Abstract
Background/Objectives:
Individuals successful at weight loss maintenance engage in high amounts of physical activity (PA). Understanding how and when weight loss maintainers accumulate PA within a day and across the week may inform PA promotion strategies and recommendations for weight management.
Methods:
We compared patterns of PA in a cohort of weight loss maintainers (WLM, n=28, maintaining ≥13.6 kg weight loss for ≥1 year, BMI 23.6 ± 2.3 kg/m2), controls without obesity (NC, n=30, BMI similar to current BMI of WLM, BMI 22.8 ± 1.9 kg/m2), and controls with overweight/obesity (OC, n=26, BMI similar to pre-weight loss BMI of WLM, 33.6 ± 5.1 kg/m2). PA was assessed during 7 consecutive days using the activPAL™ activity monitor. The following variables were quantified; sleep duration, sedentary time (SED), light-intensity PA (LPA), moderate-to-vigorous intensity PA (MVPA), and steps. Data were examined to determine differences in patterns of PA across the week and across the day using mixed effect models.
Results:
Across the week, WLM engaged in ≥60 minutes of MVPA on 73% of days, significantly more than OC (36%, p<0.001) and similar to NC (59%, p=0.10). Across the day, WLM accumulated more MVPA in the morning (i.e., within 3 hours of waking) compared to both NC and OC (p<0.01). WLM engaged in significantly more MVPA accumulated in bouts ≥10 min (p<0.05). Specifically, WLM engaged in more MVPA accumulated in bouts of ≥60 min compared to NC and OC (p<0.05).
Conclusions:
WLM engage in high amounts of MVPA (≥60 min/d) on more days of the week, accumulate more MVPA in sustained bouts, and accumulate more MVPA in the morning compared to controls. Future research should investigate if these distinct patterns of PA help to promote weight loss maintenance.
Keywords: exercise, obesity, accelerometry, diurnal
INTRODUCTION
High amounts of physical activity (PA) are consistently associated with weight loss maintenance (1–9). More specifically, ≥250 minutes per week (min/wk) of moderate-to-vigorous physical activity (MVPA) has been observed among individuals who are successfully maintaining a substantial weight loss (2, 3). This study builds upon these previous findings by determining how and when weight loss maintainers accumulate their PA across the week and within a day. Understanding temporal patterns of PA across the week and within a day (e.g., morning vs. evening; intermittently vs. sustained bouts) in weight loss maintainers may inform behavioral strategies aimed at improving long-term PA adherence.
Distinct patterns of MVPA across the week have been previously reported in other populations (10–12). The most studied patterns have compared individuals who accumulate similar amounts of PA daily versus individuals accumulating high amounts of PA on only a few days per week, often referred to as “weekend warriors.” The weekend warrior pattern has been associated with lower risk of all-cause, cardiovascular disease, and cancer mortality compared to inactive individuals, and similar risk compared to regularly active individuals (11). To date, the weekend warrior pattern of activity has typically been observed in individuals engaging in moderate amounts of weekly MVPA (~150 min/wk). It is unclear if individuals who engage in high amounts of weekly MVPA (>250 min/wk) can achieve this high volume of PA with a weekend warrior pattern or if they must engage in high amounts of MVPA more regularly.
In addition to MVPA accumulation across the week, MVPA can be accumulated in different patterns within a day (e.g., morning vs. evening; intermittently vs. sustained bouts). Emerging data suggests that the timing of activity within a day may impact physiology and behavior related to energy balance, body weight regulation, and adherence to PA recommendations (13–16). Collectively, these studies suggest that morning activity may help to promote negative energy balance and subsequent weight loss. In addition to timing, the pattern of activity accumulation may be important for weight loss maintenance. Data supporting the MVPA recommendations for weight loss maintenance have focused on MVPA accumulated in bouts of ≥10 minutes (2, 3, 6, 7, 17, 18). Previous PA guidelines and recommendations for general health benefits have also focused on MVPA accumulated in bouts of ≥10 minutes (19). However, the recently published 2nd Edition of the PA Guidelines for Americans notably removed the recommendation that PA needs to be accumulated in bouts of ≥10 minutes (20). Recent studies have suggested that intermittent and non-bouted MVPA (i.e., MVPA in bouts of <10 minutes) offer health benefits (21–25). However, the importance of shorter bouts of MVPA for weight loss maintenance remains unknown.
The aim of this secondary analysis was to compare device-measured temporal patterns (e.g., across the week and within a day) of PA between weight loss maintainers (WLM), controls without obesity (NC), and controls with overweight or obesity (OC). We hypothesized that WLM would engage in longer bouts of MVPA, more MVPA in the morning, and demonstrate greater consistency in patterns of PA across the week as compared to OC and NC. Additionally, this analysis compared the timing and duration of other behaviors across the PA spectrum including sleep, sedentary behavior, light physical activity (LPA), and stepping. Sleep (26), sedentary behavior (27), and LPA (3) have been independently associated with body weight regulation. However, the importance of these behaviors for weight loss maintenance remains unclear. We hypothesized that WLM would also have more consistent sleep durations, sedentary behavior, and LPA patterns across the week. Similarly, we hypothesized that WLM would have lower sedentary behavior, more LPA, and more steps in morning compared to NC and OC.
METHODS
Participants
Participants were recruited to participate in this observational, cross-sectional study from 2009 until 2012 (NCT #03422380). Study assessments took place at the University of Colorado-Anschutz Medical Campus. The Colorado Multiple Institutional Review Board approved all study procedures prior to recruitment and data collection. Other demographic, body composition, PA, and energetic comparisons from this study have been published previously, including comparisons of mean levels of PA between groups summarized on a per week basis (2, 28, 29). The present study is a secondary data analysis with a more rigorous examination of the objective PA data with the primary goal of understanding the temporal patterns of PA and sedentary behavior across the day and week.
Participants were recruited from the general public through advertisements and email announcements as previously described (2, 28, 29): weight loss maintainers (WLM, maintaining ≥13.6 kg weight loss for ≥ 1 year, current BMI 18–28.0 kg/m2), controls without obesity (NC, current BMI similar to WLM, current BMI 18–28.0 kg/m2), and controls with overweight or obesity (OC, BMI similar to maximum BMI of WLM, current BMI >27.0 kg/m2). Individuals in the three groups were required to be weight stable prior to enrollment (<5 kg fluctuation in body weight over the past 6 months). A nested subject selection procedure was employed to ensure similar group means for age, sex, and similar distribution between current BMI of NC and WLM (categories <22.0, 22.0–<25.0, and 25.0–30.0 kg/m2) and similar distribution between current BMI of OC and pre-weight loss maximum BMI of WLM (categories 25.0–<30.0, 30.0–<35.0, 35.0–<40.0, and ≥40.0 kg/m2).
Interested volunteers completed a telephone screen to determine eligibility. Following the telephone screen, eligible participants were invited to an in-person screening visit to review medical history, assess vitals and body weight, and receive a physical examination. Prior to study procedures, volunteers provided written informed consent. Individuals were excluded if they had any physical or medical contraindications to PA (i.e. cardiovascular disease, cancer, significant metabolic musculoskeletal, neurological, and psychiatric disorders), had undergone bariatric surgery, were current smokers, or were taking medications known to affect appetite, metabolism, or body weight. Women were excluded if they were currently pregnant or lactating.
Assessment of Height, Weight, and Body Composition
Weight was measured in duplicate using a regularly calibrated digital scale (to the nearest 0.1 kg) and height was measured with a wall-mounted stadiometer (to the nearest 0.1 cm). Body composition was assessed using dual-energy x-ray absorptiometry (DXA; Delphi-W Version 13.1.0; Hologic Inc; Bedford, MA). Body composition is reported as fat mass (FM), fat free mass (FFM), and percent body fat.
Assessment of Physical Activity, Sedentary Behavior, and Sleep
PA, sedentary time (SED), and sleep duration were assessed using the activPAL™ (PAL Technologies; Glasgow, Scotland), which utilizes accelerometry and a paired inclinometer to detect movement and posture. Participants were instructed to wear the activPAL™ on their right anterior thigh for seven consecutive days. activPAL™ event files were utilized for data analysis and all data processing was performed in R. First, the event file was converted to a second-by-second file and the first and last day of wear were removed to ensure that PA timing data were not influenced by the time the devices were put on/taken off. Bedtime (time the participant got into bed at night) and waketime (time the participants got out of bed in the morning), were determined via visual inspection of the raw accelerometry and postural data as published previously (2). Time in bed was calculated as the time from bedtime from waketime and was used as proxy measure for sleep. Data were considered valid if a participant had ≥10 hours of waking data on ≥3 weekdays and ≥1 weekend day, resulting in a minimum of 4 valid days. Second-by-second metabolic equivalent (MET) values were encoded as sedentary time (SED; <1.5 METs), light physical activity which included standing (LPA; 1.5 to <3.0 METs), or MVPA (≥3.0 METs). SED, LPA, MVPA, and total steps were summarized for each day of the week by summing the second-by-second values as previously described (2). The activPAL™ uses a cadence-based linear regression model to estimate METs which does not take into account body size or body composition. Further this model does not accurately delineate between moderate and vigorous intensity activity; thus, we have focused our data on MVPA. PA accumulation was examined considering activity profiles in 3 hour (h) “bins” starting from when the participant got out of bed (i.e. h from wake). SED, LPA, MVPA, and steps were summarized across the day in the following bins: 0–3, 3–6, 6–9, 9–12, 12–15, 15–18, 18–21, and 21–24 hours from wake. Due to exclusion of sleep data, participants frequently had no data for the 18–21 and 21–24 bins. We chose normalize the data to wake time to limit potential circadian effects. Thus, those bins were excluded in the final analysis. Finally, bouts of MVPA (Bout-MVPA) were examined by creating summaries of MVPA accumulated in different bout durations. For this analysis, the mean MET value was calculated for each minute of data, then coded as SED, LPA, or MVPA using the same intensity criteria as above. A bout of MVPA began anytime a minute was classified as MVPA, and the bout continued until three consecutive minutes of non-MVPA had elapsed. Within that period, 80% of minutes had to be classified as MVPA for the bout to be considered valid (2). Only minutes classified as MVPA were counted towards the Bout-MVPA. Bout-MVPA accumulation was then examined in bouts of 1–9, 10–29, 30–59, and ≥60 minutes.
Statistical Analyses
Statistical analyses were performed using SAS 9.4 (SAS System for Microsoft; SAS Institute Inc., Cary, North Carolina). Baseline variables were compared using Fisher’s exact tests for categorical variables and parametric and nonparametric analysis of variance (ANOVA) as appropriate for continuous variables. To compare differences in total MVPA and bout-MVPA, the Kruskal-Wallis test was utilized for group differences and Wilcoxon rank sum test was used for pairwise comparisons. Logistic regression with generalized estimation equation (GEE) was used to examine between group differences in likelihood of accumulating ≥60 minutes per day (min/d) of MVPA, ≥10 000 steps/d, and at least one bout-MVPA ≥30 min/d, while accounting for correlation of observations from the same subject. These criteria were selected based upon previous studies and PA guidelines and recommendations which state that this level of activity is important for weight loss maintenance (1, 7–9, 18, 20, 30). Within and between-group comparisons of PA patterns across the week and across the day were tested using linear mixed effect models that included group, time, and group × time interaction terms as fixed effects, and an unstructured covariance. If the interaction term was significant, post-hoc comparisons were conducted. There were no adjustments for multiple comparisons because there was no concern with the universal null hypothesis that subject groups were identical on all variables (31). Power was estimated for the previously published primary outcome of the study (difference in total daily energy expenditure between groups) using PASS (power and sample size) software (NCSS, Kayesville, Utah). It was estimated that 35 participants per group would be needed to have 80% power to detect a 130 kcal/d difference in total daily energy expenditure (28). There was no a-priori power analysis for the outcomes of this secondary data analysis. A sensitivity analysis was performed to examine the effect of seasonality on indices of PA. No differences in PA were observed based on seasonality. Results are reported as mean ± SD.
RESULTS
114 participants were screened, and 107 completed the outcomes assessment (Figure 1). 23 participants were missing data due to device errors or insufficient wear time, resulting in a final sample size of 84 participants. Baseline characteristics of the three groups are shown in Table 1. BMI of WLM (23.6 ± 2.3 kg/m2) was similar to BMI of NC (22.8 ± 1.9 kg/m2). Pre-weight loss BMI of WLM (32.4 ± 4.3 kg/m2) was similar to the current BMI of OC (33.6 ± 5.1 kg/m2). Overall differences in body composition were driven by the comparisons between WLM and NC to OC; there were no significant differences in body composition in pairwise comparisons between NC and WLM (p>0.05). WLM were maintaining weight loss for 9.0 ± 10.0 years. Participants wore the activPAL™ for a median of 4 weekdays and 2 weekend days with mean time spent awake (excluding time in bed) of 16.3 ± 1.6 hours per day (h/d), 16.2 ± 1.1 h/d, 15.7 ± 1.4 h/d for WLM, NC, and OC, respectively with no differences between groups.
FIGURE 1.

STUDY ENROLLMENT
TABLE 1.
PARTICIPANT CHARACTERISTICS
| WLM (n=28) |
NC (n=30) |
OC (n=26) |
Overall p-value |
|
|---|---|---|---|---|
| Female, n, (%) | 20, (71%) | 22, (73%) | 22, (85%) | 0.50 |
| Ethnicity | 0.13 | |||
| Hispanic/Latino | - | 4, (13%) | 3, (12%) | - |
| Not Hispanic/Latino | 28, (100%) | 26, (87%) | 23, (88%) | - |
| Race | 0.03 | |||
| Asian | - | 2, (7%) | - | - |
| Black/African American | - | 1, (3%) | 4, (15%) | - |
| White | 28, (100%) | 26, (87%) | 22, (85%) | - |
| Not Reported | - | 1, (3%) | - | - |
| Age (years) | 45.1 ± 12.1 | 47.6 ± 13.7 | 47.6 ± 10.9 | 0.70 |
| Current BMI (kg·m−2) | 23.6 ± 2.3 | 22.8 ± 1.9 | 33.6 ± 5.1 | <0.01 |
| Maximum BMI (kg·m−2) | 32.4 ± 4.3 | 24.4 ± 2.1 | 35.9 ± 6.1 | <0.01 |
| Weight (kg) | 68.2 ± 11.4 | 63.8 ± 10.6 | 93.6 ± 19.0 | <0.01 |
| Fat Mass (kg) | 17.1 ± 4.7 | 18.2 ± 4.5 | 38.1± 10.5 | <0.01 |
| Fat Free Mass (kg) | 49.4 ± 10.4 | 44.5± 9.4 | 54.2 ± 10.7 | <0.01 |
| Weight Loss Duration (y) | 9.0 ± 10.0 | - | - | - |
Data reported as Mean ± SD
Significant p-values are bolded (p<0.05)
Summary Measures
Weekly summary measures of SED, LPA, MVPA and steps have been published (2). WLM exhibited significantly higher mean weekly steps per day (11959 ± 5015 steps/d) and MVPA (93.3 ± 39.9 min/d) compared to NC (9001 ± 2629 steps/d, 68.8 ± 19.6 min/d) and OC (7110 ± 2370 steps/d, 56.2 ± 20.0 min/d) across the observation period (p<0.05). WLM also engaged in significantly higher amounts of mean LPA (291.4 ± 91.2 min/d) compared to OC (234.9 ± 69.5 min/d) across the observation period (p<0.05). There were no between group differences in mean time in bed (h/d) or SED (min/d).
Patterns of Physical Activity and Sedentary Behavior across the Week
There were no significant group × time interactions for time in bed, SED, LPA, and MVPA across the different days of the week (Figure 2A–2C, p>0.05). WLM accumulated ≥10 000 steps/d on 67% of days which was significantly more than NC (42%, p=0.02) and OC (8%, p<0.001). Similarly, WLM engaged in ≥60 min/d of MVPA on 73% of days which was significantly more than OC (36%, p<0.001) but not different from NC (59%, p=0.10).
FIGURE 2. PHYSICAL ACTIVITY AND SEDENTARY BEHAVIOR ACROSS THE WEEK.

A – mean daily sedentary time (SED) across the week by group
B – mean daily light physical activity (LPA) across the week by group
C – mean daily moderate to vigorous physical activity (MVPA) across the week by group Error bars indicate SEM
WLM had significantly lower SED on weekend days (−58.0 min/d; p=0.01) compared to weekdays, but there were no significant differences in LPA and MVPA. NC had lower SED by 61.6 min/d (p<0.01) and higher LPA by 39.2 min/d (p=0.02) on weekend days compared to weekdays, with no significant differences in MVPA. OC had higher SED by 50.6 min/d (p=0.04) and longer time in bed by 0.8 h·d−1 (p=0.04) on weekend days, with no significant differences in LPA and MVPA.
Patterns of Physical Activity and Sedentary Behavior across the Day
There was a significant group × time interaction for SED and MVPA within the day (Figure 3A–3C, p≤0.05). Compared to OC, WLM engaged in higher amounts of MVPA 0–3, 3–6, 9–12, and 12–15 hours from wake. Compared to NC, WLM engaged in significantly higher amounts of steps in 0–3 and 12–15 hours from wake. NC engaged in significantly higher amounts of steps 9–12 hours from wake compared to OC. The most pronounced difference between WLM and both NC and OC in MVPA and steps was observed within 3 hours of waking. WLM engaged in significantly lower amounts of SED compared to NC and OC for the 0–3, 12–15 and 0–3, 6–9, 9–12 bins, respectively. Compared to OC, NC engaged in significantly lower amounts of SED 6–9 and 9–12 hours from wake. The group × time interaction for LPA neared significance (p=0.052).
FIGURE 3. PHYSICAL ACTIVITY AND SEDENTARY BEHAVIOR ACROSS THE DAY.
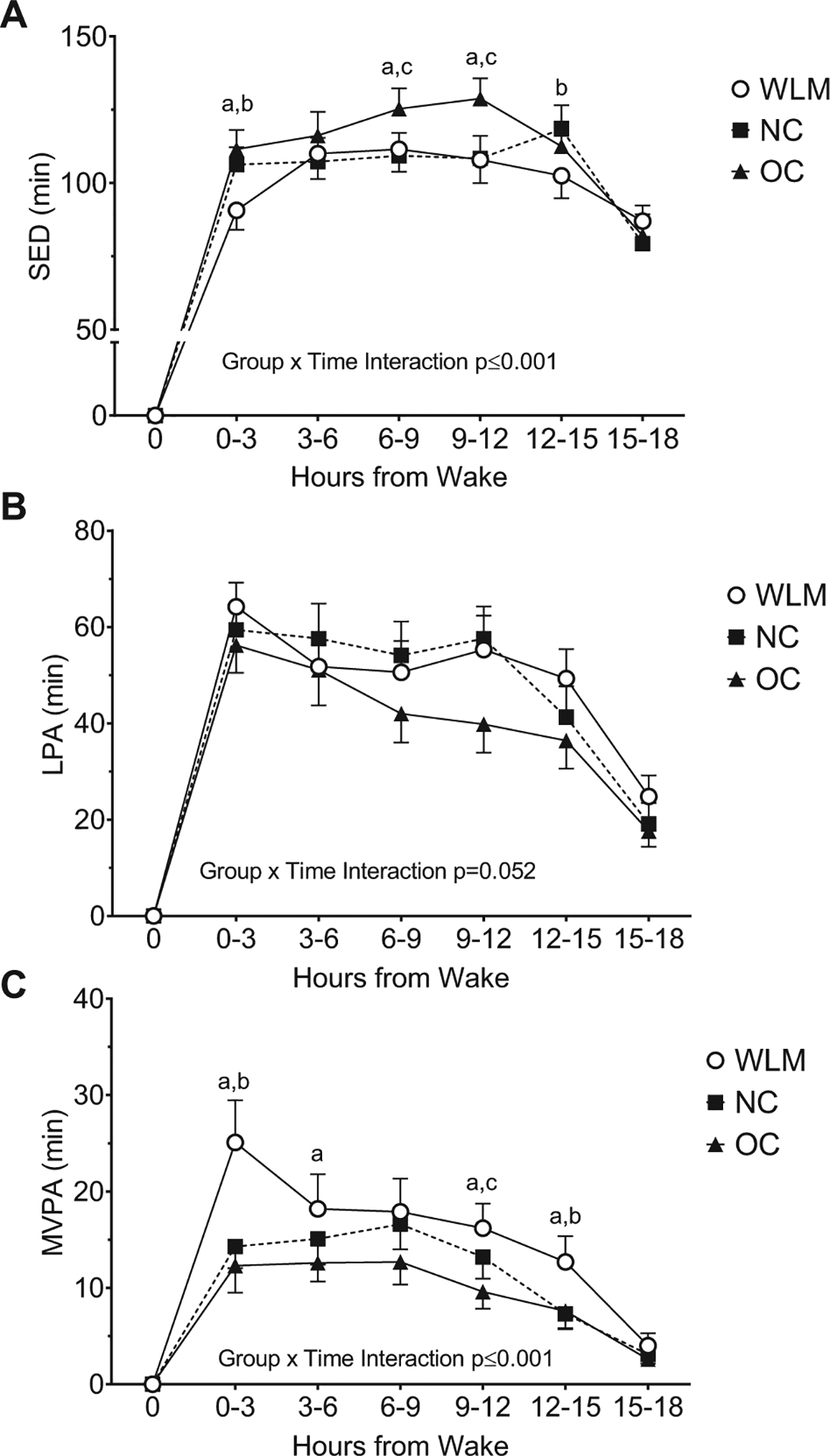
A – mean sedentary time (SED) in each 3-hour window across the day by group
B – mean light physical activity (LPA) in each 3-hour window across the day by group
C – mean moderate to vigorous physical activity (MVPA) in each 3-hour window across the day by group
a significant difference between WLM and OC (p<0.05); b significant difference between WLM and NC (p<0.05); c significant difference between NC and OC (p<0.05); Error bars indicate SEM
Patterns of Bout-MVPA Accumulation
Bout-MVPA accumulated across the week is presented in Figure 4. WLM engaged in significantly higher levels of total bout-MVPA than both NC and OC (p<0.001), and NC engaged in significantly higher levels of total bout-MVPA than OC (p<0.05). WLM engaged in significantly more MVPA in bout durations of 10–29 min, 30–59 min, and ≥60 min compared to OC (p<0.05) and more MVPA in bout durations of ≥60 min compared to NC (p<0.05). NC accumulated more MVPA in bout durations of 30–59 min compared to OC. When examining the proportion of total bout-MVPA accumulated in the different duration categories, OC accumulated the majority of their bout-MVPA in bout durations of 1–9 min (51%; 62.0 min/wk), whereas WLM (72%; 218.1 min/wk) and NC (57%; 106.0 min/wk) accumulated the majority their bout-MVPA in bout durations of ≥10 min. WLM had at least one bout of MVPA ≥30 min on 41% of valid days; this was significantly more than NC (24%, p=0.03) and OC (9%, p<0.001).
FIGURE 4. WEEKLY BOUT MVPA PATTERNS.

Mean duration of Bout-MVPA in different bout durations across the week by group
a significant difference between WLM and OC (p<0.05); b significant difference between WLM and NC (p<0.05); c significant difference between NC and OC (p<0.05); Letters at the top of bars represent differences in total Bout-MVPA
DISCUSSION
Successful weight loss maintenance is consistently associated with engagement in high levels of PA (1). Previous studies using self-report measures of PA have found that individuals who successfully maintain weight loss engage in ≥200 min/wk of MVPA (6, 7, 17). More recently, these findings have been reproduced using device measured MVPA (2, 3). This study builds upon these previous findings by determining how and when individuals maintaining a significant weight loss accumulate their PA across the week and within a day. This study had three primary findings. First, WLM consistently engaged in high amounts of PA (e.g., ≥60 min of MVPA per day) on more days of the week than controls. Second, WLM accumulated more MVPA in sustained bouts (≥10 minutes) compared to controls. In particular, WLM engaged in more MVPA in bouts ≥60 minutes. Third, WLM accumulated higher amounts of MVPA (~30 min) and steps (~3000 steps) within 3 hours of waking compared to controls. These differences in temporal patterns of PA are novel and may inform future studies of PA interventions targeting long-term weight loss.
The 2009 American College of Sports Medicine (ACSM) Position Stand titled Appropriate Physical Activity Intervention Strategies for Weight Loss and Prevention of Weight Regain for Adults highlights that ≥250 min/wk of MVPA is associated with improved weight loss maintenance (1). In addition, it was concluded that engaging in ~60 min/d of walking at a moderate intensity was associated with weight loss maintenance. The present study demonstrates that WLM consistently engage in high levels of MVPA on most days of the week, accruing ≥60 min/d of MVPA on 73% of days (~5 d/wk). NC and OC achieved ≥60 min/d of MVPA with a lower frequency (~4 d/wk and ~2 d/wk respectively). Our device-measured data align with a recently published study, which found that weight loss maintainers self-reported engaging in ~300–400 min/wk of MVPA accumulated across 4–5 d/wk (16). It is possible that to attain such high levels of weekly MVPA, individuals need to engage in high amounts of MVPA almost daily (≥5 d/wk). It remains unclear if engaging in high amounts of daily PA helps to promote weight loss maintenance beyond the effect of the total weekly dose of PA. Future studies are needed to understand if the pattern of PA accumulation across the week influences physiological and/or behavioral parameters that are known to affect body weight regulation. For example, future PA and comprehensive behavioral weight loss interventions could evaluate whether expressing PA goals for weight loss maintenance as a daily goal rather than expressed based on a per week basis may be more effective. Further, studies may seek to identify which populations respond best to these different prescriptions leading to more tailored interventions in the future.
Because many individuals monitor their PA in steps/d rather than min/wk, we also quantified PA in steps/d. WLM averaged ~12 000 steps/d, which was significantly more than NC and OC. WLM accumulated ≥10,000 steps/d most days of the week. This finding is similar to previous literature citing that individuals who maintained ≥10% weight loss at 18 months following a behavioral weight loss intervention average ~10 000 steps/d (18). Based on these two studies it appears that recommending the accumulation of ≥10 000 steps/d is an adequate threshold for weight loss maintenance; however, the intensity and pattern of step accumulation may also be important (18). In particular, higher stepping cadences or higher intensity stepping is associated with increased energy expenditure (32, 33). Thus, both the total volume of steps and the stepping intensity may have important implications for long-term weight management.
Several cross-sectional and prospective studies have found that weight loss maintenance is associated with high levels of MVPA, specifically MVPA accumulated in bouts ≥10 minutes (2, 3). This bout threshold of ≥10 minutes typically comes from past studies using self-reported assessment tools; however, with advances in wearable technology, capturing PA behaviors in epochs of one minute or even shorter has become feasible. Thus, it is now possible to determine whether the minute-by-minute pattern of PA accumulation is an important factor for weight management. In the present analysis, we found that WLM accumulate a high amount of MVPA in bouts ≥10 minutes (~220 min/wk). This amount was substantially greater than both NC and OC. These data align with previous findings from Jakicic et al. in which individuals maintaining a weight loss of ≥10% across an 18-month behavioral weight loss intervention engaged in the equivalent of 200–300 min/wk of device measured MVPA in bouts of ≥10 minutes (3). In the present study, WLM also accumulated significantly higher amounts of MVPA in bouts of longer duration (≥30 and ≥60 minutes) compared to OC and NC, respectively. In a previous study examining the effect of prescribing PA in short bouts (10 min per bout) versus long bouts (30 min per bouts) across an 18-month weight loss intervention, Jakicic et al. found that prescribing PA in long bouts did not lead to improved long-term engagement in PA or enhanced weight loss compared to short bouts (7). In contrast, our findings suggest that accumulating high levels of weekly MVPA may require engagement in longer, sustained bouts of MVPA. Thus, it is possible that structured, planned PA (e.g., exercise) is needed to achieve the levels of PA required for weight loss maintenance. However, future randomized studies are needed to determine the optimal strategy for accumulating the high amounts of PA which are associated with weight loss maintenance.
Recent studies suggest that time of day PA is performed may influence energy balance and body weight regulation (13, 14, 34). In a secondary analysis of a tightly controlled supervised exercise study, Willis et al. found that morning exercisers lost significantly more body weight (nearly 3 fold greater) compared to evening exercisers despite similar levels of adherence and exercise energy expenditure (13). In that study it appeared that morning exercisers exhibited attenuated physiologic and behavioral compensation (i.e. reduced increases in energy intake and reduced decreases in non-exercise PA) resulting in a greater energy deficit compared to evening exercisers. In the current study, we found that WLM engaged in more MVPA and less sedentary behavior across most of the waking day compared to both NC and OC, suggesting that WLM are generally more active across the day. In addition, we observed that WLM were markedly more active within 3 hours of waking, significantly more so than both NC and OC. WLM accumulated over 3,000 steps and nearly 30 minutes of MVPA within 3 hours of waking, indicative of morning exercise. While the current study did not capture the chronotype of participants, one previous study found that weight loss maintainers are more likely to be morning-type people (35). Our PA data support this previous finding. It is unclear if morning PA helps to promote weight loss maintenance through physiologic or behavioral mechanisms or both. A recent study by Schumacher et al. found that consistency in the time of day of exercise rather than the specific time of day was associated with higher amounts of overall PA (16), suggesting that a behavioral mechanism (i.e. habit formation) may be important for engaging in high amounts of PA. More studies are needed to understand how the timing of PA affects both physiologic and behavioral factors related to weight management. Additionally, research is needed in more diverse populations to identify if other factors such as age, race/ethnicity, and sex influence the relationship between time of PA and body weight.
The present study has several strengths including the use of device-measured PA, novel analyses of PA data, and a unique understudied population, weight loss maintainers. However, this study has several limitations. This was an observational study; thus, it is not possible to determine causation. Further, this study enrolled a cohort of 28 WLM who were primarily white, non-Hispanic females; thus, the PA patterns of these WLM are not representative of all individuals who are maintaining weight loss. Future studies should seek to recruit a more diverse sample to determine if the observed results translate to other populations. Nonetheless, studies of WLM are lacking, specifically studies with device-measured PA. The PA measurement period in this study was 7 days with 5 days used for analysis. Although efforts were made to ensure this observation represented a normal week, it is possible that the reported weekly and daily patterns of PA may be unrepresentative of habitual PA. Due to limitations of the activPAL™ algorithms to identify activity intensity based on step cadence it is also possible that PA was misclassified for some participants in this study. The activPAL™ algorithms used to identify activity intensity based on step cadence have been noted to misclassify light to moderate intensity PA, such that it may overestimate MVPA in some individuals (36). However, this misclassification error is likely smaller than what would be expected with self-reported PA measures. Future studies should attempt to replicate these findings with other PA devices. Despite these limitations, this study expands our current understanding of PA and weight management by moving beyond simply reporting traditional weekly summary measures of device measured PA data in a sample who has maintained weight loss on average for 9.0 ± 10.0 years. Understanding the temporal patterns of PA across the day and week in successful WLM may provide insight for future experimental studies to evaluate novel strategies for promoting PA for weight management.
In summary, individuals successfully maintaining a substantial weight loss were highly active most days of week (~5 d/wk), significantly more days per week than controls. These individuals accumulated the majority of their MVPA in bouts of ≥10 minutes. In particular, they accumulated more total Bout-MVPA and more MVPA in bouts of >60 min compared to controls with and without obesity. Finally, individuals who are successfully maintaining weight loss engaged in significantly more PA in the morning (i.e. within 3 hours of waking) compared to controls. When promoting PA for weight management it may be advantageous to provide recommendations related to consistency across days, bout duration, and PA timing across the day.
ACKNOWLEDGEMENTS
The primary funding source for this study was K23 DK078913 (PI Catenacci). Additionally, the Colorado Nutrition and Obesity Research Center P30 DK048520 and the Colorado Clinical and Translational Sciences Institute UL1 TR002535 provided resources and support. SAC is supported by an NIH award (K01 HL145023) as is DMO (F32 DK122652). VAC designed the study, wrote the protocol, and acquired the data. SAC, PRH, EC, and KL processed and summarized the data. SAC, PRH, EC, KL, DMO, EAW, ZP, ELM, and VAC interpreted the data, generated tables and figures, and wrote, revised, and approved the final manuscript. We would like to thank Rena R. Wing, PhD, James O. Hill, PhD, and Holly R. Wyatt, MD, for assisting with the original design and recruitment of this this study, as well as providing mentorship.
COMPETING INTERESTS:
This study was supported by the following NIH grant funding: K23 DK078913 (PI Catenacci), K01 HL145023 (PI Creasy), F32 DK122652 (PI Ostendorf), P30 DK048520, and UL1 TR002535. ELM is supported by resources from the Geriatric Research, Education, and the Clinical Center at the Denver VA Medical Center. The contents do not represent the views of the U.S. Department of Veterans Affairs or the United States Government. Authors have nothing else to disclose.
Footnotes
CLINICAL TRIALS IDENTIFIER
REFERENCES
- 1.Donnelly JE, Blair SN, Jakicic JM, Manore MM, Rankin JW, Smith BK. American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009;41(2):459–71. [DOI] [PubMed] [Google Scholar]
- 2.Ostendorf DM, Lyden K, Pan Z, Wyatt HR, Hill JO, Melanson EL, et al. Objectively Measured Physical Activity and Sedentary Behavior in Successful Weight Loss Maintainers. Obesity. 2018;26(1):53–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jakicic JM, Tate DF, Lang W, Davis KK, Polzien K, Neiberg RH, et al. Objective physical activity and weight loss in adults: The step-up randomized clinical trial. Obesity. 2014;22(11):2284–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Klem ML, Wing RR, McGuire MT, Seagle HM, Hill JO. A descriptive study of individuals successful at long-term maintenance of substantial weight loss. Am J Clin Nutr. 1997;66(2):239–46. [DOI] [PubMed] [Google Scholar]
- 5.Phelan S, Roberts M, Lang W, Wing RR. Empirical evaluation of physical activity recommendations for weight control in women. Med Sci Sports Exerc. 2007;39(10):1832–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jakicic JM, Marcus BH, Lang W, Janney C. Effect of exercise on 24-month weight loss maintenance in overweight women. Arch Intern Med. 2008;168(14):1550–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jakicic JM, Winters C, Lang W, Wing RR. Effects of intermittent exercise and use of home exercise equipment on adherence, weight loss, and fitness in overweight women: a randomized trial. JAMA. 1999;282(16):1554–60. [DOI] [PubMed] [Google Scholar]
- 8.Fogelholm M, Stallknecht B, Van Baak M. ECSS position statement: Exercise and obesity. Eur J Sport Sci. 2006;6(1):15–24. [Google Scholar]
- 9.Saris WH, Blair SN, van Baak MA, Eaton SB, Davies PS, Di Pietro L, et al. How much physical activity is enough to prevent unhealthy weight gain? Outcome of the IASO 1st Stock Conference and consensus statement. Obes Rev. 2003;4(2):101–14. [DOI] [PubMed] [Google Scholar]
- 10.Lee IM, Sesso HD, Oguma Y, Paffenbarger RS Jr. The “weekend warrior” and risk of mortality. Am J Epidemiol. 2004;160(7):636–41. [DOI] [PubMed] [Google Scholar]
- 11.O’Donovan G, Lee IM, Hamer M, Stamatakis E. Association of “Weekend Warrior” and Other Leisure Time Physical Activity Patterns With Risks for All-Cause, Cardiovascular Disease, and Cancer Mortality. JAMA Intern Med. 2017;177(3):335–42. [DOI] [PubMed] [Google Scholar]
- 12.Shiroma EJ, Lee IM, Schepps MA, Kamada M, Harris TB. Physical Activity Patterns and Mortality: The Weekend Warrior and Activity Bouts. Med Sci Sports Exerc. 2019;51(1):35–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Willis EA, Creasy SA, Honas JJ, Melanson EL, Donnelly JE. The effects of exercise session timing on weight loss and components of energy balance: midwest exercise trial 2. Int J Obes (Lond). 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Alizadeh Z, Younespour S, Rajabian Tabesh M, Haghravan S. Comparison between the effect of 6 weeks of morning or evening aerobic exercise on appetite and anthropometric indices: a randomized controlled trial. Clin Obes. 2017;7(3):157–65. [DOI] [PubMed] [Google Scholar]
- 15.Ezagouri S, Zwighaft Z, Sobel J, Baillieul S, Doutreleau S, Ladeuix B, et al. Physiological and Molecular Dissection of Daily Variance in Exercise Capacity. Cell Metab. 2019;30(1):78–91.e4. [DOI] [PubMed] [Google Scholar]
- 16.Schumacher LM, Thomas JG, Raynor HA, Rhodes RE, O’Leary KC, Wing RR, et al. Relationship of Consistency in Timing of Exercise Performance and Exercise Levels Among Successful Weight Loss Maintainers. Obesity (Silver Spring, Md). 2019;27(8):1285–91. [DOI] [PubMed] [Google Scholar]
- 17.Jakicic JM, Marcus BH, Gallagher KI, Napolitano M, Lang W. Effect of exercise duration and intensity on weight loss in overweight, sedentary women: a randomized trial. JAMA. 2003;290(10):1323–30. [DOI] [PubMed] [Google Scholar]
- 18.Creasy SA, Lang W, Tate DF, Davis KK, Jakicic JM. Pattern of Daily Steps is Associated with Weight Loss: Secondary Analysis from the Step-Up Randomized Trial. Obesity (Silver Spring, Md). 2018;26(6):977–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Physical Activity Guidelines Advisory Committee. Physical activity guidelines advisory committee report, 2008. US Deparment of Health and Human Services. Washington, DC. 2008. p. A1–H14. [Google Scholar]
- 20.US Department of Health and Human Services. Physical Activity Guidelines for Americans, 2nd Edition. US Department of Health and Human Services. Washington, DC. 2018. [Google Scholar]
- 21.De Jong NP, Rynders CA, Goldstrohm DA, Pan Z, Lange AH, Mendez C, et al. Effect of frequent interruptions of sedentary time on nutrient metabolism in sedentary overweight male and female adults. J Appl Physiol (Bethesda, Md : 1985). 2019;126(4):984–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dunstan DW, Kingwell BA, Larsen R, Healy GN, Cerin E, Hamilton MT, et al. Breaking up prolonged sitting reduces postprandial glucose and insulin responses. Diabetes Care. 2012;35(5):976–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fan JX, Brown BB, Hanson H, Kowaleski-Jones L, Smith KR, Zick CD. Moderate to vigorous physical activity and weight outcomes: does every minute count? Am J Health Promot. 2013;28(1):41–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Saint-Maurice PF, Troiano RP, Matthews CE, Kraus WE. Moderate-to-Vigorous Physical Activity and All-Cause Mortality: Do Bouts Matter? J Am Heart Assoc. 2018;7(6). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jakicic JM, Kraus WE, Powell KE, Campbell WW, Janz KF, Troiano RP, et al. Association between Bout Duration of Physical Activity and Health: Systematic Review. Med Sci Sports Exerc. 2019;51(6):1213–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Thomson CA, Morrow KL, Flatt SW, Wertheim BC, Perfect MM, Ravia JJ, et al. Relationship between sleep quality and quantity and weight loss in women participating in a weight-loss intervention trial. Obesity (Silver Spring, Md). 2012;20(7):1419–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Creasy SA, Rynders CA, Bergouignan A, Kealey EH, Bessesen DH. Free-Living Responses in Energy Balance to Short-Term Overfeeding in Adults Differing in Propensity for Obesity. Obesity (Silver Spring, Md). 2018;26(4):696–702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ostendorf DM, Caldwell AE, Creasy SA, Pan Z, Lyden K, Bergouignan A, et al. Physical Activity Energy Expenditure and Total Daily Energy Expenditure in Successful Weight Loss Maintainers. Obesity (Silver Spring, Md). 2019;27(3):496–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ostendorf DM, Melanson EL, Caldwell AE, Creasy SA, Pan Z, MacLean PS, et al. No consistent evidence of a disproportionately low resting energy expenditure in long-term successful weight-loss maintainers. Am J Clin Nutr. 2018;108(4):658–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Jakicic JM, Wing RR, Butler BA, Robertson RJ. Prescribing exercise in multiple short bouts versus one continuous bout: effects on adherence, cardiorespiratory fitness, and weight loss in overweight women. Int J Obes Relat Metab Disord. 1995;19(12):893–901. [PubMed] [Google Scholar]
- 31.Perneger TV. What’s wrong with Bonferroni adjustments. Bmj. 1998;316(7139):1236–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Butts NK, Dodge C, McAlpine M. Effect of stepping rate on energy costs during StairMaster exercise. Med Sci Sports Exerc. 1993;25(3):378–82. [PubMed] [Google Scholar]
- 33.MacDonald MJ, Fawkner SG, Niven AG, Rowe D. Real World, Real People: Can We Assess Walking on a Treadmill to Establish Step Count Recommendations in Adolescents? Pediatr Exerc Sci. 2019;31(4):488–94. [DOI] [PubMed] [Google Scholar]
- 34.Brooker PG, Gomersall SR, King NA, Leveritt MD. The feasibility and acceptability of morning versus evening exercise for overweight and obese adults: A randomized controlled trial. Contemp Clin Trials Commun. 2019;14:100320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ross KM, Graham Thomas J, Wing RR. Successful weight loss maintenance associated with morning chronotype and better sleep quality. J Behav Med. 2016;39(3):465–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.O’Brien MW, Johns JA, Fowles JR, Kimmerly DS. Validity of the activPAL and Height-Adjusted Curvilinear Cadence-METs Equations in Healthy Adults. Meas Phys Educ Exerc Sci. 2020;24(2):147–56. [Google Scholar]


