Abstract
The COVID-19 pandemic and its impact on patients with cancer and cardiovascular disease have confirmed the particular vulnerability of these populations. Indeed, not only a higher risk of contracting the infection has been reported but also an increased occurrence of a more severe course and unfavourable outcome. Beyond the direct consequences of COVID-19 infection, the pandemic has an enormous impact on global health systems. Screening programmes and non-urgent tests have been postponed; clinical trials have suffered a setback. Similarly, in the area of cardiology care, a significant decline in STEMI accesses and an increase in cases of late presenting heart attacks with increased mortality and complication rates have been reported. Health care systems must therefore get ready to tackle the ‘rebound effect’ that will likely show a relative increase in the short- and medium-term incidence of diseases such as heart failure, myocardial infarction, arrhythmias, and cardio- and cerebrovascular complications. Scientific societies are taking action to provide general guidance and recommendations aimed at mitigating the unfavourable outcomes of this pandemic emergency. Cardio-oncology, as an emerging discipline, is more flexible in modulating care pathways and represents a beacon of innovation in the development of multi-specialty patient management. In the era of the COVID-19 pandemic, cardio-oncology has rapidly modified its clinical care pathways and implemented flexible monitoring protocols that include targeted use of cardiac imaging, increased use of biomarkers, and telemedicine systems. The goal of these strategic adjustments is to minimize the risk of infection for providers and patients while maintaining standards of care for the treatment of oncologic and cardiovascular diseases. The aim of this document is to evaluate the impact of the pandemic on the management of cardio-oncologic patients with the-state-of-the-art knowledge about severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease (COVID-19) in order to optimize medical strategies during and after the pandemic.
Keywords: SARS-CoV-2, COVID-19, Cancer, Cardiovascular disease, Cardio-oncology, Cardiovascular imaging, Biomarkers, Telehealth
Introduction
Cancer and cardiovascular diseases (CVD) represent the two most frequent causes of morbidity and mortality worldwide. In recent decades, due to widespread screening programmes and improved care, we have seen a rapid increase in cancer survival, with more than 400 000 new cured or long-survivors each year. The COVID-19 pandemic and its impact on patients with cancer and cardiovascular disease have confirmed the particular vulnerability of these populations. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the causal agent of coronavirus disease (COVID-19) is a novel, zoonotic, single-stranded RNA betacoronavirus1 whose strong ability to spread has rapidly transformed the disease in a pandemic with a devastating impact on health all over the world. In the first outbreak of infection fever was the most common symptom in hospitalized patients (almost 90% of patients) followed by dry cough (60–86%) and shortness of breath (53–80%), other symptoms were fatigue (38%) nausea, vomiting or diarrhoea (15–39%), headache and myalgia (15–55%), olfactory and gustatory dysfunction in 64–89% of patients; in almost 3% of patients anosmia and ageusia were the only symptoms. Laboratory abnormalities of hospitalized patients included lymphopoenia (83%), elevated inflammatory marker such as ESR, CPR, ferritin, TNF-α, IL-1, IL-6, and abnormal coagulation parameters: prolonged prothrombin time, thrombocytopenia, elevated D-dimer, and low fibrinogen. The hallmark of the disease was bilateral lower-lobe infiltrates on chest radiographic imaging and bilateral peripheral lower-lobe ground-glass opacities and/or consolidation on chest computed tomographic imaging. Complications included pneumonia (75% of patients); acute respiratory distress syndrome (ARDS) (15%); acute liver injury (19%); cardiac injury with troponin elevation (7–17%), acute heart failure (HF), arrhythmias, and myocarditis; coagulopathy with venous and arterial thrombo-embolism (10–25%); acute kidney injury (9%); neurologic manifestations: impaired consciousness (8%) and acute cerebrovascular disease (3%); and shock (6%). In critically ill patients with COVID-19, cytokine storm and macrophage activation syndrome were observed.2 After the first outbreak in December 2019, we have increased our knowledge about the virus and the disease. We have learned that SARS-CoV-2 transmembrane spike protein (S) has a strong affinity to angiotensin-converting enzyme (ACE2) receptor and uses this receptor to enter the host cells.3 We have also learned that ACE2 receptors are expressed in lung epithelial cells, but are also abundant in the cardiovascular system, making COVID-19 both a pulmonary and vascular disease.4 Beyond the direct consequences of COVID-19 infection, the pandemic has had an enormous impact on global health systems. Screening programmes and non-urgent tests have been postponed. Delays and postponements involved not only non-urgent treatments but also clinical trials that suffered a setback. The media impact of the pandemic has significantly reduced the access of cancer patients to hospitals for fear of infection as a further deleterious effect. The pandemic has led to reductions and delays in the identification of new cancers and in the delivery of treatment in the UK and it is expected that this will result in excess preventable deaths for the more frequent types of malignancies.5 Similarly, in the area of cardiology care, there is a significant decline in STEMI accesses and an increase in cases of late presenting heart attacks with increased mortality and complication rates; in an Italian Region (Emilia Romagna) a 17% cardiac out-of-hospital excess death rate in the first semester of 2020 has been documented with a peak of +62% in April 2020.6 Recent observations from Europe and the USA have reported a reduction of ∼40% in interventional cardiology accesses for STEMI.7,8 A monocentric Italian study has showed a 37% reduction of hospital admission for acute coronary syndrome (with a sharp increase in the beginning of the lock-down period), an increased number of patients with late presenting myocardial infarction, and a reduced number of interventional cardiology procedures.9
Health care systems must therefore get ready to tackle the ‘rebound effect’ that will likely show a relative increase in the short- and medium-term incidence of diseases such as HF, myocardial infarction, arrhythmias, and cardio- and cerebrovascular complications. Scientific societies are taking action to provide general guidance and recommendations aimed at mitigating the unfavourable outcomes of this pandemic emergency. While awaiting for an effective novel treatment or an adequate herd immunity obtained with extensive vaccination, we have to struggle with the challenge of the pandemic in our medical practice. We have to engage in health policies that have the priority of safeguarding both patient and staff while avoiding undue delays in care delivery to patients. The aim of this document is to evaluate the impact of the pandemic on the management of cardio-oncologic patients with the state-of-the-art knowledge about SARS-CoV-2 and COVID-19 in order to optimize medical strategies during and after the pandemic.
Epidemiology
To better describe the impact of a pandemic we have to define10 the following items:
The full spectrum of the disease severity (from asymptomatic to severe)
Severe acute respiratory syndrome coronavirus 2 infection has a wide spectrum of clinical manifestations that ranges from asymptomatic carriers to patients with fatal disease. A small proportion of SARS-CoV-2 infected patients develop severe illness (8–15%) with respiratory failure, ARDS, multiple organ failure. Case fatality rates ranges from 0.3 deaths per 1000 cases among patients aged 5–17 years to 304.9 deaths per 1000 cases among patients aged 85 years or older in the USA. Case fatality rates in patients hospitalized in the intensive care unit may reach 40%. Approximately 5% of patients with COVID-19, and 20% of those hospitalized, experience severe symptoms necessitating intensive care.2
The transmissibility of the virus
Severe acute respiratory syndrome coronavirus 2 infection has a great ability to spread, higher than SARS-CoV, emerging genetic variants of SARS-CoV-2 seem to have an even greater ability to spread. The WHO reports (July 2020) that transmission of SARS-CoV-2 can occur through direct, indirect, or close contact with infected people through infected secretions such as saliva and respiratory secretions or their respiratory droplets, which are expelled when an infected person coughs, sneezes, talks, or sings. Indirect contact transmission involving contact of a susceptible host with a contaminated object or surface (fomite transmission) may also be possible. Airborne transmission of SARS-CoV-2 can occur during medical procedures that generate aerosols (‘aerosol generating procedures’).11
The infectors (asymptomatic and pre-symptomatic patients), the duration of the virus in respiratory secretion
Asymptomatic, pre-symptomatic, and symptomatic carriers can spread the infection. The average time from exposure to symptomatology onset is 5 days, the majority of symptomatic people (97.5%) manifest their symptoms within 11.5 days of infection. The basic reproductive number (R0), is defined as the expected average number of additional infectious cases that one infectious case can generate, it was thought to range from 2.2 to 2.7 for SARS-CoV-2 infection in the early stages of the epidemic in China, meaning that one person infected with SARS-CoV-2 could spread the infection to ∼2.2–2.7 people.12
The risk factors for severe illness or death, the identification of patients with a high propensity to a poor outcome
Even though individuals of all ages and sexes are susceptible to COVID-19, CVD and cancer emerge as catalysts for Sars-CoV-2, making patients with these comorbidities more vulnerable to the infection and more prone to a fatal outcome.13 Patients with established CVD and cancer will suffer the worst effects of SARS-CoV-2 infection.14 Obesity also constitutes a major contributor to mortality, a Public Health England report of July 2020 estimated that ‘having a BMI of 35 to 40 could increase a person’s chances of dying from covid-19 by 40%, while a BMI greater than 40 could increase the risk by 90%’.15
Cancer, cardiovascular diseases, and COVID-19
Cancer and COVID-19
Early reports from China suggested that patients with COVID-19 were more likely to have a history of cancer than the general population, supporting a potential susceptibility of the cancer population to COVID-19; the infection rate reported among cancer patients was twice the rate of COVID-19 in the general population in Wuhan. Specifically, among 1524 cancer patients admitted to Zhongnan Hospital in Wuhan, 0.79% had COVID-19 vs. 0.37% in the general population. Patients with cancer had a higher risk of serious events, defined as the percentage of patients admitted to the intensive care unit requiring invasive ventilation or death, than patients without cancer (39% vs. 8%; P = 0.0003); in addition, patients receiving chemotherapy in the previous 14 days required more frequent admission to the intensive care unit (HR 4.1, 95% CI 1.086–15; P = 0.037) .16 In a study of 218 patients admitted to a New York hospital, a COVID-19 mortality of 28% was observed in cancer patients with a mortality rate of 37% for haematological malignancies and 25% for solid tumours. Haematological patients are probably more severely immunocompromised by being treated with myelosuppressive therapy and may be more susceptible to cytokine storm syndrome.17,18 It should be noted, however, that not only patients with active cancer but also cancer survivors were more susceptible to COVID-19 and advanced age was the only risk factor for serious events (OR 1–43, 95% CI 0.97–2.12; P = 0.072).19
Although the above-mentioned studies have shown that cancer patients are more susceptible to COVID-19 infection and to more severe consequences, the results were obtained on cohorts with small numbers of patients. Subsequently, studies were conducted on larger cohorts. In one of them, 928 patients were enrolled and a 30-day mortality of 13% was observed; cancer-specific factors such as ECOG (Eastern Cooperative Oncology Group performance status) of 2 or higher and active cancer were associated with increased mortality.20 In another study of 800 patients with cancer and COVID-19, a 30-day mortality of 28% was observed and the factors that increased the risk of death were: older age (OR 9.42, 95% CI 6.56–10.02, P < 0. 001), male sex (OR 1.67, 95% CI 1.19–2.34, P = 0.003), history of hypertension (OR 1.95, 95% CI 1.36–2.80, P = 0.002), and cardiovascular disease (OR 2.32, 95% CI 1.47–3.64, P = 0.002). It was also observed that neither cytotoxic chemotherapy given within 4 weeks of the development of COVID-19 nor immunotherapy, target therapy, hormone therapy, and radiotherapy (RT) resulted in an increased risk of death.21 In another study, immunotherapy during the 40 days preceding COVID-19 infection was shown to be a predictor of hospitalization and poorer outcome in patients treated for both lung cancer and other malignancies.22
In terms of tumour type, mortality was particularly high in a thoracic malignancy registry and smoking was the strongest predictor of death in multivariate analysis.23
Cardiovascular system and COVID-19
Risk factors such as smoking, hypertension, diabetes, obesity, and pre-existing CVD have been observed to be associated with increased susceptibility to SARS-CoV-2 infection, as well as increased disease severity.24–26 Since the first studies published in China, the prevalence of risk factors and CVD has been observed in patients hospitalized for COVID, and in addition to a more severe course of the disease, higher case fatality rates have also been observed.27 A study conducted on 138 patients admitted to Zhongnan Hospital in Wuhan showed the coexistence of hypertension in 31.2% of cases, diabetes in 10.1%, CVD in 14.5%, with an increased frequency of admission to intensive care units (ICUs).28 The case fatality rate observed in a large Chinese population (44 672 confirmed cases) was 2.3% and was higher in patients with pre-existing comorbidities: 10.5% for CVD, 7.3% for diabetes, 6.3% for chronic respiratory disease, 6.0% for hypertension, and 5.6% for cancer.29
A meta-analysis of six studies confirmed a two-fold increase in severity of the disease in hypertensive patients and a three-fold more severe increase in patients with CVD.30
There is a bidirectional relationship between risk factors/CVD and COVID-19. Risk factors and CVD result in increased susceptibility to infection; indeed, the SARS-CoV-2 spike protein has a high affinity for individuals with pre-existing risk factors or CVD who have increased expression of ACE2 receptors at the level of vascular endothelium, pericytes, cardiomyocytes, fibroblasts, and myocardial adipocytes. Angiotensin-converting enzyme counteracts the negative effects of angiotensin II with vasodilatory, anti-inflammatory, antioxidant, and antifibrotic effects. Activation of ACE2 results in its endocytosis and down-regulation of activity followed by up-regulation of inflammatory cytokines, decreased degradation of angiotensin (AT) II and decreased AT1–7. Increased ATII and hyperactivation of AT1 receptors results in endothelial dysfunction, vasoconstriction, inflammation, myocardial hypertrophy, decreased NO, increased endothelin resulting in hypertension, myocardial damage, known as ‘myocardial injury’, and arrhythmias. A decrease in AT1–7 leads to a reduction in the activation of Mas receptors on platelets, which in combination with the up-regulation of inflammatory cytokines results in platelet dysfunction and intravascular thrombosis (myocardial infarction, stroke, venous thrombo-embolism).
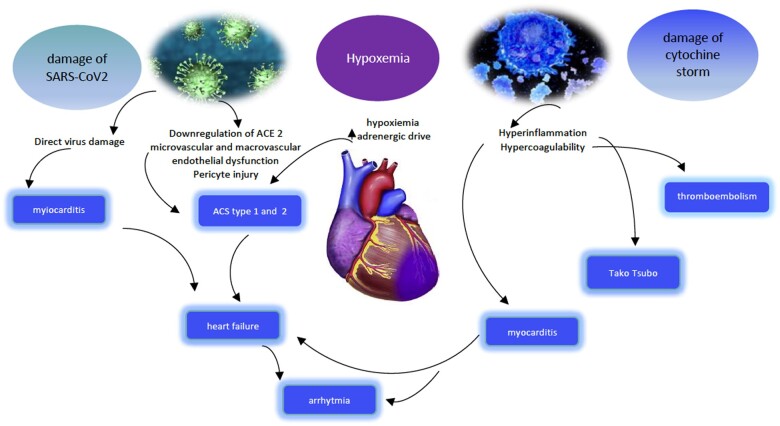
In conclusion, myocardial damage can occur through a triple pathway: activation of ACE2, systemic inflammatory activation leading to immune activation and cytokine storm, hypoxaemia, and infection-induced increase in the adrenergic drive (Figure 1).
Figure 1.
Pathways of myocardial damage.
Clinical cardiovascular manifestations in patients with COVID-19 infection include myocarditis, stress cardiomyopathy, arrhythmias, and acute coronary syndromes with the prevalence of type 2 forms induced by hypoxaemia or microvascular dysfunction elicited by pericyte infection, contributing to myocardial infarction with non-obstructive coronary arteries.31,32
It has been observed that up to 28% of patients with COVID have myocardial injury, expressed by increased troponin values33 and the presence of myocardial injury is more often accompanied by significantly higher complications and in-hospital mortality. It has also been recently observed that the injury is accompanied not only by electrocardiographic abnormalities but in nearly two-thirds of patients also by echocardiographic abnormalities that include segmental abnormalities or left ventricular dysfunction, Grade II or III diastolic dysfunction, right ventricular dysfunction, and pericardial effusion.34
During the early phase of the pandemic, there was theoretical uncertainty regarding the safety of the use of angiotensin-converting enzyme inhibitors (ACEIs)/angiotensin II receptor blockers (ARBs) in patients with COVID-19. Since ACE2 is a receptor for SARS-CoV-2, concern was initially raised in the medical and scientific community that the use of ACEIs and ARBs could result in increased mortality and severity from COVID-19.35
As a matter of fact, the goals of ACE and ACE2 are different despite the high structural similarity between the two enzymes. Angiotensin-converting enzyme converts ATI to ATII, whereas ACE2 degrades ATII to AT (1–7). Angiotensin-converting enzyme inhibitors prevent the conversion from ATI to ATII, whereas ARBs inhibit the AT1 receptor of ATII. Therefore, neither class of drugs acts directly on ACE2.
Even recent studies have removed initial fears by not only demonstrating the potential benefit of ACEIs/ARBs in the treatment of hospitalized patients with hypertension with COVID-19 but also a reduction in all-cause mortality from COVID-19 in treated versus untreated patients.36
A recent meta-analysis of 26 studies confirmed that treatment with ACEIs and ARBs compared with other antihypertensive drugs or no treatment was associated with reduced mortality as well as a lower risk of ventilatory support among COVID-19-infected hypertensive patients.37 Many scientific societies such as the American Heart Association, the American College of Cardiology, the Heart Failure Society of America, the ESC Council on Hypertension, and the Chinese Society of Cardiology have provided recommendations in favour of continuing treatment with ACEIs and ARBs in patients with hypertension, HF, and ischaemic heart disease.38–40
Cardio-oncology and COVID-19
Not many studies regarding CVD complications in patients with cancer and COVID-19 are available in the literature because studies have described cancer patients and those with cardiovascular disease separately. In the cardio-oncologic population, there is an additional level of diagnostic complexity due to ‘overlapping’ phenomena between COVID-19 complications, cancer complications, and cardiovascular effects of cancer treatments. Indeed, troponin increases may also be indicative of subclinical cardiotoxicity induced by treatments with anthracyclines and/or anti-HER2 agents as well as it may be observed in patients receiving tyrosine kinase inhibitors at high prothrombotic risk (ponatinib) or fluoropyridines that induce coronary vasospasm.
Elevated cardiac biomarkers have been associated with cytokine release syndrome (CRS) from chimeric antigen therapy,41,42 HF from proteasome inhibitor (carfilzomib) use, myocarditis during treatment with immune checkpoint inhibitors (ICI), which are associated with 25–50% mortality.43 To date, few data are available to draw definitive conclusions about the clinical outcome of ICI-treated cancer patients with COVID, but since ICI treatment cannot be considered highly immunosuppressive, avoiding treatment to reduce coronavirus infections could deprive these patients of a highly effective class of drugs as shown by data from a recently published review.44 Indeed, recent studies not only confirm the safety of ICI treatment of patients with cancer and COVID but also indicate its potential utility as an immunostimulant.45
Many of these intricate processes can be confounding in the treatment of patients with cancer also affected by COVID-19 and therefore a multidisciplinary evaluation, particularly by a cardio-oncologist, may be crucial in ensuring the optimal management in this high-risk population.
General approach strategies to the oncologic patient in COVID-19 pandemia
The problem of cardio-oncology services in the COVID-19 era has different aspects in different settings. Cancer patients need to be protected from SARS-CoV-2 infection, and this can only be guaranteed with dedicated COVID hospitals and COVID-free hospital.
Thus, the dedicated oncologic hospitals are—as far as possible—COVID-free. All patients undergo nasopharyngeal/oropharyngeal swab testing before admission to a medical or surgical ward or to the day-hospital treatments. The access of visitors and relatives is restricted. Oncological patients who need visits/exams have a structured triage before entering the hospital (Table 1). In some Italian regions, a reassessment of the sanitary offer has been performed, with dedicated COVID hospitals and other hospitals COVID-free to guarantee a regular activity of departments as neurosurgery, stroke units, cardiac or oncology surgery, oncology, and geriatric medicine.46
Table 1.
A proposal for the cardiotoxicity surveillance during COVID-19 pandemic
| Treatment | Recommendations before pandemic | Recommendations during pandemic |
|---|---|---|
| Anthracyclines: basal evaluation |
|
|
| Anthracyclines: during treatment |
|
|
| Anthracyclines: follow-up |
|
In asymptomatic patients defer the echo-imaging |
| Trastuzumab: basal evaluation | Echocardiography to all patients | Echocardiography only in high-risk patients. |
| Trastuzumab: during treatment |
|
|
| Trastuzumab: follow-up | The same as anthracyclines | In asymptomatic patients defer the echo-imaging. |
Adapted from Calvillo-Argüelles et al.111
ACEI, angiotensin-converting enzyme inhibitor; CVR, cardiovascular risk; HF, heart failure; LVEF, left ventricular ejection fraction; RT, radiotherapy.
On the contrary, most of the general hospitals with oncology and radiation therapy facilities may also have sections dedicated to COVID patients; the oncologic section usually follows the same precautions of the Cancer Hospitals (test before admission for cures), but the risk of infection in other areas must be considered. Some hospitals have planned separated ‘clean’ accesses and pathways in order to avoid any contact between frail patients—who must be protected—and infected (or even possibly infected) patients.47,48
In order to limit the risk—for a cancer patient—to get infected, different paths should be planned.
Infected or swab positive patients have usually their treatments postponed by the oncologists, if this does not interfere with the oncologic prognosis.49 Those who need urgent surgery or medical treatments should be sent to a general hospital with dedicated COVID facilities, even if they were usually followed in a cancer hospital.
As a general rule, Cancer COVID-free hospitals and general hospitals should be open to a cooperation, offering the possibility to cancer patients, wherever usually followed, to have their cardiologic evaluation in the safest way for both themselves and other patients.
Both in these hospitals and in general hospital, cancer patients who need in-person visits or diagnostic tests follow a structured triage before entering the hospital.
The general recommendations for reducing the transmission of COVID infection are summarized in Kampf et al.50 and Zhou et al.51 papers.
To reduce the risk of infection, it is important to reduce the ‘face-to face’ consultation when it is possible, according to a careful evaluation of both the oncologic and the cardiologic risk of patients, and also the COVID-19-related risk.52 When a consultation is indicated, visits, exams, and therapies should be concentrated in the same day if possible, mostly for patients living far away from the healthcare centres.
The European Society of Medical Oncology (ESMO) and the American Society of Clinical Oncology (ASCO) have already published their specific recommendations for the management of cardiac disease in cancer patients53 and clinical practice guidelines for the management of myocardial dysfunction54 due to cardiotoxic treatment. In the era of pandemic disease, these recommendations must be revised without exposing the cancer patients to further risk of cardiac complications.52,55
Cardio-oncological counselling in COVID-19 pandemia
Cardio-oncology studies and treats the intersection of two pathologies that both affect, by definition, ‘fragile’ patients. For this reason, during the COVID-19 pandemic, the Cardio Oncology Services and the Cardiology Department that deal with cancer patients with or without cardiovascular history, have had to face a series of particularly delicate problems, which have essentially affected both the clinical and organizational areas:
The subgroups most at risk seem to be represented by all those who are on therapy for the active oncological disease, in particular those with signs/symptoms attributable to cardiotoxicity, by patients being treated with immunosuppressive drugs (e.g. for onco-haematological diseases) and by those taking specific antineoplastic treatments or who have undergone stem cell transplantation, always in the context of onco-haematological pathologies.17,18 For this reason, the absolute need to protect these subgroups of patients from the possibility of contracting COVID-19 has emerged since the very beginning of the pandemic.
In addition to the risk represented by possible SARS-CoV2 infection, cancer patients with or without pre-existing cardiovascular disease were in any case indirectly involved in the profound reorganization of both territorial and hospital health services, dictated by the need to reduce the chances of contagion in the hospital, as well as by the reallocation of human and structural resources to the management of COVID-19 patients. This has led to the postponement and reprogramming, both at a cardiological and oncological level, of diagnostic tests, especially of advanced imaging and therapeutic procedures, with effects that will already be evident in the near future56–59 and that, for cancer patients, have already been estimated in their impact on outcome.5,60
As far as cardio-oncological counselling is concerned, this has been heavily involved in the reallocation of medical and technological resources aimed at identifying and treating COVID-19 patients. For cardio-oncological patients, a first distinction must be made between the outpatient and hospital level, with a further differentiation, not irrelevant in this area, between ‘Cancer Centers’ (generally without an Emergency Department and which by definition should be COVID-free) and general hospital. In both contexts, the keyword is appropriateness.
The COVID-19 pandemic has represented and represents a unique opportunity for a reasoned review on the appropriateness of our clinical practice which, thanks to the rapid and tumultuous growth of cardio-oncology, still lacks shared guidelines, and is frequently anchored to local habits that are not reflected in literature (that is in any case growing exponentially) and often involve a waste of resources.
Cardio-oncological consulting in outpatients
In consideration of the easy transmissibility and particularly high mortality of COVID-19 in high-risk patients, the only effective strategy to contain the spread of the disease immediately appeared that of social distancing.61 For cancer patients, this translates into the need to limit access to the hospital only to those for whom it is really essential.
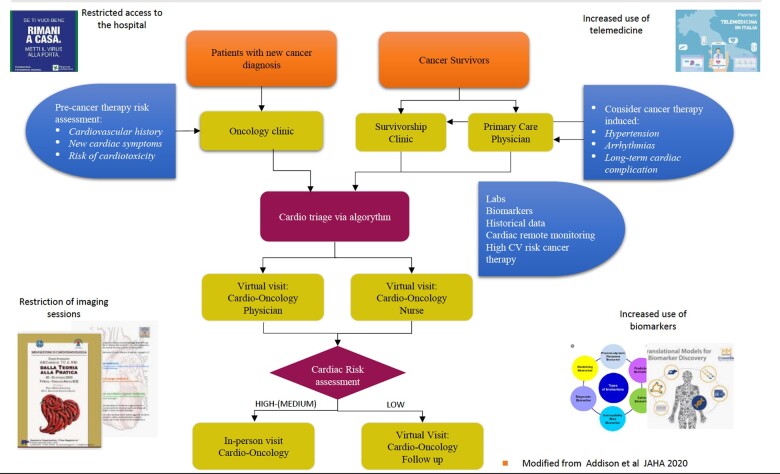
Figure 2 indicates a platform designed ad hoc, supported by four pillars which are: the limitation of hospital access, the spread of telemedicine, the restriction of imaging sessions, and the more extensive and reasoned use of biomarkers, with the last two points which also affect hospitalized patients, how we will see later on.
Figure 2.
Modified from Addison et al.52
In the case of cancer patients with no previous CVD, more frequent contacts between oncologist and cardiologist can help in a first selection of patients for whom a clinical or instrumental cardiological evaluation is really necessary through an accurate risk stratification based on the anamnestic criteria alone, which should be done in the oncology clinic. The cardiologist's task is to provide the oncologist with simple flowcharts, the application of which allows to quickly and safely identify low-risk patients, for whom cardiological consultation in presence is not necessary once a baseline Electrocardiogram (ECG) and a pre-treatment echocardiogram (if needed) have been acquired.
For patients with known cardiovascular pathology, it is not always possible to safely defer or to skip clinical or instrumental checks: this evaluation can and must be done directly by the cardiologist, and in the pre-COVID era this almost always took place through a cardiological visit. Today, in order to limit access to hospital or outpatient clinics to patients who really need it, a first approach could include an initial telephone contact aimed at ascertaining the clinical stability of the patient by the cardiologist, defined as absence in the last 6–12 months of hospital admissions for cardiological reasons and onset/progression of symptoms such as dyspnoea on exertion, chest pain, and/or syncope. This evaluation can possibly be integrated by one of the telemedicine tools, for example for the transmission and subsequent filing of the instrumental tests held by the patient. The coronavirus pandemic has put telemedicine in the spotlight, especially in the USA, where in 2020 Congress approved a regulation (Public Law 116-123, Coronavirus Preparedness and Response Supplemental Appropriations Act, 2020),62 which allows certain providers to charge Medicare for some healthcare services provided through telemedicine platforms.
Before the COVID-19 pandemic, the use of telemedicine in the cardiology field was not so common, even if it was gradually growing.63 The first experiences concerned hypertensive patients and patients with advanced chronic HF, the latter ones in many ways similar to cancer patients.64
In the first months of 2020, following the pandemic outbreak of COVID-19, there was a rapid spread and increasingly frequent use of online platforms, some already known, others even conceived ‘ad hoc’, as a tool to keep the access of patients to the hospital to a minimum and therefore to contain infections.65,66 However, it must be said that in many countries, the regulatory framework and the possibility of reimbursement for telemedicine activities are still very poor. Furthermore, even if it is certainly very useful for patients residing in rural or decentralized areas compared with tertiary reference centres, the impossibility of having the technology at the basis of telemedicine could accentuate the inequalities in access to specialized medical care that are already the prerogative of the most disadvantaged population groups, such as patients of low socioeconomic status, the elderly and immigrants.67 As far as telemedicine in the cardioncology field is specifically concerned, an international survey conducted between March and April 2020, which involved over 1400 cardiologists and oncologists from 43 countries, the vast majority from Europe, North America, and Latin America, showed a rapid growth in telemedicine already in the first months of the pandemic (from March to April), especially in academia and universities.68 This paper reports that on one hand, a high global percentage of cardiologists and oncologists had early resorted to telemedicine, with a significant increase between March (82%) and April 2020 (91.5%), on the other, there were significant differences between different geographical areas, with Europe (81%) and Latin America (64%), significantly behind the USA (88%, with P = 0.021 for EU vs. USA and <0.001 for Latin America vs. USA).
In this work, it is interesting to note how cardiologists more often than oncologists (92% vs. 63%, P = 0.01) reported the need to cancel or postpone elective visits or treatments, that can partly be explained by the fact that cardiologists more often than oncologists (46% vs. 25%, P < 0.001) were asked to change their area of expertise, with a more frequent temporary relocation to departments dedicated to the care of COVID-19 patients.
Cardio-oncological counselling in hospitalized patients
In this context too, the primary need is to protect ‘fragile’ patients, minimizing the chances of contagion. Within non-COVID-free general hospitals, it is necessary to provide and organize protected pathways for cancer patients. More extensive use of biomarkers to reduce imaging sessions and the use of portable hardware (POCUS, point-of care ultrasound) could find application in hospitalized patients even more than in outpatient ones. In this patient population, a problem that could arise from the wider use of biomarkers is represented by the differential diagnosis between manifestations of cardiotoxicity and possible cardiac involvement in the course of SARS-CoV-2 infection, considering, however, that the former is much more frequent than the latter. Finally, the clinical and instrumental preoperative cardiological evaluation of patients to be sent to oncological surgery which, especially in Cancer Centres, is widely used often in an inappropriate manner, should even more be limited to cases in which the result of the consultation is able to modify the surgical choices and/or the subsequent therapeutic conduct.69
Pre-treatment risk stratification
Three kinds of risk should be considered and balanced in the decision-making on clinical interventions in cancer patients: (i) the risk of getting infected by SARS-CoV-2; (ii) the risk of delaying or discontinuing the antineoplastic therapies; and (iii) the risk of cardiovascular side-effects of antineoplastic therapies.
The patients with active cancer and even the long-term survivors may be at higher risk of getting infected by SARS-CoV-2, mostly the patients with lung or colon cancer.70 A worse clinical outcome has been reported by several studies.71,72 In Italy, 20% of the patients who died of COVID-19 during the early phase of the outbreak had active cancer.73 In a Chinese study, cancer was amongst the risk factors for cardiac injury during COVID-19.74 However, other studies did not confirm the risk of a more severe outcome in cancer patients.75,76 Noteworthy, not only the patients with active cancer, or recently treated, but also many long-term survivors might be at increased risk of both SARS-CoV-2 infection and more severe COVID-19 course. Lymphopoenia, altered neutrophil/lymphocytes ratio, thrombocytopenia, and pancytopenia are all risk factors for both infection and poor outcome identified by retrospective and prospective studies on COVID-19.71,77,78 Lymphopoenia, thrombocytopenia, and pancytopenia are common during cytotoxic therapies and expose to an increased risk of bacterial and viral infections. A retrospective study on 205 Chinese patients with cancer confirmed that lymphocytopaenia and recent chemotherapy was a risk factor for poor outcome.79 It should also be emphasized that oncology patients may present a pulmonary fragility related to the outcomes of antineoplastic treatments. A wide variety of anticancer drugs, from the oldest ones (as bleomycin, alkylating agents, and antimetabolites) to the more recently introduced in therapy (as several monoclonal antibodies) may induce an acute or chronic lung injury.80,81 Chest radiation therapy (especially when used for lung cancer or mediastinal masses) can result in acute lung damage and chronic pulmonary fibrosis, and even patients who have made a complete recovery from cancer may have severe lung dysfunction many years later, as we have learned by the experience with the long-term childhood and adolescents cancer survivors.82,83
With respect to oncology, it is necessary to stratify patients as being at high or low risk of disease progression without oncologic therapy. In high-risk patients, therapy will be started according to standard criteria, while in low-risk patients, the type of treatment, the mode of administration, and the timing can be remodulated. Oncology societies and national authorities have issued guidelines on cancer care during the pandemic, with specific indications for different tumours; there is a general consensus that urgent, life-saving therapies should be continued.84,85
the role of co-morbidities, such as hypertension, ischaemic heart disease, diabetes, and left ventricular dysfunction in affecting the prognosis of COVID-19 has emerged in all the epidemiological studies on SARS-CoV-2 infection; these co-morbidities are common in cancer patients, both as common risk factors for cancer, and as a consequence of antineoplastic treatments: hypertension may be induced or worsened by antiangiogenic therapies, as well as cardiac ischaemia; diabetes may be a side effect of steroid therapy, ischaemic heart disease may be also a late sequel of chest RT, or of platinum treatments.86,87
The first step is to assess the risk of cardiotoxicity in a given patient with a given therapy.
Cardiovascular risk (CVR) can be defined by using simple flow charts, which allow the rapid and safe identification of low-risk patients. Pre-treatment cardiological evaluation can be omitted in patients at low risk of cardiotoxicity,88 including those without
a history of cardiovascular disease
two or more CVR factors
history of cardiotoxicity
history of previous cardiotoxic therapy and/or RT.
In the high-risk patient, a tailored therapeutic strategy should be planned together by the cardiologist and the oncologist, as well as a strict and timely follow-up.
Essentially, we can have several scenarios:
Patients at high risk of (or in course of) infection and low oncologic risk, who may defer treatment.
Patients who have a high oncologic risk and normal infectious risk (overlapping with the general population, followed in ‘safe’ hospitals, in areas where the risk of infection is lower) can do therapies with the normal treatment and follow-up schemes.
Patients with a strong indication for cancer therapy, high infectious risk, and high risk of cardiotoxicity. These patients should possibly receive therapies with reduced risk of cardiotoxicity (e.g. liposomal anthracyclines instead of standard anthracyclines, regimens that exclude the most dangerous drugs for that patient) and that require the minimum number of accesses for treatment (oral therapies preferable to infusional therapies, except in the case of those at risk for acute ischaemia) and for monitoring.
Use of echocardiographic techniques
Point-of-care ultrasound can be used to improve patient management, especially in this long pandemic period89 by ruling out ‘unnecessary’ examinations and reducing the physician–patient contact. Bedside POCUS is focused on a specific clinical issue in different clinical scenarios such as ICU (Focused Intensive Care Echo—FICE),90 emergency room (Focused Echocardiography in Emergency room—FEEL),91 or cardiac examination (Focused cardiac Ultrasound—FOCUS).92
Recently, the acronym FECO (Focused Echo in Cardio-Oncology)93 has been proposed as a protocol to be used in cardio-oncology patients, mainly during pandemic. The FECO should give answer to some specific issues during antineoplastic treatment by the use of an ECG-gating echograph with standard protocols (linked to an electronic storage system) allowing the evaluation of both the heart and other organs such as the lung. The FECO has a problem-oriented, semi-quantitative, repeatable, and ‘time saving’ approach, which must give unambiguous answers with bimodal response (yes/no) using dedicated projections.
In the symptomatic patient, the FECO is guided by the symptoms while in the asymptomatic patient, the examination is guided by the risk of a specific cardiac toxicity. The approach is aimed at the heart, lung, and vena cava, but with a problem-oriented and not organ-oriented ‘vision’.94
In the differential diagnosis between cardiac and respiratory dyspnoea,95 it is mandatory to perform a chest scan in search of pulmonary B lines (‘comets’) with the near certainty that their absence with the presence of A lines rules out a cardiac cause.96 In case of hypotension, an echoscopy of the left ventricle might show a ‘kissing ventricle’ with a collapsed vena cava97 and absence of pulmonary comets. In asymptomatic patients at risk for ventricular dysfunction, the FECO has been proposed in follow-up period98 depending on the basal risk for cardiac toxicity and on the drug used. In the case of a foreseeable valvular pathology, it is fundamental to describe only the severity of valvular dysfunction and the right/left ventricle function. Pericardial involvement may be the result of radiation therapy, chemotherapy, or specific tumours, such as lung, breast, laryngeal, leukaemia, or lymphomas,99–102 but it has also been reported in COVID-19 patients, therefore, aetiologic diagnosis may be complex. Repeated FECO exams should be aimed at the identification of pericardial effusion and its quantification through careful measurement and accurate description of the patient’s decubitus, ultrasound projection, and location where the different measurements occurred, thus allowing a proper monitoring. Confirmation of tamponade, constriction, and restriction must take into account the clinical and haemodynamic context and requires a standard complete echocardiographic study.
It has been widely described that COVID infection is known to induce a pro-thrombotic state103,104 that can overlap with a similar condition related to cancer itself or anticancer treatments.
When pulmonary hypertension is a possible side-effect of cancer treatments in a COVID-19 patient, differential diagnosis could be a hard challenge. The FECO protocol in this setting includes measurement of ventricular size and detection of right-section overload signs. The presence of pericardial effusion as a negative prognostic sign should also be highlighted.
It can be concluded that FECO performed in the outpatient cardiology clinic can play a central role in the management of cancer patients, ensuring a wide and cost-effective access during and after treatment. The FECO could select patients with high probability of cardiac toxicity requiring a full echocardiographic examination. The FECO can allow an effective evaluation of the patient avoiding unnecessary hospital visits and therefore reducing the risk of infection not only for patients but also for healthcare providers.
Monitoring cardiotoxicity in course of pandemia
Cardiovascular screening and monitoring in patients receiving potentially cardiotoxic cancer therapies are a pillar of the cardio-oncology practice in order to decrease cardiac side-effects resulting in a global survival gain.105 Given the risks of infection for both physicians and patients during in-person consultation, consideration should be given to provide a new organization in the current practice of cardiac screening, monitoring, and follow-up during cancer treatment.52 It is important to remember that the present recommendations have been written during the pandemic period and is based on the consensus of experts and must be considered as temporary. It is suggested to continue cardiac surveillance in those cancer patients with a higher probability to develop cardiotoxicity in a short time and/or when an appropriate cardiological treatment could be useful to avoid delays or early interruptions of anticancer treatment programme.
A multidisciplinary and multi-professional involvement is mandatory to get this goal. In accordance with the oncologists/haematologists, cardiological visits should coincide with cancer therapy administration to reduce the need of hospital accesses. Cardiac imaging monitoring should be focused on the predicted toxicity such as the evaluation of left ventricular ejection fraction (LVEF) for anthracyclines and anti-Her2 therapy. Alternative imaging techniques [as computed tomography (CT) scan, cardiac magnetic resonance, and nuclear medicine techniques],106,107 although increasing social distance, are not universally available in a timely way.
During pandemic, it could be reasonable to reduce the general duration of echo examination and to postpone global longitudinal strain analysis.108 Monitoring with serial troponin (T) and/or brain natriuretic peptide has been proposed to reduce the frequency of imaging given its high negative predictive value.109 It can be reasonable to delay examinations in those asymptomatic patients with persistent negative values (<99° percentile) but this approach should be reserved to those centres with a specific expertise.
The proposed recommendations are focused on the general surveillance schedule for patients receiving anthracyclines and anti-HER2 agents but they should be tailored on each single cancer patient needs. To date, there are no common recommendations for patients monitoring during fluoropyrimide but it could be appropriate to use stress imaging instead of exercise stress technique when needed. Cardiac side-effects of immunotherapy (myocarditis and CRS-associated myocardial injury) may mimic cardiovascular complications secondary to COVID-19 and may delay the diagnosis and the appropriate management.110 Therefore, the cardiology consultation is of primary importance.
Baseline evaluation of cancer patient
Anthracyclines
Baseline cardiac imaging should be offered to patients with a known or suspected cardiac disease, to those with signs or symptoms of ventricular dysfunction and/or with two or more cardiotoxicity risk factors (age ≥60 years, hypertension, diabetes mellitus, dyslipidaemia, smoking, or obesity). It may thus be reasonable to temporarily delay basal evaluation in asymptomatic and low-risk patients. However, for adult patients whose only risk factor is a planned high cumulative anthracycline dose (≥250 mg/m2), it may be reasonable to delay imaging until this threshold dose is reached or at the end of treatment.111
Trastuzumab
Basal screening should be reserved to those patients with a known cardiac disease, with signs or symptoms of ventricular dysfunction and/or with 2 or more cardiotoxicity risk factors (age ≥60 years, hypertension, diabetes mellitus, dyslipidaemia, smoking, or obesity) in association with anthracyclines. In patients without valvular disease and a normal ventricular function (LVEF ≥55%) assessed in the previous 6 months, it is reasonable to avoid basal evaluation.111
Surveillance during treatment
Anthracyclines
A recent multi-centre observational study in patients receiving anthracycline reported a high cumulative incidence of cardiac dysfunction of about 37.5%, but severe toxicities were very rare. The majority of cardiac dysfunction were mild and moderate with a very low mortality rate. Therefore, it could be reasonable to delay routine imaging during anthracycline therapy in the general population and reserve it to the following cases: signs and symptoms of HF or anthracycline dosages >400 mg/m2 or cardiac risk factors and need for anthracycline therapy >250 mg/m2 particular when there is a potential clinical impact of cardio-protective strategies.
In those centres where biomarkers are routinely tested, we suggest to use routine cancer treatment-related blood draws to minimize exposures. In case of significant rise of biomarkers, the patients will undergo cardiological evaluation.111
Trastuzumab
In the adjuvant setting, asymptomatic women without CVR factors and not previously treated with anthracycline may undergo echocardiography at 6 and 12 months only. In the metastatic setting, an echocardiogram could be performed every 6 months in asymptomatic patients. In patients with risk factors such as previous anthracycline treatment, age ≥60 years, hypertension, diabetes, dyslipidaemia, smoking, and obesity, it is necessary to keep cardiac surveillance every 3 months as ESMO guidelines suggested. Patients with borderline [ejection fraction (EF) 50–55%] or reduced LVEF or with signs or symptoms of HF must continue to have imaging as per clinical practice.
In those centres where biomarkers are routinely tested, we suggest to use routine cancer treatment-related blood draws to minimize exposures. In case of significant rise of biomarkers, the patients will undergo cardiological evaluation.111
Follow-up
It may be reasonable to delay routine follow-up in asymptomatic survivors of paediatric, adolescent, and young adult cancers during pandemic. Immediate cardiological consultation will be provided in case of symptoms or signs of cardiac toxicity (Table 1).
Telemedicine, patient, and caregiver empowerment
Pandemic has forced many patients to stay at home for long time. The availability of electronic devices together with the closeness of caregivers could promote a wider use of telemedicine or web-based platforms for consultations. This obviously applies to cardio-oncology monitoring strategies. Patient (or caregiver)-reported symptoms coupled with electronic devices able to monitor cardiovascular parameters could represent the first step to select patients needing an in-person visit. A dedicated nurse is the key to successfully manage this process.
Modulation of therapeutic strategies in cancer patients with COVID-19
Heart failure
The patients with chronic HF have an increased risk of ARDS and death when infected by common influenza viruses, because of increased viscosity during febrile illnesses, heightened coagulation systems, proinflammatory effects, endothelial cell dysfunction, and bacterial infection.112 The same mechanisms are common in the COVID-19 patients, with the additional frequent manifestation of interstitial pneumonia and pulmonary thrombo-embolism.27,113
Diuretics. The doses must be adjusted considering both the risk of lung congestion, worsening of EF and the risk of hypovolaemia, dehydration (from losses due to fever, sweating, anorexia, increased respiratory rate, shift from intravascular and extravascular space, gastrointestinal losses), and/or COVID-19-related hypotension.114
Angiotensin-converting enzyme inhibitors, ARBs, or AT receptor–neprilysin inhibitors. Arterial hypotension due to COVID infection, antiviral treatment, or an evolution to the cardiogenic shock may require dose reduction or discontinuation of the drug.
Beta-blockers may be started or up-titrated if patients, as frequently happens, have tachycardia or rapid atrial fibrillation (AF). Caution should be used in case of hypotension, and in patients treated with antiviral agents, which can decrease heart rate.
Ivabradine is a valid alternative or integration to beta-blockers in the patients in sinus rhythm.
Anticoagulants are indicated in all hospitalized patients with COVID-19, because of the increased risk of thrombo-embolic complications especially with elevated D-dimer levels or signs of sepsis-induced coagulopathy.115 This suggestion can be extended to patients with HF and is even stronger in patients with active cancer, who are already at high thrombotic risk. Prophylactic doses of low molecular weight heparin (LMWH) are recommended for all cancer patients with HF and COVID-19.
Myocardial infarction
Primary angioplasty is the standard therapy for acute ST-elevation myocardial infarction (STEMI). While fibrinolytic therapy is proposed for patients without cancer disease when coronary angiography is not feasible, cancer patients typically have absolute or relative contraindications to this therapy with a high risk of bleeding. Although a significant percentage of these patients do not require myocardial revascularization because of a high prevalence of non-obstructive coronary artery disease,116 evaluating the risks and benefits in this particular context, an initial invasive strategy may be appropriate. The Cardiac Angiography and Interventions Society and the American College of Cardiology recommend this approach even during the pandemic period.117 The majority of cancer patients with COVID-19 has a type 2 myocardial infarction, secondary to acute stress, hypoxaemia, or excessive inflammation secondary to cytochine release,118 in these cases, a conservative approach, aimed to treat the acute underlying condition, is suggested.119 In patients with COVID-19 and diagnosis of NSTEMI or unstable angina, a conservative strategy should be considered, too. A dual antiplatelet therapy is usually suggested in cancer patients; with aspirin proven to be safe even in presence of thrombocytopenia.120,121 However, the possible interactions with other drugs (mostly antivirals), which might be prescribed for COVID-19 must be taken into account: Aspirin and Prasugrel are less affected, while the activity of clopidogrel may be reduced, and that of ticagrelor increased.122,123 Although no significant clinical data are available, based on its potential benefits and safety data, it is recommended that statins continue to be administered in all patients. As far as beta-blockers are concerned, the same pros and contras already mentioned above should be considered.
Takotsubo syndrome
Takotsubo syndrome (TTS) is frequent in cancer patients: in a wide multicentre database, 16.6% of patients were affected by cancer.124 Since emotional stress is one of the leading causes of TTS, it is not surprising that during COVID-19 pandemic the incidence of TTS increased from 1.5–1.8% to 7.8%.125 The haemodynamically stable patients may be treated following the guidelines above described for the low EF Congestive Heart Failure (CHF).126 Beta-blocker therapy can prevent stress triggers and subsequent catecholamine spikes, it may be associated with an ACEI or ATII receptor blocker (ARB) and/or diuretics when there is volume overload.
Myocarditis
Myocarditis has been described in COVID-19 patients, even if its true incidence is unknown, because the clinical presentation and the ECG and biomarkers changes may be similar to those observed in ACS, STEMI, CHF, or cardiogenic shock.127 The rationale of therapy depends on the nature of myocarditis: cytopathic (by virus replication) vs. immune-mediated. The presence of SARS-CoV-2 virus in the myocardium has been seldom reported128 and the delayed onset of signs of myocarditis (up to 10–15 days after the onset of symptoms) is consistent with other pathogenic mechanisms: endothelitis, a cytokine-related autoimmune myocarditis, or an autoimmune reaction secondary to myocardial damage.129,130 Current data on the use of glucocorticoids remain controversial, because no studies have been conducted to confirm their efficacy in COVID-19 myocarditis. While it has been reported that corticosteroid therapy may delay virus clearance, in contrast, a Wuhan study involving 84 patients with ARDS secondary to COVID-19, administration of corticosteroids reduced mortality.131 Immunoglobulins have been found to be useful in some types of myocarditis.132 To date, there is still no evidence-based treatment for COVID-19 myocarditis; the patients reported in the literature were treated with a variety of approaches beside support and CHF therapy, with a mortality of 27%.133–136 In the setting of cancer patients, it is of utmost importance to make a differential diagnosis between myocarditis secondary to SARS-CoV-2 and myocarditis due to antineoplastic therapies (mostly to ICI), the latter being responsive to high-dose steroid therapy.137
Valvular heart disease
During and after the COVID-19 pandemic, limited resources in ICUs or hospital beds may make it difficult to schedule valve surgery. In this context, less invasive procedures with a low/reasonable risk of complications and minimal use of resources, as well as limited risk of exposure for health care staff, should be promoted. The Transcatheter Aortic Valve Implantation (TAVI),138,139 to improve the patient’s condition is reported to be safe and effective even in cancer patients, whose traditional surgery is considered high risk.140 However, when the patient's clinical condition allows a delay, percutaneous valve replacement should be postponed with a priority for rescheduling. Selected patients with mitral regurgitation or tricuspid regurgitation may receive transcatheter treatment rather than traditional cardiac surgery. However, these patients should be carefully evaluated taking into account the increased risks to the medical team associated with aerosol during transoesophageal echocardiography.141 If possible, in patients with severe mitral insufficiency, therapy should be optimized to delay implantation of the Mitraclip until the COVID-19 infection has resolved.
COVID treatments
Steroids
Steroids are used in severe COVID-19 pneumonia (in the RECOVERY study the incidence of death was lower in the dexamethasone group than that in the usual care among patients receiving invasive mechanical ventilation [29.3% vs. 41.4%; rate ratio (RR) 0.64; 95% CI 0.51–0.81] and among those receiving oxygen without invasive mechanical ventilation (23.3% vs. 26.2%; RR 0.82; 95% CI 0.72–0.94]), even if they had no effect on the mortality rate of those patients with a mild form of the condition.142–144 The common side-effects of corticosteroids used for pneumonia include diabetes and hypertension, but not an increase of cardiac adverse events and superinfections.145
Experimental drugs
A wide variety of antiviral agents and anti-inflammatory drugs have been tested for COVID-19 treatment; many of them may have cardiac adverse side effects (as QT interval prolongation and potentially severe arrhythmias, for instance) or metabolic interaction with some cardiovascular drugs. Amongst these treatments, drug interactions involving the HIV protease inhibitor lopinavir/ritonavir were the most frequent, followed by chloroquine, hydroxychloroquine, and ruxolitinib, with anakinra, baricitinib, favipiravir, interferon-β, nitazoxanide, ribavirin, remdesivir, sarilumab, and tocilizumab having low propensity for drug interactions.146,147 Due to the continuous evolution of the treatment approved for clinical use, a constantly updated website as https://www.covid19-druginteractions.org should be consulted before prescribing any new drug.
Atrial fibrillation in cancer patients: management in the COVID-19 era
One of the arrhythmic complications of COVID-19 is AF, the treatment of which is notoriously complex in cancer patient.
Inflammation and atrial fibrillation in COVID-19
Inflammation, which is high in cancer patients, becomes even higher when these patients contract COVID-19 infection. The physiopathology underlying this process is linked to an abnormal immune response that can result in cytokine storm syndrome. In fact, there is an increase in a large number of inflammation markers including TNF-alpha, interleukin IL 1-β, IL-1RA, IL-7, IL-8, IL-9, IL-10, fibroblast growth factor, granulocyte colony-stimulating factor), granulocyte-macrophage colony-stimulating factor, interferon gamma, interferon gamma-induced protein 10, monocyte chemoattractant protein-1, macrophage inflammatory proteins 1A, 1B, platelet-derived growth factor, and vascular endothelial growth factor.148 Some cytokines may affect cardiomyocytes, and thus cause AF. Many cytokines are regulated by the multi-protein complex NLRP3 inflammasome. The hyperactivation of this complex induced by the SARS-CoV-2 virus triggers strong inflammation in cardiomyocytes and endothelial cells, which in turn results in the hypersecretion of growth factors and chemokines that increase fibrosis and apoptosis. Selective inhibitors of NLRP3 are currently used to mitigate respiratory distress and prevent AF and myocarditis in COVID-19 patients. There is evidence that hydroxychloroquine may reduce the activity of NLRP3 in inflammatory cells. Tocilizumab, which is an inhibitor of IL-6, has also been used in trials to treat COVID-19.
Management of atrial fibrillation
The European Heart Rhythm Association has cleared the use of direct oral anticoagulants (DOACs) to treat AF.149 The sub-analyses of the ARISTOTLE,150 ENGAGE,151 and ROCKET152 studies support the use of apixaban, edoxaban, and rivaroxaban in cancer patients. More recently, in a meta-analysis, Cavallari et al.153 reported that, in patients with both AF and cancer, DOACs are at least as effective as vitamin K antagonists (VKAs) in preventing thrombotic events. Moreover, DOACs reduce intracranial bleeding and may be a valid and more practical alternative to VKAs in these high-risk patients. Deng et al.154 reported that, in patients with AF and cancer, DOACs had similar rates of thrombo-embolic and bleeding events and a reduced risk of venous thrombo-embolism and intracerebral haemorrhage. Therefore, DOACs are increasingly used in cancer patients. The Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis recommendations regarding the use of DOAC are shown below155:
A DOAC is recommended over a VKAs or LMWH as anticoagulant therapy if no clinically relevant drug‐to‐drug interactions are expected in cancer patients with de novo non-valvular AF receiving chemotherapy, exceptions being patients with luminal gastrointestinal cancers with an intact primary and patients with active gastrointestinal mucosal abnormalities such as duodenal ulcers, gastritis, esophagitis, or colitis.
In cancer patients with non-valvular AF who were on an anticoagulant regimen before starting chemotherapy, continuing the same anticoagulation regimen is recommended, unless there are clinically relevant drug–drug interactions.
Obviously, in case of COVID-19 infection, all the aspects linked to the virus-induced hypercoagulable state have to be considered. The rates of hypercoagulability are higher in patients with COVID-19 than in the general population, and more than one-fourth of COVID-19 patients have venous thrombo-embolism, which is known to be related to fibrin hyperpolymerization. Moreover, vein thrombosis is more likely in cancer patients, since venous thrombo-embolism is the second leading cause of death after cancer.
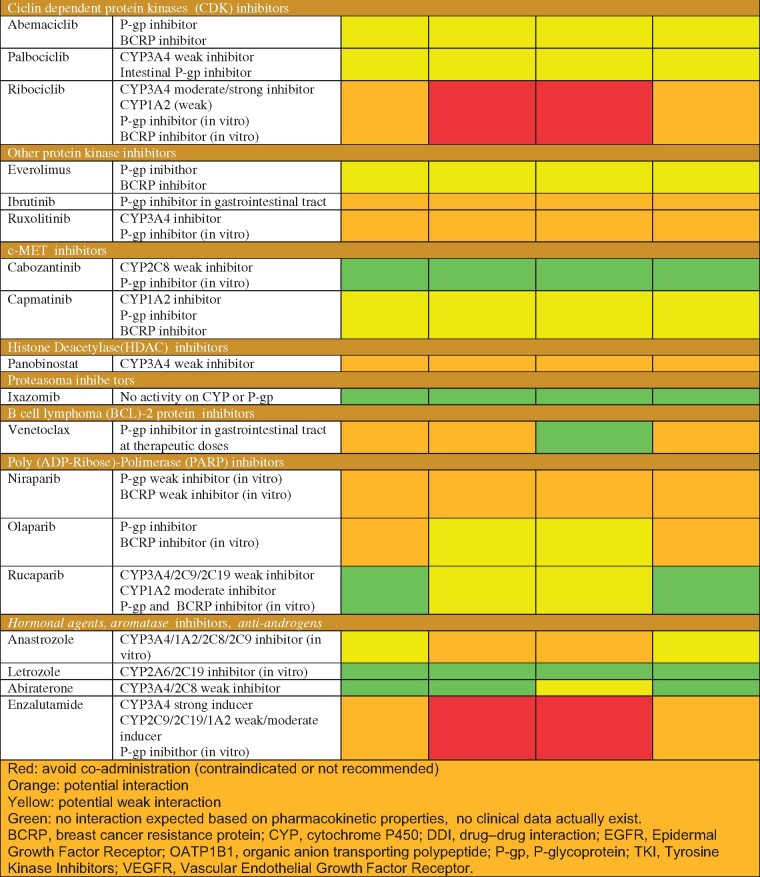
Drug interactions, too, must be taken into account and managed accordingly in patients simultaneously affected by CVD, cancer, and COVID-19—and undergoing treatment for active cancers. Both interactions between DOACs and anti-cancer drugs and interactions between DOACs and drugs used to treat COVID-19 need to be carefully addressed (Table 2).
Table 2.
Predictable pharmacokinetic interactions between oral anticancer agents and direct oral anticoagulants modified from Gatti et al.156
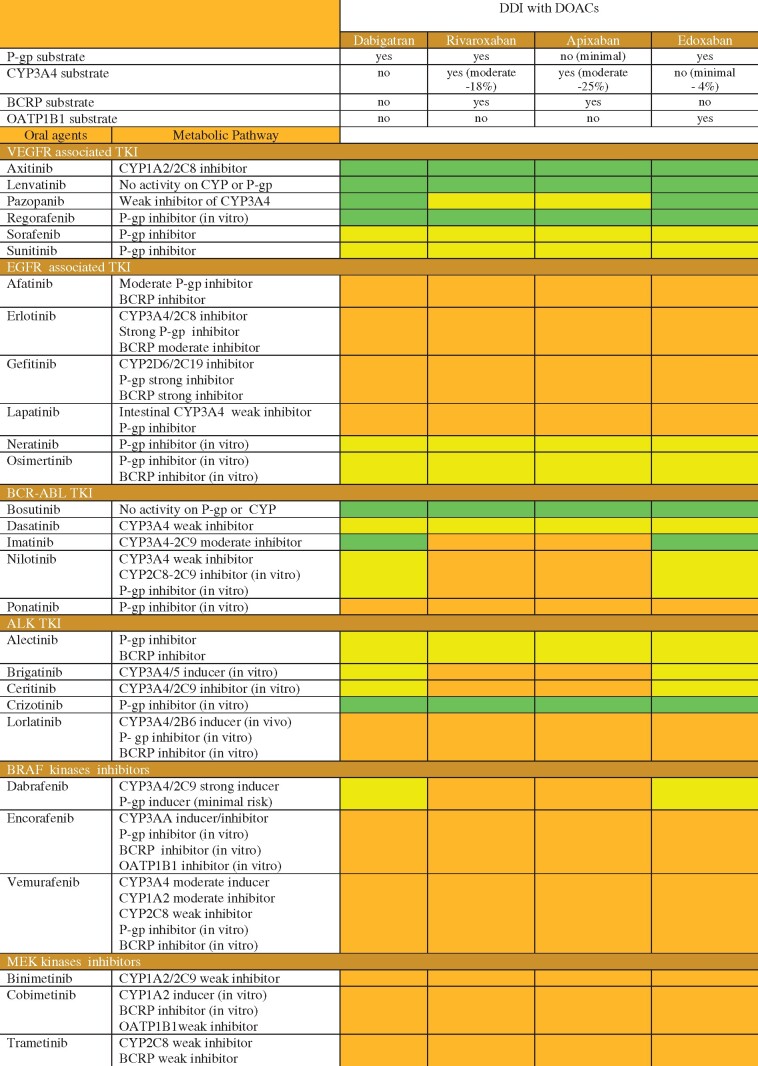
|
All DOACs are P-glycoprotein substrates, whereas only rivaroxaban, apixaban, and—to a lesser extent—edoxaban are substrates of cytochrome P450. The interactions occur because anti-cancer drugs (traditional, biological, and hormones) and COVID-19 drugs are either inductors or inhibitors of these metabolic pathways.
Even though some DOACs have a mild effect on the activity of cytochrome P450 enzymes, they do not affect the plasma level, effectiveness, and/or toxicity of cancer drugs. However, haemorrhagic toxicity is possible depending on cancer location, characteristics of patients, and co-administration of cancer drugs that have intrinsic gastrointestinal toxicity. On the contrary, cancer drugs may increase or decrease the plasma levels of DOACs depending on whether they induce or inhibit the metabolic pathways of cytochrome or glycoprotein and thereby affect the safety and efficacy of DOACs.156
Direct oral anticoagulants and drugs used to treat COVID-19
Chloroquine and hydroxychloroquine may increase plasma levels of dabigatran and edoxaban, the doses of which should be reduced accordingly, but they do not affect the levels of rivaroxaban or apixaban. Remdesivir, a widely used antiviral medication does not affect the plasma level of any DOAC whereas other antiviral drugs such as Lopinavir/Ritonavir and Atazanavir are CYP3A4 inhibitors and moderately increase the plasmatic level of dabigatran and edoxaban while greatly increasing the level of apixaban and rivaroxaban.156,157 Tocilizumab and sarilumab, both interleukin inhibitors, may increase the plasma levels of rivaroxaban and apixaban. The mechanism underlying the increase in plasma levels of these two DOACs is related to the fact that high levels of IL-6 suppress the activity of cytochrome P450 and glycoprotein metabolic pathways.158,159 Treatment with tocilizumab or sarilumab restores enzyme activity to its pre-COVID infection level.160,161 Therefore, caution should be exercised in COVID-19 patients undergoing treatment with IL-6 receptor antagonists and in using DOACs metabolized by cytochrome P450 as apixaban and rivaroxaban. Thus, in some cases, it is advisable to switch to LMWH at anticoagulant doses when administering antiviral drugs that may affect plasma levels of DOACs. Moreover, managing macrolides is also very important, the most widely used one being azithromycin. Macrolides are mild inhibitors of P-glycoprotein and an over exposure to DOACs can occur during concomitant treatment156; therefore, a switch to LMWH at anticoagulant doses may be suggested during macrolide treatment.
In conclusion, patients with AF infected with SARS-CoV-2 are at a high risk of thrombo-embolism, they need a tailored antithrombotic treatment that takes into account the interactions between DOACs and antiviral or cancer drugs.
Prophylaxis and treatment of thrombo-embolic complications in severe acute respiratory syndrome coronavirus 2 infection
Cancer disease and some anticancer therapies are established risk factors for venous thrombo-embolism (VTE)162 and COVID-19 seems to be an additional risk factor.
Scientific literature has documented a higher rate of VTE in patients hospitalized with COVID-19 when compared with hospitalized patients without COVID-19.163 In a population of cancer patients (in and outpatients) with COVID-19, the reported rate of VTE complications was 3.5%. Furthermore, VTE was more common in patients on anticancer therapy than in those without recent or ongoing anticancer treatment (5.2% vs. 2.2%) and in patients with the progressive disease compared with those in remission (7.1% vs. 2.0%).164
Although the exact pathophysiologic mechanisms underlying thrombotic complications are not clearly defined, a severe systemic inflammatory response and endothelial activation due to endothelial cell infection seem to be the main causes of a prothrombotic state in patients with COVID-19.165 In these patients, COVID-19-associated coagulopathy has been reported, which is characterized by increased D-dimer and fibrinogen levels, a modest decrease in platelet count and prolongation of prothrombin time.166 These coagulation abnormalities have been found to be associated with an increased risk of adverse events, such as subsequent mechanical ventilation, ICU admission, and death. Of note, SARS-CoV-2 RNA has been documented in platelets of COVID-19 patients.167 It has been postulated that COVID-19 VTE pathophysiology could involve platelet hyper-reactivity and be more platelet-dependent than in non-COVID-19 conditions.168 A Chinese nationwide study that evaluated VTE risk with the Padua Prediction Score found that 40% of hospitalized patients with COVID-19 were at high risk of VTE.169 In a meta-analysis including 18 093 hospitalized patients with COVID-19, the overall pooled reported incidence of VTE was 17%.170 Venous thrombo-embolism risk should be evaluated in all hospitalized COVID-19 patients utilizing risk-assessment tools, such as the Caprini model or Padua score.171 Since patients with COVID-19 can rapidly develop severe complications, including renal, respiratory, and liver failure, that can impact both VTE and bleeding risk, antithrombotic treatment should be implemented early and cautiously in hospitalized patients.
COVID-19 amplifies the risk of VTE of cancer and antineoplastic therapies. In a retrospective study that first compared patients hospitalized for COVID without cancer vs. patients with active cancer, a high rate of thrombosis was observed among patients hospitalized with COVID-19 with a cumulative incidence of 18% at 28 days among those without cancer and 14% among those with cancer. Considering that the incidence of hospitalization-related thrombosis in patients with cancer ranges from 2% to 22% the study surprisingly found similar VTE data between COVID-19 patients with cancer and without cancer. This could reflect the considerable thrombo-inflammatory state of active COVID-19 overshadowing the hypercoagulable state of cancer.172
Venous thrombo-embolism management in hospitalized patients
Prophylaxis of venous thrombo-embolism in patients hospitalized with COVID-19 and malignancies
In clinical practice, VTE prophylaxis must be considered in all hospitalized COVID-19 patients. Firstly, bleeding risk and coagulation parameters, including complete blood cell count, prothrombin time, and activated partial thromboplastin time (aPTT), fibrinogen, and D-dimer levels, should be assessed in all patients. A comprehensive evaluation must also consider comorbidities such as renal or hepatic dysfunction. In the absence of randomized clinical trials conducted in the COVID-19 patient population and in the COVID and cancer population, pharmacologic management should take into account the recently published recommendations of the COVID-19 Thrombosis Collaborative Group166 and the guidelines on VTE in oncology.173,174
Patients with COVID-19 and cancer should receive pharmacological thromboprophylaxis unless contraindicated. First-line treatment should be with LMWH [i.e. enoxaparin 40 mg subcutaneous (sc) once a day], a possible alternative is fondaparinux 2.5 mg sc once a day. It seems reasonable to suggest that, due to very high thrombotic risk, patients with active cancer and severe COVID-19 would receive intermediate doses of LMWH and that monitoring of anti-Xa levels could optimize anticoagulation. If pharmacologic prophylaxis is contraindicated, mechanical VTE prophylaxis (intermittent pneumatic compression) should be considered in immobilized patients.175
Actually, due to the lack of clear benefits of therapeutic or intermediate anticoagulant doses, and pending findings of ongoing randomized trials investigating the most effective VTE prophylaxis in COVID-19 patients, standard thromboprophylaxis anticoagulant dosing is currently recommended by the World Health Organization.176 Once-daily LMWH or fondaparinux are preferred over unfractionated sodium heparin (UFH) due to lower healthcare professional exposure and a more stable anticoagulant effect over time. Of note, particular clinical settings such as obesity or renal failure may require dosing adjustments or different strategies.177,178
Post-hospital discharge venous thrombo-embolism prophylaxis in patients hospitalized with COVID-19 and malignancies
The role of extended prophylaxis after hospital discharge has not been studied in COVID-19 patients. However, in patients with active cancer, extended thromboprophylaxis with LMWH (for up to 6 weeks) seems reasonable after hospitalization for COVID-19, especially in cases of reduced mobility and low bleeding risk.176
Venous thrombo-embolism prophylaxis in home-managed cancer patients with COVID-19
Asymptomatic COVID-19 patients or those with mild symptoms are often managed at home. Overall, the role of thromboprophylaxis in this setting is not well established. However, the presence of active cancer associated with COVID-19 and reduced mobility due to quarantine are all conditions that increase VTE risk, therefore, the use of pharmacological thromboprophylaxis should be considered in these patients.173
Venous thrombo-embolism treatment in hospitalized patients with COVID-19 and malignancies
In hospitalized patients, parenteral anticoagulation (LMWH or UHF) is preferred as it can be temporarily discontinued and has no known drug interactions with experimental COVID-19 therapies. In patients hospitalized with COVID-19 and already on oral anticoagulant treatment, a switch to parenteral anticoagulant therapy should be considered.175 Indeed, as compared with parenteral anticoagulants, oral anticoagulants have a higher risk of drug interaction with experimental COVID-19 pharmacological treatment. We have already described some interactions, further informations on potential drug interactions of oral anticoagulants with anti-COVID-19 drugs are available at https://www.covid19-druginteractions.org/.
Another advantageous aspect of parenteral anticoagulation is the shorter duration of the anticoagulant effect, which may be crucial if urgent invasive procedures are required. Moreover, it is necessary to consider that patients treated with UFH require monitoring of the therapeutic effect through blood samples to be performed several times a day to control the aPTT, thus exposing the health care personnel to a greater risk of infection.
It is necessary to consider that in patients with onco-haematologic diseases severe thrombocytopenia may be present and may require platelet transfusion (e.g. if the platelet count is <30 000/µL) before starting anticoagulant treatment.179
In COVID-19 patients imaging examinations should be promptly performed in case of pulmonary embolism (PE) clinical suspicion. However, in ICU patients, the difficulty in mobilizing mechanically ventilated patients to CT machines and the need to limit healthcare exposure to COVID-19 may hinder CT examination. Lower extremity ultrasound may also be limited due to patient positioning. When it is not possible to obtain lung CT angiography, the occurrence of sudden respiratory decompensation or evidence of acute unexplained right ventricular dysfunction on echocardiography may raise the suspicion of acute PE. Due to the common presence of increased levels of D-dimer in critically ill COVID-19 patients and the absence of established cut-off values to identify a higher risk of VTE in these patients, elevated D-dimer values are not enough to raise the suspicion for VTE. Furthermore, it should be considered that increased D-dimer levels are also dependent on tumour-related factors in cancer patients.180
In COVID-19 patients with a high suspicion of acute PE that cannot be confirmed with diagnostic imaging, a therapeutic dose of parenteral anticoagulants is suggested unless specific contraindications exist.181 Even in VTE treatment, parenteral anticoagulation is suggested over oral anticoagulation due to the high risk of an abrupt decline in clinical status.182 In patients with a VTE diagnosis and spontaneous prolonged clotting times (especially aPTT) or thrombo-embolism recurrence despite appropriate anticoagulation, lupus anticoagulant testing is suggested.162 At discharge, parenteral anticoagulation may be switched to oral anticoagulation. In order to limit patient access to healthcare services, DOACs may be preferred over VKAs, which require coagulation monitoring. Anticoagulation therapy is recommended for at least 3 months.181–183
In conclusion, VTE prophylaxis and treatment in cancer patients with COVID-19 is challenging. Due to the scarcity of data, current management is based on available recommendations and on VTE guidelines in oncology. However, the particularly high risk of thrombosis and bleeding events requires a tailored approach in each clinical case. Prospective randomized trials are needed to validate the most appropriate antithrombotic strategy in this specific clinical setting.
Management of arrhythmic complications and devices in the oncologic patient affected by COVID-19
Management of arrhythmias in cancer patients with SARS-CoV-2 infection is of utmost importance because both cardiotoxicity from oncologic treatment and SARS-CoV-2 infection may elicit arrhythmias.
On the one hand, the increase of the average age of people is strictly correlated to the increase of cancer and arrhythmias; on the other hand, the wide use of chemotherapy, targeted therapy, immunotherapy, and RT causes a huge increase in arrhythmic complications,184 due to myocardial ischaemia and HF.185
The most common arrhythmic complications are AF and supraventricular arrhythmias, but a QT prolongation along with ventricular arrhythmias including torsade de pointes can also occur (Table 3).
Table 3.
Potential arrhythmic adverse effects of antineoplastic drugs
| Antineoplastic drugs | Potential arrhythmic adverse effect | |
|---|---|---|
Anthracyclines
|
|
|
|
Alkylating agents Melphalan |
|
|
Inibitori delle tirosin chinasi
|
|
|
| Osimertinib |
|
|
| Pazopanib |
|
|
| Trametinib |
|
|
| Vandetanib |
|
|
| Vemurafenib |
|
|
Immune checkpoint inhibitors
|
|
|
PD-L1 inhibitors
| ||
CTLA-4 inhibitors
| ||
Histone deacetylase inhibitors
|
|
|
| Terapia endocrina | Modulatori selettivi dei recettori oestrogenici
|
|
Endocrine therapy selective modulators of oestrogen receptors
|
|
|
| Ribociclib |
|
|
| Arsenic dioxide |
|
|
The scenario of cancer treatment-induced arrhythmias has been complicated by SARS-CoV-2 intrinsic arrhythmogenic potential. Arrhythmias can be due to a direct viral effect, or may be caused by the systemic consequences of the infection and the pharmacological interactions.
The association of the viral infection with cancer and CVD is of great concern because cancer and CVD are highly common in the population and both have a worse impact on COVID-19 patients; therefore, risk stratification and measures of prevention should become a public health objective and a prompt valuation of syncope and palpitations should be part of the standard of care.
The National Health Commission of China Report shows that some patients have cardiac symptoms as chest pain and palpitations before any pulmonary manifestations.118
Ventricular arrhythmias can be the first clinical sign of COVID-19.186 Atrial fibrillation, atrial flutter, heart block, monomorphic, polymorphic, multifocal ventricular tachycardia, and ventricular fibrillation have been also described. These arrhythmias have also been associated to SARS-CoV-2-induced myocarditis that can be due to a direct toxic effect of the virus and myocardial involvement, but also to extrapulmonary macrophages migration which could damage the conduction system.
Severe acute respiratory syndrome coronavirus disease determines a huge release of inflammatory agents, which play a crucial role in arrhythmogenicity. Cytokine storm and T lymphocytes cause an immune activation feedback, and a myocardial injury with increase of cardiac markers such as troponin,187,188 a trigger for arrhythmias,189 with an incidence of 44% in patients with severe COVID-19 infection,190 leading to a higher mortality risk.74 Interleukin-6, tumoural necrosis alfa factor and interleukin 1 release determine a prolongation of potential ventricular action acting on potassium and calcium channels.191 Interleukin 6 increase can cause QT prolongation favouring Torsade de Points.192 Myocardial localization of the virus, electrolytic alterations, and myocardial remodelling associated with myocarditis cause life-threatening arrhythmias, due to metabolic disarray, hypoxia, inflammation neuro-hormonal stress,193 and a possible concomitant coagulopathy causing hypoxia-related thrombosis.194
Cardiac arrhythmia incidence is significantly higher in patients with poor outcome with a rate of 48%195; it can be considered a marker of poor prognosis.
Bradyarrhythmias are associated with particularly high values of inflammatory markers and a high short-term mortality rate. The management strategy of these patients should take into account both the potential adverse outcome of invasive pacing and the physician’s potential risk of transmission.
In patients with pre-existing cardiovascular comorbidities, the viral infection can have a highly negative effect due to the increased metabolic demand associated with reduced cardiac reserve.196 This precarious balance, added to the direct myocardial damage and the inflammatory response triggered by the viral agent, can increase the risk of acute coronary syndrome, HF, and cardiac arrhythmias.197
Finally, an increasing number of cancer patients have implantable cardiac devices (pacemakers or defibrillators), so that the problem of RT comes up; this treatment, although usually safe, in some circumstances can cause safety trouble to the devices and it is essential for cardiologists to have adequate knowledge in order to choose the best and safest treatment for their patients.198
Management of the cardio-oncology patient with COVID-19
Drug interactions are an important issue in the treatment of COVID-19 especially between antineoplastic, antiarrhythmic drugs, and anticoagulants drugs; therefore, it is necessary to evaluate possible interactions in each case. In COVID-19 patients, drugs that prolong QT, such as azithromycin and hydrochloroquine,199 are frequently used, increasing the risk of cardiac arrhythmias.
Some recent studies have investigated the risk of ventricular arrhythmias linked with hydrochloroquine and azithromycin therapy.200,201 It is also possible to use the Tisdale score202 for predicting the lengthening effect of the QTc interval and to apply it for choosing drugs to be used in patients with COVID-19. This effect is even more relevant if COVID-19 and neoplastic disease occur together since in this case, drugs that lengthen the QT are frequently used, and there is an additional intrinsic risk of developing arrhythmias.
The strategies of monitoring the QT interval and arrhythmias are constantly evolving. Although the standard 12-lead ECG is the most accurate method for assessing the QT interval and any cardiac arrhythmias, it is important to make some considerations on the resources to be used and on the management in the setting of COVID-19 patients. The acquisition of the standard 12-lead ECG involves both personal exposure and the equipments; therefore, the execution of electrocardiograms should be limited and only some equipment should be dedicated to COVID patients to limit possible contamination. Additionally, telemetry monitoring should be considered in high-risk patients. Other alternatives could also be considered, such as wearable devices and digital devices.
During the lockdown, a 50% reduction in the number of elective Pace Maker (PM) and Implantable Cardioverter Defibrillator (ICD) implants procedures, and AF ablation has been registered along with a decrease in emergency procedures, with a reduction of more than 50% in the number of urgent pacemaker implants for severe bradyarrhythmia. At the same time, there was an overuse of Remote Monitoring (RM), although with large differences between the various centres, The use of RM was strongly recommended by the consensus document of the Heart Rhythm Society COVID-19 Task Force.194 The consensus document splits the electrophysiological procedures into urgent, semi-urgent, non-urgent, or elective, considering urgent only procedures that considerably reduce the risk of clinical worsening, hospitalization, and death. Patients undergoing urgent procedures should always be evaluated for fever, COVID-19 symptoms, and tested for COVID-19; the infectious risk must always be limited with the use of Personal Protective Equipment (PPE) not only by the operator but also by the patient by wearing surgical masks. If it is necessary to intubate the patient, notably a procedure that generates aerosols, it is recommended to use negative pressure chambers both in the room and in the pre-room. It is also recommended to limit the number of staff in the room during intubation and extubation, and to follow the protocols relating to the length of time spent in the operating theatre which should be between 15 and 30 min. Local anaesthesia should also be preferred, if the patient's safety is not compromised. Electrocautery, a procedure routinely used in the electrophysiology room during device implants, should also be limited as it generates aerosols, producing smoke with a high viral load, so in addition to masks, it is recommended to use glasses to limit exposure of the conjunctiva.
Conclusions
One year after the COVID-19 crisis broke out, the pandemic is still in full swing. The emergence of aggressive viral variants and the difficulties in achieving vaccination coverage in the general population do not allow us to define with certainty when we will be able to overcome the COVID-19 epidemic. What we do know for sure is that social distancing and controlled access to places at greatest risk of infection, such as hospitals, are already the most effective measures to contain SARS-CoV-2 infection. In addition, the management of COVID-19 disease has led to a significant change in the organization of healthcare systems, as entire hospitals or hospital wards have been shifted to the exclusive treatment of the disease, limiting the resources dedicated to the management of other diseases The pandemic has challenged cardio-oncologists who must consider not only patients CVR but also the risk of deferring cancer treatment, and the infectious risk. Consequently, the COVID-19 pandemic had a significant impact on the management of diseases not directly related to SARS-CoV-2 infection. The uncertainty in predicting when the COVID-19 crisis will be overcome requires substantial reflection also in cardiology practice in order to effectively prevent and treat cardiotoxicity.
The fundamental question that the COVID-19 crisis forces us to ask is therefore: how can we create an effective and efficient management programme while maintaining social distances and limiting access to the hospital? One positive fact that emerged during the COVID-19 era was the impetus given to the development and dissemination of telemedicine, which can be a valuable tool for respecting distances and avoiding infections without reducing control. The progression towards electronic medical records can facilitate the sharing of information between the different categories of specialists involved in patient care and in different environments (hospital and outpatient clinics) thus improving continuity of care. Virtual platforms can be particularly useful for multidisciplinary specialist discussion on the care of the cardio-oncological patient and in general can also be used for video consultation with the staff involved in cardio-oncological care and with the patient himself. If telemedicine is an answer to the question of how to follow patients, it is also crucial to understand which patients should be followed. In this perspective, the basal assessment before the start of therapy becomes fundamental to intercept and select the high-risk conditions that in the cardio-oncology field are always to be related to the therapeutic programme.
In the near future, it may be useful to have virtual-hybrid clinics that provide virtual and in-person visits from the outset to address, in a more personalized way, the needs of cancer patients.203
The SARS-CoV-2 pandemic has also stimulated the study of thrombogenicity and inflammation, preparing us for a unique challenge for translational investigations that may pave the way for tailored therapeutic interventions. The tremendous impact of the virus on CVD and cancer patients should fuel a vigorous campaign to implement healthy lifestyles to reduce the burden of CVD and cancer and improve the health of our planet.
Disclaimers
This Position Paper was originally published in the Italian language in ‘Position paper ANMCO: Cardio-oncologia in era COVID-19’, official journal of Italian Federation of Cardiology (IFC), published by Il Pensiero Scientifico Editore. Translated by a representative of the Italian Association of Hospital Cardiologists (ANMCO) and reprinted by permission of IFC and Il Pensiero Scientifico Editore.
Conflict of interest: none declared.
References
- 1.Zhang X.Epidemiology of Covid-19. N Engl J Med 2020;382:1869–1870. [DOI] [PubMed] [Google Scholar]
- 2.Wiersinga WJ, Rhodes A, Cheng AC, Peacock SJ, Prescott HC.. Pathophysiology, transmission, diagnosis and treatment of coronavirus disease 2019 (COVID-19) a review. JAMA 2020;324:782–793. [DOI] [PubMed] [Google Scholar]
- 3.Hoffmann M, Kleine-Weber H, Schroeder S, Krüger N, Herrler T, Erichsen S, Schiergens TS, Herrler G, Wu N-H, Nitsche A, Müller MA, Drosten C, Pöhlmann S.. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 2020;181:271–280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Siddiqi HK, Libby P, Ridker PM.. COVID-19—a vascular disease. Trends Cardiovasc Med 2021;31:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maringe C, Spicer J, Morris M, Purushotham A, Nolte E, Sullivan R, Rachet B, Aggarwal A.. The impact of the COVID-19 pandemic on cancer deaths due to delays in diagnosis in England, UK: a national, population-based, modelling study. Lancet Oncol 2020;21:1023–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Di Pasquale G, De Palma R, Fortuna D, Campo BE, Casella G.. Effetti indiretti della pandemia COVID-19 sulla mortalità cardiovascolare. G Ital Cardiol 2021;22:188–192. [DOI] [PubMed] [Google Scholar]
- 7.Rodriguez-Leor O, Cid-Alvarez B, Ojeda S.. Impact of the COVID-19 pandemic on interventional cardiology activity in Spain. REC Interv Cardiol 2020;2:82–89. [Google Scholar]
- 8.Garcia S, Albaghdadi MS, Meraj PM, Schmidt C, Garberich R, Jaffer FA, Dixon S, Rade JJ, Tannenbaum M, Chambers J, Huang PP, Henry TD.. Reduction in ST-segment elevation cardiac catheterization laboratory activations in the United States during COVID-19 pandemic. J Am Coll Cardiol 2020;75:2871–2872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vecchio S, Fileri L, Moschini RA, Lorenzetti C, Rubboli S.. Impatto della pandemia COVID-19 sui ricoveri per sindrome coronarica acuta: revisione della letteratura ed esperienza monocentrica. G Ital Cardiol 2020;21:502–508. [DOI] [PubMed] [Google Scholar]
- 10.Lipsitch M, Swerdlow DL, Finelli L.. Defining the epidemiology of Covid-19—studies needed. N Engl J Med 2020;382:1194–1196. [DOI] [PubMed] [Google Scholar]
- 11.World Health Organization. Modes of Transmission of Virus Causing COVID-19: Implications for IPC Precaution Recommendations. Report of July 9; 2020. WHO reference number: WHO/209-nCoV/Sci_Brief/Transmission_modes/2020.2.
- 12.Zheng J.SARS-CoV-2: an emerging coronavirus that causes a global threat. Int J Biol Sci 2020;16:1678–1685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Amraei R, Rahimi N.. COVID-19, renin-angiotensin system and endothelial dysfunction. Cells 2020;9:1652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ganatra S, Hammond SP, Nohria A.. The novel coronavirus disease (COVID-19) threat for patients with cardiovascular disease and cancer. JACC CardioOncol 2020;2:350–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Public Health England. Excess Weight and Covid-19. 2020. Public Health, official journal of The Royal Society for Public Health. ScienceDirect.
- 16.Yu J, Ouyang W, Chua MLK, Xie C.. SARS-CoV-2 transmission in patients with cancer at a tertiary care hospital in Wuhan, China. JAMA Oncol 2020;6:1108–1110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mehta V, Goel S, Kabarriti R, Cole D, Goldfinger M, Acuna-Villaorduna A, Pradhan K, Thota R, Reissman S, Sparano JA, Gartrell BA, Smith RV, Ohri N, Garg M, Racine AD, Kalnicki S, Perez-Soler R, Halmos B, Verma A.. Case fatality rate of cancer patients with COVID-19 in a New York hospital system. Cancer Discov 2020;10:935–941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Dai M, Liu D, Liu M.. Patients with cancer appear more vulnerable to SARSCOV-2: a multi-center study during theCOVID-19 outbreak. Cancer Discov 2020;10:783–791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Liang W, Guan W, Chen R, Wang W, Li J, Xu K, Li C, Ai Q, Lu W, Liang H, Li S, He J.. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol 2020;21:335–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kuderer NM, Choueiri TK, Shah DP.. Clinical impact of COVID-19 on patients with cancer (CCC19): a cohort study. Lancet 2020;395:190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yuen KCJ, Mortensen MJ, Azadi A, Fonkem E, Findling JW.. COVID-19 mortality in patients with cancer on chemotherapy or other anticancer treatments: a prospective cohort study. Lancet 2021;4:e00246. [Google Scholar]
- 22.Robilotti EV, Babady NE, Mead PA, Rolling T, Perez-Johnston R, Bernardes M, Bogler Y, Caldararo M, Figueroa-Ortiz C, Glickman M, Joanow A, Kaltsas A, Lee YJ, Lucca Bianchi A, Mariano A, Morjaria S, Nawar T, Papanicolaou GA, Predmore J, Redelman-Sidi G, Schmidt E, Seo SK, Sepkowitz K, Shah M, Wolchok JD, Hohl TM, Taur Y, Kamboj M.. Determinants of severity in cancer patients with COVID-19 illness. medRxiv 2020. doi:10.1101/2020.05.04.20086322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Garassino MC, Whisenant JG, Huang L-C, Trama A, Torri V, Agustoni F, Baena J, Banna G, Berardi R, Bettini AC, Bria E, Brighenti M, Cadranel J, De Toma A, Chini C, Cortellini A, Felip E, Finocchiaro G, Garrido P, Genova C, Giusti R, Gregorc V, Grossi F, Grosso F, Intagliata S, La Verde N, Liu SV, Mazieres J, Mercadante E, Michielin O, Minuti G, Moro-Sibilot D, Pasello G, Passaro A, Scotti V, Solli P, Stroppa E, Tiseo M, Viscardi G, Voltolini L, Wu Y-L, Zai S, Pancaldi V, Dingemans A-M, Van Meerbeeck J, Barlesi F, Wakelee H, Peters S, Horn L; TERAVOLT investigators. COVID-19 in patients with thoracic malignancies (TERAVOLT): first results of an international, registry-based, cohort study. Lancet Oncol 2020;21:914–922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Schmoldt A, Benthe HF, Haberland G.. ACE2 expression in the small airway epithelia of smokers and COPD patients: implications for COVID-19. Eur Respir J 1975;55: 2000688–2000692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Úri K, Fagyas M, Kertész A, Borbély A, Jenei C, Bene O, Csanádi Z, Paulus WJ, Édes I, Papp Z, Tóth A, Lizanecz E.. Circulating ACE2 activity correlates with cardiovascular disease development. J Renin Angiotensin Aldosterone Syst 2016;17:1470320316668435. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Goyal P, Choi JJ, Pinheiro LC, Schenck EJ, Chen R, Jabri A, Satlin MJ, Campion TR, Nahid M, Ringel JB, Hoffman KL, Alshak MN, Li HA, Wehmeyer GT, Rajan M, Reshetnyak E, Hupert N, Horn EM, Martinez FJ, Gulick RM, Safford MM.. Clinical characteristics of Covid-19 in New York City. N Engl J Med 2020;382:2372–2374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ibañez C, Perdomo J, Calvo A, Ferrando C, Reverter JC, Tassies D, Blasi A.. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2021;395:1054–1062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wang D, Hu B, Hu C, Zhu F, Liu X, Zhang J, Wang B, Xiang H, Cheng Z, Xiong Y, Zhao Y, Li Y, Wang X, Peng Z.. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020;323:1061–1069. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Wu Z, McGoogan JM.. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020;323:1239–1242. [DOI] [PubMed] [Google Scholar]
- 30.Li B, Yang J, Zhao F, Zhi L, Wang X, Liu L, Bi Z, Zhao Y.. Prevalence and impact of cardiovascular metabolic diseases on COVID-19 in China. Clin Res Cardiol 2020;109:531–538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Hendren NS, Drazner MH, Bozkurt B, Cooper LT.. Description and proposed management of the acute COVID-19 cardiovascular syndrome. Circulation 2020;141:1903–1914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Guzik TJ, Mohiddin SA, Dimarco A, Patel V, Savvatis K, Marelli-Berg FM, Madhur MS, Tomaszewski M, Maffia P, D'Acquisto F, Nicklin SA, Marian AJ, Nosalski R, Murray EC, Guzik B, Berry C, Touyz RM, Kreutz R, Wang DW, Bhella D, Sagliocco O, Crea F, Thomson EC, McInnes IB.. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res 2020;116:1666–1687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Guo T, Fan Y, Chen M, Wu X, Zhang L, He T, Wang H, Wan J, Wang X, Lu Z.. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020;5:811–818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Giustino G, Croft LB, Stefanini GG, Bragato R, Silbiger JJ, Vicenzi M, Danilov T, Kukar N, Shaban N, Kini A, Camaj A, Bienstock SW, Rashed ER, Rahman K, Oates CP, Buckley S, Elbaum LS, Arkonac D, Fiter R, Singh R, Li E, Razuk V, Robinson SE, Miller M, Bier B, Donghi V, Pisaniello M, Mantovani R, Pinto G, Rota I, Baggio S, Chiarito M, Fazzari F, Cusmano I, Curzi M, Ro R, Malick W, Kamran M, Kohli-Seth R, Bassily-Marcus AM, Neibart E, Serrao G, Perk G, Mancini D, Reddy VY, Pinney SP, Dangas G, Blasi F, Sharma SK, Mehran R, Condorelli G, Stone GW, Fuster V, Lerakis S, Goldman ME.. Characterization of myocardial injury in patients with COVID-19. J Am Coll Cardiol 2020;76:2043–2055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Vaduganathan M, Vardeny O, Michel T, McMurray JJV, Pfeffer MA, Solomon SD.. Renin-angiotensin-aldosterone system inhibitors in patients with Covid-19. N Engl J Med 2020;382:1653–1659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Zhang P, Zhu L, Cai J, Lei F, Qin J-J, Xie J, Liu Y-M, Zhao Y-C, Huang X, Lin L, Xia M, Chen M-M, Cheng X, Zhang X, Guo D, Peng Y, Ji Y-X, Chen J, She Z-G, Wang Y, Xu Q, Tan R, Wang H, Lin J, Luo P, Fu S, Cai H, Ye P, Xiao B, Mao W, Liu L, Yan Y, Liu M, Chen M, Zhang X-J, Wang X, Touyz RM, Xia J, Zhang B-H, Huang X, Yuan Y, Loomba R, Liu PP, Li H.. Association of inpatient use of angiotensin-converting enzyme inhibitors and angiotensin II receptor blockers with mortality among patients with hypertension hospitalized with COVID-19. Circ Res 2020;126:1671–1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang Y, Chen B, Li Y, Zhang L, Wang Y, Yang S, Xiao X, Qin Q.. The use of renin-angiotensin-aldosterone system (RAAS) inhibitors is associated with a lower risk of mortality in hypertensive COVID-19 patients: a systematic review and meta-analysis. J Med Virol 2021;93:1370–1377. [DOI] [PubMed] [Google Scholar]
- 38.Bozkurt B, Kovacs R, Harrington B.. Joint HFSA/ACC/AHA statement addresses concerns Re: using RAAS antagonists in COVID-19. J Cardiac Fail 2020;26:370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.De Simone G. Position statement of the ESC council on hypertension on ACE-inhibitors and angiotensin receptor blockers. ESC Councils Council on Hypertension 21 March 2020. This is a statement of prof. Giovanni de Simone Chair of the European Society of Cardiology (ESC) Council on Hypertension.
- 40.Chinese Society of Cardiology. Scientific statement on using renin–angiotensin system blockers in patients with cardiovascular disease and COVID-19. Chin J Cardiol 2020;48:E014. [DOI] [PubMed] [Google Scholar]
- 41.Ghosh AK, Chen DH, Guha A, Mackenzie S, Walker JM, Roddie C.. CAR T Cell therapy–related cardiovascular outcomes and management: systemic disease or direct cardiotoxicity? JACC CardioOncology 2020;2:97–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Amigues I, Pearlman AH, Patel A, Reid P, Robinson PC, Sinha R, Kim AH, Youngstein T, Jayatilleke A, Konig M.. Coronavirus disease 2019: investigational therapies in the prevention and treatment of hyperinflammation. Expert Rev Clin Immunol 2020;16:1185–1204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Wang DY, Salem J-E, Cohen JV, Chandra S, Menzer C, Ye F, Zhao S, Das S, Beckermann KE, Ha L, Rathmell WK, Ancell KK, Balko JM, Bowman C, Davis EJ, Chism DD, Horn L, Long GV, Carlino MS, Lebrun-Vignes B, Eroglu Z, Hassel JC, Menzies AM, Sosman JA, Sullivan RJ, Moslehi JJ, Johnson DB.. Fatal toxic effects associated with immune checkpoint inhibitors: a systematic review and meta-analysis. JAMA Oncol 2018;4:1721–1728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kattan J, Kattan C, Assi T.. Do checkpoint inhibitors compromise the cancer patients' immunity and increase the vulnerability to COVID-19 infection? Immunotherapy 2020;12:351–354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Gambichler T, Reuther J, Scheel CH, Becker JC.. On the use of immune checkpoint inhibitors in patients with viral infections including COVID-19. J Immunother Cancer 2020;8:e001145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Rocco B, Bagni A, Bertellini E, Sighinolfi MC.. Planning of surgical activity in the COVID-19 era: a proposal for a step toward a possible healthcare organization. Urol J 2020;87:175–177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pasin L, Sella N, Correale C, Boscolo A, Rosi P, Saia M, Mantoan D, Navalesi P.. Regional COVID-19 network for coordination of SARS-CoV-2 outbreak in Veneto, Italy. J Cardiothorac Vasc Anesth 2020;34:2341–2345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Perrone AM, Dondi G, Giunchi S, De Crescenzo E, Boussedra S, Tesei M, D'Andrea R, De Leo A, Zamagni C, Morganti AG, De Palma A, De Iaco P.. COVID-19 free oncologic surgical hub: the experience of reallocation of a gynecologic oncology unit during pandemic outbreak. Gynecol Oncol 2021;161:89–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Berghoff AS, Gansterer M, Bathke AC, Trutschnig W, Hungerländer P, Berger JM, Kreminger J, Starzer AM, Strassl R, Schmidt R, Willschke H, Lamm W, Raderer M, Gottlieb AD, Mauser NJ, Preusser M.. SARS-CoV-2 testing in patients with cancer treated at a tertiary care hospital during the COVID-19 pandemic. J Clin Oncol 2020;38:3547–3554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Kampf G, Brüggemann Y, Kaba HEJ, Steinmann J, Pfaender S, Scheithauer S, Steinmann E.. Potential sources, modes of transmission and effectiveness of prevention measures against SARS-CoV-2. J Hosp Infect 2020;106:678–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Zhou J, Otter JA, Price JR, Cimpeanu C, Garcia DM, Kinross J, Boshier PR, Mason S, Bolt F, Holmes AH, Barclay WS.. Investigating SARS-CoV-2 surface and air contamination in an acute healthcare setting during the peak of the COVID-19 pandemic in London. Clin Infect Dis 2020;ciaa905. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Addison D, Campbell CM, Guha A, Ghosh AK, Dent SF, Jneid H.. Cardio-oncology in the era of the COVID-19 pandemic and beyond. J Am Heart Assoc 2020;9:e017787. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Curigliano G, Lenihan D, Fradley M, Ganatra S, Barac A, Blaes A, Herrmann J, Porter C, Lyon AR, Lancellotti P, Patel A, DeCara J, Mitchell J, Harrison E, Moslehi J, Witteles R, Calabro MG, Orecchia R, de Azambuja E, Zamorano JL, Krone R, Iakobishvili Z, Carver J, Armenian S, Ky B, Cardinale D, Cipolla CM, Dent S, Jordan K; ESMO Guidelines Committee. Electronic address: clinicalguidelines@esmo.org. Management of cardiac disease in cancer patients throughout oncological treatment: ESMO consensus recommendations. Ann Oncol 2020;31:171–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Armenian SH, Lacchetti C, Barac A, Carver J, Constine LS, Denduluri N, Dent S, Douglas PS, Durand J-B, Ewer M, Fabian C, Hudson M, Jessup M, Jones LW, Ky B, Mayer EL, Moslehi J, Oeffinger K, Ray K, Ruddy K, Lenihan D.. Prevention and monitoring of cardiac dysfunction in survivors of adult cancers: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol 2017;35:893–911. [DOI] [PubMed] [Google Scholar]
- 55.Lenihan D, Carver J, Porter C, Liu JE, Dent S, Thavendiranathan P, Mitchell JD, Nohria A, Fradley MG, Pusic I, Stockerl-Goldstein K, Blaes A, Lyon AR, Ganatra S, López-Fernández T, O'Quinn R, Minotti G, Szmit S, Cardinale D, Alvarez-Cardona J, Curigliano G, Neilan TG, Herrmann J.. Cardio-oncology care in the era of the coronavirus disease 2019 (COVID-19) pandemic: an International Cardio-Oncolog Society (ICOS) statement CA. Cancer J Clin 2020;70:480–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Tuech J-J, Gangloff A, Di Fiore F, Michel P, Brigand C, Slim K, Pocard M, Schwarz L.. Strategy for the practice of digestive and oncological surgery during the COVID 19 epidemic. J Visc Surg 2020;157:S7–S12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.COVIDSurg Collaborative. Gobal guidance for surgical care during the COVID 19 pandemic. Br J Surg 2020;107:1097–1103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Skulstad H, Cosyns B, Popescu BA, Galderisi M, Salvo GD, Donal E, Petersen S, Gimelli A, Haugaa KH, Muraru D, Almeida AG, Schulz-Menger J, Dweck MR, Pontone G, Sade LE, Gerber B, Maurovich-Horvat P, Bharucha T, Cameli M, Magne J, Westwood M, Maurer G, Edvardsen T.. COVID-19 pandemic and cardiac imaging: EACVI recommendations in precautions, indications, prioritization, and protections for patients and healthcare personnel. Eur Heart J Cardiovasc Imaging 2020;21:592–598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Driggin E, Madhavan MV, Bikdeli B, Chuich T, Laracy J, Biondi-Zoccai G, Brown TS, Der Nigoghossian C, Zidar DA, Haythe J, Brodie D, Beckman JA, Kirtane AJ, Stone GW, Krumholz HM, Parikh SA.. Cardiovascular considerations for patients, healthcare workers, and health systems during the COVID-19 pandemic. J Am Coll Cardiol 2020;75:2352–2371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Hanna TP, King WD, Thibodeau S.. Mortality due to cancer treatment delay: systematic review and meta-analysis. BMJ 2020;371:m4087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hellewell J, Abbott S, Gimma A, Bosse NI, Jarvis CI, Russell TW, Munday JD, Kucharski AJ, Edmunds WJ, Funk S, Eggo RM; Centre for the Mathematical Modelling of Infectious Diseases COVID-19 Working Group. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Global Health 2020;8:e488–e496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.H.R.6074-116th Congress (2019. –2020): Coronavirus Preparedness and Response Supplemental Appropriations Act, 2020 j Congress.gov j Library of Congress. https://www.congress.gov/bill/116th-congress/house-bill/6074 (February 2021).
- 63.Whitten P, Holtz B.. A series of papers for those yearning to propel telehealth to new heights. Telemed J E Health 2008;14:952–956. [DOI] [PubMed] [Google Scholar]
- 64.Gensini GF, Alderighi C, Rasoini R, Mazzanti M, Casolo G.. Value of telemonitoring and telemedicine in heart failure management. Card Fail Rev 2017;3:116–121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Fix OK, Serper M.. Telemedicine and telehepatology during the COVID 19 pandemic. Clin Liver Dis 2020;15:187–190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Smith AC, Thomas E, Snoswell CL, Haydon H, Mehrotra A, Clemensen J, Caffery LJ.. Telehealth for global emergencies. Implications for COVID 19. J Telemed Telecare 2020;26:309–313. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Smith CB, Bhardwaj AS.. Disparities in the use of telehealth during the COVID-19 pandemic. J Clin Oncol 2020;38:87. [Google Scholar]
- 68.Sadler D, DeCara JM, Herrmann J, Arnold A, Ghosh AK, Abdel-Qadir H, Yang EH, Szmit S, Akhter N, Leja M, Silva CMPDC, Raikhelkar J, Brown S-A, Dent S, O'Quinn R, Thuny F, Moudgil R, Raez LE, Okwuosa T, Daniele A, Bauer B, Kondapalli L, Ismail-Khan R, Lax J, Blaes A, Nahleh Z, Elson L, Baldassarre LA, Zaha V, Rao V, Lara DS, Skurka K; Cardio-Oncology International Collaborative Network. Perspectives on the COVID-19 pandemic impact on cardio-oncology: results from the COVID-19 International Collaborative Network survey. Cardio-Oncology 2020;6:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Duceppe E, Parlow J, MacDonald P, Lyons K, McMullen M, Srinathan S, Graham M, Tandon V, Styles K, Bessissow A, Sessler DI, Bryson G, Devereaux PJ.. Canadian Cardiovascular Society Guidelines on perioperative cardiac risk assessment and management for patients who undergo noncardiac surgery. Can J Cardiol 2017;33:17–32. Erratum in: Can J Cardiol 2017;33:1735. [DOI] [PubMed] [Google Scholar]
- 70.Wang B, Huang Y.. Which type of cancer patients are more susceptible to the SARS-CoV-2: Evidence from a meta-analysis and bioinformatics analysis. Crit Rev Oncol Hematol 2020;153:103032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Asokan I, Rabadia SV, Yang EH.. The COVID-19 pandemic and its impact on the cardio-oncology population. Curr Oncol Rep 2020;22:95.Erratum in: Curr Oncol Rep 2020;22:95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Sorouri M, Kasaeian A, Mojtabavi H, Radmard AR, Kolahdoozan S, Anushiravani A, Khosravi B, Pourabbas SM, Eslahi M, Sirusbakht A, Khodabakhshi M, Motamedi F, Azizi F, Ghanbari R, Rajabi Z, Sima AR, Rad S, Abdollahi M.. Clinical characteristics, outcomes, and risk factors for mortality in hospitalized patients with COVID-19 and cancer history: a propensity score-matched study. Infect Agent Cancer 2020;15:74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Onder G, Rezza G, Brusaferro S.. Case-fatality rate and characteristics of patients dying in relation to COVID-19 in Italy. JAMA 2020;323:1775–1776. Erratum in: JAMA 323:1619. [DOI] [PubMed] [Google Scholar]
- 74.Shi S, Qin M, Shen B, Cai Y, Liu T, Yang F, Gong W, Liu X, Liang J, Zhao Q, Huang H, Yang B, Huang C.. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol 2020;5:802–810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Wang B, Huang Y.. Immunotherapy or other anti-cancer treatments and risk of exacerbation and mortality in cancer patients with COVID-19: a systematic review and meta-analysis. Oncoimmunology 2020;9:1824646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Brar G, Pinheiro LC, Shusterman M, Swed B, Reshetnyak E, Soroka O, Chen F, Yamshon S, Vaughn J, Martin P, Paul D, Hidalgo M, Shah MA.. COVID-19 severity and outcomes in patients with cancer: a matched cohort study. J Clin Oncol 2020;38:3914–3392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Richardson S, Hirsch JS, Narasimhan M, Crawford JM, McGinn T, Davidson KW, Barnaby DP, Becker LB, Chelico JD, Cohen SL, Cookingham J, Coppa K, Diefenbach MA, Dominello AJ, Duer-Hefele J, Falzon L, Gitlin J, Hajizadeh N, Harvin TG, Hirschwerk DA, Kim EJ, Kozel ZM, Marrast LM, Mogavero JN, Osorio GA, Qiu M, Zanos TP; the Northwell COVID-19 Research Consortium. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA 2020;323:2052–2059. Erratum in: JAMA 2020;323:2098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Zhang N, Zhang H, Tang Y, Zhang H, Ma A, Xu F, Sun Y, Jiang L, Shan F.. Risk factors for illness severity in patients with COVID-19 pneumonia: a prospective cohort study. Int J Med Sci 2021;18:921–928. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Yang K, Sheng Y, Huang C, Jin Y, Xiong N, Jiang K, Lu H, Liu J, Yang J, Dong Y, Pan D, Shu C, Li J, Wei J, Huang Y, Peng L, Wu M, Zhang R, Wu B, Li Y, Cai L, Li G, Zhang T, Wu G.. Clinical characteristics, outcomes, and risk factors for mortality in patients with cancer and COVID-19 in Hubei, China: a multicentre, retrospective, cohort study. Lancet Oncol 2020;21:904–913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tashiro M, Izumikawa K, Yoshioka D, Nakamura S, Kurihara S, Sakamoto N, Seki M, Kakeya H, Yamamoto Y, Yanagihara K, Mukae H, Hayashi T, Fukushima K, Tashiro T, Kohno S.. Lung fibrosis 10 years after cessation of bleomycin therapy. Tohoku J Exp Med 2008;216:77–80. [DOI] [PubMed] [Google Scholar]
- 81.Li L, Mok H, Jhaveri P, Bonnen MD, Sikora AG, Eissa NT, Komaki RU, Ghebre YT.. Anticancer therapy and lung injury: molecular mechanisms. Expert Rev Anticancer Ther 2018;18:1041–1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Huang T-T, Hudson MM, Stokes DC, Krasin MJ, Spunt SL, Ness KK.. Pulmonary outcomes in survivors of childhood cancer: a systematic review. Chest 2011;140:881–901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Lo AC, Chen B, Samuel V, Savage KJ, Freeman C, Goddard K.. Late effects in survivors treated for lymphoma as adolescents and young adults: a population-based analysis. J Cancer Surviv 2021. doi:10.1007/s11764-020-00976-7. [DOI] [PubMed] [Google Scholar]
- 84.Hanna TP, Evans GA, Booth CM.. Cancer, COVID-19 and the precautionary principle: prioritizing treatment during a global pandemic. Nat Rev Clin Oncol 2020;17:268–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Tsamakis K, Gavriatopoulou M, Schizas D, Stravodimou A, Mougkou A, Tsiptsios D, Sioulas V, Spartalis E, Sioulas AD, Tsamakis C, Charalampakis N, Mueller C, Arya D, Zarogoulidis P, Spandidos DA, Dimopoulos MA, Papageorgiou C, Rizos E.. Oncology during the COVID-19 pandemic: challenges, dilemmas and the psychosocial impact on cancer patients. Oncol Lett 2020;20:441–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Domercant J, Polin N, Jahangir E.. Cardio-oncology: a focused review of anthracycline-, human epidermal growth factor receptor 2 inhibitor-, and radiation-induced cardiotoxicity and management. Ochsner J 2016;16:250–256. [PMC free article] [PubMed] [Google Scholar]
- 87.Mrotzek SM, Rassaf T, Totzeck M.. Cardiovascular damage associated with chest irradiation. Front Cardiovasc Med 2020;7:41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Farmakis D, Keramida K, Filippatos G.. Cardio-oncology services during the COVID-19 pandemic: practical considerations and challenges. Eur J Heart Fail 2020;22:929–932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Hussain A, Via G, Melniker L, Goffi A, Tavazzi G, Neri L, Villen T, Hoppmann R, Mojoli F, Noble V, Zieleskiewicz L, Blanco P, Ma IWY, Wahab MA, Alsaawi A, Al Salamah M, Balik M, Barca D, Bendjelid K, Bouhemad B, Bravo-Figueroa P, Breitkreutz R, Calderon J, Connolly J, Copetti R, Corradi F, Dean AJ, Denault A, Govil D, Graci C, Ha Y-R, Hurtado L, Kameda T, Lanspa M, Laursen CB, Lee F, Liu R, Meineri M, Montorfano M, Nazerian P, Nelson BP, Neskovic AN, Nogue R, Osman A, Pazeli J, Pereira-Junior E, Petrovic T, Pivetta E, Poelaert J, Price S, Prosen G, Rodriguez S, Rola P, Royse C, Chen YT, Wells M, Wong A, Xiaoting W, Zhen W, Arabi Y.. Multi-organ point-of-care ultrasound for COVID-19 (PoCUS4COVID): international expert consensus. Crit Care 2020;24:702–705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Walley PE, Walley KR, Goodgame B, Punjabi V, Sirounis D.. A practical approach to goal-directed echocardiography in the critical care setting. Critical Care 2014;18:681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Neskovic AN, Hagendorff A, Lancellotti P, Guarracino F, Varga A, Cosyns B, Flachskampf FA, Popescu BA, Gargani L, Zamorano JL, Badano LP; European Association of Cardiovascular Imaging. Emergency echocardiography: the European Association of Cardiovascular Imaging recommendations. Eur Heart J Cardiovasc Imaging 2013;14:1–11. [DOI] [PubMed] [Google Scholar]
- 92.Ma IWY, Arishenkoff S, Wiseman J, Desy J, Ailon J, Martin L, Otremba M, Halman S, Willemot P, Blouw M; Canadian Internal Medicine Ultrasound (CIMUS) Group. Internal medicine point-of-care ultrasound curriculum: consensus recommendations from the Canadian Internal Medicine Ultrasound (CIMUS) group. J Gen Intern Med 2017;32:1052–1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Keramida K, Farmakis D, López Fernández T, Lancellotti P.. Focused echocardiography in cardio-oncology. Echocardiography 2020;37:1149–1322. [DOI] [PubMed] [Google Scholar]
- 94.Posteraro A, Severino S, Trambaiolo P, Colonna P.. Manuale di ecocardiografia in emergenza urgenza. Il Pensiero Scientifico Editore, via san Giovanni Valdarno, 8 00138 Rome (Italy); 2017. [Google Scholar]
- 95.Copetti R, Soldati G, Copetti P.. Chest sonography: a useful tool to differentiate acute cardiogenic pulmonary edema from acute respiratory distress syndrome. Cardiovasc Ultrasound 2008;6:16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Gargani L.Lung ultrasound: a new tool for the cardiologist. Cardiovasc Ultrasound 2011;9:6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Chew MS.Haemodynamic monitoring using echocardiography in the critically Ill: a review. Cardiol Res Pract 2012;2012:139537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Plana JC, Galderisi M, Barac A, Ewer MS, Ky B, Scherrer-Crosbie M, Ganame J, Sebag IA, Agler DA, Badano LP, Banchs J, Cardinale D, Carver J, Cerqueira M, DeCara JM, Edvardsen T, Flamm SD, Force T, Griffin BP, Jerusalem G, Liu JE, Magalhães A, Marwick T, Sanchez LY, Sicari R, Villarraga HR, Lancellotti P.. Expert consensus for multimodality imaging evaluation of adult patients during and after cancer therapy: a report from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging 2014;15:1063–1093. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Hull MC, Morris CG, Pepine CJ, Mendenhall NP.. Valvular dysfunction and carotid, subclavian, and coronary artery disease in survivors of hodgkin lymphoma treated with radiation therapy. JAMA 2003;290:2831–2837. [DOI] [PubMed] [Google Scholar]
- 100.Madan R, Benson R, Sharma DN, Julka PK, Rath GK.. Radiation induced heart disease: pathogenesis, management and review literature. J Egypt Natl Canc Inst 2015;27:187–193. [DOI] [PubMed] [Google Scholar]
- 101.Lestuzzi C.Neoplastic pericardial disease: old and current strategies for diagnosis and management. World J Cardiol 2010;2:270–279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Di Liso E, Menichetti A, Dieci MV, Ghiotto C, Banzato A, Bianchi A, Pintacuda G, Padovan M, Nappo F, Cumerlato E, Miglietta F, Mioranza E, Zago G, Corti L, Guarneri V, Conte P.. Neoplastic pericardial effusion: a monocentric retrospective study. J Palliat Med 2019;22:691–695. [DOI] [PubMed] [Google Scholar]
- 103.Hu B, Huang S, Yin L.. The cytokine storm and COVID-19. J Med Virol 2021;93:250–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Fajgenbaum DC, June CH.. Cytokine storm. N Engl J Med 2020;383:2255–2273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.López-Sendón J, Álvarez-Ortega C, Zamora Auñon P, Buño Soto A, Lyon AR, Farmakis D, Cardinale D, Canales Albendea M, Feliu Batlle J, Rodríguez Rodríguez I, Rodríguez Fraga O, Albaladejo A, Mediavilla G, González-Juanatey JR, Martínez Monzonis A, Gómez Prieto P, González-Costello J, Serrano Antolín JM, Cadenas Chamorro R, López Fernández T.. Classification, prevalence, and outcomes of anticancer therapy-induced cardiotoxicity: the CARDIOTOX registry. Eur Heart J 2020;41:1720–1729. [DOI] [PubMed] [Google Scholar]
- 106.Choi AD, Abbara S, Branch KR, Feuchtner GM, Ghoshhajra B, Nieman K, Pontone G, Villines TC, Williams MC, Blankstein R.. Society of Cardiovascular Computed Tomography guidance for use of cardiac computed tomography amidst the COVID-19 pandemic endorsed by the American College of Cardiology. J Cardiovasc Comput Tomogr 2020;14:101–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Society for Cardiovascular Magnetic Resonance. SCMR’s COVID-19 Preparedness Toolkit. 2020. This is a statement of the Society for Cardiovascular Magnetic Resonance.
- 108.American Society of Echocardiography. ASE Statement on COVID-19. 2020. This is a statement of the American Society of Echocardiography.
- 109.European Society of Cardiology. Routine Cardiotoxicity Echo Screening for Chemotherapy Patients during COVID-19. 2020. This is a statement from the Council of Cardio-Oncology of the European Society of Cardiology. www.escardio.org.
- 110.Dal'bo N, Patel R, Parikh R.. Cardiotoxicity of contemporary anticancer immunotherapy. Curr Treat Options Cardiovasc Med 2020;22:62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Calvillo-Argüelles O, Abdel-Qadir H, Ky B, Liu JE, Lopez-Mattei JC, Amir E, Thavendiranathan P.. Modified routine cardiac imaging surveillance of adult cancer patients and survivors during the COVID-19 pandemic. JACC CardioOncol 2020;2:345–349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Nguyen JL, Yang W, Ito K, Matte TD, Shaman J, Kinney PL.. Seasonal influenza infections and cardiovascular disease mortality. JAMA Cardiol 2016;1:274–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Di Pasquale G.Coronavirus COVID-19: quali implicazioni per la Cardiologia? G Ital Cardiol 2020;21:243–245. [DOI] [PubMed] [Google Scholar]
- 114.Bhatraju PK, Ghassemieh BJ, Nichols M, Kim R, Jerome KR, Nalla AK, Greninger AL, Pipavath S, Wurfel MM, Evans L, Kritek PA, West TE, Luks A, Gerbino A, Dale CR, Goldman JD, O'Mahony S, Mikacenic C.. Covid‐19 in critically ill patients in the Seattle region—case series. N Engl J Med 2020;382:2012–2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Thachil J, Tang N, Gando S, Falanga A, Cattaneo M, Levi M, Clark C, Iba T.. ISTH interim guidance on recognition and management of coagulopathy in COVID-19. J Thromb Haemost 2020;18:1023–1026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Stefanini GG, Montorfano M, Trabattoni D, Andreini D, Ferrante G, Ancona M, Metra M, Curello S, Maffeo D, Pero G, Cacucci M, Assanelli E, Bellini B, Russo F, Ielasi A, Tespili M, Danzi GB, Vandoni P, Bollati M, Barbieri L, Oreglia J, Lettieri C, Cremonesi A, Carugo S, Reimers B, Condorelli G, Chieffo A.. ST-elevation myocardial infarction in patients with COVID-19. Circulation 2020;141:2113–2116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Mahmud E, Dauerman HL, Welt FGP, Messenger JC, Rao SV, Grines C, Mattu A, Kirtane AJ, Jauhar R, Meraj P, Rokos IC, Rumsfeld JS, Henry TD.. Management of acute myocardial infarction during the COVID-19 pandemic. A position statement from the Society for Cardiovascular Angiography and Interventions (SCAI), the American College of Cardiology (ACC), and the American College of Emergency Physicians (ACEP). J Am Coll Cardiol 2020;76:1375–1384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Zheng Y-Y, Ma Y-T, Zhang J-Y, Xie X.. COVID-19 and the cardiovascular system. Nat Rev Cardiol 2020;17:259–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Levy BI, Heusch G, Camici PG.. The many faces of myocardial ischaemia and angina. Cardiovasc Res 2019;115:1460–1470. [DOI] [PubMed] [Google Scholar]
- 120.Feher A, Kampaktsis PN, Parameswaran R, Stein EM, Steingart R, Gupta D.. Aspirin is associated with improved survival in severely thrombocytopenic cancer patients with acute myocardial infarction. Oncologist 2017;22:213–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Radmilovic J, Di Vilio A, D'Andrea A, Pastore F, Forni A, Desiderio A, Ragni M, Quaranta G, Cimmino G, Russo V, Scherillo M, Golino P.. The pharmacological approach to oncologic patients with acute coronary syndrome. J Clin Med 2020;9:3926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Neumann F-J, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, Byrne RA, Collet J-P, Falk V, Head SJ, Jüni P, Kastrati A, Koller A, Kristensen SD, Niebauer J, Richter DJ, Seferovic PM, Sibbing D, Stefanini GG, Windecker S, Yadav R, Zembala MO; ESC Scientific Document Group. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J 2019;40:87–165. [DOI] [PubMed] [Google Scholar]
- 123.Egan G, Hughes CA, Ackman ML.. Drug interactions between antiplatelet or novel oral anticoagulant medications and antiretroviral medications. Ann Pharmacother 2014;48:734–740. [DOI] [PubMed] [Google Scholar]
- 124.Cammann VL, Sarcon A, Ding KJ.. Clinical features and outcomes of patients with malignancy and Takotsubo syndrome: observations from the International Takotsubo Registry. J Am Heart Assoc 2019;8:e010881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Jabri A, Kalra A, Kumar A, Alameh A, Adroja S, Bashir H, Nowacki AS, Shah R, Khubber S, Kanaa'N A, Hedrick DP, Sleik KM, Mehta N, Chung MK, Khot UN, Kapadia SR, Puri R, Reed GW.. Incidence of stress cardiomyopathy during the coronavirus disease 2019 pandemic. JAMA Netw Open 2020;3:e2014780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Bybee KA, Kara T, Prasad A, Lerman A, Barsness GW, Wright RS, Rihal CS.. Systematic review: transient left ventricular apical ballooning: a syndrome that mimics ST-segment elevation myocardial infarction. Ann Intern Med 2004;141:858–865. [DOI] [PubMed] [Google Scholar]
- 127.Imazio M, Klingel K, Kindermann I, Brucato A, De Rosa FG, Adler Y, De Ferrari GM.. COVID-19 pandemic and troponin: indirect myocardial injury, myocardial inflammation or myocarditis? Heart 2020;106:1127–1131. [DOI] [PubMed] [Google Scholar]
- 128.Tavazzi G, Pellegrini C, Maurelli M, Belliato M, Sciutti F, Bottazzi A, Sepe PA, Resasco T, Camporotondo R, Bruno R, Baldanti F, Paolucci S, Pelenghi S, Iotti GA, Mojoli F, Arbustini E.. Myocardial localization of coronavirus in COVID-19 cardiogenic shock. Eur J Heart Fail 2020;22:911–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Varga Z, Flammer AJ, Steiger P, Haberecker M, Andermatt R, Zinkernagel AS, Mehra MR, Schuepbach RA, Ruschitzka F, Moch H.. Endothelial cell infection and endotheliitis in COVID-19. Lancet 2020;395:1417–1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Chen C, Zhou Y, Wang DW.. SARS-CoV-2: a potential novel etiology of fulminant myocarditis. Herz 2020;45:230–232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Wu C, Chen X, Cai Y, Xia J, Zhou X, Xu S, Huang H, Zhang L, Zhou X, Du C, Zhang Y, Song J, Wang S, Chao Y, Yang Z, Xu J, Zhou X, Chen D, Xiong W, Xu L, Zhou F, Jiang J, Bai C, Zheng J, Song Y.. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med 2020;180:934–943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Huang X, Sun Y, Su G, Li Y, Shuai X.. Intravenous immunoglobulin therapy for acute myocarditis in children and adults. Int Heart J 2019;60:359–365. [DOI] [PubMed] [Google Scholar]
- 133.Kow CS, Hasan SS.. Glucocorticoid versus immunoglobulin in the treatment of COVID-19-associated fulminant myocarditis. Infection 2020;48:805–806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Siripanthong B, Nazarian S, Muser D, Deo R, Santangeli P, Khanji MY, Cooper LT, Chahal CAA.. Recognizing COVID-19-related myocarditis: the possible pathophysiology and proposed guideline for diagnosis and management. Heart Rhythm 2020;17:1463–1471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Hu H, Ma F, Wei X, Fang Y.. Coronavirus fulminant myocarditis treated with glucocorticoid and human immunoglobulin. Eur Heart J 2021;42:206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Ho JS, Sia C-H, Chan MY, Lin W, Wong RC.. Coronavirus-induced myocarditis: a meta-summary of cases. Heart Lung 2020;49:681–685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Tocchetti CG, Galdiero MR, Varricchi G.. Myocarditis in patients treated with immune checkpoint inhibitors. J Am Coll Cardiol 2018;71:1755–1764. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Hosoba S, Yamamoto M, Shioda K, Sago M, Koyama Y, Shimura T, Kagase A, Tada N, Naganuma T, Araki M, Yamanaka F, Shirai S, Watanabe Y, Hayashida K.. Safety and efficacy of minimalist approach in transfemoral transcatheter aortic valve replacement: insights from the Optimized transCathEter vAlvular interventioN–Transcatheter Aortic Valve Implantation (OCEAN-TAVI) registry. Interact Cardiovasc Thorac Surg 2018;26:420–424. [DOI] [PubMed] [Google Scholar]
- 139.Wood DA, Sathananthan J.. ‘Minimalist’ transcatheter aortic valve implantation during the COVID-19 pandemic: previously optional but now a necessity. EuroIntervention 2020;16:e451–e452. [DOI] [PubMed] [Google Scholar]
- 140.Guha A, Dey AK, Arora S.. Contemporary trends and outcomes of percutaneous and surgical aortic valve replacement in patients with cancer. J.Am Heart Assoc 2020;9:e014248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Shah PB, Welt FGP, Mahmud E, Phillips A, Kleiman NS, Young MN, Sherwood M, Batchelor W, Wang DD, Davidson L, Wyman J, Kadavath S, Szerlip M, Hermiller J, Fullerton D, Anwaruddin S.. Triage considerations for patients referred for structural heart disease intervention during the COVID-19 pandemic: an ACC/SCAI position statement. Catheter Cardiovasc Interv 2020;96:659–663. [DOI] [PubMed] [Google Scholar]
- 142.Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ; HLH Across Speciality Collaboration, UK. COVID-19: consider cytokine storm syndromes and immunosuppression. Lancet 2020;395:1033–1034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Horby P, Lim WS, Emberson JR; RECOVERY Collaborative Group. Dexamethasone in hospitalized patients with Covid-19. N Engl J Med 2021;383:693–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Ahmed MH, Hassan A.. Dexamethasone for the treatment of coronavirus disease (COVID-19): a review. SN Compr Clin Med 2020;31:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Stern A, Skalsky K, Avni T, Carrara E, Leibovici L, Paul M.. Corticosteroids for pneumonia. Cochrane Database Syst Rev 2017;12:CD007720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Lemaitre F, Solas C, Grégoire M, Lagarce L, Elens L, Polard E, Saint-Salvi B, Sommet A, Tod M, Barin-Le Guellec C; French Society of Pharmacology, Therapeutics (SFPT), the International Association of Therapeutic Drug Monitoring, Clinical Toxicology (IATDMCT). Potential drug-drug interactions associated with drugs currently proposed for COVID-19 treatment in patients receiving other treatments. Fundam Clin Pharmacol 2020;34:530–547. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Hodge C, Marra F, Marzolini C, Boyle A, Gibbons S, Siccardi M, Burger D, Back D, Khoo S.. Drug interactions: a review of the unseen danger of experimental COVID-19 therapies. J Antimicrob Chemother 2020;75:3417–3424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Quagliariello V, Bonelli A, Caronna A, Conforti G, Iovine M, Carbone A, Berretta M, Botti G, Maurea N.. SARS-CoV-2 infection and cardioncology: from cardiometabolic risk factors to outcomes in cancer patients. Cancers 2020;12:3316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 149.Steffel J, Verhamme P, Potpara TS, Albaladejo P, Antz M, Desteghe L, Haeusler KG, Oldgren J, Reinecke H, Roldan-Schilling V, Rowell N, Sinnaeve P, Collins R, Camm AJ, Heidbüchel H; ESC Scientific Document Group. The 2018 European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Eur Heart J 2018;39:1330–1393. [DOI] [PubMed] [Google Scholar]
- 150.Melloni C, Dunning A, Granger CB, Thomas L, Khouri MG, Garcia DA, Hylek EM, Hanna M, Wallentin L, Gersh BJ, Douglas PS, Alexander JH, Lopes RD.. Efficacy and safety of apixaban versus warfarin in patients with atrial fibrillation and a history of cancer: insights from the ARISTOTLE trial. Am J Med 2017;130:1440–1448.e1. [DOI] [PubMed] [Google Scholar]
- 151.Fanola CL, Ruff CT, Murphy SA, Jin J, Duggal A, Babilonia NA, Sritara P, Mercuri MF, Kamphuisen PW, Antman EM, Braunwald E, Giugliano RP.. Efficacy and safety of edoxaban in patients with active malignancy and atrial fibrillation: analysis of the ENGAGE AF—TIMI 48 trial. J Am Heart Assoc 2018;7:e008987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Chen ST, Hellkamp AS, Becker RC, Berkowitz SD, Breithardt G, Fox KAA, Hacke W, Halperin JL, Hankey GJ, Mahaffey KW, Nessel CC, Piccini JP, Singer DE, Patel MR, Melloni C.. Efficacy and safety of rivaroxaban vs. warfarin in patients with non-valvular atrial fibrillation and a history of cancer: observations from ROCKET AF. Eur Heart J Qual Care Clin Outcomes 2019;5:145–152. [DOI] [PubMed] [Google Scholar]
- 153.Cavallari I, Verolino G, Romano S, Patti G.. Efficacy and safety of nonvitamin K oral anticoagulants in patients with atrial fibrillation and cancer: a study-level meta-analysis. Thromb Haemost 2020;120:314–321. [DOI] [PubMed] [Google Scholar]
- 154.Deng Y, Tong Y, Deng Y, Zou L, Li S, Chen H.. Non–vitamin K antagonist oral anticoagulants versus warfarin in patients with cancer and atrial fibrillation: a systematic review and meta-analysis. J Am Heart Assoc 2019;8:e012540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 155.Delluc A, Wang T-F, Yap E-S, Ay C, Schaefer J, Carrier M, Noble S.. Anticoagulation of cancer patients with non-valvular atrial fibrillation receiving chemotherapy: guidance from the SSC of the ISTH. J Thromb Haemost 2019;17:1247–1252. [DOI] [PubMed] [Google Scholar]
- 156.Gatti M, Raschi E, Poluzzi E, Martignani C, Salvagni S, Ardizzoni A, Diemberger I.. The complex management of atrial fibrillation and cancer in the COVID-19 era: drug interactions, thromboembolic risk, and proarrhythmia. Curr Heart Fail Rep 2020;17:365–383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Testa S, Prandoni P, Paoletti O, Morandini R, Tala M, Dellanoce C, Giorgi-Pierfranceschi M, Betti M, Danzi GB, Pan A, Palareti G.. Direct oral anticoagulant plasma levels’ striking increase in severe COVID-19 respiratory syndrome patients treated with antiviral agents: the Cremona experience. J Thromb Haemost 2020;18:1320–1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Lombardy Section Italian Society Infectious and Tropical Diseases. Vademecum for the treatment of people with COVID-19. Edition 2.0, 13 March 2020. Infez Med 2020;28:143–152. [PubMed] [Google Scholar]
- 159.Jover R, Bort R, Gómez-Lechón MJ, Castell JV.. Down-regulation of human CYP3A4 by the inflammatory signal interleukin-6: molecular mechanism and transcription factors involved. FASEB J 2002;16:1799–1801. [DOI] [PubMed] [Google Scholar]
- 160.Clarivet B, Robin P, Pers YM, Ferreira R, Lebrun J, Jorgensen C, Hillaire-Buys D, Brés V, Faillie JL.. Tocilizumab and mesenteric arterial thrombosis: drug-drug interaction with anticoagulants metabolized by CYP450 and/or by P-glycoprotein. Eur J Clin Pharmacol 2016;72:1413–1414. [DOI] [PubMed] [Google Scholar]
- 161.Lee EB, Daskalakis N, Xu C, Paccaly A, Miller B, Fleischmann R, Bodrug I, Kivitz A.. Disease-drug interaction of sarilumab and simvastatin in patients with rheumatoid arthritis. Clin Pharmacokinet 2017;56:607–615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 162.Mosarla RC, Vaduganathan M, Qamar A, Moslehi J, Piazza G, Giugliano RP.. Anticoagulation strategies in patients with cancer: JACC review topic of the week. J Am Coll Cardiol 2019;73:1336–1349. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.McBane RD, Torres Roldan VD, Niven AS, Pruthi RK, Franco PM, Linderbaum JA, Casanegra AI, Oyen LJ, Houghton DE, Marshall AL, Ou NN, Siegel JL, Wysokinski WE, Padrnos LJ, Rivera CE, Flo GL, Shamoun FE, Silvers SM, Nayfeh T, Urtecho M, Shah S, Benkhadra R, Saadi SM, Firwana M, Jawaid T, Amin M, Prokop LJ, Murad MH.. Anticoagulation in COVID-19: a systematic review, meta-analysis, and rapid guidance from Mayo Clinic. Mayo Clin Proc 2020;95:2467–2486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Rosovsky R, Li A, Desai A; on behalf of the COVID-19 and Cancer Consortium (CCC19). Venous thrombotic complications in cancer patients with SARS-CoV-2 infection: report from the COVID-19 and Cancer Consortium (CCC19) Registry Analysis [abstract]. Res Pract Thromb Haemost 2020;4. https://abstracts.isth.org/abstract/venous-thrombotic-complications-in-cancer-patients-with-sars-cov-2-infection-report-from-the-covid-19-and-cancer-consortium-ccc19-registry-analysis/ (17 July 2021). [Google Scholar]
- 165.Bakouny Z, Hawley JE, Choueiri TK, Peters S, Rini BI, Warner JL, Painter CA.. COVID-19 and cancer: current challenges and perspectives. Cancer Cell 2020;38:629–646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, Nigoghossian CD, Ageno W, Madjid M, Guo Y, Tang LV, Hu Y, Giri J, Cushman M, Quéré I, Dimakakos EP, Gibson CM, Lippi G, Favaloro EJ, Fareed J, Caprini JA, Tafur AJ, Burton JR, Francese DP, Wang EY, Falanga A, McLintock C, Hunt BJ, Spyropoulos AC, Barnes GD, Eikelboom JW, Weinberg I, Schulman S, Carrier M, Piazza G, Beckman JA, Steg PG, Stone GW, Rosenkranz S, Goldhaber SZ, Parikh SA, Monreal M, Krumholz HM, Konstantinides SV, Weitz JI, Lip GYH; Global COVID-19 Thrombosis Collaborative Group, Endorsed by the ISTH, NATF, ESVM, and the IUA, Supported by the ESC Working Group on Pulmonary Circulation and Right Ventricular Function. COVID-19 and thrombotic or thromboembolic disease: implications for prevention, antithrombotic therapy, and follow-up: JACC state-of-the-art review. J Am Coll Cardiol 2020;75:2950–2973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Schmoldt A, Benthe HF, Haberland G.. Platelets can associate with SARS-CoV-2 RNA and are hyperactivated in COVID-19. Circ Res 1975;24:1404–1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Piazza G, Morrow DA.. Diagnosis, management, and pathophysiology of arterial and venous thrombosis in COVID-19. JAMA 2020;324:2548–2549. [DOI] [PubMed] [Google Scholar]
- 169.Wang T, Chen R, Liu C, Liang W, Guan W, Tang R, Tang C, Zhang N, Zhong N, Li S.. Attention should be paid to venous thromboembolism prophylaxis in the management of COVID-19. Lancet Haematol 2020;7:E362–E363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Jiménez D, García-Sanchez A, Rali P, Muriel A, Bikdeli B, Ruiz-Artacho P, Le Mao R, Rodríguez C, Hunt BJ, Monreal M.. Incidence of VTE and bleeding among hospitalized patients with coronavirus disease 2019: a systematic review and meta-analysis. Chest 2021;159:1182–1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.Zhou H, Hu Y, Li X, Wang L, Wang M, Xiao J, Yi Q.. Assessment of the risk of venous thromboembolism in medical inpatients using the padua prediction score and caprini risk assessment model. J Atheroscler Thromb 2018;25:1091–1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Patell R, Bogue T, Bindal P, Koshy A, Merrill M, Aird WC, Bauer KA, Zwicker JI.. Incidence of thrombosis and hemorrhage in hospitalized cancer patients with COVID-19. J Thromb Haemost 2020;18:2349–2357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Key NS, Khorana AA, Kuderer NM, Bohlke K, Lee AYY, Arcelus JI, Wong SL, Balaban EP, Flowers CR, Francis CW, Gates LE, Kakkar AK, Levine MN, Liebman HA, Tempero MA, Lyman GH, Falanga A.. Venous thromboembolism prophylaxis and treatment in patients with cancer: ASCO clinical practice guideline update. J Clin Oncol 2020;38:496–520. [DOI] [PubMed] [Google Scholar]
- 174.Lyman GH, Carrier M, Ay C, Di Nisio M, Hicks LK, Khorana AA, Leavitt AD, Lee AYY, Macbeth F, Morgan RL, Noble S, Sexton EA, Stenehjem D, Wiercioch W, Kahale LA, Alonso-Coello P.. American Society of Hematology 2021 guidelines for management of venous thromboembolism: prevention and treatment in patients with cancer. Blood Adv 2021;5:927–974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Horowitz NA, Brenner B.. Thrombosis and hemostasis issues in cancer patients with COVID-19. Semin Thromb Hemost 2020;46:785–788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.World Health Organization. Clinical management of severe acute respiratory infection (SARI) when COVID-19 disease is suspected. Interim guidance. https://www.who.int/publications/i/item/clinicalmanagement-of-covid-19 (17 July 2021).
- 177.Spyropoulos AC, Levy JH, Ageno W, Connors JM, Hunt BJ, Iba T, Levi M, Samama CM, Thachil J, Giannis D, Douketis JD; Subcommittee on Perioperative, Critical Care Thrombosis, Haemostasis of the Scientific, Standardization Committee of the International Society on Thrombosis and Haemostasis. Scientific and Standardization Committee communication: clinical guidance on the diagnosis, prevention, and treatment of venous thromboembolism in hospitalized patients with COVID-19. J Thromb Haemost 2020;18:1859–1865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Wang T-F, Milligan PE, Wong CA, Deal EN, Thoelke MS, Gage BF.. Efficacy and safety of high-dose thromboprophylaxis in morbidly obese inpatients. Thromb Haemost 2014;111:88–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Napolitano M, Saccullo G, Marietta M.. Platelet cut-off for anticoagulant therapy in thrombocytopenic patients with blood cancer and venous thromboembolism: an expert consensus. Blood Transfus 2019;17:171–180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Dirix LY, Salgado R, Weytjens R, Colpaert C, Benoy I, Huget P, van Dam P, Prové A, Lemmens J, Vermeulen P.. Plasma fibrin D-dimer levels correlate with tumour volume, progression rate and survival in patients with metastatic breast cancer. Br J Cancer 2002; 86:389–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.COVID-19 Treatment Guidelines Panel. Coronavirus Disease 2019 (COVID-19) Treatment Guidelines. National Institutes of Health. https://www.covid19treatmentguidelines.nih.gov/ (17 July 2021). [PubMed]
- 182.Moores LK, Tritschler T, Brosnahan S, Carrier M, Collen JF, Doerschug K, Holley AB, Jimenez D, Le Gal G, Rali P, Wells P.. Prevention, diagnosis, and treatment of VTE in patients with coronavirus disease 2019: CHEST guideline and expert panel report. Chest 2020;158:1143–1163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Barnes GD, Burnett A, Allen A, Blumenstein M, Clark NP, Cuker A, Dager WE, Deitelzweig SB, Ellsworth S, Garcia D, Kaatz S, Minichiello T.. Thromboembolism and anticoagulant therapy during the COVID-19 pandemic: interim clinical guidance from the anticoagulation forum. J Thromb Thrombolysis 2020;50:72–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Raschi E, Diemberger I, Cosmi B, De Ponti F.. ESC position paper on cardiovascular toxicity of cancer treatments: challenges and expectations-authors’ reply. Intern Emerg Med 2018;13:635–636. [DOI] [PubMed] [Google Scholar]
- 185.Guha A, Dey AK, Jneid H, Ibarz JP, Addison D, Fradley M.. Atrial fibrillation in the era of emerging cancer therapies. Eur Heart J 2019;40:3007–3010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Inciardi RM, Lupi L, Zaccone G, Italia L, Raffo M, Tomasoni D, Cani DS, Cerini M, Farina D, Gavazzi E, Maroldi R, Adamo M, Ammirati E, Sinagra G, Lombardi CM, Metra M.. Cardiac involvement in a patient with coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020;5:819–824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Lindner D, Fitzek A, Bräuninger H, Aleshcheva G, Edler C, Meissner K, Scherschel K, Kirchhof P, Escher F, Schultheiss H-P, Blankenberg S, Püschel K, Westermann D.. Association of cardiac infection with SARS-CoV-2 in confirmed COVID-19 autopsy cases. JAMA Cardiol 2020;5:1281–1285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 188.Pranata R, Huang I, Lukito AA, Raharjo SB.. Elevated N-terminal pro-brain natriuretic peptide is associated with increased mortality in patients with COVID-19: systematic review and meta-analysis. Postgrad Med 2020;96:387–391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 189.Lazzerini PE, Boutjdir M, Capecchi PL.. COVID-19, arrhythmic risk and inflammation: mind the gap! Circulation 2020;142:7–8. [DOI] [PubMed] [Google Scholar]
- 190.Cao J, Tu W-J, Cheng W, Yu L, Liu Y-K, Hu X, Liu Q.. Clinical features and shortterm outcomes of 102 patients with corona virus disease 2019 in Wuhan, China. Clin Infect Dis 2020;71:748–755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 191.Lazzerini PE, Laghi-Pasini F, Boutjdir M, Capecchi PL.. Cardioimmunology of arrhythmias: the role of autoimmune and inflammatory cardiac channelopathies. Nat Rev Immunol 2019;19:63–64. [DOI] [PubMed] [Google Scholar]
- 192.Lazzerini PE, Laghi-Pasini F, Bertolozzi I, Morozzi G, Lorenzini S, Simpatico A, Selvi E, Bacarelli MR, Finizola F, Vanni F, Lazaro D, Aromolaran A, El Sherif N, Boutjdir M, Capecchi PL.. Systemic inflammation as a novel QT-prolonging risk factor in patients with torsades de pointes. Heart 2017;103:1821–1829. [DOI] [PubMed] [Google Scholar]
- 193.Lim MA, Pranata R, Huang I, Yonas E, Soeroto AY, Supriyadi R.. Multiorgan failure with emphasis on acute kidney injury and severity of COVID-19: systematic review and meta-analysis. Can J Kidney Health Dis 2020;7:205435812093857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Lakkireddy DR, Chung MK, Gopinathannair R, Patton KK, Gluckman TJ, Turagam M, Cheung JW, Patel P, Sotomonte J, Lampert R, Han JK, Rajagopalan B, Eckhardt L, Joglar J, Sandau KE, Olshansky B, Wan E, Noseworthy PA, Leal M, Kaufman E, Gutierrez A, Marine JE, Wang PJ, Russo AM.. Guidance for cardiac electrophysiology during the COVID-19 pandemic from the Heart Rhythm Society COVID-19 Task Force; Electrophysiology Section of the American College of Cardiology; and the Electrocardiography and Arrhythmias Committee of the Council on Clinical Cardiology, American Heart Association. Heart Rhythm 2020;17:e233–e241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Pranata R, Huang I, Raharjo SB.. Incidence and impact of cardiac arrhythmias in coronavirus disease 2019 (COVID-19): a systematic review and meta-analysis. Indian Pacing Electrophysiol J 2020;20:193–198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 196.Xiong T-Y, Redwood S, Prendergast B, Chen M.. Coronaviruses and the cardiovascular system: acute and long-term implications. Eur Heart J 2020;41:1798–1800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 197.Kochi AN, Tagliari AP, Forleo GB, Fassini GM, Tondo C.. Cardiac and arrhythmic complications in patients with COVID-19. J Cardiovasc Electrophysiol 2020;31:1003–1008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198.Viganego F, Singh R, Fradley MG.. Arrhythmias and other electrophysiology issues in cancer patients receiving chemotherapy or radiation. Curr Cardiol Rep 2016;18:52. [DOI] [PubMed] [Google Scholar]
- 199.Kapoor A, Pandurangi U, Arora V, Gupta A, Jaswal A, Nabar A, Naik A, Naik N, Namboodiri N, Vora A, Yadav R, Saxena A.. Cardiovascular risks of hydroxychloroquine in treatment and prophylaxis of COVID-19 patients: a scientific statement from the Indian Heart Rhythm Society. Indian Pacing Electrophysiol J 2020;20:117–120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Sapp JL, Alqarawi W, MacIntyre CJ, Tadros R, Steinberg C, Roberts JD, Laksman Z, Healey JS, Krahn AD.. Guidance on minimizing risk of drug-induced ventricular arrhythmia during treatment of COVID-19: a statement from the Canadian Heart Rhythm Society. Can J Cardiol 2020;36:948–951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Roden DM, Harrington RA, Poppas A, Russo AM.. Considerations for drug interactions on QTc in exploratory COVID- 19 (coronavirus disease 2019) treatment. Circulation 2020;141:e906–e907. [DOI] [PubMed] [Google Scholar]
- 202.Tisdale JE, Jaynes HA, Kingery JR, Mourad NA, Trujillo TN, Overholser BR, Kovacs RJ.. Development and validation of a risk score to predict QT interval prolongation in hospitalized patients. Circ Cardiovasc Qual Outcomes 2013;6:479–487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Brown S-A, Patel S, Rayan D, Zaharova S, Lin M, Nafee T, Sunkara B, Maddula R, MacLeod J, Doshi K, Meskin J, Marks D, Saucedo J.. A virtual-hybrid approach to launching a cardio-oncology clinic during a pandemic. Cardio-Oncology 2021;7:2. [DOI] [PMC free article] [PubMed] [Google Scholar]