Abstract
Objectives
Although there is evidence that work-related exposures cause post-traumatic stress disorder (PTSD), there are few quantitative studies assessing the degree to which these factors contribute to PTSD. This systematic review with meta-analysis identified work-related exposures associated with PTSD, and quantified their contribution to this disorder.
Methods
We searched Medline, PsycINFO, Embase, PILOTS and Web of Science (2005–10 September 2019) for longitudinal studies on work-related exposures and PTSD. We described included articles, and conducted meta-analyses for exposures with sufficient homogeneous information. We performed subgroup analyses for risk of bias, study design and PTSD ascertainment. We assessed evidence quality using Grades of Recommendations, Assessment, Development and Evaluation, and estimated population attributable fractions.
Results
After screening 8590 records, we selected 33 studies (n=5 719 236). From what was moderate quality evidence at best, we identified various work-related exposures that were associated with PTSD, mainly involving individuals in the military and first responder (eg, police or fire brigade) occupations. These exposures included the number of army deployments (OR: 1.15 (95% CI 1.14 to 1.16)), combat exposure (OR 1.89 (95% CI 1.46 to 2.45)), army deployment (OR 1.79 (95% CI 1.45 to 2.21)) and confrontation with death (OR 1.63 (95% CI 1.41 to 1.90)). Effects were robust across subgroups and exposures attributed modestly (7%–34%) to PTSD. We identified additional exposures in other occupations, including life threats, being present during an attack, and hearing about a colleague’s trauma.
Conclusions
We identified various work-related exposures associated with PTSD and quantified their contribution. While exposure assessment, PTSD ascertainment and inconsistency may have biased our findings, our data are of importance for development of preventive interventions and occupational health guidelines.
Keywords: mental health, epidemiology, occupational & industrial medicine
Strengths and limitations of this study.
The strengths of this review are the systematic methods, including the a priori registered protocol, a thorough meta-analysis with sensitivity analyses, estimation of population attributable fractions and the assessment of evidential quality with Grades of Recommendations, Assessment, Development and Evaluation.
Reported studies bear sources of heterogeneity and possible bias, for example, in the ascertainment of post-traumatic stress disorders (which was not always clinically diagnosed but sometimes based on self-reports).
The external validity of our findings is limited as the majority of the studies in our review were based on armed forces, first responders and other male dominated occupations, and mainly from Western countries.
Evidence reported in our review was moderate quality at best, among other elements, due to risk of bias regarding participation (ie, selection bias), attrition and misclassification.
Background
Post-traumatic stress disorder (PTSD) can be triggered when individuals experience or witness traumatic events. PTSD has been a clinical diagnosis since 1980, when the third edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM) was published.1 The most recent DSM-52 states that PTSD results from exposure to severely traumatic event(s), while exhibiting a pattern of symptoms characterised by intrusion, avoidance, negative moods and cognitions, arousal and reactivity. A diagnosis of PTSD also involves duration and functional impairment criteria, and the patient’s symptoms should be exclusive (ie, not caused by drugs or other illnesses). Estimates of PTSD prevalence among the general population differ widely. For example, lifetime PTSD prevalence ranged from 6% to 9% in USA and Canadian samples, while prevalence rates in Australian samples range from 1% to 2%.3 The substantial differences between individual studies could result from different ways in which PTSD was ascertained, varying from any type of clinical diagnosis, to self-reports of DSM-5 criteria and PTSD symptoms assessed as probable PTSD.
PTSD can have a major impact on individuals and society as a whole, as it is associated with mental comorbidities,4 substance abuse5 and suicide.6 PTSD is particularly prevalent among certain occupational groups, such as police officers, firefighters, medical workers and military personnel, all of whom can experience events that might trigger PTSD.7 8 One particular systematic review showed that the prevalence of PTSD in military veterans and other high-risk occupational groups can be almost twice as high as among the general population.8 Another more recent review identified a number of occupational groups, including healthcare workers, police officers, prison workers and emergency personnel, with an increased risk of PTSD.9 Also, various specific work-related exposures (ie, exposures to situations or conditions at work that may have an effect on PTSD) and their association with PTSD have been reported.7 This included traumatic events experienced by military personnel and first responders (eg, police officers or fire fighters). The latter review also identified journalists, healthcare workers or individuals in other occupations who are exposed to traumatic events or the aftermath thereof.7
Despite this evidence, the association of work-related exposures with PTSD has not yet been quantified in a meta-analysis. Such knowledge is of importance to answer questions regarding work-related causation and prevention, as a prelude to developing interventions. With regard to prevention, we need to quantify the contribution of work-related exposures in the onset of PTSD.10 Such data could be used to formulate clinically relevant exposure threshold limits, as has been done with other disorders.11 12 It could also be of use in occupational health guidelines, as many countries provide financial compensation for individuals diagnosed with an occupational disease.
In this study, our aim was to (1) identify the work-related exposures associated with the onset of PTSD and (2) quantify the extent to which such exposures contribute to this disorder. Evidence on the contribution of work-related factors to PTSD could be used to facilitate decisions in reporting schemes. It could also help to identify and prioritise preventive interventions against those exposures with the strongest effect, in terms of triggering PTSD.
Methods
The protocol for this systematic review with meta-analysis was registered in PROSPERO13 a priori. The review itself was conducted in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement guidelines.14
Searches
The Medline, PsycINFO, Embase, PILOTS and Web of Science databases were systematically searched for material published from 2005 (January) to 2019 (September 10). This was an arbitrarily chosen period on the basis of changes in people’s exposure to work-related traumatic events and changes in the definition of PTSD over time.2 The search strategy consisted of a combination of controlled search terms (eg, Medical Subject Headings) and free-text words used to specify search terms related to: (1) PTSD (2) exposure and (3) work. A methodological filter was used to select longitudinal studies (prospective, retrospective or case–control), studies published in English, and those involving human participants only. The search strategy used is described in detail in online supplemental file 1. We validated this search with various key references, to avoid term bias. In addition to the database search, we conducted snowball searches for additional studies. These were based on citation tracking (forwards and backwards) from the articles and reviews retrieved in our electronic search. We also conducted scoping searches for key researchers on this topic, and used ResearchGate profiles to identify relevant records and projects (including unpublished projects). Outcome articles were compared with potential protocol papers, to assess selective reporting.
bmjopen-2021-049651supp001.pdf (81.5KB, pdf)
Inclusion and exclusion criteria
Two reviewers, working independently of one another, used Rayyan (an online tool: https://rayyan.qcri.org/) to screen for eligible references. The full texts of any such references (whose eligibility was based on the screening title and abstract) were retrieved for further screening. Any conflicts were resolved during a consensus meeting. We included studies on the association between any work-related exposure and the onset of PTSD (acute or delayed) in paid workers of working age (aged 18–65). Any studies that described work-related exposures in terms of work demands or other occupational factors were eligible for inclusion. However, studies in which exposures were related to job title or work title only were excluded. Studies were included if there was an actual diagnosis of PTSD (either using checklists with defined cut-off values or clinical criteria, eg, using DSM criteria2 and/or coded according to the International Classification of Disorders-9-CM 309.81-). Studies in which PTSD was assessed by means of self-reports only (not using any criteria) were excluded. We excluded any studies into the persistence or growth of PTSD. Those studies in which the exposure–outcome association was quantified, for example, in terms of effect sizes such as a HR, relative risk (RR) or OR, were included. We restricted ourselves to original articles, in English or Dutch, published in peer-reviewed scientific journals from 2005 onwards. Studies with a prospective, retrospective or case–control longitudinal design were included, while cross-sectional studies were excluded, to be able to monitor the time sequence between exposure and the PTSD onset, in which the assessments of exposure precede the actual onset of the disorder. The above-mentioned set of criteria were finalised after a pilot screening of 300 references.
Data extraction and risk of bias assessment
Two reviewers, working independently of one another, extracted data and assessed risk of bias from each of the eligible articles. Any conflicts were resolved during a consensus meeting. We extracted first author and year of publication, study name and design, sample (country, occupational group, age and sex), exposure assessment, PTSD ascertainment and effect size. Where it was not possible to retrieve sufficient information from the published articles, additional data were requested from study researchers.
Risk of bias was assessed using the ‘Quality in Prognosis Studies’ tool,15 with criteria related to study participation, attrition, prognostic factor (ie, exposure) measurements, outcomes, confounding and statistical analysis. Here, we attributed a low risk of bias regarding attrition to studies with a >80% participant retention.
Data analysis
The included articles were described in terms of extracted data and risk of bias. Work-related exposures were categorised according to the DSM-5 criteria for PTSD stressors2: (1) direct exposure to the trauma, (2) witnessing a trauma, (3) hearing about a colleague/coworkers (adapted to work context) was/were exposed to a trauma or (4) indirect exposure to aversive details of a trauma (eg, first responders and medics).
Where sufficient clinically and methodologically homogeneous information were available, a quantitative meta-analysis was conducted to determine a pooled effect size for the association of each exposure with PTSD. Review Manager (RevMan V.5) was used for the meta-analyses, and to generate forest and funnel plots. The latter were used to assess publication bias, through visual inspection. According to the Cochrane collaboration handbook, funnel plots were only generated for exposures with effect sizes from ≥10 studies.16 Most of the exposure–outcome associations featured statistical heterogeneity (I2 >75%), so random-effects estimates were adopted for statistical pooling. We assumed that the interpretation of effect estimates (eg, HR and OR) was consistent, and we estimated pooled OR with 95% CI. We adopted the OR, as this was the most frequently reported effect size in the articles found (being reported in 32 articles, whereas two articles reported HRs and three articles reported RRs).
When more than one article reported on the same study, information from just one of these articles was used for analyses, using effect sizes from the article with the shortest follow-up duration (with a latency time of at least 4 weeks) to ensure that the work-related exposure of interest is indeed the most likely cause of PTSD. Wherever possible, we used information from fully adjusted models and we did not consider subgroups (eg, sex differences). Population attributable fractions (PAFs) were estimated17 to assess the extent to which work-related exposures contributed to the development of PTSD. Here, the proportion of workers exposed to the exposure of interest (Pe) were multiplied by the attributable proportion in the exposed workers: Pe(OR−1)/(1+Pe(OR−1)).
In line with our registered protocol,13 subgroup analyses were based on the risk of bias (with a cut-off score of 60% for the risk of bias scale summary score, to obtain two subgroups), on the study design (prospective vs retrospective) and on PTSD ascertainment (clinically diagnosed PTSD vs probable PTSD). In contrast to the protocol that we registered a priori,13 we were unable to compare other characteristics of PTSD (ie, acute vs delayed) due to limited available data. Any information that could not be qualitatively analysed was described narratively.
Strength of evidence
The strength of the evidence was assessed using the Grades of Recommendations, Assessment, Development and Evaluation (GRADE) framework.18 Four quality levels were distinguished: high, moderate, low and very low. Our starting point for evidence grading was ‘moderate’, which has previously been proposed for use in the assessment of prognostic factors.19 Various study limitations could have detracted from the strength of the evidence (if the majority of the studies scored <60% on the risk of bias scale), as could inconsistency (I2 >50%), indirectness, imprecision (95% CI boundaries are <1 and >2) and publication bias (based on the funnel plots). Study findings with moderate or large effect sizes (ie, lower limit of 95% CI OR >2.0) or an exposure–response gradient could boost the quality of the evidence.
Patient and public involvement
There was no patient or public involvement in designing and conducting this study.
Results
Study selection
The study selection procedure is described in figure 1. We identified 14 529 records during database searches. After discarding duplicates, we screened the remaining 8590 records on title and abstract. Of these, we assessed 107 full-text articles and excluded 65 for various reasons (see online supplemental file 2 for more details). As no additional articles were found during snowball and scoping searches, 42 articles from 33 studies were described in this review.20–61
Figure 1.
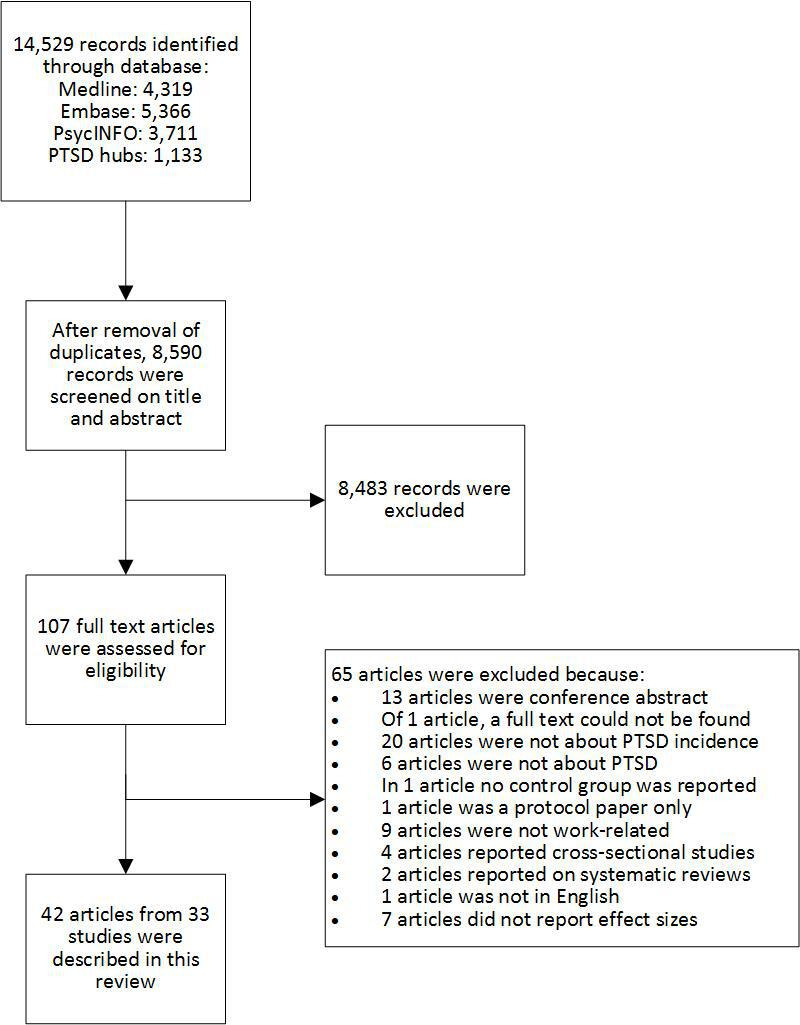
Flow chart depicting the search for literature. PTSD, post-traumatic stress disorder.
bmjopen-2021-049651supp002.pdf (102.7KB, pdf)
Study description and methodological quality/risk of bias
Online supplemental file 3 contains the extracted data, and risk of bias assessment is shown in online supplemental files 4 and 5. The 33 included studies provided data on n=5 719 236 participants, ranging from n=19 to n=2 549 949 participants per study. Eighteen studies were from the USA, four were from the UK, two were from Denmark and two others from Japan. There was one study from each of the following countries: Israel, The Netherlands, Germany, Portugal, Italy, Norway and Korea. The majority of the studies (N=21) involved participants from armed forces. Five studies featured first responders who had attended the scene of a disaster, three focused on healthcare workers, two on employers at the scene of a disaster, one on bank workers and one on public transport workers.
bmjopen-2021-049651supp003.pdf (442.2KB, pdf)
bmjopen-2021-049651supp004.pdf (58.2KB, pdf)
bmjopen-2021-049651supp005.pdf (109.4KB, pdf)
Four studies reported no details of sex, five studies only used male participants, and 17 used samples in which the majority of participants were male (≤20% females). In only seven studies, did female participants make up a reasonable proportion (>20%) of the study sample. Twenty-eight studies reported exposures obtained from self-reports, 12 studies used deployment administration databases and 2 studies were based on a combination of these two measurements. Baseline exposure assessment was carried out for the period 1983–2012. Twenty-five articles assessed PTSD (by clinical diagnosis) while the remaining 17 articles assessed probable PTSD/PTSD symptoms (by self-reports using predefined (eg, DSM-5) criteria). The weighted average for PTSD prevalence during in the follow-up periods was 7.3%, while individual study prevalence ranged from 1.0% to 70.5%. The average prevalence for diagnosed cases of PTSD was slightly higher (7.3%) than for probable PTSD (6.4%).
Twenty-five studies were prospective studies and eight were retrospective studies. On average, methodological quality was 62% (SD:19%), ranging from 25% to 100%. Most articles showed a low risk of bias on analysis/reporting (N=37) and confounding (N=25). Less than half of the articles showed a low risk of bias on participation selection (N=11), attrition (N=9), prognostic factor (exposure) assessment (N=9) and outcome (PTSD) ascertainment (N=13).
Work-related exposures
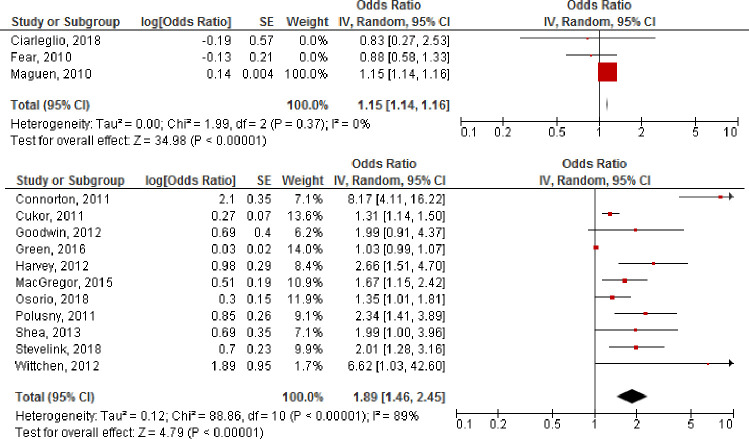
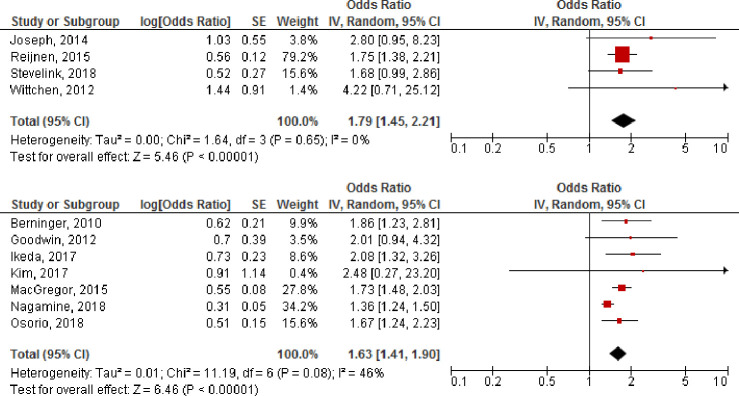
Each of the exposure–outcome associations presented have been described and categorised according to the DSM-5 criteria for PTSD stressors2: (1) direct exposure, (2) witnessing a trauma, (3) hearing that a colleague or coworker was exposed to a trauma or (4) indirect exposure to aversive details of a trauma. An overview of qualitative and quantitative analyses of all exposure–outcome associations is shown in table 1. Figures 2 and 3 depict quantitative analyses, while table 2 contains an overview of any exposure–outcome associations that could not be statistically pooled.
Table 1.
Overview of the evidence from both qualitative and quantitative analyses, with exposures categorised according to DSM-5 criteria
| DSM-5 criterion | Exposure | N | N | Limit* | Incons† | Indirect‡ | Imprec§ | Pub bias¶ | OR (95% CI)** | Grad†† | GRADE | PAF | Reference |
| Direct exposure | No of army deployments‡‡ | 3 | 333 024 | No | 0% | No | No | N/A | 1.15 (1.14 to 1.16) | No | Moderate | 7% | Figure 2 |
| Combat exposure | 11 | 28 304 | Yes | 89% | No | No | Yes | 1.89 (1.46 to 2.45) | No | Very low | 14% | Figure 2 | |
| Army deployment§§ | 4 | 11 023 | Yes | 0% | No | No | N/A | 1.79 (1.45 to 2.21) | No | Low | 34% | Figure 3 | |
| Undergoing a traumatic event | 13 | 1 703 107 | – | – | – | – | – | Min: 0.86 (0.32 to 2.28) Max: 5.65 (3.27 to 9.74) |
– | – | Table 2 | ||
| Cumulative exposure | 8 | 1 749 762 | – | – | – | – | – | Min: 0.97 (0.92 to 1.03) Max: 6.5 (1.6 to 25.6) |
– | – | Table 2 | ||
| Exposure severity | 3 | 2558 | – | – | – | – | – | Min: 1.01 (0.67 to 1.35) Max: 6.5 (1.6 to 26.0) |
– | – | Table 2 | ||
| Witnessing trauma | – | 5 | 4876 | – | – | – | – | – | Min: 1.01 (0.63 to 1.64) Max: 9.3 (6.1 to 14.2) |
– | – | Table 2 | |
| Colleague exposed¶¶ | – | 1 | 980 | – | – | – | – | – | 0.55 (0.12 to 2.47) | – | – | Table 2 | |
| Indirect exposure | Confrontation with death | 7 | 75 902 | No | 46% | No | No | N/A | 1.63 (1.41 to 1.90) | No | Moderate | 15% | Figure 3 |
| 4 | 14 085 | – | – | – | – | – | Min: 1.03 (1.00 to 1.06) Max: 4.0 (2.5 to 6.6) |
– | – | Table 2 | |||
| Other exposures | Stress | 4 | 1 390 641 | – | – | – | – | – | Min: 1.01 (0.98 to 1.04) Max: 3.52 (2.94 to 4.21) |
– | – | Table 2 | |
| Time since event | 3 | 1 358 468 | – | – | – | – | – | Min: 0.47 (0.32 to 0.70) Max: 1.89 (0.99 to 3.60) |
– | – | Table 2 | ||
| Other | 3 | 69 176 | – | – | – | – | – | Min: 1.08 (0.97 to 1.20) Max: 5.72 (3.37 to 9.71) |
– | – | Table 2 |
For exposures for which quantitative analyses could be performed (figures 2 and 3), quality of the evidence for the relationship between work-related exposures and PTSD according to the GRADE framework is shown. Other exposures are described qualitatively (table 2).
*Limitation: downgraded if the majority of studies score lower than 60% on the risk of bias scale.
†Inconsistency: downgrade if I2 ≥50%.
‡Indirectness: downgrade if indirectness is present.
§Imprecision: downgrade if the 95% CI is <1 and >2.
¶Publication bias: downgraded if publication bias is present (based on the funnel plots).
**Effect size: upgrade if the lower limit of the 95% CI is >2.0.
††Gradient: upgraded if there is a dose–response gradient available.
‡‡Depicting the effect of being deployed more than once, as compared with being deployed once.
§§Depicting the effect of being deployed, as compared with not being deployed.
¶¶For this study on occupational exposures, the DSM-5 criterion ‘relative/friend’ was adapted to ‘colleague or coworker’.
DSM-5, Diagnostic and Statistical Manual of Mental Disorders, fifth edition; GRADE, Grades of Recommendations, Assessment, Development and Evaluation; NA, not available; PAF, population attributable fractions; PTSD, post-traumatic stress disorder.
Figure 2.
Study findings (ie, effect sizes) for articles reporting on the association of number of army deployments (depicting the effect of being deployed more than once, as compared with being deployed once; upper panel) and combat exposure (lower panel) with PTSD. Individual study as well as pooled effects are presented. IV, inverse variance; PTSD, post-traumatic stress disorder.
Figure 3.
Study findings (ie, effect sizes) for articles reporting on the association of deployments status (depicting the effect of being deployed, as compared with not being deployed; upper panel) and confrontation with death (lower panel) with PTSD. Individual study as well as pooled effects are presented. IV, Inverse variance; PTSD, post-traumatic stress disorder.
Table 2.
Overview of all exposure–outcome effect sizes from qualitative analyses, with exposures categorised according to DSM-5 criteria
| DSM-5 criterion | Exposure category | Exposure | Effect size (OR (95% CI)) |
| Direct exposure | Undergoing an event | Work-related threats20 | 1.10 (1.04 to 1.15) |
| Work-related violence20 | 1.02 (0.98 to 1.06) | ||
| Previous disaster experience23 | 1.4 (1.2 to 1.6) | ||
| One injury sustained during the 9/11 attacks29 | 1.1 (0.6 to 2.0) | ||
| Two or more injuries sustained during the 9/11 attacks29 | 1.4 (0.6 to 3.4) | ||
| Participation in abusive violence33 | 3.32 (1.81 to 6.08) | ||
| Robberies during working life34 | 1.18 (0.97 to 1.44) | ||
| Physical contacts with robbers34 | 0.86 (0.32 to 2.28) | ||
| Scuffle (taking part or being present)34 | 1.92 (0.63 to 5.79) | ||
| Being injured during the robbery34 | 1.28 (0.31 to 5.21) | ||
| Discharged weapon on deployment36 | 1.48 (0.61 to 3.60) | ||
| Experience of life-threatening danger42 | 4.32 (2.89 to 6.48) | ||
| Major property loss42 | 3.45 (2.28 to 5.23) | ||
| Escape from tsunami42 | 5.65 (3.27 to 9.74) | ||
| Life threatening war45 | 1.91 (1.07 to 3.24) | ||
| Conflict with passengers46 | 3.21 (1.14 to 9.03) | ||
| Felt in great danger of being killed48 | 3.44 (2.50 to 4.72) | ||
| Exposure to blast50 | 4.72 (2.9 to 7.7) | ||
| Encountering explosive devices54 | 1.26 (0.95 to 1.66) | ||
| Cumulative exposure | Prolonged work at the WTC site23 | 2.0 (1.7 to 2.3) | |
| Length of deployment37 | 0.97 (0.92 to 1.03) | ||
| ≥5 critical cases per call for traumatic surgeons43 | 7 (1.1 to 8) | ||
| ≥7 call duties a month for traumatic surgeons43 | 3.8 (0.9 to 7.2) | ||
| ≥15 operative cases per month43 | 2.8 (0.4 to 3.2) | ||
| Cumulative years deployed in navy47 | 2.04 (1.93 to 2.15) | ||
| Cumulative years deployed in army47 | 1.74 (1.71 to 1.76) | ||
| No of combat exposures48 | 1.62 (1.46 to 1.79) | ||
| Two combat exposure deployment48 | 1.37 (1.17 to 1.61) | ||
| Three combat exposure deployment48 | 1.30 (0.94 to 1.82) | ||
| Two deployments48 | 1.00 (1.00 to 1.01) | ||
| Three deployments48 | 1.00 (0.99 to 1.01) | ||
| One exposure (compared with no exposure)50 | 4.67 (3.1 to 7.1) | ||
| Two or more deployments (compared with no exposure)50 | 6.15 (4.4 to 8.7) | ||
| Deployment length 1–3 months53 | 1.53 (1.37 to 1.70) | ||
| Deployment length ≥3 months53 | 2.64 (2.33 to 2.99) | ||
| Low frequency of violence (compared with no violence)55 | 4.0 (1.0 to 16.3) | ||
| Medium frequency of violence (compared with no violence)55 | 5.9 (1.4 to 24.2) | ||
| High frequency of violence (compared with no violence)55 | 6.5 (1.6 to 25.6) | ||
| Exposure severity | Combat exposure scale33 | 1.98 (1.50 to 2.62) | |
| Severity of battles45 | 1.01 (0.67 to 1.35) | ||
| Max. mild violence (compared with no violence)55 | 3.8 (0.3 to 46.2) | ||
| Max. threats of violence (compared with no violence)55 | 5.4 (1.2 to 24.2) | ||
| Max. moderate violence (compared with no violence)55 | 2.6 (0.6 to 10.8) | ||
| Max. severe violence (compared with no violence)55 | 6.5 (1.6 to 26.0) | ||
| Witnessing the trauma | Perceived life threat56 | 1.01 (0.63 to 1.64) | |
| Observation of abusive violence33 | 8.36 (4.56 to 15.35) | ||
| Presence during attack38 | 9.3 (6.1 to 14.2) | ||
| Witnessing of plant explosions42 | 2.09 (1.43 to 3.06) | ||
| Person under train experience46 | 1.54 (0.52 to 4.55) | ||
| One person under train experiences46 | 1.77 (0.31 to 4.47) | ||
| Two or more person under train experiences46 | 2.36 (0.57 to 9.70) | ||
| Sudden train stop46 | 3.66 (0.82 to 16.4) | ||
| Near train accident46 | 8.81 (1.96 to 39.3) | ||
| Damage to train46 | 1.71 (0.48 to 6.14) | ||
| Colleague exposed | Person under train experience of colleague46 | 0.55 (0.12 to 2.47) | |
| Indirect exposure to aversive details | Aftermath of battle37 | 1.03 (1.00 to 1.06) | |
| Morning of 9/11 (compared with >3 days)27 | 4.0 (2.5 to 6.6) | ||
| Afternoon of 9/11 (compared with >3 days)27 | 2.1 (1.3 to 3.3) | ||
| Day 2 (compared with >3 days)27 | 1.4 (0.9 to 2.4) | ||
| Morning of 9/11 (compared with >3 days)23 | 2.0 (1.3 to 2.9) | ||
| Afternoon of 9/11 (compared with >3 days)23 | 1.1 (0.8 to 1.5) | ||
| Exposure to aftermath of battle56 | 1.81 (1.08 to 3.06) | ||
| Other exposures | Stress | High deployment stress21 | 3.52 (2.94 to 4.21) |
| Deployment concerns summary score28 | 1.01 (0.98 to 1.04) | ||
| Worried by other issues related to robbery34 | 2.64 (0.95 to 7.36) | ||
| Unit cumulative high deployment stress rate (marine)47 | 1.04 (1.03 to 1.05) | ||
| Unit cumulative high deployment stress rate (army)47 | 1.05 (1.04 to 1.06) | ||
| Time since event | Months since most recent deployment28 | 1.00 (0.98 to 1.02) | |
| Time since return from deployment (up to 2 years)32 | 1.18 (0.75 to 1.86) | ||
| Time since return from deployment (up to 3 years)32 | 1.80 (1.05 to 3.10) | ||
| Time since return from deployment (up to 4 years)32 | 1.88 (0.98 to 3.62) | ||
| Time since return from deployment (up to 5 years)32 | 1.53 (0.92 to 2.55) | ||
| Time since return from deployment (up to 6.5 years)32 | 1.89 (0.99 to 3.60) | ||
| Dwell to deployment ratio (1:1 vs <1:1)48 | 0.83 (0.60 to 1.13) | ||
| Dwell to deployment ratio (2:1 vs <1:1)48 | 0.47 (0.32 to 0.70) | ||
| Other | Supervising responsibilities23 | 2.2 (1.7 to 2.9) | |
| Discrimination/slurs42 | 5.72 (3.37 to 9.71) | ||
| Duties with radiation exposure risk53 | 1.08 (0.97 to 1.20) |
OR with 95% CI are shown.
DSM-5, Diagnostic and Statistical Manual of Mental Disorders, fifth edition; WTC, World Trade Center.
Direct exposure
The exposure–outcome associations for direct exposures were quantitatively analysed for: number of army deployments (OR (95% CI): 1.15 (1.14 to 1.16), I2=0%, n=333 024, figure 2), combat exposure (OR (95% CI): 1.89 (1.46 to 2.45), I2=89%, n=28 304, figure 2) and army deployment (OR (95% CI): 1.79 (1.45 to 2.21), I2=0%, n=11 023, figure 3). The PAFs for these exposures were 7%, 14% and 34%, respectively. Evidence for these exposure–outcome associations was moderate, very low and low quality, respectively. In some cases, the evidence was downgraded due to high risk of bias and inconsistency. There was some evidence for publication bias, although it was only possible to assess that for the ‘combat exposure’ variable (online supplemental file 6). Subgroup analyses based on risk of bias (online supplemental files 7–9), study design (online supplemental files 10–12) and PTSD ascertainment (online supplemental files 13–15) showed no statistically significant differences between effects for those subgroups.
bmjopen-2021-049651supp006.pdf (31.1KB, pdf)
bmjopen-2021-049651supp007.pdf (42.1KB, pdf)
bmjopen-2021-049651supp008.pdf (47.9KB, pdf)
bmjopen-2021-049651supp009.pdf (42.8KB, pdf)
bmjopen-2021-049651supp010.pdf (42KB, pdf)
bmjopen-2021-049651supp011.pdf (47.6KB, pdf)
bmjopen-2021-049651supp012.pdf (42.4KB, pdf)
bmjopen-2021-049651supp013.pdf (41.9KB, pdf)
bmjopen-2021-049651supp014.pdf (47.5KB, pdf)
bmjopen-2021-049651supp015.pdf (42.7KB, pdf)
In our qualitative analyses of exposures that could not be statistically pooled, we found exposure–outcome associations for exposures related to undergoing a traumatic event, cumulative exposure and the severity of exposure (table 2). With regard to undergoing a traumatic event, the effect sizes ranged from OR (95% CI): 0.86 (0.32 to 2.28) (physical contacts with thieves)34 to OR (95% CI): 5.65 (3.27 to 9.74) (workers fleeing from a tsunami).42 Cumulative exposure was, for example, expressed in length of deployment37 (OR (95%CI): 0.97 (0.92 to 1.03)) and high frequency of violence (compared with no violence)55 (OR (95% CI): 6.5 (1.6 to 25.6)). The effect sizes for exposure severity ranged from OR (95% CI): 1.01 (0.67 to 1.35) (severity of battles)45 to OR (95% CI): 6.5 (1.6 to 26.0) (severe compared with no violence).55
Witnessing a trauma
With regard to the DSM-5 criterion ‘witnessing a trauma’, there was insufficient homogeneous data to pool studies statistically (table 2). In five studies (with n=4876 participants), effect sizes ranged from OR (95% CI): 1.01 (0.63 to 1.64) (‘perceiving a life threat’)56 to OR (95% CI): 9.3 (6.1 to 14.2) (‘being present during an attack’).38
A colleague or coworker was exposed to a trauma
Only one study (n=980) reported on effect sizes regarding ‘colleague or coworker exposed to a trauma’. This study, among public transport workers, found that ‘hearing that a close colleague had suffered a person under train experience’ was not significantly association with PTSD (OR (95% CI): 0.55 (0.12 to 2.47))46
Indirect exposure to aversive details
Regarding indirect exposure to adverse events, we statistically pooled the effect sizes from seven studies (n=75 902 participants) with moderate-quality evidence for an association between confrontation with death and PTSD (figure 3; OR (95% CI): 1.63 (1.41 to 1.90)). Subgroup analyses regarding risk of bias (online supplemental file 16), study design (online supplemental file 17) and PSTD ascertainment (online supplemental file 18) showed no statistically significant differences between any of those subgroups.
bmjopen-2021-049651supp016.pdf (45.1KB, pdf)
bmjopen-2021-049651supp017.pdf (44.2KB, pdf)
bmjopen-2021-049651supp018.pdf (44.4KB, pdf)
Additional evidence from four studies (n=14 085 participants), which could not be statistically pooled, showed effect sizes ranging from OR (95% CI): 1.03 (1.00 to 1.06) (being exposed to the aftermath of a battle)37 to OR (95% CI): 4.0 (2.5 to 6.6) (being present during the morning of the 9/11 attacks).27
Other exposures
We found additional evidence that could not be categorised into any of the DSM-5 criteria. An increased risk of PTSD was associated with experiencing stress, with evidence ranging from OR (95% CI): 1.01 (0.98 to 1.04) (deployment concerns)28 to OR (95% CI): 3.52 (2.94 to 4.21) (high deployment stress).21 Also, the time that has passed since a given traumatic event seems to be associated with PTSD. This factor can either reduce the PTSD risk (OR (95% CI): 0.47 (0.32 to 0.70) with a longer dwell time between deployments)48 or increase it (OR (95% CI): 1.89 (0.99 to 3.60) if the period since the return from deployment exceeds 6.5 years).32 Other exposures included experiencing discrimination at work (OR (95% CI): 5.72 (3.37 to 9.71))42 and having to perform duties that involved a risk of radiation exposure (OR (95% CI): 1.08 (0.97 to 1.20)).53
Discussion
In this systematic review with meta-analysis and evidence grading, we found various associations, although based on moderate-quality evidence at best, showing that several work-related exposures are associated with PTSD development. This includes exposures such as the number of army deployments, combat exposure, army deployment and confrontation with death. The corresponding effect sizes ranged from 1.15 (1.14 to 1.16) to 1.89 (1.46 to 2.45) and PAFs varied from 7% (for the number of army deployments) to 34% (for army deployment). The latter values indicate the proportion of PTSD cases that could potentially be avoided in a working population, if the exposure in question were to be totally eliminated. The data suggest that there could be an only moderate relationship between PTSD and work situations. However, they could also indicate that PTSD cannot be attributed to a single work-related exposure and that it is multifactorial in nature and/or is mediated by other factors. This could, perhaps, also account for the relatively low ORs found for some of the effects.
Only a limited data, which could not be statistically pooled, was available concerning exposures that corresponded to the DSM-5 criteria ‘witnessing a trauma’ and ‘hearing that a colleague/coworker was exposed to a trauma’. These exposures include ‘perceiving a life threat’, ‘being present during an attack’ and ‘hearing that a close colleague had suffered a person under train experience’. The additional exposures that could not be categorised according to DSM-5 criteria include ‘military deployment’, ‘deployment stress’ and ‘time since return from deployment’. In future, it may be worth considering exposures of this kind when diagnosing work-related PTSD.
The details uncovered by this review are key to a better understanding of work-related causes of PTSD, to the selection or development of preventive interventions, and to the identification of thresholds for occupational health guidelines. This review has updated earlier work7 9 and we are the first to quantify the association between work-related exposures and PTSD. This update identifies occupational groups and exposures that do not feature in previous reviews, such as public transport workers46 and bank workers (being exposed to robberies).34
Although the prevention of occupational diseases, including PTSD, is preferable, not all risks can be fully eliminated as witnessing traumatic events, disasters and war situations are likely to remain present in our working situations. In the working environment it is also important to attenuate the impact of exposures on workers or to treat them when having developed work-related PTSD. In the current review, we also identified work-related factors that can reduce the risk of PTSD, which can be helpful to attenuate the impact of stressful exposures. For instance, among highly exposed occupational groups, a high level of preparedness (OR (95% CI): 0.6 (0.4 to 0.9)),62 unit support (OR (95% CI): 0.5 (0.3 to 0.8)),62 postdeployment support (OR (95% CI): 0.3 (0.2 to 0.4))62 and social support (OR (95% CI): 0.96 (0.93 to 0.98))37 were all found to be associated with a reduced risk of PTSD. These elements can be used in the development of interventions, especially for those in occupations that involve high PTSD risks.
Methodological strengths and limitations
The strengths of this review are the systematic methods used plus a protocol that was registered a priori, the systematic review with meta-analysis and the assessment of evidential quality using GRADE.18 The findings appear to be quite robust, since subgroup analyses based on risk of bias, study design and PTSD ascertainment produced results that did not differ between any of those subgroups. Moreover, the PAFs estimated in our study provide insight into the extent to which the identified exposures were occupationally related to PTSD.
We deviated from our a prior registered protocol13 in that we were unable to compare different PTSD diagnoses (acute vs delayed). In our meta-analysis, we used effect sizes from the article with the shortest follow-up duration (with a latency time of at least 4 weeks). There were, however, also data available from few studies measuring both the short-term and long-term effects of exposure and their association with PTSD. For example, ‘being present during a terrorist attack’ was strongly associated with PTSD in the acute phase (after 10 months; OR (95% CI): 9.3 (6.1 to 14.2)), but this association was even stronger in the long term (after 34 months; OR (95% CI): 10.0 (5.4 to 18.6)).38 Regarding ‘being exposed to combat’, the opposite was true. Stronger effects were seen in short term (OR (95% CI): 2.91 (1.34 to 6.31)) than long term (OR (95% CI): 2.42 (1.04 to 5.62)).39 This is in line with another review indicating that, following exposure, the risk of PTSD attenuates over time.7
Another potential source of heterogeneity stems from the method used to ascertain PTSD. In 25 articles, PTSD was assessed by clinical diagnosis while 17 articles assessed probable PTSD/PTSD symptoms, based on self-reports using predefined (eg, DSM-5) criteria. We found that the average prevalence was slightly higher for diagnosed PTSD (7.3%) than for probable PTSD (6.4%). This is in line with a study of disaster workers, following the 9/11 attacks, in which 2%–9% had probable self-reported PTSD, respectively.31 However, 6%–15% of these workers were diagnosed with PTSD. Nevertheless, our pooled effect sizes were robust across different methods for ascertaining PTSD. While ascertaining PTSD by clinical diagnosis may be more valid, this source of heterogeneity is unlikely to have substantially affected the findings presented. We have only assessed incidence of PTSD. Accordingly, this review does not address the persistence or growth of PTSD. Future studies should, therefore, focus on different types of PTSD diagnoses. They should also assess the work-relatedness of PTSD persistence and growth, as an aid to the development of occupational health guidelines.
One limitation of our study is that the majority of the studies in this review were based on participants from armed forces (N=21) and first responders (N=5). There was limited information on other occupations, such as public transport workers, bank employees and healthcare workers. Furthermore, most studies of the armed forces and of first responders tend to be male dominated and from Western countries. Future research should address these issues, by assessing previously unexplored occupational sectors and groups, as well as data from other countries. In this review, we only included longitudinal studies in which the exposure would proceed the outcome, as a result of which a better inference of causality can be provided than with cross-sectional studies only. Moreover, we focused in our review on articles published from 2005 onwards. This cut-off was based on changes in people’s exposure to work-related traumatic events and changes to the definition of PTSD over time.2
While our use of the GRADE framework provides an adequate way to assess quality of the evidence, it does not necessarily provide insights into causation of the association of work-related exposures and PTSD, for which other approaches such as the Bradford Hill criteria63 could be used. It has been argued that the majority of the Bradford Hill criteria are to some extent incorporated in GRADE, such as the strength and consistency of the association.64 Other criteria, such as that of the biological plausibility, are not well covered nor are they in the current review evidence regarding work-related PTSD. Future studies should, therefore, aim at providing more insights into this, to further build the evidence base around work-related PTSD and the biology of risk for PTSD.65 Although methodological quality of the included studies was of an acceptable level (62%, on average), the quality of the evidence was rated moderate at best. More than half of the articles showed a risk of bias with regard to participation (ie, selection bias), attrition (with <80% of the participants being retained during the follow-up period) and misclassification due to a limited assessment of the prognostic factors (ie, exposure) and the outcome of interest. As mentioned above, the ascertainment of PTSD is unlikely to have caused a substantial bias in our findings. However, exposures were often measured by means of self-reports, which may well have biased our findings. In addition, the quality of the evidence was downgraded due to inconsistency for some of the exposures. Our assessment of publication bias was limited to just one of the pooled exposures. It appeared, however, that none of the studies had published or registered their protocol, which could have caused publication bias.
Conclusion
In this systematic review with meta-analysis of 33 studies (with n=5 719 236 participants), based on moderate quality evidence at best, we identified a number of work-related exposures (mainly involving individuals in the armed forces and in first responder occupations) that increase the risk of PTSD (by 15%–89%). These exposures include ‘number of army deployments’, ‘combat exposure’, ‘army deployment’ and ‘confrontation with death’, for which we found a moderate contribution to the development of PTSD. We identified additional exposures in other occupations, such as bank workers, public transport workers and medics. These included ‘life threats’, ‘being present during an attack’ and ‘hearing about a colleague’s trauma’. Although exposure assessment, PTSD ascertainment and inconsistency may have biased our findings, the results of this review are quite robust and are of importance for the development of preventive interventions and occupational health guidelines.
Supplementary Material
Acknowledgments
We would like to thank Teus Brand, Bas Sorgdrager and Gerda de Groene for their critical appraisal and the relevant feedback provided. We would like to thank Joost Daams for helping us with the search for literature.
Footnotes
Contributors: Both authors (PC and HFvdM) designed the study and reviewed the manuscript for important intellectual content. Both authors identified relevant articles and conducted data extraction and analyses together. PC drafter the first version of the manuscript. HFvdM is the study guarantor.
Funding: The study has been funded by the Dutch Ministry of Social Affairs and Employment (grant no. 22968).
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as online supplemental information.
Ethics statements
Patient consent for publication
Not required.
References
- 1.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 3rd ed. Washington DC, USA, 1980. [Google Scholar]
- 2.American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 5th ed. Washington DC, USA, 2013. [Google Scholar]
- 3.Sareen J. Posttraumatic stress disorder in adults: impact, comorbidity, risk factors, and treatment. Can J Psychiatry 2014;59:460–7. 10.1177/070674371405900902 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Knowles KA, Sripada RK, Defever M, et al. Comorbid mood and anxiety disorders and severity of posttraumatic stress disorder symptoms in treatment-seeking veterans. Psychol Trauma 2019;11:451–8. 10.1037/tra0000383 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Debell F, Fear NT, Head M, et al. A systematic review of the comorbidity between PTSD and alcohol misuse. Soc Psychiatry Psychiatr Epidemiol 2014;49:1401–25. 10.1007/s00127-014-0855-7 [DOI] [PubMed] [Google Scholar]
- 6.Pompili M, Sher L, Serafini G, et al. Posttraumatic stress disorder and suicide risk among veterans: a literature review. J Nerv Ment Dis 2013;201:802–12. 10.1097/NMD.0b013e3182a21458 [DOI] [PubMed] [Google Scholar]
- 7.Skogstad M, Skorstad M, Lie A, et al. Work-Related post-traumatic stress disorder. Occup Med 2013;63:175–82. 10.1093/occmed/kqt003 [DOI] [PubMed] [Google Scholar]
- 8.Utzon-Frank N, Breinegaard N, Bertelsen M, et al. Occurrence of delayed-onset post-traumatic stress disorder: a systematic review and meta-analysis of prospective studies. Scand J Work Environ Health 2014;40:215–29. 10.5271/sjweh.3420 [DOI] [PubMed] [Google Scholar]
- 9.Lee W, Lee Y-R, Yoon J-H, et al. Occupational post-traumatic stress disorder: an updated systematic review. BMC Public Health 2020;20:768. 10.1186/s12889-020-08903-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van der Beek AJ, Dennerlein JT, Huysmans MA, et al. A research framework for the development and implementation of interventions preventing work-related musculoskeletal disorders. Scand J Work Environ Health 2017;43:526–39. 10.5271/sjweh.3671 [DOI] [PubMed] [Google Scholar]
- 11.van der Molen HF, Foresti C, Daams JG, et al. Work-related risk factors for specific shoulder disorders: a systematic review and meta-analysis. Occup Environ Med 2017;74:745–55. 10.1136/oemed-2017-104339 [DOI] [PubMed] [Google Scholar]
- 12.Kuijer PPFM, Verbeek JH, Seidler A, et al. Work-relatedness of lumbosacral radiculopathy syndrome: review and dose-response meta-analysis. Neurology 2018;91:558–64. 10.1212/01.wnl.0000544322.26939.09 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Coenen P, Brand T, Sorgdrager B, et al. What work-related risk factors are associated with post-traumatic stress disorder? PROSPERO 2020;CRD42020155434.
- 14.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ 2009;339:b2535. 10.1136/bmj.b2535 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hayden JA, van der Windt DA, Cartwright JL, et al. Assessing bias in studies of prognostic factors. Ann Intern Med 2013;158:280–6. 10.7326/0003-4819-158-4-201302190-00009 [DOI] [PubMed] [Google Scholar]
- 16.Cochrane Collaboration . Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. Available: www.cochrane-handbook.org.2011
- 17.Poole C. A history of the population attributable fraction and related measures. Ann Epidemiol 2015;25:147–54. 10.1016/j.annepidem.2014.11.015 [DOI] [PubMed] [Google Scholar]
- 18.Huguet A, Hayden JA, Stinson J, et al. Judging the quality of evidence in reviews of prognostic factor research: adapting the grade framework. Syst Rev 2013;2:71. 10.1186/2046-4053-2-71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Foroutan F, Guyatt G, Zuk V, et al. Grade guidelines 28: use of grade for the assessment of evidence about prognostic factors: rating certainty in identification of groups of patients with different absolute risks. J Clin Epidemiol 2020;121:62–70. 10.1016/j.jclinepi.2019.12.023 [DOI] [PubMed] [Google Scholar]
- 20.Andersen LP, Hogh A, Elklit A, et al. Work-related threats and violence and post-traumatic symptoms in four high-risk occupations: short- and long-term symptoms. Int Arch Occup Environ Health 2019;92:195–208. 10.1007/s00420-018-1369-5 [DOI] [PubMed] [Google Scholar]
- 21.Anderson L, Campbell-Sills L, Ursano RJ, et al. Prospective associations of perceived unit cohesion with postdeployment mental health outcomes. Depress Anxiety 2019;36:511–21. 10.1002/da.22884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Armed Forces Health Surveillance Center . Associations between repeated deployments to Iraq (OIF/OND) and Afghanistan (OEF) and post-deployment illnesses and injuries, active component, U.S. Armed Forces, 2003-2010. Part II. Mental disorders, by gender, age group, military occupation, and "dwell times" prior to repeat (second through fifth) deployments. MSMR 2011;18:2–11. [PubMed] [Google Scholar]
- 23.Berninger A, Webber MP, Niles JK, et al. Longitudinal study of probable post-traumatic stress disorder in firefighters exposed to the world Trade center disaster. Am J Ind Med 2010;53:1177–85. 10.1002/ajim.20894 [DOI] [PubMed] [Google Scholar]
- 24.Brownlow JA, Zitnik GA, McLean CP, et al. The influence of deployment stress and life stress on post-traumatic stress disorder (PTSD) diagnosis among military personnel. J Psychiatr Res 2018;103:26–32. 10.1016/j.jpsychires.2018.05.005 [DOI] [PubMed] [Google Scholar]
- 25.Brundage JF, Taubman SB, Hunt DJ, et al. Whither the "signature wounds of the war" after the war: estimates of incidence rates and proportions of TBI and PTSD diagnoses attributable to background risk, enhanced ascertainment, and active war zone service, active component, U.S. Armed Forces, 2003-2014. MSMR 2015;22:2–11. [PubMed] [Google Scholar]
- 26.Cameron KL, Sturdivant RX, Baker SP. Trends in the incidence of physician-diagnosed posttraumatic stress disorder among active-duty U.S. military personnel between 1999 and 2008. Mil Med Res 2019;6:8. 10.1186/s40779-019-0198-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Chiu S, Niles JK, Webber MP, et al. Evaluating risk factors and possible mediation effects in posttraumatic depression and posttraumatic stress disorder comorbidity. Public Health Rep 2011;126:201–9. 10.1177/003335491112600211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ciarleglio MM, Aslan M, Proctor SP, et al. Associations of stress exposures and social support with long-term mental health outcomes among U.S. Iraq war veterans. Behav Ther 2018;49:653–67. 10.1016/j.beth.2018.01.002 [DOI] [PubMed] [Google Scholar]
- 29.Cone JE, Li J, Kornblith E, et al. Chronic probable PTSD in police responders in the world Trade center health registry ten to eleven years after 9/11. Am J Ind Med 2015;58:483–93. 10.1002/ajim.22446 [DOI] [PubMed] [Google Scholar]
- 30.Connorton E, Perry MJ, Hemenway D, et al. Occupational trauma and mental illness--combat, peacekeeping, or relief work and the national co-morbidity survey replication. J Occup Environ Med 2011;53:1360–3. 10.1097/JOM.0b013e318234e2ec [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cukor J, Wyka K, Mello B, et al. The longitudinal course of PTSD among disaster workers deployed to the world Trade center following the attacks of September 11th. J Trauma Stress 2011;24:506–14. 10.1002/jts.20672 [DOI] [PubMed] [Google Scholar]
- 32.Fear NT, Jones M, Murphy D, et al. What are the consequences of deployment to Iraq and Afghanistan on the mental health of the UK armed forces? a cohort study. Lancet 2010;375:1783–97. 10.1016/S0140-6736(10)60672-1 [DOI] [PubMed] [Google Scholar]
- 33.Ferrajão PC, Oliveira RA. The effects of combat exposure, abusive violence, and sense of coherence on PTSD and depression in Portuguese colonial war veterans. Psychol Trauma 2016;8:1–8. 10.1037/tra0000043 [DOI] [PubMed] [Google Scholar]
- 34.Fichera GP, Fattori A, Neri L, et al. Post-Traumatic stress disorder among bank employee victims of robbery. Occup Med 2015;65:283–9. 10.1093/occmed/kqu180 [DOI] [PubMed] [Google Scholar]
- 35.Fink DS, Cohen GH, Sampson LA, et al. Incidence of and risk for post-traumatic stress disorder and depression in a representative sample of US reserve and national guard. Ann Epidemiol 2016;26:189–97. 10.1016/j.annepidem.2016.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Goodwin L, Jones M, Rona RJ, et al. Prevalence of delayed-onset posttraumatic stress disorder in military personnel: is there evidence for this disorder?: results of a prospective UK cohort study. J Nerv Ment Dis 2012;200:429–37. 10.1097/NMD.0b013e31825322fe [DOI] [PubMed] [Google Scholar]
- 37.Green JD, Bovin MJ, Erb SE, et al. The effect of enemy combat tactics on PTSD prevalence rates: a comparison of operation Iraqi freedom deployment phases in a sample of male and female veterans. Psychol Trauma 2016;8:634–40. 10.1037/tra0000086 [DOI] [PubMed] [Google Scholar]
- 38.Hansen MB, Birkeland MS, Nissen A, et al. Prevalence and course of symptom-defined PTSD in individuals directly or indirectly exposed to terror: a longitudinal study. Psychiatry 2017;80:171–83. 10.1080/00332747.2016.1230983 [DOI] [PubMed] [Google Scholar]
- 39.Harvey SB, Hatch SL, Jones M, et al. The long-term consequences of military deployment: a 5-year cohort study of United Kingdom reservists deployed to Iraq in 2003. Am J Epidemiol 2012;176:1177–84. 10.1093/aje/kws248 [DOI] [PubMed] [Google Scholar]
- 40.Horesh D, Solomon Z, Zerach G, et al. Delayed-Onset PTSD among war veterans: the role of life events throughout the life cycle. Soc Psychiatry Psychiatr Epidemiol 2011;46:863–70. 10.1007/s00127-010-0255-6 [DOI] [PubMed] [Google Scholar]
- 41.Hourani L, Bender RH, Weimer B, et al. Longitudinal study of resilience and mental health in Marines leaving military service. J Affect Disord 2012;139:154–65. 10.1016/j.jad.2012.01.008 [DOI] [PubMed] [Google Scholar]
- 42.Ikeda A, Tanigawa T, Charvat H, et al. Longitudinal effects of disaster-related experiences on mental health among Fukushima nuclear plant workers: the Fukushima news project study. Psychol Med 2017;47:1936–46. 10.1017/S0033291717000320 [DOI] [PubMed] [Google Scholar]
- 43.Joseph B, Pandit V, Hadeed G, et al. Unveiling posttraumatic stress disorder in trauma surgeons: a national survey. J Trauma Acute Care Surg 2014;77:148–54. 10.1097/TA.0000000000000271 [DOI] [PubMed] [Google Scholar]
- 44.Karstoft K-I, Armour C, Elklit A, et al. Long-Term trajectories of posttraumatic stress disorder in veterans: the role of social resources. J Clin Psychiatry 2013;74:e1163–8. 10.4088/JCP.13m08428 [DOI] [PubMed] [Google Scholar]
- 45.Karstoft K-I, Armour C, Elklit A, et al. The role of locus of control and coping style in predicting longitudinal PTSD-trajectories after combat exposure. J Anxiety Disord 2015;32:89–94. 10.1016/j.janxdis.2015.03.007 [DOI] [PubMed] [Google Scholar]
- 46.Kim S-E, Kim H-R, Park J-I, et al. The association between psychiatric disorders and work-related problems among subway drivers in Korea. Ann Occup Environ Med 2014;26:39. 10.1186/s40557-014-0039-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Levin-Rector A, Hourani LL, Van Dorn RA, et al. Predictors of posttraumatic stress disorder, anxiety disorders, depressive disorders, and any mental health condition among U.S. soldiers and Marines, 2001-2011. J Trauma Stress 2018;31:568–78. 10.1002/jts.22316 [DOI] [PubMed] [Google Scholar]
- 48.MacGregor AJ, Dougherty AL, Mayo JA, et al. Post-Traumatic stress disorder among navy health care personnel following combat deployment. Mil Med 2015;180:882. 10.7205/MILMED-D-14-00323 [DOI] [PubMed] [Google Scholar]
- 49.MacGregor AJ, Han PP, Dougherty AL, et al. Effect of dwell time on the mental health of US military personnel with multiple combat tours. Am J Public Health 2012;102 Suppl 1:S55–9. 10.2105/AJPH.2011.300341 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Maguen S, Madden E, Lau KM, et al. The impact of head injury mechanism on mental health symptoms in veterans: do number and type of exposures matter? J Trauma Stress 2012;25:3–9. 10.1002/jts.21669 [DOI] [PubMed] [Google Scholar]
- 51.Maguen S, Ren L, Bosch JO, et al. Gender differences in mental health diagnoses among Iraq and Afghanistan Veterans enrolled in Veterans Affairs health care. Am J Public Health 2010;100:2450–6. 10.2105/AJPH.2009.166165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Martindale SL, Rowland JA, Shura RD, et al. Longitudinal changes in neuroimaging and neuropsychiatric status of post-deployment veterans: a CenC pilot study. Brain Inj 2018;32:1208–16. 10.1080/02699052.2018.1492741 [DOI] [PubMed] [Google Scholar]
- 53.Nagamine M, Yamamoto T, Shigemura J, et al. The psychological impact of the great East Japan earthquake on Japan ground self-defense force personnel: a three-wave, one-year longitudinal study. Psychiatry 2018;81:1–9. 10.1080/00332747.2017.1333340 [DOI] [PubMed] [Google Scholar]
- 54.Osório C, Jones N, Jones E, et al. Combat experiences and their relationship to post-traumatic stress disorder symptom clusters in UK military personnel deployed to Afghanistan. Behav Med 2018;44:131–40. 10.1080/08964289.2017.1288606 [DOI] [PubMed] [Google Scholar]
- 55.Pihl-Thingvad J, Andersen LL, Brandt LPA, et al. Are frequency and severity of workplace violence etiologic factors of posttraumatic stress disorder? A 1-year prospective study of 1,763 social educators. J Occup Health Psychol 2019;24:543–55. 10.1037/ocp0000148 [DOI] [PubMed] [Google Scholar]
- 56.Polusny MA, Erbes CR, Murdoch M, et al. Prospective risk factors for new-onset post-traumatic stress disorder in national guard soldiers deployed to Iraq. Psychol Med 2011;41:687–98. 10.1017/S0033291710002047 [DOI] [PubMed] [Google Scholar]
- 57.Reijnen A, Rademaker AR, Vermetten E, et al. Prevalence of mental health symptoms in Dutch military personnel returning from deployment to Afghanistan: a 2-year longitudinal analysis. Eur Psychiatry 2015;30:341–6. 10.1016/j.eurpsy.2014.05.003 [DOI] [PubMed] [Google Scholar]
- 58.Tracie Shea M, Reddy MK, Tyrka AR, et al. Risk factors for post-deployment posttraumatic stress disorder in national guard/reserve service members. Psychiatry Res 2013;210:1042–8. 10.1016/j.psychres.2013.08.039 [DOI] [PubMed] [Google Scholar]
- 59.Soo J, Webber MP, Gustave J, et al. Trends in probable PTSD in firefighters exposed to the world Trade center disaster, 2001–2010. Disaster Med Public Health Prep 2011;5:S197–203. 10.1001/dmp.2011.48 [DOI] [PubMed] [Google Scholar]
- 60.Stevelink SAM, Jones M, Hull L, et al. Mental health outcomes at the end of the British involvement in the Iraq and Afghanistan conflicts: a cohort study. Br J Psychiatry 2018;213:690–7. 10.1192/bjp.2018.175 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wittchen H-U, Schönfeld S, Kirschbaum C, et al. Traumatic experiences and posttraumatic stress disorder in soldiers following deployment abroad: how big is the hidden problem? Dtsch Arztebl Int 2012;109:559–68. 10.3238/arztebl.2012.0559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Goldmann E, Calabrese JR, Prescott MR, et al. Potentially modifiable pre-, peri-, and postdeployment characteristics associated with deployment-related posttraumatic stress disorder among Ohio army national guard soldiers. Ann Epidemiol 2012;22:71–8. 10.1016/j.annepidem.2011.11.003 [DOI] [PubMed] [Google Scholar]
- 63.HILL AB, Bradford Hill A. The environment and disease: association or causation? Proc R Soc Med 1965;58:295–300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Schünemann H, Hill S, Guyatt G, et al. The grade approach and Bradford Hill's criteria for causation. J Epidemiol Community Health 2011;65:392–5. 10.1136/jech.2010.119933 [DOI] [PubMed] [Google Scholar]
- 65.Nievergelt CM, Maihofer AX, Klengel T, et al. International meta-analysis of PTSD genome-wide association studies identifies sex- and ancestry-specific genetic risk loci. Nat Commun 2019;10:4558. 10.1038/s41467-019-12576-w [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-049651supp001.pdf (81.5KB, pdf)
bmjopen-2021-049651supp002.pdf (102.7KB, pdf)
bmjopen-2021-049651supp003.pdf (442.2KB, pdf)
bmjopen-2021-049651supp004.pdf (58.2KB, pdf)
bmjopen-2021-049651supp005.pdf (109.4KB, pdf)
bmjopen-2021-049651supp006.pdf (31.1KB, pdf)
bmjopen-2021-049651supp007.pdf (42.1KB, pdf)
bmjopen-2021-049651supp008.pdf (47.9KB, pdf)
bmjopen-2021-049651supp009.pdf (42.8KB, pdf)
bmjopen-2021-049651supp010.pdf (42KB, pdf)
bmjopen-2021-049651supp011.pdf (47.6KB, pdf)
bmjopen-2021-049651supp012.pdf (42.4KB, pdf)
bmjopen-2021-049651supp013.pdf (41.9KB, pdf)
bmjopen-2021-049651supp014.pdf (47.5KB, pdf)
bmjopen-2021-049651supp015.pdf (42.7KB, pdf)
bmjopen-2021-049651supp016.pdf (45.1KB, pdf)
bmjopen-2021-049651supp017.pdf (44.2KB, pdf)
bmjopen-2021-049651supp018.pdf (44.4KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as online supplemental information.