Abstract
Senescent osteoblast overburden accelerates bone mass loss. Little is understood about microRNA control of oxidative stress and osteoblast senescence in osteoporosis. We revealed an association between microRNA-29a (miR-29a) loss, oxidative stress marker 8-hydroxydeoxyguanosine (8-OHdG), DNA hypermethylation marker 5-methylcystosine (5mC), and osteoblast senescence in human osteoporosis. miR-29a knockout mice showed low bone mass, sparse trabecular microstructure, and osteoblast senescence. miR-29a deletion exacerbated bone loss in old mice. Old miR-29a transgenic mice showed fewer osteoporosis signs, less 5mC, and less 8-OHdG formation than age-matched wild-type mice. miR-29a overexpression reversed age-induced senescence and osteogenesis loss in bone-marrow stromal cells. miR-29a promoted transcriptomic landscapes of redox reaction and forkhead box O (FoxO) pathways, preserving oxidation resistance protein-1 (Oxr1) and FoxO3 in old mice. In vitro, miR-29a interrupted DNA methyltransferase 3b (Dnmt3b)-mediated FoxO3 promoter methylation and senescence-associated β-galactosidase activity in aged osteoblasts. Dnmt3b inhibitor 5′-azacytosine, antioxidant N-acetylcysteine, or Oxr1 recombinant protein attenuated loss in miR-29a and FoxO3 to mitigate oxidative stress, senescence, and mineralization matrix underproduction. Taken together, miR-29a promotes Oxr1, compromising oxidative stress and FoxO3 loss to delay osteoblast aging and bone loss. This study sheds light on a new antioxidation mechanism by which miR-29a protects against osteoblast aging and highlights the remedial effects of miR-29a on osteoporosis.
Keywords: microRNA-29a, senescence, osteoporosis, Oxr1, FoxO3, Dnmt3b
1. Introduction
Osteoporosis is a chronic skeletal disease with low bone mass and fragile microstructure [1], becoming a prominent risk factor of bone fracture-associated disability or premature death [2]. Osteoblast dysfunction, marrow adipocyte overgrowth, and osteoclast overactivation are notable features of osteoporotic bone [3]. Expanding evidence reveals that oxidative stress [4], mitochondrial dysfunction [5], and mesenchymal stem cell exhaustion [6] dysregulate bone microstructure integrity. In addition, an increased osteoblast senescence program, including upregulated p16Ink4a, p21Cip1 signaling, β-galactosidase activity, DNA damage, and senescence-associated secreted phenotypes [7]. inhibits bone formation activity during osteoporosis development [8].
Epigenetic alternation is one of the hallmarks of cellular aging, whereas a chronic dysregulation of the epigenetic program accelerates the development of age-related diseases [9]. Of epigenetic changes, methyl modification of cytosine in DNA into 5-methylcytosine (5mC), catalyzed by DNA methyltransferases (DNMT), represses promoter activity, inducing transcription repression to control tissue development and degeneration [10]. Increased 5mC formation is present in human age-related tissue dysfunction or tumorigenesis [11,12]. In skeletal tissue, DNA methylation and dysregulated DNMT influence osteogenesis and bone homeostasis. High DNA methylation signatures correlate with low bone mineral density [13] and postmenopausal osteoporosis [14]. DNMT3a mediates hypoxia mimetic-induced osteoblast dysfunction [15]. The DNMT3b-mediated DNA methylome impedes osteoblastogenesis of human mesenchymal progenitor cells from bone marrow [16]. Furthermore, oxidative stress induces DNMT3b-mediated KLF5 hypermethylation, inhibiting osteogenic differentiation [17].
MicroRNAs (miR) bind to the 3′-untranslated region of mRNA targets, which interrupt protein translation and modulate plenty of biological activities [18]. These molecules affect bone-forming cell behavior or bone tissue integrity in aged skeleton. For example, miR-219-5p targets retinoic acid receptor-related orphan receptor beta, ameliorating osteogenesis loss [19]. The gain of miR-195 function increases angiogenesis, progressively improving bone mass in aged mice [20]. miR-31-5p knockdown slows osteoclastic resorption and age-mediated bone loss [21]. MicroRNAs also interplay with epigenetic pathways, regulating the osteogenic lineage specification [22] and angiogenic activity [23] of mesenchymal stem cells. Little is known about microRNA signaling control oxidative stress, which inhibits osteoblast senescence and bone mass loss.
This study aimed to investigate whether miR-29a correlated with oxidative stress and osteoblast aging in human osteoporosis and examined if miR-29a knockout or overexpression affected osteoblast senescence and bone loss in old mice and characterized the epigenetic mechanism by which miR-29a controlled oxidative stress and senescence program in osteoblasts of osteoporotic skeleton.
2. Materials and Methods
2.1. Clinical Specimens
Studies on human bone biopsies were approved by the Chang Gung Medical Foundation Institutional Review Board (Affidavit #202000823B0). Informed consent was obtained from patients preoperatively. Thirteen patients with osteoporosis (5 males and 8 females) and 13 patients without osteoporosis (6 males and 7 females) who required lumbar spine decompression, fixation, discectomy, or vertebroplasty were enrolled in the osteoporosis group and control group, respectively. The BMD of the hip was quantified using dual-energy X-ray absorptiometry before surgery. Leftover bone biopsies and 10 mL peripheral blood were harvested.
2.2. miR-29a Knockout Mice
Animal experiments were approved by Institutional Animal Use and Care Committee, Kaohsiung Chang Gung Memorial Hospital (Affidavit #2014120401). The homologous arms of C57BL/B6 mouse miR-29a gene (Chromosome 6, 31029595-31049694) (RP23-173G8) of Bacterial Artificial Chromosome (BAC) library (BACPAC Genomics Resource Center; Emeryville, CA, USA) were cloned using PCR protocols. The loxP site and the neomycin (Neo) resistance cassette (PL452) were inserted into PL253 plasmid (Addgene, Watertown, MA, USA). The Neo gene driven by T7 promoter in mammalian cells was removed by Cre recombinase. The linearized BAC construct was transferred into embryonic stem cells of C57BL/6 mice to produce miR-29a chimera, which further crossed with Sox2-Cre mice (Jackson Laboratory, Bar Harbor, ME, USA) to breed miR-29aKO mice. The genotype of miR-29aKO mice was confirmed using customized primers (Supplementary Table S1) and PCR protocols. Mice were raised in a specific pathogen-free laboratory animal facility with feed and drinking water ad libitum.
2.3. Bone-Specific miR-29a Transgenic Mice
Osteoblast-specific miR-29a transgenic mice (C57L/B6; miR-29aTg), which carried osteocalcin (Bgp) promoter-driven human miR-29a precursor construct, were generated. In brief, linear constructs with osteocalcin (Bgp) promoter–human miR-29a precursor (506 bp) –bovine growth hormone (BGH) polyadenylation (polyA) were transfected into fertilized eggs from C57L/B6 mice through microinjection protocols. The micro-injected eggs were grafted into foster mother mice, as previously described [24]. Genotypes of littermates were characterized using PCR protocols and primers. Mice carrying the 506-bp gene coded human miR-29a precursor were considered miR-29aTg mice, whereas mice that did not carry the gene of interest were considered wild-type (WT) mice [24].
2.4. Age-Mediated Osteoporosis
Three-month-old and 9-month-old male miR-29aTg or WT mice were divided into young and old groups, respectively. To label bone mineralization, 10 mg/kg calcein was injected 9 days and 3 days before euthanasia. Peripheral blood was drawn and centrifuged to harvest serum. Femurs and tibiae specimens were dissected for subsequent experiments.
2.5. μCT Analysis of Bone Tissue and Marrow Adipose
The microstructure of femurs and tibiae was visualized using SkyScan 1176 μCT (Bruker, Belgium) and captured 200 radiographs (9-μm voxel size), as previously described [24]. BMD (g/cm3), trabecular volume (BV/TV, %), trabecular thickness (Tb.Th, mm), and trabecular number (Tb.N/mm) of proximal tibiae, were measured using SKYSCAN® CT-Analysis software, according to the maker’s instructions. In a subset experiment, μCT radiography of marrow fat in tibiae was performed upon soaking in OsO4, as previously described [25]. The images of OsO4-soaked specimens were reconstructed and merged using the software. Marrow fat volume (mm3) and fat surface (mm2) were calculated automatically.
2.6. Biomechanical Test
Upon measuring the cross-section area of the middle region of femurs using μCT scanning protocols, the biomechanical properties, including breaking force (N/mm2) and energy (N.mm), of the middle region of femurs upon 3-point bending were quantified using SHIMADZU EZ-SX Material Test System (Shimadzu Corporation, Kyoto, Japan) with TRAPEZIVMX software, according to the maker’s instructions.
2.7. Histomorphometry and Immunohistochemistry
The calcein labeling in methyl acrylate (Polysciences Inc., Warrington, PA, USA)-embedded tibia sections was evaluated using a fluorescence microscope (Carl Zeiss, Oberkochen, Germany). Trabecular bone histology was evaluated using von Kossa staining kits (ab150687; Abcam, Cambridge, UK) and hematoxylin–eosin stain kits (Sigma-Aldrich, St Louis, MO, USA). Osteoclasts were probed using a tartrate-resistant acid phosphatase (TRAP) staining kit (B-Bridge International Inc., Mountain View, CA, USA). Trabecular volume (BV/TV, %), mineral acquisition rate (MAR, μm/day), and osteoclast number (Oc.N/mm) were quantified using Axio Image Analysis System (Carl Zeiss, Oberkochen, Germany). Six random fields in each section and 3 sections in each animal were selected for histomorphometry. Immunohistochemical staining for paraffine-embedded sections was performed using β-galactosidase (ab136776, Abcam, Cambridge, UK), p16Ink4a (1E12E10, Invitrogen Thermo Fisher Scientific Inc., Waltham, MA, USA), 5-methylcytosine (5mC) (GT411, Invitrogen, Carlsbad, CA, USA), and 8-hydroxydeoxyguanosine (8-OHdG) (BS-1278R; Thermo Fisher Scientific Inc., Waltham, MA, USA). Immunostained osteoblasts in each high-power field (×400 magnification) were counted. Three random fields in each section and 3 sections in each tibia specimen were selected to quantify immunostained cells.
2.8. Ex Vivo Osteogenesis, Adipocyte, and Osteoclast Formation
Mesenchymal cells and macrophage precursor cells in bone marrow were isolated, as previously described [24]. Bone-marrow stromal cells (105 cells/well, 24-well plates) were seeded in an osteogenic condition using StemProTM Osteogenesis Differentiation Kits (A1007201 Thermo Fisher Scientific Inc., Waltham, MA, USA) and in an adipogenic condition using StemProTM Adipogenic Differentiation Kits (A1007001) for 21 days and 15 days, respectively. Mineralized matrices and adipocytes were stained using von Kossa stain kits and Nile Red stain kits (Abcam, Cambridge, UK). Bone-marrow macrophage precursor cells (5 × 104 cells/well, 48-well plates) were incubated in αMEM with 15 ng/mL M-CSF and 40 ng/mL RANKL (R&D Systems, Minneapolis, MN, USA) for 1 week. Osteoclasts were probed using TRAP stain kits. Von-Koss-stained mineralized matrices in each low-power field (x125 magnification) and Nile-red-stained adipocytes and TRAP-stained osteoclasts in each high-power field were measured using the Zeiss Image Analysis System.
2.9. Aged Osteoblast Cultures
Osteoblasts were multiple-passaged as an in vitro model of age-induced bone loss, as previously described [26,27,28]. Upon euthanasia, primary (P0) calvarial osteoblasts were isolated from 3-month-old mice and incubated in DMEM and 10% FBS. Primary osteoblasts (5 × 105/well, 6-well plates) were incubated in medium for 3 days. After 10 passages, osteoblasts were designated to the aged group (P10). In some experiments, 105 cells/well (24-well plates) were incubated in 100 nM 5-Aza-2′-deoxycystidine (5-aza; A3656, Sigma-Aldrich, St Louis, MO, USA) or 10 μM N-acetylcysteine (NAC; A9165, Sigma-Aldrich, St Louis, MO, USA) for 4 h and incubated in an osteogenic medium.
2.10. Oxidative Stress-Induced Osteoblast Senescence
Murine MC3T3-E1 preosteoblasts (2 × 104 cells/48-well plate) were incubated in DMEM and 10% FBS with or without 300 µm H2O2 (H1009, Sigma-Aldrich, St Louis, MO, USA) [29] or 50 µM Oxr1 recombinant protein (MSB1070208; MyBiosource, San Diego, CA, USA) for 6 h and further incubated in osteogenic differentiation medium (DMEM, 10% FBS, 10 mM β-glcerophosphate and 50 mM ascorbate) for 15 days to investigate cellular senescence and mRNA expression.
2.11. Transfection of miR-29a Mimic and Antisense Oligonucleotide
A total of 10 nM miR-29a mimetic, antisense oligonucleotide, and scramble control (miRVana; Thermo Fischer Scientific Inc., Waltham, MA, USA) were added to LipofectamineTM 3000 (InvitrogenTM; Thermo Fischer Scientific Inc., Waltham, MA, USA) and transferred into P0 or P10 osteoblasts (5 × 105 cells/well, 24-well plates).
2.12. Senescence-Association β-galactosidase (SA-β-gal) Staining
SA-β-gal activity in osteoblasts (103 cells/slide) was probed using Senescence β-Galactosidase Staining Kits (#9860, Cell Signaling, Danvers, MA, USA). SA-β-gal-stained cells in each field, 3 fields in each slide, and 3 slides for each experiment were counted.
2.13. RT-PCR
Total RNA was extracted from WT and miR-29aTg osteoblasts using TRI Reagent™ Solution (Thermo Fisher Scientific Inc., Waltham, MA, USA). High-Capacity cDNA Reverse Transcription Kits (Thermo Fisher Scientific Inc., Waltham, MA, USA) were utilized to reversely transcribe 1 μg of total RNA. PCR was investigated using primers (Supplementary Table S1), 2× TaqMan® Universal PCR Master Mix with ABI 7900 Detection System (Applied Biosystems, Foster City, CA, USA), and the threshold value for amplification reaction was probed. Equation 2−ΔΔCt was used to calculate the fold change of mRNA expression.
2.14. Whole Genome Microarray Assay
A total of 10 μg of RNA was amplified using Amino Allyl MessageAmp II aRNA amplification kits (Ambion, Thermo Fisher Scientific Inc., Waltham, MA, USA) and coupled with CyDye using CyDye Post-Labeling Reactive Dye Packs (Cytiva, Marlborough, MA, USA), according to the makers’ instructions. Upon purification, the labeled aRNA was hybridized onto Mouse MOA2.0 whole-genome arrays (Phalanx Biotech Inc., San Diego, CA, USA). Data and clustering were processed using Rosetta Resolver Biosoftware®. Fold change of the gene expression log2 > 1 was considered differentially expressed. Gene ontology and KEGG pathway were clustered using Kobas bioinformatics engine (http://kobas.cbi.pku.edu.cn, accessed on 19 July 2021), as previously described [30].
2.15. Luciferase Activity Assay
Wild-type (5′-UUUUACCUAAUUACAGGUGCUAU-3′; ENST00000344505.4) or 5-bp mutant (5′-UUUUACCUAAUUACAGTAAACAU-3′) of the 3′-UTR of Dnmt3b was constructed into luciferase reporter pCRII-TOPO II vector (InvitrogenTM; Thermo Fischer Scientific Inc., Waltham, MA, USA). A total of 10 ng of luciferase vector and 10 ng Renilla luciferase reporter vector were mixed with LipofectamineTM 3000 Transfection Reagent (InvitrogenTM; Thermo Fischer Scientific Inc., Waltham, MA, USA) and transfected into osteoblasts (104 cells/well, 96-well plate). The reporter cells were transfected into 30 nM scramble control, miR-29a mimetic, or antisense oligonucleotide. Fluorescent luciferase activity was probed using Dual Luciferase Detection Kits and normalized with Renilla luciferase activity.
2.16. Methylation-Specific PCR
Genomic DNA in 5 × 106 osteoblasts was harvested using MagMAX™-96 DNA Multi-Sample Kits (4413021; Invitrogen, Danvers, MA, USA). Methylated DNA was probed using the EZ DNA Methylation™ Kit (Zymo Research, Irvine, CA, USA), according to the maker’s manuals. A total of 10 ng genomic DNA was mixed with 100 μL CT Conversion Reagent with bisulfite at 50 ℃ in the dark for 16 h and incubated at 4 ℃ for 10 min. Upon eluting through Zymo-Spin™ IC Column, the elute was washed with an M-Wash Buffer and mixed with a M-Desulphonation Buffer and an Elution Buffer. PCR analysis of the eluted DNA was performed using the ABI 7900 Detection System together with specific primers, methylated and unmethylated FoxO3 promoter, and miR-29a promoter. PCR analysis of GADPH gene was performed to confirm the equal loading of elute DNA (Supplementary Table S1).
2.17. Immunoblotting
Lysates of 5 × 106 osteoblasts were extracted using Mammalian Cell Lysis Kits (Sigma-Aldrich, St. Louis, MO, USA). Immunoblotting of 5mC, 5hmC, Foxo3, Dnmt3b, and actin levels in the lysates was performed using specific antibodies and SuperSignal™ Western Blotting Kits (Thermo Fisher Scientific Inc., Waltham, MA, USA).
2.18. Statistical Analysis
Differences of age, hip BMD, serum miR-29a, and immunostaining in the non-osteoporosis and osteoporosis groups were analyzed using a Wilcoxon test. The patients’ gender of both groups was analyzed using a Chi-square test. The investigations of WT and miR-29aKO mice were analyzed using a Student’s t-test. The investigations of young and old WT and miR-29aTg mice and in vitro models were analyzed using an ANOVA test and a Bonferroni post hoc test. p value < 0.05 resembled significant difference.
3. Results
3.1. miR-29a Loss, Senescent Osteoblast Overburden, and Oxidative Stress in Human Osteoporosis
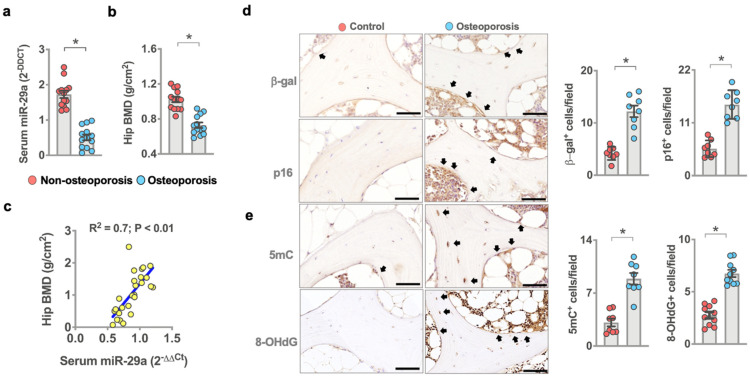
We examined if oxidative stress or osteoblast senescence or miR-29a expression correlated with human osteoporosis. We collected bone biopsies and serum from 13 patients with osteoporosis (5 males and 8 females; 75.8 ± 1.1 years old) and 13 patients without osteoporosis (6 males and 7 females; 36.6 ± 1.9 years old) who required lumbar spine decompression, fixation, discectomy, or vertebroplasty. Serum miR-29a levels (Figure 1a) and bone mineral density of hips (Figure 1b) in patients with osteoporosis were less than in patients without osteoporosis. Serum miR-29a level significantly correlated with the development of osteoporosis (Figure 1c). Plenty of osteoblasts in osteoporotic bone specimens showed strong cellular senescence markers, including β-galactosidase and p16Ink4a immunostaining (Figure 1d), as compared to the control group. Bone cells in the osteoporosis group also displayed strong DNA methylation marker 5-methylcytosine (5mC) immunoreaction and oxidative damage marker 8-hydroxydeoxyguanosine (8-OHdG) (Figure 1e) immunoreactivity, suggesting that DNA hypermethylation and oxidative stress were present in the development of osteoporosis.
Figure 1.
Analysis of miR-29a, osteoblast senescence, oxidative stress, and DNA methylation in human osteoporosis. Decreased serum miR-29a levels (a) and hip BMD (b) in the osteoporosis group. Serum miR-29a levels correlated with osteoporosis (c). Data are mean ± standard error calculated from 13 patients without osteoporosis and 13 patients with osteoporosis who required spine surgery. Osteoblasts in age-mediated osteoporotic bone showed strong β-galactosidase, p16 (d), 5mC, and 8-OHdG (e) immunostaining (arrows) (scale bar, 20 µm). Immunohistochemical data (mean ± standard error) are calculated from 7–8 bone biopsies. Significant difference (asterisks *) was analyzed using a Wilcoxon test.
3.2. miR-29a Deletion Induced Bone Loss and Inhibited Bone Formation Activity
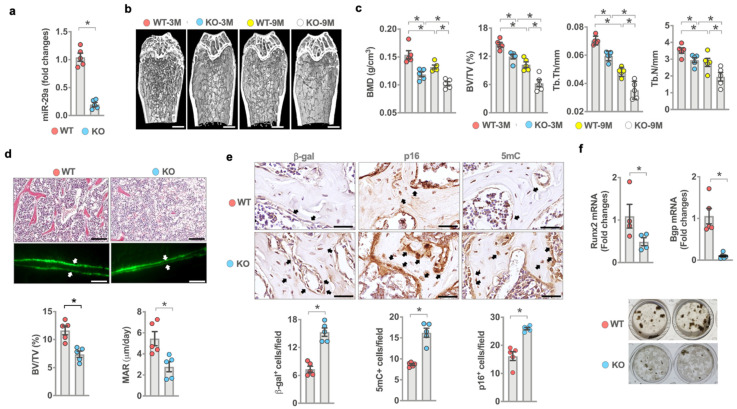
The findings of human bone specimens prompted us to investigate whether miR-29a loss affected bone tissue integrity. To this end, ubiquitous miR-29a knockout mice (miR-29aloxp-Sox2Cre; miR-29aKO) were generated by crossing miR-29aloxP mice with Sox2Cre mice. RT-PCR confirmed miR-29a loss in the bone tissue of 3-month-old miR-29a KO mice (Figure 2a). We divided 3- and 9-month-old mice into young and old mouse groups, respectively. Three-month-old miR-29aKO mice developed sparse trabecular bone microstructure (Figure 2b) together with deceased bone mineral density (BMD), trabecular volume (BV/TV), trabecular thickness (Tb.Th), and trabecular number (Tb.N) (Figure 2c). Of note, bone mass loss and porous trabecular architecture were worsened in 9-month-old miR-29aKO mice as compared to age-matched WT mice. Histological investigations revealed trabecular bone loss and marrow adiposis together with decreased trabecular volume (BV/TV) and low calcein-labeled mineral acquisition rate (MAR) in 3-month-old miR-29aKO skeleton (Figure 2d). Loss of miR-29a function upregulated senescence and DNA methylation in a high number of osteoblasts, which showed strong β-galactosidase, p16, and 5mC immunostaining (Figure 2e). Furthermore, bone-marrow mesenchymal cells in 3-month-old miR-29aKO mice showed less osteogenic differentiation potential, including decreased Runx2 and osteocalcin (Bgp) expression and mineralized extracellular matrix underproduction (Figure 2f), as compared to age-matched WT mice.
Figure 2.
Analysis of miR-29a expression, osteoblast senescence, bone mass, and microstructure in miR-29a knockout mice. Low miR-29a expression in the bone tissue of 3-month-old miR-29aKO mice (a). μCT images showing sparse trabecular microstructure (b) (scale bar, 50 μm) and decreased BMD, BV/TV, Tb.Th, and Tb.N (c) in young and old miR-29aKO bone tissue. Significant differences of investigations (mean ± standard error, n = 5 mice) were analyzed using an ANOVA test and Bonferroni post hoc test. Three-month-old miR-29aKO bone tissue showed trabecular bone loss, marrow adiposis (scale bar, 20 μm), weak calcein labeling (scale bar, 40 μm), and decreased BV/TV and MAR (d). Osteoblasts in miR-29aKO bone tissue showed strong β-gal, p16, and 5mC immunostaining (e) (scale bar, 10 μm). miR-29a knockout reduced osteogenic gene expression and von-Kossa-stained mineralization matrix deposition of bone-marrow stromal cells (f). Significant differences (asterisks *) of investigations (mean ± standard error, n = 5–6 mice) were analyzed using the Wilcoxon test.
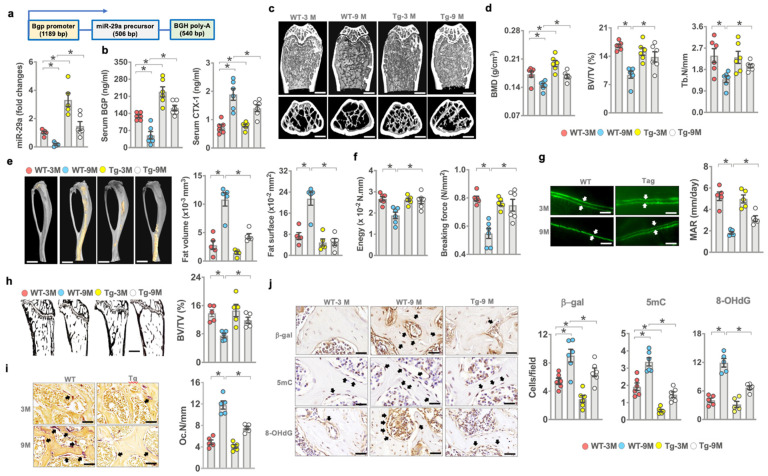
3.3. Transgenic Overexpression of miR-29a Slowed Bone Loss in Old Mice
Given that miR-29a loss accelerated bone mass loss and microstructure deterioration, we asked whether transgenic overexpression of miR-29a in bone tissue changed the skeletal integrity of old animals. We bred osteoblast-specific miR-29a transgenic mice under the control of the Bgp promoter (miR-29aTg) [24] (Figure 3a). We divided 3- and 9-month-old mice into young and old mouse groups, respectively. miR-29a expression in bone tissue (Figure 3a) and serum bone formation marker Bgp levels were downregulated in old WT animals, whereas serum resorption marker C-telopeptide of collagen I (CTX-1) levels were increased (Figure 3b). miR-29a loss and serum bone marker alteration were compromised in old miR-29aTg mice. Old WT mice developed sparse bone microstructure (Figure 3c) as evident from decreased BMD, BV/TV, and Tb.N (Figure 2d). Old miR-29aTg mice showed mild BMD loss and a well-connected trabecular bone network. Old WT bone tissue developed marrow adiposity as evidenced in increases in marrow fat volume and surface (Figure 3e). These animals had less bone biomechanical strength, including breaking force and energy (Figure 3f), than young WT mice. miR-29a overexpression compromised marrow fat overproduction and biomechanics loss in old mice.
Figure 3.
Effects of miR-29a overexpression on bone mass, mechanics, and histomorphometry of young and aged mice. Schematic drawing for the linear gene construct for the generation of osteoblast-specific miR-29aTg mice. miR-29a overexpression attenuated miR-29a loss in bone tissue (a) and serum Bgp and CTX-1 level alteration in old mice (b). μCT revealing sparse trabecular microstructure in old WT mice and well-woven bone architecture in old miR-29aTg mice (c); scale bar, 50 μm in upper panels; 90 μm in lower panels. miR-29a overexpression improved age-induced loss in BMD, BV/TV, and Tb.N (d). miR-29a compromised fatty marrow development (scale bar, 5 mm) (e) and biomechanics loss (f) and reversed mineral acquisition (scale bar, 40 μm) (g) and von-Koss-stained trabecular bone volume (scale bar, 40 μm) (h), as well as reduced TRAP-stained osteoclast formation (scale bar, 20 μm) (i). miR-29a overexpression attenuated β-galactosidase, 5mC, and 8-OHdG immunoreactivity (j); scale bar, 15 μm. The significant difference (asterisks *) of investigations (mean ± standard error, n = 5–6 mice) was analyzed using an ANOVA test and Bonferroni post hoc test.
Old WT bone tissue showed less von-Kossa-stained trabecular bone morphology (BV/TV; Figure 3g) and decreased bone mineral acquisition (MAR; Figure 3h) together with plenty of tartrate-resistant acid-phosphate-stained osteoclasts developed along trabecular bone (Oc.N/mm; Figure 3i) as compared to young WT mice. miR-29Tg bone revealed a mild loss in static and dynamic bone formation and osteoclast overburden. A high number of osteoblasts in old WT bone showed strong β-galactosidase, 5mC, and 8-OHdG immunoreactivity. Mild senescence, DNA methylation, and oxidative stress were present in osteoblasts in old miR-29aTg mice (Figure 3j).
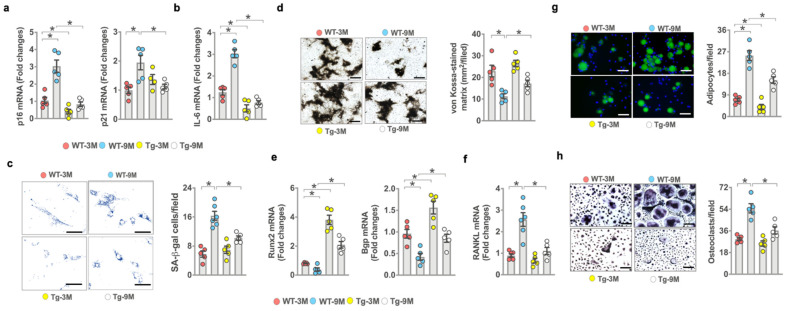
3.4. miR-29a Attenuated Senescence and Osteogenesis Loss in Old Mice
Consistent with the analysis of senescent osteoblast overburden in osteoporotic bone, senescence program, including p16Ink4a, p21CIP expression (Figure 4a), inflammatory cytokine IL-6 expression (Figure 4b), and SA-β-gal activity (Figure 4c) were significantly increased in bone-marrow mesenchymal cells of old WT mice. However, the osteogenesis of bone-marrow stromal cells as evidenced in von-Kossa-stained mineralized matrix production (Figure 4d), Runx2, and Bgp expression (Figure 4e) was reduced in old WT mice. Senescence program, inflammation, and osteogenesis loss were improved in old miR-29aTg mice. On the other hand, osteoclast factor RANKL expression (Figure 4f) and fluorescent Nile-red-stained adipocyte formation of bone-marrow stromal cells (Figure 4g), as well as TRAP-stained osteoclast formation of bone-marrow macrophage precursor cells (Figure 4h), were upregulated in old WT mice. The ex vivo adipocytic activity and osteoclastogenic differentiation capacity were compromised in old miR-29aTg mice.
Figure 4.
Effects of miR-29a overexpression on ex vivo osteogenic, adipogenic, and osteoclastogenic differentiation capacity. miR-29a repressed age-induced p16, p21 (a), IL-6 expression (b), and SA-β-galactosidase activity of primary bone-marrow mesenchymal cells (c); scale bar, 20 μm. miR-29a reversed age-induced loss in mineralized nodule formation (d) (scale bar, 40 μm) and (e) Runx2 and Bgp expression (e) and decreased RANKL expression (f). miR-29a compromised (g) fluorescent Nile-red-stained adipocyte formation (scale bar, 20 μm) and (h) TRAP-stained osteoclast formation (scale bar 20 μm) in old mice. Significant difference (asterisks *) of investigations (mean ± standard error, n = 5) analyzed using an ANOVA test and a Bonferroni post hoc test.
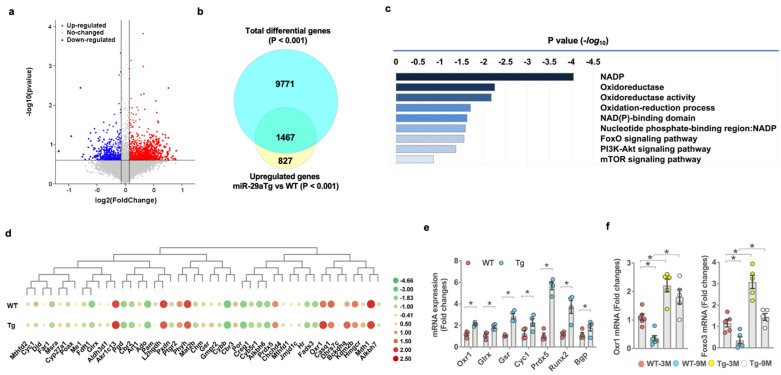
3.5. miR-29a Controlled Redox Reaction, Oxidation Resistance-1, and FoxO3 Signaling
We characterized transcriptomic landscapes of 3-month-old miR-29aTg and WT osteoblasts using whole-genome microarray analysis (Figure 5a). Of 9971 differentially expressed genes, miR-29a upregulated 1467 gene transcription (Figure 5b) related to a plethora of redox reactions and intracellular pathways, including NADP, oxidoreductase, oxidoreduction activity, FoxO, PI3K/Akt, and mTOR signaling pathways, as evidenced in pathway ontology analysis (Figure 5c). miR-29a overexpression increased the gene transcription of antioxidant proteins, such as oxidation resistance 1 (Oxr1), glutaredoxin (Glrx), glutathione disulfide reductase (Gsr), cytochrome 1 (cyc1), and peroxiredoxin 5 (Prdx5) (Figure 5d). RT-PCR analysis confirmed significant increases in Oxr1, Glrx, Gsr, Cyc1, and Prdx5 expression and promoted Runx2 and Bgp expression in miR-29aTg osteoblasts (Figure 5e). Oxr1 and FoxO3 are important to counteract oxidative stress or cellular senescence [31,32]. We uncovered that Oxr1 and FoxO3 expression of bone-marrow stromal cells was significantly inhibited in old WT bone tissue. Oxr1 and FoxO3 loss were improved in old miR-29aTg mice (Figure 5f).
Figure 5.
Transcriptomic landscapes of miR-29aTg and wild-type osteoblasts. Volcanic plots showing differential gene expression in osteoblasts between 3-month-old miR-29aTg and WT mice (a). Red, blue, and grey spots indicate a gene expression that is upregulated, downregulated, and unaffected, respectively. Venn diagram showing the gene transcripts, which were increased the miR-29aTg group (b). Pathway ontology analysis revealing significantly affected biological reactions in the miR-29aTg group (c). Heatmap of transcriptomic profile showing 45 gene transcripts in redox reactions (d). Transcriptomic profiles of miR-29aTg and wild-type osteoblasts were analyzed in 3 mice. Orx1, Glrx, Gsr, Cyc1, Prdx5, Runx2, and Bgp mRNA expression was increased in miR-29aTg osteoblasts, as evidenced in RT-PCR analysis (e). Significant difference of investigations (mean ± standard error, n = 4 mice) was analyzed using a Student’s t-test. Orx1 and FoxO3 loss in bone-marrow mesenchymal cells was compromised in old miR-29aTg mice (f). Significant differences (asterisks *) of investigations (n = 5 mice) were analyzed using an ANOVA test and a Bonferroni post hoc test.
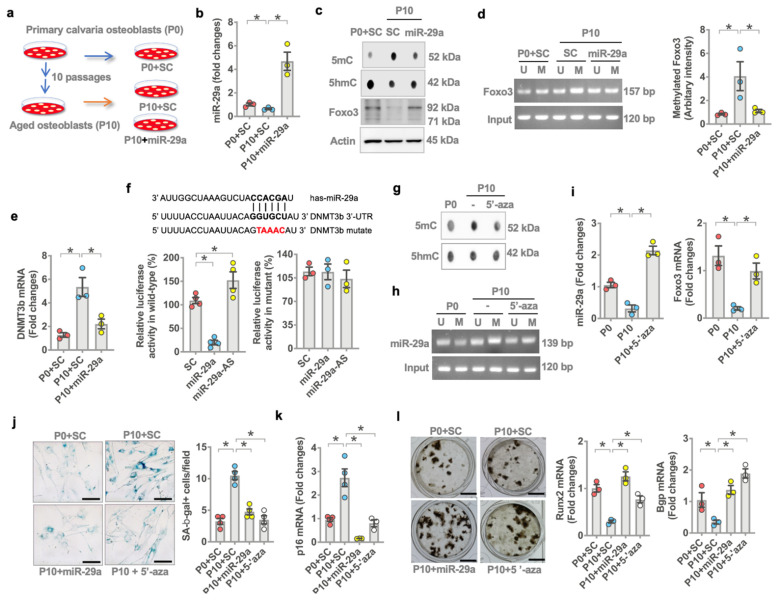
3.6. miR-29a Repressed DNMT3b-Mediated Foxo3 Methylation
The analysis of less DNA methylation and mild FoxO3 loss in an old miR-29aTg bone microenvironment was used to verify if the microRNA affected FoxO3 methylation in aged osteoblasts. Multiple passaged osteoblasts (passage 10, P10) (Figure 6a) were incubated as a model of osteoblast aging [26,27,28]. miR-29a expression (Figure 6b) and FoxO3 level were reduced upon multiple passages, whereas 5mC levels were increased (Figure 6c). Forced miR-29a expression by miR-29a mimetic downregulated DNA methylation, reversing FoxO3 signaling in multiple-passaged osteoblasts (Figure 6c). The methylation of CpG dinucleotide around −4057~−2058 bp in the transcription start site of the FoxO3 promoter (Figure 6d) was significantly upregulated in multiple-passaged cells. miR-29a attenuated FoxO3 promoter hypermethylation in aged osteoblasts (Figure 6d), as is evident from the bisulfite conversion of DNA and methylation-specific PCR analysis.
Figure 6.
Effects of miR-29a on FoxO3 promoter methylation and Dnmt3b expression in aged osteoblasts. Schematic drawing for a model of multiple passages-induced osteoblast aging (a). Forced miR-29a expression reversed miR-29a (b) and FoxO3 levels but decreased 5mC levels (c) and FoxO3 promoter methylation (d) in multiple-passaged osteoblasts. miR-29a attenuated (e) Dnmt3b expression (e) and luciferase reporter activity of 3′-UTR of Dnmt3b (f). 5-aza decreased 5mC levels (g) and miR-29a promoter methylation (h), reversing miR-29a and FoxO3 expression (i) in multiple passage osteoblasts. miR-29a or 5-aza compromised multiple-passage-induced SA-β-gal activity (j) and p16 expression (k), improving mineralized matrix production and Runx2 and Bgp expression (l). Significant differences (asterisks *) of investigations (mean ± standard error, n = 3–4 experiments) were analyzed using an ANOVA test and a Bonferroni post hoc test. SC, scramble control; U, unmethylated amplicons; M, methylated amplicons. AS, antisense oligonucleotide; 5-aza, 5′-azacytosine.
We investigated the mechanism by which miR-29a repressed FoxO3 methylation in aged osteoblasts. A bioinformatics prediction (http://targetscan.org/vert_72/, accessed on 19 July 2021) shows that DNA methyltransferase 3b (Dnmt3b) catalyzes DNA methylation and is a putative target of miR-29a. Dnmt3b expression was increased in multiple-passaged osteoblasts. This effect was downregulated in miR-29a mimetic-treated osteoblasts (Figure 6e). miR-29a also reduced luciferase reporter activity of wild-type rather than mutated 3′-untranslated regions (3′-UTR) of Dnmt3b (Figure 6f). miR-29a interference by antisense oligonucleotide increased the luciferase activity, indicating that miR-29a directly disrupted Dnmt3b mRNA expression (Figure 6f). Of interest, the inhibition of Dnmt3b activity by 5-aza-2-deoxycytidine (5-aza) attenuated DNA hypermethylation (Figure 6g), downregulating methylation of the CpG island around −788~1912 bp in the transcription start site of miR-29a promoter (Figure 6h) and improving miR-29a and Foxo3 expression (Figure 6i) in multiple-passaged osteoblasts. As a result, miR-29a or 5-aza downregulated SA-β-gal activity (Figure 6j) and p16 expression (Figure 6k), preserving mineralized matrix production, Runx2 and Bgp expression (Figure 6l) in multiple-passaged cells.
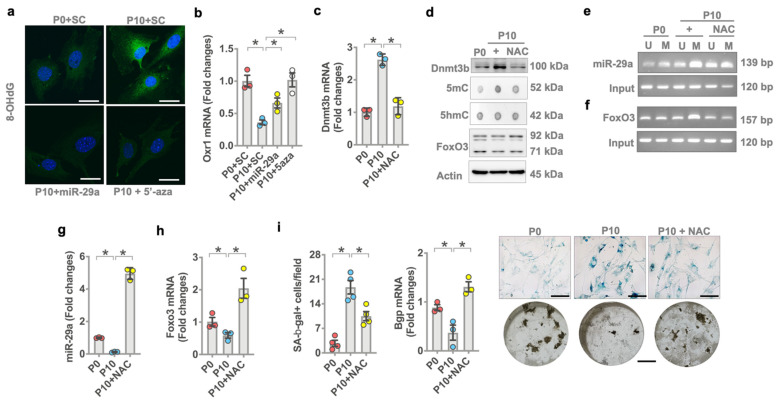
3.7. miR-29a Attenuated Oxidative Stress, Aging and Osteogenic Activity
Of interest, forced miR-29a expression or 5-aza also reversed oxidative stress in multiple-passaged cells as was evident from weak 8-OHdG immunofluorescence (Figure 7a) and increased antioxidant protein Oxr1 expression (Figure 7b). We investigated whether the repression of oxidative stress changed miR-29a or FoxO3 methylation in aged osteoblasts. Antioxidant N-acetylcysteine (NAC) repressed Dnmt3b mRNA expression (Figure 7c) and protein levels together with decreased 5mC levels (Figure 7d) in multiple-passaged osteoblasts. NAC also inhibited miR-29a promoter methylation (Figure 7e) and FoxO3 promoter methylation (Figure 7f) to reverse miR-29a (Figure 7g) and FoxO3 mRNA expression (Figure 7h) and protein levels (Figure 7d) and improved SA-β-gal activity, osteocalcin expression, and mineralized nodule formation in multiple-passaged osteoblasts (Figure 7i).
Figure 7.
Effects of N-acetylcysteine on miR-29a expression and osteoblast senescence. miR-29a mimetic or 5-aza attenuated age-induced 8-OHdG immunofluorescence (a) (scale bar, 10 μm) and Orx1 loss (b). Antioxidant NAC attenuated Dnmt3b mRNA expression (c) and 5mC levels (d). NAC attenuated age-induced miR-29a promoter methylation (e) and FoxO3 promoter methylation (f), reversing miR-29a (g) and FoxO3 mRNA expression (h) in aged osteoblasts to decrease SA-β-gal activity (i); (scale bar, 20 μm) and reversed Bgp expression and mineralized nodule formation (i). Significant differences (asterisks *) of investigations (mean ± standard error, n = 3 experiments) were analyzed using an ANOVA test and a Bonferroni post hoc test. SC, scramble control; U, unmethylated amplicon; M, methylated amplicon. 5-aza, 5′-azacytosine; NAC, N-acetylcysteine.
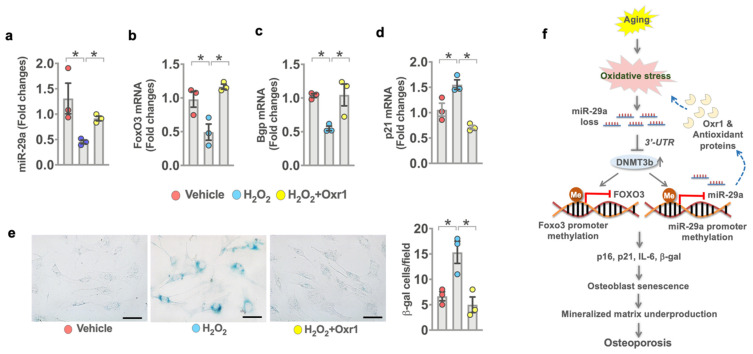
3.8. Oxr1 Attenuated Oxidative Stress-Induced miR-29a Loss and Senescence
Given that miR-29a and Orx1 loss were present in senescent osteoblasts, we investigated what role antioxidant protein Oxr1 may play in miR-29a control of osteoblast senescence. Osteoblasts were incubated in H2O2 as an in vitro model of oxidative stress2-induced cellular senescence [29]. Murine MC3T3-E1 osteoblasts were incubated in an osteogenic medium with or without H2O2 or Oxr1 recombinant protein for 15 days. H2O2 significantly reduced miR-29a (Figure 8a), FoxO3 (Figure 8c), and Bgp expression (Figure 8c), whereas oxidative stress upregulated p21 expression (Figure 8d) as compared to the vehicle group. Oxr1 recombinant protein reversed H2O2-induced loss in miR-29a, FoxO3, and Bgp expression and attenuated p21 expression. Plenty of osteoblasts showed strong SA-β-gal activity upon incubating in H2O2. Oxr1-treated cells showed weak SA-β-gal staining (Figure 8e).
Figure 8.
Effects of Oxr1 recombinant protein on miR-29a signaling and senescence in MC3T3-E1 osteoblasts. Oxr1 attenuated H2O2-mediated loss in miR-29a (a), FoxO3 (b), and Bgp (c) expression and the inhibited p21 expression (d) of murine osteoblasts. Orx1 reversed H2O2-induced SA-β-gal activity (e); scale bar, 15 μm. A significant difference (asterisk *) of investigations (mean ± standard error, n = 3 experiments) was analyzed using an ANOVA test and a Bonferroni post hoc test. Schematic graphs showing miR-29a protection against oxidative stress, osteoblast senescence, and osteoporosis. miR-29a targets Dnmt3b-mediated Foxo3 promoter hypermethylation and increased antioxidant protein Oxr1, compromising age-induced Foxo3 loss, oxidative stress, osteoblast senescence, and osteoporosis development (f).
4. Discussion
Osteogenic cell senescence involves postnatal bone homeostasis, microstructure integrity, or osteoporosis development [33]. Programmed senescence in osteogenic progenitor cells sustains long bone development in late pubertal mice [34]; however, senescent osteoblast overburden in a skeletal microenvironment correlates with the development of age [3], chemotherapy [35], and irradiation [36]-induced bone mass loss and architecture damage. Accumulating studies reveal that oxidative stress [37] and the epigenetic pathway [38], including DNA methylation and microRNA signaling, regulate cell fate and metabolism. Little is known about the epigenetic pathway control of oxidative stress in osteoblast aging and bone loss. This study uncovered that miR-29a slowed osteoblast senescence, preserving extracellular mineralized matrix production to protect from bone loss in old mice. miR-29a attenuated FoxO3 loss and oxidative stress through repressing Dnmt3b-mediated antioxidant protein Oxr1 loss and DNA hypermethylation in aged osteoblasts. Collective evidence conveys a new insight into the antioxidation and anti-aging potential of miR-29a against bone loss.
Investigations of clinical specimens uncovered a plethora of reactions, such as miR-29a loss, DNA hypermethylation, osteoblast senescence, and oxidative stress in human osteoporosis. Expanding studies show increased p16 expression [39] or DNA methylome alteration [13] in bone biopsies of human postmenopausal osteoporosis. This analysis prompted us to investigate what role miR-29a may play in DNA methylation and oxidative stress in osteoporosis.
We, for the first time, have revealed phenotypes of low bone mass in miR-29a knockout mice, suggesting that this molecule was required to maintain skeletal tissue integrity. The adverse effect of miR-29a loss on bone homeostasis is also pointed out by a study manifesting that transgenic overexpression of miR-29-3p tough decoy in mice inhibits bone mineral accretion and trabecular bone volume [40]. Nine-month-old mice develop osteoporosis, including low bone mass or trabecular volume [26,27,28,29]. In this study, the extent of skeletal deterioration was worsened in 9-month-old miR-29aKO mice. miR-29a deletion induced DNA hypermethylation and osteoblast senescence. The impact of miR-29a loss on osteoblast fate and bone integrity in this murine model further explained the histological features of senescent osteoblast overburden in human osteoporotic bone.
Striking findings were that old miR-29Tg mice showed fewer osteoporosis signs, including mild MAR loss and osteoclast formation, than age-matched WT mice. miR-29a appeared to attenuate excessive bone turnover by preserving the osteogenic differentiation capacity of mesenchymal progenitor cells and reducing RANKL expression to downregulate osteoclastic activity. The senescence-associated secretory phenotype, like IL-6 expression [41], was also repressed in mesenchymal progenitor cells of old miR-29aTg mice. These investigations underpinned the important role of miR-29a in delaying age-induced skeletal deterioration.
We revealed that miR-29a, at least in part, disrupted the Dnmt3b catalysis of FoxO3 promoter hypermethylation to compromise FoxO3 loss, reversing senescence and mineralized matrix underproduction in aged osteoblasts. Transcription factor Foxo3 is important to slow cellular aging, promoting tissue homeostasis and function [35]. FoxO3 interference induces reactive oxygen radical overproduction, inhibiting the osteogenic differentiation capacity of mesenchymal stem cells [42]. The methylation status of the FoxO3 gene correlates with human tissue aging [43]. In addition, a reciprocal regulation was present in miR-29a and Dnmt3b. Dnmt3b inhibition mitigated miR-29a promoter methylation, in turn reversing miR-29a and FoxO3 functions to drive osteoblasts away from senescence. The inhibition of DNA methyltransferase in bone-forming cells promotes osteogenic activity. DNMT3b knockdown or 5-aza-induced DNA hypomethylation promotes the osteogenic differentiation of human [17] and murine [44]. The array of analysis in this study throws a new light upon an epigenetic crosstalk through which microRNA and methyl DNA regulated osteoblast senescence in the development of osteoporosis.
Oxidative stress is a prominent deleterious reaction, dysregulating protein stability or epigenetic pathways to hinder survival or biological activity in senescent cells [45]. Of note, miR-29a repressed 8-OHdG formation in aged osteoblasts. A transcriptomic landscape was that miR-29a affected redox reactions by promoting a plethora of antioxidant proteins in osteoblasts. Expanding studies reveal the biological roles of Oxr1, Glrx, and Gsr in cellular senescence. For example, forced Gsr expression downregulates Klotho loss-mediated renal cell aging and dysfunction [46]. Antioxidant protein Oxr1 promotes senolytic activity to sustain the viability of aged fibroblasts. Oxr1 knockdown aggravates oxidative stress and apoptosis [31]. In this study, Orx1 was advantageous to fend off oxidative stress, FoxO3 loss, and senescence in H2O2-treated osteoblasts and aged skeleton. Oxidative stress dysregulates epigenetic signatures, affecting the differentiation capacity of mesenchymal progenitor cells [47]. miR-29 involves the oxidative stress and viability of human mesenchymal stem cells upon DGCR8 interference [48]. The in vitro analysis of this study consolidated the importance of miR-29a and Oxr1 in repressing oxidative stress to downregulate DNA hypermethylation-induced osteoblast dysfunction. In this study, patients in the osteoporosis group were significantly older than the control group. However, the limitation of the experiment for human bone biopsies is the absence of osteoporosis indications in age-matched young patients who required spinal surgery. The possibility cannot be ruled out that ubiquitous miR-29a knockout may change other tissues’ integrity or function, which may influence osteoblast function and bone homeostasis. miR-29a signaling may affect other DNA methylation enzymes or redox regulators to maintain anabolic activity in aged osteoblasts. The investigations related to the interactions of miR-29a, oxidative stress, and epigenetic pathways reveal a new molecular mechanism underlying bone mass loss.
5. Conclusions
Taken together, profound evidence revealed that miR-29a loss, oxidative stress, and DNA hypermethylation correlated with osteoblast aging in human osteoporosis. miR-29a knockout accelerated osteoblast senescence and bone loss. miR-29a reversed FoxO3 loss to improve senescence program through targeting Dnmt3b-mediated FoxO3 methylation and increased antioxidant proteins, including Oxr1, to downregulate oxidative stress and DNA methylation, compromising age-induced osteoblast loss and osteoporosis (Figure 8f). This study highlights a new epigenetic mechanism underlying oxidative stress-mediated osteoblast senescence and senile osteoporosis, as well as the anti-aging and antioxidation effects of miR-29a, DNA methylation inhibitor, and Oxr1 on age-induced osteoblast dysfunction and bone loss.
Acknowledgments
This study is supported in part by [NHRI-EX110-11029SI] from the National Health Research Institute and [CMRPG8K0611-3] from Chang Gung Memorial Hospital, Taiwan. We are grateful for the Core Laboratory for Animal Phenomics & Diagnostic for the use of μCT and biomechanical analysis, the Institute for Translational Research in Biomedicine, Kaohsiung Chang Gung Memorial Hospital, for the use of the laser confocal microscope, as well as the Taiwan Animal Consortium for the technical consultation.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/antiox10081248/s1, Table S1: Sequences of primers for RT-PCR and MSP-PCR analysis.
Author Contributions
Study conception and design: W.-S.L., R.-W.W., Y.-S.C., J.-Y.K., S.-Y.W., H.J. and F.-S.W.; cell culture analysis: Y.-S.C.; microarray, ChIP-PCR, and bioinformatics analysis: W.-S.L. and Y.-S.C.; in vivo and μCT analysis: Y.-S.C.; histology and immunoblotting analysis: S.-Y.W.; clinical diagnosis: R.-W.W. and J.-Y.K.; analysis and interpretation of data: W.-S.L., R.-W.W., H.J. and F.-S.W.; article drafting and revision: W.-S.L., R.-W.W., H.J. and F.-S.W. All authors have read and agreed to the published version of the manuscript.
Funding
This study was in part supported by [NHRI-EX110-11029SI] from the National Health Research Institute and [CMRPG8K0611-3] from Chang Gung Memorial Hospital, Taiwan.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki and approved by the Chang Gung Medical Foundation Institutional Review Board (Affidavit #202000823B0). Informed consent was obtained from patients who required spine surgery. Animal experiments were approved by Institutional Animal Use and Care Committee, Kaohsiung Chang Gung Memorial Hospital (Affidavit #2014120401).
Informed Consent Statement
Informed consent was obtained from patients involved in the study.
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data related to patients’ information are not publicly available due to privacy or ethical restrictions.
Conflicts of Interest
The authors declare no conflict of interest.
Footnotes
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Compston J.E., McClung M.R., Leslie W.D. Osteoporosis. Lancet. 2019;393:364–376. doi: 10.1016/S0140-6736(18)32112-3. [DOI] [PubMed] [Google Scholar]
- 2.Van den Beld A.W., Kaufman J.M., Zillikens M.C., Lamberts S.W.J., Egan J.M., van der Lely A.J. The physiology of endocrine system with ageing. Lancet Diabetes Endocrinol. 2018;6:647–658. doi: 10.1016/S2213-8587(18)30026-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Farr J.N., Xu M., Weivoda M.M., David G., Monroe D.G., Fraser D.G., Onken J.L., Negley B.A., Sfeir J.G., Ogrodnik M.B., et al. Targeting cellular senescence prevents age-related bone loss in mice. Nat. Med. 2017;23:1072–1079. doi: 10.1038/nm.4385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jacome-Galarza C.E., Percin G.I., Muller J.T., Mass E., Lazarov T., Eitler J., Rauner M., Yadav V.K., Crozet L., Bohm M., et al. Developmental origin, functional maintenance and genetic rescue of osteoclasts. Nature. 2019;568:541–545. doi: 10.1038/s41586-019-1105-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lane R.K., Hilsabeck T., Rea S.L. The role of mitochondrial dysfunction in age-related diseases. Biochem. Biophys. Acta. 2015;1847:1387–1400. doi: 10.1016/j.bbabio.2015.05.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gao B., Lin X., Jing H., Fan J., Ji C., Jie Q., Zheng C., Wang D., Xu X., Hu Y., et al. Local delivery of tetramethylpyrazine eliminates the senescent phenotype of bone marrow mesenchymal stromal cells and creates an anti-inflammatory and angiogenic environment in aging mice. Aging Cell. 2018;17:e12741. doi: 10.1111/acel.12741. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Tchknoia T., Kirkland J.L. Aging, cell senescence, and chronic disease: Emerging therapeutic strategies. JAMA. 2018;320:1319–1320. doi: 10.1001/jama.2018.12440. [DOI] [PubMed] [Google Scholar]
- 8.Farr J.N., Almeida M. The spectrum of fundamental basic science discoveries contributing to organismal aging. J. Bone Miner. Res. 2018;33:1568–1584. doi: 10.1002/jbmr.3564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.López-Otin C., Blasco M.A., Patridge L., Serrano M., Kroemer G. The hallmarks of aging. Cell. 2013;153:1194–1217. doi: 10.1016/j.cell.2013.05.039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Feinberg A.P. The key role of epigenetics in human disease prevention and mitigation. N. Engl. J. Med. 2018;378:1323–1334. doi: 10.1056/NEJMra1402513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Luo C., Hajkova P., Ecker J.R. Dynamic DNA methylation: In the right place at the right time. Science. 2018;361:1336–1340. doi: 10.1126/science.aat6806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Petkovich D.A., Podolskiy D.I., Lobanov A.V., Lee S.G., Miller R.A., Gladyshev V.N. Using DNAmethylation profiling to evaluate biological age and longevity interventions. Cell Metab. 2017;25:954–960.e6. doi: 10.1016/j.cmet.2017.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Morris J.A., Tsai P.C., Joehanes R., Zheng J., Trajanoska K., Soerensen M., Forgetta V., Castillo-Fernandez J.E., Frost M., Spector T.D., et al. Epigenome-wide association of DNA methylation in whole blood with bone mineral density. J. Bone Miner. Res. 2017;32:1644–1650. doi: 10.1002/jbmr.3148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.van Meurs J.B., Boer C.G., Lopez-Delgado L., Riancho J.A. Role of epigenomics in bone and cartilage disease. J. Bone Miner. Res. 2019;34:215–230. doi: 10.1002/jbmr.3662. [DOI] [PubMed] [Google Scholar]
- 15.Vrtacnik P., Marc J., Ostanek B. Hypoxia mimetic deferoxamine influences the expression of acetylation- and DNA methylation-associated gene in osteoblasts. Connect. Tissue Res. 2015;56:228–235. doi: 10.3109/03008207.2015.1017573. [DOI] [PubMed] [Google Scholar]
- 16.Shen W.C., Lai Y.C., Li L.H., Liao K., Lai H.C., Kao S.Y., Wang J., Chuong C.M., Hung S.C. Methylation and PTEN activation in dental pulp mesenchymal stem cells promotes osteogenesis and reduces oncogenesis. Nat. Commun. 2019;10:2226. doi: 10.1038/s41467-019-10197-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li L., Wang H., Chen X., Li X., Wang G., Jie Z., Zhao X., Sun X., Huang H., Fan S., et al. Oxidative stress-induced hypermethylation of KLF5 promoter mediated by DNMT3B impairs osteogenesis by diminishing the interaction with beta-catenin. Antioxid. Redox Signal. 2021;35:1–20. doi: 10.1089/ars.2020.8200. [DOI] [PubMed] [Google Scholar]
- 18.Mendell J.T., Olson E.N. MicroRNAs is stress signaling and human disease. Cell. 2012;148:1172–1187. doi: 10.1016/j.cell.2012.02.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Aquino-Martinez R., Farr J.N., Weivoda M.M., Negley B.A., Onken J.L., Thicke B.S., Fulcer M.M., Fraser D.G., van Wijnen A.J., Khosla S., et al. miR-219a-5p regulates Rorβ during osteoblast differentiation and in age-related bone loss. J. Bone Miner. Res. 2019;34:135–144. doi: 10.1002/jbmr.3586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yang M., Li C.J., Sun X., Guo Q., Xiao Y., Su T., Tu M.L., Peng H., Lu Q., Liu Q., et al. MiR-497∼195 cluster regulates angiogenesis during coupling with osteogenesis by maintaining endothelial Notch and HIF-1α activity. Nat. Commun. 2017;8:16003. doi: 10.1038/ncomms16003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Xu R., Shen X., Si Y., Fu Y., Zhu W., Xiao T., Fu Z., Zhang P., Cheng J., Jiang H. MicroRNA-31a-5p from aging BMSCs links bone formation and resorption in the aged bone marrow microenvironment. Aging Cell. 2018;17:e12794. doi: 10.1111/acel.12794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Li B., Zhao J., Ma J.X., Li G.M., Zhang Y., Xing G.S., Liu J., Ma X.L. Overexpression of DNMT1 leads to hypermethylation of H19 promoter and inhibition of Erk signaling pathway in disuse osteoporosis. Bone. 2018;111:82–91. doi: 10.1016/j.bone.2018.03.017. [DOI] [PubMed] [Google Scholar]
- 23.Zhang R., Wang N., Zhang L.N., Huang N., Song T.F., Li Z.Z., Li M., Luo X.G., Zhou H., He H.P., et al. Knockdown of DNMT1 and DNMT3a promotes the angiogenesis of human mesenchymal stem cells leading to arterial specific differentiation. Stem Cells. 2016;34:1273–1283. doi: 10.1002/stem.2288. [DOI] [PubMed] [Google Scholar]
- 24.Lian W.S., Wu R.W., Lee M.S., Chen Y.S., Sun Y.C., Wu S.L., Ke H.J., Ko J.Y., Wang F.S. Subchondral mesenchymal stem cells from osteoarthritic knees display high osteogenic differentiation capacity through microRNA-29a regulation of HDAC4. J. Mol. Med. 2017;95:1327–1340. doi: 10.1007/s00109-017-1583-8. [DOI] [PubMed] [Google Scholar]
- 25.Scheller E.L., Doucette C.R., Learman B.S., Cawthorn W.P., Khandaker S., Schell B., Wu B., Ding S.Y., Bredella M.A., Fazeli P.K., et al. Region-specific variation in the properties of skeletal adipocytes reveals regulated and constitutive marrow adipose tissues. Nat. Commun. 2015;6:7808. doi: 10.1038/ncomms8808. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Yang R., Chen J., Zhang J., Qin R., Wang R., Qiu Y., Mao Z., Goltzman D., Miao D. 1,25-Dihydroxyvitamin D protects against age-related osteoporosis by a novel VDR-Ezh2-p16 signal axis. Aging Cell. 2020;19:e13095. doi: 10.1111/acel.13095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fang J., Yan Y., Teng X., Wen X., Li N., Peng S., Liu W., Donadeu F.X., Zhao S., Hua J. Melatonin prevents senescence of canine adipose-derived mesenchymal stem cells through activating NRF2 and inhibiting ER stress. Aging. 2018;10:2954–2972. doi: 10.18632/aging.101602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chen J.H., Ozanne S.E., Hales N. Methods of cellular senescence induction using oxidative stress. Methods Mol. Biol. 2007;371:179–189. doi: 10.1007/978-1-59745-361-5_14. [DOI] [PubMed] [Google Scholar]
- 29.Zou D.B., Mou Z., Wu W., Liu H. TRIM33 protects osteoblasts from oxidative stress-induced apoptosis in osteoporosis by inhibiting FOXO3a ubiquitylation and degradation. Aging Cell. 2021;8:e13367. doi: 10.1111/acel.13367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Huang D.W., Sherman B.T., Lempicki R.A. Systematic and integrative analysis of large gene lists using DAVID bioinformatics resources. Nat. Protoc. 2009;4:44–57. doi: 10.1038/nprot.2008.211. [DOI] [PubMed] [Google Scholar]
- 31.Zhang X., Zhang S., Liu X., Wang Y., Chang J., Zhang X., Mackintosh S.G., Tackett A.J., He Y., Lv D., et al. Oxidation resistance 1 is a novel senolytic target. Aging Cell. 2018;17:e12780. doi: 10.1111/acel.12780. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Calissi G., Lam E.W., Link W. Therapeutic strategies targeting FOXO transcription factors. Nat. Rev. Drug Discov. 2020;20:21–38. doi: 10.1038/s41573-020-0088-2. [DOI] [PubMed] [Google Scholar]
- 33.Khosla S., Farr J.N., Tchkonia T., Kirkland J.L. The role of cellular senescence in ageing and endocrine disease. Nat. Rev. Endocrinol. 2021;16:263–275. doi: 10.1038/s41574-020-0335-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Li C., Chai Y., Wang L., Gao B., Chen H., Gao P., Zhou F.Q., Luo X., Crane J.L., Yu B., et al. Programmed cell senescence in skeleton during late puberty. Nat. Commun. 2017;8:1312. doi: 10.1038/s41467-017-01509-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yao Z., Murali B., Ren Q., Luo X., Faget D.V., Cole T., Ricci B., Thotala D., Monahan J., van Deursen J.M., et al. Therapy-induced senescence drives bone loss. Cancer Res. 2020;80:1171–1182. doi: 10.1158/0008-5472.CAN-19-2348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chandra A., Lagnado A.B., Farr J.N., Monroe D.G., Park S., Hachfeld C., Tchkonia T., Kirkland J.L., Khosla S., Passos J.F., et al. Targeted reduction of senescent cell burden alleviates focal radiotherapy-related bone loss. J. Bone Miner. Res. 2020;35:1119–1131. doi: 10.1002/jbmr.3978. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Vatner S.F., Zhang J., Oydanich M., Berkman T., Naftalovich R., Vatner D.E. Healthful aging mediated by inhibition of oxidative stress. Ageing Res. Rev. 2020;64:101194. doi: 10.1016/j.arr.2020.101194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Yang T.L., Shen H., Liu A., Dong S.S., Zhang L., Deng F.Y., Zhao Q., Deng H.W. A road map for understanding molecular and genetic determinants of osteoporosis. Nat. Rev. Endocrinol. 2020;16:91–103. doi: 10.1038/s41574-019-0282-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Farr J.N., Rowsey J.L., Eckhardt B.A., Thicke B.S., Fraser D.G., Tchkonia T., Kirkland J.L., Monroe D.G., Khosla S. Independent roles of estrogen deficiency and cellular senescence in the pathogenesis of osteoporosis: Evidence in young adult mice and older humans. J. Bone Miner. Res. 2019;34:1407–1418. doi: 10.1002/jbmr.3729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hrdlicka H.C., Pereira R.C., Shin B., Yee S.P., Deymier A.C., Lee S.K., Delany A.M. Inhibition of miR-29-3p isoforms via tough decoy suppresses osteoblast function in homeostasis but promotes intermittent parathyroid hormone-induced bone anabolism. Bone. 2021;143:115779. doi: 10.1016/j.bone.2020.115779. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Xiong L., Zhao K., Cao Y., Guo H.H., Pan J.X., Yang X., Ren X., Mei L., Xiong W.C. Linking skeletal muscle aging with osteoporosis by lamin A/C deficiency. PLoS Biol. 2020;18:e3000731. doi: 10.1371/journal.pbio.3000731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Gómez-Puerto M.C., Verhagen L.P., Braat A.K., Lam E.W., Coffer P.J., Lorenowicz M.J. Activation of autophagy by FOXO3 regulates redox homeostasis during osteogenic differentiation. Autophagy. 2016;12:1804–1816. doi: 10.1080/15548627.2016.1203484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lazarus J., Mather K.A., Thalamuthu A., Kwok J.B. Genetic factors and epigenetic mechanisms of longevity: Current perspectives. Epigenomics. 2015;7:1339–1349. doi: 10.2217/epi.15.80. [DOI] [PubMed] [Google Scholar]
- 44.Wang F.S., Lian W.S., Lee M.S., Weng W.T., Huang Y.H., Chen Y.S., Sun Y.C., Wu S.L., Chuang P.C., Ko J.Y. Histone demethylase UTX counteracts glucocorticoid deregulation of osteogenesis by modulating histone-dependent and -independent pathways. J. Mol. Med. 2017;95:499–512. doi: 10.1007/s00109-017-1512-x. [DOI] [PubMed] [Google Scholar]
- 45.Lee B.W.L., Ghode P., Ong D.S.T. Redox regulation of cell state and fate. Redox Biol. 2019;25:101056. doi: 10.1016/j.redox.2018.11.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gao D., Wang S., Lin Y., Sun Z. In vivo AAV delivery of glutathione reductase gene attenuates anti-aging gene klotho deficiency-induced kidney damage. Redox Biol. 2020;37:101692. doi: 10.1016/j.redox.2020.101692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cakouros D., Gronthos S. The changing epigenetic landscape of mesenchymal stem/stromal cells during aging. Bone. 2020;137:115440. doi: 10.1016/j.bone.2020.115440. [DOI] [PubMed] [Google Scholar]
- 48.Jung Y.D., Park S.K., Kang D., Hwang S., Kang M.H., Hong S.W., Moon J.H., Shin J.S., Jin D.H., You D., et al. Epigenetic regulation of miR-29a/miR-30c/DNMT3A axis controls SOD2 and mitochondrial oxidative stress in human mesenchymal stem cells. Redox Biol. 2020;37:101716. doi: 10.1016/j.redox.2020.101716. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data that support the findings of this study are available on request from the corresponding author. The data related to patients’ information are not publicly available due to privacy or ethical restrictions.