Abstract
Objective
Mass gathering events (MGEs) are associated with the transmission of COVID-19. Between 6 and 10 March 2020, several MGEs related to the Falles festival took place in Borriana, a municipality in the province of Castellon (Spain). The aim of this study was to estimate the incidence of COVID-19 and its association with these MGEs, and to quantify the potential risk factors of its occurrence.
Methods
During May and June 2020, a population-based retrospective cohort study was carried out by the Public Health Center of Castelló and the Hospital de la Plana in Vila-real. Participants were obtained from a representative sample of 1663 people with potential exposure at six MGEs. A questionnaire survey was carried out to obtain information about attendance at MGEs and COVID-19 disease. In addition, a serologic survey of antibodies against SARS-Cov-2 was implemented. Inverse probability weighted regression was used in the statistical analysis.
Results
A total of 1338 subjects participated in the questionnaire survey (80.5%), 997 of whom undertook the serologic survey. Five hundred and seventy cases were observed with an attack rate (AR) of 42.6%; average age was 36 years, 62.3% were female, 536 cases were confirmed by laboratory tests, and 514 cases were found with SARS-CoV-2 total antibodies. Considering MGE exposure, AR was 39.2% (496/1264). A dose-response relationship was found between MGE attendance and the disease, (adjusted relative risk [aRR] = 4.11 95% confidence interval [CI]3.25–5.19). Two MGEs with a dinner and dance in the same building had higher risks. Associated risk factors with the incidence were older age, obesity, and upper and middle class versus lower class; current smoking was protective.
Conclusions
The study suggests the significance of MGEs in the COVID-19 transmission that could explain the subsequent outbreak in Borriana.
Introduction
Mass gathering events (MGEs) are important risk factors of severe acute respiratory coronavirus 2 (SARS-CoV-2) transmissions, which causes coronavirus disease 2019 (COVID-19) pandemic [1]. According to the World Health Organization [2] “Mass gatherings are events characterized by the concentration of people at a specific location for a specific purpose over a set period of time that have the potential to strain the planning and response resources of the host country or community”. MGEs cover different types of event and contexts such as public and private celebrations, festivals, religious events and pilgrimages, sporting and touristic events, and political meetings. The crucial role of MGEs in the global propagation of the disease has been evidenced in several countries, including China [3], Iran [4], Malaysia [5], Italy [6], Spain [7], France [8], Germany [9], Jordan [10], Malta [11], Switzerland [12], and Malawi [13]. Significant international efforts have been made to implement specific measures, risk assessment and surveillance, and event cancellations in order to prevent the spread of SARS-CoV-2 from MGEs [14–17]. The propagation of SARS-CoV-3 in these MGEs was measured with the basic reproductive number (Ro), which reflects the efficiency of transmission of the disease [18], and “is defined as the expected number of secondary cases produced by a single (typical) infection in a completely susceptible population” [19]. A meta-analysis of medical literature estimated a Ro = 3.38±1.40 from a range of 1.90–6.49 for the COVID-19 pandemic [20].
MGEs imply the gathering of people in restricted spaces, either indoor or outdoor, over a prolonged period of time, where food and/or drink are generally consumed, usually in close proximity to others, and involving the movement of populations [14, 21–23]. The conditions of MGEs have been associated with the spread of SARS-CoV-2, but few MGE studies [24, 25] have published quantification and adjustment for potential risk factors. In addition, several epidemiologic biases such as selection and misclassification have been observed in some studies of SARS-CoV-2 outbreaks, considering the novelty of the disease and the emergency situation [26].
Spain has had a high incidence of COVID-19 [27, 28], with a large number of COVID-19 outbreaks occurring in households, nursing homes, hospitals, workplaces and leisure facilities [29–33]. We studied a MGE COVID-19 outbreak that took place in the first wave of the pandemic. During March and April 2020 in Borriana, a municipality with 34,683 inhabitants located in the province of Castellon in the Valencian Community (Spain), a COVID-19 outbreak occurred with an incidence of 260 cases (749.6 cases per 100,000 inhabitants) confirmed by reverse-transcriptase polymerase chain reaction (RT-PCR) [34]. Between February and the first days of March 2020, before the COVID-19 outbreak in Borriana, several MGEs took place in connection with the traditional Falles festival, which is held annually in Borriana. Our hypothesis was that the MGEs held during the Falles festival were associated with the COVID-19 outbreak in Borriana.
Using a population-based retrospective cohort study, we aimed to estimate the association of the incidence of COVID-19 disease with the MGEs in Borriana, and quantify potential risk factors of its occurrence.
Material and methods
Description of MGEs during the Falles festival in Borriana
Borriana is a municipality located 5.7 km from the Mediterranean Sea in the province of Castellon, Spain. A series of MGEs took place between March 6 and 10, 2020 during the traditional Falles festival in Borriana. This popular festival is organized by people in the town’s different neighborhoods, clustered in social groups, known as a “falla” (singular) or “falles” (plural), with the purpose of bringing the festivities to the streets. Falles groups consider themselves as a large family. Their final objective is to build a monument with humorous scenes of daily life, which is burned on March 19 [35, 36]. During the 2020 festivities, 19 falles with a total of 2800 members were active in Borriana; each group had between 26 and 384 people and a median of 143 members. The members of the falles comprise around 8.1% of Borriana’s population.
The MGEs analyzed in this study took place in three locations: building A, purposely designed for MGEs with a surface area of 1670 m2 and a capacity of 900 people (three events); theater B (two events and a capacity of 884), and an outdoor square in the city of Valencia. Building A and theater B had air conditioning and ventilation equipment. The MGEs are described below:
First, a pa-i-porta (‘bring your own’ supper) (building A; March 6), a community dinner with an estimated total attendance of approximately 1400 people over a seven hour period (9:30 p.m. to 4:30 a.m.) and dancing after midnight.
Second, the Queen’s gala dinner (building A; March 7), with 400 people gathered together over six and a half hours (10:00 p.m. to 4:30 a.m.) and dancing after midnight. A detailed list of attendees and their distribution in building A was available.
Third, a trip to see fireworks in a square in Valencia (March 8). About 800 people gathered for half an hour (at 2:00 p.m.).
Fourth, a senior citizens’ dance (building A; March 8). Around 100 people attended for one and a half hours (5:30 p.m. to 7:00 p.m.).
Fifth, the theater awards gala (theater B; March 8): indoor show attended by 300 people for two hours (7:00 p.m. to 9:00 p.m.).
Sixth, the Queen’s offering (theater B; March 10): a show attended by 400 people for one and a half hours (10:30 p.m. to 0:00 a.m.).
A summary of the characteristics of these MGEs is presented in Table 1.
Table 1. Characteristics of Mass Gathering Events (MGEs) connected to the Falles festival in Borriana from March 6 to 10.
| MGEs | Location | Date | Hours | People in attendance | Activities |
|---|---|---|---|---|---|
| Pa-i-porta supper | Building A | 3/6/2020 | 7.00 | 14001 | Dinner and dance |
| Queen’s gala dinner | Building A | 3/7/2020 | 6.30 | 400 | Dinner and dance |
| Trip to Valencia | Square outdoor | 3/8/2020 | 0.30 | 800 | Attendance |
| Senior citizen’s dance | Building A | 3/8/2002 | 1.30 | 100 | Dance |
| Theater awards gala | Theater B | 3/8/2020 | 2.00 | 300 | Attendance |
| Queen’s offering | Theater B | 3/10/2020 | 1.30 | 400 | Attendance |
1. Throughout the duration of the MGE.
Design of the study
A population-based retrospective cohort study was carried out from May 14 to June 31, 2020 in Borriana. The study was jointly designed by the Public Health Center of Castellon and the Emergency Service of the Hospital de la Plana (HP) in Vila-real. The study had two phases: 1) a survey with a specific questionnaire to estimate the incidence of COVID-19, and 2) a serologic study of antibodies against SARS-CoV-2 to confirm cases with laboratory tests and to uncover the extent of the infection and the epidemic situation.
Questionnaire survey
In the first phase, starting on May 14, 2020, a standardized questionnaire was administered to obtain information about MGE exposure, demographic characteristics, occupation, habits, health condition, symptoms of the disease, the evolution of COVID-19 disease, previously conducted COVID-19 laboratory tests, and family members affected by COVID-19. The study period covering COVID-19 cases ranged from January 1 to June 31, 2020. The questionnaire was completed through a telephone survey carried out by the health staff of HP, Borriana health centers, and other health centers in the Health Department of La Plana in Vila-real, Castellon. In the telephone survey, parents were requested to ask the questions to their children when a child had been chosen in the simple random sampling. In general, parents were able to answer the questionnaire. Social class was estimated from occupations; children’s social class was that of their parents. Two groups were considered: I and II included professional, managerial and technical occupations (upper and middle class); group III-VI included skilled, non-manual or manual, semi-skilled, and unskilled occupations (lower class).
Participants were recruited from two sources. First, a representative sample of the 19 falles (n = 2800 members) was obtained by simple random sampling with design effect 1 and 19 clusters (one per falla), considering an attack rate of COVID-19 disease of 50% in MGEs, a confidence level of 80%, and an alpha error 5%. The sample comprised 1558 people, which corresponds to 82 people per falla for those with a population larger than 82, or all the members of the falla for those with a population smaller than 82. The Open-Epi program [37] was used to randomly select the participants from a numbered list of all members of each falla until 82 people, including adults and children, were obtained. The phone numbers of each selected participant or their family member were then obtained from the Borriana Falles organization. Second, in order to maximize the number of participants from the Queen’s gala dinner (n = 400), given that the complete list of attendees to the event was available, an additional random sample of 105 people from the list of diners was recruited. The same procedure described above was used to randomly select the 105 people.
Serologic survey and laboratory tests
During the second phase, a serologic survey of anti-SARS-CoV-2 antibody prevalence was carried out from 23 to 27 June 2020 by the Clinical Analysis and Microbiology Service (CAMS) of HP. Qualitative detection of antibodies against SARS-CoV-2 was carried out by an electrochemiluminescence immunoassay (ECLIA) (Elecsys® Anti-SARS-CoV-2, Roche Diagnostics) [38]. IgG and IgM antibodies against SARS-CoV-2 were detected by a lateral flow immunochromatographic assay (LFIC) (Healgen Scientific LLC for COVID-19 IgG/IgM rapid test cassette) [39].
Additionally, information about previously conducted laboratory tests for COVID-19 was gathered during the questionnaire survey. These data consisted of 1) RT-PCR tests, including LightMix® Modular Sarbecovirus E-gene with the LightCycler® 480 II system (Roche, Basel, Switzerland) [40], 2) ECLIA with LFIC, and 3) rapid anti-SARS-CoV-2 antibody tests. These tests were conducted by HP and other public and private laboratories.
Case definitions
A probable COVID-19 case was defined as a patient who presented clinical and epidemiological criteria of COVID-19 disease during the study period, according to the case-definition proposed by the Center for Disease Control and Prevention [41]. Clinical and epidemiological criteria must fulfill two conditions. The first is the reporting of at least two of the following symptoms: fever, chills, rigors, myalgia, headache, sore throat, and new olfactory and taste disorder; or one of the following symptoms: cough, shortness of breath, or difficulty breathing; or severe respiratory illness such as pneumonia or acute respiratory distress syndrome. The second condition is contact with a confirmed COVID-19 patient, or living in an area where a COVID-19 outbreak has been reported.
A confirmed COVID-19 case was defined as a patient who had positive antibodies of SARS-CoV-2 by ECLIA with LFIC, positive PCR, or positive rapid anti-SARS-CoV-2 antibody tests during the study period.
Non-cases (negative cases) were defined as participants who had no COVID-19 clinical criteria or had negative COVID-19 test results during the study period.
Statistical methods
The program Epi-Info® version 7 [42] was used to calculate the sample size. COVID-19 attack rates (AR) were estimated as the quotient between cases and total exposed population, considering different variables. To estimate the risk of the MGEs, COVID-19 cases with onset of symptoms between March 6 and 31, 2020 were included. The pa-i-porta and Queen’s gala dinner MGE events were analyzed in greater detail than the other events, considering the attendance population and the potential risk of COVID-19. Chi2 and Fisher’s exact test were used in the comparisons among variables.
Associations of risk factors with COVID-19 were measured by the relative risk (RR) using Poisson regression and multilevel Poisson regression, considering falles as a level group with a 95% confidence interval (CI). In order to adjust for potential confounding factors, the directed acyclic graphs (DAGs) method [43] was used with the DAGitty® program (version 3.0) [44], together with inverse probability weighted regression [45] to obtain adjusted AR (aAR) and RR (aRR). The DAG provides a picture of the relationship between an exposure (mass gathering event) and an outcome (COVID-19 disease) and factors that could be potential confounders. An adjustment was made for these factors. The factors were age, sex, social class (upper and middle class versus lower class), chronic illness, family COVID-19 case and falla (social group); all these factors could alter the relationship between exposure and outcome. In addition, a sensitivity analysis was carried out including participants who were tested for COVID-19 disease, to gain more specificity of the results. The Stata ® program (version 14) [46] was used in the calculation.
Ethical aspects
The study was approved by the director of the Public Health Center of Castellon and the management of the Health Department of La Plana, taking into account the situation of the COVID-19 pandemic in the province of Castellon. Participation was voluntary, and after an explanation of the study objective, oral informed consent was obtained from all participants (or their parents, in the case of minors) included in the study. To ensure explicit consent, several clarifications were made before administering the survey questionnaire, including voluntary participation, the option to withdraw from the study without prejudice, the opportunity to receive information about the study, a guarantee that personal information would be kept in the strictest confidentiality and that privacy would be safeguarded as the data collected would be used anonymously for scientific research; the researcher responsible for data collection was identified. When a child was selected in the sampling process, permission to participate was requested from their parents, who would also help them to answer the questionnaire; all the above clarifications were also made before the survey questionnaire was administered.
Results
Description of participants in the questionnaire survey
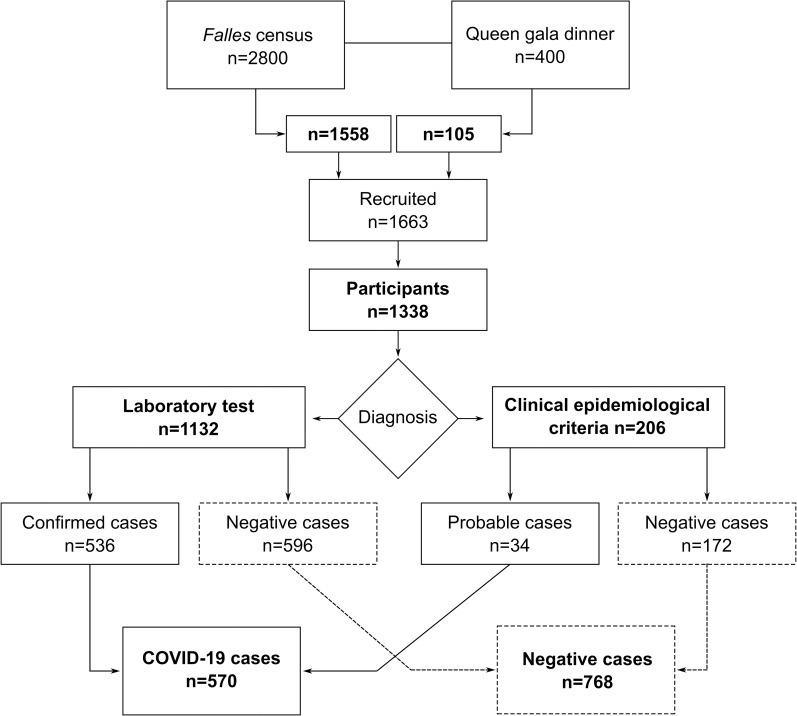
Participation rates in the questionnaire survey were 80.5% (1338/1663) (Fig 1). Participation was higher among females than males (58.9% versus 41.1%). The mean age was 33.9 ± 17.8 years (rank of 1–80 years) (Table 2). The most represented age groups were 45–64 years (28.2%) and 15–24 years (20.1%), and the least represented groups were 1–4 years (2.3%) and 65 years and above (3.4%) (Table 2). The occupation III-VI group (lower class) was higher than the I-II group (upper and middle classes) (74.3% versus 25.7%) (Table 2). Chronic illness was present in 30.9% of participants. The pa-i-porta event was the most highly attended MGE (60.5%), followed by the Queen’s gala dinner (24.8%). The theater award gala (12.4%) and the senior citizens’ dance (2.8%) had the lowest attendances (Table 2). A total of 397 participants in the questionnaire survey (25.3%) did not attend any MGEs.
Fig 1. Flow diagram of the study population in the MGEs in Borriana between January and June 2020.
COVID-19 cases included those diagnosed by laboratory tests (confirmed cases) or by clinical and epidemiological criteria (probable cases). Cases confirmed by laboratory tests included participants with positive results from the serologic survey as well as from private and public medical laboratories.
Table 2. Characterization of the participants included in the study of Mass Gathering Events (MGEs) from January 1 to June 31, 2020, Borriana.
| Variable | Participants (n) | Participants1 (%) | COVID-19 tests (n) | COVID-19 tests (%) |
|---|---|---|---|---|
| Total participants | 1338 | - | 1132 | 84.61 |
| Female | 788 | 58.9 | 680 | 60.1 |
| Male | 550 | 41.1 | 452 | 39.9 |
| Mean age ± SD2 | 33.9 ± 17.8 | - | 36.9 ± 17.1 | - |
| Age (years) | ||||
| 0–4 | 31 | 2.3 | 20 | 1.8 |
| 5–14 | 190 | 14.2 | 137 | 12.1 |
| 15–24 | 269 | 20.1 | 217 | 19.2 |
| 25–34 | 185 | 13.8 | 157 | 13.9 |
| 35–44 | 241 | 18.0 | 213 | 18.8 |
| 45–64 | 377 | 28.2 | 349 | 30.8 |
| 65 and above | 45 | 3.4 | 39 | 3.4 |
| Social class3,4 | ||||
| Occupation I-II | 339 | 25.7 | 283 | 25.0 |
| Occupation III-VI | 978 | 74.3 | 840 | 74.2 |
| Chronic illness5 | ||||
| Yes | 411 | 30.9 | 364 | 32.2 |
| No | 920 | 69.1 | 763 | 67.4 |
| MGE total attendees | ||||
| Pa-i-porta (n = 1400) | 809 (57.8%) | 60.5 | 740 | 65.4 |
| Queen’s gala dinner (n = 400) | 332 (83.0%) | 24.8 | 317 | 28.0 |
| Valencia trip (n = 800) | 211 (26.4%) | 15.8 | 190 | 16.8 |
| Queen’s offering (n = 400) | 239 (59.8%) | 17.9 | 230 | 20.3 |
| Senior citizens’ dance (n = 100) | 38 (38.0%) | 2.8 | 38 | 3.4 |
| Theater awards gala (n = 300) | 166 (55.3%) | 12.4 | 151 | 13.3 |
| No attendance | 397 | 25.3 | 274 | 24.2 |
1. Of total participants.
2. Standard deviation.
3. Occupation group I and II: Professional, managerial and technical occupations (upper and middle class); Group III-VI: Skilled, non-manual or manual; semi-skilled; unskilled occupations (lower class).
4. Missing answer from 21 participants.
5. Missing answer from 7 participants.
Description of participants in the serologic survey and COVID-19 laboratory tests
A total of 1132 participants (84.6%) underwent laboratory tests for COVID-19 disease (Table 2), considering both the tests carried out as part of the serologic survey (n = 997) and those from private and public medical laboratories (n = 135) (Fig 1, see Methods for further information). Participation rates in the serologic survey were 74.5% (997/1338). Female participation in laboratory tests for COVID-19 (including both the serologic survey and medical records) was higher (60.1%) than that of males (39.9%). The mean age of participants that underwent a COVID-19 laboratory test was 36.9 ± 17.1 years. The 45–64 years and 15–24 years age groups were the most highly represented (30.8% and 19.2%, respectively), while 0–4 years (1.8%) and 65 years and above (3.4%) were the least represented (Table 2). Participation of the occupation III-VI group (lower class) was higher than in the I-II group (upper and middle class) (74.2% versus 25.0%) (Table 2). A total of 32.2% of the participants reported suffering from a chronic illness (Table 2). MGE attendance among participants with COVID-19 laboratory tests showed the pa-i-porta event as the most highly attended event (65.4%), again followed by the Queen’s gala dinner (28.9%), while the theater award gala (13.3%) and the senior citizens’ dance (3.4%) had the lowest attendance (Table 2). A total of 274 participants (24.1%) with COVID-19 laboratory tests did not attend any MGEs (Table 2).
Description of COVID-19 outbreak
During the study period, 570 COVID-19 cases were found (Fig 1, Table 2). Among these, 536 (94.0%) were confirmed cases with positive COVID-19 laboratory tests and 34 (6.0%) were probable cases as diagnosed according to clinical and epidemiological criteria (Fig 1). Specifically, confirmed cases included 514 participants (90.2%) with positive total anti-SARS-CoV-2 antibodies (32 of whom also reported a positive PCR test), seven participants (1.2%) with positive PCR only (a total of 39 participants had a positive PCR, 6.8%), and 15 participants (2.6%) with positive rapid anti-SARS-CoV-2 antibody tests. From the subset of 997 participants in the serologic survey, 508 were positive for anti-SARS-CoV-2 IgG antibodies, and eight participants were also positive for anti-SARS-CoV-2 IgM antibodies. AR was 42.6% (570/1338) among total participants, 47.3% (536/1132) among participants undergoing laboratory tests, and 16.5% (34/206) among those classified according to clinical and epidemiological criteria (Fig 1).
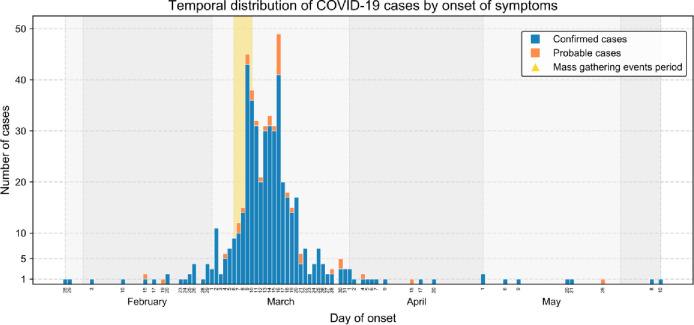
The temporal distribution of confirmed and probable COVID-19 cases is shown by onset of symptoms (Fig 2). The first cases were reported on 28 and 29 January 2020. The incidence then slowly progressed during February with a small peak of cases on March 2. Two maximum peaks of cases occurred on March 9 (45 cases) and March 16 (49 cases). After April, only isolated cases were reported, which is consistent with the general lockdown in Spain that was implemented on March 15. According to these observations, the distribution of COVID-19 cases in this study showed a bimodal epidemic curve with two maxima. Interestingly, the aforementioned peaks took place between 3 and 10 days after the MGEs (see Methods for further information). This indicates several point sources of the outbreak, with the pa-i-porta and Queen’s gala dinner events being the first ones on March 6 and 7, respectively.
Fig 2. Temporal distribution of COVID-19 cases by onset of symptoms.
The numbers of confirmed and probable COVID-19 cases are shown in blue and orange, respectively. The yellow vertical line highlights the time period when the six MGEs took place (March 6–10, 2020).
Epidemiological characterization of COVID-19 cases
Regarding the sex of total cases, 355 (62.3%) were female and 215 (37.7%) were male (Table 3). The AR for males (39.1%) was smaller than for females (45.1%) (RR = 0.87, 95% CI 0.73–1.03) (Table 2). Similarly, COVID-19 incidence was lower in males than in females for both confirmed (44.9% versus 49.0%) and probable cases (12.2% versus 20.4%), although differences in AR were not significant.
Table 3. Characteristics of patients of COVID-19.
From January 1 to June 31, 2020, Borriana.
| Variables | Cases | Non-cases | Total | AR1 (%) | RR (95% IC)2 | p-value |
|---|---|---|---|---|---|---|
| Total cases | 570 | 768 | 1338 | 42.6 | - | - |
| PCR positive | 39 | 1299 | 1338 | 2.9 | - | - |
| Hospitalizations | 13 | 1325 | 1338 | 1.0 | - | - |
| Deaths | 1 | 1337 | 1338 | 0.07 | - | ´- |
| Sex | ||||||
| Male | 215 | 335 | 550 | 39.1 | 0.87(0.73–1.03) | 0.110 |
| Female | 355 | 433 | 788 | 45.1 | 1.00 | |
| Age mean ± SD3 | 36.4±17.1 32.0±18.0 | 1.01 (1.00–1.01) | 0.001 | |||
| Age groups (years) | ||||||
| 0–4 | 8 | 23 | 31 | 25.8 | 1.00 | |
| 5–14 | 58 | 133 | 190 | 30.5 | 1.11(0.56–2.44) | 0.685 |
| 15–24 | 110 | 159 | 269 | 41.1 | 1.54(0.75–3.17) | 0.243 |
| 25–34 | 72 | 113 | 185 | 38.9 | 1.48(0.71–3.08) | 0.293 |
| 35–44 | 114 | 127 | 241 | 47.3 | 1.80(0.88–3.68) | 0.110 |
| 45–64 | 189 | 188 | 377 | 50.1 | 1.92(0.94–3.90) | 0.073 |
| 65 and above | 19 | 26 | 45 | 42.2 | 1.56(0.68–3.57) | 0.297 |
| Confirmed cases | ||||||
| Male | 203 | 249 | 452 | 44.9 | 0.91(0.77–1.09) | 0.322 |
| Female | 333 | 347 | 680 | 49.0 | 1.00 | |
| Probable cases | ||||||
| Male | 12 | 86 | 98 | 12.2 | 0.63(0.30–1.28) | 0.200 |
| Female | 22 | 86 | 108 | 20.4 | 1.00 | |
| Asymptomatic | ||||||
| Male | 30 | 520 | 550 | 5.5 | 1.17(0.72–1.90) | 0.519 |
| Female | 37 | 751 | 788 | 4.7 | 1.00 | |
| Family with COVID-194 Yes | 347 | 254 | 601 | 57.7 | 1.91(1.59–2.23) | <0.001 |
| No | 221 | 506 | 727 | 30.4 | 1.00 | |
| Medical assistance Yes | 247 | 94 | 341 | 72.4 | 2.22(1.88–2.62) | <0.001 |
| No | 323 | 674 | 997 | 32.1 | 1.00 | |
| Chronic illness5 Yes | 189 | 222 | 411 | 46.0 | 1.13(0.95–1.35) | 0.183 |
| No | 375 | 545 | 920 | 40.8 | 1.00 | |
| Diabetes Mellitus6 Yes | 10 | 18 | 28 | 35.7 | 0.84(0.45–1.56) | 0.574 |
| No | 552 | 743 | 1295 | 42.6 | 1.00 | |
| Cardiovascular diseases6Yes | 69 | 66 | 135 | 51.1 | 1.23(0.95–1.58) | 0.114 |
| No | 493 | 695 | 1188 | 41.5 | 1.00 | |
| Hypertension6 Yes | 47 | 51 | 98 | 48.0 | 1.14(0.84–1.54) | 0.393 |
| No | 514 | 711 | 1225 | 42.0 | 1.00 | |
| Hypothyroidism7 Yes | 28 | 22 | 50 | 56.0 | 1.32(0.90–1.94) | 0.150 |
| No | 534 | 740 | 1274 | 41.9 | 1.00 | |
| Digestive diseases6 Yes | 16 | 15 | 31 | 51.6 | 1.21(0.74–2.00) | 0.450 |
| No | 545 | 747 | 1292 | 42.2 | 1.00 | |
| Asthma7 Yes | 11 | 27 | 38 | 29.0 | 0.66(0.36–1.20) | 0.174 |
| No | 551 | 735 | 1286 | 42.8 | 1.00 | |
| Allergic Rhinitis7 Yes | 27 | 31 | 58 | 46.6 | 1.11(0.75–1.62) | 0.613 |
| No | 535 | 731 | 1266 | 42.3 | 1.00 | |
1. AR = attack rate.
2. Adjusted for falla.
3. SD = Standard deviation.
4. Missing answers from 10 participants.
5. Missing answers from 7 participants.
6. Missing answers from 15 participants.
7. Missing answers from 14 participants.
Regarding age, cases were older than non-cases (36.4 ± 17.1 years versus 32.0 ± 18.0 years; p<0.001) (Table 3). When split by age groups, the highest ARs were found in the 55–64 years group (50.1%) and the 35–44 years group (47.3%), whereas the lowest ARs were observed in the 0–4 years group (25.8%) and 5–14 years group (30.5%) (Table 3), but no significant differences were observed among age groups when models were adjusted for falla.
Regarding the clinical presentation of the disease, a total of 503 cases (88.2%), including 469 confirmed cases and 34 probable cases, showed COVID-19 illness. The signs and symptoms reported by COVID-19 patients included weakness (56.3%), fever (55.1%), loss of smell and/or taste (53.8%), myalgia (51.3%), headache (46.2%) cough (49.0%), sore throat (35.7%), coryza (31.8%), diarrhea (26.6%), dermatologic lesions (12.1%), vomiting (5.7%) dyspnea (4.6%) and pneumonia (2.4%). The average disease duration was 16.1 ± 20.9 days, with a median of 7.0 days (rank 1–100). Long-term symptoms or aftermaths of COVID-19 were reported in 6.6% of cases. Of note, 247 cases (43.4%) sought medical assistance and 13 cases (2.3%) required hospitalization due to COVID-19. Only one death attributable to COVID-19 was reported during the period of the study. On the other hand, asymptomatic cases made up 12.5% of all confirmed cases (67/536), with an average age of 25.2 ± 17.6 years. No differences in the number of asymptomatic cases were found between males and females. Among total cases, 33.5% reported having a chronic disease, the most frequent of which were cardiovascular disease, hypertension, allergic rhinitis, and hypothyroidism (Table 3). No significant associations with COVID-19 incidence were found in any of the analyzed diseases. Finally, the effect of having a family member with COVID-19 at the time of disease onset was analyzed. AR among those participants who reported having a COVID-19 positive family member was 57.7% (347/601). In contrast, AR among participants who did not report a COVID-19 positive family member was 30.4% (221/727). Therefore, having a family member with COVID-19 increased the risk of COVID-19 incidence (RR = 1.91, 95% CI 1.59–2.23) (Table 3).
Analysis of COVID-19 outbreak and MGEs
General analysis of MGEs
Considering the dates of the MGEs (6 and 10 March 2020) and the temporal distribution of COVID-19 cases in the study (Fig 2), the analysis focused further on COVID-19 cases attributable to the MGEs associated with the Falles in Borriana. The 74 cases that presented the onset of symptoms or a positive test obtained before March 6 or after March 31 were therefore excluded since their illness onset (before the MGEs or more than three weeks after the last MGE) could not be related to the studied MGEs. Consequently, 1264 participants were included in the analysis with 496 cases, and AR of 39.2% (496/1264). DAGs were used to study MGEs (exposure) and COVID-19 disease (outcome) and potential confounding factors (Fig 3). Raw AR and adjusted (aAR), as well as RR and aRR, of MGEs are presented in Table 4. The aRR of males and females did not differ significantly. The aRR increased with age, from 0–4 years (aAR = 17.0%) to 35–44 years, which presented the highest values (aAR = 46.9%) (aRR = 2.77 95% CI 1.30–5.88). The age groups of 45–64 years and 65 years and above also presented high values (aAR = 44.2%) (aRR = 2.60 95% CI 1.22–5.52) and (aAR = 39.2%) (aRR = 2.31 95% CI 1.07–4.99), respectively. In addition, COVID-19 disease was associated with occupations I-II (upper and middle class) (aRR = 1.22 95% CI 1.06–1.40).
Fig 3. Directed Acyclic Graphs (DAG) of mass gathering events (exposure) effect on COVID-19 disease (outcome).
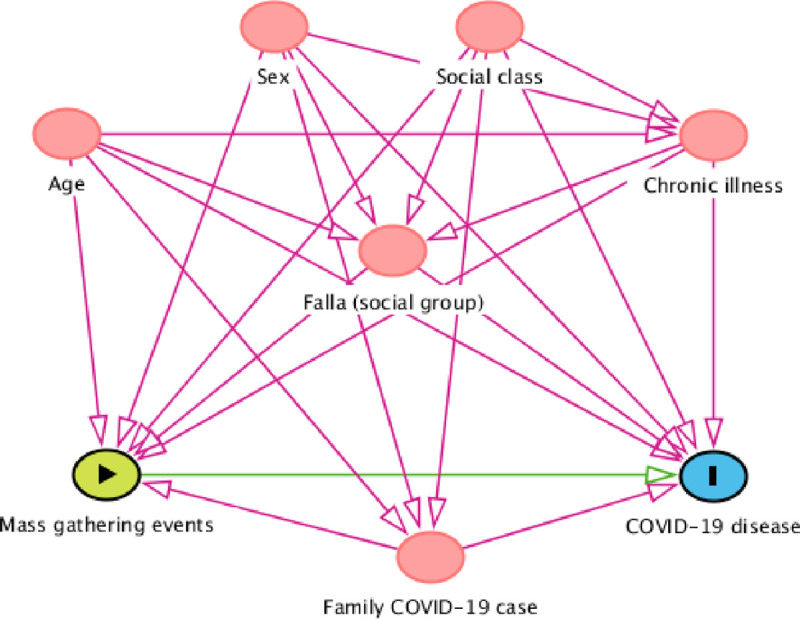
Ancestors of exposure and outcome (in red). Based on DAGitty version 3.0.
Table 4. Mass Gathering Event (MGE) attendance, Attack Rate (AR), adjusted AR (aAR), Relative Risk (RR), and adjusted (aRR).
Confidence interval (CI). From March 6 to 31, 2020, Borriana.
| Variables | Cases | Non-cases | AR (%) | RR (95% IC) | aAR1 (%) | aRR (95% IC)1 | p-value |
|---|---|---|---|---|---|---|---|
| Male | 189 | 335 | 36.1 | 0.87(0.73–1.04) | 39.2 | 0.98(0.86–1.16) | 0.785 |
| Female | 307 | 433 | 41.5 | 1.00 | 39.9 | 1.00 | |
| Age 0–4 (years)2 | 6 | 23 | 20.7 | 1.00 | 17.0 | ||
| 5–14 | 49 | 132 | 27.1 | 1.31(0.56–3.05) | 25.6 | 1.51(0.69–3.31) | 0.305 |
| 15–24 | 93 | 159 | 36.7 | 1.77(0.78–4.05) | 35.9 | 2.12(0.99–4.54) | 0.054 |
| 25–34 | 64 | 113 | 36.2 | 1.74(0.76–4.04) | 38.1 | 2.25(1.04–4.83) | 0.039 |
| 35–44 | 106 | 127 | 45.5 | 2.20(0.97–5.00) | 46.9 | 2.77(1.30–5.88) | 0.008 |
| 45–64 | 161 | 188 | 46.1 | 2.23(0.99–5.04) | 44.2 | 2.60(1.22–5.52) | 0.013 |
| 65 and above | 18 | 26 | 40.9 | 1.97(0.78–4.98) | 39.2 | 2.31(1.07–4.99) | 0.032 |
| Occupation I-II1 | 153 | 166 | 48.0 | 1.30(1.08–1.58) | 45.7 | 1.22(1.06–1.40) | 0.005 |
| Occupation III-VI | 340 | 585 | 36.8 | 1.00 | 37.6 | 1.00 | |
| Chronic illness1 Yes | 162 | 222 | 42.3 | 1.12(0.93–1.36) | 39.7 | 1.01(0.88–1.17) | 0.882 |
| No | 328 | 545 | 37.6 | 1.00 | 39.3 | 1.00 | |
| Family with COVID-19 Yes | 305 | 254 | 54.6 | 2.01 (1.67–2.41) | 51.3 | 1.71(1.49–1.97) | <0.001 |
| No | 189 | 506 | 27.2 | 29.9 | 1.00 | ||
| Body Mass Index1,3 | 12 | 31 | 27.9 | 1.00 | 17.5 | 1.00 | |
| <18.5 Kg/m2 | |||||||
| 18.5–24.9 Kg/m2 | 203 | 327 | 38.3 | 1.32(0.96–1.80) | 41.5 | 2.37(0.96–5.85) | 0.062 |
| 25.0–29.9 Kg/m2 | 143 | 177 | 44.7 | 1.57(1.13–2.17) | 45.2 | 2.58(1.04–6.40) | 0.040 |
| ≥30.0 Kg/m2 | 81 | 74 | 52.3 | 1.68(1.18–2.40) | 56.3 | 3.21(1.29–7.98) | 0.012 |
| Physical exercise1 3 Yes | 258 | 401 | 39.2 | 0.89(0.74–1.06) | 40.1 | 0.88(0.77–1.01) | 0.077 |
| No | 183 | 211 | 46.5 | 1.00 | 45.3 | 1.00 | |
| Drink alcohol 1 3 Yes | 109 | 138 | 44.1 | 1.13(0.91–1.40) | 46.9 | 1.14(0.99–1.32) | 0.065 |
| No | 332 | 473 | 41.2 | 1.00 | 40.9 | 1.00 | |
| Current smoker1 3 | 75 | 197 | 27.6 | 0.66(0.51–0.85) | 28.7 | 0.63(0.52–0.78) | <0.001 |
| Ex smoker1 3 | 108 | 100 | 51.9 | 1.25 (1.00–1.59) | 50.8 | 1.13 (0.97–1.31) | 0.122 |
| Never smoker1 3 | 256 | 311 | 45.9 | 1.00 | 45.0 | 1.00 | |
| Pa-i-porta2 Yes | 386 | 367 | 51.3 | 2.38(1.93–2.94) | 49.9 | 2.15(1.80–2.56) | <0.001 |
| No | 110 | 401 | 21.5 | 1.00 | 23.4 | 1.00 | |
| Queen’s gala dinner2 Yes | 198 | 110 | 64.3 | 2.06(1.72–2.47) | 61.9 | 1.90(1.67–2.17) | <0.001 |
| No | 298 | 658 | 31.2 | 1.00 | 32.5 | 1.00 | |
| Valencia trip2 Yes | 92 | 105 | 46.7 | 1.23(0.98–1.55) | 47.9 | 1.25(1.06–1.46) | 0.007 |
| No | 404 | 663 | 37.9 | 1.00 | 38.5 | 1.00 | |
| Queen’s offering2 Yes | 139 | 74 | 65.3 | 1.92(1.58–2.34) | 62.0 | 1.77(1.54–2.04) | <0.001 |
| No | 357 | 694 | 34.0 | 1.00 | 35.0 | 1.00 | |
| Senior citizens’ dance2 Yes | 23 | 8 | 74.2 | 1.93(1.27–2.94) | 57.3 | 1.48(1.14–1.93) | 0.004 |
| No | 473 | 760 | 38.4 | 1.00 | 38.8 | 1.00 | |
| Theater awards2 Yes | 89 | 69 | 56.3 | 1.53(1.21–1.93) | 54.1 | 1.44(1.22–1.70) | <0.001 |
| No | 407 | 699 | 36.8 | 1.00 | 37.6 | 1.00 | |
| 5 MGEs attended2 | 6 | 1 | 85.7 | 4.97(2.16–11.47) | 77.7 | 4.11(3.25–5.19) | <0.001 |
| 4 MGEs attended2 | 52 | 18 | 74.3 | 4.31(3.00–6.20) | 75.9 | 4.01(3.08–5.23) | <0.001 |
| 3 MGEs attended2 | 95 | 53 | 64.2 | 3.72(2.72–5.10) | 61.2 | 3.24(2.49–4.21) | <0.001 |
| 2 MGEs attended2 | 125 | 116 | 51.9 | 3.01(2.23–4.06) | 49.4 | 2.61(2.02–3.39) | <0.001 |
| 1 MGE attended2 | 152 | 263 | 36.6 | 2.13(1.59–2.84) | 36.5 | 1.93(1.49–2.49) | <0.001 |
| 0 MGEs attended2 | 66 | 317 | 17.2 | 1.00 | 18.9 | 1.00 |
1. Adjusted for age, sex, chronic illness, social class, family COVID-19 case, falla, and MGEs attended.
2. Adjusted for all factors except MGEs.
3. Age 15 years and above.
Those who had a family member with COVID-19 had a higher risk of SARS-CoV-2 infection (aRR = 1.71 95% CI 1.49–1.97). Additionally, the risk of contracting COVID-19 increased with higher body mass index (BMI), up to the group of 30 Kg/m2 or higher (aRR = 3.21 95% CI 1.29–7.98), and marginally with habitual alcoholic beverage consumption (aRR = 1.14 95% CI 0.99–1.32). Chronic illness and physical exercise were not associated with contracting COVID-19. On the other hand, the current smoker group presented lower risk (aRR = 0.63 95% CI 0.52–0.78). Regarding MGEs, the aAR ranged from 62.0% (the Queen’s offering) to 47.9% (the Valencia trip). The disease was associated with the pa-i-porta event with an aRR of 2.15 (95% CI 1.80–2.56), followed by the Queen’s gala dinner with aRR of 1.90 (95% CI 1.67–2.17). The other MGEs had lower aRR, but still presented a significant and considerable risk (Table 4). When MGE exposure was measured by the number of events the participants had attended, a dose-response relationship was found with raw and adjusted AR. The aAR for participants who attended no MGEs was 18.9%, increasing to 77.7% for participants who attended five MGEs (aRR = 4.11 95% CI 3.25–5.19).
Analysis of the pa-i-porta event
The analysis of the MGE with the highest number of participants, the pa-i-porta, together with different exposure variables, is shown in Table 5.
Table 5. Pa-i-porta, Mass Gathering Event (MGE) attendance, Attack Rate (AR), adjusted AR (aAR), Relative Risk (RR), and adjusted (aRR).
Confidence interval (CI). From March 6 to 31, 2020, Borriana.
| Variables | Cases | Non- cases | AR (%) | RR (95% IC) | aAR (%) | aRR(95% IC)1 | p-value |
|---|---|---|---|---|---|---|---|
| Total | 386 | 367 | 51.3 | ||||
| Male | 143 | 132 | 52.0 | 1.02(0.83–1.26) | 49.3 | 0.96(0.83–1.11) | 0.407 |
| Female | 243 | 235 | 50.8 | 1.00 | 51.5 | ||
| Attendance time2 | |||||||
| Less than half | 32 | 37 | 46.4 | 1.00 | 44.2 | 1.0 | |
| Half | 111 | 143 | 43.7 | 0.94(0.64–1.40) | 44.5 | 1.01(0.75–1.35) | 0.956 |
| More than half | 104 | 86 | 54.7 | 1.18(0.80–1.75) | 53.6 | 1.21(0.91–1.62) | 0.189 |
| All the time | 138 | 100 | 58.0 | 1.25(0.85–1.84) | 58.4 | 1.32(0.98–1.74) | 0.051 |
| Dinner2 | |||||||
| Ate own food | 67 | 63 | 51.5 | 0.97(0.74–1.27) | 55.5 | 1.07(0.88–1.29) | 0.505 |
| Ate falla food | 268 | 238 | 53.0 | 1.00 | 52.0 | 1.00 | |
| Ate other food2 | |||||||
| Yes | 110 | 92 | 54.5 | 1.08(0.86–1.36) | 51.0 | 1.00(0.85–1.18) | 0.839 |
| No | 225 | 222 | 50.3 | 1.00 | 50.8 | 1.00 | |
| Cake consumption2 | |||||||
| Yes | 218 | 182 | 54.5 | 1.14 (0.99–1.43) | 53.2 | 1.10(0.94–1.28) | 0.236 |
| No | 120 | 132 | 47.6 | 1.00 | 48.7 | 1.00 | |
| Drank alcohol beverages at this event2 3 | |||||||
| Yes | 251 | 217 | 53.6 | 0.95(0.74–1.21) | 54.0 | 0.98(0.83–1.16) | 0.913 |
| No | 87 | 67 | 56.5 | 1.00 | 54.9 | 1.00 | |
| Attendance2 | |||||||
| Only dance | 43 | 58 | 42.6 | 0.81(0.59–1.11) | 44.2 | 0.84 (0.67–1.06) | 0.137 |
| All event | 332 | 300 | 52.5 | 1.00 | 52.5 | 1.00 | |
| Dance2 | |||||||
| Not at all | 94 | 93 | 51.3 | 1.00 | 47.6 | 1.00 | |
| A little | 104 | 100 | 51.0 | 1.01(0.77–1.34) | 48.5 | 1.04(0.84–1.29) | 0.708 |
| Some of the time | 103 | 97 | 51.5 | 1.02(0.77–1.35) | 53.2 | 1.12(0.91–1.38) | 0.292 |
| A lot | 82 | 71 | 53.6 | 1.06(0.79–1.43) | 56.8 | 1.19(0.96–1.48) | 0.120 |
| Dinner table with a COVID-19 symptomatic case4 | |||||||
| Yes | 338 | 311 | 52.4 | 1.18(0.86–1.62) | 55.7 | 2.19(1.40–3.42) | 0.001 |
| No | 44 | 56 | 44.0 | 1.00 | 25.5 | ||
| Quadrant of building A5 | |||||||
| Upper left | 130 | 118 | 52.1 | 1.36 (1.01–1.84) | 47.0 | 1.10 (0.79–1.52) | 0.570 |
| Lower left | 118 | 113 | 51.1 | 1.32 (0.98–1.81) | 51.7 | 1.18 (0.82–1.16) | 0.309 |
| Upper right | 71 | 35 | 67.0 | 1.74 (1.24–2.45) | 67.7 | 1.44 (1.12–1.85) | 0.005 |
| Lower right | 63 | 101 | 38.4 | 1.00 | 40.0 | 1.00 | |
1. Adjusted for age, sex, chronic illness, social class, family COVID-19 case, and falla.
2. Missing information of two cases.
3. Age 15 years and above.
4. Adjusted age, sex, mean of attendance time, and mean MGEs attended.
5. Adjusted for median of MGEs attended.
The aRR by sex was similar in females and males. Interestingly, COVID-19 disease was marginally associated with the total time attended in a dose-response relationship from less than half of the event up to the whole event (aRR = 1.32 95% CI 0.98–1.74). The food or alcoholic beverages provided by the event organizers, or those brought to the event by the participants (which included cakes or other foods) were not associated with the disease. Participants who did not participate in the dinner and only attended the dance had a lower risk, but with limited effect (aRR = 0.84 95% CI 0.67–1.16). In addition, more time spent dancing was a marginal risk factor (aRR = 1.19 95% CI 0.96–1.48). Two groups of participants were defined according to whether or not they shared a dinner table with a participant reporting onset of COVID-19 symptoms between February 26 and March 6. The exposed group presented a higher aAR of disease than those who were not exposed, 55.7% versus 25.5% (aRR = 2.19 95% CI 1.40–3.42). Finally, the location and distribution of the dinner tables in building A were analyzed. To this end, the dinner tables were classified into four quadrants and an adjusted analysis was carried out. Results showed that the upper right quadrant had a higher COVID-19 incidence than the lower right quadrant (aRR = 1.44 95% 1.12–1.85), but no difference was found with the other quadrants (Table 5).
Analysis of the Queen’s gala dinner event
The Queen’s gala dinner was the MGE with the second highest number of participants in the study (Table 6). The aRR by sex was similar in females and males. The time of attendance at this event presented a dose-response relationship from less than half attendance to whole event attendance (aRR = 1.76 95% CI 1.18–2.62). At dinner, several dishes were consumed: starters (tomato bread, pork sausages, cheese and foie gras salad and scallops), second course (sirloin), and dessert (chocolate cream). The consumption of these foods and alcoholic beverages was not associated with COVID-19 risk. Next, two groups of participants were defined according to whether or not they shared a dining table with a participant with COVID-19 disease and symptoms onset between February 27 and March 7. The exposed group showed a higher aAR than the non-exposed group (76.1% and 58.6%, respectively) (aRR = 1.30 95%1.10–1.53). The adjusted analysis of the incidence of COVID-19 cases across the four quadrants of tables in building A (same building as for the pa-i-porta event), revealed that the lower left quadrant had the highest COVID-19 incidence and differed from that of the lower right quadrant, which was the one with the lowest incidence (aRR = 1.29 95% 1.00–1.65). No differences were found with the other table quadrants (Table 6). Interestingly, the lower right quadrant was the one with the lowest COVID-19 incidence in both the pa-i-porta and the Queen’s gala dinner events.
Table 6. Queen’s gala dinner, Mass Gathering Event (MGE) attendance, Attack Rate (AR), adjusted AR (aAR), Relative Risk (RR), and adjusted (aRR).
Confidence interval (CI). From March 6 to 31, 2020, Borriana.
| Variable | Cases | Non-cases | AR (%) | RR (95% IC) | aAR (%) | aRR(95% IC)1 | p-value |
|---|---|---|---|---|---|---|---|
| Total | 198 | 110 | 64.3 | ||||
| Male | 75 | 44 | 63.0 | 0.97(0.72–1.29) | 62.1 | 0.96(0.80–1.15) | 0.653 |
| Female | 123 | 66 | 65.1 | 1.00 | 64.7 | 1.00 | |
| Attendance time | |||||||
| Less than half | 11 | 13 | 45.8 | 1.00 | 39.8 | 1.00 | |
| Half | 31 | 16 | 66.0 | 1.44 (0.78–2.88) | 65.3 | 1.64(1.05–2.55) | 0.028 |
| More than half | 42 | 31 | 57.5 | 1.26(0.64–2.44) | 56.3 | 1.42(0.91–2.20) | 0.121 |
| All time | 114 | 50 | 69.5 | 1.52(0,82.2.82) | 70.2 | 1.76(1.18–2.62) | 0.005 |
| Dinner | |||||||
| Tomato bread Yes | 185 | 101 | 64.7 | 0.94(0.51–1.73) | 65.0 | 1.14(0.89–1.46) | 0.312 |
| No | 11 | 5 | 68.8 | 1.00 | 57.1 | 1.00 | |
| Pork sausages Yes | 182 | 99 | 64.8 | 0.97(0.56–1.67) | 64.7 | 0.88(0.71–1.09) | 0.249 |
| No | 14 | 7 | 66.7 | 73.6 | 1.00 | ||
| Foie salad Yes | 163 | 93 | 63.7 | 0.89(0.61–1.29) | 63.9 | 0.82(0.68–0.97) | 0.022 |
| No | 33 | 13 | 71.7 | 78.4 | 1.00 | ||
| Scallops Yes | 158 | 86 | 64.8 | 0.99(0.69–1.41) | 65.3 | 0.96(0.79–1.17) | 0.673 |
| No | 38 | 20 | 63.8 | 68.1 | 1.00 | ||
| Sirloin Yes | 173 | 96 | 64.3 | 0.92(0.60–1.43) | 65.0 | 0.77(0.67–0.89) | <0.001 |
| No | 23 | 10 | 69.7 | 1.00 | 84.4 | 1.00 | |
| Chocolate Yes | 165 | 82 | 66.8 | 1.19(0.81–1.74) | 67.5 | 1.13(0.91–1.40) | 0.263 |
| No | 31 | 24 | 54.5 | 59.8 | 1.00 | ||
| Drank alcohol 2 Yes | 163 | 94 | 63.4 | 0.93(0.65–1.35) | 63.6 | 1.20(0.95–1.52) | 0.123 |
| No | 34 | 14 | 70.8 | 52.8 | 1.00 | ||
| Dinner table with a COVID-19 symptomatic case3 | |||||||
| Yes | 88 | 35 | 71.5 | 1.18(0.89–1.57) | 76.1 | 1.30(1.10–1.53) | 0.002 |
| No | 103 | 67 | 60.6 | 1.00 | 58.6 | 1.00 | |
| Quadrant of building A4 | |||||||
| Upper left | 44 | 18 | 71.0 | 1.27 (0.84–1.91) | 63.4 | 0.98(0.72–1.34) | 0.917 |
| Lower left | 43 | 15 | 74.1 | 1.33 (0.88–2.00) | 83.0 | 1.29(1.00–1.65) | 0.047 |
| Upper right | 57 | 32 | 64.0 | 1.44 (0.78–1.68) | 64.6 | 1.00(0.76–1.32) | 0.990 |
| Lower right | 47 | 37 | 56.0 | 1.00 | 64.4 | 1.00 | |
1. Adjusted for age, sex, chronic illness, social class, family COVID-19 case, and falla.
2. Age 15 years and above.
3. Adjusted for age, sex, chronic illness, social class, family COVID-19 case, falla, attendance time, quadrant, and number of MGEs attended.
4. Adjusted for age, sex, chronic illness, social class, family COVID-19 case, falla, symptomatic case in dinner table, and number of MGEs attended.
Finally, our analysis also found that four out of the five food handlers who served in the two MGE dinners were confirmed COVID-19 cases by laboratory tests. Three of them reported having COVID-19 symptomatology starting on March 16, 17, and 24 March 2020, respectively, after the MGEs were over. One case was asymptomatic.
Sensitivity analysis
The sensitivity analysis included the 1064 participants with laboratory tests of COVID-19 and cases between 6 and 31 March 2020 (Tables 7 and 8). The AR of this group was 44.0% from 468 COVID-19 cases and 596 non-cases. Some variations with the previous findings were found, considering its lower sample size and the higher age of participants (Table 2). Risk factors such as age and BMI lost significance, but alcohol consumption was associated with COVID-19 disease. Other factors did not show considerable changes. The pa-i-porta and the Queen’s gala dinner maintained significant associations with COVID-19, including attendance time, table shared with a COVID-19 symptomatic participant, and quadrants in building A. In the Queen’s gala dinner, quadrants lost significance.
Table 7. Sensitivity analysis.
Participants with laboratory tests of SARS-CoV-2 and mass gathering event (MGEs) attendance, attack rate (AR) adjusted AR (aAR), and adjusted (aRR). Confidence interval (CI). From March 6 to 31, 2020, Borriana.
| Variables | Cases | Non-cases | AR (%) | aAR (%) | aRR (95% IC)1 | p-value |
|---|---|---|---|---|---|---|
| Male | 180 | 249 | 42.0 | 44.1 | 1.01(0.89–1.16) | 0.862 |
| Female | 288 | 347 | 45.4 | 43.6 | 1.00 | |
| Age 0–4 (years)2 | 4 | 14 | 22.2 | 16.4 | 1.00 | |
| 5–14 | 44 | 84 | 34.4 | 29.4 | 1.79(0.50–6.38) | 0.370 |
| 15–24 | 88 | 115 | 43.4 | 42.1 | 2.46(0.69–9.00) | 0.143 |
| 25–34 | 60 | 90 | 40.0 | 42.3 | 2.58(0.73–9.08) | 0.142 |
| 35–44 | 100 | 105 | 48.8 | 49.9 | 3.03(0.87–10.63) | 0.083 |
| 45–64 | 155 | 167 | 48.1 | 46.7 | 2.84(0.81–9.94) | 0.102 |
| 65 and above | 17 | 21 | 44.7 | 41.1 | 2.50(0.71–8.83) | 0.154 |
| Occupation I-II1 | 142 | 122 | 53.8 | 51.6 | 1.23(1.07–1.42) | 0.003 |
| Occupation III-VI | 323 | 469 | 40.8 | 41.9 | 1.00 | |
| Chronic illness1 Yes | 155 | 184 | 42.9 | 43.7 | 0.99(0.87–1.15) | 0.992 |
| No | 309 | 411 | 45.7 | 43.9 | 1.00 | |
| Family with COVID-19 Yes | 293 | 213 | 57.9 | 55.6 | 1.64(1.43–1.88) | <0.001 |
| No | 174 | 376 | 31.6 | 33.9 | 1.00 | |
| Body Mass Index1,3 <18.5 Kg/m2 | 11 | 24 | 31.4 | 6.7 | 1.00 | |
| 18.5–24.9 Kg/m2 | 189 | 252 | 42.9 | 45.6 | 6.81(0.41–113.91) | 0.182 |
| 25.0–29.9 Kg/m2 | 139 | 154 | 47.4 | 48.8 | 7.29(0.44–121.98) | 0.167 |
| ≥30.0 Kg/m2 | 79 | 66 | 54.5 | 59.1 | 8.83(0.53–401.56) | 0.130 |
| Physical exercise1,3 Yes | 244 | 322 | 43.1 | 44.1 | 0.90(0.78–1.02) | 0.109 |
| No | 176 | 176 | 50.0 | 49.2 | 1.00 | |
| Drank alcohol 1,3 Yes | 104 | 108 | 49.1 | 53.4 | 1.19(1.04–1.37) | 0.015 |
| No | 316 | 390 | 44.8 | 44.8 | 1.00 | |
| Current smoker1,3 | 68 | 169 | 28.7 | 30.7 | 0.62(0.50–0.75) | <0.001 |
| Ex smoker1,3 | 104 | 83 | 55.6 | 54.8 | 1.10 (0.95–1.28) | 0.215 |
| Never smoker1,3 | 246 | 245 | 50.1 | 49.8 | 1.00 | |
| 5 MGEs attended2 | 6 | 1 | 85.7 | 82.6 | 3.62(2.83–4.61) | <0.001 |
| 4 MGEs attended2 | 52 | 15 | 77.6 | 78.7 | 3.44(2.63–4.49) | <0.001 |
| 3 MGEs attended2 | 94 | 48 | 66.2 | 64.3 | 2.81(2.15–3.67) | <0.001 |
| 2 MGEs attended2 | 121 | 101 | 54.5 | 53.0 | 2.32(1.78–3.02) | <0.001 |
| 1 MGE attended2 | 139 | 224 | 38.3 | 37.9 | 1.66(1.27–2.16) | <0.001 |
| 0 MGEs attended2 | 56 | 207 | 21.3 | 22.9 | 1.00 |
1. Adjusted for age, sex, chronic illness, social class, family COVID-19 case, falla, and MGEs attended.
2. Adjusted for all factors except MGEs.
3. Age 15 years and above.
Table 8. Sensitivity analysis.
Participants with laboratory tests of SARS-CoV-2 and the pa-i-porta and Queen’s gala dinner mass gathering event (MGE) attendance, attack rate (AR), adjusted AR (aAR), and adjusted (aRR). Confidence interval (CI). From March 6 to 31, 2020, Borriana.
| Variables | Cases | Non-cases | AR (%) | aAR (%) | aRR (95%IC)1 | p-value |
|---|---|---|---|---|---|---|
| Pa-i-porta | ||||||
| Attendance1 Yes | 371 | 316 | 54.0 | 53.0 | 1.96(1.64–2.35) | <0.001 |
| No | 97 | 280 | 25.7 | 27.0 | 1.00 | |
| Attendance time1 2 | ||||||
| Less than half | 30 | 33 | 47.6 | 44.6 | 1.00 | |
| Half | 102 | 119 | 46.2 | 45.6 | 1.02(0.75–1.38) | 0.887 |
| More than half | 102 | 74 | 58.0 | 52.3 | 1.26(0.94–1.70) | 0.122 |
| All the time | 136 | 89 | 60.4 | 61.2 | 1.37(1.03–1.83) | 0.031 |
| Dinner table with a COVID-19 symptomatic case3 | ||||||
| Yes | 326 | 263 | 55.3 | 58.8 | 2.57(1.45–4.83) | 0.001 |
| No | 41 | 46 | 47.1 | 22.9 | 1.00 | |
| Quadrants building A4 | ||||||
| Upper left | 127 | 93 | 57.7 | 51.8 | 1.25(0.88–1.77) | 0.212 |
| Lower left | 112 | 98 | 53.3 | 53.3 | 1.29(0.95–1.74) | 0.105 |
| Upper right | 69 | 31 | 69.0 | 69.3 | 1.67(1.34–2.08) | 0.000 |
| Lower right | 59 | 87 | 40.4 | 41.5 | 1.00 | |
| Queen’s gala dinner | ||||||
| Attendance1 Yes | 196 | 98 | 66.7 | 65.5 | 1.80(1.58–2.05) | <0.001 |
| No | 272 | 498 | 35.3 | 36.4 | 1.00 | |
| Attendance time1 | ||||||
| Less than half | 11 | 11 | 50.0 | 42.4 | 1.00 | |
| Half | 31 | 14 | 68.9 | 69.9 | 1.65(1.08–2.51) | 0.019 |
| More than half | 42 | 26 | 61.8 | 61.0 | 1.44(0.94–2.18) | 0.086 |
| All the time | 112 | 47 | 70.4 | 71.0 | 1.67 (1.15–2.45) | 0.008 |
| Dinner table with a COVID-19 symptomatic case5 | ||||||
| Yes | 88 | 31 | 74.0 | 74.7 | 1.19 (1.01–1.40) | 0.037 |
| No | 101 | 61 | 62.4 | 62.8 | 1.00 | |
| Quadrant of building A6 | ||||||
| Upper left | 43 | 18 | 70.5 | 66.9 | 1.01(0.73–1.35) | 0.971 |
| Lower left | 43 | 14 | 75.4 | 84.9 | 1.26(0.98–1.63) | 0.075 |
| Upper right | 56 | 26 | 68.3 | 63.8 | 0.95(0.71–1.27) | 0.718 |
| Lower right | 47 | 34 | 58.0 | 67.2 | 1.00 | |
1. Adjusted for age, sex, chronic illness, social class, family COVID-19 case, and falla.
2. Missing information in two cases.
3. Adjusted age, sex, median of attendance time, and median MGEs attended.
4. Adjusted for median of MGEs attended.
5. Adjusted for age, sex, chronic illness, social class, family COVID-19 case, falla, attendance time, quadrant, and number of MGEs attended.
6. Adjusted for age, sex, chronic illness, social class, family COVID-19 case, falla, symptomatic case in dinner table, and number of MGEs attended.
Discussion
The results of this study indicate a high transmission of COVID-19 disease in the MGEs studied, which may be considered as a community outbreak with several point sources from March 6 to 10 [47]. Respiratory transmission was the predominant mode of propagation by droplets from patients to exposed persons; contact via fomites was less frequent [48, 49]. Airborne transmission has been suggested in relation to COVID-19 outbreaks in different places, and is a plausible route [50–52]. The two MGEs with the highest incidence of the disease included a dinner, as in other COVID-19 outbreaks, but food-borne transmission can be discarded in this study [53, 54].
Some characteristics of this MEG outbreak may be highlighted, including its magnitude and impact in the population of Borriana, the diversity of places where it occurred indoors (building and theater) and outdoors (square), the higher risk of COVID-19 associated with the number of MGEs attended, the estimation of risk for attendance at no MGEs, the detection of risk factors (obesity, old age, and upper and middle class versus lower class) with current smoking as a protective factor, and the rapid spread with high ARs.
In the study, the AR was 42.6%, and during the period of the MGEs, 39.2% with 94.0% of confirmed cases. If the AR were extrapolated to falles members, the total of COVID-19 cases could be between 1193 (95% CI 1269–1117) and 1098 (95% CI 1173–1023), respectively. In addition, a high proportion of cases had family members with COVID-19, suggesting a high secondary transmission among families, in line with Thompson and co-authors and with a study of secondary attack rate of COVID-19 infections in Castellon [55, 56]. It may explain the high incidence in the municipality of Borriana, which was the highest in the province of Castellon during the first outbreak period. Considering the period February to July 2020, the incidence of COVID-19 in Borriana was 307 cases with positive PCR results (885 per 100,000 inhabitants) and 40 deaths (1.2 per 1000 inhabitants) [34]. As a comparison, the COVID-19 incidence in Castellon de la Plana, the provincial capital (170,000 inhabitants), was 463 cases (272.4 per 100,000 inhabitants) and 50 deaths (0.29 per 1,000 inhabitants). The high mortality in Borriana is striking [57, 58], and it may be related to the prevalence of cardiovascular risk factors in this municipality [59]. Regarding the incidence of COVID-19, the study found 536 confirmed cases, 39 cases with positive PCR results; these were the only cases reported by the health authorities. It may be estimated that for every reported case, there could have been around 13 or 14 cases, implying that 92.7% of cases were undiagnosed. This situation is in line with two studies on undocumented infections of SARS-CoV-2 in China (86% and 93%), and France (86%), respectively [60–62].
In the context of COVID-19 outbreaks related to MGEs, different models have been proposed to estimate the number of cases deriving from MGEs or Ro values [63, 64]. Apart from assuming several premises, these models need a constant infection rate or Ro. As a tentative approximation and using the classic SIR (susceptible, infected, recovered) infection process model [65], we explored our results to obtain the Ro from the infection rate based on the date of onset of cases, number of contacts, and duration of infectiousness. We used the formula [66]:
where PI = “average probability a contact will be infected over duration of a relationship”; CR = “average rate of getting into contact”; and DI = “average duration infectiousness”. We defined PI, the infection rate, as new cases of COVID-19 divided by the susceptible participants per day; CR as a number of potential contacts, following the study of Tupper and co-authors [63], and DI as 10 days duration of infectiousness [67]. We considered a period of 19 days from the first MGE to the last MGE, plus a 14-day maximum incubation period for COVID-19. The results are shown in Table 9.
Table 9. Estimation of the basic reproductive number (Ro) from the MGE COVID-19 outbreak between 6 and 10 March 2020 plus 14 days.
| Days/Date infection onset | New cases (a) | Total cases (I) (b) | Susceptible (S) (c) | Infection rate (a/c) | Basic reproduction number Ro1 Numbers of contacts2 | ||
|---|---|---|---|---|---|---|---|
| 5 | 10 | 15 | |||||
| 3/6/2020: 03 | 9 | 9 | 1264 | 0.00712 | 0.36 | 0.71 | 1.07 |
| 3/7/2020: 13 | 11 | 20 | 1255 | 0.00877 | 0.44 | 0.88 | 1.32 |
| 3/8/2020: 23 | 15 | 35 | 1244 | 0.01206 | 0.60 | 1.21 | 1.81 |
| 3/9/2020: 3 | 45 | 80 | 1229 | 0.03662 | 1.83 | 3.66 | 5.49 |
| 3/10/20203 4 | 39 | 119 | 1184 | 0.03294 | 1.65 | 3.29 | 4.94 |
| 3/11/2020: 5 | 32 | 151 | 1145 | 0.02795 | 1.40 | 2.80 | 4.19 |
| 3/12/2020: 6 | 21 | 172 | 1113 | 0.01887 | 0.94 | 1.89 | 2.83 |
| 3/13/2020: 7 | 31 | 203 | 1092 | 0.02839 | 1.42 | 1.84 | 4.26 |
| 3/14/2020: 8 | 33 | 236 | 1061 | 0.03110 | 1.56 | 3.11 | 4.67 |
| 3/15/2020: 9 | 30 | 266 | 1028 | 0.02918 | 1.46 | 2.92 | 4.38 |
| 3/16/2020:10 | 48 | 314 | 998 | 0.04810 | 2.41 | 4.81 | 7.22 |
| 3/17/2020:11 | 20 | 334 | 950 | 0.02105 | 1.03 | 2.05 | 3.08 |
| 3/18/2020:12 | 18 | 352 | 930 | 0.01935 | 0.97 | 1.94 | 2.90 |
| 3/19/2020:13 | 15 | 369 | 912 | 0.01644 | 0.82 | 1,64 | 2.47 |
| 3/20/2020:14 | 15 | 382 | 897 | 0.01672 | 0.84 | 1.67 | 2.51 |
| 3/21/2020:15 | 6 | 388 | 882 | 0.00680 | 0.34 | 0.68 | 1.02 |
| 3/22/2020:16 | 7 | 395 | 876 | 0.00799 | 0.40 | 0.80 | 1.20 |
| 3/23/2020:17 | 2 | 397 | 869 | 0.00230 | 0.12 | 0.23 | 0.35 |
| 3/24/2020:18 | 4 | 401 | 867 | 0.00461 | 0.23 | 0.46 | 0.69 |
| 3/25/2020:19 | 7 | 408 | 863 | 0.00811 | 0.41 | 0.81 | 1.22 |
1. Ro = infection rate x contact numbers x duration infectiousness (10 days).
2. Considering average numbers of contacts in conferences, lectures, and restaurants (5, 10, and 15).
3. Date with MGE.
Considering the infection rate per day, an increase was observed from 0.00172 on the first day to 0.04810 on March 16 and a decline until 0.00811 on March 25. The countrywide lockdown began on March 15 and has been shown to have had a high effect [68]. With five contacts, Ro>1.0 reached only 8 days and a maximum of 2.41; with 10 contacts, Ro>1.0 reached 13 days and a maximum of 4.81; and with 15 contacts, Ro>1.0 reached 19 days and a maximum of 7.22 on the 16th day. The decline of the Ro was very steep from the maximum and Ro<1.0 values were observed, indicating that the epidemic would soon decline [69]. These results reflect the high transmission of the disease associated with MGEs.
To explore the expected numbers of cases in the COVID-19 outbreak associated with the MGEs, we followed the approach of Tupper and co-authors [63], considering the probability of infection (β), the duration time (T), time of contact (τ) and the number of contacts (k). We calculated k from two MGEs (pa-i-porta and the Queen’s gala dinner). The formula yields the expected number of new infections:
Attendances at the pa-i-porta and Queen’s gala dinner events were used to estimate expected cases and compare them with observed cases. For the pa-i-porta event, the number of contacts was 85 for less than half the attendance time and 60 for more than half the attendance time, to obtain a similar number of observed and expected cases. For the Queen’s gala dinner the numbers of contacts were 20 for less than half the attendance time and 40 for more than half the attendance time. Considering that 9 and 11 cases of COVID-19 (Table 10) had the onset of symptoms the day of the pa-i-porta and the Queen’s gala dinner, respectively, the number of contacts k could be divided by 9 and 11, and contacts could be 7 to 10 for pa-i-porta and 2 to 4 for the Queen’s gala dinner. These results could explain the spread of the epidemic, and underline the importance of the duration of the event, the number of contacts, and the number of participants, which were much higher in the pa-i-porta than in the Queen’s gala dinner. However, a major limitation of this approach is the theoretical assumption of homogeneous mixing of population in the epidemic [70]. In addition, asymptomatic or undiagnosed cases may bias the results and 67 cases were asymptomatic in our study.
Table 10. Attendance at pa-i-porta and Queen’s gala dinner MGEs and number of contacts (k) to obtain expected cases of COVID-19 compared with observed cases from the formula of Tupper and co-authors [63].
| MGEs | Attendance time | Probability infection β | Time T hours | Contact time τ | Number contacts k | Number expected Cases | Number observed cases |
|---|---|---|---|---|---|---|---|
| Pa-i-porta | Less than half | 0.465 | 3.30 | 0.2 | 85 | 132.1 | 132 |
| More than half | 0.594 | 7.0 | 0.2 | 60 | 235.2 | 238 | |
| Queen’s gala dinner | Less than half | 0.627 | 3.15 | 0.2 | 20 | 41.2 | 42 |
| More than half | 0.678 | 6.30 | 0.2 | 40 | 152.2 | 154 |
1. Infection rates of attendance at pa-i-porta and Queen’s gala dinner
2. Contact time from Tupper and co-authors [63].
In our study the iceberg-like pattern of COVID-19 could be observed, considering the percentages of 0.17% patient deaths, 2.3% hospitalized, 12% asymptomatic, and 85.8% symptomatic [71]. The most frequent symptoms of COVID-19 cases were weakness, fever, and lost smell or/and taste; the severe course of the disease was less frequent in accordance with the average age of the patients [59, 72, 73]. In addition, the medical assistance was low and chronic illness was weakly associated with COVID-19, but cardiovascular diseases, hypertension, and hypothyroidism increased the risk of COVID-19, as indicated in some studies [74, 75]. The presence of sequels remains low, but this is a new disease and follow-up of these patients would be useful.
Considering the risk factors of COVID-19, higher age was associated with the disease, and children and adolescents were less affected [76, 77]; in contrast with other studies [78], sex was not a risk factor. Young patients constituted asymptomatic cases, and their frequency was lower than in other studies [79–81]. The validity of self-reported lifestyle data has been considered good [82], and overweight and obesity were risk factors in line with population-based studies of COVID-19 [83, 84]. In addition, Merzon and co-authors [85] found that vitamin D deficiency was a risk factor of COVID-19 infection and severity. Alcohol consumption was a marginal risk factor, but has not been found in some studies [86, 87]. Upper and middle social classes were associated with the disease, in contrast with other studies [85, 88]. Smoking is a controversial factor because it has been found to be both protective and a risk factor [85–87, 89, 90].
When observing the MGEs, it may be useful to consider that participation in the Falles festival was extensive, since the population of Borriana, both adults and children, took part in many cultural, touristic, leisure, and dinner events [35], and many MGEs were held in February and March 2020. These MGEs may be considered as super-spreading events [91, 92]. In this context, several points stand out. First, COVID-19 cases began in January and February 2020, with the onset of symptoms before the MGEs took place. Second, the pa-i-porta and the Queen’s gala dinner included dancing, which involved more contact among participants. In these MGEs the presence of participants with symptoms at the same dinner table was a significant risk factor of COVID-19, which is consistent with symptomatic cases being more contagious than asymptomatic cases [10, 93, 94]. Third, indoor MGEs had a high attendance, mainly in building A; considering the building’s capacity and the close proximity among participants, a higher risk of transmission was found [3, 95, 96]. Attendance at the other MGEs was lower and full capacity was not reached. Fourth, several MGEs lasted for more than six hours and ended in the early morning. The average temperature in Borriana in March is 13.4°C, and the average relative humidity is 64% [97]. These weather conditions have been shown to favor SARS-CoV-2 transmission, estimated to range between 5°-15°C and 30–100% of temperature and relative humidity, respectively [98, 99]. Fifth, all the MGEs except the Valencia trip occurred in closed indoor places, building A and theater B; both locations have air conditioning and heating, which are more modern in the case of theater B, and no breakdowns or malfunctions were observed. Finally, airborne transmission [100] may be possible, and our results indicate one quadrant of building A with a lower incidence of COVID-19, but the two quadrants with the highest incidence were not the same in the two events, and these two quadrants were occupied by the Falles organizers and guests, who had attended the most MGEs. However, the presence of asymptomatic cases, the variability of the incubation period, and other potential transmission sources make it difficult to confirm this transmission in these MGEs.
A potential causal relationship between MGE attendance and COVID-19 may be considered following the Austin Bradford-Hill criteria [101]; aRR of MGE attendance ranged from moderate to high. It has been suggested that there is a biological plausibility of COVID-19 transmission happening in closed places, where many participants gather in areas that are smaller than 1.83 m2 per individual [102]. This is consistent with other COVID-19 outbreaks in MGEs in several countries [21, 24, 42, 103, 104]. The temporal relationship between MGE attendance and COVID-19 was established after the event. A dose-response relationship was demonstrated between MGE attendance, attendance time, and risk of the disease [105]. As an observational study, a retrospective cohort design could estimate the causality relationship more precisely than descriptive studies.
The strengths of our study are as follows. First, it has a population-based design that allows a more integral approach to COVID-19. Second, a representative sample of a population exposed to MGEs was analyzed. Third, the response rate was high. Fourth, a serologic survey was carried out to confirm COVID-19 cases [106, 107] with a highly sensitive and specific technique. Fifth, statistical analysis was adjusted for potential confounding factors. Finally, the sensitivity analysis confirmed the previous results with an improvement in study precision.
The study’s limitations are as follows. First, there was a period of time between exposure at the MGEs and the start of the study. In addition, the impact of the COVID-19 pandemic could have caused some recall and misclassification biases. Second, only the Falles population was included in the study. Third, other MGEs were not studied, such as the Ninot parade, community dinners, children’s entertainments, and others that may have played a role in COVID-19 transmission in Borriana. Fourth, an estimation of incubation periods was difficult considering the variety of MGE attendance. Fifth, no genetic studies were carried out into the SARS-CoV-2 of positive PCR patients. Sixth, some residual biases may persist despite adjustments. Finally, as a new disease, COVID-19 could have some factors that were not considered in the study.
Some recommendations may be addressed based on the results of the study. First, and with immediate effect, MGEs should be considered as potential triggers of high transmission of SARS-CoV-2. The maintenance, conservation, and inspection of the closed indoor building where these MGEs took place should also be strengthened. We must highlight that MEGs have continued to be held successfully with measures in place to prevent SARS-CoV-2 transmission, suggesting that MGEs could be implemented again with specific prevention measures [108–112]. Second, COVID-19 patients should be monitored to find out about this new disease and its evolution. Third, population-based studies, including serologic surveys, should be carried out to estimate the extent of COVID-19 [113, 114]. Finally, regarding our study, new lines of research could be implemented, including estimating other risk factors of COVID-19 disease, determining serologic variations of antibodies against SARS-CoV-2 in the coming months, following-up patients and potential sequels, and exploring factors associated with the spread of the COVID-19 pandemic [115].
As an epilogue to our study, we are carrying out a prospective cohort study with patients who tested positive for COVID-19, and a second sero-epidemiological study, started in October 2020, to research evolution, sequelae and antibodies against SARS-CoV-2.
Conclusions
The results of this study suggest the importance of MGEs in COVID-19 transmission that could explain the subsequent COVID-19 outbreak in Borriana. Population-based studies, including serologic COVID-19 surveys, may usefully inform the adoption of preventive measures that help to contain the COVID-19 pandemic.
Supporting information
(DOCX)
(DTA)
(DTA)
(DOCX)
Acknowledgments
We are grateful to all the people who participated in the study and to the organizers of the Falles in Borriana for their help and support. In addition, we wish to thank Roser Blasco-Gari, Helena Buj-Jorda, Israel Borras-Acosta, Lucia Castell-Agusti, Mercedes De Francia-Valero, Maria Domènech-Molinos, Marc Garcia, Maria Gil-Fortuño, Elena Grañana-Toran, Noelia Hernández-Perez, Laura Lopez-Diago, Salvador Martinez-Parra, Sara Moner-Marin, Silvia Pesudo-Calatayud, Lara Sabater-Hernández, Maria Luisa Salve-Martinez, Irene Suarez-Linares, Juan José Ventura-Buchardo, and Alberto Yagüe-Muñoz for their assistance and support in carrying out the study. We acknowledge the help of Francis Conde-Mollà, Cristina Devis-Drago, and Carolina Vicente-Rodriguez in implementing this study, Jose Monserrat-Vicent for his assistance with the English and Mary B Savage Cooper for her English revision. We thank Claudia Arnedo-Pac and Jose Antonio Valer for their advice and for constructing the figures.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
The author(s) received no specific funding for this work.
References
- 1.Zhou P, Yang XL, Wang XG, Hu B, Zhang L, Zhang W, et al. A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature. 2020;579:270–273. doi: 10.1038/s41586-020-2012-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.World Health Organization. Public health for mass gatherings: key considerations (Interim Guidance). 2015. Available from https://apps.who.int/iris/rest/bitstreams/717805/retrieve
- 3.Shen Y, Li C, Dong H, Wang Z, Martinez L, Sun Z, et al. Community outbreak investigation of SARS-CoV-2 transmission among bus riders in Eastern China. JAMA Intern Med. 2020:e205225. doi: 10.1001/jamainternmed.2020.5225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pourmalek F, Rezaei Hemami M, Janani L, Moradi-Lakeh M. Rapid review of COVID-19 epidemic estimation studies for Iran. BMC Public Health. 2021;21:257. doi: 10.1186/s12889-021-10183-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Che Mat NF, Edinur HA, Abdul Razab MKA, Safuan S. A single mass gathering resulted in massive transmission of COVID-19 infections in Malaysia with further international spread. J Travel Med. 2020;27:taaa059. doi: 10.1093/jtm/taaa059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Signorelli C, Odone A, Riccò M, Bellini L, Croci R, Oradini-Alacreu A, et al. Major sports events and the transmission of SARS-CoV-2: analysis of seven case-studies in Europe. Acta Biomed. 2020;91:242–244. doi: 10.23750/abm.v91i2.9699 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Perez-Bermejo M, Murillo-Llorente MT. The fast territorial expansion of COVID-19 in Spain. J Epidemiol. 2020;30:236. doi: 10.2188/jea.JE20200123 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gerbaud L, Guiguet-Auclair C, Breysse F, Odoul J, Ouchchane L, Peterschmitt J, et al. Hospital and population-based evidence for COVID-19 early circulation in the East of France. Int J Environ Res Public Health. 2020;17):7175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brandl M, Selb R, Seidl-Pillmeier S, Marosevic D, Buchholz U, Rehmet S. Mass gathering events and undetected transmission of SARS-CoV-2 in vulnerable populations leading to an outbreak with high case fatality ratio in the district of Tirschenreuth, Germany. Epidemiol Infect;148:e252. doi: 10.1017/S0950268820002460 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yusef D, Hayajneh W, Awad S, Momany S, Khassawneh B, Samrah S, et al. Large outbreak of coronavirus disease among wedding attendees, Jordan. Emerg Infect Dis. 2020;26:2165–7. doi: 10.3201/eid2609.201469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cuschieri S, Balzan M, Gauci C, Aguis S, Grech V. Mass events trigger Malta’s second peak after initial successful pandemic suppression. J Community Health. 2020: Sep16:1–8. doi: 10.1007/s10900-020-00925-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stange M, Mari A, Roloff T, Seth-Smith HM, Schweitzer M, Brunner M, et al. SARS-CoV-2 outbreak in a tri-national urban area is dominated by a B.1 lineage variant linked to a mass gathering event. PLoS Pathog. 2021;17:e1009374. doi: 10.1371/journal.ppat.1009374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Nyasulu JCY, Munthali RJ, Nyondo-Mipando AL, Pandya H, Nyirenda L, Nyasulu P,et al. COVID-19 pandemic in Malawi: Did public social-political events gatherings contribute to its first wave local transmission? Int J Infect Dis. 2021:106:269–275. doi: 10.1016/j.ijid.2021.03.055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.World Health Organization. Key planning recommendations for mass gatherings in the context of COVID-19 outbreak. Interim guidance 29May2020. Available from https://www.who.int/publications/i/item/10665-332235 [Google Scholar]
- 15.Center Disease Control and Prevention. Guidance for Organizing Large Events and Gatherings. https://www.cdc.gov/coronavirus/2019-ncov/community/large-events/considerations-for-events-gatherings.html.
- 16.McCloskey B, Zumla A, Ippolito G, Blumberg L, Arbon P, Cicero A, et al. Mass gathering events and reducing further global spread of COVID-19: a political and public health dilemma. Lancet. 2020;395:1096–1099. doi: 10.1016/S0140-6736(20)30681-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Escher AR Jr. An ounce of prevention: Coronavirus (COVID-19) and mass gatherings. Cureus. 2020;12(3):e7345. doi: 10.7759/cureus.7345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ebrahim SH, Memish ZA. COVID-19 the role of mass gatherings. Travel Med Infect Dis. 2020;34:101617. doi: 10.1016/j.tmaid.2020.101617 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.JH Jones. Notes on Ro. Califonia: Department of Anthropological Sciences; 2007:323. Available from: https://web.stanford.edu › Jones_R0_notes2019.
- 20.Alimohamadi Y, Taghdir M, Sepandi M. Estimate of the basic reproduction number for COVID-19: A systematic review and meta-analysis. J Prev Med Public Health. 2020; 53:151–157. doi: 10.3961/jpmph.20.076 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Liu Y, Eggo RM, Kucharski AJ. Secondary attack rate and superspreading events for SARS-CoV-2. Lancet. 2020;395:e47. doi: 10.1016/S0140-6736(20)30462-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Leclerc QJ, Fuller NM, Knight LE; CMMID COVID-19 Working Group, Funk S, Knight GM. What settings have been linked to SARS-CoV-2 transmission clusters? Wellcome Open Res. 2020;5:83. doi: 10.12688/wellcomeopenres.15889.2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Al-Rousan N, Al-Najjar H. Is visiting Qom spread CoVID-19 epidemic in the Middle East? Eur Rev Med Pharmacol Sci. 2020;24:5813–5818. doi: 10.26355/eurrev_202005_21376 [DOI] [PubMed] [Google Scholar]
- 24.James A, Eagle L, Phillips C, Hedges DS, Bodenhamer C, Brown R, et al. High COVID-19 attack rate among attendees at events at a church—Arkansas, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69:632–635. doi: 10.15585/mmwr.mm6920e2 [DOI] [PubMed] [Google Scholar]
- 25.Addetia A, Crawford KH, Dingens A, Zhu H, Roychoudhury P, Huang ML, et al. Neutralizing antibodies correlate with protection from SARS-CoV-2 in humans during a fishery vessel outbreak with high attack rate. medRxiv [Preprint]. 2020. Aug 14:2020.08.13.20173161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Accorsi EK, Qiu X, Rumpler E, Kennedy-Shaffer L, Kahn R, Joshi K, et al. How to detect and reduce potential sources of biases in studies of SARS-CoV-2 and COVID-19. Eur J Epidemiol. 2021;36:179–196. doi: 10.1007/s10654-021-00727-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Members of the Working group for the surveillance and control of COVID-19 in Spain. The first wave of the COVID-19 pandemic in Spain: characterisation of cases and risk factors for severe outcomes, as at 27 April 2020. Euro Surveill. 2020;25:2001431. doi: 10.2807/1560-7917.ES.2020.25.50.2001431 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pollán M, Pérez-Gómez B, Pastor-Barriuso R, Oteo J, Hernán MA, Pérez-Olmeda M, et al. Prevalence of SARS-CoV-2 in Spain (ENE-COVID): a nationwide, population-based seroepidemiological study. Lancet. 2020;396:535–544. doi: 10.1016/S0140-6736(20)31483-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Soriano-Arandes A, Gatell A, Serrano P, Biosca M, Campillo F, Capdevila R, et al. Household SARS-CoV-2 transmission and children: a network prospective study. Clin Infect Dis. 2021:ciab228. doi: 10.1093/cid/ciab228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marks M, Millat-Martinez P, Ouchi D, Roberts CH, Alemany A, Corbacho-Monné M, et al. Transmission of COVID-19 in 282 clusters in Catalonia, Spain: a cohort study. Lancet Infect Dis. 2021:S1473-3099(20)30985-3. doi: 10.1016/S1473-3099(20)30985-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bernabeu-Wittel M, Ternero-Vega JE, Díaz-Jiménez P, Conde-Guzmán C, Nieto-Martín MD, Moreno-Gaviño L, et al. Death risk stratification in elderly patients with covid-19. A comparative cohort study in nursing homes outbreaks. Arch Gerontol Geriatr. 2020;91:104240. doi: 10.1016/j.archger.2020.104240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Suárez-García I, Martínez de Aramayona López MJ, Sáez Vicente A, Lobo Abascal P. SARS-CoV-2 infection among healthcare workers in a hospital in Madrid, Spain. J Hosp Infect. 2020;106:357–363. doi: 10.1016/j.jhin.2020.07.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.The national COVID-19 outbreak monitoring group. COVID-19 outbreaks in a transmission control scenario: challenges posed by social and leisure activities, and for workers in vulnerable conditions, Spain, early summer 2020. Euro Surveill. 2020;25:2001545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Conselleria de Sanitat Universal i Salut Públic. Portal de servei sanitari sobre coronavirus. Generalitat Valenciana. Available from: http://coronavirus.san.gva.es/
- 35.Gumbau-Gonzalez JE, Boix-Bort P. Què és la falla?. Borriana: Falla Don Bosco; 2018. [Google Scholar]
- 36.Aymerich-Tormo J. Burriana en sus Fallas (1928–1936). Tomo I. Burriana: Grup D’Estudis Històrics Fallers 1996. [Google Scholar]
- 37.Dean AG, Sullivan KM, Soe MM. OpenEpi: Open Source Epidemiologic Statistics for Public Health, Versión. Available from www.OpenEpi.com
- 38.Egger M, Bundschuh C, Wiesinger K, Gabriel C, Clodi M, Mueller T, et al. Comparison of the Elecsys® Anti-SARS-CoV-2 immunoassay with the EDI™ enzyme linked immunosorbent assays for the detection of SARS-CoV-2 antibodies in human plasma. Clin Chim Acta. 2020;509:18–21 doi: 10.1016/j.cca.2020.05.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Dellière S, Salmona M, Minier M, Gabassi A, Alanio A, Le Goff J, et al. Evaluation of the COVID-19 IgG/IgM rapid test from Orient Gene Biotech. J Clin Microbiol. 2020;58:e01233–20. doi: 10.1128/JCM.01233-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yip CC, Sridhar S, Cheng AK, Leung KH, Choi GK, Chen JH, et al. Evaluation of the commercially available LightMix® Modular E-gene kit using clinical and proficiency testing specimens for SARS-CoV-2 detection. J Clin Virol. 2020;129:104476. doi: 10.1016/j.jcv.2020.104476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Council of State and Territorial Epidemiologists. Standardized surveillance case definition and national notification for 2019 novel coronavirus disease (COVID-19). Atlanta, GA: Council of State and Territorial Epidemiologists; 2020. Available from: https://cdn.ymaws.com/www.cste.org/resource/resmgr/2020ps/interim-20-id-01_covid-19.
- 42.Epi Info version 7. Atlanta: Centers for Disease Control and Prevention 2013. Available from: https://www.cdc.gov/epiinfo.
- 43.Greenland S, Pearl J, Robins JM. Causal diagrams for epidemiologic research. Epidemiology. 1999;10:37–48. [PubMed] [Google Scholar]
- 44.Textor J, van der Zander B, Gilthorpe MS, Liskiewicz M, Ellison GT. Robust causal inference using directed acyclic graphs: the R package ’dagitty’. Int J Epidemiol. 2016;45:1887–1894. doi: 10.1093/ije/dyw341 [DOI] [PubMed] [Google Scholar]
- 45.Robins JM, Hernán MA, Brumback B. Marginal structural models and causal inference in epidemiology. Epidemiology 2000;11:550–60. doi: 10.1097/00001648-200009000-00011 [DOI] [PubMed] [Google Scholar]
- 46.Stata® version 14.2. College Station, TX Stata Corporation 2015.
- 47.Fontaine R, Goodman RA. Describing the finding. In Gregg MB(Editor). Field epidemiology. Second edition. New York Oxford University Press; 2002: p. 78–116. [Google Scholar]
- 48.Meyerowitz EA, Richterman A, Gandhi RT, Sax PE. Transmission of SARS-CoV-2: A review of viral, host, and environmental factors. Ann Intern Med. 2020:M20–5008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Kasper MR, Geibe JR, Sears CL, Riegodedios AJ, Luse T, Von Thun AM, et al. An outbreak of Covid-19 on an aircraft carrier. N Engl J Med. 2020:NEJMoa2019375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Miller SL, Nazaroff WW, Jimenez JL, Boerstra A, Buonanno G, Dancer SJ, et al. Transmission of SARS-CoV-2 by inhalation of respiratory aerosol in the Skagit Valley Chorale superspreading event. Indoor Air. 2020. doi: 10.1111/ina.12751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Lu J, Gu J, Li K, Xu C, Su W, Lai Z, et al. COVID-19 Outbreak Associated with Air Conditioning in Restaurant, Guangzhou, China, 2020. Emerg Infect Dis. 2020; 26:1628–1631. doi: 10.3201/eid2607.200764 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Hamner L, Dubbel P, Capron I, et al. High SARS-CoV-2 attack rate following exposure at a choir practice—Skagit County, Washington, March 2020. MMWR Morb Mortal Wkly Rep. 2020;69:606–610. doi: 10.15585/mmwr.mm6919e6 [DOI] [PubMed] [Google Scholar]
- 53.Aherfi S, Gautret P, Chaudet H, Raoult D, La Scola B. Clusters of COVID-19 associated with Purim celebration in the Jewish community in Marseille, France, March 2020. Int J Infect Dis. 2020;100:88–94 doi: 10.1016/j.ijid.2020.08.049 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pung R, Chiew CJ, Young BE, Chin S, Chen MI, Clapham HE, et al. Investigation of three clusters of COVID-19 in Singapore: implications for surveillance and response measures. Lancet. 2020;395:1039–1046. doi: 10.1016/S0140-6736(20)30528-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Thompson HA, Mousa A, Dighe A, Fu H, Arnedo-Pena A, Barrett P, et al. SARS-CoV-2 setting-specific transmission rates: a systematic review and meta-analysis. Clin Infect Dis. 2021:ciab100. doi: 10.1093/cid/ciab100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Arnedo-Pena A, Sabater-Vidal S, Meseguer-Ferrer N, Pac-Sa R, Mañes-Flor P, Gascó-Laborda JC, et al. COVID-19 secondary attack rate and risk factors in household contacts in Castellon (Spain): Preliminary report. Rev Enf Emer 2020;19:64–70. [Google Scholar]
- 57.Berenguer J, Ryan P, Rodríguez-Baño J, Jarrín I, Carratalà J, Pachón J, et al. Characteristics and predictors of death among 4035 consecutively hospitalized patients with COVID-19 in Spain. Clin Microbiol Infect. 2020;26:1525–1536. doi: 10.1016/j.cmi.2020.07.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Harrison SL, Fazio-Eynullayeva E, Lane DA, Underhill P, Lip GYH. Comorbidities associated with mortality in 31,461 adults with COVID-19 in the United States: A federated electronic medical record analysis. PLoS Med. 2020;17(9):e1003321. doi: 10.1371/journal.pmed.1003321 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Pallares-Carratala V, Piñón-Selles F, Diago-Torrent JL, et al. Diabetes mellitus y otros factores de riesgo cardiovascular mayores en una población del Mediterraneo español. Estudio Burriana. Endocrinol. Nutr. 2006;53:158–167. [Google Scholar]
- 60.Li R, Pei S, Chen B, Song Y, Zhang T, Yang W, et al. Substantial undocumented infection facilitates the rapid dissemination of novel coronavirus (SARS-CoV-2). Science. 2020;368:489–493. doi: 10.1126/science.abb3221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Maugeri A, Barchitta M, Battiato S, Agodi A. Estimation of unreported novel coronavirus (SARS-CoV-2) infections from reported deaths: A susceptible-exposed-infectious-recovered-dead model. J Clin Med. 2020;9:1350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Pullano G, Di Domenico L, Sabbatini CE, Valdano E, Turbelin C, et al. Underdetection of cases of COVID-19 in France threatens epidemic control. Nature. 2021;590:134–139. doi: 10.1038/s41586-020-03095-6 [DOI] [PubMed] [Google Scholar]
- 63.Tupper P, Boury H, Yerlanov M, Colijn C. Event-specific interventions to minimize COVID-19 transmission. Proc Natl Acad Sci U S A. 2020;117:32038–32045. doi: 10.1073/pnas.2019324117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Saidan MN, Shbool MA, Arabeyyat OS, Al-Shihabi ST, Abdallat YA, Barghash MA, et al. Estimation of the probable outbreak size of novel coronavirus (COVID-19) in social gathering events and industrial activities. Int J Infect Dis. 2020;98:321–327. doi: 10.1016/j.ijid.2020.06.105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Cliff A, Smallman-Raynor M. Infectious disease control. Oxford: Oxford University Press; 2013, p 2–20. [Google Scholar]
- 66.Lipkin I. SARS outbreak study 2. Columbia University Mailman School of Public Health Available from: https://epiville.ccnmtl.columbia.edu/sars_outbreak_study_2/data_analysis.html
- 67.He X, Lau EHY, Wu P, Deng X, Wang J, Hao X, et al. Temporal dynamics in viral shedding and transmissibility of COVID-19. Nat Med. 2020;26:672–675. doi: 10.1038/s41591-020-0869-5 [DOI] [PubMed] [Google Scholar]
- 68.Siqueira CADS, Freitas YNL, Cancela MC, Carvalho M, Oliveras-Fabregas A, de Souza DLB. The effect of lockdown on the outcomes of COVID-19 in Spain: An ecological study. PLoS One. 2020;15:e0236779. doi: 10.1371/journal.pone.0236779 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Becker NG. Analysis of infectious disease data. London: Chapman and Hall Ltd; 1989. p 1–10. [Google Scholar]
- 70.Anderson RM, May RM. Infectious disease of humans: Dynamics and control. New York: Oxford University Press; 1991. p 13–23. [Google Scholar]
- 71.Salzberger B, Buder F, Lampl B, Ehrenstein B, Hitzenbichler F, Holzmann T, et al. Epidemiology of SARS-CoV-2. Infection. 2020Oct8; 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Argenziano MG, Bruce SL, Slater CL, Tiao JR, Baldwin MR, Barr RG, et al. Characterization and clinical course of 1000 patients with coronavirus disease 2019 in New York: retrospective case series. BMJ. 2020;369:m1996. doi: 10.1136/bmj.m1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Suleyman G, Fadel RA, Malette KM, Hammond C, Abdulla H, Entz A, et al. Clinical characteristics and morbidity associated with coronavirus disease 2019 in a series of patients in metropolitan Detroit. JAMA Netw Open. 2020;3:e2012270. doi: 10.1001/jamanetworkopen.2020.12270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Adams ML, Katz DL, Grandpre J. Updated estimates of chronic conditions affecting risk for complications from coronavirus disease, United States. Emerg Infect Dis. 2020;26:2172–5. doi: 10.3201/eid2609.202117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Vila-Córcoles Á, Ochoa-Gondar O, Torrente-Fraga C, Vila-Rovira Á, Satué-Gracia E, Hospital-Guardiola I, et al. Evaluación de la incidencia y perfil de riesgo de Covid-19 según comorbilidad previa en adultos ≥50 años del área de Tarragona. Rev Esp Salud Publica. 2020;94:e202006065. [PubMed] [Google Scholar]
- 76.Viner RM, Mytton OT, Bonell C, Melendez-Torres GJ, Ward J, Hudson L, et al. Susceptibility to SARS-CoV-2 infection among children and adolescents compared with adults: A systematic review and meta-analysis. JAMA Pediatr. 2020:e204573. doi: 10.1001/jamapediatrics.2020.4573 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Stein-Zamir C, Abramson N, Shoob H, Libal E, Bitan M, Cardash T, et al. A large COVID-19 outbreak in a high school 10 days after schools’ reopening, Israel, May 2020. Euro Surveill. 2020;25:2001352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Giorgi Rossi P, Marino M, Formisano D, Venturelli F, Vicentini M, Grilli R et al. Characteristics and outcomes of a cohort of COVID-19 patients in the province of Reggio Emilia, Italy. PLoS One. 2020;15:e0238281. doi: 10.1371/journal.pone.0238281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Buitrago-Garcia D, Egli-Gany D, Counotte MJ, Hossmann S, Imeri H, Ipekci AM, et al. Occurrence and transmission potential of asymptomatic and presymptomatic SARS-CoV-2 infections: A living systematic review and meta-analysis. PLoS Med. 2020;17:e1003346. doi: 10.1371/journal.pmed.1003346 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Jung CY, Park H, Kim DW, Choi YJ, Kim SW, Chang TI. Clinical characteristics of asymptomatic patients with COVID-19: A nationwide cohort study in South Korea. Int J Infect Dis. 2020;99:266–268. doi: 10.1016/j.ijid.2020.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Yanes-Lane M, Winters N, Fregonese F, Bastos M, Perlman-Arrow S, Campbell JR, et al. Proportion of asymptomatic infection among COVID-19 positive persons and their transmission potential: A systematic review and meta-analysis. PLoS One. 202015:e0241536. doi: 10.1371/journal.pone.0241536 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Amster R, Reychav I, McHaney R, Zhu L, Azuri J. Credibility of self-reported health parameters in elderly population. Prim Health Care Res Dev. 2020;21:e20. doi: 10.1017/S1463423620000201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Leong A, Cole J, Brenner LN, Meigs JB, Florez JC, Mercader JM. Cardiometabolic risk factors for COVID-19 susceptibility and severity: A Mendelian randomization analysis. medRxiv [Preprint]. 2020. Sep 1:2020.08.26.20182709. doi: 10.1101/2020.08.26.20182709 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Zhu Z, Hasegawa K, Ma B, Fujiogi M, Camargo CA Jr, Liang L. Association of obesity and its genetic predisposition with the risk of severe COVID-19: Analysis of population-based cohort data. Metabolism. 2020;112:154345. doi: 10.1016/j.metabol.2020.154345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Merzon E, Tworowski D, Gorohovski A, Vinker S, Golan Cohen A, Green I, et al. Low plasma 25(OH) vitamin D level is associated with increased risk of COVID-19 infection: an Israeli population-based study. FEBS J. 2020Jul23: doi: 10.1111/febs.15495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Gu T, Mack JA, Salvatore M, Sankar SP, Valley TS, Singh K, et al.COVID-19 outcomes, risk factors and associations by race: a comprehensive analysis using electronic health records data in Michigan Medicine. medRxiv [Preprint]. 2020. Jun 18:2020.06.16.20133140. doi: 10.1101/2020.06.16.20133140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Hamer M, Kivimäki M, Gale CR, Batty GD. Lifestyle risk factors, inflammatory mechanisms, and COVID-19 hospitalization: A community-based cohort study of 387,109 adults in UK. Brain Behav Immun. 2020;87:184–187. doi: 10.1016/j.bbi.2020.05.059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Estrela FM, Soares CFSE, Cruz MAD, Silva AFD, Santos JRL, Moreira TMO, et al. Covid-19 pandemic: reflecting vulnerabilities in the light of gender, race and class. Cien Saude Colet. 2020;25:3431–3436. doi: 10.1590/1413-81232020259.14052020 [DOI] [PubMed] [Google Scholar]
- 89.Farsalinos K, Barbouni A, Poulas K, Polosa R, Caponnetto P, Niaura R. Current smoking, former smoking, and adverse outcome among hospitalized COVID-19 patients: a systematic review and meta-analysis. Ther Adv Chronic Dis. 202025;11:2040622320935765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Usman MS, Siddiqi TJ, Khan MS, Patel UK, Shahid I, Ahmed J, et al. Is there a smoker’s paradox in COVID-19? BMJ Evid Based Med. 2020:bmjebm-2020-111492. [DOI] [PubMed] [Google Scholar]
- 91.Lemieux J, Siddle KJ, Shaw BM, Loreth C, Schaffner S, Gladden-Young A, et al. Phylogenetic analysis of SARS-CoV-2 in the Boston area highlights the role of recurrent importation and super-spreading events. medRxiv [Preprint]. 2020. Aug 25:2020.08.23.20178236. [Google Scholar]
- 92.Frieden TR, Lee CT. Identifying and interrupting super-spreading events-implications for control of severe acute respiratory syndrome coronavirus 2. Emerg Infect Dis. 2020;26:1059–1066. doi: 10.3201/eid2606.200495 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Sayampanathan AA, Heng CS, Pin PH, Pang J, Leong TY, Lee VJ. Infectivity of asymptomatic versus symptomatic COVID-19. Lancet. 2020;S0140-6736(20)32651-9. doi: 10.1016/S0140-6736(20)32651-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Ravindran B, Hogarth F, Williamson K, Wright R, Kirk M, Dalton C. High COVID-19 attack rate among attendees of wedding events in Bali, Indonesia, March 2020. Commun Dis Intell (2018). 2020;44. doi: 10.33321/cdi.2020.44.76 [DOI] [PubMed] [Google Scholar]
- 95.Park SY, Kim YM, Yi S, Lee S, Na BJ, Kim CB, et al. Coronavirus disease outbreak in call center, South Korea. Emerg Infect Dis. 2020;26:1666–1670. doi: 10.3201/eid2608.201274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Steinberg J, Kennedy ED, Basler C, Grant MP, Jacobs JR, Ortbahn D, et al. COVID-19 outbreak among employees at a meat processing facility—South Dakota, March-April 2020. MMWR Morb Mortal Wkly Rep. 2020;69:1015–1019. doi: 10.15585/mmwr.mm6931a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Agencia Estatal de Meteorología (AEMET). Ministerio de la Transición Ecológica y del Reto demográfico. España. Estación de Castellon-Almassora. Available from: http://www.aemet.es/es/serviciosclimaticos/datosclimatologicos/valoresclimatologicos.
- 98.Sajadi MM, Habibzadeh P, Vintzileos A, Shokouhi S, Miralles-Wilhelm F, Amoroso A. Temperature, humidity, and latitude analysis to estimate potential spread and seasonality of coronavirus disease 2019 (COVID-19). JAMA Netw Open. 2020;3:e2011834. doi: 10.1001/jamanetworkopen.2020.11834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Huang Z, Huang J, Gu Q, Du P, Liang H, Dong Q. Optimal temperature zone for the dispersal of COVID-19. Sci Total Environ. 2020;736:139487. doi: 10.1016/j.scitotenv.2020.139487 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Buonanno G, Morawska L, Stabile L. Quantitative assessment of the risk of airborne transmission of SARS-CoV-2 infection: Prospective and retrospective applications. Environ Int. 2020;145:106112. doi: 10.1016/j.envint.2020.106112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Hill AB. The environment and disease: association or causation? Proc R Soc Med 1965;58:295–300. [PMC free article] [PubMed] [Google Scholar]
- 102.Centers Disease Control and Prevention. Available from: https://www.cdc.gov/coronavirus/2019-ncov/community/large-events/considerations-for-events-gatherings.html.
- 103.Ghinai I, Woods S, Ritger KA, McPherson TD, Black SR, Sparrow L, et al. Community transmission of SARS-CoV-2 at two family gatherings—Chicago, Illinois, February-March 2020. MMWR Morb Mortal Wkly Rep. 2020;69:446–450. doi: 10.15585/mmwr.mm6915e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Furuse Y, Sando E, Tsuchiya N, Miyahara R, Yasuda I, Ko YK, et al. Clusters of coronavirus disease in communities, Japan, January-April 2020. Emerg Infect Dis. 2020; 26:2176–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Hu M, Lin H, Wang J, Xu C, Tatem AJ, Meng B, et al. The risk of COVID-19 transmission in train passengers: An epidemiological and modelling study. Clin Infect Dis. 2020:ciaa1057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Payne DC, Smith-Jeffcoat SE, Nowak G, Chukwuma U, Geibe JR, Hawkins RJ, et al. SARS-CoV-2 infections and serologic responses from a sample of U.S. Navy service members—USS Theodore Roosevelt, April 2020. MMWR Morb Mortal Wkly Rep. 2020;69:714–721. doi: 10.15585/mmwr.mm6923e4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Indenbaum V, Koren R, Katz-Likvornik S, Yitzchaki M, Halpern O, Regev-Yochay G, et al. Y. Testing IgG antibodies against the RBD of SARS-CoV-2 is sufficient and necessary for COVID-19 diagnosis. PLoS One. 2020;15:e0241164. doi: 10.1371/journal.pone.0241164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Limbachia J, Owens H, Matean M, Khan SS, Novak-Lauscher H, Ho K. Organizing a mass gathering amidst a rising COVID-19 public health crisis: Lessons learned from a Chinese public health forum in Vancouver, BC. Cureus. 2020;12:e12365. doi: 10.7759/cureus.12365 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Ebrahim SH, Ahmed Y, Alqahtani SA, Memish ZA. The Hajj pilgrimage during the COVID-19 pandemic in 2020: event hosting without the mass gathering. J Travel Med. 2021;28:taaa194. doi: 10.1093/jtm/taaa194 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Callaway D, Runge J, Mullen L, Rentz L, Staley K, Stanford M, et al. Risk and the Republican National Convention: Application of the novel COVID-19 operational risk assessment. Disaster Med Public Health Prep. 2021:1–6. doi: 10.1017/dmp.2020.499 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Sokhna C, Goumballa N, Hoang VT, Bassene H, Parola P, Gautret P. The Grand Magal of Touba was spared by the COVID-19 pandemic. Int J Infect Dis. 2021;105:470–471. doi: 10.1016/j.ijid.2021.01.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Furuse Y. Risk at mass-gathering events and the usefulness of complementary events during COVID-19 pandemic. J Infect. 2021;82:e20–e21. doi: 10.1016/j.jinf.2020.11.040 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Chadeau-Hyam M, Bodinier B, Elliott J, Whitaker MD, Tzoulaki I, Vermeulen R, et al. Risk factors for positive and negative COVID-19 tests: A cautious and in-depth analysis of UK biobank data. Int J Epidemiol. 2020;49:1454–1467. doi: 10.1093/ije/dyaa134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Wellinghausen N, Plonné D, Voss M, Ivanova R, Frodl R, Deininger S. SARS-CoV-2-IgG response is different in COVID-19 outpatients and asymptomatic contact persons. J Clin Virol. 2020;130:104542. doi: 10.1016/j.jcv.2020.104542 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Goumenou M, Sarigiannis D, Tsatsakis A, Anesti O, Docea AO, Petrakis D, et al. COVID-19 in Northern Italy: An integrative overview of factors possibly influencing the sharp increase of the outbreak (Review). Mol Med Rep. 2020;22:20–32. doi: 10.3892/mmr.2020.11079 [DOI] [PMC free article] [PubMed] [Google Scholar]