Abstract
Objectives
Coronavirus disease 2019 (COVID-19) -associated pulmonary aspergillosis (CAPA) has emerged as a complication in critically ill COVID-19 patients. The objectives of this multinational study were to determine the prevalence of CAPA in patients with COVID-19 in intensive care units (ICU) and to investigate risk factors for CAPA as well as outcome.
Methods
The European Confederation of Medical Mycology (ECMM) conducted a multinational study including 20 centres from nine countries to assess epidemiology, risk factors and outcome of CAPA. CAPA was defined according to the 2020 ECMM/ISHAM consensus definitions.
Results
A total of 592 patients were included in this study, including 11 (1.9%) patients with histologically proven CAPA, 80 (13.5%) with probable CAPA, 18 (3%) with possible CAPA and 483 (81.6%) without CAPA. CAPA was diagnosed a median of 8 days (range 0–31 days) after ICU admission predominantly in older patients (adjusted hazard ratio (aHR) 1.04 per year; 95% CI 1.02–1.06) with any form of invasive respiratory support (HR 3.4; 95% CI 1.84–6.25) and receiving tocilizumab (HR 2.45; 95% CI 1.41–4.25). Median prevalence of CAPA per centre was 10.7% (range 1.7%–26.8%). CAPA was associated with significantly lower 90-day ICU survival rate (29% in patients with CAPA versus 57% in patients without CAPA; Mantel–Byar p < 0.001) and remained an independent negative prognostic variable after adjusting for other predictors of survival (HR 2.14; 95% CI 1.59–2.87, p ≤ 0.001).
Conclusion
Prevalence of CAPA varied between centres. CAPA was significantly more prevalent among older patients, patients receiving invasive ventilation and patients receiving tocilizumab, and was an independent strong predictor of ICU mortality.
Keywords: Aspergillus, Coronavirus disease 2019, Coronavirus disease 2019-associated pulmonary aspergillosis, Intensive care unit, Survival
Introduction
The release of danger-associated molecular patterns during coronavirus disease-19 (COVID-19) acute respiratory failure (ARF) may contribute to a highly permissive inflammatory environment that favours pathogenesis of COVID-19-associated pulmonary aspergillosis (CAPA) [1,2]. CAPA was first described in early 2020 in case reports or small case series [[3], [4], [5]]. Since then, larger case series and cohorts have followed [1,[6], [7], [8], [9], [10]] and CAPA is now considered a potential life-threatening secondary infection in a significant number of critically ill COVID-19 patients [11]. Reported CAPA prevalence rates vary widely between different studies (3%–33%) [[12], [13], [14], [15], [16]]. Several factors may explain the wide variation of CAPA rates including differences in awareness and local diagnostic strategies (e.g. bronchoscopies not done [17]), as well as various different criteria applied for definition of aspergillosis in COVID-19 patients [16,18].
The recently published consensus criteria for definition of CAPA [19] will lead to more uniform CAPA classification across studies and will thereby increase comparability of results. According to those consensus criteria, diagnosis of CAPA relies on microbiological workup, clinical characteristics, and imaging studies; however, diagnosis of CAPA remains a complex clinical challenge [20].
Several risk factors for CAPA have been described in single-centre cohorts, including azithromycin use, use of corticosteroids, use of anti-interleukin-6 treatment and underlying pulmonary disease [6,7,21,22]; however, for identification of factors that would allow for targeted prevention efforts, larger prospective cohort studies are needed. Some single-centre studies have reported that CAPA was associated with higher mortality rates [6,7], but larger studies are needed to elucidate the role of CAPA in overall mortality in COVID-19 ARF.
To determine the prevalence of CAPA in patients with COVID-19 in intensive care units (ICUs) and to investigate risk factors for CAPA as well as potential associations with mortality, the European Confederation of Medical Mycology (ECMM) has initiated a multicentre, multinational cohort study comparing risk factors, and clinical outcomes in patients with COVID-19-associated ARF with and without CAPA.
Materials and methods
Study design and participating centres
We performed a multicentre, multinational cohort study including 20 centres in nine countries: Austria (n = 2), Belgium (n = 4), France (n = 3), Germany (n = 4), Italy (n = 2), Pakistan (n = 1), Spain (n = 1), the UK (n = 1) and the USA (n = 2). The main objectives of this study were to assess the epidemiology of CAPA, risk factors associated with development of CAPA and outcomes of patients with CAPA in ICUs. The study was initiated in March 2020 and data entry was open until May 2021.
All participating centres were invited to provide data on demographics, underlying medical conditions, risk factors for invasive fungal infections, details on diagnostic workup (including radiological and microbiological data), treatment and outcome via an online case report form. Based on the dynamic evolution of the COVID-19 pandemic in 2020 the study protocol did not include target enrolment numbers per participating centre. Among the 20 participating centres, eight (Medical University of Graz; all five centres in Belgium, University of Cologne; San Martino Polyclinic Hospital Genoa; University of Manchester) provided prospectively collected data (different time periods between March 2020 and April 2021) on all consecutive COVID-19 patients (i.e. during the centre-specific different enrolment periods) admitted to an ICU, enabling calculation of CAPA prevalence. The remaining 12 centres provided data for limited numbers of CAPA cases and/or patients without CAPA only.
Inclusion criteria were as follows: (a) Adults (over 18 years of age) with PCR-confirmed severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection and (b) ICU admission for COVID-19-associated ARF. The exclusion criterion was ICU admission due to other conditions besides COVID-19 ARF.
For data acquisition and storage, we used FungiScope® (NCT 01731353), providing an anonymized electronic case report form accessible through www.clinicalsurveys.net [23]. Results on treatment and diagnosis [24] as well as a few of the included CAPA cases have been published [5,[24], [25], [26]].
For classification of cases, we used the 2020 ECMM/ISHAM consensus criteria [19]. According to the criteria, patients were categorized as proven pulmonary and/or tracheobronchial CAPA, probable pulmonary and/or tracheobronchial CAPA, possible pulmonary and/or tracheobronchial CAPA or no evidence for CAPA.
Statistical analysis and ethics
All statistical analyses were performed using IBM SPSS Statistics 25 (IBM, Armonk, NY, USA) and Stata (Windows version 16.0; Stata Corp., Houston, TX, USA). Baseline characteristics between patients with and without disease progression or death during follow up were compared with rank-sum tests, χ2 tests and Fisher's exact tests, as appropriate. Median follow up was computed according to the method of Schemper and Smith, and overall survival was calculated with a Kaplan–Meier estimator. For comparison of survivor functions between the two study groups, we used log-rank tests. To investigate the association of risk factors with survival, univariable and multivariable Cox models were estimated. The proportionality of hazard assumption was evaluated by fitting an interaction between a variable of interest and linear follow-up time. To eliminate immortal time bias, time from CAPA diagnosis was modelled as a so-called time-dependent variable within Cox models. This was achieved by partitioning the follow-up time of patients who did and did not develop CAPA. For visual display of the association between the groups, we performed landmark analyses 14 days after ICU admission. A p value less than 0.05 was considered statistically significant. For calculation of CAPA prevalence, the number of patients diagnosed with CAPA according to the definitions was divided by the total number of COVID-19 patients on ICU presenting during the study period (for prospective cohorts only). Each participating study centre was responsible for obtaining local institutional review board approval, if required by local ethics policy. For the eight centres with data collection on all consecutive ICU patients, institutional review board approval numbers are as follows: Medical University of Graz EC #32-296 ex 19/20; University of Genoa Liguria Region Ethics Committee registry number 163/2020; for the centres from Belgium the study was approved by the ethical board of the University Hospital Leuven (S64071); at the University of Cologne patients were included in the FungiScope® global registry, which was approved by the local ethics committee of the University of Cologne, Cologne, Germany (identifier 05-102); at the University of Manchester data acquisition was conducted as a retrospective audit, which does not require local ethics but was approved by the hospital's audit committee. All centres followed local ethical requirements. The study has been performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments.
Results
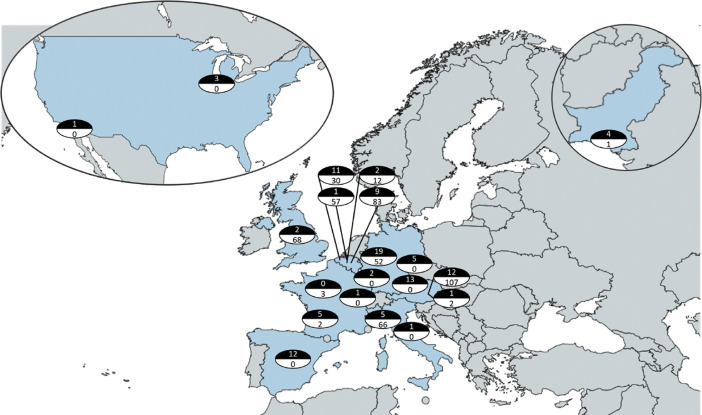
A total of 592 patients with PCR-confirmed SARS-CoV-2 infection requiring ICU admission due to COVID-19-associated acute respiratory failure have been included in this study. Numbers of included patients per centre are displayed in Fig. 1 . Out of the 592 included patients, 11 (1.9%) had histologically proven CAPA, 80 (13.5%) had probable CAPA, 18 (3%) had possible CAPA and 483 (81.6%) had no evidence for CAPA. CAPA prevalence was estimated from cases entered by eight of the participating centres, which have entered all consecutively enrolled COVID-19 ICU patients with CAPA (n = 57: six proven, 48 probable, three possible) and without CAPA (n = 475). CAPA prevalence between the eight centres ranged from 1.7% (Roeselare, Belgium) to 26.8% (Antwerp, Belgium and Cologne, Germany) for proven, probable or possible CAPA.
Fig. 1.
Map of participating centres and numbers of coronavirus disease 2019-associated pulmonary aspergillosis (CAPA) cases (black semicircle) and cases without CAPA (white semicircle) entered per centre. Centres from Europe and centres from the USA and Pakistan are displayed.
Characteristics of the study cohort
Table 1 displays differences in demographic and clinical characteristics and outcomes between patients with CAPA and those without. CAPA was diagnosed after a median of 8 days (25th–75th centile: 4–13 days) after ICU admission. Patients who were diagnosed with CAPA were older, more often male, and more frequently received invasive mechanical ventilation (Table 1). Patients who developed CAPA during ICU treatment more frequently received tocilizumab, but there was no difference in the use of systemic corticosteroids.
Table 1.
Demographic data and characteristics of patients with and without CAPA
| Total (n = 592)a | CAPA groupb (n = 109)a | Non-CAPA group (n = 483)a | P valuec | |
|---|---|---|---|---|
| Age (years), median (25th–75th centile) | 64 (55–73) | 68 (60–75) | 63 (54–73) | 0.003 |
| Female sex, n (%) | 173 (29.2) | 23 (21.1) | 150 (31.1) | 0.039 |
| Underlying diseases, n (%) | ||||
| Cardiovascular disease | 329 (55.6) | 63 (57.8) | 266 (55.1) | n.s. |
| Diabetes mellitus | 160 (27.0) | 32 (29.4) | 128 (26.5) | n.s. |
| History of smoking | 66/587 (11.2) | 14/105 (13.3) | 52/482 (10.8) | n.s. |
| Active malignant diseased | 43 (7.3) | 11 (10.3) | 32 (6.6) | n.s. |
| Obesity (BMI >30 kg/m2) | 168/544 (30.9) | 24/85 (28.2) | 144/459 (31.4) | n.s |
| Pulmonary disease | 113 (19.1) | 26 (23.9) | 87 (18.0) | n.s. |
| Solid organ transplantation | 14 (2.4) | 5 (4.9) | 9 (1.9) | n.s. |
| Maximal ventilation on ICU, n (%) | ||||
| Non-invasive ventilation | 218/584 (37.3) | 14/103 (13.6) | 204/481 (42.4) | <0.001 |
| Invasive mechanical ventilation | 418/591 (70.7) | 96/109 (88.1) | 322/482 (66.8) | <0.001 |
| ECMO | 49/587 (8.3) | 8/106 (7.5) | 41/481 (8.5) | n.s. |
| Any invasive ventilation | 419/587 (71%) | 93/106 (88%) | 326/481 (68%) | <0.001 |
| COVID-19 treatment, n (%) | ||||
| Azithromycin | 75/296 (25.3) | 11/62 (17.7) | 64/234 (27.4) | n.s. |
| Corticosteroids systemic | 346/585 (59.1) | 68/109 (62.4) | 278/476 (58.4) | n.s. |
| Tocilizumab | 39/581 (6.7) | 15/104 (14.4) | 24/477 (5.0) | 0.001 |
| Survival day 28, n (%) | 380/583 (65.2) | 64/105 (61.0) | 316/478 (66.1) | n.s. |
| Survival day 84, n (%) | 333/592 (56.3) | 48/109 (44.0) | 285/483 (59.0) | 0.004 |
| Survival at ICU discharge, n (%) | 337/572 (58.9) | 43/89 (48.3) | 294/483 (60.9) | 0.027 |
| Survival end of follow up, n (%)e | 327 (55.4) | 47 (45.2) | 280 (58.0) | 0.008 |
| ICU stay (days), median, (25th–75th centile) | 16 (7–29) | 27 (17–42) | 14 (6–27) | <0.001 |
Abbreviations: BMI, body mass index; CAPA, COVID-19 associated pulmonary aspergillosis; COVD-19, coronavirus disease 2019; ECMO, extracorporeal membrane oxygenation; ICU, intensive care unit; n.s., not significant (p > 0.05).
All % calculated for 592, 109 or 483 patients, respectively, unless stated otherwise. In case % were calculated for less than the maximal number of patients, data for some patients were missing and the actual denominator is displayed.
Including proven, probable and possible CAPA.
CAPA group versus non-CAPA group; only displayed if p < 0.05.
Active malignancy is defined as solid malignancies for which treatment had been administered within 6 months (7/43) or haematological cancer that is not in complete remission (36/43).
Maximum follow up was 384 days from ICU admission.
Systemic antifungal treatment was initiated in 99 out of 109 patients with CAPA (90.7%) and 52% of those were alive at ICU discharge versus 10% of those not receiving antifungal treatment. Among those who received antifungal monotherapy with voriconazole or isavuconazole, 33/50 (66%) survived at ICU discharge and 34/65 (52%) survived at day 84.
Univariable and multivariable predictors of CAPA
In the univariable time-to-90-day CAPA Cox regression model older age (hazard ratio (HR) 1.18; 95% CI 1.08–1.28 per year), any kind of invasive respiratory support (which displays a composite variable from invasively ventilated patients and patients receiving extracorporeal membrane oxygenation) (HR 2.93; 95% CI 1.60–1.50) and the administration of tocilizumab (HR 2.34; 95% CI 1.35–4.06) were associated with significantly higher risk for developing CAPA (Table 2 ). When including the specific study centres in our Cox model to account for local differences in CAPA incidence, this failed to influence CAPA incidence significantly (HR 1.02; 95% CI 0.99–1.05 for participating centre). We then included all univariable predictors of CAPA in multivariable Cox models where age (HR 1.04; 95% CI 1.02–1.06 per year), any kind of invasive respiratory support (HR 3.4; 95% CI 1.84–6.25) and tocilizumab treatment (HR 2.45; 95% CI 1.41–4.25) remained independent predictors of 90-day CAPA.
Table 2.
Univariable and multivariable Cox regression models for development of CAPA within 90 days
| Variable | Univariable hazard ratio | 95% CI | p value |
|---|---|---|---|
| Demographic variables | |||
| Age (per 5 years) | 1.18 | 1.08–1.28 | <0.001 |
| Female gender | 0.68 | 0.42–1.09 | 0.117 |
| Study centre | 1.02 | 0.99–1.05 | 0.071 |
| Coexisting conditions | |||
| Number of coexisting conditions | 0.92 | 0.76–1.10 | 0.380 |
| Obesity | 0.89 | 0.54–1.44 | 0.638 |
| Active malignant disease | 1.56 | 0.81–3.00 | 0.181 |
| Solid organ transplantation | 2.20 | 0.90–5.42 | 0.084 |
| Cardiovascular disease | 1.20 | 0.81–1.78 | 0.348 |
| Pulmonary disease | 1.42 | 0.89–2.24 | 0.133 |
| Diabetes | 1.12 | 0.73–1.73 | 0.605 |
| History of smoking | 1.36 | 0.76–2.44 | 0.293 |
| Maximum ventilation | |||
| vvECMO (included in any invasive respiratory support) | 0.80 | 0.37–1.70 | 0.547 |
| Invasive ventilation (included in any invasive respiratory support) | 2.53 | 1.53–4.17 | <0.001 |
| Non-invasive ventilation | 0.08 | 0.02–0.33 | <0.001 |
| Any invasive respiratory support | 2.93 | 1.60–5.35 | <0.001 |
| Specific medication | |||
| Glucocorticoids | 1.01 | 0.68–1.50 | 0.962 |
| Tocilizumab | 2.34 | 1.35–4.06 | 0.002 |
| Azithromycin |
0.63 |
0.33–1.21 |
0.167 |
|
Variable |
Multivariable hazard ratio |
95% CI |
p value |
| Age per year | 1.04 | 1.02–1.06 | <0.001 |
| Any invasive respiratory support | 3.40 | 1.84–6.25 | <0.001 |
| Tocilizumab | 2.45 | 1.41–4.25 | <0.001 |
Abbreviations: CAPA, COVID-19-associated pulmonary aspergillosis; vvECMO, veno-venous extracorporeal membrane oxygenation.
Survival in those with and without CAPA
Overall, 261 deaths were observed. In the re-applied univariable Cox models for time-to-90 days ICU survival development of CAPA (HR 1.36; 95% CI 1.02–1.81), older age (HR 1.24; 95% CI 1.17–1.31 per year), the participating centre (HR 0.96; 95% CI 0.95–0.98), active malignant disease (HR 1.68; 95% CI 1.12–2.51), solid organ transplantation (HR 1.89; 95% CI 1.04–3.46), cardiovascular disease (HR 1.33; 95% CI 1.04–1.72), diabetes mellitus (HR 1.44; 95% CI 1.11–1.86) and a history of smoking (HR 1.58; 95% CI 1.12–2.24) were univariable predictors of worse 90-day-ICU outcomes.
To control for immortal time, i.e. time between ICU admission and CAPA diagnosis where patients cannot die from CAPA, we used a multistate regression model in which ICU survival time was divided into survival before CAPA diagnosis and survival after CAPA diagnosis. The model showed that patients who developed CAPA during their ICU stay displayed worse outcomes regarding 90-day ICU survival (HR 2.14; 95% CI 1.59–2.87, p ≤ 0.001). CAPA remained an independent negative prognostic variable after adjusting this post-event data for important univariable predictors of survival (Table 3 ). In a landmark analysis after 14 days, 90-day ICU survival estimates were 57% (95% CI 52%–62%) in patients who were not diagnosed with CAPA and 29% (95% CI 19%–39%) in patients who were diagnosed with CAPA during their ICU stay (Mantel–Byar; p < 0.001; Fig. 2 ).
Table 3.
Univariate and multivariable Cox regression models for 90-day ICU mortality
| Univariate model | Variable | Univariable hazard ratio | 95% CI | p value |
|---|---|---|---|---|
| Demographic variablesrow | ||||
| CAPA | 1.36 | 1.02–1.81 | <0.001 | |
| Age (per 5 years) | 1.24 | 1.17–1.31 | <0.001 | |
| Female gender | 1.07 | 0.82–1.39 | 0.607 | |
| Study centre | 0.96 | 0.95–0.98 | <0.001 | |
| Coexisting conditions | ||||
| Number of coexisting conditions | 1.11 | 0.99–1.24 | 0.05 | |
| Obesity | 0.77 | 0.58–1.02 | 0.076 | |
| Active malignant disease | 1.68 | 1.12–2.51 | 0.013 | |
| Solid organ transplantation | 1.89 | 1.04–3.46 | 0.038 | |
| Cardiovascular disease | 1.33 | 1.04–1.72 | 0.021 | |
| Pulmonary disease | 1.35 | 0.98–1.77 | 0.060 | |
| Diabetes mellitus | 1.44 | 1.11–1.86 | –0.001 | |
| History of smoking | 1.58 | 1.12-2.24 | 0.001 | |
| Maximum Respiratory Treatment | ||||
| ECMO | 0.99 | 0.65–1.51 | 0.982 | |
| Invasive mechanical ventilation | 1.05 | 0.81–1.35 | 0.708 | |
| Non-Invasive ventilation |
0.86 |
0.62–1.19 |
0.361 |
|
|
Multivariable Model |
Variable |
Multivariable hazard ratio |
95% CI |
p value |
| #1 (n = 592) | CAPA | 1.77 | 1.31–2.37 | <0.001 |
| Age | 1.04 | 1.03–1.05 | <0.001 | |
| #2 (n = 592) | CAPA | 2.23 | 1.66–2.99 | <0.001 |
| Study centre | 0.96 | 0.94–0.98 | <0.001 | |
| #3 (n = 592) | CAPA | 1.97 | 1.46–2.67 | <0.001 |
| Active malignancy | 1.47 | 0.98–2.23 | 0.062 | |
| Solid organ transplantation | 1.38 | 0.74–2.58 | 0.304 | |
| Cardiovascular disease | 1.19 | 0.92–1.54 | 0.178 | |
| Diabetes mellitus | 1.31 | 1.00–1.72 | 0.047 | |
| History of smoking | 1.46 | 1.02–2.08 | 0.037 | |
| #4 (n = 592) | CAPA | 1.68 | 1.23–2.28 | 0.001 |
| Age | 1.04 | 1.03–1.06 | <0.001 | |
| Study centre | 0.95 | 0.94–0.97 | <0.001 | |
| Active malignancy | 1.30 | 0.86–1.97 | 0.207 | |
| Solid organ transplantation | 1.59 | 0.85–2.98 | 0.145 | |
| Cardiovascular disease | 0.84 | 0.64–1.09 | 0.204 | |
| Diabetes mellitus | 1.36 | 1.04–1.78 | 0.022 | |
| History of smoking | 1.50 | 1.04–2.15 | 0.028 | |
Abbreviations: CAPA, COVID-19-associated pulmonary aspergillosis; COVID-19, coronavirus disease 2019; ECMO, extracorporeal membrane oxygenation.
Fig. 2.
Intensive care unit survival in patients diagnosed with coronavirus disease 2019-associated pulmonary aspergillosis and patients who were not. Landmark analysis after 14 days for 90-day survival.
Discussion
We performed a large multinational study on CAPA in critically ill COVID-19 patients and found that prevalence varied widely between centres with a median prevalence of 11%. CAPA was diagnosed at a median of 8 days after ICU admission and was more often diagnosed in elderly patients who needed invasive ventilation and received tocilizumab. CAPA was associated with devastating mortality, and remained an independent negative prognostic variable after adjusting for other predictors of survival.
The true prevalence of CAPA is still a matter of debate and depends on various factors including socio-economic factors (e.g. general health condition of a population; access to health-care institutions), local epidemiology and/or seasonal variations in the spread of Aspergillus spores [27], local awareness regarding fungal infections in critically ill patients and the availability and turnaround time of diagnostic tools to diagnose CAPA (e.g. bronchoscopies [17], easy access to CT scans, fungal biomarkers) and also criteria used for classification of CAPA. The importance of bronchoscopy was highlighted in this cohort where galactomannan testing from bronchoalveolar lavage fluid had higher sensitivity (77% with 1.0 Optical Density Index cut-off) than from serum (19%) [24]. In this study, we have classified all patients according to the recently published standardized ECMM/ISHAM consensus definitions for CAPA [19], and found a median CAPA prevalence among the participating centres of 10.7%, ranging between 1.7% and 26.8%. This range is similar to the CAPA rates reported in the literature, even if a wide range of definitions had previously been used [8].
Understanding the main drivers and risk factors for development of CAPA is important, to be able to better target aggressive screening or even use of antifungal prophylaxis to prevent CAPA in high-risk COVID-19 patients. In our multivariable model need for invasive ventilation, older age and treatment with tocilizumab were significantly associated with increased probability of CAPA development. These variables may primarily reflect patients with more severe COVID-19, more severe lung damage and impaired immune response in the elderly. However, other factors described before as being associated with CAPA development, like the use of systemic corticosteroids [7] or azithromycin [21], were not significantly associated with CAPA in our study. Whereas, corticosteroids are a well-known risk factor for impaired neutrophil function and so development of invasive fungal infections, it is now considered standard of care treatment in critically ill COVID-19 patients and therefore less likely to turn out as a significant predictor of CAPA [28]. Indeed, the majority of patients with severe COVID-19 in this study received systemic corticosteroids, which is in contrast to some of the earlier studies where use of systemic corticosteroids was less frequent [6,7,29]. Tocilizumab was a risk factor for CAPA development in our cohort. The use of anti-interleukin-6 treatment or inhibition of Janus kinase seem to increase the overall risk of secondary infections in critically ill COVID-19 patients, but there was no convincing evidence from previous single center studies that risk for CAPA is increased by the use of anti-IL-6 treatment [6,29], which is in contrast to our finding. Nevertheless, as treatment strategies for critical COVID-19 have changed several times within the last year, comparison among the different trials and different study centres is difficult, as is a potential impact of combinations of different immunosuppressive/immunomodulatory treatment regimens.
Some previous, single-centre studies, have indicated that CAPA may prolong stay in hospital and invasiveness of ventilation [29], and may also be associated with higher mortality compared with non-CAPA patients [6,7], whereas others did not show any impact on mortality [12]. Our results show that CAPA was associated with a nearly two-fold increased risk of ICU mortality compared with patients who did not develop CAPA (71% versus 43%), even after accounting for various other factors that impact mortality. This finding supports the hypothesis that CAPA development has negative effects on overall outcome in critically ill COVID-19 patients. Whether this is a causal association—and therefore prevention of CAPA by applying antifungal prophylaxis strategies may improve the overall outcome of these patients—needs to be clarified in future, randomized controlled trials. For influenza-associated invasive aspergillosis, the results of a randomized controlled trial were recently published and showed no significant benefit of prophylaxis because the invasive aspergillosis often occurred within a few hours of ICU admission [30]. Given that CAPA seems to develop later, prophylaxis may be more promising.
This multicentre multinational study has several limitations. Presented data reflect a real-life scenario with no predefined CAPA screening, fungal diagnostics strategies or treatment protocols. Also, the study was initiated in March 2020 and data entry was closed in May 2021. However, despite enrolling prospectively not all centres had CAPA and non-CAPA patients reported for the entire study period. As a result of changes in diagnostic strategies for CAPA, as well as treatment strategies for critically ill COVID-19 patients, this might have influenced our findings and their generalizability. Detailed data on dosage and frequency of tocilizumab administration was not available from all centres, although the majority appeared to have used 8 mg/kg bodyweight. Some centres only entered a few cases and/or controls, and those data had therefore to be excluded from calculation of CAPA prevalence. CAPA prevalence may have been underestimated because a minority (<6%) of patients without CAPA received antifungal prophylaxis or empirical therapy. In addition, time from ICU admission to CAPA development may have been underestimated, as external ICU stays that occurred before the admission into the current ICU may not have been covered in our database. Finally, month of diagnosis and some other data were not available for all patients.
In conclusion, CAPA was more often diagnosed in elderly patients, in patients who needed invasive ventilation and in patients who received tocilizumab and was strongly associated with mortality, remaining an independent negative prognostic variable after adjusting for other predictors of survival. Future studies should evaluate whether antifungal prophylaxis may reduce CAPA prevalence.
ECMM-CAPA study group contributors
Yves Debaveye (Surgical Intensive Care Unit, University Hospital Leuven, Belgium), Marisa H. Miceli (University of Michigan Hospitals, Ann Arbor, MI, USA), Jean-Jacques Tudesq (Medical Intensive Care Unit, Saint-Louis Teaching Hospital, AP-HP, Université de Paris, Paris, France), Gregor Paul (Klinik für Gastroenterologie, Pneumologie und Infektiologie, Katharinenhospital Stuttgart, Zentrum Innere Medizin, Klinikum Stuttgart, Stuttgart, Germany), Robert Krause (Medical University of Graz, Graz, Austria), Marina Linhofer (Medical University of Graz, Graz, Austria), Jonas Frost (Medical Universit of Graz, Graz, Austria), Peter Zechner (LKH Graz II Standort West, Graz, Austria), Matthias Kochanek (University of Cologne, Medical Faculty and University Hospital Cologne, Department I of Internal Medicine, Excellence Centre for Medical Mycology (ECMM), Cologne, Germany), Philipp Eller (Medical Universtiy of Graz, Graz, Austria), Jeffrey D. Jenks (University of California San Diego, San Diego, CA, USA,), Sara Volpi (Infectious Disease Department of the Universitiy of Modena, Modena, Italy), Anne-Pauline Bellanger (Laboratoire de Parasitologie-Mycologie Pôle Biologie Anatomie Pathologique CHRU Jean Minjoz, Besançon, France), P Lewis White (Public Health Wales Microbiology Cardiff, University Hospital of Wales, Cardiff, UK), Gustavo H. Goldman (Faculdade de Ciências Farmacêuticas de Ribeirão Preto, Universidade de São Paulo, Brazil), Paul Bowyer (The University of Manchester, Manchester, UK), Antonis Rokas (Department of Biological Sciences, Vanderbilt University, Nashville, TN, USA), Sara Gago (The University of Manchester, Manchester, UK), Paolo Pelosi (Department of Surgical Sciences and Integrated Diagnostics, University of Genoa, Genoa, Italy), Chiara Robba (A.O.U. San Martino - IST, Istituto Nazionale Ricerca sul Cancro, Genoa, Italy), Jean-Pierre Gangneux (Mycology-Parasitology Laboratory, Rennes Teaching Hospital, Rennes, France), Cornelia Lass-Floerl (Innsbruck Medical University, Austria), Marina Machado and Patricia Muñoz (Clinical Microbiology and Infectious Diseases Department, Hospital General Universitario Gregorio Marañón, Madrid, Spain).
Author contributions
JP, JW, DRG, JM, RRR, PK, KL and MH made substantial contribution to study concept and design. JP, JW, DRG, JS-G, MB, MR, LR, NvR, PL, SF, ACR, TL, MV, LD, KJ, JS, SH, AR, MC and MH made substantial contribution to the acquisition of data for the work. JP, JW, DRG, SH, KL, RRR and MH Substantial contribution to the statistical analysis or interpretation of data. JP, DRG, SH, KL and MH drafted the manuscript. All authors critically reviewed the manuscript and gave final approval for publication.
Funding
RR was supported by the NIHR Manchester Biomedical Research Centre. PK is supported by the German Federal Ministry of Research and Education and the State of North Rhine-Westphalia, Germany and has received non-financial scientific grants from the Cologne Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases, University of Cologne, Cologne, Germany. MH is supported by NIH (UL1TR001442) and investigator initiated grants from Astellas, Gilead and Pfizer.
Transparency declaration
JP has received personal fees from Gilead Sciences and Pfizer, research funding from MSD outside of the submitted work and is stakeholder of AbbVie and Novo Nordisk. JW reports grants and personal fees from Gilead and Pfizer: investigator-initiated grants, personal fees and also on-financial support from MSD, outside the submitted work. DRG reports an unconditional grant from Correvio Italia and a grant for his institution by Pfizer Inc. outside the submitted work. JM reports grants, personal fees and non-financial support from MSD, grants, personal fees and non-financial support from Pfizer Inc., grants, personal fees and non-financial support from Gilead Sciences, personal fees and non-financial support from Astellas Pharam, personal fees and non-financial support from Cidara, personal fees and non-financial support from F2G, personal fees and non-financial support from Mundipharma, personal fees and non-financial support from Takeda/Shire, outside of the submitted work. OAC reports grants and personal fees from Actelion, personal fees from Allecra Therapeutics, personal fees from Al-Jazeera Pharmaceuticals, grants and personal fees from Amplyx, grants and personal fees from Astellas, grants and personal fees from Basilea, personal fees from Biosys, grants and personal fees from Cidara, grants and personal fees from DaVolterra, personal fees from Entasis, grants and personal fees from F2G, grants and personal fees from Gilead, personal fees from Grupo Biotoscana, personal fees from IQVIA, grants from Janssen, personal fees from Matinas, grants from Medicines Company, grants and personal fees from Medpace, grants from Melinta Therapeutics, personal fees from Menarini, grants and personal fees from Merck/MSD, personal fees from Mylan, personal fees from Nabriva, personal fees from Noxxon, personal fees from Octapharma, personal fees from Paratek, grants and personal fees from Pfizer, personal fees from PSI, personal fees from Roche Diagnostics, grants and personal fees from Scynexis, personal fees from Shionogi, grants from DFG, German Research Foundation, grants from German Federal Ministry of Research and Education, grants from Immunic, personal fees from Biocon, personal fees from CoRe Consulting, personal fees from Molecular Partners, from MSG-ERC, from Seres, other from Wiley (Blackwell), outside the submitted work. LD has received personal fees from Gilead Sciences outside the submitted work. JS has received lecture honoraria from Gilead and Pfizer, outside the submitted work. MB has received funding for scientific advisory boards, travel and speaker honoraria from Angelini, Astellas, Bayer, BioMérieux, Cidara, Cipla, Gilead, Menarini, MSD, Pfizer and Shionogi. RRR has received speaker honoraria from Astellas Pharma, Gilead Sciences, Pfizer and research funding from Associates of Cape Cod. PK is supported by the German Federal Ministry of Research and Education and the State of North Rhine-Westphalia, Germany and has received non-financial scientific grants from Miltenyi Biotec GmbH, Bergisch Gladbach, Germany, and the Cologne Excellence Cluster on Cellular Stress Responses in Aging-Associated Diseases, University of Cologne, Cologne, Germany, and received lecture honoraria from and/or is advisor to Akademie für Infektionsmedizin e.V., Ambu GmbH, Astellas Pharma, European Confederation of Medical Mycology, Gilead Sciences, GPR Academy Ruesselsheim, MSD Sharp & Dohme GmbH, Noxxon N.V., and University Hospital, LMU Munich outside the submitted work. KL received consultancy fees from SMB Laboratoires Brussels, MSD and Gilead, travel support from Pfizer, speaker fees from FUJIFILM WAKO, Pfizer and Gilead and a service fee from Thermo Fisher Scientific. MH received research funding from Gilead Sciences, Astellas, Scynexis, F2G and Pfizer, all outside the submitted work. All other authors declare no conflict of interest for this study.
Editor: A. Kalil
Contributor Information
the ECMM-CAPA Study Group:
Yves Debaveye, Marisa H. Miceli, Jean-Jacques Tudesq, Gregor Paul, Robert Krause, Marina Linhofer, Jonas Frost, Peter Zechner, Matthias Kochanek, Philipp Eller, Jeffrey D. Jenks, Sara Volpi, Anne-Pauline Bellanger, P.Lewis White, Gustavo H. Goldman, Paul Bowyer, Antonis Rokas, Sara Gago, Paolo Pelosi, Chiara Robba, Jean-Pierre Gangneux, Cornelia Lass-Floerl, Marina Machado, and Patricia Muñoz
References
- 1.Arastehfar A., Carvalho A., van de Veerdonk F.L., Jenks J.D., Koehler P., Krause R., et al. COVID-19 associated pulmonary aspergillosis (CAPA)—from immunology to treatment. J Fungi (Basel) 2020;6 doi: 10.3390/jof6020091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arastehfar A., Carvalho A., Houbraken J., Lombardi L., Garcia-Rubio R., Jenks J.D., et al. Aspergillus fumigatus and aspergillosis: from basics to clinics. Stud Mycol. 2021;100:100115. doi: 10.1016/j.simyco.2021.100115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Prattes J., Koehler P., Hoenigl M., ECMM-CAPA Study Group COVID-19 associated pulmonary aspergillosis: regional variation in incidence and diagnostic challenges. Intensive Care Med. 2021 doi: 10.1007/s00134-021-06510-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.van Arkel A.L.E., Rijpstra T.A., Belderbos H.N.A., van Wijngaarden P., Verweij P.E., Bentvelsen R.G. COVID-19-associated pulmonary aspergillosis. Am J Resp Crit Care Med. 2020;202:132–135. doi: 10.1164/rccm.202004-1038LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Koehler P., Cornely O.A., Böttiger B.W., Dusse F., Eichenauer D.A., Fuchs F., et al. COVID-19 associated pulmonary aspergillosis. Mycoses. 2020;63:528–534. doi: 10.1111/myc.13096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bartoletti M., Pascale R., Cricca M., Rinaldi M., Maccaro A., Bussini L., et al. PREDICO Study Group Epidemiology of invasive pulmonary aspergillosis among COVID-19 intubated patients: a prospective study. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.White P.L., Dhillon R., Cordey A., Hughes H., Faggian F., Soni S., et al. A national strategy to diagnose COVID-19 associated invasive fungal disease in the ICU. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Salmanton-García J., Sprute R., Stemler J., Bartoletti M., Dupont D., Valerio M., et al. COVID-19-associated pulmonary aspergillosis, March–August 2020. Emerg Infect Dis. 2021;27:1077–1086. doi: 10.3201/eid2704.204895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Marr K., Platt A., Tornheim J., Zhang S., Datta K., Cardozo C., et al. Aspergillosis complicating severe coronavirus disease. Emerg Infect Dis J. 2021;27 doi: 10.3201/eid2701.202896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gangneux J.P., Reizine F., Guegan H., Pinceaux K., Le Balch P., Prat E., et al. Is the COVID-19 pandemic a good time to include aspergillus molecular detection to categorize aspergillosis in ICU patients? A monocentric experience. J Fungi (Basel) 2020;6 doi: 10.3390/jof6030105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Thompson G.R., III, Cornely O.A., Pappas P.G., Patterson T.F., Hoenigl M., Jenks J.D., et al. European Confederation of Medical Mycoses Study Group Invasive aspergillosis as an underrecognized superinfection in COVID-19. Open Forum Infect Dis. 2020;7 doi: 10.1093/ofid/ofaa242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Alanio A., Delliere S., Fodil S., Bretagne S., Megarbane B. Prevalence of putative invasive pulmonary aspergillosis in critically ill patients with COVID-19. Lancet Respir Med. 2020;8:e48–e49. doi: 10.1016/S2213-2600(20)30237-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Segrelles-Calvo G., Araujo G.R.S., Llopis-Pastor E., Carrillo J., Hernandez-Hernandez M., Rey L., et al. Prevalence of opportunistic invasive aspergillosis in COVID-19 patients with severe pneumonia. Mycoses. 2021;64:144–151. doi: 10.1111/myc.13219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hoenigl M. Invasive fungal disease complicating COVID-19: when it rains it pours. Clin Infect Dis. 2020 doi: 10.1093/cid/ciaa1342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Machado M., Valerio M., Álvarez-Uría A., Olmedo M., Veintimilla C., Padilla B., et al. Invasive pulmonary aspergillosis in the COVID-19 era: an expected new entity. Mycoses. 2021;64:132–143. doi: 10.1111/myc.13213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Verweij P.E., Rijnders B.J.A., Brüggemann R.J.M., Azoulay E., Bassetti M., Blot S., al Tet. Review of influenza-associated pulmonary aspergillosis in ICU patients and proposal for a case definition: an expert opinion. Intens Care Med. 2020;46:1524–1535. doi: 10.1007/s00134-020-06091-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Koehler P., Cornely O.A., Kochanek M. Bronchoscopy safety precautions for diagnosing COVID-19 associated pulmonary aspergillosis—a simulation study. Mycoses. 2021;64:55–59. doi: 10.1111/myc.13183. [DOI] [PubMed] [Google Scholar]
- 18.Jenks J.D., Nam H.H., Hoenigl M. Invasive aspergillosis in critically ill patients: review of definitions and diagnostic approaches. Mycoses. 2021;64:1002–1014. doi: 10.1111/myc.13274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Koehler P., Bassetti M., Chakrabarti A., Chen S.C.A., Colombo A.L., Hoenigl M., et al. Defining and managing COVID-19-associated pulmonary aspergillosis: the 2020 ECMM/ISHAM consensus criteria for research and clinical guidance. Lancet Infect Dis. 2021;21:e149–e162. doi: 10.1016/S1473-3099(20)30847-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lang M., Som A., Mendoza D.P., Flores E.J., Li M.D., Jo Shepard, et al. Detection of unsuspected coronavirus disease 2019 cases by computed tomography and retrospective implementation of the radiological society of North America/society of thoracic radiology/American college of radiology consensus guidelines. J Thorac Imag. 2020;35:346–353. doi: 10.1097/RTI.0000000000000542. [DOI] [PubMed] [Google Scholar]
- 21.Dellière S., Dudoignon E., Fodil S., Voicu S., Collet M., Oillic P.A., et al. Risk factors associated with COVID-19-associated pulmonary aspergillosis in ICU patients: a French multicentric retrospective cohort. Clin Microbiol Infect. 2020;27:790. doi: 10.1016/j.cmi.2020.12.005. e1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Meijer E.F.J., Dofferhoff A.S.M., Hoiting O., Meis J.F. COVID-19-associated pulmonary aspergillosis: a prospective single-center dual case series. Mycoses. 2021;64:457–464. doi: 10.1111/myc.13254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Seidel D., Durán Graeff L.A., Vehreschild M., Wisplinghoff H., Ziegler M., Vehreschild J.J., et al. FungiScope, FungiScope™—global emerging fungal infection registry. Mycoses. 2017;60:508–516. doi: 10.1111/myc.12631. [DOI] [PubMed] [Google Scholar]
- 24.Prattes J., Wauters J., Giacobbe D.R., Lagrou K., Hoenigl M., ECMM-CAPA Study Group Diagnosis and treatment of COVID-19 associated pulmonary apergillosis in critically ill patients: results from a European confederation of medical mycology registry. Intens Care Med. 2021 doi: 10.1007/s00134-021-06471-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nasir N., Farooqi J., Mahmood S.F., Jabeen K. COVID-19-associated pulmonary aspergillosis (CAPA) in patients admitted with severe COVID-19 pneumonia: an observational study from Pakistan. Mycoses. 2020;63:766–770. doi: 10.1111/myc.13135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lahmer T., Rasch S., Spinner C., Geisler F., Schmid R.M., Huber W. Invasive pulmonary aspergillosis in severe coronavirus disease 2019 pneumonia. Clin Microbiol Infect. 2020;26:1428–1429. doi: 10.1016/j.cmi.2020.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Richardson M., Bowyer P., Sabino R. The human lung and Aspergillus: you are what you breathe in? Med Mycol. 2019;57:S145–S154. doi: 10.1093/mmy/myy149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.RECOVERY Collaborative Group. Horby P., Lim W.S., Emberson J.R., Mafham M., Bell J.L., Linsell L., et al. Landray, Dexamethasone in hospitalized patients with COVID-19. N Engl J Med. 2021;384:693–704. doi: 10.1056/NEJMoa2021436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Permpalung N., Chiang T.P., Massie A.B., Zhang S.X., Avery R.K., Nematollahi S., et al. COVID-19 associated pulmonary aspergillosis in mechanically ventilated patients. Clin Infect Dis. 2021 doi: 10.1093/cid/ciab223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Vanderbeke L., Janssen N.A.F., Bergmans D., Bourgeois M., Buil J.B., Debaveye Y., et al. Posaconazole for prevention of invasive pulmonary aspergillosis in critically ill influenza patients (POSA-FLU): a randomised, open-label, proof-of-concept trial. Intens Care Med. 2021;47:674–686. doi: 10.1007/s00134-021-06431-0. [DOI] [PMC free article] [PubMed] [Google Scholar]