Abstract
The COVID-19 pandemic may have a compounding effect on the substance use of American veterans with posttraumatic stress disorder (PTSD). This study investigated the relationship between PTSD and current reactions to COVID-19 on alcohol and cannabis use among veterans who completed a survey 1 month prior to the pandemic in the USA and a 6-month follow-up survey. We hypothesized that veterans with PTSD would experience more negative reactions to COVID-19 and increased alcohol and cannabis use behaviors over those without PTSD. Veterans with PTSD prior to the pandemic, relative to those without, endorsed poorer reactions, greater frequency of alcohol use, and greater cannabis initiation and use during the pandemic. Veterans with PTSD may use substances to manage COVID-related stress. Clinicians may see an increase in substance use among this group during and after the pandemic and may need to implement specific behavioral interventions to mitigate the negative effects of COVID-19.
Keywords: COVID-19, Posttraumatic stress disorder, Veterans, Alcohol, Cannabis
The COVID-19 pandemic has had considerable implications for behavioral health on a global scale, with current research reporting poor outcomes in terms of mental health symptomology and substance use within the general population (Ettman et al., 2020; Gallagher et al., 2020; Pollard et al., 2020; Rajkumar, 2020; Rogers et al., 2020). Current research reveals heightened feelings of anxiety, distress, and traumatic stress among adults during the pandemic (Gallagher et al., 2020; Liu et al., 2020; Rajkumar, 2020). Several pandemic-related factors are thought to contribute to the observed rises in mental health symptomology, including fear of COVID-19, economic hardship, loneliness, and social isolation (Fitzpatrick et al., 2020; Horigian et al., 2020; McGinty et al., 2020; Witteveen & Velthorst, 2020). In addition to mental health concerns, substance use is concerning during the pandemic, and research has reported increases in use and initiation of substance use during COVID-19 (Rogers et al., 2020), with particular increases in alcohol use among adults compared to other substances (Pollard et al., 2020; Sharma et al., 2020; Vanderbruggen et al., 2020). Results regarding changes in cannabis use have been more mixed, with some reporting increases in use and other reporting decreases or no change in use (Sharma et al., 2020; Vanderbruggen et al., 2020).
Of great concern is addressing populations with pre-pandemic behavioral health conditions as these conditions may amplify adverse changes in substance use behaviors and mental health during the pandemic (Alonzi et al., 2020; Horigian et al., 2020; Kim et al., 2020). For example, those already struggling with posttraumatic stress disorder (PTSD) may react differently to the global stress that surrounds the pandemic and, further, may resort to increased substance use behaviors, the latter of which may be used as a means to cope with the added stress of the pandemic or the exacerbation of symptoms (Rogers et al., 2020). Increases in substance use behaviors have been observed as coping reactions to stressful life events (Hyman & Sinha, 2009; Kevorkian et al., 2015; Werner et al., 2016). Thus, for those with PTSD, additional stressful events could exacerbate pre-existing symptoms and make coping with the new stressors more difficult or perhaps lead to maladaptive coping behaviors (Evans et al., 2013; Green et al., 2010).
There is an urgent need to understand if, and how, the COVID-19 pandemic has influenced behavioral health outcomes among at-risk groups, such as American veterans. Prior work notes that, veterans report rates of PTSD ranging from 11 to 30% and are at heightened risk for problematic substance use (Dursa et al., 2014; Gradus, 2014; Lapierre et al., 2007; Teeters et al., 2017). American veterans who report PTSD prior to the pandemic may be at heightened risk for exacerbated substance use as well as more negative reactions to the pandemic. Yet, little is known regarding veterans’ ability to manage substance use, PTSD symptomology, and COVID-specific stressors. Such work is needed to inform clinical and outreach efforts in the post-pandemic period. Currently, studies with veterans that include a pre-pandemic time point are limited, making it difficult to draw conclusions about changes in substance use behaviors over time for veterans.
The Present Study
The overall purpose of this study was to examine veterans’ reactions to COVID-19 and substance use patterns, with particular attention to those who screened positive for PTSD prior to the pandemic. More specifically, in February 2020 (Time 1), approximately 1 month prior to the Trump administration’s declaration of a national emergency in the USA (AJMC, 2020), we conducted a survey of veteran substance use behaviors and PTSD symptoms. Six months later, in August 2020 (Time 2), we conducted a follow-up survey with veterans to assess their substance use behaviors, PTSD symptoms, and reactions to COVID-19. First, we sought to examine veterans’ reactions to the pandemic, including emotions (e.g., anxiety, depression), behaviors (e.g., sleep problems), stress (e.g., financial), and family and social relationships. We hypothesized that veterans would report poorer reactions as the course of the pandemic progressed. Second, we sought to examine changes in substance use from Time 1 to Time 2. We expected drinking and cannabis use to either stay approximately the same or increase due to stress related to the pandemic. Third, we examined whether veterans who screened positive for PTSD at Time 1 reported poorer reactions to the pandemic and more substance use at Time 2 compared to those who did not screen positive, hypothesizing that veterans with positive PTSD screens would report poorer outcomes. Lastly, we assessed if reactions to COVID-19 during the course of the pandemic moderated the association between PTSD and substance use, hypothesizing that those with poorer reactions to COVID-19 and who screened positive for PTSD would report greater substance use.
Methods
Participants and Procedures
In February 2020, participants were recruited via social media ad campaigns for a study on “veteran attitudes and behaviors” as part of a survey effort to examine drinking and mental health symptoms among a sample of young adult veterans recruited outside of VA settings. The purpose of the larger study was to learn more about recently discharged veterans’ mental health and substance use behaviors to inform future intervention content. Eligibility criteria were (1) age 18 to 40 and (2) separation from the Air Force, Army, Marine Corps, or Navy. Participants were excluded if they were active duty or in the reserve or guard components of the US armed forces. Ads were displayed on Facebook, Instagram, and veteran-specific social media sites (RallyPoint, We Are The Mighty) for 8 days. Veterans were directed to a secure study website that hosted an online consent form and survey. Once consented, participants completed a 30-minute online survey and received a $20 Amazon gift card.
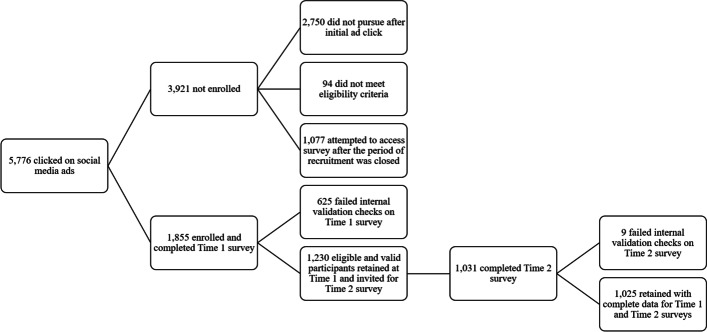
The flow of recruitment and retention of the sample can be found in Fig. 1. In total, 5,776 individuals clicked on ads and reached the online consent form, of which 2,750 (48%) did not pursue participation. An additional 94 (2%) were screened and found to be ineligible (i.e., over age 40, not a US veteran), and 1,077 (19%) attempted to access the study once we had reached an IRB-approved quota to prevent new participants from filling out the survey. The remaining 1,855 individuals (32%) consented and completed the survey. Of those, 625 (34%) failed internal validation checks, such as not endorsing consistent responses between items (e.g., rank, branch, and paygrade needed to match), completing the survey in an impossible amount of time, completing the survey more than once (e.g., reviewing IP addresses for duplicates), or failing to answer test items correctly that assessed for careless responding (e.g., asking participants to endorse a specific value to check for attention).
Fig. 1.
Flow of participant recruitment
In August 2020, 6 months after the first survey, the 1,230 participants that completed the February 2020 survey (Time 1) were sent an email invitation to complete a 30-minute follow-up survey (Time 2) about “their experiences and reactions to COVID-19.” Of these, 1,031 consented to the study and completed the Time 2 survey (84% of the final Time 1 sample). Nine participants failed internal validation checks and were removed from the Time 2 sample, leaving a sample of 1,025 that completed both surveys.
Measures
Demographics and Military Characteristics
Participants reported on their age, race/ethnicity, gender, and branch of service. Participants also filled out a measure of combat exposure using 11 items from prior work with veterans (e.g., witnessing an accident resulting in serious injury or death; engaging in hand-to-hand combat; Schell & Marshall, 2008) and an additional item of ever feeling like they were in great danger of being killed. Participants responded to each of the 12 items with Yes or No, and participants with any Yes response were coded as having combat exposure.
Reactions to COVID
On the Time 2 survey, we included 13 items modified from prior work (JHSPH, 2020) related to emotional, stress, sleep, and relationship reactions to the pandemic. Participants were asked to rate the 13 items from 0 “not at all” to 4 “a great deal” for two separate time periods of the first 3 months of the pandemic in the USA (March, April, May 2020) and the past 3 months (June, July, August 2020). In the effort to create a composite score for each time period, we used an exploratory factor analysis and concluded the items fell into a single factor at each time period. We then dropped four items from the scale with a factor loading of less than 0.35. This gave us a 9-item scale. These nine items fit the data well (CFI = 0.97, RMSEA = 0.02, SRMR = 0.02 for the first 3 months; CFI = 0.97, RMSEA = 0.03, SRMR = 0.02 for the past 3 months). We took the mean of the 9 items at each time period to create a composite score.
Posttraumatic Stress Disorder
PTSD symptom severity at Time 1 was assessed using the 20-item Posttraumatic Stress Disorder Checklist for DSM-V (PCL-5; (Bovin et al., 2016), where participants indicated how bothered they were by 20 symptoms of PTSD in the past month in relation to a stressful experience (e.g., natural disaster, combat, sexual assault) from not at all (0) to extremely (4). The PCL-5 yields a total sum score from 0 to 80 and was reliable in the current sample (α = 0.96). Using the cutoff score of 33 (Bovin et al., 2016), participants who scored at or above were classified with a positive screen for possible PTSD at Time 1.
Substance Use
At Time 1 and Time 2, participants completed items for past 30-day alcohol use: days of any alcohol use, days of alcohol use with binge drinking (i.e., 4 or more drinks on a drinking occasion for females, 5 or more drinks for males), number of drinks consumed on a typical drinking occasion, and the number of drinks consumed on the occasion when the participant drank the most (max drinks). At Time 1, participants reported whether or not they had used cannabis in their lifetime, and if so, they were asked how many days in the past 30 days they had used cannabis in any form (e.g., smoking, vaping, edibles). At Time 2, participants reported on any cannabis use in the past 6 months (since the Time 1 survey), and if they reported any use, they indicated how many days in the past 30 days they used cannabis.
Analytic Plan
The analytic plan was guided by the four aims of the paper. First, we used paired samples t-tests to compare means of the reactions to COVID-19 measure during the first 3 month of the pandemic (March to May 2020) to the past 3 months of the pandemic (June to August 2020). We report Cohen’s d effect sizes (Cohen, 1992) to describe the relative magnitude of change. We then used paired samples t-tests to compare means for past 30-day substance use outcomes: drinking days and binge drinking days for all participants, average drinks and max drinks per occasion for past 30 day drinkers, and cannabis use frequency among all participants and among cannabis users only (i.e., those who reported any cannabis use at either time point). A chi-square test was used to examine whether lifetime cannabis non-users at Time 1 began using cannabis during the past 6 months of the pandemic at Time 2. Third, we used logistic and linear regression models that controlled for demographic and military characteristics to examine if individuals who screened positive for PTSD at Time 1 reported greater substance use at Time 2 compared to those without a positive PTSD screen. Lastly, we ran a series of linear regression models with each of the reactions to COVID-19 composite scores separately (i.e., first 3 months and then past 3 months of the pandemic) to determine if poorer reactions moderated the relationship between PTSD and substance use and explored whether those moderators varied by substance or time period. Significant interactions were plotted for interpretation using +1 and −1 standard deviations from the mean for all continuous measures. All continuous variables were grand mean centered to facilitate interpretation.
Results
Sample Description
Table 1 contains a description of the sample. Participants reported a mean age of 34.6 (SD = 3.5), and the majority were white (82.9%) and male gender (89.5%). Most participants were veterans of the Army (70.4%), and nearly all had experienced some combat (96.1%). Nearly one-third met criteria for possible PTSD (31.2%).
Table 1.
Sample description
| All participants (N = 1,025) | |
|---|---|
| M (SD) or N (%) | |
| Age | 34.6 (3.51) |
| Race/ethnicity | |
| Hispanic/Latinx | 90 (8.8%) |
| Black/African American | 62 (6.0%) |
| Asian | 12 (1.2%) |
| White | 850 (82.9%) |
| Multiracial/other | 11 (1.1%) |
| Gender | |
| Men | 917 (89.5%) |
| Women | 96 (9.3%) |
| Other | 12 (1.2%) |
| Branch | |
| Air Force | 123 (12.0%) |
| Army | 722 (70.4%) |
| Marine Corps | 94 (9.2%) |
| Navy | 86 (8.4%) |
| Combat exposure | |
| Any combat exposure | 985 (96.1%) |
| Combat severity | 5.05 (2.13) |
| PTSD | |
| PCL-5 positive screen | 320 (31.2%) |
| PCL-5 severity score | 21.60 (15.35) |
Note: PTSD posttraumatic stress disorder, PCL-5 posttraumatic stress disorder checklist for DSM-5
Reactions to COVID-19
Individual means for each of the reactions to COVID-19 items are included in Table 2. During the months of June through August 2020 (past 3 months of the pandemic), participants reported higher means for the reactions to COVID-19 composite, as well as for the individual items, compared to the first 3 months of pandemic (March to May 2020), with effects sizes ranging from 0.18 to 0.55 (see Table 2). Participants who screened positive for PTSD at Time 1 reported significantly higher composite scores on the reactions to COVID-19 measure for the first 3 months of the pandemic (M = 1.30, SD = 0.48) compared to those who did not screen positive for PTSD (M = 0.99, SD = 0.40), t (1020) = 10.91, p < .001; Cohen’s d = 0.73). Participants who screened positive for PTSD at Time 1 also reported significantly higher composite scores on the reactions to COVID-19 measure for the past 3 months of the pandemic (M = 1.73, SD = 0.66) compared to those who did not screen positive for PTSD (M = 1.21, SD = 0.54), t (1020) = 12.42, p < .001; Cohen’s d = 0.89).
Table 2.
Means and standard deviations of individual reactions to COVID items for the first 3 and past 3 months of the pandemic
| How often did you feel the following ways when thinking about your experience with the coronavirus (COVID-19) pandemic | First 3 months of the pandemic (March, April, May 2020) | Past 3 months of the pandemic (June, July, August 2020) | Standardized difference (Cohen’s d [95%CI]) |
|---|---|---|---|
| Feel nervous, anxious, or on edge | 1.08 (0.84) | 1.42 (1.09) | 0.35 [0.26, 0.43] |
| Feel depressed | 1.05 (0.88) | 1.36 (1.11) | 0.30 [0.22, 0.39] |
| Feel lonely | 1.07 (0.87) | 1.34 (1.14) | 0.26 [0.18, 0.34] |
| Sleep less than typical | 1.02 (0.85) | 1.37 (1.12) | 0.34 [0.26, 0.43] |
| Have physical reactions, such as sweating, trouble breathing, nausea, or a pounding heart | 1.00 (0.85) | 1.27 (1.12) | 0.26 [0.19, 0.35] |
| Was stressed by the restrictions on leaving home | 1.14 (0.91) | 1.47 (1.17) | 0.31 [0.23, 0.39] |
| Feel that your family relationships were suffering | 1.06 (0.87) | 1.31 (1.11) | 0.25 [0.17, 0.33] |
| Feel that your social relationships were suffering | 1.10 (0.88) | 1.34 (1.14) | 0.23 [0.15, 0.32] |
| Was stressed about finances | 1.15 (0.95) | 1.49 (1.20) | 0.18 [0.10, 0.26] |
| Mean of 9 items | 1.07 (0.45) | 1.37 (0.63) | 0.55 [0.47, 0.62] |
Note: Higher mean reflects “poorer” COVID-related reactions. Means reflect response options of 1 (a little bit) and 2 (a moderate amount) on a scale from 0 to 4
Substance Use
Alcohol Use
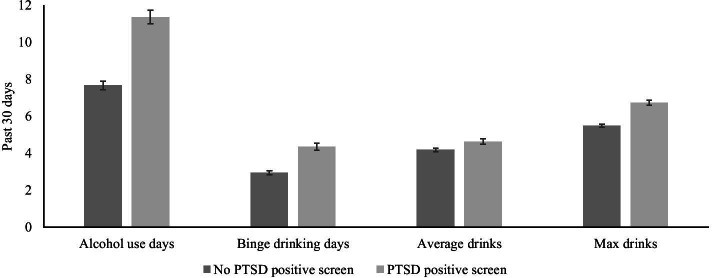
Means and standard deviations for alcohol use outcomes are presented in Table 3. Participants reported significantly decreasing their drinking days and binge drinking days. Past 30 days drinkers significantly decreased their average drinks per occasion and max drinks on one occasion. In Fig. 2, we display the estimated marginal means for Time 2 alcohol use outcomes by PTSD screening status at Time 1. Across all four alcohol outcomes, those who screened for PTSD at Time 1 reported greater alcohol use at Time 2 after controlling for age, race/ethnicity, combat severity, and the Time 1 alcohol use outcome: drinking days (β = 3.70, SE = 0.46, p < .001; b = 0.28), binge drinking days (β= 1.41, SE = 0.24, p < .001; b = 0.21), average drinks (β= 0.45, SE = 0.19, p = 0.018; b = 0.09), and max drinks on one occasion (β= 1.25, SE = 0.18, p < .001; b = 0.27). Using the standard effects for drinking days as an example, we can see that veterans with PTSD reported approximately 0.28 standard deviations (or ~28%) greater drinking days at Time 2 compared to veterans who did not screen for PTSD.
Table 3.
Changes in substance use outcomes from Time 1 to Time 2
| Substance use |
Time 1 Mean (SD)/N (%) |
Time 2 Mean (SD)/N (%) |
t (df)/ X2 (df) | p-value |
|---|---|---|---|---|
| Alcohol use days (past 30 days) | 11.37 (5.21) | 8.82 (6.05) | 12.32 (1024) | < 0.001 |
| Binge drinking days (past 30 days) | 5.09 (3.61) | 3.39 (3.14) | 15.27 (1024) | < 0.001 |
| Average drinks per occasion (past 30 days)a | 5.59 (2.56) | 4.32 (2.20) | 14.23 (977) | < 0.001 |
| Max drinks on one occasion (past 30 days)a | 7.77 (2.84) | 5.88 (2.11) | 20.54 (977) | < 0.001 |
| Any cannabis use (lifetime) | 200 (19.5%) | 314 (30.7%) | 220.59 (1, 1024) | < 0.001 |
| Cannabis use days among full sample (past 30 days) | 1.12 (3.74) | 1.23 (3.81) | 0.99 (1024) | 0.323 |
| Cannabis use days among lifetime users (past 30 days)b | 3.67 (6.04) | 4.02 (6.01) | 0.98 (313) | 0.322 |
Note: aAmong past 30-day drinkers only. bAmong lifetime cannabis users only
Fig. 2.
Past 30-day alcohol outcomes at time 2 by Time 1 PTSD status. Note. Figure contains estimated marginal means and 95% confidence intervals. PTSD posttraumatic stress disorder. Models controlled for age, race/ethnicity, gender, combat severity, and the Time 1 outcome
Cannabis Use
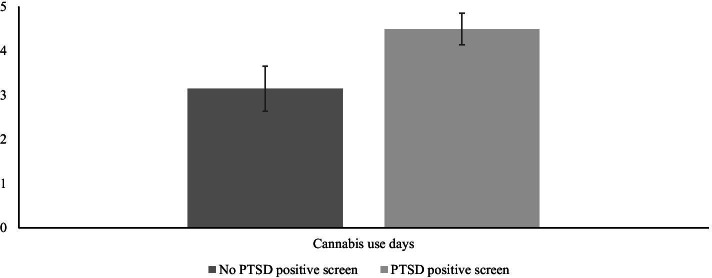
Among the full sample, 19.5% of participants (n = 200) at Time 1 reported any use of cannabis in their lifetime, while at Time 2, 23.5% of the sample (n = 241) reported use during the past 6 months. Nearly 14% of those who reported no lifetime use of cannabis at Time 1 reported use of cannabis within the past 6 months at Time 2 (see Table 3). There were no significant differences in the mean number of cannabis days from Time 1 to Time 2 for all participants and for lifetime users. For the full sample, a positive PTSD screen at Time 1 was associated with a 3.82 (95% CI [2.45, 5.95]) greater odds (or ~282% increase) of using cannabis in the past 6 months at Time 2, after controlling for age, race/ethnicity, combat severity, and lifetime cannabis use. For those who reported cannabis use at either time point (n = 314), a positive PTSD screen at Time 1 was associated with greater frequency of cannabis use (β= 1.35, SE = 0.65, p = .040; b = 0.11) at Time 2 (see Fig. 3).
Fig. 3.
Cannabis outcome at Time 2 for lifetime cannabis users by time 1 PTSD status. Note. Figure contains estimated marginal means and 95% confidence intervals. PTSD posttraumatic stress disorder. Models controlled for age, race/ethnicity, gender, combat severity, and the Time 1 outcome. Cannabis use days are days in the past 30 days
PTSD and Reactions to COVID-19 Interactions
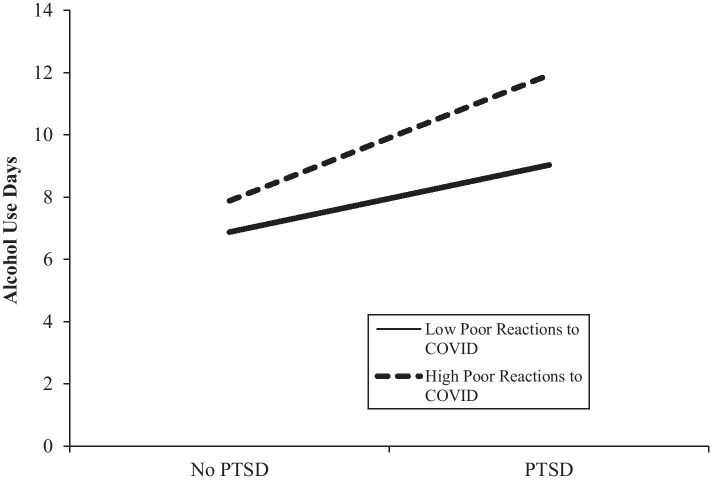
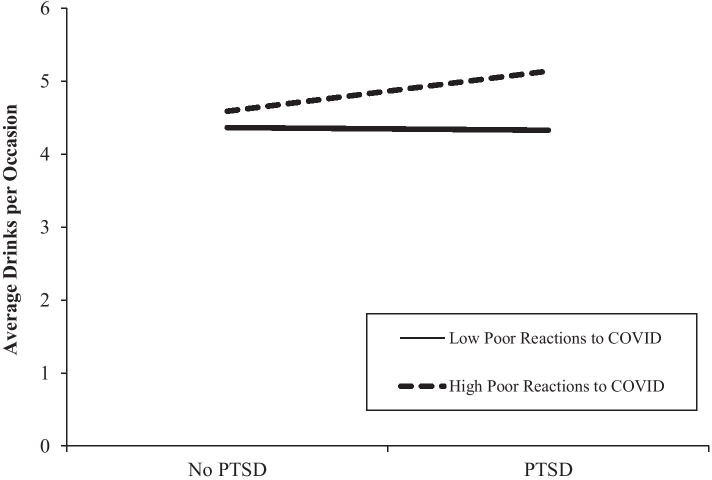
In the models for number of past month drinking days, there was a significant interaction for PTSD and reactions to COVID-19 in the first 3 months of the pandemic, such that those who screened positive for PTSD and reported high (+1 SD) poor reactions to COVID-19 reported drinking the most frequently (see Fig. 4). This difference resulted in over three additional alcohol use days for those with PTSD and high poor reactions to COVID compared to veterans who also screened for PTSD but reported relatively low poor reactions to COVID-19. Simple slopes analyses revealed significant slopes for both high (slope gradient = 4.05, t = 7.53, p < 0.001) and low poor reactions to the pandemic (slope gradient = 2.15, t = 3.39, p = 0.001), with a steeper slope for those with higher poor reactions. There was no interaction effect for the past 3 months of the pandemic. Similarly, in the models for average drinks per occasion, there was a significant interaction for PTSD and reactions to COVID-19 in the first 3 months of the pandemic, such that those who screened positive for PTSD reported drinking the most number of drinks if they also reported experiencing higher poor reactions to COVID-19 (see Fig. 5). Simple slopes analyses revealed a significant slope for higher poor reactions to the pandemic (slope gradient = 0.55, t = 2.49, p = 0.013) but not lower poor reactions to the pandemic (p = 0.888). Again, there was no interaction effect for the past three months of the pandemic. There were no significant interactions for binge drinking days, max drinks, or cannabis use days.
Fig. 4.
Interaction plot for PTSD and poor reactions to COVID during the first 3 months of the pandemic for alcohol use days outcomes
Fig. 5.
Interaction plot for PTSD and poor reactions to COVID during the first 3 months of the pandemic for average drinks per occasion outcome
Discussion
In this study, we assessed how American veterans, a group at-risk for experiencing PTSD prior to the pandemic, fared in terms of their reactions to the pandemic and substance use behaviors during the initial months after COVID-19 was declared a national emergency in the USA. In a sample of 1,025 veterans, participants reported increasingly poorer reactions throughout the first 6 months of the pandemic, including greater feelings of anxiety; depression; and stress, less sleep than typical, and suffering of family and social relationships. Those veterans screening positive for PTSD prior to the pandemic reported poorer reactions to COVID-19 than those without positive PTSD screens. This fits with prior literature from multiple countries, including studies in North America, Europe, Australia, and Asia, demonstrating that individuals with pre-existing mental health conditions may have a harder time coping with the pandemic (Alonzi et al., 2020; Ettman et al., 2020; Neill et al., 2020; Rajkumar, 2020; Varga et al., 2021; Wardell et al., 2020). In our study, poor reactions to the pandemic tended to increase from the first 3 months to the next 3 months of the initial outbreak in the USA; thus, it will be important to assess veterans for increased poor reactions as the pandemic continues to help inform prevention and intervention efforts with this group.
Regarding substance use, veterans generally reported lower drinking levels from pre-pandemic levels. This is inconsistent with prior work in the general global population, as studies have generally found significant increases in drinking, although these increases have tended to be small (e.g., average increase of less than 0.2 days of binge drinking in Pollard et al. 2020) or based on cross-sectional retrospective reports (e.g., asking participants if their drinking changed over the pandemic rather than assessing at a pre-pandemic time point as in Kilian et al., 2021). Given the stay-at-home orders in many US states, it may be that American veterans were drinking less due to limited social engagement with friends outside their homes, such as in bars or at sporting events. However, consistent with the idea that individuals may use alcohol to cope with pre-pandemic mental health problems, veterans who screened positive for PTSD prior to the pandemic reported greater frequency (overall days, binge drinking days) and quantity (average amount, maximum amount on one occasion) of alcohol use than those veterans without positive PTSD screens. Though we did not assess reasons for veterans’ use of substances, prior work has shown an increase in using substances to cope with pandemic stressors (Czeisler et al., 2020; Ornell et al., 2020).
For cannabis use, an interesting pattern emerged. First, there was no significant increase in days of cannabis use, which fits with some prior work of American and Belgian adults during the first few months of the pandemic (Sharma et al., 2020; Vanderbruggen et al., 2020). However, a substantial proportion of veterans in our study (14%) who had never used cannabis (i.e., no lifetime use at Time 1) reported using cannabis use during the first 6 months of the pandemic. Veterans may have begun using cannabis during the pandemic simply due to availability; cannabis has become increasingly more available for recreational sale and possession, and multiple states determined that cannabis outlets could remain open during the lockdown, with reports of increased sales during the first 3 months of 2020 (Groshkova et al., 2020). Alternatively, for veterans with PTSD, motives for cannabis use have been associated with enjoyment, coping, and use as a sleep aid (Metrik et al., 2018; Metrik et al., 2016); and given the pandemic’s effect on bars closing, stay-at-home orders, and social distancing, some veterans with PTSD may have shown greater inclination toward the initiation of cannabis use during this period. Moreover, veterans in our sample with pre-pandemic positive PTSD screens reported greater odds of cannabis use during the pandemic and greater frequency of use, which fits with prior work showing cannabis initiation as a reaction to stressful life events (Hyman & Sinha, 2009; Kevorkian et al., 2015). Veterans with PTSD are also more likely to use cannabis to cope than those without PTSD (Boden et al., 2013). Veterans with pre-pandemic PTSD may require special attention to prevent heavy drinking and cannabis use during and after the pandemic, especially considering the detrimental physical and behavioral health effects that may occur with co-occurring disorders during the COVID-19 pandemic.
Veterans with positive PTSD screens who reported poorer reactions to COVID-19 during February through May 2020 reported the most frequent drinking and the greatest quantity of drinks per occasion during the pandemic. Cumulative risk perspectives posit that various risks can co-occur and accumulate (Evans et al., 2013) leading to a variety of undesirable or negative outcomes such as substance use disorders (Green et al., 2010). Unfortunately, veterans already face unique context-specific risks related to their deployment and subsequent reintegration into civilian life (Derefinko et al., 2018), which can be compounded by COVID-19 pandemic stressors like financial insecurity/job loss, social isolation, and relationship difficulties. Such compounding effects may lead to greater drinking for those already impacted by PTSD. There were no significant interactions between PTSD and poor reactions to the pandemic during the second 3 months (June–August), suggesting that during the initial months of the pandemic in the USA, poor reactions were more impactful on drinking among those with PTSD than during the later months of the pandemic.
Though the general population has been affected by COVID-19 and its aftermath, American veterans with PTSD are a unique group likely requiring targeted outreach and intervention efforts to assist them with stress, mental health symptoms, and substance use during and after the pandemic. Researchers and clinicians from the USA, Australia, Canada, England, and the Netherlands have joined together to outline several steps that can be taken to help veterans during the pandemic, including promoting and using telehealth options to provide behavioral health services to veterans, increasing financial supports and long-term investments in suicide prevention programs, targeting those with pre-existing behavioral health conditions that may be at increased risk, and assisting those healthcare workers treating veterans (Mcfarlane, Jetly, Castro, Greenberg, & Vermetten, 2020). The Veterans Affairs Healthcare System has ramped up telehealth efforts for veterans (Connolly et al., 2021), which has made access to care easier for many veterans. Despite this, rates of care initiation declined during the initial months of the pandemic for VA veterans, making it essential to continue to reach out to veterans in need through targeted outreach campaigns aiming to increase behavioral healthcare enrollment for those with PTSD in particular.
Limitations
Strengths include a large sample of veterans and two assessment time points, with one immediately prior to the outbreak of COVID-19 and another 6 months later. Limitations include the use of self-report data, which for substance use has been shown to be valid (Simons et al., 2015), but underreporting/overreporting or errors due to retrospective recall may have been present. The sample was also restricted to young adults, and generalizability to older veterans may be limited. In addition, we attempted to capture reactions to COVID-19 using a limited burden measure that encompassed emotional, stress, and relationship reactions to the pandemic. In doing so, we may have missed other aspects of COVID-19 reactions. We also asked about COVID-19 reactions during the first 3 months of the pandemic and the during the 3 months after that during the same assessment point (Time 2). Although the salience of COVID-19 likely made it easy to recall how much one was impacted by the pandemic during the initial versus the latter months of the pandemic, this is nonetheless a limitation. Future work should consider reactions to COVID-19 in the months and years following the outbreak to determine whether these negative reactions continue to increase or at some point begin to reduce. Additionally, our sample consisted of predominately white, male-identifying individuals, and we may have missed important effects within veteran populations in terms of gender, race, and/or ethnic identity. Others have noted the physical and behavioral health burdens that the COVID-19 pandemic poses on minority populations in particular (Egede & Walker, 2020; Gravlee, 2020; Gray et al., 2020).
Conclusions
Results from this study suggest that veterans struggling with PTSD prior to the COVID-19 pandemic may be at particularly high risk for difficulties managing COVID-related stress. Clinicians working with veterans may see increases in substance use and coping-related substance behaviors among veterans with PTSD during, and after, the pandemic, which may require specific treatments targeting co-occurring symptoms of PTSD and substance use disorders. Outreach efforts may be necessary to reach those with PTSD to bring them in for care to address these issues and prepare veterans to use alterative coping strategies to manage stressful reactions during this unprecedented time.
Acknowledgements
The authors wish to thank Michael Woodward, Jennifer Parker, and the RAND Survey Research Group for their assistance with data collection.
Funding
This research was funded by grant R01AA026575 from the National Institute on Alcohol Abuse and Alcoholism (NIAAA), supplement R01AA026575-02S1, and a Keck School of Medicine COVID-19 Research Funding Grant awarded to Eric R. Pedersen.
Declarations
Conflict of Interest
The authors declare no competing interests.
Informed Consent
All procedures followed were in accordance with the ethical standards of the University of Southern California Institutional Review Board and with the Helsinki Declaration of 1975, as revised in 2000 (5). Informed consent was obtained from all patients for being included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- AJMC. (2020). A Timeline of COVID-19 Developments in 2020. American Journal of Managed Care. Website accessed 9 Dec 2020 at https://www.ajmc.com/view/a-timeline-of-covid19-developments-in-2020.
- Alonzi S, La Torre A, Silverstein MW. The psychological impact of preexisting mental and physical health conditions during the COVID-19 pandemic. Psychological Trauma: Theory, Research, Practice, and Policy. 2020;12:S236–S238. doi: 10.1037/tra0000840. [DOI] [PubMed] [Google Scholar]
- Boden MT, Babson KA, Vujanovic AA, Short NA, Bonn-Miller MO. Posttraumatic stress disorder and cannabis use characteristics among military veterans with cannabis dependence. The American Journal on Addictions. 2013;22(3):277–284. doi: 10.1111/j.1521-0391.2012.12018.x. [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, Keane TM. Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (PCL-5) in veterans. Psychological Assessment. 2016;28(11):1379. doi: 10.1037/pas0000254. [DOI] [PubMed] [Google Scholar]
- Cohen J. A power primer. Psychological Bulletin. 1992;112(1):155–159. doi: 10.1037/0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Connolly SL, Stolzmann KL, Heyworth L, Weaver KR, Bauer MS, Miller CJ. Rapid increase in telemental health within the Department of Veterans Affairs during the COVID-19 pandemic. Telemedicine and e-Health. 2021;27(4):454–458. doi: 10.1089/tmj.2020.0233. [DOI] [PubMed] [Google Scholar]
- Czeisler MÉ, Lane RI, Petrosky E, Wiley JF, Christensen A, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. Morbidity and Mortality Weekly Report. 2020;69(32):1049–1057. doi: 10.15585/mmwr.mm6932a1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derefinko KJ, Hallsell TA, Isaacs MB, Salgado Garcia FI, Colvin LW, Bursac Z, McDevitt-Murphy ME, Murphy JG, Little MA, Talcott GW. Substance use and psychological distress before and after the military to civilian transition. Military Medicine. 2018;183(5–6):e258–e265. doi: 10.1093/milmed/usx082. [DOI] [PubMed] [Google Scholar]
- Dursa EK, Reinhard MJ, Barth SK, Schneiderman AI. Prevalence of a positive screen for PTSD among OEF/OIF and OEF/OIF-era veterans in a large population-based cohort. Journal of Traumatic Stress. 2014;27(5):542–549. doi: 10.1002/jts.21956. [DOI] [PubMed] [Google Scholar]
- Egede, L. E., & Walker, R. J. (2020). Structural racism, social risk factors, and Covid-19—a dangerous convergence for black Americans. New England Journal of Medicine, 383(12), e77. [DOI] [PMC free article] [PubMed]
- Ettman CK, Abdalla SM, Cohen GH, Sampson L, Vivier PM, Galea S. Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Network Open. 2020;3(9):e2019686–e2019686. doi: 10.1001/jamanetworkopen.2020.19686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Evans GW, Li D, Whipple SS. Cumulative risk and child development. Psychol Bull. 2013;139(6):1342–1396. doi: 10.1037/a0031808. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick KM, Harris C, Drawve G. Fear of COVID-19 and the mental health consequences in America. Psychological Trauma: Theory, Research, Practice, and Policy. 2020;12:S17–S21. doi: 10.1037/tra0000924. [DOI] [PubMed] [Google Scholar]
- Gallagher MW, Zvolensky MJ, Long LJ, Rogers AH, Garey L. The impact of covid-19 experiences and associated stress on anxiety, depression, and functional impairment in American adults. Cognitive Therapy and Research. 2020;44(6):1043–1051. doi: 10.1007/s10608-020-10143-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gradus, J. L. (2014). Epidemiology of PTSD. National Center for PTSD, Department of Veterans Affairs. https://www.ptsd.va.gov/professional/treat/essentials/epidemiology.asp.
- Gravlee, C. C. (2020). Systemic racism, chronic health inequities, and COVID-19: A syndemic in the making? American Journal of Human Biology, 32, e23482 [DOI] [PMC free article] [PubMed]
- Gray DM, Anyane-Yeboa A, Balzora S, Issaka RB, May FP. COVID-19 and the other pandemic: Populations made vulnerable by systemic inequity. Nature Reviews Gastroenterology & Hepatology. 2020;17(9):520–522. doi: 10.1038/s41575-020-0330-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green JG, McLaughlin KA, Berglund PA, Gruber MJ, Sampson NA, Zaslavsky AM, Kessler RC. Childhood adversities and adult psychiatric disorders in the national comorbidity survey replication I: Associations with first onset of DSM-IV disorders. Archives of General Psychiatry. 2010;67(2):113–123. doi: 10.1001/archgenpsychiatry.2009.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groshkova T, Stoian T, Cunningham A, Griffiths P, Singleton N, Sedefov R. Will the current COVID-19 pandemic impact on long-term cannabis buying practices? Journal of Addiction Medicine. 2020;14(4):e13–10. doi: 10.1097/ADM.0000000000000698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Horigian VE, Schmidt RD, Feaster DJ. Loneliness, mental health, and substance use among US young adults during COVID-19. Journal of Psychoactive Drugs. 2020;28:1–9. doi: 10.1080/02791072.2020.1836435. [DOI] [PubMed] [Google Scholar]
- Hyman SM, Sinha R. Stress-related factors in cannabis use and misuse: implications for prevention and treatment. Journal of Substance Abuse Treatment. 2009;36(4):400–413. doi: 10.1016/j.jsat.2008.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- JHSPH. (2020). Mental health survey items from the COVID-19 and mental health measurement working group. Department of Mental Health at Johns Hopkins Bloomberg School of Public Health. Available at https://www.elizabethstuart.org/files/MH_survey-items-request_03_20.pdf.
- Kevorkian S, Bonn-Miller MO, Belendiuk K, Carney DM, Roberson-Nay R, Berenz EC. Associations among trauma, posttraumatic stress disorder, cannabis use, and cannabis use disorder in a nationally representative epidemiologic sample. Psychology of Addictive Behaviors. 2015;29(3):633–638. doi: 10.1037/adb0000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim JU, Majid A, Judge R, Crook P, Nathwani R, Selvapatt N, Lovendoski J, Manousou P, Thursz M, Dhar A. Effect of COVID-19 lockdown on alcohol consumption in patients with pre-existing alcohol use disorder. The Lancet Gastroenterology & Hepatology. 2020;5(10):886–887. doi: 10.1016/S2468-1253(20)30251-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lapierre CB, Schwegler AF, LaBauve BJ. Posttraumatic stress and depression symptoms in soldiers returning from combat operations in Iraq and Afghanistan. Journal of Traumatic Stress. 2007;20(6):933–943. doi: 10.1002/jts.20278. [DOI] [PubMed] [Google Scholar]
- Liu, C. H., Zhang, E., Wong, G. T. F., & Hyun, S. (2020). Factors associated with depression, anxiety, and PTSD symptomatology during the COVID-19 pandemic: Clinical implications for US young adult mental health. Psychiatry Research, 113172. [DOI] [PMC free article] [PubMed]
- Mcfarlane A, Jetly R, Castro CA, Greenberg N, Vermetten E. Impact of COVID-19 on mental health care for Veterans: Improvise, adapt, and overcome. Journal of Military, Veteran and Family Health. 2020;6(S2):17–20. doi: 10.3138/jmvfh.CO19-0001. [DOI] [Google Scholar]
- McGinty EE, Presskreischer R, Han H, Barry CL. Psychological distress and loneliness reported by US adults in 2018 and April 2020. JAMA. 2020;324:93–94. doi: 10.1001/jama.2020.9740. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metrik J, Bassett SS, Aston ER, Jackson KM, Borsari B. Medicinal versus recreational cannabis use among returning veterans. Translational issues in psychological science. 2018;4(1):6–20. doi: 10.1037/tps0000133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metrik J, Jackson K, Bassett SS, Zvolensky MJ, Seal K, Borsari B. The mediating roles of coping, sleep, and anxiety motives in cannabis use and problems among returning veterans with PTSD and MDD. Psychology of Addictive Behaviors. 2016;30(7):743. doi: 10.1037/adb0000210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Neill E, Meyer D, Toh WL, van Rheenen TE, Phillipou A, et al. Alcohol use in Australia during the early days of the COVID-19 pandemic: Initial results from the COLLATE project. Psychiatry and Clinical Neurosciences. 2020;74(10):542–549. doi: 10.1111/pcn.13099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ornell, F., Moura, H. F., Scherer, J. N., Pechansky, F., Kessler, F. H. P., & von Diemen, L. (2020). The COVID-19 pandemic and its impact on substance use: Implications for prevention and treatment. Psychiatry Research, 289, 113096 [DOI] [PMC free article] [PubMed]
- Pollard MS, Tucker JS, Green HD. Changes in adult alcohol use and consequences during the COVID-19 pandemic in the US. JAMA Network Open. 2020;3(9):e2022942–e2022942. doi: 10.1001/jamanetworkopen.2020.22942. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rajkumar, R. P. (2020). COVID-19 and mental health: A review of the existing literature. Asian Journal of Psychiatry, 102066. [DOI] [PMC free article] [PubMed]
- Rogers, A. H., Shepherd, J. M., Garey, L., & Zvolensky, M. J. (2020). Psychological factors associated with substance use initiation during the COVID-19 pandemic. Psychiatry Research, 293, 113407. [DOI] [PMC free article] [PubMed]
- Schell, T. L., & Marshall, G. N. (2008). Survey of individuals previously deployed for OEF/OIF. In T. Tanielian, & L.H. Jaycox (Eds.). Invisible wounds of war: Psychological and cognitive Injuries, their consequences, and services to assist recovery Santa Monica, CA: RAND MG-720. Available at: http://www.rand.org/pubs/monographs/2008/RAND_MG720.pdf.
- Sharma P, Ebbert JO, Rosedahl JK, Philpot LM. Changes in substance use among young adults during a respiratory disease pandemic. SAGE open medicine. 2020;8:2050312120965321. doi: 10.1177/2050312120965321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons JS, Wills TA, Emery NN, Marks RM. Quantifying alcohol consumption: Self-report, transdermal assessment, and prediction of dependence symptoms. Addictive Behaviors. 2015;50:205–212. doi: 10.1016/j.addbeh.2015.06.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teeters JB, Lancaster CL, Brown DG, Back SE. Substance use disorders in military veterans: Prevalence and treatment challenges. Substance Abuse and Rehabilitation. 2017;8:69–77. doi: 10.2147/SAR.S116720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Varga, T. V., Bu, F., Dissing, A. S., Elsenburg, L. K., Bustamante, J. J. H., et al. (2021). Loneliness, worries, anxiety, and precautionary behaviours in response to the COVID-19 pandemic: A longitudinal analysis of 200,000 Western and Northern Europeans. The Lancet Regional Health-Europe, 2, 100020. [DOI] [PMC free article] [PubMed]
- Vanderbruggen N, Matthys F, Van Laere S, Zeeuws D, Santermans L, Van den Ameele S, Crunelle CL. Self-reported alcohol, tobacco, and cannabis use during COVID-19 lockdown measures: Results from a web-based survey. European Addiction Research. 2020;26(6):309–315. doi: 10.1159/000510822. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardell JD, Kempe T, Rapinda KK, Single A, Bilevicius E, et al. Drinking to cope during COVID-19 pandemic: The role of external and internal factors in coping motive pathways to alcohol use, solitary drinking, and alcohol problems. Alcoholism, clinical and experimental research. 2020;44(10):2073–2083. doi: 10.1111/acer.14425. [DOI] [PubMed] [Google Scholar]
- Werner KB, Sartor CE, McCutcheon VV, Grant JD, Nelson EC, Heath AC, Bucholz KK. Association of specific traumatic experiences with alcohol initiation and transitions to problem use in European American and African American women. Alcoholism, clinical and experimental research. 2016;40(11):2401–2408. doi: 10.1111/acer.13220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witteveen D, Velthorst E. Economic hardship and mental health complaints during COVID-19. Proceedings of the National Academy of Sciences. 2020;117(44):27277–27284. doi: 10.1073/pnas.2009609117. [DOI] [PMC free article] [PubMed] [Google Scholar]