Abstract
Objective
To systematically appraise the available evidence to determine the accuracy of decision aids for emergency medical services (EMS) telephone triage of patients with chest pain suspected to be caused by acute coronary syndrome (ACS) or life-threatening conditions.
Design
Systematic review.
Data sources
Electronic searches were performed in Embase 1974, Medline 1946 and CINAHL 1937 databases from 3 March 2020 to 4 March 2020.
Eligibility criteria
The review included all types of original studies that included adult patients (>18 years) who called EMS with a primary complaint of chest pain and evaluated dispatch triage priority by telephone. Outcomes of interest were a final diagnosis of ACS, acute myocardial infarction or other life-threatening conditions.
Data extraction and synthesis
Two authors independently extracted data on study design, population, study period, outcome and all data for assessment of accuracy, including cross-tabulation of triage priority against the outcomes of interest. Risk of bias was assessed using the Quality Assessment of Diagnostic Accuracy Studies 2 assessment tool.
Results
Searches identified 553 papers, of which 3 were eligible for inclusion. Those reports described the evaluation of three different prediction models with variation in the variables used to detect ACS. The overall results showed that dispatch triage tools have good sensitivity to detect ACS and life-threatening conditions, even though they are used to triage signs and symptoms rather than diagnosing the patients. On the other hand, prediction models were built to detect ACS and life-threatening conditions, and therefore, prediction models showed better sensitivity and negative predictive value than dispatch triage tools.
Conclusion
We have identified three prediction models for telephone triage of patients with chest pain. While they have been found to have greater accuracy than standard EMS dispatch systems, prospective external validation is essential before clinical use is considered.
PROSPERO registration number
This systematic review was pre-registered on the International prospective register of systematic reviews (PROSPERO) database (reference CRD42020171184).
Keywords: myocardial infarction, coronary heart disease, accident & emergency medicine
Strengths and limitations of this study.
To our knowledge, this is the first systematic review looking into the accuracy of prehospital chest pain telephone triage.
It is possible that some relevant papers were missed because researchers only included studies that have adult participants who are >18 years old and excluded papers not published in English language.
Unfortunately, because of the paucity of data for each decision aid, the data were not suitable for meta-analysis.
Also, there was a difference in the definition of life-threatening conditions definition between included studies.
Background
Chest pain, which is one of the main symptoms of acute coronary syndromes (ACS), is one of the most common reasons for ambulance call-outs and presentations to emergency departments (EDs).1 2 However, most patients with chest pain who are transported by ambulance are ultimately diagnosed with self-limiting, non-cardiac disease. Thus, patients with chest pain tend to be systematically overtriaged, increasing ambulance resource utilisation and contributing to ED crowding.2 3
Two emergency medical services (EMS) dispatch systems are currently used in the UK: the Advanced Medical Prioritising Dispatching System (AMPDS) and the National Health Service (999) System.4 Both systems use computerised telephone triage software that identify life-threatening conditions by a series of questions at the beginning of the call. For patients with a primary complaint of chest pain, they also include a specific series of questions to identify ACS and triage the case using the patient’s sign and symptoms.3 5 However, systematic reviews have shown that there is only a low level of evidence to support the use of current triage systems.6 7 There are also insufficient data on the dispatch protocol efficiency.7 8 There is no consensus on the definitions used in Criteria-Based Dispatch, which is the programme used to triage patients by signs and symptoms, and AMPDS.9 10 Also, there is no consensus on the accepted level for overtriage or undertriage for medical emergency dispatch.6 9 Therefore, systematic overtriage for patients with chest pain is used by dispatch systems to avoid potential harm to patients. EMS resource utilisation is increased as a result,6 and there are important differences between patients’ clinical findings when examined and dispatch priority.8 9 Therefore, with the current clinical guidelines for EMS, it is hard to rule in or rule out ACS by telephone triage.11
We aimed systematically to appraise the available evidence to determine the accuracy of decision aids that have been used for EMS telephone triage of patients with chest pain suspected to be caused by ACS or life-threatening conditions.
Methods
The systematic review was conducted in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and following Cochrane methodology for diagnostic test accuracy reviews.12 A completed PRISMA checklist is provided in online supplemental appendix 1.
bmjopen-2020-045815supp001.pdf (49.4KB, pdf)
Search strategy and eligibility criteria
We searched the Embase 1974, Medline 1946 and CINAHL 1937 databases from 3 March 2020 to 4 March 2020 for the terms ‘chest pain, telephone or dispatch, triage, ACS or AMI, life-threatening conditions, and EMS or prehospital’. Retrospective and prospective cohort studies written in English were eligible. Search strategy table is provided in online supplemental appendix 2.
bmjopen-2020-045815supp002.pdf (36.7KB, pdf)
Studies included
Based on the inclusion criteria, titles and abstracts were independently screened and shortlisted by two reviewers (AAlg and CR). The inclusion criteria were: (1) the study included adult patients (>18 years); (2) the study included patients with a primary complaint of chest pain who called EMS for an ambulance; (3) the studies evaluated dispatch triage priority; (4) the study provided data for a linked final diagnosis of ACS, acute myocardial infarction (AMI) or other life-threatening conditions. Two reviewers independently reviewed and screened potentially relevant full-text papers to identify those fulfilling the inclusion criteria. Any discrepancies between the reviewers were resolved by a third reviewer (AAlo).
Outcome measures
The primary outcome was a diagnosis of ACS on hospital admission, including ST elevation myocardial infarction (STEMI), non-STEMI (NSTEMI) and unstable angina. AMI (incorporating both STEMI and NSTEMI) is defined according to the universal definition of AMI.13 Unstable angina is defined as sudden prolonged chest pain at rest >20 min, new-onset severe angina or previous angina that is increasing in severity of pain, duration of pain and/or frequency.14
The secondary outcome was the diagnosis of a life-threatening condition associated with chest pain. Since there is no universal definition for life-threatening conditions associated with chest pain, we included all relevant data from the studies, regardless of the precise definition used for ‘life-threatening conditions’.
Methodological quality assessment
The quality assessment of eligible articles was independently assessed by two reviewers (AAlo and AAlg), using a modified Quality Assessment of Diagnostic Accuracy Studies 2 (QUADAS-2) tool to suit the purpose of this systematic review.15 Discrepancies between reviewers were solved by discussion.
Data extraction
After selecting the eligible studies, two investigators (AAlo and AAlg) used a standardised data extraction form to extract and collect data as study design, population, study period and outcome. Also, both investigators extracted all data required for diagnostic accuracy assessment including 2×2 tables when available for dispatch priority and prediction models priority for suspected ACS or life-threatening conditions.
Statistical analysis
In line with our protocol, we considered pooling sensitivities, specificities, negative and positive predictive values (NPV and PPV, respectively) by meta-analysis. However, after reviewing the final list of studies meeting inclusion criteria, the reviewers unanimously concluded that meta-analysis would have been inappropriate due to clear evidence of clinical heterogeneity between studies and missing data. We, therefore, undertook a narrative synthesis of the existing evidence.
Results
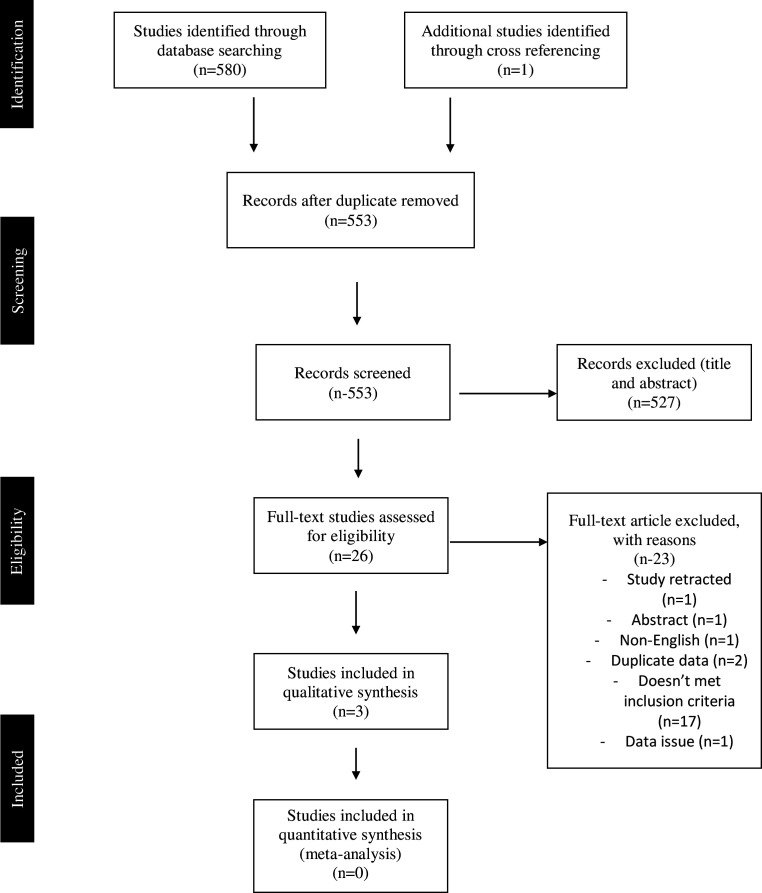
In total, our literature search identified 553 potentially relevant articles of which 26 were considered potentially eligible for inclusion after screening titles and abstracts. Following independent full-text review, 23 articles were excluded and 3 articles met the inclusion criteria for this review (figure 1). Excluded studies with reasons for exclusion are shown in online supplemental appendix 3.16–18
Figure 1.
Flow diagram of study selection.
bmjopen-2020-045815supp003.pdf (79KB, pdf)
Study characteristics and quality assessments
General study characteristics are summarised in table 1. Patient characteristics and study weaknesses are summarised in table 2. The number of patients in each study with each component of the outcome measures studied is summarised in online supplemental appendix 4. The details of the prediction models identified, together with the test characteristics (including sensitivity, specificity, NPV and PPV) for the diagnosis of ACS and life-threatening conditions, are shown in tables 3 and 4.
Table 1.
Characteristics of included studies
| Study ID | Year | Country | Study design | Sites | Study period |
| Gellerstedt et al16 | 2006 | Sweden | Prospective cohort study | 1 | 3 months |
| Reuter et al18 | 2019 | France | Follow-up prospective cohort study | 1 | 18 months, May 2010–November 2011 |
| Gellerstedt et al17 | 2016 | Sweden | Retrospective cohort study | 1 | 7 months, 1 May 2009–28 February 2010 |
Table 2.
Study and patient characteristics of all studies included in the systematic review
| Study ID | N | Population | Triage criteria | Exclusion criteria | Target condition | Study weaknesses |
| Gellerstedt et al16 | 503 | Patients who called for an ambulance and who were assessed by the dispatcher as having chest pain | Dispatcher judgement versus prediction model (derived in this cohort) | NA | AMI, life-threatening conditions | Retrospective, no sample size calculation, small simple size, out of date AMI reference standard (based on creatine kinase-MB rather than cardiac troponin) |
| Reuter et al18 | 3727 | Patients who called for an ambulance complaining of chest pain | Prediction model | Difficult communication, language barrier inability to speak with patient | ACS | Information bias, unclear how AMI was adjudicated |
| Gellerstedt et al17 | 1942 | Patients who called 112 for an emergency ambulance with a complaint of chest pain | Dispatcher judgement versus prediction model | Lost diagnosis or follow-up. | ACS, life-threatening conditions | 95% CIs for test characteristics were not presented. Only internal validation completed, and the full results of that validation were not presented |
ACS, acute coronary syndrome; AMI, acute myocardial infraction; NA, not available.
Table 3.
Diagnostic accuracy of dispatch tools and prediction models for ACS
| Study ID | N | Triage criteria | Sensitivity % | Specificity % | NPV % | PPV % | TP | FP | FN | TN |
| Gellerstedt et al16 | 503 | Dispatch system (standard care) | 85.7% | 26.9% | 87.7 | 32.02 | 90 | 291 | 15 | 107 |
| 503 | Prediction model | 92.4% | 28.6% | 93.4 | 25.5 | 97 | 284 | 8 | 114 | |
| Reuter et al18 | 2363 | Male prediction model | NA | NA | NA | NA | NA | NA | NA | NA |
| 1824 | Female prediction model | NA | NA | NA | NA | NA | NA | NA | NA | |
| Gellerstedt et al17 | 1942 | Dispatch system | 82.6 | 39.9 | 94.3 | 15.9 | 194 | 1026 | 41 | 681 |
| Full prediction model | 90.2 | 40.9 | 96.8 | 17.4 | 212 | 1008 | 23 | 699 | ||
| Limited prediction model | 91.1 | 41.1 | 96.96 | 17.5 | 214 | 1006 | 22 | 701 |
ACS, acute coronary syndrome; FN, false negative; FP, false positive; NA, not available; NPV, negative predictive value; PPV, positive predictive value; TN, true negative; TP, true positive.
Table 4.
Diagnostic accuracy of dispatch tools and prediction models for life-threatening conditions
| Study ID | N | Triage criteria | Sensitivity % | Specificity % | NPV % | PPV % | TP | FP | FN | TN |
| Gellerstedt et al16 | 493 | Dispatch system | 80.9 | 37.5 | 64.1 | 47.3 | 178 | 198 | 42 | 75 |
| 493 | Prediction model | 86.4 | 31.8 | 74.4 | 50.5 | 190 | 186 | 30 | 87 | |
| Gellerstedt et al17 | 1944 | Dispatch system | 76.5 | 39.8 | 89.9 | 19.5 | 238 | 983 | 73 | 650 |
| 1944 | Full prediction model | 88.4 | 42.1 | 95 | 22.5 | 275 | 946 | 36 | 687 | |
| 1944 | Limited prediction model | 88.7 | 42.1 | 95.1 | 22.6 | 276 | 945 | 35 | 688 |
FN, false negative; FP, false positive; NPV, negative predictive value; PPV, positive predictive value; TN, true negative; TP, true positive.
bmjopen-2020-045815supp004.pdf (54.1KB, pdf)
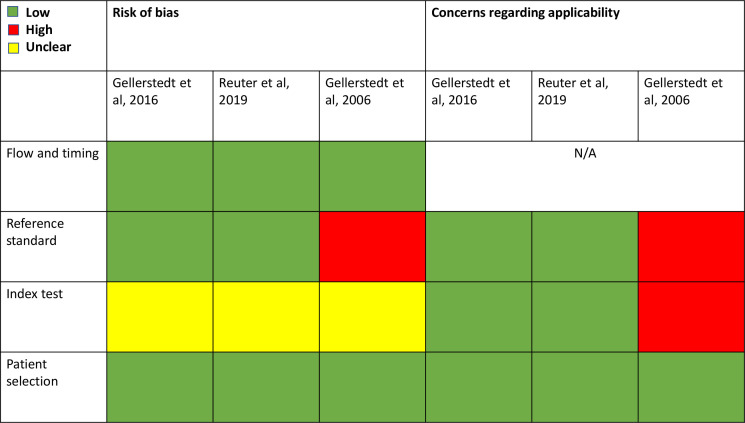
The modified QUADAS-2 methodological quality assessment tool was used to assess all eligible studies as shown in online supplemental appendix 5. A summary of the quality assessment for each eligible study is shown in figure 2. Two out of the three studies were retrospective cohort studies and compared the dispatch triage for ambulance response priority to the prediction model16 17 and one was prospective cohort study that only testing prediction model accuracy.18 ACS was adjudicated by experts in only one study18 while the other two studies used the hospital final diagnosis of ACS, AMI or life-threatening conditions. All eligible studies used the appropriate ACS or AMI definitions at the time of conducting the study.
Figure 2.
Quality Assessment of Diagnostic Accuracy Studies 2QUADAS-2 assessment of eligible studies. N/A, not available.
bmjopen-2020-045815supp005.pdf (76KB, pdf)
Summary of the existing evidence
Gellerstedt et al16 derived a prediction model to detect AMI and life-threatening conditions patients calling for an emergency ambulance with chest pain. They aimed to effectively triage calls to determine the appropriate level of response (capable of providing advanced life support vs only basic life support). The final model used eight variables (age, gender, strong pain, dyspnoea, cold sweat, nausea, vertigo and syncope) to calculate the probability of AMI or a life-threatening condition. Setting an arbitrary cut-off, the authors found that the model had greater sensitivity than and similar specificity to the judgement of the call handlers, which could potentially improve triage. However, performance of the model was only evaluated in the derivation set, with no validation presented.
In 2016, the same group derived a new prediction model in another study. They aimed to determine whether a computer-based decision support system could have superior accuracy for identifying life-threating conditions or ACS in patients who called for an emergency ambulance with chest pain. Gellerstedt et al17 collected data from patients who called 112 having chest pain using 10 questions related to ACS with yes or no answers. They derived two prediction models based on those answers. The first prediction model (full model) incorporated data from all 10 questions that dispatchers had asked, including: age, gender, central chest pain, high intensity pain, pain duration between 15 min and 24 hours, aggravated pain when breathing or moving, abnormal breathing, cold sweat, diabetes or previous cardiovascular disease, previous ACS and belief that symptoms are heart related. The authors also derived a ‘limited model’, which only included variables that had a significant association with the presence of ACS or a life-threatening condition on bivariate analysis. These included gender, age, central chest pain, high intensity pain, previous ACS and a high priority based on dispatcher judgement. There was no significant difference in performance between the full model and limited model. However, both the limited and full models had superior sensitivity to the priority assigned by dispatchers in practice, both for ACS (table 3) and life-threatening conditions (table 4), with similar specificity.17 The model was derived in 70% of the available cohort and validated in the remaining 30%. The authors state that performance was ‘similar’ in the validation set, although no further details were provided.
Reuter et al18 used backward logistic regression to derive two separate prediction models to detect ACS among men and women, respectively. The male prediction model to detect ACS consisted of eight variables, which are: age, smoking, severe pain, permanent pain, breathing non-related pain, retrosternal pain, radiating pain and additional symptoms. The female prediction model to detect ACS consisted of four variables, which are: age >60 years, history of coronary artery disease, breathing non-related pain and radiating pain.
The male prediction model had an area under the curve (AUC) of 0.76 (95% CI 0.73 to 0.79) in the derivation set (70% of the sample, which was randomly selected), which was maintained at 0.76 (95% CI 0.73 to 0.80) in the internal validation set (30% of the cohort). However, while the female prediction model had a similar AUC in the derivation set (0.79, 95% CI 0.75 to 0.83), it had lower accuracy in the validation set (AUC 0.67, 95% CI 0.60 to 0.74). No data were presented to enable calculation of sensitivity, specificity, PPV or NPV, and the output of the model was not compared with standard care or clinical judgement.
Discussion
In this systematic review, we have identified three studies that presented the derivation of clinical prediction models to enhance the telephone triage of patients calling for an emergency ambulance with chest pain. None of the models presented had sufficiently high sensitivity to avoid the need for ambulance dispatch. While two of the prediction models were shown to have greater accuracy than standard dispatch systems, unfortunately the current evidence does not support the use of these prediction models in practice without further validation. However, the evidence to date does suggest that clinical prediction models for this use case could feasibly improve on the accuracy of triage offered by standard EMS dispatch systems.
The original model derived by Gellerstedt et al used a now outdated definition of AMI (using creatine kinase-MB as the reference standard biomarker), meaning that the results could not be applied to modern clinical practice without further validation. The second model derived by Gellerstedt et al underwent internal validation, but full details of validation were not published. Finally, Reuter et al18 derived two prediction models (for men and women, respectively) but did not present sufficient data to compare their performance to standard care. The AUC for the male prediction model was 0.76, showing good overall accuracy. The prediction model for females had a poor AUC (0.67) on internal validation. We identified no prediction models that have undergone external validation.
It is an extremely challenging task for dispatchers to identify ACS over the telephone as there are so many different causes of chest pain,11 19 20 and there is very limited information available at the time of the initial phone call. It has previously been reported that only 1 out of 18 patients who request an ambulance for a complaint of chest pain has ACS.3 While a validated prediction model would have clear benefits, this systematic review has identified no validated tools that could be used in current practice.
It has also been reported that the AMPDS triage system is not an accurate tool for identifying ACS.3 Moreover, in Denmark, Criteria-based Danish index is used to triage emergency calls and it resulted in overtriage for 51% of chest pain calls as they were discharged without a specific diagnosis and AMI was only found in 11% of patients.2 Dispatch triage systems were constructed to prioritise the prehospital response based on a patient’s condition. They were not intended to make diagnoses. Therefore, it is important to highlight that the use of prediction models for telephone triage may not be expected to ‘rule out’ ACS but to identify patients who may safely receive a lower priority response, while correctly identifying the vast majority of those who require an urgent response.
It is clear that chest pain is a main symptom of ACS.2 11 19 21–23 However, previous studies have shown that some patients with ACS have been given lower priority during triage due to not having chest pain.3 24 Deakin et al found that 13% of patients who called for an ambulance with confirmed ACS presented with no chest pain A study was conducted in Australia by Coventry et al25 to identify the sex differences in symptoms related to MI reported to EMS dispatch agrees with Deakin et al3 and our findings that chest pain alone is not a solid predictor of MI. Among female patients who called for an ambulance and were finally diagnosed with MI only 54.4% presented with chest pain, while among male patients 68.7% had chest pain. As a result, priority 1 allocation for women was 67% and for men 81%.25 Also, several studies have identified differences of symptoms reported by patients with ACS. Interestingly, as we found in this systematic review, symptoms of ACS differ between male and female patients.18 19 25 One of the studies included in the search developed two different prediction models for men and women. However, the female prediction model failed to stand up to internal validation and should not be implemented.18 The most common symptom with MI following chest pain is shortness of breath (SOB), which appeared in 28.3% women vs 25.8% men. In patients presenting with no chest pain, SOB was the most common symptom, occurring in 38% women vs 32% men. These findings agree with what we have found as two studies that nausea, SOB and cold sweat were the most common symptoms reported after chest pain.16 17 Women with ACS are less likely to present with chest pain when compared with men. This may explain the relative underperformance of the female prediction model derived by Reuter et al.18
Future research
This systematic review has highlighted two potential areas for future research. First, the three prediction models identified may add value over existing telephone triage algorithms but this would require prospective external validation. Second, the existing evidence suggests that it is feasible to derive a prediction model to enhance telephone triage for patients with suspected ACS. The derivation and validation of a new, contemporary prediction model could reduce the systematic overtriage of patients in future, while ensuring that those with life-threatening conditions consistently receive an urgent response. However, given the risks of delayed responses (eg, ‘time is muscle for patients with STEMI), a higher sensitivity than has been observed in the studies identified is likely to be required.
Patient and public involvement
No patient involved.
Limitations
It is possible that some relevant papers were missed because we only included studies that have adult participants who are >18 years old and we excluded papers not published in English language. Unfortunately, we could not conduct a meta-analysis as there were variations between dispatch system tools and priority types. Also, there was a difference in the definition of life-threatening conditions between included studies.
Conclusion
We have identified three clinical prediction models for telephone triage of patients with chest pain. While the models have been found to have greater accuracy than standard EMS dispatch systems, the level of evidence to support their use is currently low. Prospective external validation is, therefore, required. However, our findings do support the feasibility of deriving and validating clinical prediction models to reduce overtriage while ensuring urgent responses for those who need them most.
Supplementary Material
Footnotes
Twitter: @do7mi, @Reynard_EM
Contributors: AAlo: writing protocol, data search, data extraction, quality assessment and writing. AAlg: data search, data extraction, quality assessment. CR: data search, data extraction, quality assessment. RB: protocol planning, writing, proofreading.
Funding: The publication fee has been funded by the Division of Cardiovascular Sciences, University of Manchester, UK. No grant or award number.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
Data are available in a public, open access repository. All the data included were obtained from published articles.
Ethics statements
Patient consent for publication
Not required.
Ethics approval
Ethical approval is not required for this systematic review.
References
- 1.Ezekowitz JA, Welsh RC, Weiss D, et al. Providing rapid out of hospital acute cardiovascular treatment 4 (PROACT‐4). J Am Heart Assoc 2015;4. 10.1161/JAHA.115.002859 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pedersen CK, Stengaard C, Friesgaard K, et al. Chest pain in the ambulance; prevalence, causes and outcome - a retrospective cohort study. Scand J Trauma Resusc Emerg Med 2019;27:84. 10.1186/s13049-019-0659-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Deakin CD, Sherwood DM, Smith A, et al. Does telephone triage of emergency (999) calls using advanced medical priority dispatch (AMPDS) with department of health (DH) call prioritisation effectively identify patients with an acute coronary syndrome? an audit of 42,657 emergency calls to Hampshire ambulance service NHS trust. Emerg Med J 2006;23:232–5. 10.1136/emj.2004.022962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Durham M, Faulkner M, Deakin C. Targeted response? an exploration of why ambulance services find government targets particularly challenging. Br Med Bull 2016;120:35–42. 10.1093/bmb/ldw047 [DOI] [PubMed] [Google Scholar]
- 5.Turner J, Jon Nicholl JN, Jon Nicholl JN, et al. Final report. Ambulance response programme, 2017. Available: https://www.england.nhs.uk/wp-content/uploads/2017/07/ARPReport_Final.pdf
- 6.Bohm K, Kurland L. The accuracy of medical dispatch - a systematic review. Scand J Trauma Resusc Emerg Med 2018;26:94. 10.1186/s13049-018-0528-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lidal IB, Holte HH, Vist GE. Triage systems for pre-hospital emergency medical services - a systematic review. Scand J Trauma Resusc Emerg Med 2013;21:28. 10.1186/1757-7241-21-28 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hoikka M, Länkimäki S, Silfvast T, et al. Medical priority dispatch codes-comparison with national early warning score. Scand J Trauma Resusc Emerg Med 2016;24:142. 10.1186/s13049-016-0336-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dami F, Golay C, Pasquier M, et al. Prehospital triage accuracy in a criteria based dispatch centre. BMC Emerg Med 2015;15:32. 10.1186/s12873-015-0058-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Torlén K, Kurland L, Castrén M, et al. A comparison of two emergency medical dispatch protocols with respect to accuracy. Scand J Trauma Resusc Emerg Med 2017;25:122. 10.1186/s13049-017-0464-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Colbeck M. Paramedic diagnosis of acute coronary syndrome in the out-of-hospital patient with acute, non-traumatic chest pain. Australas J Paramedicine 2016;13. 10.33151/ajp.13.4.523 [DOI] [Google Scholar]
- 12.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009;62:1006–12. 10.1016/j.jclinepi.2009.06.005 [DOI] [PubMed] [Google Scholar]
- 13.Thygesen K, Alpert JS, Jaffe AS, et al. Fourth universal definition of myocardial infarction (2018). Eur Heart J 2019;40:237–69. 10.1093/eurheartj/ehy462 [DOI] [PubMed] [Google Scholar]
- 14.Yusuf SW. Unstable angina. BMJ Best Practice 2018. [Google Scholar]
- 15.Whiting PF, Rutjes AWS, Westwood ME, et al. QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 2011;155:529–36. 10.7326/0003-4819-155-8-201110180-00009 [DOI] [PubMed] [Google Scholar]
- 16.Gellerstedt M, Bång A, Herlitz J. Could a computer-based system including a prevalence function support emergency medical systems and improve the allocation of life support level? Eur J Emerg Med 2006;13:290–4. 10.1097/00063110-200610000-00009 [DOI] [PubMed] [Google Scholar]
- 17.Gellerstedt M, Rawshani N, Herlitz J, et al. Could prioritisation by emergency medicine dispatchers be improved by using computer-based decision support? a cohort of patients with chest pain. Int J Cardiol 2016;220:734–8. 10.1016/j.ijcard.2016.06.281 [DOI] [PubMed] [Google Scholar]
- 18.Reuter P-G, Pradeau C, Huo Yung Kai S, et al. Predicting acute coronary syndrome in males and females with chest pain who call an emergency medical communication centre. Scand J Trauma Resusc Emerg Med 2019;27:92. 10.1186/s13049-019-0670-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Wouters LT, Zwart DL, Erkelens DC, et al. Chest discomfort at night and risk of acute coronary syndrome: cross-sectional study of telephone conversations. Fam Pract 2020;37:473–8. 10.1093/fampra/cmaa005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kelly A-M. The famous triage trial: pre-hospital chest pain research challenging the paradigm. Emerg Med Australas 2018;30:594. 10.1111/1742-6723.13116 [DOI] [PubMed] [Google Scholar]
- 21.Alghamdi A, Howard L, Reynard C, et al. Enhanced triage for patients with suspected cardiac chest pain: the history and Electrocardiogram-only Manchester acute coronary syndromes decision aid. Eur J Emerg Med 2019;26:356–61. 10.1097/MEJ.0000000000000575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sax DR, Vinson DR, Yamin CK, et al. Tele-Triage outcomes for patients with chest pain: comparing physicians and registered nurses. Health Aff 2018;37:1997–2004. 10.1377/hlthaff.2018.05079 [DOI] [PubMed] [Google Scholar]
- 23.Svensson L, Isaksson L, Axelsson C, et al. Predictors of myocardial damage prior to hospital admission among patients with acute chest pain or other symptoms raising a suspicion of acute coronary syndrome. Coron Artery Dis 2003;14:225–31. 10.1097/01.mca.0000063503.13456.0d [DOI] [PubMed] [Google Scholar]
- 24.Herlitz J, Starke M, Hansson E, et al. Early identification of patients with an acute coronary syndrome as assessed by dispatchers and the ambulance crew. Am J Emerg Med 2002;20:196–201. 10.1053/ajem.2002.33003 [DOI] [PubMed] [Google Scholar]
- 25.Coventry LL, Bremner AP, Jacobs IG, et al. Myocardial infarction: sex differences in symptoms reported to emergency dispatch. Prehosp Emerg Care 2013;17:193–202. 10.3109/10903127.2012.722175 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2020-045815supp001.pdf (49.4KB, pdf)
bmjopen-2020-045815supp002.pdf (36.7KB, pdf)
bmjopen-2020-045815supp003.pdf (79KB, pdf)
bmjopen-2020-045815supp004.pdf (54.1KB, pdf)
bmjopen-2020-045815supp005.pdf (76KB, pdf)
Data Availability Statement
Data are available in a public, open access repository. All the data included were obtained from published articles.