Abstract
Objective:
In stroke patients, extensive interventions for incidental thyroid nodules can be burdensome and costly. It appears that the risk of malignancy has not been reported in angiographically detected nodules and outcomes have not yet been described in patients, receiving acute stroke work-up.
Materials and Methods:
Incidental thyroid nodules were found on neck computerized tomography angiography or magnetic resonance angiography performed during inpatient stroke workup (January 2017 to September 2019). These patient cases were reviewed based on sonography reports, diagnosis, and follow-up care.
Results:
Of the 13 563 patients, 192 had incidental thyroid nodules (prevalence 1.4%). Twenty-six died from comorbidities and 22 received thyroid sonography. Twelve nodules from 10 patients had sonographic characteristics for biopsy: 10 benign, 1 indeterminate, and 1 papillary thyroid cancer (risk of malignancy: 8%). The cancer patient underwent hemithyroidectomy and is disease-free. Follow-up of the remaining patients showed no worsening or suspicious nodules. The American College of Radiology (ACR) guidelines would have prevented 8 unnecessary sonograms and 1 biopsy without missing malignancy.
Conclusion:
Although a small risk of malignancy was noted, 95% of patients undergoing additional diagnostic thyroid testing had clinically insignificant results. The ACR guidelines can prevent unnecessary interventions. Given the 14% mortality rate in the study cohort, it is proposed that a clinical evaluation of patients is important before undergoing further diagnostics, as comorbidities may be worse than a thyroid cancer.
Keywords: incidental, thyroid nodule, CT angiography, MRI angiography, stroke
Thyroid cancer incidence has increased dramatically in recent years,1 while death rates remain stable, suggesting increased detection of subclinical, indolent tumors.1 Incidental, or not clinically detected, thyroid nodules are present in up to 50% of the American population.2 About 90% of thyroid nodules are benign and 95% remain asymptomatic.3
Since 2015, multiple clinical trials in acute ischemic stroke were completed showing the benefits of endovascular thrombectomy, including up to 24 hours after onset.4,5 As a result, neck vascular imaging is recommended by clinical guidelines and implemented in clinical practice for patients presenting with acute stroke symptoms.6 During diagnostic neck vascular imaging, thyroid nodules are not a surprising finding. The utility of further diagnostic work-up for these nodules is unclear, especially since many of these patients have poor baseline health status. For example, patients with stroke are at risk for further disability after discharge and may face barriers to follow-up care.7 They can face an undue burden to pursue additional appointments and biopsies for thyroid nodules that may be clinically insignificant.
Two studies evaluating incidental findings on neck vascular imaging in patients with stroke have noted that thyroid nodules were the most common incidental finding,8,9 but provided no follow-up data or pathologic results. This study provides detailed follow-up information, including pathologic results, for incidental thyroid nodules seen in patients undergoing neck vascular imaging for stroke-like symptoms. These results should provide further evidence for clinical decision-making when managing patients, with unexpected diagnostic findings.
Materials and Methods
This was conducted based on a retrospective data collection at a single-center urban academic referral hospital’s IRB-approved registry. The data were pulled for patients admitted for acute stroke-like symptoms between January 2017 through September 2019. The researchers reviewed neck computerized tomography angiography (CTA) and magnetic resonance imaging angiography (MRA) reports for thyroid nodules. Patient demographics, medical history, clinical features, pathologic diagnosis, and follow-up were obtained from electronic medical records. Risk factors for thyroid carcinoma were recorded (childhood radiation exposure, family history of thyroid cancer, or hereditary cancer syndromes).3,10 All radiology images and reports with incidental thyroid nodules were manually reviewed by the study team to identify suspicious imaging findings (abnormal lymph nodes, extrathyroidal extension).11 All pathologic reports were reviewed by a board-certified cytopathologist. To include only new incidental nodules, it was important to exclude patients with clinical history of thyroid nodules, palpable neck masses, and symptomatic thyroid enlargement.
Results
Patient Population
The review identified 13 563 patients who received either neck CTAs or MRAs as part of their stroke workup between January 2017 through September 2019. Incidental thyroid nodules were found in 192 patients (prevalence 1.4%), all on CTA. Twenty-six patients (14%) subsequently died of causes unrelated to thyroid disease, preventing additional investigation. Figure 1 illustrates patient selection. Twenty-two patients (16 females, 6 males; mean age: 61 years, standard deviation ± 10 years) received subsequent sonograms. All requests for thyroid sonography included a request to perform biopsy if indicated. The characteristics of these patients are summarized in Table 1.
Figure 1.
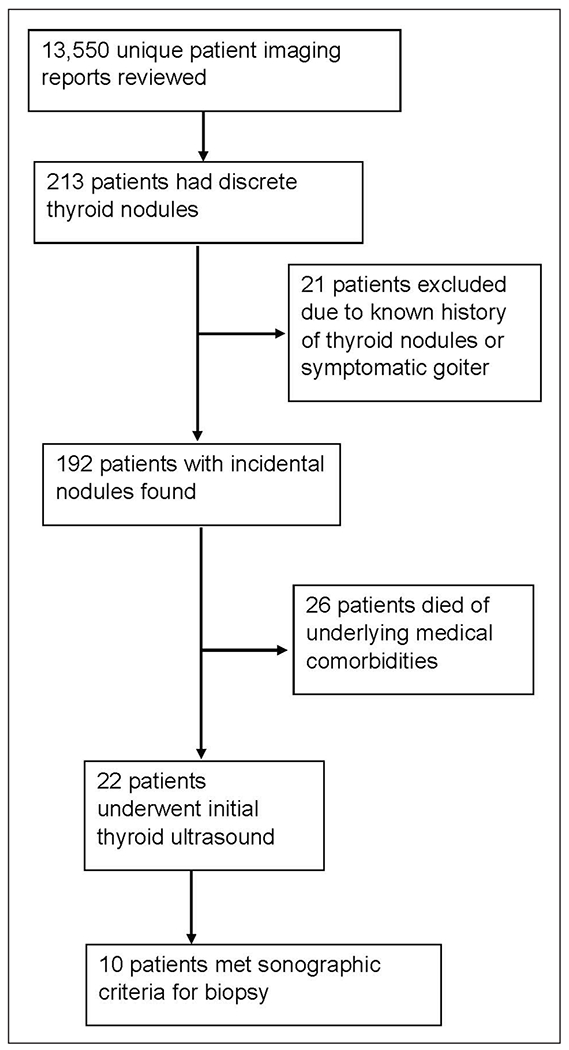
Flow diagram for selection of patient records that were reviewed in this study.
Table 1.
Characteristics of Patients Who Received Work-Up (n = 22).
| Age (mean ± SD) | 61 ± 10 |
| Sex | 16 F, 6 M |
| Nodule size (mean ± SD, [range]) | 1.5 cm ± 0.6, [0.3–3] |
| Patients who met imaging criteria for U/S | 14 |
| Patients who met sonographic criteria for FNA | 10 |
| Follow-up | Thyroid cancer: 1 No evidence of thyroid disease: 21 |
Abbreviations: F: female, FNA: fine needle aspiration, M: male, U/S: ultrasound.
Imaging Results
Of the 22 patients, CTA nodule size was 1.5 cm (standard deviation ± 0.6 cm, range: 0.3–3 cm). No suspicious imaging findings were identified, including abnormal lymph nodes and extrathyroidal extension. Based on American College of Radiology (ACR) size and age-based guidelines for non-suspicious nodules noted on CT, only 14 of the 22 patients met ACR criteria for follow-up sonogram.11
Ten of the 22 patients who received a follow-up sonogram had nodules with sonographic characteristics to merit fine-needle aspiration (FNA) biopsy, based on the Thyroid Imaging Reporting and Data System (TIRADS).12 Twelve nodules were biopsied (8 patients with 1 FNA, 2 patients with 2 FNAs).
Pathologic Findings and Diagnostic Follow-Up
FNA results are summarized in Table 2. There were 10 benign nodules, 1 indeterminate (follicular lesion of undetermined significance), and 1 papillary thyroid carcinoma, representing an 8% rate of malignancy for sampled nodules. The patient with indeterminate results opted for close clinical surveillance. The patient with malignant results underwent hemithyroidectomy with a final diagnosis of papillary thyroid carcinoma, classic type, 2.4 cm, confined to the thyroid (clinical stage II disease). However, his course was complicated by acute ischemic stroke 9 months later, apparently unrelated to cancer. He has no evidence of malignancy at 2-year follow-up. The diagnostic follow-up for the remaining patients showed asymptomatic thyroid nodules that are unchanged or diminishing in size.
Table 2.
Cytologic Results (n = 12 nodules).
| Benign | 10 |
| FLUS | 1 |
| Malignant | 1 |
| Rate of malignancy | 8% |
Abbreviation: FLUS: follicular lesion of undetermined significance.
Discussion
Based on a search of the literature, this study is the first to report clinical outcomes and risk of malignancy for incidental thyroid nodules noted in stroke work-up. Of 13 563 patients who had neck vascular imaging, only 192 patients had at least one incidental thyroid nodule (1.4% prevalence). Although prior studies have reported only prevalence of incidental thyroid nodules in stroke patients,8,9 this report also describe outcomes and includes all patients who undergoing neck vascular imaging, for acute stroke symptoms. Of 22 patients who received follow-up sonogram, 10 had at least one thyroid nodule that qualified for FNA biopsy, and only one had malignancy. Thus, 95% of this cohort of patients who received an additional sonogram, for incidentally detected CTA nodules, had clinically insignificant findings. These results may further aid clinicians in initial management of this patient population.
Incidental thyroid nodules have been reported in up to 18% of CT/MRI examination of the neck,11 with CT appearing to be more sensitive.8 Prevalence varies among studies: One reported 6% prevalence in stroke patients8 while another reported 0.6% prevalence in trauma patients.13 However, CT is not considered an appropriate diagnostic modality for thyroid disease, and concordance with dedicated thyroid sonogram is only 53%.2,11 Discrepancies include false positive nodule identification, missed lesions of 3–5 mm slices, and artifacts produced by patient positioning.2 Prevalence in CTA, as in this study, has only been sparsely described in the literature.8,9 It would appear that the risk of malignancy in CTA-detected nodules has not been previously reported. Nonetheless, this cohort’s malignancy rate of 8% falls within the reported range of 4–16% for nodules identified on chest and neck CT.2 Since this cohort’s rate of malignancy was calculated using only nodules that met TIRADS criteria for FNA, rate might be lower when one considers all CT-noted nodules.
Sonographic evaluation has been recommended for suspected thyroid nodules, although the 2015 American Thyroid Association guidelines acknowledge that sub-centimeter nodules generally do not need additional work-up.10 However, clinicians may need guidance for special populations of elderly patients or those with poor health status who may not benefit from extensive interventions. In 2015, the ACR white paper reported guidelines on work-up of CT or MRI detected incidental thyroid nodules.11 If no suspicious imaging findings (extrathyroidal extension, abnormal lymphadenopathy) are noted, suggested management is as follows:
For patients under 35 years of age, sonography is recommended if the nodule is at least 1.0 cm in size.
For patients 35 and older, sonography is recommended if the nodule is at least 1.5 cm.
Sonography is not recommended if the patient has limited life expectancy or severe comorbidities than are worse than thyroid disease itself.
Applying ACR guidelines to these study patients would have prevented 8 unnecessary thyroid sonograms and 1 unnecessary FNA. None of these patients would have had a missed malignant nodule. This report leaves evaluation of life expectancy and severe comorbidities up to clinician interpretation. Considering this cohort of patients, with incidental nodules, 14% died of severe medical comorbidities unrelated to thyroid disease. In this population, with poor health status, these patients were recommended thorough clinical evaluation to prevent unnecessary work-up. Perhaps, future clinical consensus guidelines may be helpful for more efficient work-up, especially in cases where size is difficult to ascertain.
The only malignancy was papillary thyroid carcinoma, detected during work-up for a patient diagnosed with a transient ischemic attack. The patient was 71 at the time of cancer diagnosis and subsequently suffered acute stroke less than a year after surgical treatment. It is unclear what impact thyroid cancer treatment had to his life expectancy and quality of life, if any. Multiple studies have shown incidental thyroid carcinoma shows less aggressive features, reduced recurrence, and longer progression-free survival when compared to clinically detected thyroid carcinoma.14,15 Papillary thyroid carcinoma, the most common incidental malignancy,14,15 has an excellent prognosis.16 Even untreated patients have an indolent course. Prior studies show 3 to 36% of autopsy patients have occult thyroid carcinoma with no complications in life.1,12,17,18 Studies from multiple countries have shown small papillary carcinomas can be managed with active surveillance alone, although this practice is not widespread in the United States.19 Remarkably, population-based research has demonstrated thyroid cancer incidence is positively correlated with density of endocrinologists18 and elevated socio-economic status16 and negatively correlated with percentage of uninsured patients.20 Most likely, increased access to care has led to what some have described as an “overdiagnosis” of cancer.18 With increasing incidence and excellent long-term survival, papillary thyroid carcinoma is costly to the health care system. Based on current trends, the projected cost is expected to surpass $3.5 billion by 2030, and the greatest cost is initial diagnosis and treatment.19 The initial cost includes sonographic evaluation, FNA biopsy, and surgery and adjuvant treatment. Reducing unnecessary testing and instead taking a more individualized and evidence-based approach would be beneficial for patients and the health care system.
Although the cost of a sonogram is minimal compared to the cost of surgery, there are still issues with indiscriminately ordering this evaluation for every incidental thyroid nodule. Even if the nodule does not meet criteria for FNA at the initial sonogram, the patient’s provider may elect to repeat sonography at an interval of 6–24 months. If a patient initially has benign cytology results, follow-up sonogram or repeat biopsy may be performed based on how concerning the imaging findings are.10 These extra appointments and procedures may be excessive for patients with disability and limited life expectancy due to severe medical comorbidities. Up to 30% of thyroid FNA biopsies are “indeterminate.”3 In this study, only one patient had indeterminate FNA results and opted for close clinical follow-up only. However, per current management guidelines, indeterminate nodules can receive significant additional procedures, including repeat FNA, molecular testing or even diagnostic lobectomy.10 Even though indeterminate nodules are most often benign on final pathology,3,19 all these additional procedures can lead to unnecessary post-surgical complications and health care costs. Just molecular testing alone costs $3000–$5000.3 These extra procedures and tests can pose serious implications if the initial ultrasound was not medically necessary in the first place.
Therefore, it is not necessary to perform sonography on every incidental thyroid nodule. Instead, it may be prudent to follow the ACR guidelines based on CT imaging characteristics, nodule size and patient age. These guidelines help identify patients who would most benefit from further evaluation. For example, prior studies of healthy adults have shown incidental thyroid nodules in younger patients are more likely to be malignant, so follow-up sonogram of smaller nodules is advised.11 Additionally, it may be important for patients to have a thorough baseline clinical evaluation, for those undergoing acute stroke work-up, given that the significant comorbidities that could dramatically shorten life expectancy.
The strength of this study is the large number of patients receiving neck vascular imaging for an acute stroke symptom work-up. This patient population, which was generally older and included other medical comorbidities, has not been well-reported in the literature. While most studies have focused solely on the prevalence of incidental thyroid nodules, this study also evaluated pathologic results and follow-up for all the thyroid nodules noted.
This work is limited by being a single-institution study, so clinical practice at the host hospital and therefore cannot be generalized. Additionally, these methods resulted in an older study population, so the results cannot be generalized to patients of all ages. Nonetheless, the intent was to show incidental thyroid nodule outcomes in a patient population that was unlikely to benefit from significant interventions. Further research, including large, multi-institutional studies, could shed light on widespread clinical practice.
Conclusion
This study was based on the review of incidental thyroid nodules, in patients undergoing acute stroke work-up and is a population that has not been routinely evaluated. It was noted that over 90% of patients with incidental thyroid nodules did not benefit from additional interventions, including sonography and biopsy. These results would suggest a more individualized approach based on nodule size, presence or absence of imaging findings concerning for malignancy, and ruling out significant comorbidities that would shorten life expectancy more than occult thyroid carcinoma itself.
Acknowledgment
The authors would like to thank Adarsh Velagapudi for assistance in data collection.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Research reported was supported by the National Center for Advancing Translational Sciences of the National Institutes of Health under award number UL1TR003096. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Footnotes
Declaration of Conflicting Interests
The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: Dr. Lin is on the scientific advisory board of Proteocyte AI. The other authors have nothing to disclose.
Statement of Ethics
This retrospective chart review study involving human participants was in accordance with the ethical standards of the institutional and national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. The Human Investigation Committee (IRB) of our institution approved this study. Informed consent was waived as this was a retrospective study and all procedures were performed as part of routine patient care.
References
- 1.Davies L, Morris LG, Haymart M, et al. : American association of clinical endocrinologists and American college of endocrinology disease state clinical review: the increasing incidence of thyroid cancer. Endocr Pract 2015;21(6):686–696. doi: 10.4158/EP14466.DSCR. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wilhelm S: Evaluation of thyroid incidentaloma. Surg Clin North Am 2014;94(3):485–497. doi: 10.1016/j.suc.2014.02.004. [DOI] [PubMed] [Google Scholar]
- 3.Durante C, Grani G, Lamartina L, Filetti S, Mandel SJ, Cooper DS: The diagnosis and management of thyroid nodules: a review. JAMA 2018;319(9):914–924. doi: 10.1001/jama.2018.0898. [DOI] [PubMed] [Google Scholar]
- 4.Goyal M, Menon BK, van Zwam WH, et al. : Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. The Lancet 2016;387(10029):1723–1731. doi: 10.1016/S0140-6736(16)00163-X. [DOI] [PubMed] [Google Scholar]
- 5.Nogueira RG, Jadhav AP, Haussen DC, et al. : Thrombectomy 6 to 24 hours after stroke with a mismatch between deficit and infarct. N Engl J Med 2017;378(1):11–21. doi: 10.1056/NEJMoa1706442. [DOI] [PubMed] [Google Scholar]
- 6.Powers WJ, Rabinstein AA, Ackerson T, et al. : Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 2019;50(12):e344–e418. doi: 10.1161/STR.0000000000000211. [DOI] [PubMed] [Google Scholar]
- 7.Kitzman P, Hudson K, Sylvia V, Feltner F, Lovins J: Care coordination for community transitions for individuals post-stroke returning to low-resource rural communities. J Community Health 2017;42(3):565–572. doi: 10.1007/s10900-016-0289-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Doyle SJ, George BP, Holloway RG, Kelly AG: Incidental findings in radiographic imaging for in patients with acute ischemic stroke. J Stroke Cerebrovasc Dis 2018;27(11):3131–3136. doi: 10.1016/j.jstrokecerebrovasdis.2018.07.003. [DOI] [PubMed] [Google Scholar]
- 9.Rositzka M, Hoffmann KT, Meyer HJ, Surov A: Incidental findings on CT angiography of the head and neck in stroke patients. Evaluation of frequency and detection rate. Clin Neurol Neurosurg 2020;193:105783. doi: 10.1016/j.clineuro.2020.105783. [DOI] [PubMed] [Google Scholar]
- 10.Haugen BR, Alexander EK, Bible KC, et al. : 2015 American Thyroid Association management guidelines for adult patients with thyroid nodules and differentiated thyroid cancer: the American Thyroid Association guidelines task force on thyroid nodules and differentiated thyroid cancer. Thyroid 2016;26(1):1–133. doi: 10.1089/thy.2015.0020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Hoang JK, Langer JE, Middleton WD, et al. : Managing incidental thyroid nodules detected on imaging: white paper of the ACR Incidental Thyroid Findings Committee. J Am Coll Radiol 2015;12(2):143–150. doi: 10.1016/j.jacr.2014.09.038. [DOI] [PubMed] [Google Scholar]
- 12.Grant EG, Tessler FN, Hoang JK, et al. : Thyroid ultrasound reporting lexicon: white paper of the ACR Thyroid Imaging, Reporting and Data System (TIRADS) Committee. J Am Coll Radiol 2015;12(12 Pt A):1272–1279. doi: 10.1016/j.jacr.2015.07.011. [DOI] [PubMed] [Google Scholar]
- 13.Sierink JC, Saltzherr TP, Russchen MJ, et al. : Incidental findings on total-body CT scans in trauma patients. Injury 2014;45(5):840–844. doi: 10.1016/j.injury.2013.10.009. [DOI] [PubMed] [Google Scholar]
- 14.Evranos B, Polat SB, Cuhaci FN, et al. : A cancer of undetermined significance: incidental thyroid carcinoma. Diagn Cytopathol 2019;47(5):412–416. doi: 10.1002/dc.24117. [DOI] [PubMed] [Google Scholar]
- 15.González-Sánchez-Migallón E, Flores-Pastor B, Pérez-Guarinos CV, et al. : Incidental versus non-incidental thyroid carcinoma: clinical presentation, surgical management and prognosis. Endocrinol Nutr 2016;63(9):475–481. doi: 10.1016/j.endoen.2016.10.008. [DOI] [PubMed] [Google Scholar]
- 16.Altekruse S, Das A, Cho H, Petkov V, Yu M: Do US thyroid cancer incidence rates increase with socioeconomic status among people with health insurance? an observational study using SEER population-based data. BMJ Open 2015;5(12):e009843. doi: 10.1136/bmjopen-2015-009843. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Li N, Du XL, Reitzel LR, Xu L, Sturgis EM: Impact of enhanced detection on the increase in thyroid cancer incidence in the United States: review of incidence trends by socioeconomic status within the surveillance, epidemiology, and end results registry, 1980-2008. Thyroid 2013;23(1):103–110. doi: 10.1089/thy.2012.0392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Udelsman R, Zhang Y: The epidemic of thyroid cancer in the United States: the role of endocrinologists and ultrasounds. Thyroid 2014;24(3):472–479. doi: 10.1089/thy.2013.0257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hoang JK, Nguyen XV: Understanding the risks and harms of management of incidental thyroid nodules: a review. JAMA Otolaryngol Head Neck Surg 2017;143(7):718–724. doi: 10.1001/jamaoto.2017.0003. [DOI] [PubMed] [Google Scholar]
- 20.Morris LG, Sikora AG, Tosteson TD, Davies L: The increasing incidence of thyroid cancer: the influence of access to care. Thyroid 2013;23(7):885–891. doi: 10.1089/thy.2013.0045. [DOI] [PMC free article] [PubMed] [Google Scholar]


