Description
Spontaneous coronary artery dissection (SCAD) is an important cause of acute coronary syndrome (ACS), myocardial infarction and sudden death, particularly among young to middle-aged women and individuals with few conventional atherosclerotic risk factors.1 2 The most common precipitant is high physical or emotional stress.3 Stress-induced catecholamine surge during these events has been postulated to lead to shear stress in coronary arteries that, at least partially, contributes to the pathophysiology of SCAD.
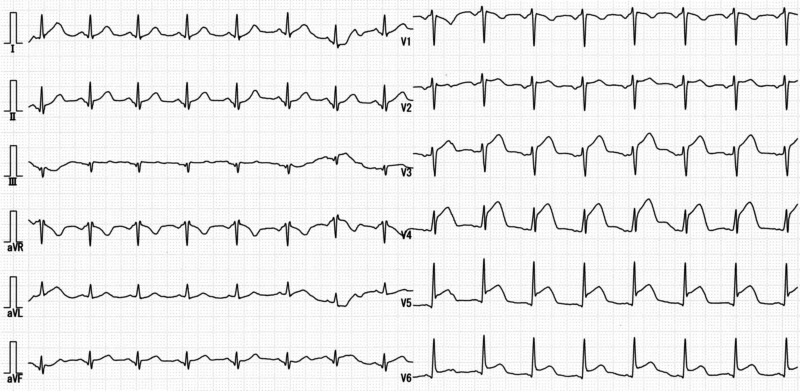
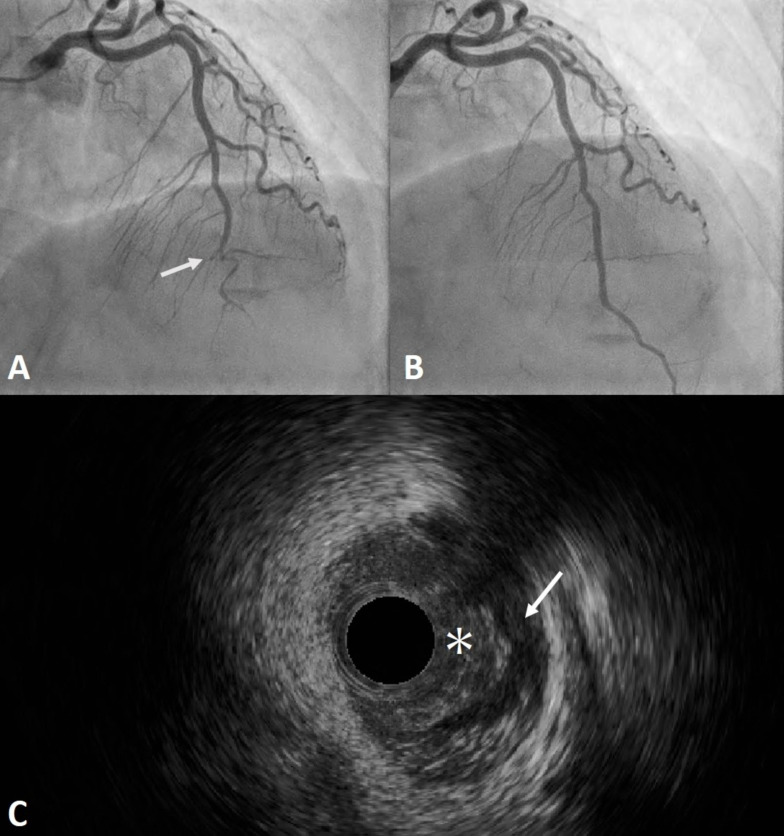
A 52-year-old woman who had a history of hypertension presented to our hospital with chest pain. Although the patient’s grandmother had a myocardial infarction in her 60s, the patient had no history of diabetes, dyslipidaemia or smoking. The chest pain episode occurred during her father’s funeral and she was deeply grieved. Her chest tightness persisted at the time of admission. The pulse rate was regular, at 100 beats/min, and blood pressure was 160/107 mm Hg. Twelve-lead ECG showed ST elevation in leads V3–V6 (figure 1), and emergent coronary angiography was performed. Coronary angiography showed total occlusion in segment 7 of the left anterior descending artery (figure 2A). Intravascular ultrasonography revealed intramural haematoma and intimal flap-like findings (figure 2C). Emergency percutaneous coronary intervention (PCI) using a drug-eluting stent was performed (figure 2B) because the level of troponin was elevated at 0.39 ng/mL (upper limit of normal, <0.04 ng/mL) and chest pain persisted with evidence of ongoing ischaemia.1 Transthoracic echocardiography revealed wall motion of the left ventricular apex was akinetic. Considering that the patient was a middle-aged woman with relatively low cardiovascular risk, she was diagnosed with SCAD (type 2B).4 Dual antiplatelet therapy as well as administration of carvedilol and enalapril was started. The patient was discharged from the hospital without any complications on day 8.
Figure 1.
Twelve-lead ECG shows ST elevation in leads V3–V6.
Figure 2.
(A) Coronary angiography shows total occlusion in segment 7 (arrow) of the left anterior descending artery. (B) Emergent percutaneous coronary intervention using a drug-eluting stent was performed. (C) Intravascular ultrasonography reveals an intramural haematoma (arrow) compressing the true lumen (asterisk).
SCAD is defined as spontaneous formation of an intramural haematoma within the wall of an epicardial coronary artery.1 2 PCI in SCAD has been associated with an increased risk of procedural complications compared with atherosclerotic ACS.3 5 Revascularisation with PCI was the initial treatment for SCAD in 16.7%–47.1% of patients. Reported PCI success rates vary (36.4%–72.5%), but they were substantially lower than that reported in control subjects with atherosclerotic ACS.3–6 Operators should be aware that the risk of complications in PCI is higher than that in atherosclerotic cases and that long stents may be required. Patients with extensive dissections, proximal dissections and no contrast penetration into the false lumen may be at high risk. While a conservative approach to revascularisation in SCAD is optimal where possible, sometimes the clinical presentation requires PCI to improve coronary perfusion and reduce myocardial damage. It is possible to achieve subjective improvements with PCI in most of these high-risk cases.7 There are many similarities in the patient demographics, clinical presentations and predisposing stressors between SCAD and takotsubo syndrome.8 A detailed review of coronary angiography with various imaging modalities, including intravascular imaging and early diagnosis of SCAD, will ultimately change both short-term and long-term management strategies.
Learning points.
Spontaneous coronary artery dissection (SCAD) is an important cause of acute coronary syndrome, myocardial infarction and sudden death, particularly among young to middle-aged women and individuals with few conventional atherosclerotic risk factors.
The most common precipitant is high physical or emotional stress. This is a case report of a 52-year-old woman who presented to our hospital with chest pain, which occurred during her father’s funeral.
Although SCAD has a challenging clinical and angiographic presentation, careful consideration with various imaging modalities, including intravascular imaging as well as a detailed review of coronary angiography, is necessary.
Footnotes
Contributors: JT, YK and AE were involved in the clinical management of the patient. All the authors contributed to drafting the article. JT and KT wrote and edited the manuscript and KT was responsible for overall supervision.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Obtained.
References
- 1.Hayes SN, Kim ESH, Saw J, et al. Spontaneous coronary artery dissection: current state of the science: a scientific statement from the American heart association. Circulation 2018;137:e523–57. 10.1161/CIR.0000000000000564 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hayes SN, Tweet MS, Adlam D, et al. Spontaneous coronary artery dissection. J Am Coll Cardiol 2020;76:961–84. 10.1016/j.jacc.2020.05.084 [DOI] [PubMed] [Google Scholar]
- 3.Saw J, Aymong E, Sedlak T, et al. Spontaneous coronary artery dissection: association with predisposing arteriopathies and precipitating stressors and cardiovascular outcomes. Circ Cardiovasc Interv 2014;7:645–55. 10.1161/CIRCINTERVENTIONS.114.001760 [DOI] [PubMed] [Google Scholar]
- 4.Kim ESH. Spontaneous coronary-artery dissection. N Engl J Med 2020;383:2358–70. 10.1056/NEJMra2001524 [DOI] [PubMed] [Google Scholar]
- 5.Tweet MS, Eleid MF, Best PJM, et al. Spontaneous coronary artery dissection: revascularization versus conservative therapy. Circ Cardiovasc Interv 2014;7:777–86. 10.1161/CIRCINTERVENTIONS.114.001659 [DOI] [PubMed] [Google Scholar]
- 6.Lettieri C, Zavalloni D, Rossini R, et al. Management and long-term prognosis of spontaneous coronary artery dissection. Am J Cardiol 2015;116:66–73. 10.1016/j.amjcard.2015.03.039 [DOI] [PubMed] [Google Scholar]
- 7.Kotecha D, Garcia-Guimaraes M, Premawardhana D, et al. Risks and benefits of percutaneous coronary intervention in spontaneous coronary artery dissection. Heart 2021;107:1398–406. 10.1136/heartjnl-2020-318914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Duran JM, Naderi S, Vidula M, et al. Spontaneous coronary artery dissection and its association with takotsubo syndrome: novel insights from a tertiary center registry. Catheter Cardiovasc Interv 2020;95:485–91. 10.1002/ccd.28314 [DOI] [PubMed] [Google Scholar]