Abstract
SARS-CoV-2 can infect a variety of wild and domestic animals worldwide. Of these, domestic cats are highly susceptible species and potential viral reservoirs. As such, it is important to investigate disease exposure in domestic cats in areas with active community transmission and high disease prevalence. In this report we demonstrate the presence of serum neutralizing antibodies against the receptor binding-domain (RBD) of the SARS-CoV-2 in cats whose owners had been infected with SARS-CoV-2 in Lima, Peru, using a commercial competitive ELISA SARS-CoV-2 Surrogate Virus Neutralization Test. Out of 41 samples, 17.1% (7/41) and 31.7% (13/41) were positive, using the cut-off inhibition value of 30% and 20%, respectively. Not all cats living in a single house had detectable neutralizing antibodies showing heterogenous exposure and immunity among cohabiting animals. This is the first report of SARS-COV-2 exposure of domestic cats in Lima, Peru. Further studies are required to ascertain the prevalence of SARS-COV-2 exposure among domestic cats.
Keywords: COVID-19, SARS-CoV-2, Cats, Serology, Neutralizing antibodies, One health
1. Introduction
The new human coronavirus, SARS-CoV-2, has been shown to mainly infect humans. However, SARS-CoV-2 infection has also been detected in a variety of animals, including wild cats, minks, ferrets, domestic dogs and cats [[1], [2], [3], [4], [5], [6]]. Cats and minks may be considered the most susceptible species because of the higher similarity of the angiotensin-converting enzyme 2 (ACE2) between these species and humans [7]. Although the majority of infected cats are asymptomatic, some animals may develop clinical disease, and the virus can be experimentally transmitted between individuals [8]. Therefore, SARS-CoV-2 could have a direct impact on animal health, while the possibility of cats becoming zoonotic reservoirs has not been totally discarded.
Serological testing is a valuable tool for screening antibody levels associated with pathogen exposure. As with other viral infections, host neutralizing serum antibodies may block the binding of viral proteins to cell surface receptors. In humans, SARS-CoV-2 neutralizing antibodies have been determined to inversely correlate with disease severity and can predict the probability of re-infections [9]. In animals, reported prevalence of neutralizing serum antibodies against SARS-CoV-2 in cats varies, with as low as 0.002% in Germany, 0.2% in Brazil, 5.8% in Italy, and 10.8% in Wuhan, China [[10], [11], [12], [13]]. In Peru, one of the most affected countries by the COVID-19 pandemic, no previous studies have been conducted investigating the seroprevalence or prevalence of SARS-CoV-2 among domestic cats. In this report we demonstrate the presence of serum neutralizing antibodies against the receptor binding-domain (RBD) of the SARS-CoV-2 viral spike protein in cats whose owners confirmed previous infection with SARS-CoV-2.
2. Materials and methods
Blood samples of cats seeking routine veterinary care were collected between August 2020 and April 2021 from three veterinary clinics in Lima, Peru. All cat owners signed an informed consent authorizing the use of the samples for research purposes. Samples were centrifuged at 3500 rpm for 5 min and the serum supernatant was transferred to microcentrifuge tubes and was stored at -20 °C. Samples from cats whose owners confirmed previous COVID-19 disease (clinical signs with positive IgG/IgM rapid test or qRT-PCR) during veterinary anamnesis were conveniently selected. To test the serum samples for the presence of neutralizing antibodies against the RBD of the viral spike protein, a commercial competitive ELISA cPass™ SARS-CoV-2 Neutralization Antibody Detection Kit also known as SARS-CoV-2 Surrogate Virus Neutralization Test (sVNT) Kit was used according to the manufacturer's instructions (Genscript, New Jersey, USA). Percent serum neutralization was calculated as follows: = (1 - OD value of sample / OD value of negative control) × 100%. A cut-off value of 20% and an updated 30% of inhibition were used to establish positivity. This study was approved by the Universidad Peruana Cayetano Heredia Animal Care and Use Ethical Committee (N° 027-08-20).
3. Results and discussion
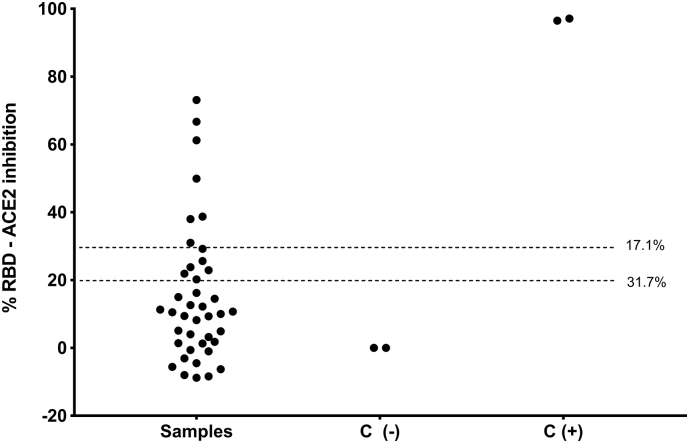
A total of 41 samples from a serum bank of 700 were selected for screening of serum neutralizing antibodies. The median age of the animals was 12 months (IQR: 8 months – 46 months), 53.7% were female (22/41), and 87.8% (36/41) were classified as domestic shorthair. 53.7% (22/41) came from the district of Comas while the remainder 46.3% came from Miraflores (5/41), Surco (5/41), San Juan de Miraflores (3/41), Independencia (2/41), San Juan de Lurigancho (1/41), San Luis (1/41), and San Martín de Porres (1/41). Out of the 41 cat samples, 22 cats (53.7%) lived in a single household (household C), and 2 cats lived in household D. Age, sex, breed, neuter status and district of all animals are shown in Table 1. Animals living in households C and D attended the veterinary clinic for neutering. The rest of the animals attended the veterinary clinics seeking for care based on unspecific clinical signs. Out of the 41 samples, 17.1% (7/41) and 31.7% (13/41) were positive for the presence of serum neutralizing antibodies, using the cut-off value of 30% and 20%, respectively (Fig. 1).
Table 1.
Data of cats with serum neutralizing antibodies against SARS-COV-2 in Lima (2020−2021).
| Household | Sample Date (MM/DD/YY) | Age (months) | Sex | Breed | Neuter status | District | Time since onset of clinical symptoms of COVID-19 in owners (weeks) | Percent Inhibition (%) |
|---|---|---|---|---|---|---|---|---|
| A | 1/20/2021 | 7 | Male | Domestic Shorthair | Intact | San Juan de Miraflores | Not available | 73.06 |
| A | 1/21/2021 | 28 | Female | Domestic Shorthair | Intact | San Juan de Miraflores | Not available | 66.69 |
| B | 4/01/2021 | 8 | Female | Domestic Shorthair | Spayed | San Juan de Miraflores | Not available | 3.2 |
| C | 10/9/2020 | 8 | Female | Domestic Shorthair | Intact | Comas | 12 | 29.15 |
| C | 10/9/2020 | 12 | Female | Domestic Shorthair | Intact | Comas | 12 | 25.59 |
| C | 10/9/2020 | 11 | Female | Domestic Shorthair | Intact | Comas | 12 | 23.81 |
| C | 10/9/2020 | 36 | Male | Domestic Shorthair | Intact | Comas | 12 | 22.88 |
| C | 10/9/2020 | 10 | Female | Domestic Shorthair | Intact | Comas | 12 | 20.24 |
| C | 10/9/2020 | 5 | Male | Domestic Shorthair | Intact | Comas | 12 | 10.69 |
| C | 10/9/2020 | 5 | Male | Domestic Shorthair | Intact | Comas | 12 | 4.92 |
| C | 10/9/2020 | 24 | Male | Domestic Shorthair | Intact | Comas | 12 | 9.27 |
| C | 10/9/2020 | 12 | Female | Domestic Shorthair | Intact | Comas | 12 | −3.14 |
| C | 10/9/2020 | 12 | Female | Domestic Shorthair | Intact | Comas | 12 | −0.64 |
| C | 10/9/2020 | 24 | Female | Domestic Shorthair | Intact | Comas | 12 | 14.47 |
| C | 10/9/2020 | 10 | Female | Domestic Shorthair | Intact | Comas | 12 | 16.18 |
| C | 10/9/2020 | 60 | Female | Domestic Shorthair | Intact | Comas | 12 | 3.99 |
| C | 10/9/2020 | 5 | Female | Domestic Shorthair | Intact | Comas | 12 | 1.8 |
| C | 10/24/2020 | 9 | Male | Domestic Shorthair | Intact | Comas | 12 | 61.22 |
| C | 10/24/2020 | 6 | Male | Domestic Shorthair | Intact | Comas | 12 | 49.87 |
| C | 10/24/2020 | 11 | Male | Domestic Shorthair | Intact | Comas | 12 | 38.03 |
| C | 10/24/2020 | 8 | Female | Domestic Shorthair | Intact | Comas | 12 | −8.38 |
| C | 10/24/2020 | 8 | Female | Domestic Shorthair | Intact | Comas | 12 | −8.75 |
| C | 10/24/2020 | 24 | Female | Domestic Shorthair | Intact | Comas | 12 | 12.58 |
| C | 10/24/2020 | 7 | Female | Domestic Shorthair | Intact | Comas | 12 | 8.18 |
| C | 10/24/2020 | 6 | Female | Domestic Shorthair | Intact | Comas | 12 | −5.59 |
| D | 1/27/2021 | 24 | Female | Domestic Shorthair | Intact | Independencia | 3 | 38.73 |
| D | 1/27/2021 | 60 | Male | Domestic Shorthair | Intact | Independencia | 3 | 30.96 |
| F | 8/17/2020 | 84 | Male | Russian Blue | Neutered | Miraflores | 8 | 21.88 |
| F | 8/31/2020 | 72 | Female | Russian Blue | Spayed | Miraflores | 10 | 9.41 |
| F | 8/31/2020 | 12 | Male | Bengal | Neutered | Miraflores | 10 | 11.26 |
| F | 8/31/2020 | 12 | Male | Bengal | Neutered | Miraflores | 10 | 15.04 |
| G | 2/14/2021 | 46 | Female | Maine Coon | Spayed | Miraflores | 10 | 10.48 |
| H | 12/29/2020 | 96 | Female | Domestic Shorthair | Intact | Surco | 24 | 5.06 |
| I | 1/13/2021 | 6 | Male | Domestic Shorthair | Neutered | Surco | Not available | −7.98 |
| J | 4/03/2021 | 58 | Male | Domestic Shorthair | Neutered | Surco | 8 | 1.31 |
| K | 1/02/2021 | 64 | Male | Domestic Shorthair | Neutered | Surco | Not available | −4.48 |
| L | 2/06/2021 | 42 | Female | Domestic Shorthair | Intact | Surquillo | 8 | −6.33 |
| M | 2/06/2021 | 77 | Male | Domestic Shorthair | Neutered | San Luis | 28 | 1.39 |
| N | 1/03/2021 | 124 | Male | Domestic Shorthair | Neutered | San Juan de Lurigancho | Not available | 12.19 |
| O | 10/13/2020 | 63 | Male | Domestic Shorthair | Neutered | San Martín de Porres | 1 | 10.05 |
| P | 2/02/2021 | 9 | Male | Domestic Shorthair | Neutered | Surco | Not available | −1.02 |
Different capital letters represent different households. Percent inhibition (%) in bold denotes positivity (>20%).
Fig. 1.
Percent inhibition against SARS-COV-2 receptor binding-domain (RBD) in serum of domestic cats whose owners had a history of COVID-19 (n = 41). C: controls, (−): negative, (+): positive. The 17.1% (7/41) and 31.7% (13/41) shows the frequency of cats with neutralizing antibodies with 30% and 20% of cut-off values of inhibition, respectively.
Out of 13 positive samples, 38.4% (5/13) showed clinical signs including sneezing and dyspnea, cough, vomit, or depression. Interestingly, one of the animals with the highest percent neutralization (73.06%) showed all the symptoms described. A subclinical infection, with a prolonged period of oral and nasal viral shedding that is generally not accompanied by symptomatology has been reported in cats [14]. Only 8 out 22 cats in household C had evidence of serum neutralizing antibodies. This suggests that infection may not be homogenous among cohabiting animals, and this could be associated with other factors such as health state, immunity, proximity to the infected owner(s), among others.
Our results show compelling evidence of SARS-CoV-2 exposure in domestic cats and it is the first report of such an event in Peru. Percent seropositivity in this population of cats is high compared to other studies published, such as that of Italy and Wuhan, China, in which 5.8% of 191 cats 10.8% of 102 cats had neutralizing antibodies, respectively [12,13]. However, these studies were not exclusively done on a pet population living with COVID-19 infected owners. In a longitudinal cohort study of pets living with COVID-19 owners conducted in Texas, USA, 43.8% of 16 cats developed neutralizing antibodies against SARS-CoV-2 [15], percentage that is closer to the results obtained in this study.
Limited sample size and a convenience sample do not permit prevalence estimation and seroconversion dynamics. Another limitation is the prolonged time between the onset of COVID-19 in owners and sampling of animals, which could have affected the sensitivity of the test. The immunity duration in pets is currently unknown. Experimentally infected cats develop neutralizing activity by seven days post-viral infection, but seroconversion is evident by 14 days with a plateaued stage at day 42 [16].
Serum neutralization activity is commonly tested using plaque reduction neutralization tests (PRNT) as gold standard. However, the commercial assay utilized in this preliminary study has shown a high correlation with serum neutralization activity using PRNT and has shown robust internal validity parameters for both humans, cats, dogs and hamster sera [17,18]. Additionally, this test has already been used in a large-scale serological survey in cats in Thailand using 20% of inhibition as the cut-off value [19]. Our study reports results based on both a 20% and a 30% inhibition cut-off value, based on the manufacturer's recommendation. Moreover, moderate to high sensitivity and specificity of the sVNT has been reported using this cut-off value correction (30%) in samples from multiple animal species (ferrets, cats, minks, hamster). Specifically, the specificity was 99% and 100% using 20% and 30% cut-off values, respectively [20]. The sensitivity of the sVNT using a cut-off value of 20% was 98.9% and 97% when compared to PRNT90 and PRNT50, respectively, yet sensitivity decreased to 93.9% when using a 30% of cut-off value (compared to PRNT50) [17]. Additionally, this commercial assay offers logistical and biosafety advantages for researchers working in resource-limited settings that do not have access to a BSL-3 containment required for SARS-CoV-2 manipulation.
The animals evaluated in our study sought routine veterinary care that was not associated with symptomatic respiratory disease in most of the cases, demonstrating potential asymptomatic infection in cats, and consequently, potential viral reservoirs. In some studies, over 21% and 25% of infected households sampled had pets with neutralizing antibodies [15,21]. Few case studies of natural infection in cats document severe clinical outcomes, and those that have revealed that co-morbidities likely played a contributing factor in illness or death [15]. Seroprevalence studies should be conducted in affected regions to monitor SARS-CoV-2 asymptomatic infections in pets such as cats, ferrets, or dogs, especially in companion animals living with COVID-19 patients [22].
4. Conclusions
It is crucial to monitor SARS-CoV-2 exposure and infection in domestic animals using rapid and affordable point-of-care serological and molecular assays that can be used by veterinarians serving low-income communities. Cats have the potential to serve as sentinels for undetected community transmission, and in this scenario, veterinarians play a key role as first-line responders.
Ethics statement
The authors confirm that the ethical policies of the journal, as noted on the journal's author guidelines page, have been adhered to and the appropriate ethical review committee approval has been received.
Conflict of interests
None noted.
CRediT authorship contribution statement
Luis M. Jara: Conceptualization, Formal analysis, Investigation, Writing – original draft, Writing – review & editing, Methodology. Cusi Ferradas: Conceptualization, Formal analysis, Investigation, Writing – original draft, Writing – review & editing, Methodology. Francesca Schiaffino: Conceptualization, Formal analysis, Investigation, Writing – original draft, Writing – review & editing, Methodology. Camila Sánchez-Carrión: Investigation, Writing – review & editing. Martínez-Vela: Investigation, Writing – review & editing. Alexandra Ulloa: Investigation, Writing – review & editing. Gisela Isasi-Rivas: Investigation, Writing – review & editing, Methodology. Angela Montalván: Investigation, Writing – review & editing, Methodology. Luis Guevara Sarmiento: Conceptualization, Formal analysis, Writing – review & editing, Methodology. Manolo Fernández: Conceptualization, Data curation, Formal analysis, Writing – review & editing, Methodology. Mirko Zimic: Conceptualization, Formal analysis, Funding acquisition, Writing – review & editing, Methodology.
Acknowledgements
Partial funding was received by D43TW007393 from the Emerging Diseases and Climate Change Research Unit (Emerge), Universidad Peruana Cayetano Heredia, Lima, Peru. We would like to acknowledge Macarena Llalla, DVM, and Camila Talavera, DVM, for helping with the collection of cat serum samples, as well as all other Veterinary supportive staff.
References
- 1.Bertzbach L.D., Vladimirova D., Dietert K., Abdelgawad A., Gruber A.D., Osterrieder N., Trimpert J. SARS-CoV-2 infection of Chinese hamsters (Cricetulus griseus) reproduces COVID-19 pneumonia in a well-established small animal model. Transbound. Emerg. Dis. 2021;68:1075–1079. doi: 10.1111/tbed.13837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mahdy M.A.A., Younis W., Ewaida Z. An overview of SARS-CoV-2 and animal infection. Front. Vet. Sci. 2020;7:596391. doi: 10.3389/fvets.2020.596391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Munnink B.B. Oude, Sikkema R.S., Nieuwenhuijse D.F., Molenaar R.J., Munger E., Molenkamp R., van der Spek A., Tolsma P., Rietveld A., Brouwer M., Bouwmeester-Vincken N., Harders F., der Honing R. Hakze-van, Wegdam-Blans M.C.A., Bouwstra R.J., GeurtsvanKessel C., van der Eijk A.A., Velkers F.C., Smit L.A.M., Stegeman A., van der Poel W.H.M., Koopmans M.P.G. Transmission of SARS-CoV-2 on mink farms between humans and mink and back to humans. Science. 2021;371:172–177. doi: 10.1126/science.abe5901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Shi J., Wen Z., Zhong G., Yang H., Wang C., Huang B., Liu R., He X., Shuai L., Sun Z., Zhao Y., Liu P., Liang L., Cui P., Wang J., Zhang X., Guan Y., Tan W., Wu G., Chen H., Bu Z. Susceptibility of ferrets, cats, dogs, and other domesticated animals to SARS-coronavirus 2. Science. 2020;368:1016–1020. doi: 10.1126/science.abb7015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Sit T.H.C., Brackman C.J., Ip S.M., Tam K.W.S., Law P.Y.T., E.M.W. To, Yu V.Y.T., Sims L.D., Tsang D.N.C., Chu D.K.W., Perera R.A.P.M., Poon L.L.M., Peiris M. Infection of dogs with SARS-CoV-2. Nature. 2020;586:776–778. doi: 10.1038/s41586-020-2334-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wang L., Mitchell P.K., Calle P.P., Bartlett S.L., McAloose D., Killian M.L., Yuan F., Fang Y., Goodman L.B., Fredrickson R., Elvinger F., Terio K., Franzen K., Stuber T., Diel D.G., Torchetti M.K. Complete genome sequence of SARS-CoV-2 in a tiger from a U.S. zoological collection. Microbiol. Resour. Announc. 2020;9 doi: 10.1128/MRA.00468-20. e00468-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sreenivasan C.C., Thomas M., Wang D., Li F. Susceptibility of livestock and companion animals to COVID-19. J. Med. Virol. 2021;93:1351–1360. doi: 10.1002/jmv.26621. [DOI] [PubMed] [Google Scholar]
- 8.Halfmann P.J., Hatta M., Chiba S., Maemura T., Fan S., Takeda M., Kinoshita N., Hattori S.-I., Sakai-Tagawa Y., Iwatsuki-Horimoto K., Imai M., Kawaoka Y. Transmission of SARS-CoV-2 in domestic cats. N. Engl. J. Med. 2020;383:592–594. doi: 10.1056/NEJMc2013400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen X., Pan Z., Yue S., Yu F., Zhang J., Yang Y., Li R., Liu B., Yang X., Gao L., Li Z., Lin Y., Huang Q., Xu L., Tang J., Hu L., Zhao J., Liu P., Zhang G., Chen Y., Deng K., Ye L. Disease severity dictates SARS-CoV-2-specific neutralizing antibody responses in COVID-19. Signal Transduct. Target Ther. 2020;5:180. doi: 10.1038/s41392-020-00301-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dias H.G., Resck M.E.B., Caldas G.C., Resck A.F., da Silva N.V., Dos Santos A.M.V., das Sousa T.C., Ogrzewalska M.H., Siqueira M.M., Pauvolid-Corrêa A., Santos F.B. Dos. Neutralizing antibodies for SARS-CoV-2 in stray animals from Rio de Janeiro, Brazil. PLoS One. 2021;16:e0248578. doi: 10.1371/journal.pone.0248578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Michelitsch A., Hoffmann D., Wernike K., Beer M. Occurrence of antibodies against SARS-CoV-2 in the domestic cat population of Germany. Vaccines. 2020;8:E772. doi: 10.3390/vaccines8040772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Patterson E.I., Elia G., Grassi A., Giordano A., Desario C., Medardo M., Smith S.L., Anderson E.R., Prince T., Patterson G.T., Lorusso E., Lucente M.S., Lanave G., Lauzi S., Bonfanti U., Stranieri A., Martella V., Solari Basano F., Barrs V.R., Radford A.D., Agrimi U., Hughes G.L., Paltrinieri S., Decaro N. Evidence of exposure to SARS-CoV-2 in cats and dogs from households in Italy. Nat. Commun. 2020;11:6231. doi: 10.1038/s41467-020-20097-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zhang Q., Zhang H., Gao J., Huang K., Yang Y., Hui X., He X., Li C., Gong W., Zhang Y., Zhao Y., Peng C., Gao X., Chen H., Zou Z., Shi Z.-L., Jin M. A serological survey of SARS-CoV-2 in cat in Wuhan. Emerg. Microbes Infect. 2020;9:2013–2019. doi: 10.1080/22221751.2020.1817796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.K. Sharun, K. Dhama, A.M. Pawde, C. Gortázar, R. Tiwari, D.K. Bonilla-Aldana, A.J. Rodriguez-Morales, J. de la Fuente, I. Michalak, Y.A. Attia, SARS-CoV-2 in animals: potential for unknown reservoir hosts and public health implications, Vet. Q. 41 (n.d.) 181–201. doi: 10.1080/01652176.2021.1921311. [DOI] [PMC free article] [PubMed]
- 15.Hamer S.A., Pauvolid-Corrêa A., Zecca I.B., Davila E., Auckland L.D., Roundy C.M., Tang W., Torchetti M.K., Killian M.L., Jenkins-Moore M., Mozingo K., Akpalu Y., Ghai R.R., Spengler J.R., Barton Behravesh C., Fischer R.S.B., Hamer G.L. SARS-CoV-2 infections and viral isolations among serially tested cats and dogs in households with infected owners in Texas, USA. Viruses. 2021;13:938. doi: 10.3390/v13050938. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Bosco-Lauth A.M., Hartwig A.E., Porter S.M., Gordy P.W., Nehring M., Byas A.D., VandeWoude S., Ragan I.K., Maison R.M., Bowen R.A. Experimental infection of domestic dogs and cats with SARS-CoV-2: pathogenesis, transmission, and response to reexposure in cats. Proc. Natl. Acad. Sci. U. S. A. 2020;117:26382–26388. doi: 10.1073/pnas.2013102117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Perera R.A.P.M., Ko R., Tsang O.T.Y., Hui D.S.C., Kwan M.Y.M., Brackman C.J., To E.M.W., Yen H., Leung K., Cheng S.M.S., Chan K.H., Chan K.C.K., Li K.-C., Saif L., Barrs V.R., Wu J.T., Sit T.H.C., Poon L.L.M., Peiris M. Evaluation of a SARS-CoV-2 surrogate virus neutralization test for detection of antibody in human, canine, cat, and Hamster sera. J. Clin. Microbiol. 2021;59:e02504–e02520. doi: 10.1128/JCM.02504-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Tan C.W., Chia W.N., Qin X., Liu P., Chen M.I.-C., Tiu C., Hu Z., Chen V.C.-W., Young B.E., Sia W.R., Tan Y.-J., Foo R., Yi Y., Lye D.C., Anderson D.E., Wang L.-F. A SARS-CoV-2 surrogate virus neutralization test based on antibody-mediated blockage of ACE2-spike protein-protein interaction. Nat. Biotechnol. 2020;38:1073–1078. doi: 10.1038/s41587-020-0631-z. [DOI] [PubMed] [Google Scholar]
- 19.Udom K., Jairak W., Chamsai E., Charoenkul K., Boonyapisitsopa S., Bunpapong N., Techakriengkrai N., Amonsin A. Serological survey of antibodies against SARS-CoV-2 in dogs and cats, Thailand. Transbound. Emerg. Dis. 2021 doi: 10.1111/tbed.14208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Embregts C.W.E., Verstrepen B., Langermans J.A.M., Böszörményi K.P., Sikkema R.S., de Vries R.D., Hoffmann D., Wernike K., Smit L.A.M., Zhao S., Rockx B., Koopmans M.P.G., Haagmans B.L., Kuiken T., GeurtsvanKessel C.H. Evaluation of a multi-species SARS-CoV-2 surrogate virus neutralization test. One Health. 2021;100313 doi: 10.1016/j.onehlt.2021.100313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fritz M., Rosolen B., Krafft E., Becquart P., Elguero E., Vratskikh O., Denolly S., Boson B., Vanhomwegen J., Gouilh M.A., Kodjo A., Chirouze C., Rosolen S.G., Legros V., Leroy E.M. High prevalence of SARS-CoV-2 antibodies in pets from COVID-19+ households. One Health. 2021;11:100192. doi: 10.1016/j.onehlt.2020.100192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Hossain Md.G., Javed A., Akter S., Saha S. SARS-CoV-2 host diversity: An update of natural infections and experimental evidence. J. Microbiol. Immunol. Infect. 2021;54:175–181. doi: 10.1016/j.jmii.2020.06.006. [DOI] [PMC free article] [PubMed] [Google Scholar]