Abstract
Objective:
To determine whether orthodontic treatment with removable aligners vs fixed orthodontic appliances is associated with a different frequency of orthodontically induced external apical root resorption (OIEARR) when genetic, radiographic, and clinical factors are accounted for.
Materials and Methods:
Three hundred seventy-two orthodontic patients treated with removable aligners (Invisalign) or fixed appliances were genetically screened for interleukin 1B gene (IL1B) (rs1143634), interleukin 1 receptor antagonist gene (IL1RN) (rs419598), and osteopontin gene (SPP1) (rs9138/rs11730582). Twelve clinical variables, potentially associated with OIEARR, were also considered. Subjects were divided according to the presence of radiographically determined OIEARR (>2 mm). The association between OIEARR and appliance type, and radiographic, clinical and genetic factors, was assessed using backward stepwise conditional logistic regression. Odds ratios (ORs) and 95% confidence intervals (CIs) were reported.
Results:
Reliability of the methods was adequate. Clinical case complexity (American Board of Orthodontics [ABO] Discrepancy Index) (OR: 1.032; 95% CI: 1.005–1.061; P = .021) and extent of incisor apical displacement in the sagittal plane (OR: 1.478; 95% CI: 1.285–1.699; P = .001) were associated with an increased OIEARR risk. After adjusting for associations between clinical/radiographic/genetic factors, there were no statistically significant differences with respect to OIEARR or type of orthodontic appliance used, whether removable aligners or fixed appliances (OR: 1.662; 95% CI: 0.945–2.924; P = .078). Only subjects homozygous for the T allele of IL1RN (rs419598) were more prone to OIEARR during orthodontic treatment (OR: 3.121; CI: 1.93–5.03; P < .001).
Conclusions:
A similar OIEARR predisposition was identified using either removable aligners (Invisalign) or fixed appliances.
Keywords: External apical root resorption, Root resorption, Orthodontics
INTRODUCTION
Orthodontically induced external apical root resorption (OIEARR) is a pathological side effect that leads to permanent loss of the dental root structure (cementum and/or dentin).1 Different orthodontic force types and magnitudes have been associated with OIEARR incidence in varying degrees of severity.2,3 OIEARR can affect any tooth, although those most susceptible to resorption are the maxillary central and lateral incisors. It has been shown that more than one-third of individuals treated with fixed appliances can lose more than 3 mm of root length,4 whereas 2% to 5% of the orthodontically treated population have been described as having severe OIEARR of up to 5 mm, which may threaten the function and lifespan of the tooth involved.5
There is a relatively recent trend to provide orthodontic treatment using removable aligners.6 Apart from the potential advantages of better esthetics, hygiene, and comfort,7 their main benefit includes the potential for predictability, reproducibility, and objectivity when orthodontic forces are applied and hence the potential for controlling the stress derived from them in the radicular-apical area.8 So far, it has not been determined whether the objectively controlled forces deriving from removable aligners can prevent, or at least reduce, the occurrence of OIEARR, compared with treatment using traditional fixed appliances. The main objective of the present study, therefore, was to determine whether orthodontic treatment with removable aligners was associated with increased, decreased, or a similar frequency of OIEARR when compared with fixed orthodontic appliances.
MATERIALS AND METHODS
Approval by the appropriate institutional ethics committee was granted. The study was designed as a case-control genetic association study. The estimated sample size was calculated beforehand with a power of 80%, alpha error of .05, and 95% confidence intervals (CIs) for case-control studies' estimation of sample size (0.48 for cases and 0.33 for controls) using Epidat 3.1 software (Dirección Xeral de Saúde Pública, Galicia, Spain). A minimum number of 167 cases and 167 controls was required with an additional 11% margin to cover unexpected dropouts.
An initial sample of 932 patients was consecutively invited to participate in the study after completing their orthodontic treatment; these then underwent examination in order to apply eligibility criteria (Table 1)9–13 for final inclusion in the study. After subject selection, a final sample of 372 Caucasian patients from a university and a private practice setting were included.
Table 1.
Inclusion/Exclusion Criteria for the Study Research and Diagnostic-Clinical and Genetic Data Recorded for Each Patient
| Eligibility Criteria |
D & Cla Recorded |
Genetic Factors |
| Complete orthodontic treatment with fixed appliances or removable aligners | Age | IL1RN (rs419598) (CC/CT/TT) |
| Complete root formation | ABO Discrepancy Index (DI) | IL1B (rs1143634) (CC/CT/TT) |
| No previous history of dental trauma | Sex | SPP1 (rs9138) (CC/CA/AA) |
| No systemic pathologies altering hard tissue biology | Angle classification (Class I, II, or III) | SPP1 (rs11730582) (CC/CT/TT) |
| No root canal treatment therapy on measured teeth | Treatment (extraction vs nonextraction) | |
| No orthodontic retreatment | Type of appliance (aligners vs fixed appliances) | |
| Available lateral and panoramic pre- and posttreatment radiographs | Treatment time | |
| Initial U1 inclination 90°–110° (ANS-PNS/U1)b | U1 final and initial inclination | |
| Changes of U1 inclination < 5°b | Vertical movement (intrusion vs extrusion) | |
| Genotyping data needed to be available | Absolute apical displacement (vertical vs sagittal) |
D & Cl indicates diagnostic and clinical factors; OIEARR, orthodontically induced external apical root resorption; U1, upper incisors; ANS, anterior nasal spine; PNS, posterior nasal spine; ABO. American Board of Orthodontics; DI, ABO Discrepancy Index (from Cangialosi TJ, et al. The ABO Discrepancy Index: a measure of case complexity. Am J Orthod Dentofacial Orthop. 2004;125:270–278); IL1RN, interleukine 1 receptor antagonist gene; IL1B, interleukine 1 beta gene; SPP1, osteopontine gene; C, cytosine; T, thymine; A, adenine.
In order to avoid error by overestimating the OIEARR measurements because of the type of radiographic projection.
All patients received comprehensive orthodontic treatment using either removable aligners (Invisalign, Align Technology, San Jose, Calif) or fixed appliances (straightwire technique, CEOSA DM, Madrid). Patients changed the removable aligners every 12 days on average. With regard to the fixed appliances (0.018-inch slot), the typical wire progression was NiTi archwires (0.014-, 0.016-, 0.018-, and 0.016 × 0.022-inch) for the aligning and leveling phase, stainless steel (0.016 × 0.022-inch) or titanium molybdenum archwires (0.017 × 0.025-inch) for the working phase, and 0.016 × 0.022-inch multistranded archwires for the finishing phase. Specific diagnostic and clinical data relevant to the risk of OIEARR were recorded for each patient (Table1); they were divided into two groups on the basis of OIEARR presence (OIEARR > 2 mm [n = 174]) or absence [OIEARR < 2 mm [n = 198]).
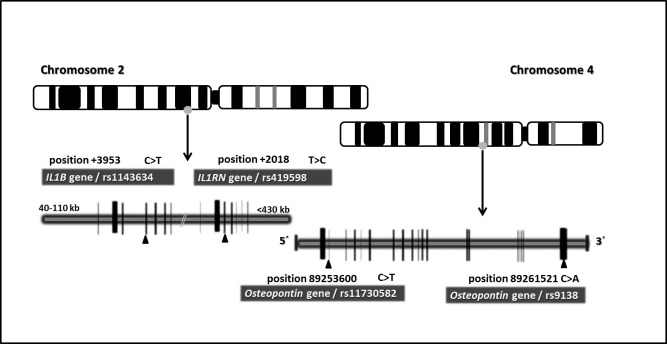
In order to prevent biological bias in subjects who were highly genetically predisposed to OIEARR, all participants were genetically screened for previously reported polymorphisms10–12 (Table 1; Figure 1). Samples for DNA analysis were obtained by collecting 2 mL saliva (Oragene Discover OGR-500, DNA Genotek, Ontario, Canada). Interleukin 1B gene (IL1B) (rs1143634), interleukin 1 receptor antagonist gene (IL1RN) (rs419598), and osteopontin gene (SPP1) (rs9138/rs11730582) were analyzed (GenoType®, PST®plus, Hain Life Science GmbH, Nehren, Germany and Sequenom MassARRAY® system (iPLEX GOLD) (Sequenom, San Diego, CA, USA) following methods validated in the literature.14
Figure 1.
Representative image of genotyped variants on interleukin 1 and osteopontin cluster genes mapped to human chromosomes 2 and 4, where the polymorphisms are represented. The IL1B, IL1RN, and SPP1 genes contain different polymorphisms, although the schema represents only the SNPs studied in this research (rs1143634, rs419598, rs9138, and rs11730582). Vertical bars represent the part of the gene that encodes the proteins.
The maxillary central and lateral incisor root lengths were measured on calibrated panoramic radiographs before and after treatment.15,16 Measurements were taken off digital radiographs and the tooth with the highest OIEARR value was selected as the dependent variable of interest for the subject.11 Pre- and posttreatment radiographic initial and final root (r1 and r2, respectively) and crown (c1 and c2, respectively) lengths were used to determine changes in tooth and root length. The formula r1−r2 (c1/c2) was used to calculate the degree of OIEARR.17–20 In addition, total vertical and sagittal displacements of the maxillary incisor apices were measured when initial and final inclinations were calculated (Nemoceph2D, Nemotec, Madrid, Spain) using stable anatomical structures. Analysis was based on a previously described reference system.21 Briefly, the stable basicranial line (SBL) was traced through the most superior point of the anterior wall of sella turcica at the junction with tuberculum sellae, drawn tangent to the lamina cribrosa of the ethmoid bone. Second, the vertical T, a line constructed perpendicular to SBL and passing through point T, was projected. The extension of a perpendicular line from the vertical T to the apical point in pre- and posttreatment radiographs allowed determining the absolute sagittal and vertical displacement. The same experienced operator performed all measurements.
Measurements from 30 randomly chosen subjects were repeated after a 20-day interval and were compared to calculate the method error (paired Student's t-test and absolute intraclass correlation coefficient (ICC) and concordance (K statistics). The equation, SE = √(Σd2/2n), was used to calculate the accuracy of measurements, where d is the difference between repeated measurements and n, the number of paired repeated measurements.22 A second experienced operator took the same measurements from these 30 chosen subjects so that interobserver reliability and method error between operators could be assessed.
Descriptive statistics were used to report the clinical and diagnostic variables of each patient (frequencies, means, and standard deviations). The risk of OIEARR associated with each factor was calculated using odds ratios (ORs) with a 95% CI. The chi-square test was used to investigate genotype distributions, allele frequencies, and the Hardy-Weinberg equilibrium of subjects in the two groups. The Mann-Whitney U test was used to find any association between the type of appliance and the absolute apical displacement.
Subsequently, control for confounding variables and interactions among the effects of potential risk factors with an impact on the predisposition to OIEARR were analyzed separately with conditional (backward) binary logistic regression (deletion criterion, P < .10).23 SPSS was used for data analysis (version 17.0; Lead Technologies, Chicago, Ill) and statistical significance was set at P < .05.
RESULTS
There was acceptable reliability and error of the OIEARR measurement method for panoramic and lateral radiograph measurements for both intraobserver (SE: .169 mm, .191 mm; ICC: .969, .913; k = .96, .98; P > .05) and interobserver measurements (SE: .32 mm, .45 mm; ICC: .90, .807; k = .86, .70; P > .05).24
Included patients had relatively homogenous initial characteristics (Table 2). The regression matrix (Table 2) that estimated the association between each of the individual clinical factors and OIEARR risk showed that patients treated with removable aligners were twice as prone as those with fixed appliances to be affected by OIEARR (OR: 2.097; 95% CI [1.301–3.382]; P = .002). Furthermore, treatments with increased discrepancy index (OR: 1.031; 95% CI [1.005–1.058]; P = .019), especially when there was increased apical displacement (absolute) in the sagittal plane (OR: 1.430; 95% CI [1.251–1.634]; P < .001), were more likely to be associated with an increase in OIEARR, compared with controls. In addition, no statistical association was found between the type of appliance and the absolute apical displacement (P = .618) in the present sample. This fact ensures that the homogeneity of the sample was quite fair for estimating real differences just by the influence of type of appliance.
Table 2.
Clinical Characteristics of Included Patients
| D & Cl parametersa |
>2 mm OIEARR* Patients (n = 174) |
None or <2 mm Root Resorption (n = 198) |
P Value** |
OR |
95% CI for OR |
|
| Mandibular |
Maxillary |
|||||
| Mean age (y) | 28.48 ± 13.60 | 26.2 9 ± 13.66 | .670 | 0.965 | 0.971 | 1.019 |
| Sex, n (%) | .350 | 0.791 | 0.484 | 1.293 | ||
| Female | 104 (59.77) | 115 (58.08) | ||||
| Male | 70 (40.22) | 83 (41.91) | ||||
| Angle classification, n (%) | .528 | – | – | – | ||
| Class I | 62 (35.63) | 94 (47.47) | .299 | 0.753 | 0.441 | 1.286 |
| Class II | 92 (52.87) | 83 (41.91) | .423 | 0.706 | 0.301 | 1.656 |
| Class III | 20 (11.49) | 21 (10.60) | ||||
| Treatment, n (%) | .576 | 0.822 | 0.414 | 1.634 | ||
| Extraction | 46 (26.43) | 49 (24.74) | ||||
| Nonextraction | 128 (73.56) | 149 (75.25) | ||||
| Type of appliance | ||||||
| Removable aligners | 84 | 75 | .002* | 2.097 | 1.301 | 3.382 |
| Fixed appliances | 90 | 123 | ||||
| Treatment time (mo) | 30.73 ± 12.37 | 29.56 ± 11.64 | .580 | 1.006 | 0.985 | 1.027 |
| ABO Discrepancy Index | 16.06 ± 9.48 | 13.49 ± 8.2 | .019* | 1.031 | 1.005 | 1.058 |
| Vertical movement | ||||||
| Intrusion | 142 (38.2%) | 230 (61.8%) | .180 | 1.640 | 0.796 | 3.380 |
| Extrusion | 172 (46.7%) | 196 (53.3%) | .152 | 1.697 | 0.824 | 3.498 |
| Apical displacement (absolute) | ||||||
| Vertical (mm) | 2.8 ± 2.32 | 2.58 ± 2.03 | .052 | 1.110 | 0.999 | 1.233 |
| Sagittal (mm) | 3.4 ± 1.91 | 2.33 ± 1.69 | .001** | 1.430 | 1.251 | 1.634 |
D & Cl indicates diagnostic and clinical factors; OIEARR, orthodontically induced external apical root resorption.
At least one maxillary incisor; ** conditional backward binary logistic regression analysis. Dependent variable = control vs >2 mm OIEARR patients.
In addition to clinical and radiographic factors, subjects in this study were genotyped for target genes associated in previous publications with a significant degree of OIEARR risk (Table 3). More importantly, when the clinical and radiographic factors of each patient in the control and affected groups were associated with their genotypic information in the logistic regression matrix, the risk of each predisposing factor was substantially adjusted. The final adjusted associations between clinical and genetic factors and predisposition to OIEARR showed no statistically significant differences (P > .05) with regard to OIEARR or type of orthodontic appliance used (OR: 1.662; 95% CI: 0.945–2.924; P = .078) (Table 4).
Table 3.
Genotype and Allele Frequencies of the IL1B (rs1143634), IL1RN (rs419598), and SPP1 (rs9138 and rs11730582) Genes in Affected Patients and Nonaffected Controls
| Gene SNPs |
>2 mm OIEARRa Patients (n = 174) |
None or <2 mm Root Resorption (n = 198) |
||||||
| Genotype fr (n [%]) |
maf (n [%]) | Genotype fr (n [%]) |
maf (n [%]) | |||||
| TT/AA |
TC/AC |
CC |
C/T |
TT/AA |
TC/AC |
CC |
C/T |
|
| IL1RN (rs419598) | 94 (54.6) | 56 (32.1) | 24 (13.7) | 104 (29.8) | 65 (32.8) | 79 (39.8) | 54 (27.2) | 187 (47.22) |
| IL1B (rs1143634) | 27 (15.5) | 71 (40.8) | 76 (43.6) | 125 (35.9) | 28 (14.4) | 97 (48.9) | 73 (36.8) | 153 (38.63) |
| SPP1 (rs9138) | 94 (54.02) | 67 (38.5) | 13 (7.47) | 93 (56.6) | 97 (48.9) | 85 (42.9) | 16 (8.08) | 117 (29.54) |
| SPP1 (rs11730582) | 48 (27.5) | 83 (47.7) | 43 (24.7) | 169 (48.56) | 58 (29.29) | 90 (45.45) | 50 (25.25) | 190 (47.97) |
OIEARR indicates orthodontically induced external apical root resorption; fr, frequencies; maf, minor allele frequency; IL1RN, interleukin 1 receptor antagonist gene; IL1B, interleukin 1 beta gene; SPP1, osteopontin gene; C, cytosine; T, thymine; A, adenine.
Table 4.
Predicted Combined Influence of Clinical and Genetic Factors to Be Affected by OIEARR
| Clinical & Genetic Factors |
β |
SE |
Odds Ratio (Adjusted) |
95% CI (Mandibular–Maxillary) |
P Value |
| Mean age (y) | 0.005 | .013 | 1.005 | 0.981–1.030 | .670 |
| Sex, n (%) | |||||
| Female | –0.234 | .251 | 0.791 | 0.484–1.293 | .350 |
| Male | |||||
| Angle classification, n (%) | – | – | – | – | .528 |
| Class I | |||||
| Class II | −0.284 | .273 | 0.753 | 0.441–1.28 | .299 |
| Class III | −0.348 | .435 | 0.706 | 0.301–1.65 | .423 |
| Treatment, n (%) | |||||
| Extraction | −0.196 | .351 | 0.822 | 0.441–1.634 | .576 |
| Nonextraction | |||||
| Type of appliance | |||||
| Removable aligners | 0.508 | .288 | 1.662 | 0.945–2.924 | .078 |
| Fixed appliances | |||||
| Treatment time (mo) | 0.014 | .011 | 1.014 | 0.993–1.036 | .181 |
| ABO Discrepancy Index | 0.032 | .014 | 1.032 | 1.005–1.061 | .021** |
| Vertical movement | |||||
| Intrusion | 0.530 | .438 | 1.699 | 0.767–3.38 | .208 |
| Extrusion | 0.536 | .285 | 1.710 | 0.978–2.988 | .060 |
| Apical displacement (absolute) | |||||
| Vertical | 0.076 | .054 | 1.079 | 0.970–1.200 | .160 |
| Sagittal | 0.391 | .071 | 1.478 | 1.28–1.699 | .001** |
| IL1RN (rs419598) | |||||
| CC vs CT/TTa | – | – | – | – | .001 |
| TT vs CT/CC | 1.138 | .244 | 3.121 | 1.93–5.037 | .001** |
| CT vs CC/TT | 0.468 | .335 | 1.59 | 0.828–3.08 | .162 |
| IL1B (rs1143634) | |||||
| CC vs CT/TT | −22.406 | 4 · 104 | 0.000 | .000 | 1.000 |
| TT vs CT/CC | −22.392 | 4 · 104 | 0.000 | .000 | 1.000 |
| CT vs CC/TT | −22.629 | 4 · 104 | 0.000 | .000 | 1.000 |
| SPP1 (rs9138) | |||||
| CC vs CA/AA | −0.205 | .504 | 0.815 | 0.303–2.188 | .684 |
| AA vs CA/CCa | – | – | – | – | .479 |
| CA vs CC/AA | −0.396 | .273 | 0.746 | 0.458–1.215 | .238 |
| SPP1 (rs11730582) | |||||
| CC vs CT/TT | 0.234 | .288 | 1.264 | 0.71–2.22 | .417 |
| TT vs CT/CCa | – | – | – | – | .602 |
| CT vs CC/TT | 0.167 | .293 | 1.182 | 0.665–2.10 | .314 |
Factor not included in the equation by backward conditional logistic regression; OIEARR, indicates orthodontically induced external apical root resorption; fr, frequencies; maf, minor allele frequency; IL1RN, interleukin 1 receptor antagonist gene; IL1B, interleukin 1 beta gene; SPP1, osteopontin gene; C, cytosine; T, thymine; A, adenine; SE, standard error; CI, confidence interval.
Finally, it should be noted that only subjects homozygous for the T allele of IL1RN (rs419598) were found to be three times more predisposed (OR: 3.121; 95% CI: 1.93–5.03; P < .001) to experience OIEARR, compared with the other genotypes (Table 4).
DISCUSSION
The objective of this study was to determine whether there was a difference in risk of OIEARR between patients (mean age 27.69 ± 13.6 years) treated with conventional fixed appliances or removable aligners (Invisalign). As OIEARR is a multifactorial pathological event, various previously associated clinically, radiographic, and genetically relevant factors were included in the analysis from each orthodontically treated patient.23 Despite the greater complexity of this type of analysis, it allowed for control and adjustment of factors other than type of appliance on the development of OIEARR.25
During the early development of Invisalign, a study,26 including Invisalign patients, was published suggesting that patients with short dental roots might be better suited for clear aligner therapy instead of fixed appliances. This was supported by information from a study of 100 patients treated with removable aligners in which there was no incidence of any type of OIEARR.26 The ability to program the aligner to control the magnitude of tooth movement and, by extrapolation, the derived stress at the radicular-apical area, was believed to be a feature that would prevent or minimize the occurrence of OIEARR, when compared with fixed appliances. The findings of the current study did not support this hypothesis. Interestingly, after analyzing the results adjusted for clinical, radiographic, and genetic data, we found no statistically significant differences for an increased predisposition to OIEARR, regardless of whether the appliance was removable aligners or fixed appliances.
Several gene-sequence variants in proteins regulating inflammation, including IL-1a, IL-1b, and IL-ra, have been described previously.27,28 Interleukin 1 is one of the first cytokines implicated in inflammation of the vessel wall during tooth movement, affecting leucocyte recruitment and transmigration.29–33 Closely connected to this, the function of interleukin 1 is antagonized by the IL1ra protein encoded in the IL1RN gene, wherein specific sequence variants have been associated with an increased predisposition to suffer OIEARR.11,32 In this connection, subjects homozygous for the T allele of the IL1RN variant studied here may be prone to imbalances in cytokine levels on the IL1ra/IL1b axis during orthodontic tooth movement, which may be associated with a decreased bone remodeling rate that directly influences the subsequent increase in radicular stress. Failure to identify the DNA information of each subject means failing to include the risk inherent in certain patient genotypes, which leads to misinterpreting the observed results of the appliance's effect on OIEARR. Therefore, to properly adjust for the effects of each clinical or treatment- related factor, subject selection in orthodontic research related to OIEARR should include DNA information.
Orthodontic loading of the teeth with either fixed or removable appliances triggers a cellular and molecular response that enables the roots to move through alveolar bone.33 It is the same type of cell response that may, in certain cases, lead to OIEARR, so that treatment with aligners is not exempt from the same iatrogenic effect.
It has been argued that there are differences in the type of force between intermittent (aligners) vs continuous (fixed) appliances and the potential control of the former over magnitude of force compared with the latter.34 It has been claimed that intermittent forces may allow the cementum at the root to heal and so prevent further resorption during the pause.35,36 Nevertheless, these forces have also been associated37 with detrimental jiggling forces and, likely of greater significance, the current aligner treatment protocols suggest an almost full-day use, which means they can almost be considered a type of continuous force with reactivation (aligner change) at a shorter time period (commonly 15 days, although several clinicians suggest changing them in less than a week). We might expect differences in the magnitude and levels of force to account for differences in the expression of OIEARR. Nevertheless, current protocols for fixed appliances usually involve the sequential use of light forces38 at each step, which may be the reason why the predisposition to OIEARR using fixed appliances is similar to that with removable aligners (P > .05).
The significance of the present study is that a preference for using removable aligners over fixed appliances should not be decided by the notion that there is less OIEARR risk in being treated with aligners.
Limitations
A few sources of error may affect assessing OIEARR. For this study sample, the same experienced examiner used panoramic and lateral radiographs to determine the presence of >2 mm OIEARR. Conventional extraoral x-rays may be less accurate than other types of imaging projections, such as periapical radiographs, for studying OIEARR extent.39 Some, however, consider that it is possible to evaluate root resorption with less radiation using lateral or panoramic radiographs.23,40 The latter may be sufficiently reliable for assessing linear measurements if the head inclination in the anteroposterior plane is controlled with a variation of 10° or less.41 Also, the accuracy of periapical projections for measuring OIEARR can be influenced by variability in tooth shape.42 Until a three-dimensional imaging method with volumetric measures that can be made accurately and with less radiation exposure for ethical application, using the same measurement method as that used in previously published studies may enable better comparisons to be made between the present results and earlier study data.
CONCLUSIONS
This clinical study is the first to offer comparative data on the incidence of OIEARR in a large sample of patients treated with Invisalign or fixed appliances, adjusting the response based on genotype and radiographic and clinical data.
Under the conditions of the present clinical study, it is suggested that the predisposition to experience OIEARR with Invisalign is similar to that of using fixed appliances.
ACKNOWLEDGMENTS
This research was awarded with the Clear Aligner International Research Award. This study P113/00310 was partially supported by the “Instituto de Salud Carlos III (Plan Estatal de I+D+i 2013-2016)” and cofinanced by the European Development Regional Fund “A way to achieve Europe” (ERDF). Dr Boris Sonnenberg is a Clinical Speaker for Invisalign.
REFERENCES
- 1.Weltman B, Vig K, Fields H, Shanker S, Kaizar E. Root resorption associated with orthodontic tooth movement: a systematic review. Am J Orthod Dentofacial Orthop. 2010;137:462–476. doi: 10.1016/j.ajodo.2009.06.021. [DOI] [PubMed] [Google Scholar]
- 2.Aras B, Cheng LL, Turk T, Elekdag-Turk S, Jones AS, Darendeliler MA. Physical properties of root cementum: part 23. Effects of 2 or 3 weekly reactivated continuous or intermittent orthodontic forces on root resorption and tooth movement: a microcomputed tomography study. Am J Orthod Dentofacial Orthop. 2012;141:e29–e37. doi: 10.1016/j.ajodo.2011.07.018. [DOI] [PubMed] [Google Scholar]
- 3.Gonzales C, Hotokezaka H, Yoshimatsu M, Yozgatian JH, Darendeliler MA, Yoshida N. Force magnitude and duration effects on amount of tooth movement and root resorption in the rat molar. Angle Orthod. 2008;78:502–509. doi: 10.2319/052007-240.1. [DOI] [PubMed] [Google Scholar]
- 4.Brezniak N, Wasserstein A. Orthodontically induced inflammatory root resorption. Part I: the basic science aspects. Angle Orthod. 2002;72:175–179. doi: 10.1043/0003-3219(2002)072<0175:OIIRRP>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 5.Killiany DM. Root resorption caused by orthodontic treatment: an evidence-based review of literature. Semin Orthod. 1999;5:128–133. doi: 10.1016/s1073-8746(99)80032-2. [DOI] [PubMed] [Google Scholar]
- 6.Ghafari JG. Centennial inventory: The changing face of orthodontics. Am J Orthod Dentofacial Orthop. 2015;148:732–739. doi: 10.1016/j.ajodo.2015.08.011. [DOI] [PubMed] [Google Scholar]
- 7.Azaripour A, Weusmann J, Mahmoodi B, et al. Braces versus Invisalign® gingival parameters and patients' satisfaction during treatment: a cross-sectional study. BMC Oral Health. 2015;15:69. doi: 10.1186/s12903-015-0060-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Long HA. Invisalign therapy in teeth with clinically short roots. J N J Dent Assoc. 2012;83:33. [PubMed] [Google Scholar]
- 9.Tieu LD, Normando D, Toogood R, Flores-Mir C. Impact on perceived root resorption based on the amount of incisal inclination as determined from conventional panoramic radiography. Am J Orthod Dentofacial Orthop. 2015;148:685–691. doi: 10.1016/j.ajodo.2015.05.019. [DOI] [PubMed] [Google Scholar]
- 10.Hartsfield JK., Jr Pathways in external apical root resorption associated with orthodontia. Orthod Craniofac Res. 2009;12:236–242. doi: 10.1111/j.1601-6343.2009.01458.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Iglesias-Linares A, Yañez-Vico R, Ballesta-Mudarra S, et al. Postorthodontic external root resorption is associated with IL1 receptor antagonist gene variations. Oral Dis. 2012;18:198–205. doi: 10.1111/j.1601-0825.2011.01865.x. [DOI] [PubMed] [Google Scholar]
- 12.Iglesias-Linares A, Yañez-Vico RM, Moreno-Fernández AM, Mendoza-Mendoza A, Orce-Romero A, Solano-Reina E. Osteopontin gene SNPs (rs9138, rs11730582) mediate susceptibility to external root resorption in orthodontic patients. Oral Dis. 2014;20:307–312. doi: 10.1111/odi.12114. [DOI] [PubMed] [Google Scholar]
- 13.Cangialosi TJ, Riolo ML, Owens SE, Jr, et al. The ABO discrepancy index: a measure of case complexity. Am J Orthod Dentofacial Orthop. 2004;125:270–278. doi: 10.1016/j.ajodo.2004.01.005. [DOI] [PubMed] [Google Scholar]
- 14.Clendenen TV, Rendleman J, Ge W, et al. Genotyping of single nucleotide polymorphisms in DNA isolated from serum using sequenom massARRAY technology. PLoS One. 2015;10:e0135943. doi: 10.1371/journal.pone.0135943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Harris EF, Kineret SE, Tolley EA. A heritable component for external apical root resorption in patients treated orthodontically. Am J Orthod Dentofacial Orthop. 1997;111:301–309. doi: 10.1016/s0889-5406(97)70189-6. [DOI] [PubMed] [Google Scholar]
- 16.Al-Qawasmi RA, Hartsfield JK, Jr, Everett ET, et al. Genetic predisposition to external apical root resorption in orthodontic patients: linkage of chromosome-18 marker. J Dent Res. 2003;82:356–360. doi: 10.1177/154405910308200506. [DOI] [PubMed] [Google Scholar]
- 17.Malmgren O, Goldson L, Hill C, Orwin A, Petrini L, Lundberg M. Root resorption after orthodontic treatment of traumatized teeth. Am J Orthod. 1982;82:487–491. doi: 10.1016/0002-9416(82)90317-7. [DOI] [PubMed] [Google Scholar]
- 18.Bastos-Lages EM, Drummond AF, Pretti H, et al. Association of functional gene polymorphism IL-1beta in patients with external apical root resorption. Am J Orthod Dentofacial Orthop. 2009;136:542–546. doi: 10.1016/j.ajodo.2007.10.051. [DOI] [PubMed] [Google Scholar]
- 19.Linge L, Linge BO. Patient characteristics and treatment variables associated with apical root resorption during orthodontic treatment. Am J Orthod Dentofacial Orthop. 1991;99:35–43. doi: 10.1016/S0889-5406(05)81678-6. [DOI] [PubMed] [Google Scholar]
- 20.Brezniak N, Goren S, Zoizner R, et al. A comparison of three methods to accurately measure root length. Angle Orthod. 2004;74:786–791. doi: 10.1043/0003-3219(2004)074<0786:ACOTMT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 21.Baccetti T, McGill JS, Franchi L, McNamara JA, Jr, Tollaro I. Skeletal effects of early treatment of Class III malocclusion with maxillary expansion and face-mask therapy. Am J Orthod Dentofacial Orthop. 1998;113:333–343. doi: 10.1016/s0889-5406(98)70306-3. [DOI] [PubMed] [Google Scholar]
- 22.Houston WJ. The analysis of error in orthodontic measurements. Am J Orthod. 1983;83:382–390. doi: 10.1016/0002-9416(83)90322-6. [DOI] [PubMed] [Google Scholar]
- 23.Pandis N, Nasika M, Polychronopoulou A, Eliades T. External apical root resorption in patients treated with conventional and self-ligating brackets. Am J Orthod Dentofacial Orthop. 2008;134:646–651. doi: 10.1016/j.ajodo.2007.01.032. [DOI] [PubMed] [Google Scholar]
- 24.Siegel S, Castellan NJ. Nonparametric Statistics for the Behavioural Sciences. New York: McGraw-Hill; 1988. [Google Scholar]
- 25.Cepeda MS, Boston R, Farrar JT, Strom BL. Comparison of logistic regression versus propensity score when the number of events is low and there are multiple confounders. Am J Epidemiol. 2003;158:280–287. doi: 10.1093/aje/kwg115. [DOI] [PubMed] [Google Scholar]
- 26.Boyd L. Complex orthodontic treatment using a new protocol for the Invisalign appliance. J Clin Orthod. 2007;9:525–547. [PubMed] [Google Scholar]
- 27.Rogus J, Beck JD, Offenbacher S, et al. IL1B gene promoter haplotype pairs predict clinical levels of interleukin-1beta and C-reactive protein. Hum Genet. 2008;123:387–398. doi: 10.1007/s00439-008-0488-6. [DOI] [PubMed] [Google Scholar]
- 28.Kahraman S, Yilmaz R, Arici M, et al. IL-10 genotype predicts serum levels of adhesion molecules, inflammation and atherosclerosis in hemodialysis patients. J Nephrol. 2006;19:50–56. [PubMed] [Google Scholar]
- 29.Dianarello CA. Biologic basis for interleukin-1 in disease. Blood. 1996;87:2095–2147. [PubMed] [Google Scholar]
- 30.Libby P, Sukhova G, Lee RT, Galis ZS. Cytokines regulates vascular function related to stability of the atherosclerotic plaque. J Cardiovasc Pharmacol. 1995;25:9–12. doi: 10.1097/00005344-199500252-00003. [DOI] [PubMed] [Google Scholar]
- 31.Girn HRS, Orsbi NM, Homer-Vanniasinkam S. An overview of cytokine interactions in atherosclerosis and implications for peripheral arterial disease. Vasc Med. 2007;12:299–309. doi: 10.1177/1358863X07083387. [DOI] [PubMed] [Google Scholar]
- 32.Linhartova P, Cernochova P, Izakovicova Holla L. IL1 gene polymorphisms in relation to external apical root resorption concurrent with orthodontia. Oral Dis. 2013;19:262–270. doi: 10.1111/j.1601-0825.2012.01973.x. [DOI] [PubMed] [Google Scholar]
- 33.Krishnan V, Davidovitch Z. On a path to unfolding the biological mechanisms of orthodontic tooth movement. J Dent Res. 2009;88:597–608. doi: 10.1177/0022034509338914. [DOI] [PubMed] [Google Scholar]
- 34.Simon M, Keilig L, Schwarze J, Jung BA, Bourauel C. Forces and moments generated by removable thermoplastic aligners: incisor torque, premolar derotation, and molar distalization. Am J Orthod Dentofacial Orthop. 2014;145:728–736. doi: 10.1016/j.ajodo.2014.03.015. [DOI] [PubMed] [Google Scholar]
- 35.Ballard DJ, Jones AS, Petocz P, Darendeliler MA. Physical properties of root cementum: part 11. Continuous vs intermittent controlled orthodontic forces on root resorption. A microcomputed-tomography study. Am J Orthod Dentofacial Orthop. 2009;136:8.e1–e8. doi: 10.1016/j.ajodo.2007.07.026. [DOI] [PubMed] [Google Scholar]
- 36.Cheng LL, Türk T, Elekdağ-Türk S, Jones AS, Yu Y, Darendeliler MA. Repair of root resorption 4 and 8 weeks after application of continuous light and heavy forces on premolars for 4 weeks: a histology study. Am J Orthod Dentofacial Orthop. 2010;138:727–734. doi: 10.1016/j.ajodo.2009.01.029. [DOI] [PubMed] [Google Scholar]
- 37.Hall A. Upper incisor root resorption during stage II of the Begg technique. Br J Orthod. 1978;5:47–50. doi: 10.1179/bjo.5.1.47. [DOI] [PubMed] [Google Scholar]
- 38.Hughes TJ. The Simplicity System: the innovation of concept and technique. Int J Orthod Milwaukee. 2011;22:53–58. [PubMed] [Google Scholar]
- 39.Sameshima GT, Asgarifar KO. Assessment of root resorption and root shape: periapical vs panoramic films. Angle Orthod. 2001;71:185–189. doi: 10.1043/0003-3219(2001)071<0185:AORRAR>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 40.Sharab LY, Morford LA, Dempsey J, et al. Genetic and treatment-related risk factors associated with external apical root resorption (EARR) concurrent with orthodontia. Orthod Craniofac Res. 2015;18(Suppl 1):71–82. doi: 10.1111/ocr.12078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Stramotas S, Geenty JP, Petocz P, Darendeliler MA. Accuracy of linear and angular measurements on panoramic radiographs taken at various positions in vitro. Eur J Orthod. 2002;24:43–52. doi: 10.1093/ejo/24.1.43. [DOI] [PubMed] [Google Scholar]
- 42.Katona TR. Flaws in root resorption assessment algorithms: role of tooth shape. Am J Orthod Dentofacial Orthop. 2006;130:698.e19–e27. doi: 10.1016/j.ajodo.2006.06.012. [DOI] [PubMed] [Google Scholar]