Abstract
Objective:
To conduct an objective assessment of the level of compliance in young patients prescribed various types of removable appliances and to determine the influence of device type, treatment duration, and patient age, gender, psychological maturity, and awareness of monitoring on compliance.
Materials and Methods:
A total of 30 patients were fitted with either a class 2 (Frankel or bionator) or a class 3 (face mask) removable appliance, each bearing a compliance indicator chip, and they were instructed to wear them for 13 hours per day. Compliance was monitored by means of the sensor for an average of 8 months. Of the patients, 14 were informed that their appliance was fitted with a monitoring sensor, and 16 were not. The psychological maturity of all patients was assessed on the Nowicki-Strickland Locus of Control Scale, and the effect on compliance of this score as well as the patient- and treatment-related variables considered were determined via statistical analysis
Results:
The mean compliance recorded by the chips was 8.6 ± 2.9 hours, far lower than the 13 hours prescribed, and younger patients showed significantly greater compliance than adolescents (P < .01). However, no significant differences in compliance were found between intra- and extraoral appliances, and neither gender, psychological scores, treatment duration, nor awareness of being monitored had any significant effect.
Conclusions:
Compliance is generally very poor in young patients, regardless of their gender and psychological maturity. Although awareness of monitoring does not appear to boost compliance, such systems may be a valuable means of providing a dentist with objective information regarding their patients' compliance.
Keywords: Compliance, Compliance indicator, TheraMon system, Removable appliance
INTRODUCTION
The success of orthodontic treatment using removable appliances is reliant on a number of factors, including accurate and individualized diagnosis, appliance selection, and prescription, that is, how many hours the device must be worn per day. However, the skill and experience of the orthodontist count for very little without adequate patient compliance.1,2
For maximum efficacy, orthopedic devices (such as extraoral traction and the protraction mask) must also be worn day and night.3–5 Nevertheless, in today's society the demands of schooling and extracurricular activities and the social pressures for esthetic conformity placed on young people mean that a more realistic prescription is between 10 and 15 hours of every 24 hours (ie, ref. 6).
However, there are many factors that may affect the willingness of young people to play such an active role in their treatment, among which their age, gender, maturity, motivation, and personality traits as well as the type of device they are asked to wear have all been investigated.6–8 The resulting literature appears to indicate that it is patients who view their malocclusion as “ugly” and psychologically disabling and see orthodontic treatment as a solution to these problems who are most motivated and compliant.9,10 More outgoing children with high self-esteem are more easily involved in their treatment than those who are introverted and hostile. Age and gender also seem to affect compliance, and many have found that female patients are more diligent than males and that prepubescents collaborate more than adolescents.11 However, these facts can merely serve as indicators and cannot be used to determine whether an individual patient will comply to a sufficient degree.
Likewise self-reporting questionnaires fail to adequately assess compliance, with the patients themselves proving to be less than realistic (or truthful) monitors of their behavior. Parents too fail in this regard, tending to overestimate the amount of time their child wears their appliance as do the orthodontists themselves.12
Among such sensors designed to monitor compliance objectively,13–16 the TheraMon System (Dentaurum Italia Spa, Bologna, Italy) has proved to be particularly reliable, with a discrepancy between real and measured compliance of only 7.92 minutes per day.17 The TheraMon micro sensor also has the added advantages of being especially small in size (13 × 9 × 4.5 mm; Figure 1). It works by measuring the temperature of its surroundings every 15 minutes, and the data it records are transmitted to a dedicated workstation by radiofrequency identification technology and displayed by proprietary software on a simple graph. By these means it is easy to see how long the appliance has spent outside the oral cavity (temperature range 34–35°C), or whether it has been tampered with. Thus the system can give the orthodontist a clear picture of a patient's compliance profile, providing information as to the mean compliance (hours/day) during the course of each day or a throughout a selected period16,18 (Figure 2).
Figure 1.
TheraMon compliance monitoring chip.
Figure 2.
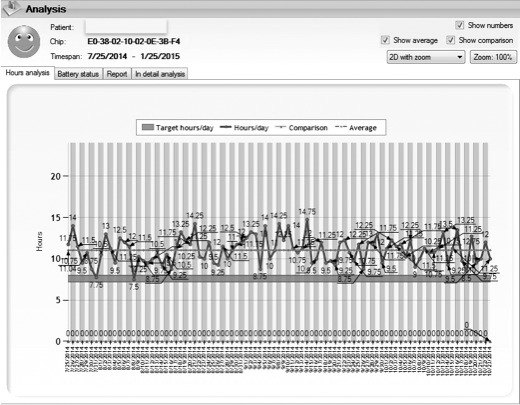
Example compliance profile.
Authors have used TheraMon micro sensors to study compliance with various types of removable appliances,19–24 and functional appliances and retainers have been investigated at prescriptions ranging from 8 hours to 15 hours per day in patients aged between 6 to 16 years, and in all cases the chips revealed compliance far lower than that required. However, no similar study has yet been conducted on extraoral orthopedic devices, and there is as yet no consensus as to how age and gender affect compliance with various types of intra- and extraoral appliances. Furthermore, more information is required as to whether specific measures of psychological maturity and/or the awareness of being monitored can predict compliance.
Hence we set out to objectively monitor compliance in young patients fitted with various types of intra- and extraoral removable functional and orthopedic orthodontic appliances and to determine the influence of device type, treatment duration, and patient age, gender, psychological maturity, and awareness of monitoring on compliance. The null hypothesis was that there would be no statistically significant difference in the degree of compliance between boys and girls, age groups, psychological maturity, or months of treatment in patients who know and do not know that they have a monitoring device fitted.
MATERIALS AND METHODS
Ethical approval was obtained from the local research ethics committees (communication no. 5, code 111546). A total of 30 consecutive patients (16 boys and 14 girls) aged between 6 and 15 years (mean age 9.8 years) treated at the Ferrara University Orthodontic Clinic formed the initial sample.
Of these, 14 patients (mean age 9.8 years) were treated for normo/hypodivergent class II skeletal malocclusion via intraoral functional appliance: the Frankel3 in 11 and the bionator in 3. The other 16 patients (mean age 10.0 years), who presented with class III skeletal malocclusion, were treated using rapid palatal expanders and extraoral protraction masks.
All removable appliances were fitted with a TheraMon chip before being given to the patients. To enable the micro sensor to reveal when the device was in place (ie, at body temperature), it was either embedded in the acrylic resin of the device (Figures 3 and 4) or, in the case of the protraction mask, cemented to the inner surface of the forehead support (Figure 5).
Figure 3.

TheraMon chip embedded in the Frankel.
Figure 4.
TheraMon chip embedded in the bionator.
Figure 5.
TheraMon chip embedded in the forehead rest of the face mask.
Before beginning treatment, each patient underwent psychological testing via the Nowicki-Strickland Locus of Control Scale.25,26 This scale features 40 questions designed to measure a child's or a teenager's beliefs in his or her ability to control his or her own life (locus of control) and has already been used in other studies to estimate the propensity for compliance.27 Low scores (1–7) correspond to a high degree of perceived control, whereas high scores (15–40) correspond to a low degree of perceived control.
Each patient was then given their appliance and instructed how to wear it, in particular that it had to be worn for 13 hours per day, that is, all night and as many hours as possible during the afternoon. A total of 14 randomly selected patients were informed that their appliance had been fitted with a sensor to accurately monitor their compliance, whereas 16 were kept blind to this fact for the duration of their treatment.
At each monthly check-up, the data recorded by the sensor were downloaded onto the workstation, and the readout graphs were generated. Patients who knew that they were being monitored were shown their data, and when called for asked to improve their compliance. Patients who did not know they were being monitored were not shown their data, and motivational advice was given on the basis of the observed clinical progress.
The mean observation period was 8 months (range 2–16 months). All recorded data were transcribed onto a Microsoft Excel file (Microsoft Excel 2007; Microsoft Corp., Redmond, Wash.) and analyzed statistically using Student's t-test (P < .05). Only the relationship between locus-of-control scores and compliance was analyzed by means of a linear correlation test. Parameters considered were the mean compliance of the overall sample and differences ascribable to prescription, type of appliance, observation interval, gender, age, psychological test scores, and awareness of being monitored.
RESULTS
When prescribed 13 hours a day, the mean compliance time revealed in the sample population of removable appliance patients was 8.6 ± 2.9 hours, that is, 65% of that required. Although mean compliance was higher in the intraoral functional appliance group (Frankel and bionator) than with extraoral orthopedic appliances (face mask), specifically 9.5 ± 2.5 hours with respect to 8.0 ± 3.2 hours, the difference was not found to be statistically significant. However, the difference between the two intraoral appliances considered was statistically significant, with the bionator being worn on average 12.6 ± 1.8 hours of 13 hours, that is, 97% of the prescription. This compares favorably with both the Frankel (8.6 ± 1.9 hours) and the protraction mask (8.0 ± 3.2 hours; Table 1).
Table 1.
Compliance With Removable Appliances and Statistical Significancea
| Category |
n |
Mean Compliance (Hours per Day) |
SD |
% Compliance |
P Value |
Significance |
| Appliance type | .2 | NS | ||||
| Intraoral | 14 | 9.5 | 2.5 | 72.9 | ||
| Extraoral | 16 | 8.0 | 3.2 | 61.5 | ||
| Appliance type | ||||||
| Frankel | 11 | 8.6 | 1.9 | 66.3 | PM vs FK: .64 | NS |
| Bionator | 3 | 12.6 | 1.8 | 97.1 | PM vs BI: .002 | S |
| Face mask | 16 | 8.0 | 3.2 | 61.5 | FK vs BI: .006 | S |
| Gender | .07 | NS | ||||
| Boy | 16 | 7.8 | 3.4 | 60.0 | ||
| Girl | 14 | 9.7 | 1.9 | 74.6 | ||
| Age | 6–8 y vs 12–15 y: .012 | S | ||||
| 6–8 | 7 | 10.4 | 1.6 | 80.0 | ||
| 9 | 9 | 8.8 | 4.1 | 67.7 | ||
| 10–11 | 8 | 7.9 | 3.1 | 60.8 | ||
| 12–15 | 6 | 7.7 | 1.2 | 59.2 | ||
| Observation period | ||||||
| Month 1 | 30 | 8.4 | 3.2 | 64.6 | 1st month vs 5th month: .16 | NS |
| Month 2 | 30 | 9.3 | 3.8 | 71.5 | ||
| Month 3 | 28 | 9.1 | 2.9 | 70.0 | ||
| Month 4 | 25 | 8.8 | 3 | 67.7 | ||
| Month 5 | 22 | 9.4 | 2 | 72.3 | 5th month vs 8th month: .25 | NS |
| Month 6 | 15 | 9.0 | 2.4 | 68.9 | ||
| Month 7 | 11 | 8.4 | 2.1 | 64.6 | ||
| Month 8 | 10 | 8.1 | 3 | 62.6 | ||
| Psychological maturity | ||||||
| High control | 2 | 9.9 | 1.4 | 76.2 | HC vs MC: .92 | NS |
| Medium control | 13 | 8.7 | 3.1 | 67.0 | HC vs LC: .77 | NS |
| Low control | 15 | 8.5 | 3.1 | 65.3 | MC vs LC: .84 | NS |
| Awareness monitoring | .2 | NS | ||||
| Informed | 14 | 9.4 | 2.6 | 72.4 | ||
| Not informed | 16 | 8.1 | 3.2 | 61.9 |
SD indicates standard deviation; NS, not significant; S, significant (P < .05); FM, face mask; FK, Frankel; BI, bionator; HC, high control; MC, medium control; and LC, low control.
As shown in Figure 6, the mean compliance remained largely stable during the first 5 months of treatment after a slight rise from the first (8.4 ± 3.2 hours) to the second month (9.3 ± 3.8 hours). From the fifth to eighth month, however, the compliance tended to progressively diminish, although no statistically significant differences were found between the monthly figures (Table 1).
Figure 6.
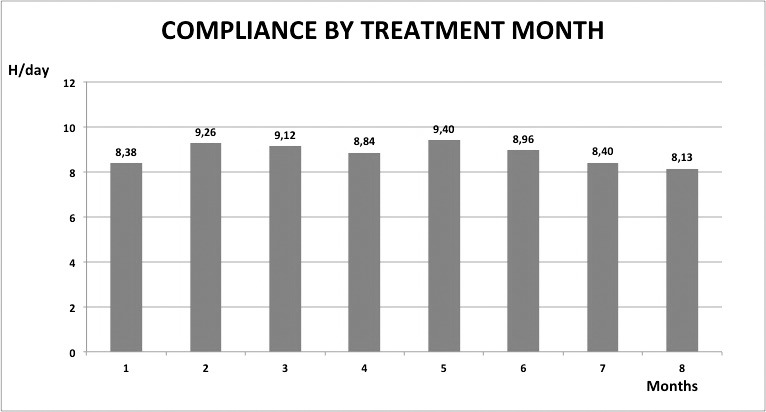
Compliance trend during the first 8 months of treatment.
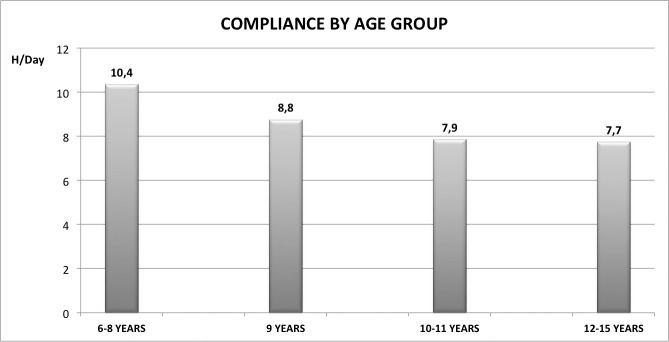
Likewise, there was no statistically significant difference between genders, although girls did tend to be slightly more compliant than boys (respectively, 75% to 60% of the prescribed 13 hours, P = .07; Table 1). When the sample was subdivided by age, however, it became evident that the compliance decreased with increasing age (Figure 7), and the difference between the group of 6- to 8-year-olds and the group of 12- to 15-year-olds was statistically significant (Table 1).
Figure 7.
Compliance across the age ranges.
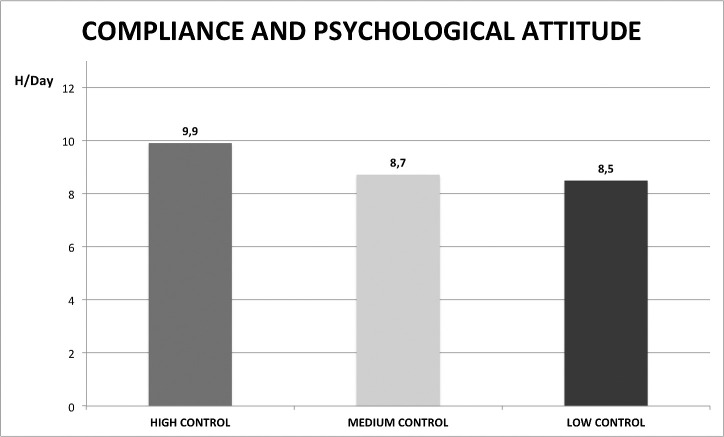
With regard to the psychological parameters, as shown in Table 1 there was no significant difference in mean compliance between those patients aware (9.4 ± 2.6 hours per day) and those not aware (8.1 ± 3.2 hours per day) that their appliances had been fitted with a monitoring sensor. In the Nowicki-Strickland test, two patients were allocated to the high locus-of-control group (score 1–7), 13 to the medium-control group (score 8–14), and 15 to the low-control group (score 15–40). Although the high-control group displayed greater compliance than both the medium and high groups, following a diminishing trend (Figure 8), no difference between the three groups was statistically significant (Table 1).
Figure 8.
Compliance and psychological maturity scores on the Nowicki-Strickland Locus of Control Scale.
DISCUSSION
In recent years, clinicians have become able to objectively monitor compliance with removable appliances during treatment by means of micro sensors. Studies on the TheraMon compliance monitoring system show that compliance is invariably less than that requested by the orthodontist,19–24 and our study in particular revealed a compliance of 8.6 ± 2.9 hours per day when 13 hours' wearing time was prescribed. This is in line with the literature in which compliance never exceeds 7 to 9 hours of the prescribed 8 to 15 hours per day,19–24 indicating that only nocturnal wear can be predicted with any degree of certainty. Indeed, Schäfer et al.24 found that compliance was only close to that required (ie, more than 12 hours per day) in 7% of patients, and Schott and Ludwig22 emphasized that 25% of patients wore their appliance for much less than 7 hours, thereby severely jeopardizing the likelihood of obtaining a successful clinical outcome.
The degree of compliance does not appear to be related to the type of appliance, as Schott et al.21 found comparably low compliance in both active (functional) and passive (Hawley retainer) appliances. Our data enabled us to confirm this conclusion because no statistically significant difference in compliance was observed between different types of intraoral devices or between intraoral and extraoral appliances. Indeed, although one appliance, the bionator, did appear to show better collaboration than the others, only three patients of our sample were treated by means of this device, and it is likely that our data on this parameter was skewed as a result.
In our sample, compliance remained fairly stable during the first 8 months of treatment, although it did begin to diminish slightly (but not significantly) from the fifth month onward. This mirrors findings by Schott et al.,21 who found a slightly increased mean compliance in the second treatment trimester, a peak in the third trimester, and a slight, but not significant, reduction in the fourth.
The literature is also consistent with our findings that correlate compliance with patient age, specifically that the younger the patient, the greater their degree of compliance. Indeed, our 6- to 8-year-old patients had a mean compliance of 10.4 hours per day, significantly greater than the 7.7 hours we recorded in 12- to 15-year-olds. Likewise, Tsomos et al.23 and Schäfer et al.24 found that 7-year-olds wore their appliance for up to 12 hours per day, whereas 15-year-olds showed less than 8.5 hours per day.
However, as yet there is no consensus as to the effect of gender on compliance. That being said, girls do not appear to be more compliant. Indeed, of the many studies to investigate this potential link, one showed significantly greater compliance in girls,24 whereas two others merely recorded a similar trend,21,23 which did not, however, reach statistical significance. In our sample too, girls showed slightly, although not significantly, greater compliance than boys (9.7 hours and 7.8 hours, respectively; P = .07).
Compliance has long been thought to be linked to psychological factors such as the level of maturity, although conclusive proof has not yet been forthcoming. Although there does appear to be a discernible relationship between compliance and Nowicki-Strickland Locus of Control scores, neither we nor other authors27 have been able to show a statistically significant correlation, even if none of them had used an objective device for measuring the compliance. In fact, it would be too reductive to predict compliance on the basis of patient maturity alone because it is dependent also on other external and environmental factors.
In fact, when the TheraMon chip was launched, it was hoped that it would incentivize patient compliance, but we show that awareness of being monitored had little effect on it. Although the group that knew they were being monitored did prove more compliant than those who did not (9.4 hours with respect to 8 hours, difference not significant), even they came nowhere near the prescribed figure of 13 hours per day. This confirms analogous findings by Paulus et al.20 Nevertheless, despite their inability to act to incentivize compliance, such monitoring systems represent a valid aid to communication between the orthodontist, patient, and patient's family. Indeed, they can reveal not only how many hours per day an appliance is worn but also how a patient's compliance pattern changes over time, which can enable targeted motivation. For example, if the readout shows that a patient wears their appliance all night, but not during the day, nocturnal wear can be praised and daytime wear can be encouraged. Similarly, if a patient's compliance profile shows that they neglect to wear their appliance for several days, seeking to make up for lost time by wearing it round the clock on others, they can be educated as to the relative benefits of compliance, with an individualized psychological approach. Furthermore, a detailed but comprehensible graph makes it easier for a clinician to communicate with a patient's parents who, it has been shown,12 have a very unrealistic perception of their child's compliance. Moreover, such systems may also provide grounds for the defense in medicolegal suits arising from treatment failure as a result of poor patient compliance.
Because this is a pilot study based on 30 consecutive patients, a larger sample for further studies is needed to have stronger statistical evidence on patient compliance with removable appliances.
CONCLUSIONS
The null hypothesis must be rejected in part.
Compliance with removable appliances is very poor at 65% of the 13 hours prescribed and is likely to compromise the efficacy of orthodontic treatment.
There is no difference in compliance between intraoral and extraoral appliances.
Compliance is stable during the first 5 months and then diminishes slightly, albeit not statistically so.
There is no statistically significant difference between boys and girls.
Younger children (6–8 years of age) are significantly more compliant than adolescents (12–15 years of age).
Patient maturity, as measured on the Nowicki-Strickland Locus of Control Scale, cannot predict the degree of compliance with removable appliances.
Awareness of monitoring does not incentivize patients to comply.
Compliance monitoring provides objective data that can be used by the orthodontist to check the efficacy of motivational input, communicate with the family, and safeguard against medicolegal suits.
Further studies should focus on how best to incentivize compliance to increase the efficacy of treatment with removable appliances.
REFERENCES
- 1.Miethke RR, Wronski C. What can be achieved with removable orthodontic appliances? J Orofacial Orthopedics. 2009;70:185–199. doi: 10.1007/s00056-009-0818-x. [DOI] [PubMed] [Google Scholar]
- 2.Casutt C, Pancherz H, Gawora M, Ruf S. Success rate and efficiency of activator treatment. Eur J Orthod. 2007;29:614–621. doi: 10.1093/ejo/cjm066. [DOI] [PubMed] [Google Scholar]
- 3.Perillo L, Cannavale R, Ferro F, Franchi L, Masucci C, Chiodini P, Baccetti T. Meta-analysis of skeletal mandibular changes during Frankel appliance treatment. Eur J Orthod. 2011;33:84–92. doi: 10.1093/ejo/cjq033. [DOI] [PubMed] [Google Scholar]
- 4.Jacobs T, Sawaengkit P. National Institute of Dental and Craniofacial Research efficacy trials of bionator Class II treatment: a review. Angle Orthod. 2002;72:571–575. doi: 10.1043/0003-3219(2002)072<0571:NIODAC>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Cordasco G, Matarese G, Rustico L, Fastuca S, Caprioglio A, Lindauer SJ, Nucera R. Efficacy of orthopedic treatment with protraction facemask on skeletal Class III malocclusion: a systematic review and meta-analysis. Orthod Craniofac Res. 2014;17:133–143. doi: 10.1111/ocr.12040. [DOI] [PubMed] [Google Scholar]
- 6.Schott TC, Goz¨ G. Young patients'attitudes toward removable appliance wear times, wear-time instructions and electronic wear-time measurements—results of a questionnaire study. J Orofac Orthop. 2010;71:108–116. doi: 10.1007/s00056-010-9925-y. [DOI] [PubMed] [Google Scholar]
- 7.Cucalon A, Smith RJ. Relationship between compliance by adolescent orthodontic patients and performance on psychological tests. Angle Orthod. 1990;60:107–114. doi: 10.1043/0003-3219(1990)060<0107:RBCBAO>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 8.Bos A, Hoogstraten J, Prahl-Andersen B. The theory of reasoned action and patient compliance during orthodontic treatment. Community Dent Oral Epidemiol. 2005;33:419–426. doi: 10.1111/j.1600-0528.2005.00241.x. [DOI] [PubMed] [Google Scholar]
- 9.Verdecchia F, Bee M, Lombardo L, Sgarbanti C, Gracco A. Influence of anterior tooth alignment on peer perception in 8- to 10-year-old children. Eur J Orthod. 2011;33:155–160. doi: 10.1093/ejo/cjq049. [DOI] [PubMed] [Google Scholar]
- 10.Lombardo L, Berveglieri C, Guarneri MP, Siciliani G. Anterior dental alignment and smile: perception and sensations in a sample of 8- to 10- year-old children and their parents. Orthodontics (Chic.) 2011;12:366–377. [PubMed] [Google Scholar]
- 11.Weiss J, Eiser HM. Psychological timing of orthodontic treatment. Am J Orthod. 1977;72:198–204. doi: 10.1016/0002-9416(77)90061-6. [DOI] [PubMed] [Google Scholar]
- 12.Bos A, Kleverlaan CJ, Hoogstraten J, Prahl-Andersen B, Kuitert R. Comparing subjective and objective measures of headgear compliance. Am J Orthod Dentofacial Orthop. 2007;132:801–805. doi: 10.1016/j.ajodo.2006.01.041. [DOI] [PubMed] [Google Scholar]
- 13.Cureton SL, Regennitter F, Orbell MG. An accurate, inexpensive headgear timer. J Clin Orthod. 1991;25:749–754. [PubMed] [Google Scholar]
- 14.Kyriacou PA, Jones DP. Compliance monitor for use with removable orthodontic headgear appliances. Med Biol Eng Comput. 1997;35:57–60. doi: 10.1007/BF02510393. [DOI] [PubMed] [Google Scholar]
- 15.Sahm G, Bartsch A, Witt E. Micro-electronic monitoring of functional appliance wear. Eur J Orthod. 1990;12:297–301. doi: 10.1093/ejo/12.3.297. [DOI] [PubMed] [Google Scholar]
- 16.Ackerman MB, McRae MS, Longley WH. Microsensor technology to help monitor removable appliance wear. Am J Orthod Dentofacial Orthop. 2009;135:549–551. doi: 10.1016/j.ajodo.2008.06.021. [DOI] [PubMed] [Google Scholar]
- 17.Schott TC, Göz G. Applicative characteristics of new microelectronic sensors Smart Retainer® and TheraMon® for measuring wear time. J Orofac Orthop. 2010;71:339–347. doi: 10.1007/s00056-010-1019-3. [DOI] [PubMed] [Google Scholar]
- 18.Schott TC, Ludwig B, Glasl BA, Lisson JA. A microsensor for monitoring removable-appliance wear. J Clin Orthod. 2011;45:518–520. [PubMed] [Google Scholar]
- 19.Schott TC, Göz G. Wearing times of orthodontic devices as measured by the TheraMon® microsensor. J Orofac Orthop. 2011;72:103–110. doi: 10.1007/s00056-011-0014-7. [DOI] [PubMed] [Google Scholar]
- 20.Pauls A, Nienkemper M, Panayotidis A, Wilmes B, Drescher D. Effects of wear time recording on the patient's compliance. Angle Orthod. 2013;83:1002–1008. doi: 10.2319/010913-25.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Schott TC, Schlipf C, Glasl B, Schwarzer CL, Weber J, Ludwig B. Quantification of patient compliance with Hawley retainers and removable functional appliances during the retention phase. Am J Orthod Dentofacial Orthop. 2013;144:533–540. doi: 10.1016/j.ajodo.2013.04.020. [DOI] [PubMed] [Google Scholar]
- 22.Schott TC, Ludwig B. Microelectronic wear-time documentation of removable orthodontic devices detects heterogeneous wear behavior and individualizes treatment planning. Am J Orthod Dentofacial Orthop. 2014;146:155–160. doi: 10.1016/j.ajodo.2014.04.020. [DOI] [PubMed] [Google Scholar]
- 23.Tsomos G, Ludwig B, Grossen J, Pazera P, Gkantidis N. Objective assessment of patient compliance with removable orthodontic appliances: a cross-sectional cohort study. Angle Orthod. 2014;84(1):56–61. doi: 10.2319/042313-315.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schäfer K, Ludwig B, Meyer-Gutknecht H, Schott TC. Quantifying patient adherence during active orthodontic treatment with removable appliances using microelectronic wear-time documentation. Eur J Orthod. 2015;37:73–80. doi: 10.1093/ejo/cju012. [DOI] [PubMed] [Google Scholar]
- 25.Hamburg BA, Inoff GE. Relationships between behavioral factors and diabetic control in children and adolescents: a camp study. Psychosom Med. 1982;44:321–339. doi: 10.1097/00006842-198209000-00002. [DOI] [PubMed] [Google Scholar]
- 26.Bellini A, Zanchi C, Martelossi S, Di Leo G, Not T, Ventura A. Compliance with the gluten-free diet: the role of locus of control in celiac disease. J Pediatr. 2011;158:463–466. doi: 10.1016/j.jpeds.2010.08.034. [DOI] [PubMed] [Google Scholar]
- 27.Lee SJ, Ahn SJ, Kim TW. Patient compliance and locus of control in orthodontic treatment: a prospective study. Am J Orthod Dentofacial Orthop. 2008;133:354–358. doi: 10.1016/j.ajodo.2006.03.040. [DOI] [PubMed] [Google Scholar]