Abstract
Objectives
Health care workers are at an increased risk of SARS – CoV-2 transmission. The risk of infection for dental teams is assumed to be high, due to work settings, proximity to mouth, exposure to saliva and aerosols. There is a lack of evidence that quantifies the risk of SARS-CoV-2 transmission for dental patients and staff. Our objective was to assess SARS-CoV-2 transmission risk for dental staff members (DSMs) and patients following exposure in dental clinics during the second wave of the pandemic in Israel.
Methods
The study analyzed new positive SARS-CoV-2 cases following exposures in dental clinics from May to September 2020. Two data sources were used: case report forms (CRFs) and epidemiological investigations. CRFs were developed by the MoH and distributed to dental clinics to identify DSMs exposed to SARS-CoV-2 positive patients, and patients exposed to positive DSMs. SARS-CoV-2 status was diagnosed using MoH approved tests in certified laboratories and verified against the national COVID-19 database. Statistical analysis on a non-identified basis was performed. The population incidence and dental setting transmission rates were calculated for the study period with 95% Confidence Intervals.
Results
Following 962 reported exposures of DSMs to 508 SARS-CoV-2 positive patients, 7 DSMs were SARS – CoV-2 positive with a 0.7% cumulative transmission rate. Following 507 reported exposures by 43 SARS-CoV-2 positive DSMs, 3 patients were SARS – CoV-2 positive, with a 0.6% cumulative transmission rate. During the study period, the SARS-CoV-2 incidence rate in dental clinics was significantly lower when compared to the population.
Conclusions
The transmission rate of SARS-CoV-2 in dental settings was very low for both patients and DSMs.
Clinical significance
Our results suggest that routine dental care could be safely provided during the pandemic. Continuous monitoring should be performed due to the emergence of new variants and the vaccination programs.
Keywords: SARS-CoV-2, COVID-19, Pandemic, Transmission, Dental healthcare, Infection control
1. Introduction
From March 2020, SARS-CoV-2 disrupted oral health care worldwide. The sudden emergence and rapid spread of the virus posed a significant challenge to dental healthcare systems. The major challenge the dental community faced was the prevention of SARS-CoV-2 transmission in the dental setting. As widely described, there are several possible routes of SARS-CoV-2 transmission, including direct contact with infected persons, airborne (via aerosols) and fomite [1,2]. At the beginning of the pandemic, in an effort to reduce the transmission risk, professional organizations and governments worldwide issued emergency guidelines for dental practices to postpone all but urgent procedures. Tele-dentistry services were prioritized, and updated infection control guidelines, which stressed the importance of triage, use of water-resistant personal protective equipment (PPE), limiting aerosol-generating procedures and strict adherence to infection control protocols were issued.
Upon the cessation of lockdown in April 2020 in Israel, the MoH allowed the renewal of all dental treatment under SARS-CoV-2 precautions. With the onset of the second wave of COVID-19 in May 2020, DSMs were allowed to continue to deliver the full range of treatments under strict MoH infection control guidelines.
It was assumed that the risk of disease transmission for DSMs would be high due to the nature of dental procedures (exposure to saliva/ production of aerosols), the close proximity of DSMs to the patient's mouth and the possible cross-infection risk by asymptomatic/presymptomatic patients. Previous pandemics caused by other coronaviruses, have familiarized DSMs with the possible risks of transmission within dental settings [3,4]. It has been suggested that infection control measures including the widespread use of PPE by DSMs may in fact mitigate the risk of SARS-CoV-2 transmission [5].
The MoH SARS-CoV-2 guidelines for dental clinics stressed the importance of preliminary triage of patients and staff. Persons self-isolating, and those with respiratory symptoms or an elevated temperature, were required to stay home and seek dental advice using tele-dentistry tools. DSMs who had symptoms were required to stay home and refrain from practice.
Currently, only minimal published data exists to evaluate the transmission risk during dental treatment. Understanding this risk in the dental practice is important for both DSMs and patients, and is crucial for establishing public health policy regarding dental healthcare provision during the pandemic.
The aim of this study was to estimate the risk of SARS-CoV-2 transmission following exposure in the dental practice.
2. Independent ethics committee (IEC) approval
This study was approved by the Ethics (Helsinki) Committee of the Israeli Ministry of Health, approval number MOH-099-2020.
3. Materials and methods
A national cohort study to identify new positive cases following SARS-CoV-2 exposures in dental practices from May 1st to September 30th 2020 was conducted, prior to the initiation of the Israeli vaccine program. Two data sources were used: case report forms (CRFs) and epidemiological investigations. CRFs for SARS-CoV-2 exposures in dental practice were developed by the MoH, and distributed to Health Maintenance Organizations (HMOs), corporate and private dental clinics in May 2020.
CRFs were returned to, and analyzed by the MoH on a weekly basis. Data reported included information on exposures in dental clinics (date, location, positive patient/DSM national ID number and PPE use). Concurrent use of surgical mask, face shield/protective glasses and water-resistant gown during the entire treatment time was considered as “full PPE”. All other combinations were considered “partial PPE”.
All exposures and positive cases were followed up by the national contact tracing epidemiological program and cross-checked against the MoH national COVID-19 database.
Once data had been collected, prevention of personal identification was assured by coding, and statistical analysis on a non-identified basis was performed.
3.1. PCR SARS-Cov-2 tests
All tests were performed by MoH approved laboratories using one of two MoH approved PCR kits for SARS-CoV-2 testing: Seegen (Allplex™ 2019-nCoV) or BGI (Real-Time Fluorescent RT-PCR kit for detecting 2019-nCoV). Both kits have been in use since January 2020. The results were interpreted according to the manufacturer's instructions. In Israel, every positive or two consecutive borderline positive tests were considered as "true" positive. All PCR test results were reported and recorded on the national MoH COVID-19 database.
3.2. Index cases
Each index case was identified by epidemiological investigation as a source of exposure in the dental setting. This was defined as an individual (patient or DSM) who received or administered dental treatment and tested positive within 10 days post treatment. Positive results of patients or DSMs were reported retrospectively following exposure to positive individuals.
3.3. Epidemiological investigations
An epidemiological investigation was performed in each case of COVID-19 diagnosis and entailed a comprehensive interview with the positive patient/DSM, which included exposure details, places visited and individuals they were exposed to up to 10 days prior to the PCR SARS-CoV-2 positive test. Upon completion of the investigation, contacts of the positive patient/DSM were required to self-isolate according to MoH guidelines.
3.4. Study population
The number of patients treated in dental clinics during the study period was estimated by using quarterly reported data by the HMOs in 2020.
The estimated number of DSMs working during the study period was calculated based on the National Health Workforce Database [6].
A total of 1,871,356 patients were treated by 14,825 DSMs between May 1st and September 30th 2020 in dental clinics.
962 DSMs were exposed to 507 SARS-CoV-2 positive patients, and 508 patients to 43 SARS-CoV-2 positive DSMs, according to the reports received by the MoH during this period.
Community incidence rates of SARS-CoV-2 (per 100,000) were calculated in the total population on the first of each month, using the number of new cases reported in the WHO COVID-19 database [7], in order to estimate the infection level in the community during the study period. An identical calculation was performed for cases reported in the dental setting (dental patient and dental staff).
3.5. Data and Statistical analysis
Reports on exposures to positive cases (DSMs and dental patients) were recorded on one database. The data included the following details: national ID number of index and exposed individuals, date of exposure, exposure direction (positive patient or DSM), and PPE use. The analysis was separately performed for two groups: DSMs exposed to positive patients, and patients exposed to positive DSMs. The average number of days between the exposure during dental treatment and SARS-CoV-2 diagnosis was also calculated.
Monthly and cumulative exposure and transmission rates in dental settings (per 100,000) and 95% Confidence Intervals were calculated and compared to the population incidence rate.
Descriptive statistical analysis was performed using SAS version 9.4. Chi-square test results were calculated and a significance level of 5% was defined.
4. Results
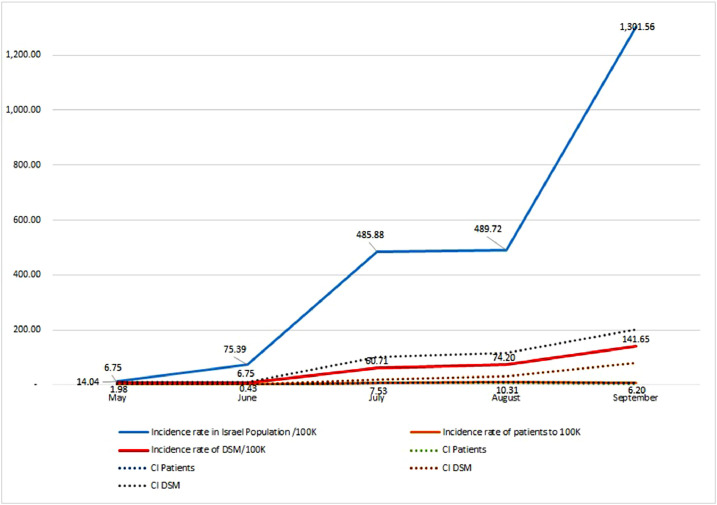
The SARS-CoV-2 incidence rate (per 100,000) in the population increased from 14.04 in May to 485.88 in July and to 1301.56 in September [7]. The incidence rate following exposures in dental clinics was low for both DSM and patient groups and increased from 6.75 and 1.98 in May to 141.65 and 6.20 in September respectively (Fig. 1 ).
Fig. 1.
SARS-CoV-2 Monthly incidence rate in dental clinics with 95% confidence interval compared to population incidence rate (per 100,000).
Between May – October 2020, 217,668 SARS-CoV-2 new cases were recorded in the population with a cumulative incidence rate of 2366.58 per 100,000 (95% CI 2356.64 – 2376.52) [8] while the cumulative incidence rate for DSMs was 290.05 (95% CI 203.36-376.74) and for dental patients 27.15 (95% CI 24.79-29.51).
There was virtually no difference in the cumulative transmission rate between DSMs and patients (Table 1 ). 962 DSMs provided dental treatment to 508 SARS-CoV-2 positive asymptomatic patients, resulting in an exposure ratio of 1.9:1. Of these, 7 (4 dentists and 3 assistants) were found to be infected post exposure in the dental settings (0.7% cumulative transmission rate over the study period). 507 patients were treated by 43 SARS-CoV-2 positive asymptomatic DSMs, resulting in an exposure ratio of 11.8:1. Of these, 3 patients were found to be infected with SARS-CoV-2 post exposure to a positive DSM (1 dentist and 2 assistants), with a 0.6% cumulative transmission rate over the study period. No other exposures were reported during epidemiological investigations for DSMs and patients positive post exposure.
Table 1.
Cumulative exposure and transmission rates in dental clinics from May 1st to September 30th 2020.
| Characteristics | Exposure to Positive DSM | Exposure to Positive Patient |
|---|---|---|
| Number of Exposures | 507 (0.03%)* | 962 (6.49 %)** |
| Number of SARS-CoV-2 Positive | 43 (0.29 %)** | 508 (0.03%)* |
| Exposure ratio- Average number exposed to one positive individual | 11.8:1 | 1.9:1 |
| Number infected following exposure | 3 Patients | 7 DSMs*** |
| Cumulative Transmission Rate over the study period**** | 0.6% | 0.7% |
| Ratio Rate (DSM to patient) | 1.23 (NS) |
*From estimated total number of Dental Patients.
**From estimated total number of DSMs.
*** 4 dentists and 3 dental team members.
**** From total number of exposures.
The average number of days between the exposure and SARS-CoV-2 diagnosis of the index case was 5.3 (SD = 5.9) with a median of 4 days.
Some of the positive individuals had minor non-specific symptoms only. No reports of hospitalizations were received for DSMs or patients. All DSMs/patients self-isolated, and were treated in the community.
All "index cases" were asymptomatic or with non-specific symptoms when they exposed other individuals. Positive results of patients or DSMs were reported retrospectively following exposure to positive individuals.
At the time of report, all positive individuals had minor symptoms or were asymptomatic, and all were treated in the community.
4.1. PPE use
Most DSMs reported full PPE use. A minor difference was found between the two DSM groups: positive DSMs and DSMs exposed to positive patients (Table 2 ).
Table 2.
Table 2: PPE use by DSMs
| Total n (%) | Positive DSMs (N=507 Exposures) | DSMs exposed to a positive patient (N=962 Exposures) | |
|---|---|---|---|
| Full PPE use | No | 38 (8.2%) | 144 (15%) |
| Yes | 425 (91.8%)* | 797 (85%)* | |
| Missing | 44 (8.7% from all) | 21 (2.1% from all) |
*Full PPE use positive DSM vs. DSM exposed to a positive patient, p<0.05.
5. Discussion
The SARS-CoV-2 pandemic has created a significant risk to all working in the healthcare field, with increased risk of infection in comparison to the general population [5]. Dental settings are often thought to be a possible portal for the dissemination of pathogens [9,10]. A limited number of studies have found SARS-CoV-2 transmission risk within dental clinics to be very low, but currently there is a sparcity of data regarding two way SARS-CoV-2 transmission between patients and DSMs during oral care delivery [11]. Despite strict adherence to infection control guidelines, e.g. patient screening and triage, SARS-CoV-2 poses a particular problem due to the possibility of virus spread via asymptomatic/presymptomatic individuals [12].
We sought to estimate the risk of SARS-CoV-2 transmission within the dental setting for both DSMs and patients in order to evaluate whether dental care could continue to be safely provided when adhering to pandemic specific infection control guidelines.
Asymptomatic/presymptomatic patients and DSMs infected by SARS-CoV-2 are potential sources of transmission in dental clinics. A recent study conducted in 2020 amongst 31 dental care centers in Scotland, found that the positivity rate among asymptomatic screened dental patients was in proportion to community prevalence and reflected the underlying prevalence at that time [13].
Similar to this, we found in our study that the exposure rate to asymptomatic/presymptomatic SARS-CoV-2 positive patients in dental clinics from May to October 2020 rose with the increase of infection level in the population [13].
Our study found a very low virus transmission by asymptomatic/presymptomatic SARS-CoV-2 positive patients and DSMs in the dental setting. Although causality could not be absolutely determined, as there are other potential and possibly unknown ways of infection outside the dental setting, the high efficiency of the national epidemiological investigation system should be taken into consideration. The epidemiological investigations were conducted in each positive case and made great effort to obtain a reasonable hypothesis as to the most probable transmission source. The average and median number of days from the exposure to the diagnosis, supported the biological plausibility with regards to index cases in our study [14].
It should be noted that an almost identical risk of COVID-19 infection for dental care providers and dental patients stemmed from a different exposure rate. While on average 1.9 DSMs were exposed to one positive patient, one positive DSM exposed 11.9 patients. However, the transmission risk following the exposure was very low for both groups and lower than the underlying incidence rate in the population during the study period. Considering the possibility that some of the cases may have occurred outside the dental setting, the risk may actually be even lower than that found in our study.
It could be suggested that the compliance with infection control guidelines may have markedly reduced the transmission risk in dental settings as shown in a recent study conducted amongst health care workers, which found that adherence to infection control guidelines including PPE use may have contributed to a reduced risk of transmission during health care delivery [15].
Our findings regarding the high use of PPE, are similar to other studies conducted amongst other medical team members [16]. Some of the DSMs reported incomplete use of full PPE for the entire treatment length which might be explained by the adaptation difficulties to certain components of PPE and by the relative discomfort and visibility related issues with regards to eye protection [16]. The findings also showed higher use of full PPE by positive DSMs, but the reporting bias, such as recall bias, cannot be excluded here.
Nevertheless, regarding the number of exposures, it was reasonable to assume that reporting bias was minimal, as the exposure reports to SARS-CoV-2 positive individuals were sent to the MoH weekly on an ongoing basis, and the exposure rate observed in dental settings reflected the underlying level of infection in the country during the study period. The data received was validated against the national MoH COVID-19 database (PCR test results in authorized laboratories). The official diagnosis dates of positive individuals were obtained from the database to ascertain biological plausibility of transmission.
Understanding transmission in dental settings is imperative for health-care systems in order to develop proper strategies to protect both patients and DSMs, and to maintain oral care provision for the population. During the current SARS-CoV-2 pandemic, DSMs were assumed to be at an increased risk of both becoming infected by and of transmitting SARS-CoV-2. Our study results showed that exposures in dental clinics occurred, yet we found minimal evidence of post exposure transmission; incidence rate and the percentage of positive cases of COVID-19 in the country during the study period were significantly higher when compared to those in dental settings. It should be noted that the calculations were based on a very small number, and so conclusions should be drawn carefully. However, we assume that considering the robust epidemiological investigation system operating in the country during the pandemic, the chance of missing information regarding positive COVID-19 cases in dental clinics is low.
The study period included the second wave of SARS-CoV-2 in Israel, prior to the identification of new variants of SARS-CoV-2 in the population and prior to the implementation of the national vaccination program.
6. Conclusion
The risk of SARS-CoV-2 transmission within the dental setting was low, and the adherence to national infection control guidelines was high. Elective dental care was safely delivered during the pandemic.
Nevertheless, continuous monitoring of exposures and transmissions should be performed due to the ever-changing epidemiological situation as new variants emerge. The vaccination program may further mitigate the transmission risk.
Future research should include the assessment of new strategies to additionally reduce and possibly eliminate the transmission of SARS-CoV-2 in the dental setting.
Authors' contributions
Lena Natapov: Conceptualization, Methodology, Writing – Original and Final draft. Dara Schwartz, Dan Dekel Markovich, Hagit Domb Herman, David Yellon, Mutaz Jarallah, Yehuda Carmeli: Methodology, Writing-Reviewing and Editing. Isabella Karakis, Irina Lipshiz, Mutaz Jarallah: Formal analysis. Dara Schwartz, Dan Dekel Markovich, Hagit Domb Herman, David Yellon, Isabella Karakis: Writing, Reviewing, Editing – Original and Final draft. Lena Natapov, Dara Schwartz, Dan Dekel Markovich, Hagit Domb Herman, David Yellon, Mutaz Jarallah Writing-Reviewing and Editing.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Footnotes
The authors have no conflicts of interest associated with this publication, and there has been no financial support for this work that could have influenced its outcome.
References
- 1.“Scientific Brief: SARS-CoV-2 and Potential Airborne Transmission | CDC.” https://www.cdc.gov/coronavirus/2019-ncov/more/scientific-brief-sars-cov-2.html (accessed Feb. 16, 2021).
- 2.“Modes of transmission of virus causing COVID-19: implications for IPC precaution recommendations.” https://www.who.int/news-room/commentaries/detail/modes-of-transmission-of-virus-causing-covid-19-implications-for-ipc-precaution-recommendations (accessed Feb. 16, 2021).
- 3.Al-Sehaibany F.S. Middle East respiratory syndrome in children: dental considerations. Saudi Med. J. Apr. 01, 2017;38(4):339–343. doi: 10.15537/smj.2017.4.15777. Saudi Arabian Armed Forces Hospital. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Samaranayake L.P., Peiris M. Severe acute respiratory syndrome and dentistry: a retrospective view. J. Am. Dent. Assoc. 2004;135(9):1292–1302. doi: 10.14219/jada.archive.2004.0405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Nguyen L.H., et al. Risk of COVID-19 among frontline healthcare workers and the general community: a prospective cohort study. medRxiv. medRxiv. May 25, 2020 doi: 10.1101/2020.04.29.20084111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6."Healthcare Professions Manpower Israel 2019". https://www.health.gov.il/PublicationsFiles/manpower2019.pdf (accessed Apr. 04, 2021).
- 7.“WHO Coronavirus (COVID-19) Dashboard | WHO Coronavirus (COVID-19) Dashboard With Vaccination Data.” https://covid19.who.int/(accessed Apr. 04, 2021).
- 8.“Coronavirus (COVID-19) Testing - Statistics and Research - Our World in Data.” https://ourworldindata.org/coronavirus-testing (accessed Apr. 04, 2021).
- 9.“Epidemiologic Notes and Reports Update: Transmission of HIV Infection During Invasive Dental Procedures — Florida.” https://www.cdc.gov/mmwr/preview/mmwrhtml/00014428.htm (accessed Feb. 16, 2021).
- 10.Merte J.L., Kroll C.M., Collins A.S., Melnick A.L. An epidemiologic investigation of occupational transmission of Mycobacterium tuberculosis infection to dental health care personnel : infection prevention and control implications. J. Am. Dent. Assoc. 2014;145(5):464–471. doi: 10.14219/jada.2013.52. [DOI] [PubMed] [Google Scholar]
- 11.Gallagher J.E., Johnson I., Verbeek J.H., Clarkson J.E., Innes N. Relevance and paucity of evidence: a dental perspective on personal protective equipment during the COVID-19 pandemic. Br. Dent. J. Jul. 2020;229(2):121–124. doi: 10.1038/s41415-020-1843-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ferretti L., et al. Quantifying SARS-CoV-2 transmission suggests epidemic control with digital contact tracing. Science. May 2020;368(80):6491. doi: 10.1126/science.abb6936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Conway D.I., et al. SARS-CoV-2 positivity in asymptomatic-screened dental patients. J. Dent. Res. Mar. 2021 doi: 10.1177/00220345211004849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.He X., et al. Author correction: temporal dynamics in viral shedding and transmissibility of COVID-19 (Nature Medicine, (2020), 26, 5, (672-675), 10.1038/s41591-020-0869-5) Nat. Med. 2020;26(9):1491–1493. doi: 10.1038/s41591-020-1016-z. Nature ResearchSep. 01doi: 10.1038/s41591-020-1016-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ren Y., Feng C., Rasubala L., Malmstrom H., Eliav E. Risk for dental healthcare professionals during the COVID-19 global pandemic: an evidence-based assessment. J. Dent. Oct. 2020;101 doi: 10.1016/j.jdent.2020.103434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Prakash G., et al. Compliance and perception about personal protective equipment among health care workers involved in the surgery of COVID-19 negative cancer patients during the pandemic. J. Surg. Oncol. Nov. 2020;122(6):1013–1019. doi: 10.1002/jso.26151. [DOI] [PMC free article] [PubMed] [Google Scholar]