Abstract
Objective:
To evaluate the effectiveness of the transpalatal arch (TPA) as an anchorage device in preventing maxillary molar mesialization during retraction of the anterior teeth after premolar extraction.
Materials and Methods:
This systematic review intended to include patients indicated for upper premolar bilateral extraction and subsequent retraction of anterior teeth, considering the use of TPA as an anchorage tool in one of the treatment groups. The search was systematically performed, up to April 2015, in the following electronic databases: Medline, Embase, and all evidence-based medicine reviews via OVID, Cochrane Library, Scopus, PubMed, and Web of Science. Risk of bias assessment was performed using Cochrane's Risk of Bias Tool for randomized clinical trials (RCTs) and Methodological Index for Nonrandomized Studies (MINORS) for non-RCTs.
Results:
Fourteen articles were finally included. Nine RCTs and five non-RCTs presented moderate to high risk of bias. Only one study investigated the use of TPA in comparison with no anchorage, failing to show significant differences regarding molar anchorage loss. A meta-analysis showed a significant increase in anchorage control when temporary anchorage devices were compared with TPA (mean difference [MD] 2.09 [95% confidence interval {CI} 1.80 to 2.38], seven trials), TPA + headgear (MD 1.71 [95% CI 0.81 to 2.6], four trials), and TPA + utility arch (MD 0.63 [95% CI 0.12 to 1.15], 3 trials).
Conclusion:
Based on mostly moderate risk of bias and with some certainty level, TPA alone should not be recommended to provide maximum anchorage during retraction of anterior teeth in extraction cases.
Keywords: Systematic review, Meta-analysis, Anchorage, Transpalatal arch, Extraction
INTRODUCTION
Orthodontic treatment may require tooth extractions.1 When full retraction of the anterior teeth is required, posterior maximum anchorage control has to be considered.2,3 Recently, temporary anchorage devices (TADs) have been proposed to maximize posterior anchorage.4–6 Transpalatal arch (TPA) has been used for many different orthodontic purposes.7 Previous reports analyzed the value of TPA to control anchorage using finite element analysis.8,9 Their findings showed that TPA did not prevent molars from moving mesially. However, many clinical trials suggested that TPAs could still be used as a secondary anchorage support, with no maximum anchorage requirement.10–13
A recent systematic review concluded that TADs provided better anchorage compared with conventional anchorage devices. However, the sole use of TPA as an anchorage tool was not assessed.14 To the best of our knowledge, there is no systematic review that has evaluated the effectiveness of TPA as an anchorage plan (sole or associated with other anchorage devices). Therefore, the objective of the present study was to systematically review the available literature that used TPA as an anchorage device in orthodontic patients having upper premolar extractions.
MATERIALS AND METHODS
The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) checklist was used as a guideline for conducting and reporting this systematic review and meta-analysis.15
Protocol and Registration
The protocol for this systematic review was registered on PROSPERO (CRD42015017287).
Eligibility Criteria
Population.
Adolescent and adult patients with full permanent dentition undergoing fixed orthodontic treatment with upper bilateral premolar extraction and retraction of anterior teeth.
Intervention.
Patients undergoing orthodontic treatment for upper (first or second) premolar bilateral extraction with subsequent retraction of anterior teeth. The anchorage implemented in these patients should include the use of TPA (sole or associated with another anchorage device) in one of the treatment groups. Studies with the sole use of TPA as a means of treating crossbites or correcting molar relationships in any malocclusion and those with the sole use of TPA as anchorage system in case of impacted teeth were excluded.
Comparison.
The study compared a TPA anchorage system group with a control or another retraction treatment group with any kind of anchorage system.
Outcomes.
Net linear measurements of molar crown mesialization and/or anterior crown retraction were reported. The percentage of mesial molar crown movement at the end of the anterior retraction phase was calculated and reported.
Study design.
Randomized and nonrandomized controlled clinical trials. Excluded articles included animal studies, review articles, abstracts, and discussions.
Information Sources and Search
The following electronic databases were systematically searched up to April 2015: Medline, Embase, and all evidence-based medicine reviews via OVID, Cochrane Library, Scopus, PubMed, and Web of Science. The used keywords included orthodontic anchorage, transpalatal arches (TPAs), or bar or bars. This search strategy was first designed for Medline (Appendix 1) and then adapted for the other databases. A partial gray literature search was performed using the Google Scholar search engine by looking over the first 100 listed hits. No restrictions were applied regarding the language or publication date.
Study Selection
During the selection phase, two reviewers (SD-B and MFNF) independently evaluated the titles and abstracts of the retrieved studies from the database searches using the inclusion criteria. In the second phase, the same reviewers performed assessment of the full-text articles. The reviewers resolved any discrepancies by discussion until consensus.
Data Collection Process
The data were first extracted according to standardized tables. Data was compared for accuracy, and any discrepancy was resolved through the reexamination of the original study until a consensus was reached.
Data Items
The variables extracted from each selected article included sample size, retraction method, type and material of TPA, anchorage device used in control groups, reference lines to which anterior teeth segment retraction and/or molar crown mesialization were measured, superimposition landmarks, percentage of mesial crown molar movement at the end of the anterior retraction phase, and the authors' conclusion.
Outcome
The primary outcome was the molar crown mesial movement during anterior teeth retraction.
Risk of Bias in Individual Studies and Quality of Evidence
Methodological quality appraisal was evaluated according to the Cochrane Collaboration's Risk of Bias tool16 for randomized clinical trials (RCTs). In case of non-RCTs, the Methodological Index for Non-randomized Trials (MINORS)17 was used. An additional summary of the certainty of the conclusions and strength of the evidence was developed using the Grading of Recommendations Assessment, Development and Evaluation (GRADE) approach (Table 1). The quality of evidence was assessed as high, moderate, low, or very low for the outcome mesial crown molar movement.
Table 1.
GRADE Summary of Findings for Meta-Analyses on Molar Mesial Movement During Incisor Retractiona
| Quality Assessment, Outcome: Mean Difference of Molar Mesial Movement During Anterior Retraction | ||||||
| Question: Will the Use of TPA Anchorage Have an Effect on the Mesial Molar Movement During Anterior Teeth Retraction? | ||||||
| No. of Studies According to Meta-Analyses Anchorage Groups |
Study Design |
Risk of Bias |
Inconsistency |
Indirectness |
Imprecision |
Other Considerations |
| 7 (Figure 2) | Randomized trials | Seriousb,c | Not serious | Not serious | Not serious | Strong association |
| 4 (Figure 3) | Observational studies | Seriousb | Not serious | Not serious | Not serious | Strong association |
| 3 (Figure 4) | Observational studies | Seriousb,c | Not serious | Not serious | Not serious | Publication bias strongly suspected |
CI indicates confidence interval; RR, risk ratio.
Inconsistent study design.
Many of these studies did not consider blinding of the participants and outcome assessors.
Table 1.
Extended
| No. of Patients |
Effect |
Quality |
||
| The Use of TPA |
TADs |
Relative (95% CI) |
Absolute (95% CI) |
|
| 158/308 (51.3%) | 150/158 (94.9%) | RR 2.09 (1.80 to 2.38) | 1000 more per 1000 (from 759 more to 1000 more) | □□□□ HIGH |
| 83/153 (54.2%) | 70/153 (45.8%) | RR 1.71 (0.81 to 2.60) | 325 more per 1000 (from 87 fewer to 732 more) | □□◯◯ LOW |
| 39/78 (50.0%) | 39/78 (50.0%) | RR 0.63 (0.12 to 1.15) | 185 fewer per 1000 (from 75 more to 440 fewer) | □◯◯◯ VERY LOW |
Data Synthesis
Data were pooled to provide an estimate of the effectiveness of the TPA using a random-effects model, given that there were more than three trials eligible for a quantitative analysis and considering the expected statistical heterogeneity.16 Random-effects models are preferred when significant differences are expected between patients and evaluation methods. The primary outcome was mesial crown molar movement (molar anchorage loss). For continuous outcomes, the mean difference with standard deviation and 95% confidence intervals were calculated. Clinical heterogeneity was examined by assessing the characteristics of the selected trials, including similarity between interventions, patients, phase of treatment in which intervention was applied, and outcome measures. Publication bias was examined for the trials to be included in a meta-analysis, using a funnel plot by visually assessing the degree of funnel plot asymmetry.18 Statistical heterogeneity across the studies was tested using the T2 and the I2 statistic, with guide for interpretation as follows: 0% to 30%, not important; 30% to 50%, moderate heterogeneity; 50% to 100%, considerable heterogeneity.19,20 The pooled effect estimate was considered significant if P was <.05. A meta-analysis software (The Cochrane Collaboration's software Review Manager, RevMan) was used to perform data analyses.
RESULTS
Study Selection
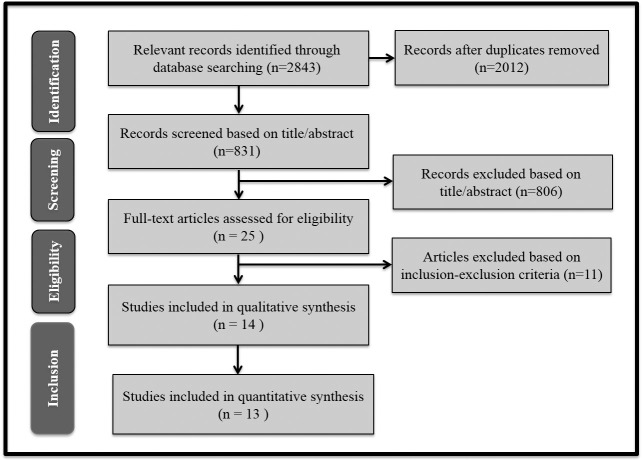
A flowchart illustrating the selection of studies for this systematic review is presented in Figure 1. Twenty-five full texts were obtained for the second phase evaluation, of which 11 articles21–31 were later excluded. The reasons for exclusion are listed in Appendix 2. Finally, 15 articles2,6,10–13,32–40 met the eligibility criteria. A summary of the key methodological data and study characteristics is presented in Tables 2 and 3.
Figure 1.
Flow chart of study selection process.
Table 2.
Summary of Study Characteristics and Results of the Included Studies (TPA Only)a
| Study |
Sample |
Retraction Method |
Other Anchorage Group Type |
Material of TPA Used |
|
| TPA Group |
Other Group |
||||
| Zablocki et al. (2008)2 | N = 30; 11 M, 13.1 ± 1.7 years; 19 F, 13.2 ± 2 years | N = 30; 11 M, 12.9 ± 2 years; 19 F, 14.1 ± 3.3 years | 18 × 25 preangulated Roth appliance and continuous arch wire | No TPA anchorage | Soldered Goshgarian TPA |
| Feldmann and Bondemark (2008)4 | |||||
| (a) | N = 30; 15 M, 15 F; 14.4 ± 1.65 years | N = 30; 15 M, 15 F; 14 ± 1.53 years | Space closure with 0.22-inch slot size and continuous light forces, space closure was carried with active tie-backs using 0.019 × 0.025 SS space closure arch wire | Subperiosteal Onplant | (2.00 × 1.00 mm) SS bar soldered to the maxillary first molar, with 2 mm of space between bar and palate |
| (b) | N = 30 ; 15 M, 15 F; 14 ± 1.53 years | Orthosystem anchorage | |||
| (c) | N = 30; 15 M, 15 F; 14 ± 1.72 years | Headgear | |||
| Wilmes et al. (2009)32 | N = 10, 20.9 years | N = 10, 20.9 years | Not reported | One mini-implant + TPA (0.8 mm) | |
| Liu et al. (2009)10 | N = 17; 3 M, 14 F; 19.71 ± 3.06 years | N = 17; 3 M, 14 F; 21.65 ± 4.49 years | Sliding mechanics and en masse retraction of anterior teeth with power chain and SS ligatures | Mini-screws | Not reported |
| Liu et al. (2009)33 | N = 23; 4 M, 19 F; 17.8 ± 4.3 years | N = 19; 3 M, 16 F; 20.2 ± 5.5 years | Sliding technique | Mini-screws | Not reported |
| Basha et al. (2010)34 | N = 7, 16 ± 1.41 years | N = 7, 17.36 ± 1.35 years | En masse sliding retraction on 0.019 × 0.025 wires | Mini-implants | Not reported |
| Sharma et al. (2012)12 | N = 15; 10 F, 20 M; 17.4 years | N = 15; 10 F, 20 M; 17.4 years | Canine retraction only using 9-mm nitinol closed coil spring of length 9 mm | Mini-screws | 0.9-mm SS wire soldered to the palatal surface of molar bands |
| Gökçe et al. (2012)35 | N = 9; 5 F, 4 M; 15.9 years | N = 9; 5 F, 4 M; 16.7 years | Canine distalization; closed coil spring with a force of 100 g | Mini-screws | 0.9-mm-diameter SS wire was soldered to palatal/lingual region of the molar bands |
| Al-Sibaie et al. (2014)13 | N = 28; 16 F, 12 M; 22.34 ± 4.56 years | N = 28; 19 F, 9 M; 22.34 ± 4.56 years | TPA group: two-step retraction with class II division 1 in mini-implant: sliding en masse retraction of upper anterior teeth | Mini-implant | Passive TPA soldered to U6 bands, 0.9-mm SS, coffin loop centered to the midpalatal line about 1–2 mm distant from palatal surface |
AP, anteroposterior; A-OLp position f the maxillary base; DUM-V, the vertical distance between the distal upper molar point and rotated SN plane; F, female; FH, Franfort horizontal; Is-OLp, position of maxillary incisor; M, male; Ms-OLp, position of maxillary molar; NS, nonsignificant; OLp, occlusal line perpendicular; PTV, pterygoid vertical plane; SS, stainless steel; TPA, transpalatal arch; U1, maxillary central incisor; U6, maxillary first molar; UIT-V, the vertical distance between the upper incisal tip and the rotated SN plane (SN′); Y, line perpendicular to Frankfort horizontal pass through sella.
Mesial molar movement is a calculated as percentage of the molar movement provided in the article.
Table 3.
Summary of Characteristics and Results of the Included Studies (Conventional Anchorage)a
| Study |
Sample |
Retraction Method |
Anchorage Type |
||
| TPA Group |
Other Group |
TPA Group |
Other Group |
||
| Lee et al. (2013)36 | N = 28; 6 M, 22 F; 19.61 ± 7.43 years | N = 23; 0 M, 23 F; 21.50 ± 6.19 years | Six anterior teeth retracted using 0.017 × 0.025-inch nicket titanium arch wires with 0.10 × 0.036-inch SS closed-coil spring | TPA + HG + interarch elastics | Two self- drilling mini-screws in midpalatal suture, fastened with a modified TPA |
| Park et al. (2012)37 | N = 12; 1 M, 11 F; 25.4 ± 8.3 | N = 12; 4 M, 8 F; 18.8 ± 4.7 | Sliding mechanics with 0.019 × 0.025-inch SS wire | TPA and/or HG | Mini-implants |
| Borsos et al. (2012)38 | N = 15; 9 M, 6 F; 1415 ± 1.2 years | N = 15; 4 M, 11 F; 14.3 ± 1.57 years | Two-step retraction using 0.016 × 0.022-inch SS for canine retraction then anterior using helical boot loops, activated 1 mm every 3 weeks | Utility arch combined with a TPA with distal loop | 1.2-mm square steel rigid wire fixed to implant abutment |
| Borsos et al. (2011)39 | N = 9; 3 M, 6 F; 13.3 years | N = 9; 7 M, 2 F; 13.9 years | Canine retraction using only super elastic closed coil spring | 0.017 × 0.025-inch heat-treated SS utility arch combined with a Goshgarian type TPA | Orthosystem midpalatal implant with 1.2-mm SS square TPA and welded to molar bands |
| Kuroda et al. (2009)11 | N = 11 F; 21.8 ± 7.9 years | N = 11 F; 18.5 ± 3.3 years | Nickel titanium coil spring/closing loop mechanics for retracting the four incisors after retracting the canines | Headgear + TPA | Mini-screws placed between maxillary second premolar and first molar |
| Lai et al. (2008)40 | |||||
| (a) | N = 16; 0 M, 16 F; 21.7 ± 2.5 years | N = 15; 1 M, 14 F; 25.1 ± 4.7 years | Sliding mechanics with en masse retraction after partial distalization of the canines and good alignment of the six anteriors | Headgear combined with TPA | Absoanchor mini-implant |
| (b) | N = 9; 2 M, 7 F; 24.1 ± 3.2 years | Miniplates on buccal side of the molars | |||
Mesial molar movement is a calculated percentage of the molar movement provided in the article. APO indicates line between A point on the maxilla and pogonion on the mandible; F, female; HG, headgear; Is-OLp, maxillary central incisor position; M, male; Ms-Olp, maxillary first permanent molar position; MXCI, maxillary central incisor; MXM1, maxillary first molar; NS, nonsignificant; PTV, pterygoid vertical line; TPA, transpalatal arch; U1, maxillary permanent incisors; U6, maxillary permanent molars.
Table 2.
Extended
| Outcome Measures |
Results |
Conclusion |
Superimposition |
|||
| TPA vs Other Group |
Net Δ |
P Value |
% Mesial Molar Movementb |
|||
| TPA |
Other |
|||||
| U1 to Pt A vertical/U6 to FH −2.7/3.2 −2.8/2.4 | U6: 0.8 U1: 0.1 | NS NS | 54.23 | 46.15 | TPA has no significant effect on AP position of maxillary first molars during extraction | Cephalometric cranial base superimposed along basion-nasion line and posterior outline of the cranium |
| Is-OLp minus A-OLp/Ms-OLp minus A-OLp 1.8/1.0 −2.2/0.0 | U1: 0.4 U6: 1.0 | NS .005 | 35 | 0 | Transpalatal bar provided insufficient anchorage throughout the observation period | Occlusal line (OL) and the occlusal line perpendiculare (OL), from the first head film were used as a reference grid; the grid was transferred by superimposition of the tracings on the nasion-sella line (NSL) with sella (s) as registering point |
| 2.8/0.1 | U1: 1.0 U6: 0.9 | NS .007 | 3.4 | |||
| 2.8/1.6 | U1: 1.0 U6: 0.6 | NS NS | 36.3 | |||
| Incisor retraction was not reported; 3D cast superimposition U6: 4.2 ± 1.17 2.05 ± 1.39 | U6: 2.15 | .013 | Skeletal molar anchorage is more effective than conventional anchorage | 3D models superimposed using three-point method | ||
| U1-perpendicular to FH/U6-perpendicular to FH: 4.76/1.47 7.03/0.06 | U1 = 2.27 U6 = 1.41 | .000 .001 | 23.59 | 0.84 | Compared with TPA, mini-screws can provide absolute anchorage | Cephalometric acetate was overlaid on a grid with 1-mm scale |
| U1-Y/U6-Y −4.59/1.65 7.05/0.45 | U1: 2.46 U6: 2.1 | .000 .014 | 26 | 6 | As orthodontic anchorage, mini-screws are different from TPA | Needed by translation |
| U6: 1.73 ± 0.43 0 | 1.73 ± 0.43 | Not reported | Significant amount of anchor loss was noticed in the non–mini-implant group (TPA group) | Pterygoid vertical to maxillary molar in pre and post lateral cephalograms | ||
| U1 movement was not recorded; PTV to centroid point on the upper first molar = 2.48 0.00 | U6 = 2.48 | <.001 | 27.55 | 0.00 | About 2.5 mm mesial movement when using TPA was as minimal movement with mini-screws | PTV line was used as a reference |
| Pterygoid vertical plane and the hook of the canine tooth bracket maxillary canine: 3.71 ± 1.2 4.38 ± 1.3 | U3: 0.67 ± 0.18 | .03 | Use of mini-implants instead of molar anchorage during canine retraction provides a safer anchorage | Superimpositions, the set points in the upper jaw, ANS-PNS (Spina nasalis anterior and posterior) plane, and the anterior wall of the upper jaw bone were superposed | ||
| UIT-V/DUM-V: 0.92/0.38 1.53/0.02 | U1 = 0.61 U6 = 0.36 | <.001 .044 | 29.2 | 1.3 | Retracting upper anterior teeth with moderate to severe protrusion, en masse retraction with mini-screws gave superior results compared to conventional anchorage | After software-based superimposition using a coordinate system, tracing using anterior cranial base |
Table 3.
Extended
| Outcome Measures |
Results |
Conclusion |
Superimposition |
|||
| TPA |
Other Group |
Net Δ |
P Value |
% Mesial Molar Movementb |
||
| Ls-OLP/Ms-OLP: | U1: 2.37 U6: 2.78 | .003 .000 | 44.64 11.01 | Skeletal anchorage achieved greater maxillary incisor retraction and less anchorage loss of the maxillary first molars than did the traditional anchorage | Superimposition on the SN line with the sella as the registering point | |
| −4.5/3.63 | −6.87/0.85 | |||||
| MXCI/MXMI: | U1: 1.62 U6: 0.98 | .000 .045 | 20.9 5.6 | In treatment of class II division 1 malocclusion, orthodontic mini-implant can provide less anchorage loss than conventional anchorage does | 3D virtual model superimposition using 3Txer program | |
| 5.25/1.39 | 6.87/0.41 | |||||
| U1-APo/U6PTV: | U1: 2.13 U6: 0.09 | NS NS | 26.30 22.8 | Conventional maximum anchorage was equivalent to palatal implant during canine retraction and stable enough during whole treatment to achieve typical treatment goals | Not reported | |
| −11.99/4.28 | −14.12/4.19 | |||||
| U6-Ptv: | U6: 0.83 | NS | The increase of the upper first molar-Ptv distance was more than two times greater in the conventional tooth tissue borne than in bone-borne anchorage group | Not reported | ||
| 1.51 | 0.68 | |||||
| U1-PTV/U6-PTV: | U1: 3 U6: 2.3 | .003 .000 | 32.25 7.0 | Orthodontic treatment with either mini-screws or headgear can achieve acceptable results with reduction of overjet and improvement of facial profile; however, anchorage with mini-screws provided more significant improvement with facial profile | 3D superimposition of for pre- and posttreatment dental modes using four reliable points | |
| −6.3/3 | −9.3/0.7 | |||||
| Incisal edge/ occlusal centroid: | U1: 1.4 U6: 1.2 | .003 | 31.25 15.85 | Mini-screws and miniplates achieved better control in the anteroposterior direction than did the traditional headgear appliance | ||
| −5.5/2.5 | 6.9/1.3 | |||||
| 7.3/1.4 | U1: 1.8 U6: 1.1 | .000 | 16.09 | |||
Risk of Bias Assessment
Methodological appraisal of the selected studies is presented in Tables 4 and 5. Nine of the included studies4,10–13,33–35,39 were RCTs, and all of them were considered to present high risk of bias.
Table 4.
Methodological Appraisal of the Selected Studies According to the Cochrane Risk of Bias Tool
| Article |
Sequence Generation |
Allocation Concealment |
Blinding of Participants, Personnel, and Outcome Assessors |
Incomplete Outcome Data |
Selection Outcome Reporting |
Other Sources of Bias |
| Feldmann et al.4 | Low | Low | High | Low | Low | Unclear |
| Liu et al.10 | Low | Unclear | Unclear | Low | Low | Unclear |
| Basha et al.34 | High | High | Unclear | Low | Low | Unclear |
| Sharma et al.12 | Low | Low | High | Low | Low | Unclear |
| Gökçe et al.35 | Unclear | Unclear | Unclear | Low | Low | Unclear |
| Al-Sibaie et al.13 | Low | Low | High | Low | Low | Unclear |
| Liu et al.33 | Low | Unclear | Unclear | Low | Low | Unclear |
| Borsos et al.39 | Low | Unclear | High | Low | Low | Unclear |
| Kuroda et al.11 | Unclear | Unclear | Unclear | Low | Low | Unclear |
Table 5.
Methodological Appraisal of the Selected Studies According to the Methodological Index for Nonrandomized Studies (MINORS) Assessment Toola
| Item |
Zablocki et al.2 |
Wilmes et al.32 |
Lai et al.40 |
Lee et al.36 |
Borsos et al.38 |
Kuroda et al.11 |
| 1. A clear stated aim | 2 | 2 | 2 | 2 | 2 | 1 |
| 2. Inclusion of consecutive patients | 1 | 1 | 1 | 2 | 1 | 0 |
| 3. Prospective collection of data | 2 | 2 | 2 | 2 | 2 | 1 |
| 4. Endpoints appropriate to the aim of the study | 2 | 2 | 2 | 2 | 2 | 2 |
| 5. Unbiased assessment of the study endpoint | 2 | 1 | 2 | 1 | 1 | 0 |
| 6. Follow-up period appropriate to the aim of the study | 2 | 2 | 2 | 2 | 2 | 2 |
| 7. Loss to follow up less than 5% | 1 | 1 | 1 | 2 | 1 | 0 |
| 8. Prospective calculation of the study size | 1 | 0 | 1 | 0 | 0 | 0 |
| 9. An adequate control group | 2 | 2 | 2 | 2 | 2 | 2 |
| 10. Contemporary groups | 1 | 2 | 1 | 2 | 1 | 2 |
| 11. Baseline equivalence of groups | 2 | 2 | 1 | 1 | 2 | 1 |
| 12. Adequate statistical analyses | 2 | 2 | 2 | 2 | 2 | 2 |
| Total | 20 | 19 | 19 | 20 | 18 | 13 |
The items are scored 0 (not reported), 1 (reported but inadequate), or 2 (reported and adequate), with the global ideal score being 16 for noncomparative studies and 24 for comparative studies.14
Six of the included studies2,11,32,36,38,40 were non-RCTs. Study scores ranged from 13 to 20 points out of 24. Significant limitations were identified for most of the studies, such as the retrospective enrollment of the sample2,11,32,40 with nonconsecutive inclusion of patients2,32,36 or unclear reports about inclusion criteria.11,38,40
Study Characteristics
TPA-only anchorage.
Nine studies that used only TPA as an anchorage device during retraction of anterior teeth were finally selected: seven were RCTs6,10,12,13,33,34,35 and two non-RCTs.2,32 Sample sizes ranged from 10 to 30 patients per study group, and age ranged from 13 to 22 years. In most of the studies, which performed en masse retraction, follow-up records were obtained at the end of retraction of the anterior teeth when extraction space was fully closed. Three of these studies12,13,35 that performed two-step retraction evaluated the anchorage capacity of TPA during canine retraction only. All of the included studies had another study group using skeletal anchorage, except for Zablocki et al.,2 in which a non-TPA control group was used.
Conventional anchorage including TPA.
Four studies11,36,37,40 used headgear and TPA in one of the groups. Two studies38,39 reported the combined use of the utility arch and TPA during retraction of anterior teeth. From the total, only one was an RCT and the remaining five studies were non-RCT. Sample sizes ranged from 9 to 28 patients per study group, and age ranged from 13 to 25 years. Follow-up records were obtained at the end of retraction of the anterior teeth and once extraction space was closed. Three of these studies11,38,39 used two-step retraction and evaluated the anchorage capacity of TPA after canine retraction only. The other three studies36,37,40 evaluated the combined conventional anchorage systems during en masse retraction of anterior teeth. All of the included studies had the control group using skeletal anchorage.
Effects of Interventions
Anchorage loss was significantly greater in the groups using TPA alone as an anchorage device, for a total of 158 individuals with a mean loss of anchorage ranging from 1.76 to 4.21 mm (Figure 2), which represents 27% to 54% of the mesial molar crown movement toward the extraction space. Groups using combined conventional anchorage devices also showed higher loss of molar crown anchorage as compared with skeletal anchorage. The conventional anchorage groups presented a mean mesial molar crown movement ranging from 1.26 to 4.28 mm (Figures 3 and 4) or approximately 20% to 40% of the extraction space. The TAD groups presented a mean loss ranging from 0.00 to 2.05 mm (0%–22%). Only one study2 investigated the use of TPA compared with no anchorage, and the values revealed no significant differences between the two groups that reported a similar loss of anchorage of about 45%.
Figure 2.
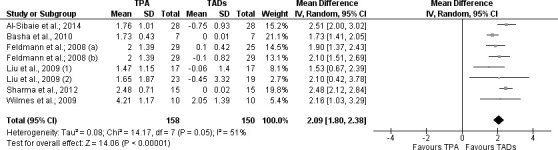
Forest plot of the clinical trials that analyzed effect of TPA vs TADs; confidence interval (CI) of 95%.
Figure 3.
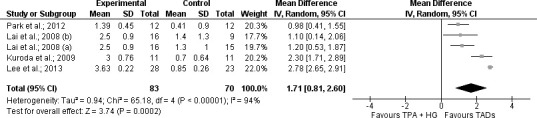
Forest plot of the clinical trials that analyzed effect of TPA and headgear vs TADs; confidence interval (CI) of 95%.
Figure 4.
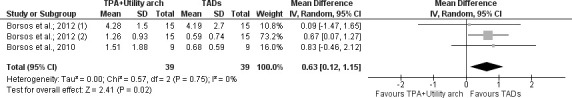
Forest plot of the clinical trials that analyzed effect of TPA and utility arch vs TADs; confidence interval (CI) of 95%.
Eight clinical trials analyzing 308 patients and comparing TPA vs TADs were combined in a meta-analysis (Figures 2–4). The meta-analysis showed a statistically significant reduction in anchorage loss in the TADs group compared with TPA alone (mean difference [MD] 2.09 [95% confidence interval {CI} 1.80 to 2.38], I2 = 51%, seven trials), TPA + headgear (MD 1.71 [95% CI 0.81 to 2.6], I2 = 94%, four trials), and TPA + utility arch (MD 0.63 [95% CI 0.12 to 1.15], I2 = 0%, three trials).
Certainty Levels and Strength of the Evidence
Based on the GRADE recommendations, the body of evidence reporting the mesial molar crown movement ranged from very low to high because of the limitations in the design and the high risk of bias in some of the included studies. Strong evidence is present among the studies that compared TAD against the use of TPA alone. Weak evidence supports the use of TPA even when it is paired with headgear or utility arch to retract either canines or anterior teeth when maximum anchorage is needed.
DISCUSSION
Summary of Evidence
In this review, RCTs and non-RCTs were selected to address the effectiveness of TPA in controlling the maxillary molars anchorage during retraction of anterior teeth in extraction cases. The studies included two categories: TPA sole use as an anchorage mean and TPA used as an adjunct with other conventional anchorage means.
It was suggested that the adjunctive use of TADs should be significantly favored over the sole use of TPA as an anchorage device during retraction when properly indicated. GRADE assessment tool application shows that there is high-quality evidence to support that claim.
The combined use of TPA and headgear did not enhance anchorage when compared with TADs. Even while retracting canines using only TPA and utility arch, adjunctive use of TADs resulted in better anchorage control. The studies considered in that matter varied from very low to low quality, mainly because of the lack of RCTs.
TPA was used in a selected number of clinical trials to test its anchorage ability. In one of the studies, Zablocki et al.2 reported no difference in the molar mesial movement between the control group where no anchorage was planned and TPA-only anchorage group; thus, the TPA did not have any added value with regard to molar anchorage. A consistent finding from all RCTs6,10,13,33–34 implementing en masse retractions is that the TPA did not prevent molar mesial movement.
On the other hand, when TPA was used as the sole anchorage mean to retract canines in a two-step retraction technique, the two related studies12,35 still failed to favor the use of TPA in preventing mesial movement of the molars. In a recent study, El-Bialy et al.41 concluded that TPA alone does not minimize anchorage loss when used with continuous arch mechanics, and they recommended not using the TPA.
The studies reporting the use of TPA as an adjunct anchorage mean with headgear or utility arch during anterior retraction again showed a consistent outcome in which molar anchorage loss was greater in the conventional anchorage group and the incisors were better controlled and more retracted with skeletal anchorage.
However, when only canine retraction was assessed in the combined TPA with other conventional anchorage means, it is suggested11,38,39 that the anchorage achieved was equivalent to that of the skeletal anchorage, as there was no statistically significant difference in the mesial molar movement between both groups, although by the end of the retraction phase of the anterior teeth, skeletal anchorage showed better incisor anteroposterior control. Based on these findings, TPA would be recommended for canine retraction only and only if it were combined with other conventional means. Bearing in mind that canine retraction precedes anterior incisor retraction in most of the extraction cases, the orthodontist then would question the use of TPA as it becomes inconvenient and burdens the clinician with an additional unnecessary procedure. Finally, it has to be mentioned that the use of TPA for other purposes or in less demanding anchorage cases is not questioned in this systematic review.
Limitations
Among the included studies, failure to blind the patients and the clinician was a common, albeit inevitable, flaw. One has to admit that in such clinical trials, blinding the patient or the clinician to the appliances used is hardly achievable. Future studies should ensure that sequence generation and allocation concealment requirements are properly met to further reduce risk of bias. Among the included studies were also non-RCTs. Even though this type of study cannot avoid selection bias, use of consecutively treated patients could at least partially account for this bias.
CONCLUSIONS
TPA alone does not provide sufficient anchorage during en masse or for two-step retraction cases when maximum anchorage is sought (high evidence).
TPA combined with other conventional anchorage means does not provide sufficient anchorage in the en masse retraction of the anterior teeth when maximum anchorage is sought (very low to low evidence).
TPA combined with other conventional anchorage techniques could be considered as an adequate anchorage means in the retraction of the canines only (low evidence).
APPENDIX 1.
Ovid MEDLINE(R) In-Process and Other Nonindexed Citations, Ovid MEDLINE(R) Daily, and Ovid MEDLINE(R) 1946 to Present
| Search Group |
Keyword |
| 1 | Orthodontic anchorage procedures/ |
| 2 | Anchorage.mp. |
| 3 | Anchorages.mp |
| 4 | 2 or 3 |
| 5 | orthodontics/or orthodont*.mp. |
| 6 | 4 and 5 |
| 7 | (transpalatal adj2 (arch or arches or bar or bars)).mp. |
| 8 | or/1,6-7 |
| 9 | 6 and 7 |
| 10 | (retract* or extract*).mp. |
| 11 | 8 and 10 |
| 12 | 9 or 11 |
| Limits | Humans |
APPENDIX 2.
Articles Excluded After Full-Text Evaluation Based on Eligibility Criteria
| Reference |
Reason for Exclusion |
| Alkumru et al.21 | Groups were not divided into anchorage types |
| Benyahia et al.22 | Transpalatal arch (TPA) groups were not specified precisely |
| Chen et al.23 | No control group |
| Cobo et al.24 | Review |
| Feldmann et al.25 | Outcomes not of interest |
| Lee et al.26 | Outcomes not of interest |
| Stivaros et al.27 | Outcomes recorded at alignment phase not retraction |
| Thiruvenkatachari et al.28 | No control group |
| Thiruvenkatachari et al.29 | No control group |
| Upadhyay et al.30 | TPA anchorage group was not specified |
| Xu et al.31 | Anchorage groups were not specified |
REFERENCES
- 1.Saelens NA, De Smit AA. Therapeutic changes in extraction versus non-extraction orthodontic treatment. Eur J Orthod. 1998;20:225–236. doi: 10.1093/ejo/20.3.225. [DOI] [PubMed] [Google Scholar]
- 2.Zablocki HL, McNamara JA, Jr, Franchi L, Baccetti T. Effect of the transpalatal arch during extraction treatment. Am J Orthod Dentofacial Orthop. 2008;133:852–860. doi: 10.1016/j.ajodo.2006.07.031. [DOI] [PubMed] [Google Scholar]
- 3.Ravindra N, Kapila S. Current Therapy in Orthodontics. St Louis, Mo: Mosby; 2010. [Google Scholar]
- 4.Feldmann I, Bondemark L. Anchorage capacity of osseointegrated and conventional anchorage systems: a randomized controlled trial. Am J Orthod Dentofacial Orthop. 2008;133:339.e19–339.e28. doi: 10.1016/j.ajodo.2007.08.014. [DOI] [PubMed] [Google Scholar]
- 5.Chen Y, Kyung HM, Zhao WT, Yu WJ. Critical factors for the success of orthodontic mini-implants: a systematic review. Am J Orthod Dentofacial Orthop. 2009;135:284–291. doi: 10.1016/j.ajodo.2007.08.017. [DOI] [PubMed] [Google Scholar]
- 6.Feldmann I, Bondemark L. Orthodontic anchorage: a systematic review. Angle Orthod. 2006;76:493–501. doi: 10.1043/0003-3219(2006)076[0493:OA]2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Rebellato J. Two-couple orthodontic appliance systems: transpalatal Arches. Semin Orthod. 1995;1:44–54. doi: 10.1016/s1073-8746(95)80088-3. [DOI] [PubMed] [Google Scholar]
- 8.Bobak V, Christiansen RL, Hollister SJ, Kohn DH. Stress-related molar responses to the transpalatal arch: a finite element analysis. Am J Orthod Dentofacial Orthop. 1997;112:512–518. doi: 10.1016/s0889-5406(97)90100-1. [DOI] [PubMed] [Google Scholar]
- 9.Kojima Y, Fukui H. Effects of transpalatal arch on molar movement produced by mesial force: a finite element simulation. Am J Orthod Dentofacial Orthop. 2008;134:335.e1–335.e7. doi: 10.1016/j.ajodo.2008.03.011. [DOI] [PubMed] [Google Scholar]
- 10.Liu YH, Ding WH, Liu J, Li Q. Comparison of the differences in cephalometric parameters after active orthodontic treatment applying mini-screw implants or transpalatal arches in adult patients with bialveolar dental protrusion. J Oral Rehabil. 2009;36:687–695. doi: 10.1111/j.1365-2842.2009.01976.x. [DOI] [PubMed] [Google Scholar]
- 11.Kuroda S, Yamada K, Deguchi T, Kyung HM, Takano-Yamamoto T. Class II malocclusion treated with miniscrew anchorage: comparison with traditional orthodontic mechanics outcomes. Am J Orthod Dentofacial Orthop. 2009;135:302–309. doi: 10.1016/j.ajodo.2007.03.038. [DOI] [PubMed] [Google Scholar]
- 12.Sharma M, Sharma V, Khanna B. Mini-screw implant or transpalatal arch-mediated anchorage reinforcement during canine retraction: a randomized clinical trial. J Orthod. 2012;39:102–110. doi: 10.1179/14653121226878. [DOI] [PubMed] [Google Scholar]
- 13.Al-Sibaie S, Hajeer MY. Assessment of changes following en-masse retraction with mini-implants anchorage compared to two-step retraction with conventional anchorage in patients with class II division 1 malocclusion: a randomized controlled trial. Eur J Orthod. 2014;36:275–283. doi: 10.1093/ejo/cjt046. [DOI] [PubMed] [Google Scholar]
- 14.Jambi S, Walsh T, Sandler J, Benson PE, Skeggs RM, O'Brien KD. Reinforcement of anchorage during orthodontic brace treatment with implants or other surgical methods. Cochrane Database Syst Rev. 2014. 8:CD005098. [DOI] [PMC free article] [PubMed]
- 15.Stewart LA, Clarke M, Rovers M, et al. Preferred Reporting Items for Systematic Review and Meta-Analyses of individual participant data: the PRISMA-IPD statement. JAMA. 2015;313:1657–1665. doi: 10.1001/jama.2015.3656. [DOI] [PubMed] [Google Scholar]
- 16.Higgins JP, Altman DG, Gotzsche PC, et al. The Cochrane Collaboration's tool for assessing risk of bias in randomised trials. BMJ. 2011. 343:d5928. [DOI] [PMC free article] [PubMed]
- 17.Slim K, Nini E, Forestier D, Kwiatkowski F, Panis Y, Chipponi J. Methodological Index for Non-Randomized Studies (MINORS): development and validation of a new instrument. ANZ J Surg. 2003;73:712–716. doi: 10.1046/j.1445-2197.2003.02748.x. [DOI] [PubMed] [Google Scholar]
- 18.Sterne JA, Egger M. Funnel plots for detecting bias in meta-analysis: guidelines on choice of axis. J Clin Epidemiol. 2001;54:1046–1055. doi: 10.1016/s0895-4356(01)00377-8. [DOI] [PubMed] [Google Scholar]
- 19.Lau J, Ioannidis JP, Schmid CH. Quantitative synthesis in systematic reviews. Ann Intern Med. 1997;127:820–826. doi: 10.7326/0003-4819-127-9-199711010-00008. [DOI] [PubMed] [Google Scholar]
- 20.Higgins J, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 21.Alkumru P, Erdem D, Altug-Atac AT. Evaluation of changes in the vertical facial dimension with different anchorage systems in extraction and non-extraction subjects treated by Begg fixed appliances: a retrospective study. Eur J Orthod. 2007;29:508–516. doi: 10.1093/ejo/cjm051. [DOI] [PubMed] [Google Scholar]
- 22.Benyahia H, Lahlou K, Rerhrhaye W, Zaoui F, Aalloula E. Loss of molar anchorage: quantitative evaluation with a method of structural superposition. Odontostomatol Trop. 2007;30:37–44. [PubMed] [Google Scholar]
- 23.Chen W, Chen RJ, Shen G. The effects of combined reverse Nance and TPA on reinforcement of anchorage [in Chinese] Shanghai Kou Qiang Yi Xue. 2004;13:262–265. [PubMed] [Google Scholar]
- 24.Cobo JM, Diaz B, de Carlos F. Maintaining anchorage with a combination Nance-Goshgarian transpalatal arch. J Clin Orthod. 1998;32:681. [PubMed] [Google Scholar]
- 25.Feldmann I, List T, Bondemark L. Orthodontic anchoring techniques and its influence on pain, discomfort, and jaw function—a randomized controlled trial. Eur J Orthod. 2012;34:102–108. doi: 10.1093/ejo/cjq171. [DOI] [PubMed] [Google Scholar]
- 26.Lee J, Miyazawa K, Tabuchi M, Sato T, Kawaguchi M, Goto S. Effectiveness of en-masse retraction using midpalatal miniscrews and a modified transpalatal arch: treatment duration and dentoskeletal changes. Korean J Orthod. 2014;44:88–95. doi: 10.4041/kjod.2014.44.2.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Stivaros N, Lowe C, Dandy N, Doherty B, Mandall NA. A randomized clinical trial to compare the Goshgarian and Nance palatal arch. Eur J Orthod. 2010;32:171–176. doi: 10.1093/ejo/cjp075. [DOI] [PubMed] [Google Scholar]
- 28.Thiruvenkatachari B, Ammayappan P, Kandaswamy R. Comparison of rate of canine retraction with conventional molar anchorage and titanium implant anchorage. Am J Orthod Dentofacial Orthop. 2008;134:30–35. doi: 10.1016/j.ajodo.2006.05.044. [DOI] [PubMed] [Google Scholar]
- 29.Thiruvenkatachari B, Pavithranand A, Rajasigamani K, Kyung HM. Comparison and measurement of the amount of anchorage loss of the molars with and without the use of implant anchorage during canine retraction. Am J Orthod Dentofacial Orthop. 2006;129:551–554. doi: 10.1016/j.ajodo.2005.12.014. [DOI] [PubMed] [Google Scholar]
- 30.Upadhyay M, Yadav S, Nagaraj K, Patil S. Treatment effects of mini-implants for en-masse retraction of anterior teeth in bialveolar dental protrusion patients: a randomized controlled trial. Am J Orthod Dentofacial Orthop. 2008;134:18–29.e1. doi: 10.1016/j.ajodo.2007.03.025. [DOI] [PubMed] [Google Scholar]
- 31.Xu TM, Zhang X, Oh HS, Boyd RL, Korn EL, Baumrind S. Randomized clinical trial comparing control of maxillary anchorage with 2 retraction techniques. Am J Orthod Dentofacial Orthop. 2010;138:544.e1–9. doi: 10.1016/j.ajodo.2009.12.027. [DOI] [PubMed] [Google Scholar]
- 32.Wilmes B, Olthoff G, Drescher D. Comparison of skeletal and conventional anchorage methods in conjunction with pre-operative decompensation of a skeletal class III malocclusion. J Orofac Orthop. 2009;70:297–305. doi: 10.1007/s00056-009-9909-y. [DOI] [PubMed] [Google Scholar]
- 33.Liu YH, Liu J, Li Q, Ding WH. An efficacy comparison between mini-screw implant and transpalatal arch on dentofacial morphology in extraction cases [in Chinese] Zhonghua Kou Qiang Yi Xue Za Zhi. 2009;44:454–459. [PubMed] [Google Scholar]
- 34.Basha AG, Shantaraj R, Mogegowda SB. Comparative study between conventional en-masse retraction (sliding mechanics) and en-masse retraction using orthodontic micro implant. Implant Dent. 2010;19:128–136. doi: 10.1097/ID.0b013e3181cc4aa5. [DOI] [PubMed] [Google Scholar]
- 35.Gökçe SM, Görgülü S, Gökçe HS, Yildirim E, Saǧdiç D. Comparison of conventional molar tooth anchorage and micro-implant anchorage regarding canine retraction in treatments with extraction. Gulhane Med J. 2012;54:205–211. [Google Scholar]
- 36.Lee J, Miyazawa K, Tabuchi M, Kawaguchi M, Shibata M, Goto S. Midpalatal miniscrews and high-pull headgear for anteroposterior and vertical anchorage control: cephalometric comparisons of treatment changes. Am J Orthod Dentofacial Orthop. 2013;144:238–250. doi: 10.1016/j.ajodo.2013.03.020. [DOI] [PubMed] [Google Scholar]
- 37.Park HM, Kim BH, Yang IH, Baek SH. Preliminary three-dimensional analysis of tooth movement and arch dimension change of the maxillary dentition in Class II division 1 malocclusion treated with first premolar extraction: conventional anchorage vs. mini-implant anchorage. Korean J Orthod. 2012;42:280–290. doi: 10.4041/kjod.2012.42.6.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Borsos G, Voko Z, Gredes T, Kunert-Keil C, Vegh A. Tooth movement using palatal implant supported anchorage compared to conventional dental anchorage. Ann Anat. 2012;194:556–560. doi: 10.1016/j.aanat.2012.08.003. [DOI] [PubMed] [Google Scholar]
- 39.Borsos G, Jianu R, Vegh A. Comparison of bone-borne and tooth tissue-borne anchorage during the maxillary canine retraction in growing patients: a randomised clinical trial. Timisoara Med J. 2011;61:98–101. [Google Scholar]
- 40.Lai EH, Yao CC, Chang JZ, Chen I, Chen YJ. Three-dimensional dental model analysis of treatment outcomes for protrusive maxillary dentition: comparison of headgear, miniscrew, and miniplate skeletal anchorage. Am J Orthod Dentofacial Orthop. 2008;134:636–645. doi: 10.1016/j.ajodo.2007.05.017. [DOI] [PubMed] [Google Scholar]
- 41.Alhadlaq A, Alkhadra T, El-Bialy T. Anchorage condition during canine retraction using transpalatal arch with continuous and segmented arch mechanics. Angle Orthod. 2016;86:380–385. doi: 10.2319/050615-306.1. [DOI] [PMC free article] [PubMed] [Google Scholar]