Abstract
Introduction: E. faecium and E. faecalis are responsible for 13.9% of hospital-acquired infections with frequent resistance to vancomycin (82.6% of E. faecium, 9.5% of E. faecalis). Medical device infections secondary to enterococci often require combination therapy due to impaired activity against biofilm embedded cells. In vitro data demonstrate synergistic activity of daptomycin combinations. Using a novel, biofilm time-kill approach, we evaluated whether daptomycin combinations maintained synergy against biofilm-producing E. faecium and E. faecalis. Methods: Broth microdilution (BMD) and biofilm MIC (bMIC) values for daptomycin, ampicillin, ceftriaxone, fosfomycin, and rifampin were determined against biofilm-producing E. faecium and E. faecalis. Daptomycin combination bMIC values were determined in the presence of biologic concentrations of other antimicrobials. Synergy was evaluated against two E. faecalis (R6981, R7808) and two E. faecium (5938 and 8019) using a previously described biofilm time-kill method. Synergy was defined as ≥2 log10 CFU/cm2 reduction over the most active agent alone. Bactericidal activity was defined as ≥3 log10 CFU/cm2 reduction. Results: Daptomycin bMICs were 2–8-fold higher than BMD. In the presence of other antimicrobials, daptomycin bMICs were reduced ≥ two-fold in dilutions. Ceftriaxone and ampicillin demonstrated the most potent combinations with daptomycin, yielding synergy against three of four strains. Daptomycin plus rifampin was synergistic against E. faecium 5938 and E. faecalis 6981 and produced bactericidal kill. The combination of daptomycin plus fosfomycin displayed synergy solely against E. faecalis 6981. Conclusions: Daptomycin combinations with beta-lactams demonstrated promising synergistic activity against both E. faecium and E. faecalis. While daptomycin plus rifampin yielded bactericidal results, the effect was not seen across all organisms. These combinations warrant further evaluation to determine the optimal dose and response.
Keywords: daptomycin, ceftriaxone, ampicillin, fosfomycin, rifampin, biofilm, medical device, enterococci
1. Introduction
Enterococci have been reported as one of the leading causes of all hospital-acquired infections [1]. The resistance rates in enterococci, especially to vancomycin, are increasing, leaving few alternative therapeutic options. Complicating matters further, both Enterococcus faecium and E. faecalis are capable of producing bacterial biofilm [2]. Biofilm formation encapsulates the organism, leading to an increased adherence to prosthetic material and the prevention of antimicrobial and host immune system penetration [3,4]. Additionally, these cells often display a decreased susceptibility to antimicrobials due to resistance mutations. Due to this, treatment failures are frequently observed with biofilm-associated medical device infections [5].
Combination therapy is typically employed to decrease the probability of antimicrobial failure. Daptomycin is likely one of the better options for combination therapy, as it provides bactericidal coverage against many vancomycin-resistant enterococci (VRE) strains and is capable of penetrating the biofilm matrix due to activity against both replicating and stationary cells [6,7]. Additionally, rifampin has the propensity to penetrate the biofilm matrix, and is utilized clinically in combination for the treatment of Staphylococcus aureus, making it a potentially viable option for a combination therapy for VRE [8,9]. While beta-lactams work only on actively dividing cells, synergistic activity has been observed when combined with daptomycin against biofilm-producing bacterial strains, warranting further evaluation [10,11,12,13]. Similarly, synergy has been observed between daptomycin and fosfomycin [14]. Despite both in vitro and in vivo data to support daptomycin combinations against Gram-positive organisms, it is unknown whether these combinations remain synergistic against biofilm-producing organisms. Therefore, our objective was to evaluate combinations of daptomycin and several antimicrobials, including ampicillin, ceftriaxone, fosfomycin, and rifampin, against VRE strains capable of producing bacterial biofilm.
2. Results
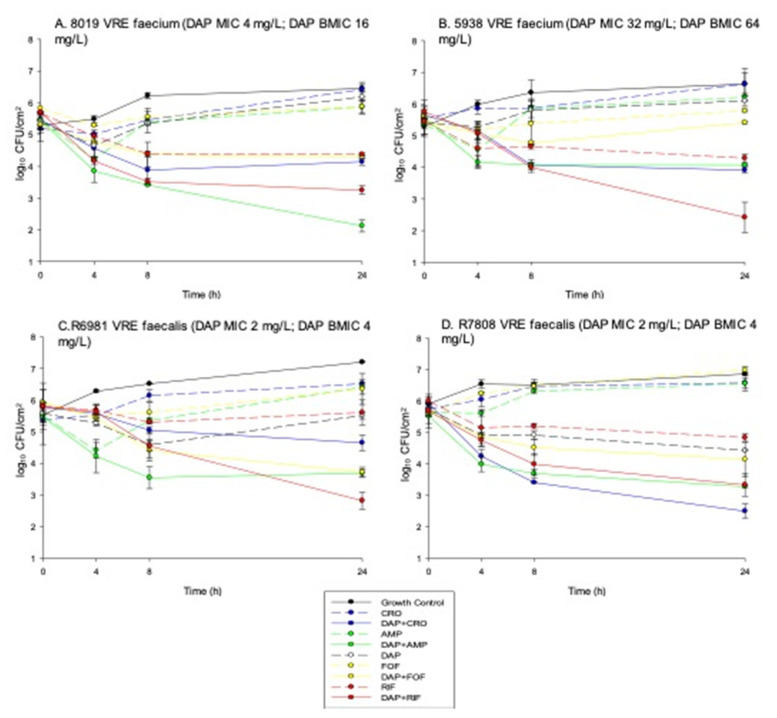
The baseline daptomycin MICs in the 10 enterococcal strains were as follows: three susceptible, six susceptible-dose dependent, and one resistant. Daptomycin biofilm MICs for all strains (excluding R1027) increased by ≥two-fold in dilutions from the standard broth microdilution (BMD) MIC. Seven of the ten strains displayed biofilm MICs greater than the daptomycin MIC breakpoint (>4 mg/L) for enterococci, and two of the remaining strains had bMICs at the breakpoint. In the presence of ampicillin, ceftriaxone, fosfomycin, or rifampin, daptomycin biofilm MICs decreased 16-fold, 4–8-fold, 8–32-fold, and 4–16-fold, respectively, often reducing the daptomycin bMIC to values that would be susceptible in BMD testing (Table 1). In the biofilm time-kill studies, none of the single agents displayed sustained activity, illustrated by regrowth within 24 h (Figure 1). In the daptomycin susceptible parent E. faecium strain (E. faecium 8019), a daptomycin combination with ampicillin, ceftriaxone, or rifampin displayed synergistic activity. Daptomycin plus ampicillin produced the most potent activity with a 3.0 ± 0.6 log10 CFU/cm2 reduction from baseline. Against the daptomycin non-susceptible mutant E. faecium strain (E. faecium 5938), synergistic activity with daptomycin plus either ampicillin or ceftriaxone combinations occurred, but the effect was less pronounced than the killing observed against the daptomycin susceptible parent strain. The combination of daptomycin plus rifampin produced bactericidal activity (3.4 ± 0.7 log10 CFU/cm2 reduction from baseline) against this strain, despite the other combinations demonstrating minimal activity. Daptomycin plus fosfomycin did not produce synergistic effects against either E. faecium strain. Against the E. faecalis strains, daptomycin combinations also produced synergistic effects. Against E. faecalis 6981, daptomycin plus rifampin, ampicillin, or fosfomycin resulted in synergy, with the rifampin combination producing bactericidal activity with a 3.0 ± 0.2 log10 CFU/cm2 reduction from baseline. Against E. faecalis 7808, the only combination that produced synergy was daptomycin plus ceftriaxone with a 3.4 ± 0.4 log10 CFU/cm2 reduction observed from baseline. While the other combinations did not produce a synergistic effect, 2.2 ± 0.3, 2.4 ± 0.5, and 2.3 ± 0.5 log10 CFU/cm2 reductions were observed for daptomycin combined with ampicillin, fosfomycin, and rifampin, respectively.
Table 1.
Standard and Biofilm Minimum Inhibitory Concentrations (mg/L).
| MIC (mg/L) | |||||||||
| Strain | DAP | AMP | CRO | FOF | RIF | DAP + AMP | DAP + CRO | DAP + FOF | DAP + RIF |
| E. faecalis | |||||||||
| R6981 | 2 | 512 | >1024 | 64 | 0.0156 | 0.125 | 0.125 | 0.5 | 0.5 |
| R7808 | 2 | >64 | >1024 | 64 | <0.0078 | 0.25 | 1 | 0.5 | 0.25 |
| R6797 | 1 | 2 | >64 | 64 | 2 | 0.25 | 1 | 0.0625 | 0.5 |
| R6798 | 1 | 1 | >64 | 64 | 2 | 0.25 | 0.5 | <0.016 | 1 |
| R6799 | 2 | 2 | >64 | 64 | 2 | 0.25 | 1 | 0.0625 | 0.5 |
| E. faecium | |||||||||
| 8019 | 4 | 4 | 32 | 64 | 0.5 | 0.125 | 0.0625 | 1 | 0.5 |
| 5938 | 32 | 16 | 64 | 64 | 0.0625 | 0.0625 | <0.031 | 8 | 8 |
| R1026 | 1 | 32 | >64 | >64 | <0.0156 | 0.5 | 1 | 0.125 | 0.25 |
| R1027 | 2 | 32 | >64 | 64 | 4 | 1 | 1 | 0.25 | 0.25 |
| R1028 | 4 | 32 | >64 | >64 | 32 | 1 | 1 | 0.5 | 0.015 |
| Biofilm MIC (mg/L) | |||||||||
| Strain | DAP | AMP | CRO | FOF | RIF | DAP + AMP | DAP + CRO | DAP + FOF | DAP + RIF |
| E. faecalis | |||||||||
| R6981 | 4 | >64 | >64 | >64 | 0.03125 | 0.25 | 0.5 | 0.25 | 0.25 |
| R7808 | 4 | >64 | >64 | >64 | 0.0156 | 0.25 | 1 | 0.5 | 0.5 |
| R6797 | 8 | >64 | >64 | >64 | 2 | 1 | 4 | 1 | 8 |
| R6798 | 8 | >64 | >64 | >64 | 2 | 2 | 4 | 2 | 8 |
| R6799 | 8 | >64 | >64 | >64 | 1 | 2 | 4 | 1 | 8 |
| E. faecium | |||||||||
| 8019 | 16 | >64 | >64 | >64 | 1 | 1 | 2 | 0.5 | 2 |
| 5938 | 64 | >64 | >64 | >64 | 0.25 | 4 | 8 | 8 | 16 |
| R1026 | 8 | 64 | >64 | 32 | 0.0156 | 1 | 1 | 1 | 0.25 |
| R1027 | 2 | 64 | >64 | 32 | <0.031 | 1 | 1 | 1 | 0.25 |
| R1028 | 8 | >64 | >64 | >64 | >64 | 1 | 1 | 1 | 0.5 |
DAP: daptomycin; AMP: ampicillin; CRO: ceftriaxone; FOF: fosfomycin; RIF: rifampin.
Figure 1.
In vitro time kill curves: (A) E. faecium 8019, (B) E. faecium 5938, (C) E. faecalis 6981, (D) E. faecalis 7808 illustrating mean +/− standard deviation of CFU/cm2.
3. Discussion
Biofilm production represents a major healthcare concern. A decreased drug and host immune system exposure, a stationary growth phase, and reductions in susceptibility contribute to the poor outcomes often observed in biofilm-associated medical device infections [5]. Enterococci are a leading cause of healthcare-associated infections with vancomycin-resistance rates increasing [1]. These VRE isolates are now recognized as one of the more challenging multidrug-resistant pathogens. Their propensity for biofilm production limits therapeutic options, warranting the exploration of combination therapies that have demonstrated resistance prevention and bactericidal activity against planktonic enterococci in previous models.
The biofilm MICs for both species of enterococci evaluated in this study displayed a 2–4-fold increase in dilutions from the standard broth microdilution MIC pending strain and antimicrobial. This increase in concentration needed to inhibit bacterial growth is consistent with the previous literature evaluating biofilm-producing organisms [10]. Additionally, we observed bactericidal activity with daptomycin plus either ampicillin, ceftriaxone, or rifampin. Unfortunately, a lack of synergy with daptomycin plus fosfomycin against three of the four biofilm-producing strains occurred.
The activity we observed is supported by case reports of treatment success with these combinations in the clinical realm [15,16,17,18]. While the majority of data on daptomycin combinations are in staphylococci, additive, or synergistic activity has been observed with combination therapy against enterococci. Additionally, these combinations have also been studied in biofilm-producing staphylococci with success [10,19]. However, this is one of the first assessments of combination therapy against biofilm-producing enterococci.
One difference in this study compared to the previous literature is the lack of synergy observed with daptomycin plus fosfomycin. Animal data exist demonstrating the potential of this combination against enterococci [20]. As there was an inhibition of growth, a possible explanation for the lack of success with fosfomycin combinations in this study may be due to the strain selection. Additionally, it is possible that the level of biofilm produced may have made this combination less effective.
Our results demonstrate that daptomycin combination regimens, specifically combined with ampicillin, ceftriaxone, fosfomycin, or rifampin, were capable of decreasing the bacterial colony counts in several biofilm-producing enterococcal strains. While these results are promising, further research with more extensive modeling is warranted.
4. Materials and Methods
4.1. Bacterial Strains
A total of 10 clinical strains (5 E. faecium and 5 E. faecalis) with varying susceptibilities to daptomycin, including an isogenic (related) strain pair of E. faecium, including one daptomycin susceptible (E. faecium 8019) and one daptomycin non-susceptible (E. faecium 5938) strain, were evaluated.
4.2. Antimicrobials
The following antibiotics were evaluated: ampicillin, ceftriaxone, daptomycin, fosfomycin, rifampin, and vancomycin. Daptomycin (Cubist Pharmaceuticals, Lexington, MA), ampicillin, ceftriaxone, fosfomycin, rifampin, and vancomycin (Sigma Chemical Company, St. Louis, MO, USA) were purchased commercially.
4.3. Media
Due to the necessity of calcium for daptomycin’s antimicrobial activity, Mueller–Hinton broth II (Difco, Detroit, MI, USA) supplemented with 50 mg/L of calcium chloride and 12.5 mg/L of magnesium chloride (SMHB) was used for susceptibility testing as well as time-kill experiments. Colony counts were determined using brain heart infusion (BHI) agar plates (Difco).
4.4. Susceptibility Testing
Minimum inhibitory concentrations (MIC) were determined by broth microdilution per Clinical Laboratory Standards Institute (CLSI) guidelines, and biofilm MICs (bMIC) determinations were performed per the Calgary method on all VRE strains [21,22]. Daptomycin combination MICs and combination bMICs were performed in the presence of ampicillin, ceftriaxone, fosfomycin, and rifampin at 0.5 × MIC or maximum concentrations of free drug achieved in human serum utilizing standard dosing regimens [10]. All strains evaluated were proven to produce biofilm via quantification techniques utilizing well-described biofilm-forming (NRSA101 and ATCC 35556) and non-biofilm-forming (ATCC12228) strains, as previously described [23,24].
4.5. Biofilm Time-Kill Evaluations
A previously described methodology utilizing microwell plates to evaluate synergy against biofilm-producing organisms was utilized [10]. In brief, 3-mm polyurethane beads were placed in 1% glucose-supplemented tryptic soy broth (GSTSB), inoculated with the test organism, and incubated at 37 °C, allowing for biofilm formation. After 24 h of incubation, GSTSB was aspirated, and the beads were carefully removed via forceps and placed into wells containing Mueller–Hinton broth supplemented with 50 mg/L of calcium due to the calcium-dependent mechanism of daptomycin. Antimicrobials were added at 1× the biofilm MIC for all agents unless the biofilm MIC was greater than the free physiologic peak concentration, in which case, free physiologic peaks were used. Free peak synergistic concentrations, utilizing simulated normal human dosage regimens, were 70 mg/L for ampicillin (2 g), 25.7 mg/L for ceftriaxone (2 g), 14.7 mg/L for daptomycin (12 mg/kg), 200 mg/L for fosfomycin (4 g), and 2.1 mg/L for rifampin (300 mg). Targeted bacterial starting inoculum for all strains was 5.5–6 log10 CFU/cm2, based upon the surface area of the beads. Beads were removed with sterile forceps at 0, 4, 8, and 24 h, washed to remove adhering non-biofilm organisms, and placed into 1 mL of normal saline. Biofilm was recovered by three alternating 60-s cycles of vortexing and sonication at 20Hz Bransonic 12 Branson Ultrasonic Corporation. Recovered biofilm cells were plated on BHI agar (EasySpiral; Interscience, Worborn, MA) and incubated for 24 h at 37 °C. Synergy was defined as a ≥2 − log10 CFU/cm2 reduction over the most active agent alone. Combinations that resulted in ≥1 − log10 bacterial growth in comparison to the least active single agent were considered antagonistic. Single drug exposures in biofilm time-kill experiments included ampicillin, ceftriaxone, daptomycin, fosfomycin, and rifampin. Additionally, combination evaluations were performed with daptomycin plus each of the previously mentioned non-daptomycin antimicrobials.
5. Conclusions
Daptomycin combinations appear effective against biofilm-producing enterococci. These combinations warrant further evaluation to determine the optimal dose and response.
Author Contributions
Conceptualization, K.E.B., J.R.S. and M.J.R.; methodology, K.E.B., J.R.S. and M.J.R.; software, K.E.B.; validation, K.E.B., J.R.S. and M.J.R.; formal analysis, K.E.B.; investigation, K.E.B., Z.S., J.R.S., R.K., and T.M.; resources, M.J.R.; data curation, K.E.B.; writing—original draft preparation, K.E.B., J.R.S. and M.J.R.; writing—review and editing, Z.S., R.K., and T.M.; visualization, K.E.B.; supervision, M.J.R.; project administration, M.J.R.. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by internal funding. The authors have not received any financial reimbursement from any pharmaceutical companies for any of the work presented in this article. The authors do not own any stocks or shares relevant to this study, nor has any funding agency been involved in the study design. No professional medical writers have been involved in this manuscript preparation, and no reimbursement has been received for preparation of this article.
Institutional Review Board Statement
Not applicable for studies not involving humans or animals.
Informed Consent Statement
Not applicable for studies not involving humans.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
K.E.B., J.R.S., R.K., and Z.S. have nothing to declare. M.J.R. has received research support, consulted or spoke on behalf of Allergan, Melinta, Merck, Nabriva, Paratek, Shionogi, Spero, and Tetraphase.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Weiner-Lastinger L.M., Abner S., Edwards J.R., Kallen A.J., Karklsson M., Magill S.S., Pollock D., See I., Soe M.M., Walters M.S., et al. Antimicrobial-resistant pathogens associated with adult healthcare-associated infections: Summary of data reported to the National Healthcare Safety Network, 2015–2017. Infect. Control. Hosp. Epidemiol. 2020;41:1–18. doi: 10.1017/ice.2019.296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Srinivasan A., Wise M., Bell M., Cardo D., Edwards J., Fridkin S., Jernigan J., Kallen A., McDonald L.C., Patel P.R., et al. Vital Signs: Central Line-Associated Blood Stream Infections—United States, 2001, 2008, and 2009. Centers for Disease Control and Prevention; Atlanta, GA, USA: 2011. pp. 243–248. MMWR Morbidity and Mortality Weekly Report 8. [PubMed] [Google Scholar]
- 3.Parra-Ruiz J., Vidaillac C., Rose W.E., Rybak M.J. Activities of high-dose daptomycin, vancomycin, and moxifloxacin alone or in combination with clarithromycin or rifampin in a novel in vitro model of Staphylococcus aureus biofilm. Antimicrob. Agents Chemother. 2010;10:4329–4334. doi: 10.1128/AAC.00455-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goeres D.M., Loetterle L.R., Hamilton M.A., Murga R., Kirby D.W., Donlan R.M. Statistical assessment of a laboratory method for growing biofilms. Microbiology. 2005;3:757–762. doi: 10.1099/mic.0.27709-0. [DOI] [PubMed] [Google Scholar]
- 5.Osmon D.R., Berbari E.F., Berendt A.R., Lew D., Zimmerli W., Steckelberg J.M., Rao N., Hanssen A., Wilson W.R. Diagnosis and management of prosthetic joint infection: Clinical practice guidelines by the Infectious Diseases Society of America. Clin. Infect. Dis. 2013;56:e1–e25. doi: 10.1093/cid/cis803. [DOI] [PubMed] [Google Scholar]
- 6.Stewart P.S., Davison W.M., Steenbergen J.N. Daptomycin rapidly penetrates a Staphylococcus epidermidis biofilm. Antimicrob. Agents Chemother. 2009;53:3505–3507. doi: 10.1128/AAC.01728-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sader H.S., Moet G.J., Farrell D.J., Jones R.N. Antimicrobial susceptibility of daptomycin and comparator agents tested against methicillin-resistant Staphylococcus aureus and vancomycin-resistant enterococci: Trend analysis of a 6-year period in US medical centers (2005–2010) Diagn. Microbiol. Infect. Dis. 2011;70:412–416. doi: 10.1016/j.diagmicrobio.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 8.Zheng Z., Stewart P.S. Penetration of rifampin through Staphylococcus epidermidis biofilms. Antimicrob. Agents Chemother. 2002;46:900–903. doi: 10.1128/AAC.46.3.900-903.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Dunne W.M., Jr., Mason E.O., Jr., Kaplan S.L. Diffusion of rifampin and vancomycin through a Staphylococcus epidermidis biofilm. Antimicrob. Agents Chemother. 1993;37:2522–2526. doi: 10.1128/AAC.37.12.2522. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barber K.E., Werth B.J., McRoberts J.P., Rybak M.J. A novel approach utilizing biofilm time-kill curves to assess the bactericidal activity of ceftaroline combinations against biofilm-producing methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 2014;58:2989–2992. doi: 10.1128/AAC.02764-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Barber K.E., King S.T., Stover K.R., Pogue J.M. Therapeutic options for vancomycin-resistant enterococcal bacteremia. Expert Rev. Anti. Infect. Ther. 2015;3:363–377. doi: 10.1586/14787210.2015.1001839. [DOI] [PubMed] [Google Scholar]
- 12.Barber K.E., Werth B.J., Rybak M.J. The combination of ceftaroline plus daptomycin allows for therapeutic de-escalation and daptomycin sparing against MRSA. J. Antimicrob. Chemother. 2015;70:505–509. doi: 10.1093/jac/dku378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Berti A.D., Sakoulas G., Nizet V., Tewhey R., Rose W.E. Beta-Lactam antibiotics targeting PBP1 selectively enhance daptomycin activity against methicillin-resistant Staphylococcus aureus. Antimicrob. Agents Chemother. 2013;57:5005–5012. doi: 10.1128/AAC.00594-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hall Snyder A.D., Werth B.J., Nonejuie P., McRoberts J.P., Pogliano J., Sakoulas G., Yim J., Singh N., Rybak M.J. Fosfomycin Enhances the Activity of Daptomycin against Vancomycin-Resistant Enterococci in an In Vitro Pharmacokinetic-Pharmacodynamic Model. Antimicrob. Agents Chemother. 2016;60:5716–5723. doi: 10.1128/AAC.00687-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Sakoulas G., Bayer A.S., Pogliano J., Tsuji B.T., Yang S.J., Mishra N.N., Nizet V., Yeaman M.R., Moise P.A. Ampicillin enhances daptomycin- and cationic host defense peptide-mediated killing of ampicillin- and vancomycin-resistant Enterococcus faecium. Antimicrob. Agents Chemother. 2012;56:838–844. doi: 10.1128/AAC.05551-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sierra-Hoffman M., Iznaola O., Goodwin M., Mohr J. Combination therapy with ampicillin and daptomycin for treatment of Enterococcus faecalis endocarditis. Antimicrob. Agents Chemother. 2012;56:6064. doi: 10.1128/AAC.01760-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Smith J.R., Barber K.E., Raut A., Rybak M.J. β-Lactams enhance daptomycin activity against vancomycin-resistant Enterococcus faecalis and Enterococcus faecium in In Vitro pharmacokinetic/pharmacodynamic models. Antimicrob. Agents Chemother. 2015;59:2842–2848. doi: 10.1128/AAC.00053-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith J.R., Barber K.E., Raut A., Aboutaleb M., Sakoulas G., Rybak M.J. β-Lactam combinations with daptomycin provide synergy against vancomycin-resistant Enterococcus faecalis and Enterococcus faecium. J. Antimicrob. Chemother. 2015;70:1738–1743. doi: 10.1093/jac/dkv007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Barber K.E., Smith J.R., Ireland C.E., Boles B.R., Rose W.E., Rybak M.J. Evaluation of Ceftaroline Alone and in Combination against Biofilm-Producing Methicillin-Resistant Staphylococcus aureus with Reduced Susceptibility to Daptomycin and Vancomycin in an In Vitro Pharmacokinetic/Pharmacodynamic Model. Antimicrob. Agents Chemother. 2015;59:4497–4503. doi: 10.1128/AAC.00386-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rice L.B., Eliopoulos C.T., Yao J.D., Eliopoulos G.M., Moellering R.C., Jr. In vivo activity of the combination of daptomycin and fosfomycin compared with daptomycin alone against a strain of Enterococcus faecalis with high-level gentamicin resistance in the rat endocarditis model. Diagn. Microbiol. Infect. Dis. 1992;15:173–176. doi: 10.1016/0732-8893(92)90045-U. [DOI] [PubMed] [Google Scholar]
- 21.Ceri H., Olson M., Morck D., Storey D., Read R., Buret A., Olson B. The MBEC Assay System: Multiple equivalent biofilms for antibiotic and biocide susceptibility testing. Methods Enzymol. 2001;337:377–385. doi: 10.1016/s0076-6879(01)37026-x. [DOI] [PubMed] [Google Scholar]
- 22.Ceri H., Olson M.E., Stremick C., Read R.R., Morck D., Buret A. The Calgary Biofilm Device: New technology for rapid determination of antibiotic susceptibilities of bacterial biofilms. J. Clin. Microbiol. 1999;37:1771–1776. doi: 10.1128/JCM.37.6.1771-1776.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Stepanovic S., Vukovic D., Dakic I., Savic B., Svabic-Vlahovic M. A modified microtiter-plate test for quantification of staphylococcal biofilm formation. J. Microbiol. Methods. 2000;40:175–179. doi: 10.1016/S0167-7012(00)00122-6. [DOI] [PubMed] [Google Scholar]
- 24.Christensen G.D., Simpson W.A., Younger J.J., Baddour L.M., Barrett F.F., Melton D.M., Beachey E.H. Adherence of coagulase-negative staphylococci to plastic tissue culture plates: A quantitative model for the adherence of staphylococci to medical devices. J. Clin. Microbiol. 1985;22:996–1006. doi: 10.1128/jcm.22.6.996-1006.1985. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.