subject C2 had a history of solid organ transplantation and was on mycophenolate and sirolimus;
Subject C9 had a history of solid organ transplantation and was on tacrolimus, mycophenolate and prednisone;
Subject C11 had a history of solid organ transplantation and was on tacrolimus;
Subject C16 had a history of autoimmune disease and was on prednisone and azathioprine
The mean age of the COVID-19 cohort (68, IQR 61–74) was significantly older than the mean age of the control (27, IQR 24–29) and moderate influenza (31, IQR 27–40) cohorts (P<0.005 in both comparisons by Kruskal-Wallis ANOVA with Dunn’s post-test), and was also higher than the mean age of the severe influenza cohort (41, IQR 30–49) although this difference was not significant (P=0.13 by Kruskal-Wallis ANOVA with Dunn’s post-test). We found no difference in the ratio of female to male subjects between the four cohorts. The mean interval between the start of illness symptoms and BAL sample collection was significantly longer in the moderate influenza cohort (14.6 days, IQR 13–18 days) when compared with the severe influenza cohort (7.5 days, IQR 7–8 days; P=0.007 by Kruskal-Wallis ANOVA with Dunn’s post-test); however, there were no differences between the moderate influenza cohort and the COVID-19 cohort or the severe influenza cohort and the COVID-19 cohort (COVID-19 cohort mean 13.2 days, IQR 10–14 days).
Increased CD14lowCD16+ non-classical monocytes, activated T cells and plasmablast B cells in the bronchoalveolar space of individuals with severe viral pneumonia
We evaluated the absolute number of major adaptive and innate immune subsets in the blood and bronchoalveolar space in our cohort. Changes in the population size of peripheral blood immune cell subsets and their activation status during acute influenza and acute COVID-19 have been extensively described by our group (23, 29) and by others (30–32); therefore, for this analysis, we focused on differences in cells found within the BAL fluid. Using quantitative flow cytometry methods (flow cytometry gating strategies are outlined in Supplementary Figure 1), we discovered that the total immune cellularity, as represented by the number of CD45+ cells in BAL, was increased in the individuals with severe viral pneumonia compared to those with moderate influenza and controls (Figure 1). The absolute number of CD14+ monocytic-lineage cells and CD19+ B cells were elevated during severe disease; however, the absolute number of total T cells and the CD4/CD8 sub-populations were not consistently different between individuals with severe viral pneumonia and those without (Figure 1). The large increase in CD14+ cell counts in the lower airways of individuals with severe viral pneumonia appeared to be driven primarily by significantly elevated CD14highCD16− cell counts and, most prominently, CD14lowCD16+ cell counts (Figure 2A and 2B)).
Figure 1.
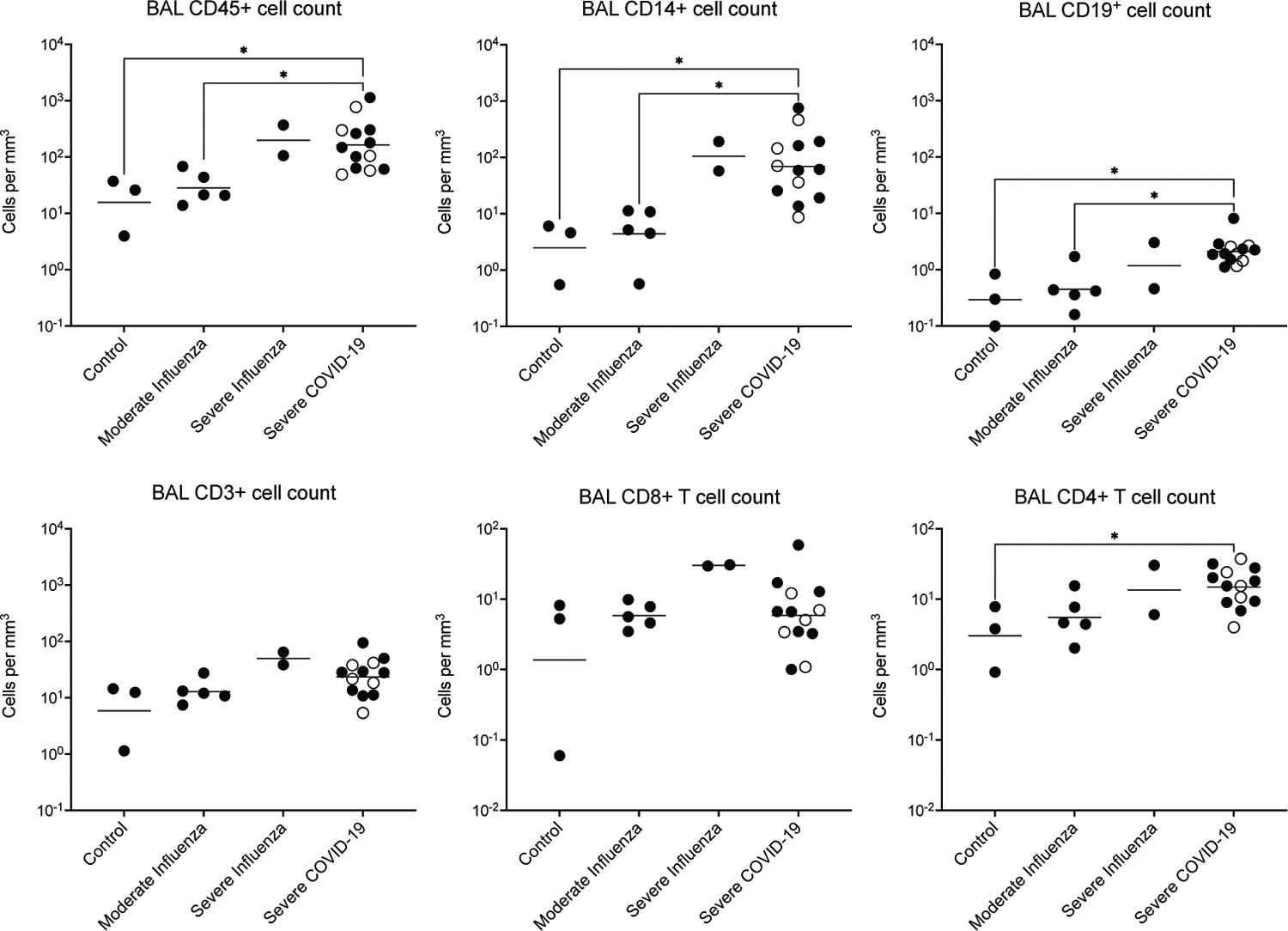
Absolute number of various immune cell subsets in BAL. The indicated cell populations were quantified by flow cytometry using counting beads. Comparisons were made using Kruskal-Wallis ANOVA with Dunn’s multiple comparisons post-test. Significance is indicated by * P<0.05. Open symbols represent COVID-19 patients on chronic immunsuppressive therapy. There were no significant differences between the COVID-19 patients on chronic immunsuppresive therapy and those who were not in any of the measured variables.
Figure 2.

Evaluation of BAL cell populations by flow cytometry. (A) Representative flow cytometry plots for a control, moderate influenza and severe COVID-19 individual illustrating the increasing CD14lowCD16+ population in the severe viral pneumonia subjects. Presented dot plots were gated on single live CD45+CD19−CD3−CD56− cells (see Supplementary Figure 1 for full gating strategies). (B) Absolute cell numbers of the CD14+ cell subsets illustrated in the previous panel. (C-E) Representative flow cytometry plots illustrating a moderate influenza subject and a severe COVID-19 subject for (C) activated CD8+ T cells gated on single live CD3+CD8+CD4− cells, (D) activated CD4+ T cells gated on single live CD3+CD8−CD4+ cells and (E) plasmablast B cells gated on single live CD45+CD19+ cells. (F) Absolute cell numbers of activated CD8+ T cells, activated CD4+ T cells and plasmablast B cells in the BAL of the indicated groups. Numbers on all flow cytometry dot plots indicate the percentage of positive events found within the indicated gate. Activated T cell gates were initially drawn on matched PBMC populations where more events were available for establishing the gates. Significance is indicated by * P<0.05, ** P<0.01 with all testing performed using Kruskal-Wallis ANOVA with Dunn’s multiple comparisons post-test. Open symbols represent COVID-19 patients on chronic immunsuppressive therapy. There were no significant differences between the COVID-19 patients on chronic immunsuppresive therapy and those who were not in any of the measured variables.
Interestingly, we found that the absolute numbers of activated CD8+ and activated CD4+ T cells were significantly increased in BAL fluid during severe COVID-19 (Figure 2C, 2D and 2F). In addition, we noted increased populations of CD19+ B cell plasmablasts (Figure 2E and 2F). We did not have cellular components from the BAL fluid available for analysis from two of four severe influenza subjects; however, increased CD14lowCD16+ cells and high absolute numbers of activated T cells and B cells were also noted in the BAL of our two included severe influenza subjects (Figure 2B and 2F).
Bronchoalveolar concentration of multiple cytokines and chemokines is increased in severe viral pneumonia leading to respiratory failure
We next measured the concentration of 35 individual cytokines and chemokines in the blood and temporally matched samples of BAL fluid from each study subject. We found that many cytokines and chemokines were elevated in the plasma of individuals with moderate or severe influenza and severe COVID-19 when compared with the four control samples (Supplementary Figure 2A), suggesting that, despite the longer interval between symptom start and collection, there was still ongoing systemic inflammation in some of our subjects with moderate influenza infection. Some cytokines were selectively higher in plasma when compared to BAL fluid regardless of infection status, including IL-12, RANTES and EOTAXIN (Supplementary Figure 2A). Notably, lower relative concentrations of nearly all cytokines were found in the BAL fluid of control and moderate influenza subjects (Figure 3A and Supplementary Figure 2A) These subjects clustered together into one group when analyzing all of the BAL samples with Euclidean hierarchical clustering (Figure 3A). We also found a large and diverse number of cytokines expressed in the BAL of all severe influenza and COVID-19 subjects which clustered into three distinct groups (Figure 3A). A group of four individuals had some of the highest relative expression levels of multiple cytokines among the BAL samples and clustered together – three individuals with severe influenza and one with severe COVID-19 (Figure 3A). The five subjects with severe COVID-19 on chronic immunosuppressive therapy equally segregated into the three distinct severe illness clusters composing 1/3 of the first cluster, 3/10 of the second cluster and 1/4 of the third cluster; therefore based upon the expression level of these 35 cytokines, the immunosuppressed COVID-19 subjects did not exhibit a different pattern of cytokine expression during severe illness when compared with the other severe viral respiratory failure subjects.
Figure 3.

Elevated BAL cytokines in patients with severe viral pneumonia. (A) Euclidean hierarchical clustering analysis of all BAL cytokine measurements. The concentration of each cytokine column was normalized by setting the highest value to 1 and the lowest value to 0. (B) Representative BAL cytokine analysis graphs for six of thirty-five measured cytokines with the highest magnitude increases during severe disease. (C) Selective elevation of IL-1 family cytokines and RANTES in severe influenza but not in severe COVID-19. In (B) and (C) cytokine concentrations are measured in pg/mL and plotted on a logarithmic scale. Individual subject values are plotted (each point) along with the group median value (line) and the 95% confidence interval. Significance is indicated by * P<0.05, ** P<0.01, and *** P<0.001, with all testing performed using Kruskal-Wallis ANOVA with Dunn’s multiple comparisons post-test.
When comparing the expression level of individual cytokines in the BAL between the four cohorts of subjects, we found that 28 of the 35 cytokines and chemokines were significantly elevated in the severe influenza cohort, the severe COVID-19 cohort or both (Figure 3B, Figure 3C and Supplementary Figure 2). Many of the highest magnitude increases we noted between the control or moderate influenza cohorts and the two severe viral pneumonia cohorts included cytokines and chemokines typically expressed by monocytic-lineage cells that enhance pro-inflammatory Th1-type immune responses, including IL-6, IL-8, MCP-1, MIG, IP-10, IL-12 and MIP-1ß (Figure 3B and Supplementary Figure 2). IL-1 signaling was noted to be significantly increased in BAL samples from the severe influenza cohort, but not the severe COVID-19 cohort (Figure 3C). Also, the chemokine RANTES appeared to be selectively increased in BAL from individuals with severe influenza but not in individuals with severe COVID-19 (Figure 3C), suggesting small, but present differences in the lower airway inflammatory environment during severe infection with these two viruses.
The measured plasma concentration of IP-10 correlates with the measured BAL concentration
Given the difficulty in sampling and measuring lower airway inflammation in human patients during acute viral infection, we sought to use our dataset to determine if individual circulating blood cytokine concentrations correlate with hyperinflammatory bronchoalveolar cytokine expression. To do this, we performed linear regression of the plasma versus the BAL concentration of each measured cytokine. We performed our initial analysis in a combined cohort that included the 13 subjects with severe COVID-19 and the 4 subjects with severe influenza (Figure 4A and Supplementary Figure 3). IP-10, also known as CXCL10, was the only cytokine or chemokine of the 35 measured which significantly correlated between the blood and BAL in this combined cohort of individuals with severe viral pneumonia (Figure 4A and Supplementary Figure 3). Furthermore, the strength of the correlation between the blood and bronchoalveolar concentration of IP-10 as measured by the R2 value was quite robust. Interestingly, many inflammatory cytokines commonly described as peripheral blood markers of severe influenza and COVID-19, including IL-6, IL-8, MCP-1, IL-1RA, G-CSF, IL-1 beta and IL-10 (3, 23, 33), did not correlate between blood and BAL (Figure 4A and Supplementary Figure 3) despite the significantly increased concentration of many of these molecules in the BAL fluid of individuals with severe viral pneumonia (Figure 3 and Supplementary Figure 2).
Figure 4.
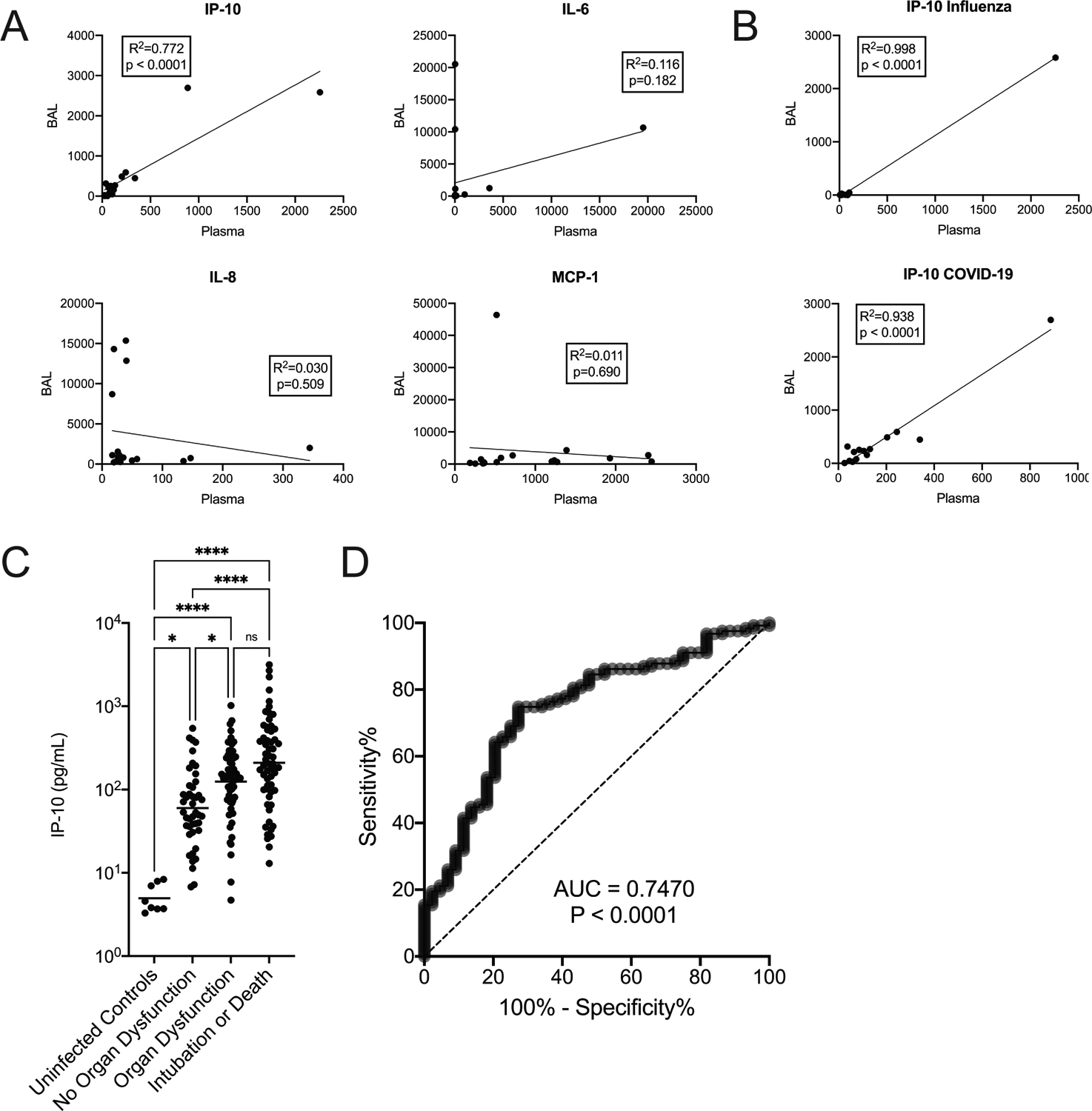
Plasma IP-10 concentrations serve as a marker of lower airway inflammation and predict severe disease outcomes in subjects with COVID-19. (A) Representative linear regression analysis plots for four of the thirty-five cytokines comparing blood plasma on the x-axis and BAL on the y-axis. All cytokine concentrations are in pg/mL. This analysis was performed using the first matched blood and BAL samples from each of the individuals with severe COVID-19 and severe influenza (N=17). The P value threshold for significance was corrected to < 0.0015 using the Bonferroni method. (B) Linear regression analysis of IP-10 in the combined moderate influenza and severe influenza cohort (top panel, N=10) and the severe COVID-19 cohort (bottom panel, N=14, includes the 350–425 day 28 sample that was excluded in panel A). (C) Blood plasma IP-10 concentrations in 168 individuals with PCR-diagnosed SARS-CoV-2 infection evaluated in hospital and 8 control uninfected individuals. This data set has been previously published (23), but this is a new analysis of the earlier data. Groups were compared using Kruskal-Wallis ANOVA with Dunn’s multiple comparisons post-test. Significance is indicated by * P<0.05, **** P<0.0001. ns – not significant. (D) Receiver operating characteristic curve evaluating the ability of various concentrations of plasma IP-10 (in pg/mL) to predict the composite outcome of organ dysfunction, intubation or death in the cohort of 168 patients with COVID-19. AUC – area under the curve.
To evaluate if a disease-specific rather than a general hyperinflammatory viral pneumonia phenotype drives the IP-10 correlation between blood and BAL that we observe, we evaluated the correlation separately in the severe COVID-19 cohort and in the combined moderate and severe influenza cohort. The IP-10 correlation remained significant in each individual disease (Figure 4B).
Circulating plasma IP-10 concentration predicts organ dysfunction, intubation or death in an independent cohort of patients with COVID-19
We next wanted to determine if the correlation we report between elevated plasma concentrations of IP-10 and elevated BAL concentrations could signal that plasma IP-10 might predict organ dysfunction in human patients, including respiratory failure, intubation or death. To accomplish this, we re-analyzed our previously published dataset of measured plasma cytokine and chemokine concentrations obtained within 48 hours of hospital admission in a cohort of 168 prospectively sampled subjects with COVID-19 (23). We reasoned that if circulating IP-10 were able to serve as a marker of a hyperinflammatory bronchoalveolar environment during respiratory failure in COVID-19 as we observe in our small cohort in the present study, then increasing circulating concentrations in the blood might predict hyperinflammatory respiratory failure in a larger cohort of patients. Indeed, we found that elevated IP-10 was significantly associated with COVID-19 severity and elevated levels predicted organ dysfunction, intubation or death (Figure 4C). Furthermore, circulating plasma IP-10 concentrations alone could serve as a diagnostic test to predict organ dysfunction, intubation or death in the cohort of 168 COVID-19 patients with an area under the receiver operating curve of 0.747 (Figure 4D). Using an IP-10 concentration cutoff of 418 pg/mL such a test would have 20% sensitivity and 98% specificity for organ dysfunction, intubation or death. A plasma IP-10 concentration cutoff of 89 pg/mL would provide 75% sensitivity and 73% specificity for organ dysfunction, intubation or death. Our previously reported dataset (23) included 26 influenza-infected subjects. We detected elevated plasma IP-10 in the influenza patients compared with uninfected individuals (data not shown) as others have reported (14). However, this dataset was not large enough to evaluate IP-10 associations with respiratory failure in influenza patients.
Discussion
In this study, we comprehensively characterize the lower airway immune response in four cohorts of human subjects: 1) subjects without acute infection, 2) influenza-infected subjects who are symptomatic but have no evidence of respiratory failure, 3) influenza-infected subjects with acute respiratory failure and 4) COVID-19 subjects with respiratory failure. We observe increased absolute numbers of activated T cells, B cells and inflammatory-type monocyte-lineage cells in the bronchoalveolar space of subjects with respiratory failure. Furthermore, we find high magnitude elevations of the cytokines and chemokines IL-6, IL-8, MCP-1, MIG, IP-10, IL-12 and MIP-1ß in the lower airways of the individuals with severe disease and respiratory failure. These cytokines are known to drive M1 monocyte, activated Th1, and cytotoxic T cell recruitment. Our findings are in line with a recent report in 23 subjects with severe COVID-19 that demonstrated an increased frequency of inflammatory transitional and non-classical monocytes in bronchial washings of individuals with respiratory failure but did not quantify the absolute number of this subset nor compare it to individuals without acute infection (17). The observations in our COVID-19 cohort also comport with another recent study demonstrating broad expansion of monocyte-derived alveolar macrophages in severe COVID-19 and associated increased recruitment of activated T cells to the bronchoalveolar space (34). Indeed, our limited findings in two individuals with severe influenza suggest that the model proposed by Grant and colleagues for COVID-19 (34), which our present observations support, may also apply to severe influenza pneumonia that leads to hyperinflammatory respiratory failure. In fact, previously published literature reported increased frequencies of activated T cells in BAL fluid from two individuals with severe influenza (14) further supporting this position. Finally, we did not observe any of these cytokine elevations or cellular immune changes in our moderate influenza cohort arguing that the inflammatory cytokine and cellular changes we observe are unique to dysregulated disease which leads to respiratory failure. However, this finding may be limited by the prolonged interval between illness onset and sample acquisition in our moderate influenza cohort when compared with our severe influenza cohort, despite continued elevated peripheral blood cytokine levels in a subset of our moderate influenza patients during BAL sampling.
We also demonstrate an association between increased circulating peripheral blood IP-10 concentration and bronchoavleolar inflammation. Furthermore, we show that blood IP-10 concentration can predict organ failure, intubation and death in a separate large COVID-19 patient cohort. Previous studies have reported associations between increasing plasma or serum IP-10 concentration and poor outcomes in patients with COVID-19 (19, 35). Increasing blood IP-10 concentrations have also been associated with increased illness severity in seasonal (36) and avian (20, 37) influenza infection. To the best of our knowledge, our work is the first to link these IP-10 elevations in circulating blood to elevated levels found within the bronchoalveolar space of human patients with severe seasonal influenza and COVID-19. Our findings suggest that measurement of peripheral blood IP-10 in individuals with severe influenza or COVID-19 may identify those with hyperinflammatory respiratory failure that may respond to immunosuppressive therapies such as corticosteroids and perhaps other targeted therapies.
Several peripheral blood cytokines have been put forward as markers of severe influenza and COVID-19 including IL-6, IL-8, MCP-1, IL-1RA, G-CSF, IL-1 beta and IL-10 (3, 23, 33). The circulating concentrations of all of these cytokines correlate with poor disease outcomes in larger cohorts of patients. Interestingly, none of these cytokines correlated between the blood and BAL in our present study, illustrating the relative weakness of these cytokines as peripheral blood biomarkers of hyperinflammatory respiratory failure when compared with the measurement of IP-10 in COVID-19. We believe that this point is best illustrated by the IL-6 cytokine. IL-6 was significantly elevated in the BAL of all subjects with severe viral pneumonia in our study by more than a 10-fold increase above values found in the BAL of controls or moderate influenza subjects. However, plasma IL-6 did not consistently serve as a marker for this bronchoalveolar elevation – 2 of the 3 individuals with the highest BAL concentration of IL-6 and values greater than 10,000 pg/mL in the BAL had plasma values of 38 and 39 pg/mL. These two values were in the lower half of the plasma measurements in all 17 of the severe viral pneumonia subjects in this study and fall within the range of healthy-uninfected individuals in other cohorts (23). Therefore, despite the importance of profound elevations of IL-6 in the BAL of individuals with severe viral pneumonia and the strong association between circulating plasma or serum levels of this cytokine and disease severity, there are still individuals with severe hyperinflammatory viral pneumonia who do not have remarkably elevated blood levels of IL-6.
Recent in vitro work has shown that human nasal epithelial cells selectively produce IP-10 on the basolateral surface following SARS-CoV-2 infection or seasonal influenza infection (38). Therefore, the IP-10 increases we observe may be due to the recruitment of inflammatory immune cells that express this chemokine in the lung or to the direct expression of IP-10 by respiratory epithelial cells following infection. If further work demonstrates that the IP-10 increases are related to direct viral infection of respiratory epithelial cells in vivo, it would suggest a mechanism whereby blocking IP-10 – a chemoattractant for pathogenic monocytes and activated T cells – may inhibit a key triggering event in the development of hyperinflammatory respiratory failure. Indeed, a mouse study found that genetically eliminating IP-10 or blocking IP-10 activity with a monoclonal antibody during H1N1 influenza infection reduced lung inflammation, animal weight loss and mortality in two models of severe influenza (36). Targeted therapies blocking IP-10 chemokine activity in human patients with hyperinflammatory respiratory failure as classified by elevated peripheral blood concentrations of IP-10 may hold promise as a therapy for individuals with severe influenza and COVID-19.
Our study does have limitations. Older age has been associated with increased inflammatory cytokine responses and diminished development of adaptive immune responses (39, 40). However, recruitment for our study was limited to the collection of samples from individuals with severe illness, and the known association of severe COVID-19 with increasing age (4) limited our ability to collect samples from comparable cohorts of younger subjects. This reflects the intrinsic nature of the populations affected by severe influenza and severe COVID-19 rather than sampling bias. Furthermore, the quicker deterioration of the clinical condition in severe influenza patients when compared with COVID-19 patients has been noted in larger cohorts (23), reflecting the differences, once again, between the time-course and pathophysiology of these two viral diseases. Our significantly longer interval between illness onset and sampling in the moderate influenza and severe influenza cohorts reflects the rapid onset of disease in individuals with severe influenza and may limit direct comparisons between our severe and moderate influenza cohorts. Finally, the association we describe between circulating IP-10 and severe COVID-19, while also observed by other scientific groups in various human cohorts, will require formal validation in a large, multicenter prospective study prior to being applied in the clinical setting.
In conclusion, we find increased absolute numbers of inflammatory-type non-classical monocytes and activated T and B cells in the bronchoalveolar space of individuals with severe viral pneumonia that are not observed in individuals with acute influenza who do not experience respiratory failure. These cellular changes are associated with significant increases in many different cytokines and chemokines in the bronchoalveolar space, most notably those expressed by epithelial cells and innate immune cells which are known to drive Th1-type immune responses. In addition, we demonstrate that plasma IP-10 serves as a marker of severe hyperinflammatory respiratory failure. Measurement of circulating IP-10 predicts respiratory failure in COVID-19 and may allow more precise targeting of anti-inflammatory therapies to those who will benefit the most.
Supplementary Material
Key Points:
Humans with severe viral pneumonia have excessive cytokines in the lower airways.
This inflammation is associated with influxes of monocytes and activated lymphocytes.
Blood IP-10 concentration correlates with lung inflammation and severe disease.
Acknowledgements
The authors would like to thank Hailey Freres and Diane Bender in the Bursky Center for Human Immunology & Immunotherapy Program Immunomonitoring Laboratory for their assistance with Luminex assays performed in this study.
This work was supported by grants from the Barnes Jewish Hospital Foundation awarded to PAM and CVG and by a grant from the Washington University Institute of Clinical and Translational Sciences awarded to PAM. The Washington University Institute of Clinical and Translational Sciences is supported by grant UL1TR002345 from the National Center for Advancing Translational Sciences (NCATS) of the National Institutes of Health (NIH). The content is solely the responsibility of the authors and does not necessarily represent the official view of the NIH. Cytokine measurements were supported, in part, by the Bursky Center for Human Immunology and Immunotherapy Programs at Washington University, Immunomonitoring Laboratory. This project also received funding from the National Council of Science and Technology of Mexico (CONACyT) under the research contracts: SECTEI/050/2020, Secretaría de Ciencia, Tecnología e Innovación de la Ciudad de México (SECTEI CDMX); FORDECYT/10SE/2020/05/14-06 and FORDECYT/10SE/2020/05/14-07.
Footnotes
PAM is listed as inventor on a patent application based on the findings of this study. All other authors declare that they do not have any commercial interests or other associations that pose a conflict of interest with this work.
References
- 1.Grasselli G, Greco M, Zanella A, Albano G, Antonelli M, Bellani G, Bonanomi E, Cabrini L, Carlesso E, Castelli G, Cattaneo S, Cereda D, Colombo S, Coluccello A, Crescini G, Forastieri Molinari A, Foti G, Fumagalli R, Iotti GA, Langer T, Latronico N, Lorini FL, Mojoli F, Natalini G, Pessina CM, Ranieri VM, Rech R, Scudeller L, Rosano A, Storti E, Thompson BT, Tirani M, Villani PG, Pesenti A, Cecconi M, and C.-L. I. Network. 2020. Risk Factors Associated With Mortality Among Patients With COVID-19 in Intensive Care Units in Lombardy, Italy. JAMA Intern Med 180: 1345–1355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Grasselli G, Zangrillo A, Zanella A, Antonelli M, Cabrini L, Castelli A, Cereda D, Coluccello A, Foti G, Fumagalli R, Iotti G, Latronico N, Lorini L, Merler S, Natalini G, Piatti A, Ranieri MV, Scandroglio AM, Storti E, Cecconi M, Pesenti A, and C.-L. I. Network. 2020. Baseline Characteristics and Outcomes of 1591 Patients Infected With SARS-CoV-2 Admitted to ICUs of the Lombardy Region, Italy. JAMA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang C, Wang Y, Li X, Ren L, Zhao J, Hu Y, Zhang L, Fan G, Xu J, Gu X, Cheng Z, Yu T, Xia J, Wei Y, Wu W, Xie X, Yin W, Li H, Liu M, Xiao Y, Gao H, Guo L, Xie J, Wang G, Jiang R, Gao Z, Jin Q, Wang J, and Cao B. 2020. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 395: 497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, and Prescott HC. 2020. Pathophysiology, Transmission, Diagnosis, and Treatment of Coronavirus Disease 2019 (COVID-19): A Review. JAMA 324: 782–793. [DOI] [PubMed] [Google Scholar]
- 5.Iuliano AD, Roguski KM, Chang HH, Muscatello DJ, Palekar R, Tempia S, Cohen C, Gran JM, Schanzer D, Cowling BJ, Wu P, Kyncl J, Ang LW, Park M, Redlberger-Fritz M, Yu H, Espenhain L, Krishnan A, Emukule G, van Asten L, Pereira da Silva S, Aungkulanon S, Buchholz U, Widdowson MA, Bresee JS, and N. Global Seasonal Influenza-associated Mortality Collaborator. 2018. Estimates of global seasonal influenza-associated respiratory mortality: a modelling study. Lancet 391: 1285–1300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Huang QS, Bandaranayake D, Wood T, Newbern EC, Seeds R, Ralston J, Waite B, Bissielo A, Prasad N, Todd A, Jelley L, Gunn W, McNicholas A, Metz T, Lawrence S, Collis E, Retter A, Wong SS, Webby R, Bocacao J, Haubrock J, Mackereth G, Turner N, McArdle B, Cameron J, Reynolds EG, Baker MG, Grant CC, McArthur C, Roberts S, Trenholme A, Wong C, Taylor S, Thomas P, Duque J, Gross D, Thompson MG, Widdowson MA, I. Southern Hemisphere, R. Vaccine Effectiveness, and T. Surveillance Investigation. 2019. Risk Factors and Attack Rates of Seasonal Influenza Infection: Results of the Southern Hemisphere Influenza and Vaccine Effectiveness Research and Surveillance (SHIVERS) Seroepidemiologic Cohort Study. J Infect Dis 219: 347–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Phua J, Weng L, Ling L, Egi M, Lim CM, Divatia JV, Shrestha BR, Arabi YM, Ng J, Gomersall CD, Nishimura M, Koh Y, Du B, and G. Asian Critical Care Clinical Trials. 2020. Intensive care management of coronavirus disease 2019 (COVID-19): challenges and recommendations. Lancet Respir Med 8: 506–517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Alhazzani W, Moller MH, Arabi YM, Loeb M, Gong MN, Fan E, Oczkowski S, Levy MM, Derde L, Dzierba A, Du B, Aboodi M, Wunsch H, Cecconi M, Koh Y, Chertow DS, Maitland K, Alshamsi F, Belley-Cote E, Greco M, Laundy M, Morgan JS, Kesecioglu J, McGeer A, Mermel L, Mammen MJ, Alexander PE, Arrington A, Centofanti JE, Citerio G, Baw B, Memish ZA, Hammond N, Hayden FG, Evans L, and Rhodes A. 2020. Surviving Sepsis Campaign: Guidelines on the Management of Critically Ill Adults with Coronavirus Disease 2019 (COVID-19). Crit Care Med 48: e440–e469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tobin MJ 2020. Basing Respiratory Management of COVID-19 on Physiological Principles. Am J Respir Crit Care Med 201: 1319–1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Beigel JH, Tomashek KM, Dodd LE, Mehta AK, Zingman BS, Kalil AC, Hohmann E, Chu HY, Luetkemeyer A, Kline S, Lopez de Castilla D, Finberg RW, Dierberg K, Tapson V, Hsieh L, Patterson TF, Paredes R, Sweeney DA, Short WR, Touloumi G, Lye DC, Ohmagari N, Oh MD, Ruiz-Palacios GM, Benfield T, Fatkenheuer G, Kortepeter MG, Atmar RL, Creech CB, Lundgren J, Babiker AG, Pett S, Neaton JD, Burgess TH, Bonnett T, Green M, Makowski M, Osinusi A, Nayak S, Lane HC, and A.-S. G. Members. 2020. Remdesivir for the Treatment of Covid-19 - Final Report. N Engl J Med 383: 1813–1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lytras T, Mouratidou E, Andreopoulou A, Bonovas S, and Tsiodras S. 2019. Effect of Early Oseltamivir Treatment on Mortality in Critically Ill Patients With Different Types of Influenza: A Multiseason Cohort Study. Clin Infect Dis 69: 1896–1902. [DOI] [PubMed] [Google Scholar]
- 12.Group RC, Horby P, Lim WS, Emberson JR, Mafham M, Bell JL, Linsell L, Staplin N, Brightling C, Ustianowski A, Elmahi E, Prudon B, Green C, Felton T, Chadwick D, Rege K, Fegan C, Chappell LC, Faust SN, Jaki T, Jeffery K, Montgomery A, Rowan K, Juszczak E, Baillie JK, Haynes R, and Landray MJ. 2020. Dexamethasone in Hospitalized Patients with Covid-19 - Preliminary Report. N Engl J Med. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Group, W. H. O. R. E. A. f. C.-T. W., Sterne JAC, Murthy S, Diaz JV, Slutsky AS, Villar J, Angus DC, Annane D, Azevedo LCP, Berwanger O, Cavalcanti AB, Dequin PF, Du B, Emberson J, Fisher D, Giraudeau B, Gordon AC, Granholm A, Green C, Haynes R, Heming N, Higgins JPT, Horby P, Juni P, Landray MJ, Le Gouge A, Leclerc M, Lim WS, Machado FR, McArthur C, Meziani F, Moller MH, Perner A, Petersen MW, Savovic J, Tomazini B, Veiga VC, Webb S, and Marshall JC. 2020. Association Between Administration of Systemic Corticosteroids and Mortality Among Critically Ill Patients With COVID-19: A Meta-analysis. JAMA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Zhao Y, Zhang YH, Denney L, Young D, Powell TJ, Peng YC, Li N, Yan HP, Wang DY, Shu YL, Kendrick Y, McMichael AJ, Ho LP, and Dong T. 2012. High levels of virus-specific CD4+ T cells predict severe pandemic influenza A virus infection. Am J Respir Crit Care Med 186: 1292–1297. [DOI] [PubMed] [Google Scholar]
- 15.Chua RL, Lukassen S, Trump S, Hennig BP, Wendisch D, Pott F, Debnath O, Thurmann L, Kurth F, Volker MT, Kazmierski J, Timmermann B, Twardziok S, Schneider S, Machleidt F, Muller-Redetzky H, Maier M, Krannich A, Schmidt S, Balzer F, Liebig J, Loske J, Suttorp N, Eils J, Ishaque N, Liebert UG, von Kalle C, Hocke A, Witzenrath M, Goffinet C, Drosten C, Laudi S, Lehmann I, Conrad C, Sander LE, and Eils R. 2020. COVID-19 severity correlates with airway epithelium-immune cell interactions identified by single-cell analysis. Nat Biotechnol 38: 970–979. [DOI] [PubMed] [Google Scholar]
- 16.Liao M, Liu Y, Yuan J, Wen Y, Xu G, Zhao J, Cheng L, Li J, Wang X, Wang F, Liu L, Amit I, Zhang S, and Zhang Z. 2020. Single-cell landscape of bronchoalveolar immune cells in patients with COVID-19. Nat Med 26: 842–844. [DOI] [PubMed] [Google Scholar]
- 17.Sanchez-Cerrillo I, Landete P, Aldave B, Sanchez-Alonso S, Sanchez-Azofra A, Marcos-Jimenez A, Avalos E, Alcaraz-Serna A, de Los Santos I, Mateu-Albero T, Esparcia L, Lopez-Sanz C, Martinez-Fleta P, Gabrie L, Del Campo Guerola L, de la Fuente H, Calzada MJ, Gonzalez-Alvaro I, Alfranca A, Sanchez-Madrid F, Munoz-Calleja C, Soriano JB, Ancochea J, Martin-Gayo E, Reinmun C, and E. groups. 2020. COVID-19 severity associates with pulmonary redistribution of CD1c+ DCs and inflammatory transitional and nonclassical monocytes. J Clin Invest. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Blot M, Jacquier M, Aho Glele LS, Beltramo G, Nguyen M, Bonniaud P, Prin S, Andreu P, Bouhemad B, Bour JB, Binquet C, Piroth L, Pais de Barros JP, Masson D, Quenot JP, Charles PE, and g. Pneumochondrie study. 2020. CXCL10 could drive longer duration of mechanical ventilation during COVID-19 ARDS. Crit Care 24: 632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hue S, Beldi-Ferchiou A, Bendib I, Surenaud M, Fourati S, Frapard T, Rivoal S, Razazi K, Carteaux G, Delfau-Larue MH, Mekontso-Dessap A, Audureau E, and de Prost N. 2020. Uncontrolled Innate and Impaired Adaptive Immune Responses in Patients with COVID-19 Acute Respiratory Distress Syndrome. Am J Respir Crit Care Med 202: 1509–1519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.de Jong MD, Simmons CP, Thanh TT, Hien VM, Smith GJ, Chau TN, Hoang DM, Chau NV, Khanh TH, Dong VC, Qui PT, Cam BV, Ha do Q, Guan Y, Peiris JS, Chinh NT, Hien TT, and Farrar J. 2006. Fatal outcome of human influenza A (H5N1) is associated with high viral load and hypercytokinemia. Nat Med 12: 1203–1207. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fajgenbaum DC, and June CH. 2020. Cytokine Storm. N Engl J Med 383: 2255–2273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Moore JB, and June CH. 2020. Cytokine release syndrome in severe COVID-19. Science 368: 473–474. [DOI] [PubMed] [Google Scholar]
- 23.Mudd PA, Crawford JC, Turner JS, Souquette A, Reynolds D, Bender D, Bosanquet JP, Anand NJ, Striker DA, Martin RS, Boon ACM, House SL, Remy KE, Hotchkiss RS, Presti RM, O’Halloran JA, Powderly WG, Thomas PG, and Ellebedy AH. 2020. Distinct inflammatory profiles distinguish COVID-19 from influenza with limited contributions from cytokine storm. Sci Adv 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kox M, Waalders NJB, Kooistra EJ, Gerretsen J, and Pickkers P. 2020. Cytokine Levels in Critically Ill Patients With COVID-19 and Other Conditions. JAMA. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sinha P, Matthay MA, and Calfee CS. 2020. Is a “Cytokine Storm” Relevant to COVID-19? JAMA Intern Med. [DOI] [PubMed] [Google Scholar]
- 26.Salama C, Han J, Yau L, Reiss WG, Kramer B, Neidhart JD, Criner GJ, Kaplan-Lewis E, Baden R, Pandit L, Cameron ML, Garcia-Diaz J, Chavez V, Mekebeb-Reuter M, Lima de Menezes F, Shah R, Gonzalez-Lara MF, Assman B, Freedman J, and Mohan SV. 2021. Tocilizumab in Patients Hospitalized with Covid-19 Pneumonia. N Engl J Med 384: 20–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stone JH, Frigault MJ, Serling-Boyd NJ, Fernandes AD, Harvey L, Foulkes AS, Horick NK, Healy BC, Shah R, Bensaci AM, Woolley AE, Nikiforow S, Lin N, Sagar M, Schrager H, Huckins DS, Axelrod M, Pincus MD, Fleisher J, Sacks CA, Dougan M, North CM, Halvorsen YD, Thurber TK, Dagher Z, Scherer A, Wallwork RS, Kim AY, Schoenfeld S, Sen P, Neilan TG, Perugino CA, Unizony SH, Collier DS, Matza MA, Yinh JM, Bowman KA, Meyerowitz E, Zafar A, Drobni ZD, Bolster MB, Kohler M, D’Silva KM, Dau J, Lockwood MM, Cubbison C, Weber BN, Mansour MK, and B. B. T. T. Investigators. 2020. Efficacy of Tocilizumab in Patients Hospitalized with Covid-19. N Engl J Med 383: 2333–2344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Supady A, Weber E, Rieder M, Lother A, Niklaus T, Zahn T, Frech F, Muller S, Kuhl M, Benk C, Maier S, Trummer G, Flugler A, Kruger K, Sekandarzad A, Stachon P, Zotzmann V, Bode C, Biever PM, Staudacher D, Wengenmayer T, Graf E, and Duerschmied D. 2021. Cytokine adsorption in patients with severe COVID-19 pneumonia requiring extracorporeal membrane oxygenation (CYCOV): a single centre, open-label, randomised, controlled trial. Lancet Respir Med. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Turner JS, Lei T, Schmitz AJ, Day A, Choreno-Parra JA, Jimenez-Alvarez L, Cruz-Lagunas A, House SL, Zuniga J, Ellebedy AH, and Mudd PA. 2020. Impaired Cellular Immune Responses During the First Week of Severe Acute Influenza Infection. J Infect Dis 222: 1235–1244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lucas C, Wong P, Klein J, Castro TBR, Silva J, Sundaram M, Ellingson MK, Mao T, Oh JE, Israelow B, Takahashi T, Tokuyama M, Lu P, Venkataraman A, Park A, Mohanty S, Wang H, Wyllie AL, Vogels CBF, Earnest R, Lapidus S, Ott IM, Moore AJ, Muenker MC, Fournier JB, Campbell M, Odio CD, Casanovas-Massana A, Yale IT, Herbst R, Shaw AC, Medzhitov R, Schulz WL, Grubaugh ND, Dela Cruz C, Farhadian S, Ko AI, Omer SB, and Iwasaki A. 2020. Longitudinal analyses reveal immunological misfiring in severe COVID-19. Nature 584: 463–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hadjadj J, Yatim N, Barnabei L, Corneau A, Boussier J, Smith N, Pere H, Charbit B, Bondet V, Chenevier-Gobeaux C, Breillat P, Carlier N, Gauzit R, Morbieu C, Pene F, Marin N, Roche N, Szwebel TA, Merkling SH, Treluyer JM, Veyer D, Mouthon L, Blanc C, Tharaux PL, Rozenberg F, Fischer A, Duffy D, Rieux-Laucat F, Kerneis S, and Terrier B. 2020. Impaired type I interferon activity and inflammatory responses in severe COVID-19 patients. Science 369: 718–724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Files JK, Boppana S, Perez MD, Sarkar S, Lowman KE, Qin K, Sterrett S, Carlin E, Bansal A, Sabbaj S, Long DM, Kutsch O, Kobie J, Goepfert PA, and Erdmann N. 2021. Sustained cellular immune dysregulation in individuals recovering from SARS-CoV-2 infection. J Clin Invest 131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Guo XJ, and Thomas PG. 2017. New fronts emerge in the influenza cytokine storm. Semin Immunopathol 39: 541–550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Grant RA, Morales-Nebreda L, Markov NS, Swaminathan S, Querrey M, Guzman ER, Abbott DA, Donnelly HK, Donayre A, Goldberg IA, Klug ZM, Borkowski N, Lu Z, Kihshen H, Politanska Y, Sichizya L, Kang M, Shilatifard A, Qi C, Lomasney JW, Argento AC, Kruser JM, Malsin ES, Pickens CO, Smith SB, Walter JM, Pawlowski AE, Schneider D, Nannapaneni P, Abdala-Valencia H, Bharat A, Gottardi CJ, Budinger GRS, Misharin AV, Singer BD, Wunderink RG, and N. S. S. Investigators. 2021. Circuits between infected macrophages and T cells in SARS-CoV-2 pneumonia. Nature. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Laing AG, Lorenc A, Del Molino Del Barrio I, Das A, Fish M, Monin L, Munoz-Ruiz M, McKenzie DR, Hayday TS, Francos-Quijorna I, Kamdar S, Joseph M, Davies D, Davis R, Jennings A, Zlatareva I, Vantourout P, Wu Y, Sofra V, Cano F, Greco M, Theodoridis E, Freedman J, Gee S, Chan JNE, Ryan S, Bugallo-Blanco E, Peterson P, Kisand K, Haljasmagi L, Chadli L, Moingeon P, Martinez L, Merrick B, Bisnauthsing K, Brooks K, Ibrahim MAA, Mason J, Lopez Gomez F, Babalola K, Abdul-Jawad S, Cason J, Mant C, Seow J, Graham C, Doores KJ, Di Rosa F, Edgeworth J, Shankar-Hari M, and Hayday AC. 2020. A dynamic COVID-19 immune signature includes associations with poor prognosis. Nat Med. [DOI] [PubMed] [Google Scholar]
- 36.Wang W, Yang P, Zhong Y, Zhao Z, Xing L, Zhao Y, Zou Z, Zhang Y, Li C, Li T, Wang C, Wang Z, Yu X, Cao B, Gao X, Penninger JM, Wang X, and Jiang C. 2013. Monoclonal antibody against CXCL-10/IP-10 ameliorates influenza A (H1N1) virus induced acute lung injury. Cell Res 23: 577–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Chi Y, Zhu Y, Wen T, Cui L, Ge Y, Jiao Y, Wu T, Ge A, Ji H, Xu K, Bao C, Zhu Z, Qi X, Wu B, Shi Z, Tang F, Xing Z, and Zhou M. 2013. Cytokine and chemokine levels in patients infected with the novel avian influenza A (H7N9) virus in China. J Infect Dis 208: 1962–1967. [DOI] [PubMed] [Google Scholar]
- 38.Gamage AM, Tan KS, Chan WOY, Liu J, Tan CW, Ong YK, Thong M, Andiappan AK, Anderson DE, Wang Y, and Wang LF. 2020. Infection of human Nasal Epithelial Cells with SARS-CoV-2 and a 382-nt deletion isolate lacking ORF8 reveals similar viral kinetics and host transcriptional profiles. PLoS Pathog 16: e1009130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Michaud M, Balardy L, Moulis G, Gaudin C, Peyrot C, Vellas B, Cesari M, and Nourhashemi F. 2013. Proinflammatory cytokines, aging, and age-related diseases. J Am Med Dir Assoc 14: 877–882. [DOI] [PubMed] [Google Scholar]
- 40.Nikolich-Zugich J 2018. The twilight of immunity: emerging concepts in aging of the immune system. Nat Immunol 19: 10–19. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


