Introduction
Pemphigus is a group of rare acquired autoimmune blistering diseases characterized by acantholysis and includes pemphigus vulgaris (PV), pemphigus foliaceus (PF), fogo salvagem, drug-induced pemphigus, and paraneoplastic pemphigus. PF is characterized by immunoglobulin G (IgG) autoantibodies against desmoglein (DSG) 1, primarily located in the granular layer of the epidermis, while PV is characterized by autoantibodies against DSG-3, primarily located in the mucous membranes. Autoantibodies against these molecules destroy the connection between keratinocytes, resulting in acantholysis and the formation of subcorneal blisters.1, 2, 3 PV is characterized by painful blisters and erosions on the skin and mucous membranes, most commonly inside the mouth, and accounts for 70% of all pemphigus cases worldwide. PF typically presents with crusted scaly erosions in a seborrheic distribution and has a low worldwide incidence and prevalence.1
While some reports of localized pemphigus occurring primarily on the face exist, such lesions remain extremely rare.4 Reports of pemphigus isolated to the nose is an even rarer event. The 2 patients presented here are of interest as localized pemphigus presents a diagnostic challenge often leading to a delay in diagnosis and treatment. We report 2 cases of pemphigus of the nose, explore other similar previously reported cases, and discuss the potential mechanisms behind this unique disease presentation.
Case report
Case 1
A 75-year-old man with a past medical history of PV isolated to the nose, hypertension, hyperlipidemia, and osteoporosis presented with a 4-week history of erosions on the bilateral nasal alae (Fig 1). The patient had not received treatment for PV for several years prior to presentation and had no prior history of herpes simplex infection. The medications at presentation included alendronate, atenolol/ chlorthalidone, terazosin, aspirin, simvastatin, alprazolam, and calcium with vitamin D. He was believed to have localized pemphigus and was started on mycophenolate mofetil (MMF) at 1000 mg, oral prednisone at 20 mg daily, and triamcinolone ointment 0.1% topically twice daily.
Fig 1.
Case 1: Pemphigus vulgaris. Crusted erosion on the right side of the nose.
For 3 months, he developed new erosions on the nasal alae, bridge, and tip as well as within the nares, with all of his lesions remaining isolated to the nose. A biopsy of the nasal ala demonstrated crusted suprabasilar acantholytic separation consistent with PV. Indirect immunofluorescence showed IgG antibodies against monkey esophagus (titer, 1:80) and human skin (titer, 1:20). No anti-DSG-1 antibodies (0 units) and increased anti-DSG-3 antibodies (40 units) were seen in enzyme-linked immunosorbent assay (UIC Labs/RayBio).
After several months of treatment with MMF and prednisone, the patient complained of gastrointestinal upset and diarrhea. Adjustment to the dosages was made, and dapsone at 25 mg daily was added. Despite these medication adjustments, the patient's erosions continued to worsen, prompting an increase of MMF to 1500 mg twice daily, dapsone 50 mg daily, and prednisone 17.5 mg daily.
No improvement was observed; therefore, MMF and dapsone were discontinued, azathioprine at 25 mg daily was started, and prednisone increased to 20 mg daily. With minimal improvement, the patient's azathioprine was increased to 100 mg daily, again without improvement after some time; therefore, trimethoprim/sulfamethoxazole double strength twice daily was added. After 3 months of treatment with azathioprine at 100 mg daily, trimethoprim/sulfamethoxazole double strength twice daily, and a slow prednisone taper, the patient cleared.
Case 2
A 40-year-old previously healthy man on omeprazole for gastroesophageal reflux disease, presented with a recent onset of an eruption on the lower third of his nose (Fig 2). He denied any symptoms associated with the eruption, had no other mucocutaneous lesions, and denied trauma. His employment results in repeated sun exposure, but the patient reported using sunscreens and wearing a hat while working in the sun. The initial diagnoses included seborrheic dermatitis, rosacea, and impetigo.
Fig 2.
Case 2: Pemphigus foliaceus. Shallow erosions on the lower portion of the nose.
He was treated with oral minocycline and topical mupirocin. He returned 6 weeks later without improvement. A biopsy was taken (Fig 3) and initially reported as acantholytic actinic keratosis, and the patient was given topical 5-fluorouracil.
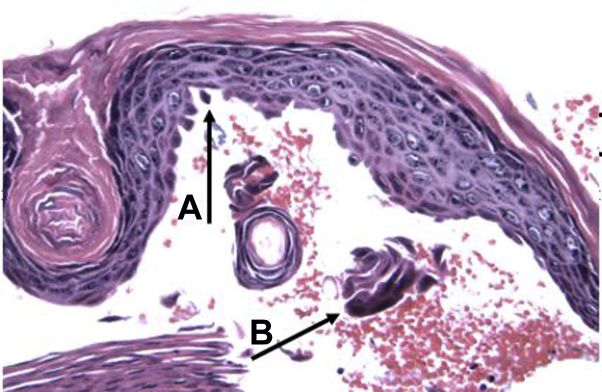
Fig 3.
Case 2: Pemphigus foliaceus. Biopsy taken from the nose exhibited intracorneal split within the granular layer (A) with associated acantholytic keratinocytes (B). There was a complete separation of the granular layer from the epidermis and dermis, which contained a mild perivascular infiltrate (not shown) (hematoxylin-eosin stain; original magnification: ×400.)
Eruptions continued, and rebiopsy revealed probable PF. He was referred to an academic center, where direct immunofluorescence was positive for PF revealing intercellular space deposition of IgG in the upper dermis. Indirect immunofluorescence showed IgG antibodies to monkey esophagus (titer, 1:320) and to human skin (titer, 1:80). Enzyme-linked immunosorbent assay for anti-DSG-1 antibodies showed elevation at 77 units and was negative for anti-DSG-3 antibodies (UIC Labs/RayBio). Hepatitis screening was negative. He was started on hydroxyzine and topical tacrolimus. Minimal improvement was observed, and the patient was given oral doxycycline 100 mg daily.
The patient returned to our clinic where topical tacrolimus was discontinued and topical crisaborole was added. Anti-DSG-1 antibodies at 34 units and anti-DSG-3 antibodies at 10 units were both elevated (Quest Labs). The patient improved; however, because of his sun exposure, the patient was changed to minocycline with good control of disease.
Discussion
Localized pemphigus is quite rare with reported cases numbering in the teens.5 Rarer still are cases localized to the nasal region. Drugs may be a cause of pemphigus; however, more than one precipitating factor is typically found.4 It is unknown why localized pemphigus has a predilection for the seborrheic distribution of the face and, specifically, the nose. Explanations for the occurrence of pemphigus in sun-exposed areas include increased expression of pemphigus antigen and the role of ultraviolet light, which may induce the binding of anti-DSG-1.1,6, 7, 8 Localized PF typically presents as an isolated, erythematous, scaly, crusted plaque of the nose, cheek, or scalp and may be diagnosed as seborrheic dermatitis, rosacea, contact dermatitis, cutaneous sarcoidosis, discoid lupus erythematosus, lupus vulgaris, impetigo, actinic keratosis, and even nonmelanoma skin cancer.1,2 Case 1 presented with medications that may induce pemphigus, and case 2 had a long history of chronic sun exposure.
Table I summarizes previously published cases of PV and PF with predominantly nasal involvement. Pemphigus remained localized to the nose in several cases, while other patients experienced disease progression beyond the nose. Of note, the Mandel case showed features of PF as well as PV.9 Cases where pemphigus was not exclusively observed on the nose were excluded from the table.
Table I.
Previously reported cases of pemphigus primarily localized to the nasal region
| Reference | Age (y), sex | Pemphigus type | Remained localized | Antibodies | Treatment |
|---|---|---|---|---|---|
| Paramsothy15 | 34, M | PF | No | DIF: IgG deposition between epidermal cells IIF: Positive |
Oral prednisone |
| Paramsothy15 | 65, M | PF | No | DIF: IgG between epidermal cells and IgM in basement membrane IIIF: Positive |
Topical clobetasol propionate |
| Newton et al13 | 27, M | PF | Yes | DIF: Intercellular IgG and C3 | Topical clobetasol propionate |
| Newton et al13 | 62, F | PF | No | DIF: Intercellular IgG | Oral cyclophosphamide |
| Newton et al13 | 43, M | PF | Yes | DIF: None | Oral prednisolone, 20 mg/d |
| Kishibe16 | 63, M | PF | Yes | DIF: IgG deposition | Oral prednisolone 40 mg/d |
| Ghoneim and Zaiac11 | 37, M | PF | Yes | DIF: Intercellular IgG and C3 throughout epidermis | Triamcinolone ointment and one-time intralesional injection of triamcinolone 2.5 mg/mL |
| Fleming17 |
51, M | PF | Yes | DIF: Intercellular IgG and C3 | Topical steroids (unspecified) and oral prednisolone |
| Mandel et al9 | 74, M | PF/PV | Yes | Histopathology: Acantholysis with formation of clefts in the granular and spinous layers of the epidermis DIF: IgG and C3 throughout epidermis IIF: Intracellular antibodies (titer, 1:40) in suprabasal epidermis |
Oral prednisone 25 mg/d for 1 mo |
| Aizawa18 | M | PF/PV | Unknown | Histopathology: Subcorneal acantholysis DIF: None IIF: IgG deposits on keratinocyte cell surface CLIA: Anti-DSG-1 antibodies (391 U/mL); anti-DSG-3 antibodies (23.5 U/mL; normal level, <20 U/mL for both) ELISA: Negative result for desmocollins 1-3 |
Topical corticosteroids (unspecified) |
| Zhang19 | 36, M | PV | Yes | DIF: IgG and C3 in a patchy net-like intercellular pattern in the epidermis IIF: Monkey esophagus, negative ELISA: Anti-DSG-3 antibodies (89.6 U/mL, normal < 20); negative result for anti-DSG-1 antibody |
Mometasone furoate cream 1% |
| Sigmund20 | 43, F | PV, vegetans type | Yes | Histopathology: Mixed inflammatory cell infiltrate that included a large number of eosinophils and plasma cells; pseudoepitheliomatous hyperplasia; intraepidermoid microabscesses; eosinophilic spongiosis | Prednisone 60 mg daily for 2 wk and maintained on prednisone 30 mg daily |
| Taylor21 | 65, M | PV | No | Topical and intralesional steroids |
CLIA, Chemiluminescent immunoassay; DIF, direct immunofluorescence; DSG, desmoglein; ELISA, enzyme-linked immunosorbent assay; Ig, immunoglobulin; IIF, indirect immunofluorescence; PF, pemphigus foliaceus; PV, pemphigus vulgaris.
Many treatment options for PF appear in the literature and include topical agents for less severe cases, including steroids, pimecrolimus, and tacrolimus. The use of intralesional steroids has also been reported.10 For more severe cases, systemic treatments, including steroids, mycophenolate, azathioprine, antibiotics, nicotinamide, rituximab, plasmapheresis, and intravenous immunoglobulin have been reported.10, 11, 12, 13, 14
Localized pemphigus is an exceptionally rare entity with few reports in the literature and even fewer involving only the nose. We report 2 additional cases to the 9 previously published cases. The diagnosis of localized pemphigus is often challenging and must be a diagnostic consideration, as the presentation simulates other disease states.
Conflicts of interest
None disclosed.
Footnotes
Funding sources: None.
IRB approval status: Not applicable.
References
- 1.James K.A., Culton D.A., Diaz L.A. Diagnosis and clinical features of pemphigus foliaceus. Dermatol Clin. 2011;29(3):405–412. doi: 10.1016/j.det.2011.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kasperkiewicz M., Ellebrect C.T., Takahashi H. Pemphigus. Nat Rev Dis Primers. 2017;3(1):1–18. doi: 10.1038/nrdp.2017.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krase I.Z., Wickenheiser M., Chao J. A rare cause of unilateral facial rash. Clin Exp Dermatol. 2019;44(4):425–427. doi: 10.1111/ced.13749. [DOI] [PubMed] [Google Scholar]
- 4.Brenner S., Goldberg I. Drug-induced pemphigus. Clin Dermatol. 2011;29(4):455–457. doi: 10.1016/j.clindermatol.2011.01.016. [DOI] [PubMed] [Google Scholar]
- 5.Aoki V., Rivitti E.A., Diaz L.A. Cooperative Group on Fogo Selvagem Research. Update on fogo selvagem, an endemic form of pemphigus foliaceus. J Dermatol. 2015;42(1):18–26. doi: 10.1111/1346-8138.12675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Maderal A.D., Miner A., Nousari C., Alonso-Llamazares J. Localized pemphigus foliaceus with unilateral facial involvement. Actas Dermosifiliogr. 2014;105(4):413–417. doi: 10.1016/j.adengl.2013.02.020. [DOI] [PubMed] [Google Scholar]
- 7.Kano Y., Shimosegawa M., Mizukawa Y., Shiohara T. Pemphigus foliaceus induced by exposure to sunlight. Dermatology. 2000;201(2):132–138. doi: 10.1159/000018456. [DOI] [PubMed] [Google Scholar]
- 8.Ioannides D., Hytiroglou P., Phelps R.G., Bystryn J.C. Regional variation in the expression of pemphigus foliaceus, pemphigus erythematosus, and pemphigus vulgaris antigens in human skin. J Invest Dermatol. 1991;96(2):159–161. doi: 10.1111/1523-1747.ep12460927. [DOI] [PubMed] [Google Scholar]
- 9.Mandel V.D., Farnetani F., Vaschieri C. Pemphigus with features of both vulgaris and foliaceus variants localized to the nose. J Dermatol. 2016;43(8):940–943. doi: 10.1111/1346-8138.13314. [DOI] [PubMed] [Google Scholar]
- 10.Culton D.A., Qian Y., Li N. Advances in pemphigus and its endemic pemphigus foliaceus (Fogo Selvagem) phenotype: a paradigm of human autoimmunity. J Autoimmun. 2008;31(4):311–324. doi: 10.1016/j.jaut.2008.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ghoneim S., Zaiac M. The use of intralesional steroids in a case of localized pemphigus foliaceus. Case Rep Dermatol. 2017;9(2):91–97. doi: 10.1159/000477959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Groves R.W. Pemphigus: a brief review. Clin Med (Lond) 2009;9(4):371–375. doi: 10.7861/clinmedicine.9-4-371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Newton J.A., McGibbon D.H., Monk B., Rowell N.R. Pemphigus foliaceus localized to the nose. Br J Dermatol. 1988;118(2):303–305. doi: 10.1111/j.1365-2133.1988.tb01786.x. [DOI] [PubMed] [Google Scholar]
- 14.Tyros G., Kalapothakou K., Christofidou E., Kanelleas A., Stavropoulos P.G. Successful treatment of localized pemphigus foliaceus with topical pimecrolimus. Case Rep Dermatol Med. 2013;2013:489618. doi: 10.1155/2013/489618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Paramsothy Y., Lawrence C.M. “TIn-tack” sign in localized pemphigus foliaceus. Br J Dermatol. 1987;116:127–129. doi: 10.1111/j.1365-2133.1987.tb05800.x. [DOI] [PubMed] [Google Scholar]
- 16.Kishibe M., Kinouchi M., Ishida-Yamamoto A., Koike K., Iizuka H. Pemphigus foliaceus localized to the nose. Clin Exp Dermatol. 2003;28:560–562. doi: 10.1046/j.1365-2230.2003.01343.x. [DOI] [PubMed] [Google Scholar]
- 17.Fleming C.L., Meligonis G., Sterling J. The nose as the predominant site for pemphigus foliaceus. Clin Exp Dermatol. 2019;44:235–236. doi: 10.1111/ced.13755. [DOI] [PubMed] [Google Scholar]
- 18.Aizawa N., Asahina A., Ishii N., Hashimoto T., Nakagawa H. The nose as a predilection site for pemphigus. Clin Exp Dermatol. 2018;43(1):71–72. doi: 10.1111/ced.13275. [DOI] [PubMed] [Google Scholar]
- 19.Zhang C., Goldscheider I., Ruzicka T., Sardy M. Pemphigus vulgaris persistently localized to the nose with local and systemic response to topical steroids. Acta Derm Venereol. 2017;97(9):1136–1137. doi: 10.2340/00015555-2725. [DOI] [PubMed] [Google Scholar]
- 20.Sigmund G.A., Oppenheimer R. Pemphigus vegetans of the nose. Ear Nose Throat J. 2012;91(1):E14–E15. doi: 10.1177/014556131209100117. [DOI] [PubMed] [Google Scholar]
- 21.Taylor J., Westfried M., Lynfield Y.L. Pemphigus vulgaris localized to the nose. Cutis. 1984;34(4):394–395. [PubMed] [Google Scholar]