Abstract
The introduction of behavioral, including psychiatric, genetic information in American courts has gained traction but raises concerns of undue influence on judicial outcomes. We conducted a vignette-based survey of a nationally representative sample of US adults to assess how evidence about a parent’s psychiatric genetic makeup and explicit and implicit stigmatizing beliefs about psychiatric conditions may affect key decisions in child custody proceedings. Psychiatric genetic evidence did not affect public perspectives on custody decisions, but it increased the genetic essentialist understanding of psychiatric conditions (regardless of a diagnosis). Explicit stigma was associated with a preference to deny parents with a (or with an alleged) psychiatric condition joint custody. Our newly created Implicit Association Test identified an association between psychiatric conditions and perceived bad parenting. Research to identify effective interventions and educational programs to address genetic essentialism and to reduce bias against people, including parents, with psychiatric conditions is urgently needed.
Keywords: child custody, genetic essentialism, implicit bias, psychiatric genetic evidence, stigma
I. INTRODUCTION
Since the early 2000s, there has been exponential growth in genetic testing relating to personal health, including single- or multiple-gene testing,1 and complex gene–gene and gene–environment interaction studies aimed at improving understanding of behavioral, including psychiatric, conditions.2 Likewise, the introduction of behavioral genetic claims in courts has gained traction, encompassing criminal cases3 and civil proceedings such as torts4 and cases to terminate parental rights.5 Although the complexity of cases and limits of current scientific knowledge make it difficult to gauge the exact impact of genetic evidence on judicial outcomes,6 it is unlikely that this trend will abate anytime soon.
The use of psychiatric genetic evidence may be particularly alluring—and concerning—in child custody cases. Studies have found that environments such as parenting styles can interact with children’s genetic makeup to produce pathological psychiatric outcomes.7 With assessment of parental fitness serving as a key factor in judicial determinations of child custody,8 the possibility of psychiatric genetic information informing custody decisions may seem appealing. Some research indicates that the general public holds an essentialist view of genes as unchangeable and strongly deterministic of behavioral outcomes,9 and that attributions of psychiatric disorders to genetic causes are associated with increased belief in the severity and persistence of these conditions.10 In child custody disputes, a parent litigant may view psychiatric genetic evidence as a powerful tool to cast doubt on the other parent’s mental health status and prospective parenting capacity, regardless of the other parent’s actual ability.11
A related—and possibly independent—concern is that stigma surrounding psychiatric conditions may unduly influence child custody decisions. Studies show that public stigma is a major barrier for the inclusion of people with psychiatric conditions in daily life activities, including housing, employment, and medical care.12 Public perceptions of people with psychiatric conditions as incompetent decision-makers13 and as a danger to themselves and others14 are common, notwithstanding evidence to the contrary.15 Despite decades of educational efforts to reduce public stigma of psychiatric disorders, stigma associated with such conditions, including prejudice, discrimination, and desire for social distance, remains high.16 Fear of people with psychiatric conditions has increased over the last several decades, even expanding to encompass people with run-of-the-mill troubles, along with growing public support for coerced treatment of such individuals (including medication, physician visits, and hospitalization).17 Likewise, hopes that public understanding of the genetic underpinnings of psychiatric conditions would reduce stigma have not materialized: some studies even indicate that higher endorsements of biological explanations for psychiatric conditions are associated with increased stigma.18 The possible impact of stigma (including perceptions of dangerousness) on child custody decisions is further complicated as it may be implicit and affect decision-making without the decision-maker realizing it.19
To date, studies that explored the impact of psychiatric genetic evidence on judicial decisions have focused on judges and potential jurors in criminal cases,20 whereas research on bias in civil courts has centered on race, gender, and socioeconomic status.21 A study that assessed public views on children’s psychiatric genetic data in cases on termination of parental rights found that genetic evidence increased the child’s labeling as having a psychiatric disorder, regardless of the presence of symptoms, and that participants who did not think that the child had a psychiatric disorder were more likely to support termination of parental rights after positive genetic test results.22 However, these findings cannot be generalized to child custody disputes in which the parents’ psychiatric genetic makeup is introduced. Children’s genetic makeup is often viewed as more malleable than adults’,23 psychiatric conditions are less stigmatized in the pediatric population,24 and children are not expected to seek mental health support on their own, as are adults.
Concurrently, a survey of civil cases suggested that litigants with an alleged current diagnosis or history of a psychiatric disorder often lose credibility due to judicial bias,25 and there are worries that similar biases exist toward parents with psychiatric conditions who are embroiled in child custody proceedings.26 Although a psychiatric diagnosis per se does not indicate parental unfitness, scholars have highlighted that research on parents with psychiatric conditions has largely only focused on parental pathology, with psychiatric conditions presumed to be a predictor of child abuse and neglect.27 As in other contexts28 involving presumed presence of a psychiatric condition, such perceptions may lead to inappropriate endorsement of coerced treatment and affect judicial decisions about child custody. In a study of family court judges, for instance, some judges explicitly connected the willingness of parents with psychiatric conditions to take medication with greater parental mental stability.29 The limited data that exist further indicate that parents with psychiatric conditions (especially fathers) are far more likely than parents in the general population to have involvement of Child Protective Services (CPS), be viewed as requiring some type of intervention, and experience a change in living arrangements of the child, including loss of custody (even controlling for other factors impacting CPS involvement such as poverty).30 Also among parents with psychiatric conditions outside of the CPS system, research shows that child custody challenges are common and often result in a loss or change of custody. A 2020 study of a national sample found that about a third of parents with ‘severe’ psychiatric conditions lost custody;31 other studies report even higher rates of child custody loss (70–80% of parents with psychiatric conditions).32 Given the concerns about genetic essentialism and stigma of adult psychiatric conditions, including increasing public support for coerced treatment, and the already high rate of custody loss among parents with psychiatric conditions, better understanding of whether and how these factors may impact child custody decisions is merited.
We report findings from a survey of a nationally representative sample of US adults (n = 300) exploring the effects of evidence about a parent’s psychiatric genetic makeup and stigma on key decisions in child custody proceedings. The general public’s views on these issues are informative for several reasons. First, public perceptions can affect laws and policies relating to child custody cases, including by parent litigants introducing innovative scientific evidence in court proceedings. Second, judges may hold misconceptions about genetics33 and, regardless of expertise, they are no less influenced than laypeople by common societal biases (eg gender, race) in legal decision-making.34 Exploring whether laypeople hold essentialist views regarding psychiatric genetic evidence and the effect of explicit and implicit stigma on their preferences regarding child custody can serve as a window on judicial perspectives. To our knowledge, this is the first study to empirically assess these intersecting issues.
II. BACKGROUND AND METHODOLOGY OF THE STUDY
To assess the impact of psychiatric genetic evidence on child custody proceedings, we administered an anonymous, 20-minute, online survey to a nationally representative sample of 300 adults. The survey comprised two vignettes, one of which is reported here. Participants were recruited by YouGov, a professional research firm that operates an internet-based panel of the general public that can be sampled to be representative of the US population (Table 1). YouGov collected demographic characteristics, administered the survey and offered participants ‘Polling Points’ redeemable for small gifts (equivalent of $1) for their participation. Additional details concerning the sample, methods and data collected for this study are detailed elsewhere.35 The N.Y. State Psychiatric Institute Institutional Review Board approved the study.
Table 1.
Demographic Characteristics (n =300)*
| Participants demographic characteristics | % or Mean (SD) | |
| Gender | ||
| Female | 165 | 55.0% |
| Male | 135 | 45.0% |
| Age | 48.6 | (16.8) |
| 18–29 | 47 | 15.7% |
| 30–59 | 159 | 53.0% |
| 60+ | 94 | 31.3% |
| Race | ||
| Black or African American | 33 | 11% |
| White | 233 | 77.7% |
| Asian or Pacific Islander | 10 | 3.3% |
| American Indian or Alaska Native | 3 | 1.0% |
| Native Hawaiian or other Pacific Islander | 0 | 0.0% |
| Mixed race** | 9 | 3.0% |
| Missing | 12 | 4.0% |
| Hispanic | ||
| Yes | 38 | 12.7% |
| No | 262 | 87.3% |
| Region of residence | ||
| Northeast | 51 | 17.0% |
| Midwest | 75 | 25.0% |
| South | 109 | 36.3% |
| West | 65 | 21.7% |
| Highest education level attained | ||
| ≤High school graduate | 100 | 33.3% |
| Some college—2 years of college | 101 | 33.7% |
| 4 years of college/Postgraduate | 99 | 33.0% |
| Marital status | ||
| Divorced/Separated | 41 | 13.7% |
| Never married | 101 | 33.7% |
| Married/Widowed*** | 158 | 52.7% |
| Income | ||
| ≤$19,999 | 42 | 14.0% |
| $20,000–$49,999 | 99 | 33.0% |
| $50,000–$99,999 | 82 | 27.3% |
| $100,000 or more | 40 | 13.3% |
| Prefer not to say/Missing | 37 | 12.3% |
*The sample was selected to be nationally representative of the adult US population (based on variables such as age, gender, race/ethnicity, education, and party identification, drawn from data in the 2010 American Community Survey).
**Mixed-race participants selected both white and another racial category. In the analysis, the race category was collapsed into white/non-white participants. Mixed-race participants were classified as non-white.
***‘Married’ includes domestic/civil partnership. Married/widowed participants were grouped together because the views of these participants, who are in a relationship or whose relationship was involuntarily ended, are likely to be different than participants who are divorced or are in the process of getting a divorce.
II.A. Vignette
Modeled on the facts of various child custody court cases, we constructed a vignette to depict a divorcing couple who disagree about the custody of their 8-year-old son (Appendix A). We randomly varied the sex of the putatively unfit parent, presence of a psychiatric diagnosis, and presence of psychiatric genetic evidence (see below); psychiatric genetic evidence was our primary independent variable.
The vignette described parents who worked throughout their marital life and shared household and child-care responsibilities, and the questionable behaviors of the putatively unfit parent (mother/father) preceding the divorce, including spontaneous expensive vacations, inappropriate sexual jokes, and forgetfulness of arrangements that led to bickering. In court proceedings, the other parent requested primary custody (hereinafter: ‘parent-claimant’), relating the aforementioned behaviors to parental mental instability and claiming that the child’s best interests would not be met by joint custody. A court-appointed psychiatrist conducted a child custody evaluation, including clinical interviews with the parents, the child (who expressed no preference as to his primary custodian), and a psychologist with whom the putatively unfit parent had consulted during the marriage. Evidence of the presence or absence of a psychiatric condition and types of psychiatric genetic information were introduced during the psychiatrist’s testimony in court.
The ‘psychiatric condition’ was bipolar disorder (none/moderately severe), described in the case as a condition that is ‘characterized by periods of alternating elevated and depressed moods’. Bipolar disorder was selected because it is the main condition that arises in custody disputes.36
‘Psychiatric genetic evidence’ encompassed one of four conditions: (i) family history of bipolar disorder (hereinafter: family history); (ii) genetic test results showing an increased risk of the parent developing bipolar disorder (hereinafter: genetic results); (iii) both family history and genetic results; and (iv) neither family history nor genetic results. For (i–iii), participants were either told about positive results or not told at all about the presence of genetic evidence [yielding (iv)]. The evidence about family history (‘bipolar disorder in several family members of the parent’) was selected because family history is the most reliable risk factor identified to date and our preliminary review of child custody cases indicated that it is commonly introduced for courts’ consideration of parental medical history and (un)fitness.
The vignette was followed by case-related questions to assess the effect of psychiatric genetic evidence on participants’ decisions about the child’s primary custody and genetic essentialist thinking. We also included questions to assess the impact of explicit stigma regarding psychiatric conditions on child custody decisions and a newly created computerized Implicit Association Test (IAT) to assess bias toward parents with psychiatric conditions (section III.C. below). We hypothesized that the introduction of psychiatric genetic evidence (ie each of categories i–iii above, with ascending impact) would be positively associated with decisions to award custody to the parent-claimant and stronger genetic essentialist thinking. Based on studies indicating high stigma associated with psychiatric conditions and findings that genetic information may exacerbate psychiatric-related stigma (see above), we also predicted that a professional psychiatric diagnosis as well as explicit and implicit biases would be positively associated with decisions to award custody to the parent-claimant, especially in the presence of psychiatric genetic evidence.
II.B. Statistical Analysis
Variables and participant demographic characteristics were described using counts, percentages, means, and standard deviations (SD). Dependent variables from the questionnaire were dichotomized [eg likely (somewhat/very likely) vs. unlikely (somewhat unlikely/not likely at all)]. For case-related questions, multiple logistic regression was used to assess the impact of psychiatric genetic evidence on the dependent variable. Psychiatric genetic evidence was our primary independent variable. Parental sex, psychiatric diagnosis, and the demographic covariates (race, ethnicity, gender, and educational attainment) were controlled for in the analysis. Multiple logistic regression was used to assess the impact of explicit stigma on child custody decisions. Implicit bias was assessed by following established procedures for obtaining an overall D-score for participants’ IAT37 (Table 5). A multiple linear regression model was fit for the continuous IAT score. The vignette’s independent variables (psychiatric genetic evidence, psychiatric diagnosis, parent’s sex) and the demographic covariates were controlled for in the stigma analysis. For all analyses, missing data were rare [generally <5%, except likelihood that the parent has a psychiatric disorder (n = 21; 7.0%)] and handled by using complete case analysis. P-values <0.05 were considered significant. Analyses of parental sex and participants’ demographics (not shown) found no or very little effect on the variables discussed here, and they are not discussed in this article. Data were analyzed using SAS 9.4.
Table 5.
IAT to assess bias against parents with psychiatric conditions*
| Category | Items |
| Mentally ill | Manic, depressed, mentally ill, delusional, impaired |
| Mentally healthy | Balanced, functional, flexible, mentally healthy, self-aware |
| Good parent | Affectionate parent, attentive parent, consistent parent, responsible parent, safe parent, capable parent |
| Bad parent | Cold parent, neglectful parent, unpredictable parent, irresponsible parent, dangerous parent, inept parent |
*The IAT included five computerized tasks. It started with one set of category pairs presented and then included two sets of category pairs presented simultaneously. For example, the paired categories of ‘mentally ill’ and ‘dangerous parent’ were first shown separately at the top right and left of the computer screen. Participants were then shown in the middle of the screen word items from either the mentally ill/mentally healthy or good/bad parenting categories (one word at a time) and requested to sort them as belonging to either ‘mentally ill’ or ‘dangerous parent’. Later on, the paired categories of ‘mentally ill’ and ‘dangerous parent’ were shown together at the top left of the computer screen, whereas eg ‘mentally healthy’ and ‘safe parent’ were shown at the top right, followed by similar word items sorting task by participants as described above.
III. PSYCHIATRIC GENETIC EVIDENCE, PSYCHIATRIC DIAGNOSIS, AND STIGMA
III.A. Child-Custody Decisions
The data on the impact of psychiatric genetic evidence on participants’ responses are provided in Table 2. Participants were asked to indicate whether the parent-claimant should ‘be awarded primary custody of [the child] at this time’. Most participants (68%) decided to award primary custody to the parent-claimant. However, genetic evidence was not associated with this decision.
Table 2.
Impact of psychiatric genetic evidence and diagnosis on child custody decisions and genetic essentialist thinking
| Dependent variable (participants’ agreement) | OR | 95% CI ** | P value |
| Award custody to parent-claimant * (n = 204/299, 68.0%) | |||
| Family history vs. no evidence | 1.93 | (0.93, 4.01) | 0.08 |
| Genetic results vs. no evidence | 1.39 | (0.68, 2.81) | 0.36 |
| Both family history and genetic results vs. no evidence | 1.48 | (0.74, 2.99) | 0.27 |
| Diagnosis vs. no diagnosis | 2.79 | (1.66,4.69) | <0.001 |
| Genetic essentialism | |||
| Attribution: the parent has a psychiatric disorder (n = 253/279, 90.7%) | |||
| Family history vs. no evidence | 4.96 | (1.39, 17.67) | 0.01 |
| Genetic results vs. no evidence | 5.42 | (1.32, 22.23) | 0.02 |
| Both family history and genetic results vs. no evidence | 2.71 | (0.86, 8.52) | 0.09 |
| Diagnosis vs. no diagnosis | 12.50 | (3.45, 45.25) | <0.001 |
|
Treatment: The parent should … Go to a general medical doctor (n = 150/298, 50.3%) | |||
| Family history vs. no evidence | 0.86 | (0.44, 1.69) | 0.67 |
| Genetic results vs. no evidence | 0.71 | (0.37, 1.39) | 0.32 |
| Both family history and genetic results vs. no evidence | 1.29 | (0.67, 2.48) | 0.45 |
| Diagnosis vs. no diagnosis | 1.12 | (0.70, 1.79) | 0.65 |
| Go to a psychiatrist (n = 239/297, 80.5%) | |||
| Family history vs. no evidence | 1.55 | (0.69, 3.49) | 0.29 |
| Genetic results vs. no evidence | 1.54 | (0.68, 3.48) | 0.30 |
| Both family history and genetic results vs. no evidence | 1.87 | (0.81, 4.30) | 0.14 |
| Diagnosis vs. no diagnosis | 2.52 | (1.36, 4.68) | 0.003 |
| Go to a therapist, counselor, or other mental health professional (n = 272/300, 90.7%) | |||
| Family history vs. no evidence | 1.79 | (0.54, 5.92) | 0.34 |
| Genetic results vs. no evidence | 0.83 | (0.29, 2.43) | 0.74 |
| Both family history and genetic results vs. no evidence | 1.15 | (0.38, 3.48) | 0.80 |
| Diagnosis vs. no diagnosis | 1.52 | (0.67, 3.44) | 0.31 |
| Be evaluated for prescription medication (n = 251/300, 83.7%) | |||
| Family history vs. no evidence | 1.83 | (0.82, 4.11) | 0.14 |
| Genetic results vs. no evidence | 3.05 | (1.26, 7.39) | 0.01 |
| Both family history and genetic results vs. no evidence | 5.69 | (2.08, 15.55) | 0.001 |
| Diagnosis vs. no diagnosis | 1.69 | (0.88, 3.25) | 0.11 |
| Be evaluated for admission to a mental hospital (n = 50/294, 17.0%) | |||
| Family history vs. no evidence | 1.07 | (0.39, 2.92) | 0.90 |
| Genetic results vs. no evidence | 1.32 | (0.50, 3.47) | 0.57 |
| Both family history and genetic results vs. no evidence | 2.53 | (1.05, 6.10) | 0.04 |
| Diagnosis vs. no diagnosis | 1.46 | (0.77, 2.77) | 0.25 |
|
Condition’s seriousness: A judge should require the parent to …. | |||
| Go to general medical doctor (n = 129/292, 44.2%) | |||
| Family history vs. no evidence | 0.77 | (0.39, 1.53) | 0.45 |
| Genetic results vs. no evidence | 0.60 | (0.30, 1.19) | 0.14 |
| Both family history and genetic results vs. no evidence | 1.30 | (0.67, 2.53) | 0.43 |
| Diagnosis vs. no diagnosis | 1.09 | (0.68, 1.77) | 0.71 |
| Go to a psychiatrist (n = 215/294, 73.1%) | |||
| Family history vs. no evidence | 1.65 | (0.79, 3.43) | 0.18 |
| Genetic results vs. no evidence | 1.89 | (0.90, 3.99) | 0.09 |
| Both family history and genetic results vs. no evidence | 2.09 | (0.99, 4.40) | 0.052 |
| Diagnosis vs. no diagnosis | 2.11 | (1.23, 3.63) | 0.01 |
| Go to a therapist, counselor, or other mental health professional (n = 254/296, 85.8%) | |||
| Family history vs. no evidence | 2.25 | (0.82, 6.18) | 0.11 |
| Genetic results vs. no evidence | 1.12 | (0.46, 2.77) | 0.80 |
| Both family history and genetic results vs. no evidence | 1.35 | (0.54, 3.34) | 0.52 |
| Diagnosis vs. no diagnosis | 1.43 | (0.73, 2.83) | 0.30 |
| Be evaluated for prescription medication (n = 223/296, 75.3%) | |||
| Family history vs. no evidence | 1.62 | (0.77, 3.41) | 0.20 |
| Genetic results vs. no evidence | 1.93 | (0.91, 4.07) | 0.09 |
| Both family history and genetic results vs. no evidence | 3.09 | (1.39, 6.84) | 0.01 |
| Diagnosis vs. no diagnosis | 1.69 | (0.97, 2.94) | 0.06 |
| Be evaluated for admission to a mental hospital (n = 56/290, 19.3%) | |||
| Family history vs. no evidence | 1.28 | (0.49, 3.34) | 0.62 |
| Genetic results vs. no evidence | 1.58 | (0.63, 3.99) | 0.33 |
| Both family history and genetic results vs. no evidence | 2.53 | (1.06, 6.04 | 0.04 |
| Diagnosis vs. no diagnosis | 1.46 | (0.79, 2.69) | 0.22 |
*Parent-claimant refers to the parent who requested primary custody of the child and whose mental health was ‘not’ questioned. ‘Parent’ in all other questions of genetic essentialism (attribution, treatment, condition’s seriousness) refers to the parent whose mental health was questioned.
**In addition to psychiatric genetic evidence, psychiatric diagnosis, and parental gender in the vignette, the model controlled for participants’ race, ethnicity (Hispanic/non-Hispanic), gender, and educational attainment.
The diagnosis of bipolar disorder in the putatively unfit parent was significantly associated with the decision to award custody to the parent-claimant [odds ratio (OR) = 2.79, 95% confidence interval (CI) 1.66–4.66, P < 0.001] as well as belief that the putatively unfit parent had a psychiatric disorder (OR = 12.50, 95% CI 3.45–45.25, P < 0.001), recommendation for that parent to go to a psychiatrist (OR = 2.52, 95% CI 1.36–4.68, P = 0.003), and agreement that the judge should require that parent go to a psychiatrist (OR = 2.11, 95% CI 1.23–3.63, P = 0.01).
III.B. Genetic Essentialism
Attribution of psychiatric conditions was assessed by asking participants how likely it was that the putatively unfit parent has a psychiatric disorder (measured on Likert scale, 1 = not at all likely to 4 = very likely; ‘I don’t know’ option (n = 21) was treated in the analysis as missing data, as it is impossible to derive from this response any further information). In total, 90.7% of participants believed that the parent was likely to have a psychiatric disorder. This response was positively associated with the presence of either family history (OR = 4.96, 95% CI 1.39–17.67, P = 0.01) or genetic results (OR = 5.42, 95% CI 1.32–22.23, P = 0.02) but not with both family history and genetic results (OR = 2.71, 95% CI 0.86–8.52, P = 0.09).
To assess perceived need for treatment, we utilized a previously validated scale,38 querying whether the putatively unfit parent should seek consultation with various health professionals or be evaluated for medical interventions. Response options were yes/no; participants could choose more than one consultant. In total, 90.7% of participants endorsed the option of ‘a therapist or counselor, such as a psychologist, clinical social worker, or other mental health professional’, followed by an evaluation for prescription medication (83.7%), visiting a psychiatrist (80.5%), and going to a general medical doctor (50.3%). Only 17.0% of the participants believed that the parent should be evaluated for admission to a psychiatric hospital. Participants who were provided with genetic results alone (OR = 3.05, 95% CI 1.26–7.39, P = 0.01) or both genetic results and family history (OR = 5.69, 95% CI 2.08–15.55, P = 0.001) were significantly more likely to recommend evaluation for prescription medication and admission to a mental hospital (OR = 2.53, 95% CI 1.05, 6.10, P = 0.04). In addition, participants who were provided with either family history or genetic results compared with those who received neither were significantly more likely to recommend more types of treatment (n = 3.28 vs. 2.97, respectively; P = 0.04).
To assess perceived seriousness of the parent’s alleged psychiatric condition, participants were asked whether, upon the psychiatrist’s recommendation that the parent receive the treatment options above, a judge should ‘require’ the parent to receive them ‘if [s/he] wants to have unsupervised visitation with [the child]’. Response options were yes/no. Participants who were provided with both genetic results and family history were significantly more likely than those presented with neither to recommend that the judge require the parent to be evaluated for prescription medication (OR = 3.09, 95% CI 1.39–6.84, P = 0.01) and admission to a mental hospital (OR = 2.45, 95% CI 1.00–6.01, P = 0.0497).
To assess perceptions of treatment efficacy, participants were asked about the likelihood that ‘[the parent’s] situation will improve with professional mental health treatment’. Response options were on a Likert scale (1 = not at all likely; 4 = very likely). Almost 91% of participants responded positively, but perceived treatment efficacy was not associated with any type of genetic evidence (all P > 0.69).
III.C. Impact of Explicit and Implicit Stigma on Child Custody Decisions
To assess explicit stigma, two validated scales were used. The first, ‘social distance’, a five-item measure,39 asked participants how willing they would be to work closely with, live next door to, spend a social evening with, be friends with, and have family relations with someone like the parent in the vignette. Response options were on a 1–4 Likert scale (1 = definitely willing, 4 = definitely unwilling). Social distance score was calculated as the average of five items (alpha = 0.91). Higher social distance scores reflect higher stigma and less willingness to be in contact with people with psychiatric conditions. Most participants expressed willingness to interact with someone like the parent in the vignette in each of the items (range: 69.1–76.7%), but only 50.3% expressed willingness to have someone like the person in the vignette marry into their family. Participants with higher social distance scores (mean = 2.18, standard deviation (STD) = 0.71) had higher odds (per unit change) of awarding custody to the parent-claimant (OR = 2.89, 95% CI 1.87–4.47, P < 0.0001; Fig. 1), and all individual social distance items were positively associated with this response (Table 3).
Figure 1.
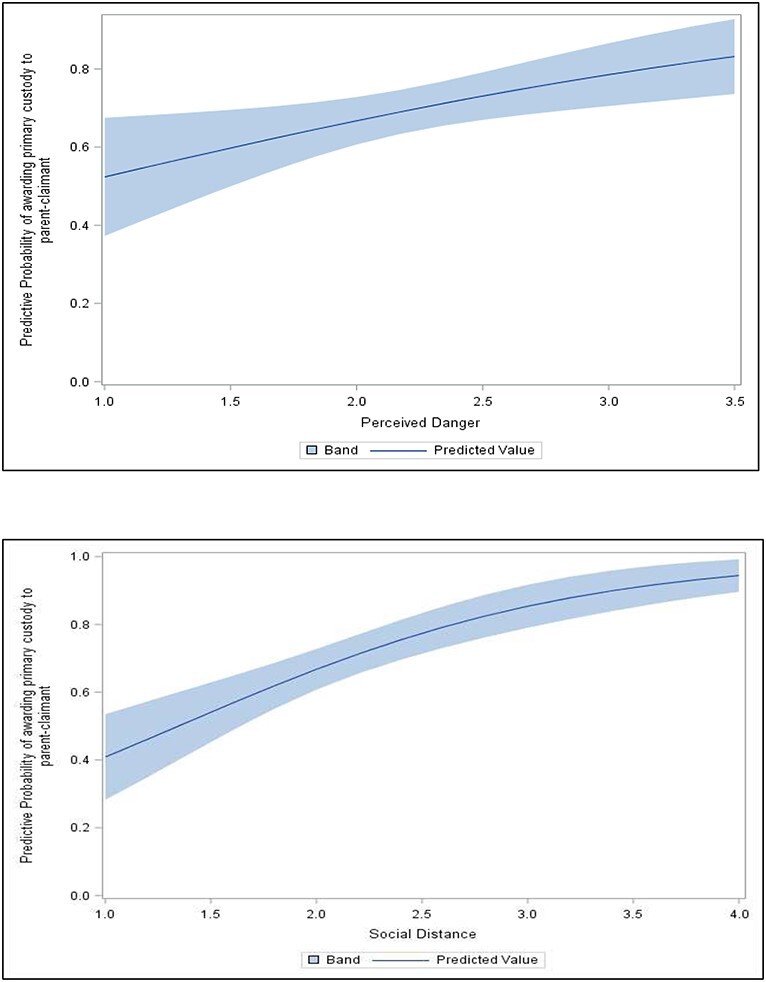
Impact of explicit stigma on award of primary custody to parent-claimant*. *Parent-claimant refers to the parent who requested primary custody of the child and whose mental health was ‘not’ questioned. Predictive probability of awarding primary custody to parent-claimant by (i) level of perceived danger and (ii) level of social distance, adjusting for sociodemographic characteristics (race, gender, education, ethnicity, and parental status) and vignette features (genetic evidence, case gender, and case diagnosis).
Table 3.
Impact of explicit stigma on child custody decisions
| Odds of awarding custody to the parent-claimant | ||||
| Award custody to the parent-claimant * | % | OR | 95% CI ** | P value |
| Social distancing, unwilling to (mean=2.18, STD=0.71, range=1-4, n=293) | N/A | 2.89 | (1.87, 4.47) | <0.001 |
| Work closely with someone like the parent on job | 27.3% | 4.96 | (2.30, 10.70) | <0.001 |
| Live next door to someone like the parent | 23.3% | 5.00 | (2.21, 11.30) | <0.001 |
| Spend an evening socializing with someone like the parent | 30.9% | 3.43 | (1.78, 6.59) | <0.001 |
| Have someone like the parent marry into family | 50.3% | 2.96 | (1.73, 5.09) | <0.001 |
| Have someone like the parent as friend | 27.4% | 3.69 | (1.83, 7.45) | <0.001 |
| Perceived dangerousness, agree (mean=2.21, STD=0.59, range=1-3.50, n=293) | N/A | 1.80 | (1.13, 2.88) | 0.01 |
| Although some people who have been patients in mental hospitals may seem alright, it is important to remember that they may be dangerous | 50.8% | 1.74 | (1.03, 2.95) | 0.04 |
| Most people who have been mentally ill are no more dangerous than the average person (reversed coded) | 25.9% | 1.51 | (0.82, 2.80) | 0.19 |
| One important thing about people who have been mentally ill is that you cannot tell what they will do from one minute to the next | 56.8% | 2.08 | (1.21.3.57) | 0.01 |
| It’s only natural to be afraid of a person who is mentally ill | 41.7% | 1.96 | (1.13, 3.37) | 0.02 |
| The main purpose of mental hospitals should be to protect the public from mentally ill people | 16.5% | 1.21 | (0.60, 2.45) | 0.60 |
| Mentally ill people are more likely to commit violent crimes than other people | 34.5% | 1.77 | (1.01, 3.12) | 0.047 |
*Parent-claimant refers to the parent who requested primary custody of the child and whose mental health was ‘not’ questioned. ‘Parent’ in the social distance and perceived dangerousness scales refers to the parent whose mental health was questioned.
**Controlled for vignette’s independent variables (ie genetic evidence, parental diagnosis of bipolar disorder, parental gender) and demographic covariates (ie participant’s race, ethnicity (Hispanic vs. non-Hispanic), gender, and educational attainment.
The second measure was ‘perceived dangerousness’, a six-item scale40 comprising items such as: ‘although some people who have been patients in mental hospitals may seem alright, it is important to remember that they may be dangerous’ and ‘it’s only natural to be afraid of a person who is mentally ill’ (Table 3). Response options were on a Likert scale (1 = ‘definitely false’, 4 = ‘definitely true’); scores were calculated as the average of the items (alpha = 0.79). Higher scores indicate higher stigma and stronger perceptions of people with psychiatric conditions as dangerous. Participants who obtained higher scores on the dangerousness scale (mean = 2.21, SD = 0.59, range 1–3.5) had higher odds (per unit change) of awarding custody to the parent-claimant than participants with lower scores (OR = 1.80, 95% CI 1.13–2.88, P = 0.01; Fig. 1), and most individual items were positively associated with awarding custody to the parent-claimant. Spearman correlation between social distance and perceived dangerousness was 0.317 (P < 0.001).
Neither social distance (P = 0.42) nor perceived dangerousness (P = 0.91) scores were associated with positive genetic results.
In addition, we created a seven-item scale to assess participants’ views about the capability of the parent to perform various daily life activities, such as remarrying, opening a new bank account, owning property (eg a car or apartment), and making a decision to receive or refuse psychiatric treatment (two separate items). These items were developed based on scholarship in disability studies highlighting worries about frequently held beliefs related to incapacities of people with psychiatric conditions. Response options were on a 1–4 point Likert scale (reversed coded in analysis: 1 = ‘very capable’, 4=‘not at all capable’). The impact of each item on custody decisions was assessed separately [dichotomized responses (somewhat/very capable vs. not very/not at all capable)] and overall scores were calculated as the average of the items (alpha = 0.91). The overall mean capability score was 1.66 (SD = 0.61, range 1–4). As shown in Table 4, participants who rated the parent as having higher scores on each of the seven items (indicating an opinion of the parent as less capable) as well as generating a higher overall mean capability score, were more likely to award custody to the parent-claimant (for individual items, all P ≤ 0.03; for overall score, P < 0.001).
Table 4.
Impact of perceptions of capabilities on child custody decisions
| Odds of awarding custody to the parent-claimant | ||||
| Award custody to the parent-claimant* | % | OR | 95% CI ** | P value |
| Putatively unfit parent incapable of: (mean=1.66, STD=0.61, range=1-4, n=300) | N/A | 4.31 | (2.54, 7.32) | <0.001 |
| Remarrying | 16.4 | 4.94 | (1.78 - 13.68) | 0.002 |
| Opening a new bank account | 8.4 | 5.09 | (1.14 - 22.72) | 0.033 |
| Owning property (eg a car of apartment) | 12.1 | 5.52 | (1.61 - 19.00) | 0.007 |
| Signing a contract involving financial transaction | 18.4 | 4.00 | (1.66 - 9.60) | 0.002 |
| Providing testimony in court proceedings unrelated to the child custody dispute | 14.4 | 2.64 | (1.08 - 6.43) | 0.033 |
| Making a decision to receive psychiatric treatment | 11.4 | 3.88 | (1.28 - 11.75) | 0.017 |
| Making a decision to refuse psychiatric treatment | 22.3 | 2.78 | (1.33 - 5.82) | 0.007 |
*Parent-claimant refers to the parent who requested primary custody of the child and whose mental health was ‘not’ questioned.
**Controlled for vignette’s independent variables (ie genetic evidence, parental diagnosis of bipolar disorder, parental gender) and demographic covariates (ie participant’s race, ethnicity (Hispanic vs. non-Hispanic), gender, and educational attainment).
No significant association was found between genetic evidence and capability scores (P = 0.73). However, participants who were told that the parent had a diagnosis of bipolar disorder were more likely than those who were not to assess the parent as less capable in overall score (OR = 1.35, 95% CI 1.19–1.54, P < 0.001) and across items [P < 0.030, except providing testimony in nonchild custody court proceeding (0.072)]. Further analysis found that participants who were not told that the parent had a bipolar diagnosis but believed anyway that the parent had a psychiatric condition were less likely to deem the parent incapable compared with those who were provided with a diagnosis and believed the parent had a psychiatric condition (OR = 0.82, 95% CI 0.71–0.95, P = 0.007). However, they were more likely to deem the parent incapable compared with those who were neither given a diagnosis nor thought that the parent had a psychiatric disorder (OR = 1.40, 95% CI 1.08–1.82, P = 0.0115).
To assess implicit stigma, we developed a computerized IAT to assess automatic associations between good/bad parenting and psychiatric disorders (Table 5). The IAT was developed in consultation with and administered by Project Implicit, a nonprofit collaborative network of researchers investigating implicit social cognition.41 The IAT assesses the relative speed at which participants classify word stimuli (concepts) into attribute categories that match or contradict automatic associations.42 Reaction time is the dependent measure (faster responses reflect stronger automatic association).
As mentioned above, we hypothesized that parents with psychiatric conditions would be viewed negatively, that is: that they would be associated with ‘bad’ parenting, a common claim in child custody proceedings.43 Participants were required to categorize stimuli relating to psychiatric conditions (eg mentally ill vs. mentally healthy) into attribute dimensions assessing good/bad parenting (eg safe parent vs. dangerous parent). The IAT included five tasks and word pairing was switched to allow for comparison of responses across paired categories (eg showing first mentally ill/dangerous parent and then mentally ill/safe parent or showing first mentally healthy/dangerous parent and then mentally healthy/safe parent). An overall D-score was obtained for participants’ IAT [range: (−2, 2)]; a positive D-score reflects an association that is consistent with the hypothesized stereotype. The mean D-score for the IAT was 1.02 (SD = 0.034; 95% CI 0.953–1.087), indicating a strong association between psychiatric conditions and perceived bad parenting, and between absence of psychiatric conditions and perceived good parenting. The IAT was not associated with custody decisions in the vignette (P = 0.520) or with social distancing (P = 0.059) or dangerousness (P = 0.767) scales.
IV. JUSTICE IN FAMILY COURTS AT RISK?
The expansion of genetic knowledge in psychiatry raises hopes for improved prevention and treatment options,44 but the use of such data in child custody proceedings heightens concerns about misunderstanding of genetic data and the possible unintended consequences for parent-litigants whose mental health is being questioned. This study explored how the introduction of a parent’s psychiatric genetic evidence may affect public perceptions about child custody decisions and genetic essentialist thinking relating to psychiatric conditions. It also explored how explicit and implicit stigma of psychiatric conditions—a leading cause for discrimination—may affect public perceptions about child custody decisions. The dual exploration of stigma and psychiatric genetic data resonates with recent anti-stigma campaigns to reconceptualize psychiatric conditions as ‘a disease like any other’ by educating the public about the genetic underpinnings of such conditions.45 It also expands on existing scholarship as neither the impact of psychiatric genetic evidence nor stigma on public perceptions of child custody decisions has been explored previously in an empirical study.
The introduction of genetic evidence did not significantly affect views on custody decisions. Participants who read a vignette describing family history of bipolar disorder, genetic results showing propensity to bipolar disorder, or both were not more likely than those who read a vignette with neither family history nor genetic results to indicate that they would deny joint custody to the putatively unfit parent. This finding is contrary to our expectation. The reasons for this finding are unclear. Participants’ demographic characteristics (eg race, ethnicity, sex, marital and parental status) did not affect decisions to award custody to the parent-claimant (P > 0.22). Similarly, genetic knowledge of participants in our study (assessed by the sum of correct responses to a 12-item scale) was not associated with custody decisions (P > 0.09). Our finding could thus reflect skepticism about the role of or reluctance to use genetics in life-changing decisions such as parental rights. In this regard, our finding can assuage some worries that psychiatric genetic evidence may be overly influential with the general public (and by extension, judges) and unduly impact judicial outcomes in child custody proceedings.
However, our finding of no association between psychiatric genetic evidence and child custody awards needs to be considered in light of other findings in our study. First, two-thirds of our participants stated that they would have awarded custody to the parent-claimant and a large majority of the participants (>82%) believed that the parent in the vignette had a psychiatric disorder, regardless of whether a diagnosis was said to have been made. As the parent’s behaviors as described in the vignette may have been deemed inappropriate, it seems that participants translated them into parental unfitness—sufficiently to outweigh other parental characteristics (ie the vignette specified that both parents worked throughout their marital life, shared household responsibilities, and equally loved and cared for their child) and to discourage award of joint custody. It also appears that participants attributed the putatively unfit parent’s deviant behaviors to the presence of a psychiatric condition even without a professional diagnostic label,46 and that these attributions too were sufficient to affect views about child custody. This finding highlights how perceptions of behavioral deviancy are entangled with labeling of psychiatric conditions and is troubling.
Second, in line with previous research,47 the introduction of psychiatric genetic evidence was positively associated with genetic essentialist thinking (including when controlling for a diagnosis). Participants who received family history or genetic results were more likely than those who did not receive such evidence to believe that the parent had bipolar disorder and to endorse a larger number of possible treatments. Such participants were also more likely to agree that the parent should be evaluated for prescription medication and admission to a mental hospital—and even be required by judicial order to do so. It can only be speculated why such effects were found among participants who received either family history or genetic results but not both types of evidence. For example, it could be that the general public views family history and genetics as independent sources of impact on mental health outcomes (rather than cumulative sources), thus evoking a similar reaction only when considered separately. It could also be an effect of the sample that received the vignette with both types of evidence, although vignettes were randomly assigned. Still, the positive associations found are important for future consideration of the use of psychiatric genetic evidence in judicial settings. With parental fitness and child safety serving as primary considerations in child custody proceedings, it is possible that these genetic essentialist views of psychiatric conditions and the increased medicalization of the parent’s behaviors overshadowed a direct effect of genetic evidence but played an indirect role in determining participants’ views on child custody decisions.
This possibility is strengthened by our findings on the effects of a psychiatric diagnosis and stigma on child custody decisions and perceptions of parental fitness. As we hypothesized, both a diagnosis of bipolar disorder and higher levels of explicit stigma, assessed by the desire for social distance and perceived dangerousness, strongly shaped participants’ views about awarding custody to the parent-claimant. Although many of our participants expressed willingness to interact with a person similar to the parent in the vignette in various settings (eg at work, as a neighbor), desire to maintain social distance was positively associated with perceptions of dangerousness, and only half expressed willingness to have such a person marry into the family. In addition, responses to the IAT indicated participants’ strong perceived association between psychiatric conditions and bad parenting.
Moreover, our findings of association between perceptions of capability and child custody award merit consideration. As we expected, lower capability scores were associated with awarding child custody to the parent-claimant. Although no significant association was found between participants’ capability scores and genetic evidence, the introduction of a diagnosis of bipolar disorder was associated with lower capability scores relating to the parent’s ability to perform each of the daily activities considered. Similar results were found among participants who believed the parent had a psychiatric disorder, even in the absence of a professional diagnosis. Our findings thus expand on others’ findings on the negative impacts of labeling of psychiatric conditions to include not only a desire for reduced social interaction48 but also preferences regarding parenting rights and negative views about the parent’s capabilities to perform daily activities not directly related to child custody, such as remarrying, owning property, and opening a bank account.
Scholarship on the legal capacity of people with psychiatric conditions has long raised concerns about the myths that a psychiatric diagnosis precludes ability to make daily decisions, and that decision-making capacity is an ‘all or nothing’ phenomenon.49 Others have warned that such conceptualizations may result in loss of legal personhood, with its most extreme form of all-encompassing and hard to reverse guardianship decisions, whereby individuals with psychiatric conditions lose autonomy over matters related to their person and property50 (often referred to as ‘civil death’). Although the parent in our vignette was not under guardianship, our findings of associations between perception of a psychiatric condition (with or without a professional diagnosis) and lower capability scores in areas unrelated to the child custody proceedings provide initial empirical evidence to support these worries.
These findings may have real-time application. Although US and international disability laws prohibit discrimination in family rights,51 there is a long history of discrimination against, and high rate of child custody loss among, parents with psychiatric disabilities.52 And while US law requires that parental fitness be evaluated based on ability not mental health status,53 our findings indicate that the latter, including nonprofessional labeling of ‘deviant behaviors’54 may play a detrimental role in public perspectives on child custody decisions and other aspects of legal personhood. Thus, the need for developing effective stigma-reduction methods cannot be overstated.
Our finding of high implicit bias is particularly concerning for fairness in family law. Research on racial bias in decision-making processes such as employment and criminal justice suggests that implicit biases have greater effects when the decision-maker is (i) unaware of the possibility of bias55 or (ii) engages in complex decisions, especially involving ambiguous information.56 The challenge for parents with psychiatric conditions in child custody disputes is that both of these bias-triggering situations are likely to exist. Studies show that perceptions of incompetence57 and biases regarding people with psychiatric conditions are widespread,58 making conscious rejection of such associations less likely to occur.59 Child custody disputes are typically also highly complex. They involve multiple actors, including family members and various custody evaluators (eg psychologists, psychiatrists, social workers) who have different priorities and whose opinions influence judicial determinations;60 reflect extensive and often inconclusive evidence about family characteristics, parental fitness, environmental factors, and expert opinions;61 and require making emotionally charged and future-oriented decisions under significant time constraints.62 As in criminal cases,63 such complexity tends to evoke biased and stereotyped beliefs affecting judicial decision-making. In child custody proceedings, the triggering of biases may result in parents with psychiatric conditions unjustly losing custody, without the decision-maker even being aware of their impact.64
Although there is growing awareness of the need to debias the public and judicial decision-makers,65 it is unclear how to do so effectively. A 2019 systematic review of 47 interventions found that those that provide practical, action-oriented strategies to override bias and expose participants to counter-stereotypical exemplars are most promising,66 but none of these interventions focused on psychiatric conditions. Efforts to address bias and improve health professional education on disability found that ongoing contact with people with disabilities who are the experts about their needs and challenges is most useful to reduce bias.67 Studies of the general public similarly found that contact with people with psychiatric conditions is associated with reduced bias.68 Further research to identify effective bias-reduction interventions that can be widely implemented and maintained is needed.
IV.A. Limitations
The vignette’s depiction of questionable parental behaviors without many countering arguments may have primed participants to interpret those behaviors as instability undermining parental fitness, irrespective of the introduction of genetic evidence. However, the need for simplification of facts is inherent to vignette studies. Although it is possible that a change to some aspect of the vignette would have produced different outcomes (eg the child’s gender, the description of the parent’s behaviors), this possibility is inherent to every vignette study and can only inform future research. Second, the IAT has been subject to criticism, including its limited ability to predict individual behaviors.69 In this study, administering the IAT at the end of the survey may also raise a concern that participants’ IAT scores had been primed by the vignettes. However, the IAT is the most widely recognized measure of implicit bias and is considered more reliable than other implicit measures.70 Concurrently, since the IAT measures the ‘speed’ of participants’ unconscious responses, the likelihood of the vignettes having such an immediate impact on deeply seated associations so as to affect the IAT scores is largely diminished. Finally, our sample comprised participants from the general public and their views may not reflect those of family court judges, the usual adjudicators of child custody cases. However, it is plausible that judges are influenced by societal, media, and cultural depictions of genetics and psychiatric disorders as members of the general public71 (as was found regarding racial bias in judicial decision-making72). Thus, while our findings are suggestive of how genetic and mental health biases may affect judicial decisions in child custody disputes, further research with judges could provide a more definitive conclusion.
V. CONCLUSION
The introduction of psychiatric genetic evidence did not have the effect we expected on child custody decisions, but it increased the genetic essentialist understanding of psychiatric conditions. This is only a partial reassurance to those concerned with the possible misuse of genetic information in nonclinical settings. Genetic essentialism indicates a misunderstanding of the genetic and environmental underpinning of psychiatric conditions, and it may feed into persisting stigma against parents with, or with predispositions to, psychiatric conditions. It may also reinforce (uninformed) societal presumptions about an association between psychiatric conditions and dangerousness and need for coerced treatment of parents with a psychiatric label, whether professionally or nonprofessionally determined. Our findings of an association between explicit stigma and clear public preference to deny parents with a (or with an alleged) psychiatric condition joint custody, and of implicit attribution of bad parenting to people with psychiatric conditions, are worrying. Research to identify effective interventions and educational programs to address genetic essentialism and to reduce bias against people, including parents, with psychiatric conditions is urgently needed.
Funding
National Human Genome Research Institute grants K01HG008653, RM1HG007257
Disclosure
Maya Sabatello is a member of the NIH All of Us Research Program’s Institutional Review Board.
Supplementary Material
ACKNOWLEDGEMENTS
We thank the judges from the NCJFCJ for their comments and insights on the vignettes.
Footnotes
K.A. Phillips et al., Genetic Test Availability and Spending: Where Are We Now? Where Are We Going?, 37 Health Affairs 710 (2018).
P.F. Sullivan et al., Psychiatric Genomics: An Update and an Agenda, 175 Am. J. Psychiatry 15 (2018).
Deborah W. Denno, Behavioral Genetics Evidence in Criminal Cases: 1994-2007, in The Impact of Behavioral Sciences on Criminal Law 317 (N.A. Farahany ed., 2009); Deborah W. Denno, Courts’ Increasing Consideration of Behavioral Genetics Evidence in Criminal Cases: Results of a Longtitudinal Study, 2011 Mich. St. L. Rev. 967 (2011).
Gary E. Marchant & Jason S. Robert, Genetic Testing for Autism Predisposition: Ethical, Legal and Social Challenges, 9 Hous. J. Health L. & Pol’y 203 (2009); Gary E. Marchant, Genetic Data in Toxic Tort Litigation, 14 J. L. & Pol’y 7 (2006).
Maya Sabatello & Paul S. Appelbaum, Behavioral Genetics in Criminal and Civil Courts, 25 Harv. Rev. Psychiatry 289 (2017) [hereinafter Behavioral Genetics in Criminal and Civil Courts].
Sally McSwiggan, Bernice Elger & Paul S. Appelbaum, The Forensic Use of Behavioral Genetics in Criminal Proceedings: Case of the MAOA-L Genotype, 50 Int’l J. L. & Psychiatry 17 (2017).
M.J. Bakermans-Kranenburg & M.H. van Ijzendoorn, Gene-Environment Interaction of the Dopamine D4 Receptor (DRD4) and Observed Maternal Insensitivity Predicting Externalizing Behavior in Preschoolers, 48 Developmental Psychobiology 406 (2006); B.E. Shees et al., Parenting Quality Interacts with Genetic Variation in Dopamine Receptor D4 to Influence Temperament in Early Childhood, 19 Developmental Psychopathology 1039 (2007); Ariel Knafo, Salomon Israel & Richard P. Ebstein, Heritability of Children’s Prosocial Behavior and Differential Susceptibility to Parenting by Variation in the Dopamine Receptor D4 Gene, 23 Developmental Psychopathology 53 (2011).
Elizabeth Lightfoot, Katharine Hill, & Traci LaLiberte, The Inclusion of Disability as a Condition for Termination of Parental Rights, 34 Child Abuse & Neglect 927 (2010).
Jo C. Phelan, Geneticization of Deviant Behavior and Consequences for Stigma: The Case of Mental Illness, 46 J. Health & Soc. Behav. 307 (2005).
Jo C. Phelan, Lawrence H. Yang & Rosangely Cruz-Rojas, Effects of Attributing Serious Mental Illnesses to Genetic Causes on Orientations to Treatment, 57 Psychiatric Serv. 382 (2006); Jo C. Phelan, Geneticization of Deviant Behavior and Consequences for Stigma: The Case of Mental Illness, 46 J. Health & Soc. Behav. 307 (2005); B.A. Pescosolido et al., “A Disease Like Any Other”? A Decade of Change in Public Reactions to Schizophrenia, Depression, and Alcohol Dependence, 167 Am. J. Psychiatry 1321 (2010) [hereinafter A Disease Like Any Other?].
Craig Hemmens et al., The Consequences of Official Labels: An Examination of the Rights Lost by the Mentally Ill and Mentally Incompetent Since 1989, 52 Community Mental Health J. 272 (2016); Nat’l Council on Disability, Rocking the Cradle: Ensuring the Rights of Parents with Disabilities and Their Children (2012), available at https://ncd.gov/publications/2012/Sep272012 (accessed Jul. 14, 2021); Maya Sabatello & Paul S. Appelbaum, Psychiatric Genetics in Child Custody Proceedings: Ethical, Legal, and Social Issues, 4 Current Genetic Med. Rep. 98 (2016) [hereinafter Psychiatric Genetics in Child Custody Proceedings].
B.A. Pescosolido, The Public Stigma of Mental Illness: What Do We Think; What Do We Know; What Can We Prove?, 54 J. Health & Soc. Behav. 1 (2013).
B.A. Pescosolido et al. The Public’s View of the Competence, Dangerousness, and Need for Legal Coercion of Persons with Mental Health Problems, 89 Am. J. Pub. Health 1339 (1999) [hereinafter The Public’s View].
Bruce G. Link et al., Public Conceptions of Mental Illness: Labels, Causes, Dangerousness, and Social Distance, 89 Am. J. Pub. Health 1328 (1999); Phelan et al., Public Conceptions of Mental Illness in 1950 and 1996: What Is Mental Illness and Is It to be Feared?, 41 J. Health & Soc. Behav. 188 (2000).
Linda Ganzini et al., Ten Myths About Decision-Making Capacity, 5 J. Am. Med. Directors Ass’n 263 (2004); Mohit Varshney et al., Violence and Mental Illness: What is the True Story?, 70 J. Epidemiology & Community Health 223 (2016); Jeffrey W. Swanson, Mental Illness and Reduction of Gun Violence and Suicide: Bringing Epidemiologic Research to Policy, 25 Annals Epidemiology 366 (2015).
Angela M. Parcesepe & Leopoldo J. Cabassa, Public Stigma of Mental Illness in the United States: A Systematic Literature Review, 40 Admin. Pol’y Mental Health 384 (2013).
B.A. Pescolido, Bianca Manago & John Monahan, Evolving Public Views On The Likelihood Of Violence From People With Mental Illness: Stigma And Its Consequences, 38 Health Aff. 1735 (2019).
Jo C. Phelan, Geneticization of Deviant Behavior and Consequences for Stigma: The Case of Mental Illness, 46 J. Health & Soc. Behav. 307 (2005); Nick Haslam, Genetic Essentialism, Neuroessentialism, and Stigma: Commentary on Dar-Nimrod and Heine, 137 Psychol. Bull. 819 (2011).
Jerry Kang et al., Implicit Bias in the Courtroom, 59 UCLA L. Rev. 1124 (2012).
Nicholas Scurich & Paul S. Appelbaum, The Blunt-Edged Sword: Genetic Explanations of Misbehavior Neither Mitigate nor Aggravate Punishment, 3 J. L. & Biosciences 140 (2016); Lisa G. Aspinwall, Teneille R. Brown & James Tabery, The Double-Edged Sword: Does Biomechanism Increase or Decrease Judges’ Sentencing of Psychopaths?, 337 Science 846 (2012); Johannes Fuss, Harald Dressing & Peer Briken, Neurogenetic Evidence in the Courtroom: A Randomised Controlled Trial with German Judges, 52 J. Med. Genetics 730 (2015); Colleen M. Berryessa, Judicial Stereotyping Associated with Genetic Essentialist Biases Toward Mental Disorders and Potential Negative Effects on Sentencing, 53 L. & Soc’y Rev. 202 (2019).
Vered Ben-David, Judicial Bias in Adjudicating the Adoption of Minors in Israel, 33 Child. & Youth Serv. Rev. 195 (2011); Jeffrey J. Rachlinski et al., Does Unconscious Racial Bias Affect Trial Judges?, 84 Notre Dame L. Rev. 1195 (2009); Andrea L. Miller, Expertise Fails to Attenuate Gendered Biases in Judicial Decision-Making, 10 Soc. Psychol. & Personality Sci. 227 (2019).
Maya Sabatello et al. The Psychiatric Genetic Data of Children in Proceedings to Terminate Parental Rights. 49(2) J Am Acad Psychiatry Law Online,166–178 (2021). doi: 10.29158/JAAPL.200066-20.
Mairi Levitt, Perceptions of Nature, Nurture and Behaviour, 9 Life Sci., Soc’y & Pol’y 13 (2013).
Pescosolido, supra note 12.
Deirdre M. Smith, The Disordered and Discredited Plaintiff: Psychiatric Evidence in Civil Litigation, 31 Cardoza L. Rev. 749 (2009).
Maya Sabatello & Paul S. Appelbaum, Behavioral Genetics in Criminal and Civil Courts, Harv. Rev. Psychiatry 289 (2017).
Lightfoot, Hill, & LaLiberte, supra note 8; Barry J. Ackerson, Parents With Serious and Persistent Mental Illness: Issues in Assessment and Services, 48 Soc. Work 187 (2003).
Pescosolido, Manago, & Monahan, supra note 17.
Anat S. Geva, Judicial Determination of Child Custody When a Parent is Mentally Ill: A Little Bit of Law, a Little Bit of Pop Psychology, and a Little Bit of Common Sense, 16 U.C. Davis J. Juv. L. & Pol’y 1 (2012); D.T. Marsh, Parental mental illness: Issues in custody determinations, 23 Am. J. Fam. L. 28 (2009).
Katy Kaplan et al., Child Protective Service Disparities and Serious Mental Illnesses: Results From a National Survey, 70 Psychiatric Serv. 202 (2019).
Mark S. Salzer et al., Custody Challenges Experienced by Parents with Serious Mental Illnesses Outside of Child Protective Services Proceedings, Psychiatric Rehabilitation J. (Oct. 8, 2020), https://pubmed.ncbi.nlm.nih.gov/33030933/ (accessed Jul. 14, 2021).
Loran B. Kundra & Leslie B. Alexander, Termination of Parental Rights Proceedings: Legal Considerations and Practical Strategies for Parents with Psychiatric Disabilities and the Practitioners Who Serve Them, 33 Psychiatric Rehabilitation J. 142 (2009); Nat’l Council on Disability, Rocking the Cradle: Ensuring the Rights of Parents with Disabilities and Their Children (2012), available at https://ncd.gov/publications/2012/Sep272012 (accessed Jul. 14, 2021).
Fatos Selita et al., Judging in the Genomic Era: Judges’ Genetic Knowledge, Confidence and Need for Training, 28 Eur. J. Hum. Genetics 1322 (2020).
Miller, supra note 21; Rachlinski et al., supra note 21.
Psychiatric Genetics in Child Custody Proceedings, supra note 11.
Anat S. Geva, Judicial Determination of Child Custody When a Parent is Mentally Ill: A Little Bit of Law, a Little Bit of Pop Psychology, and a Little Bit of Common Sense, 16 U.C. Davis J. Juv. L. & Pol’y 1 (2012); D.T. Marsh, Parental mental illness: Issues in custody determinations, 23 Am. J. Fam. L. 28 (2009).
Anthony G. Greenwald, Brian A. Nosek & Mahzarin R. Banaji, Understanding and Using the Implicit Association Test: I. An Improved Scoring Algorithm, 85 J. Personality & Soc. Psychol. 197 (2003).
Phelan, Yang, & Cruz-Rojas, supra 10; A Disease Like any Other?, supra note 10.
A Disease Like Any Other?, supra note 10; Bruce G. Link et al. Measuring Mental Illness Stigma, 30 Schizophrenia Bull. 511 (2004).
Jo C. Phelan & Bruce G. Link, Fear of People with Mental Illnesses: The Role of Personal and Impersonal Contact and Exposure to Threat or Harm, 45 J. Health Soc. Behav. 68 (2004); Bruce G. Link & Francis T. Cullen, Contact with the Mentally Ill and Perceptions of How Dangerous They are, 27 J. Health Soc. Behav. 289 (1986).
Project Implicit, https://implicit.harvard.edu/implicit/aboutus.html (accessed Nov. 11, 2020).
Bethany A. Teachman, Joel G. Wilson & Irina Komarovskaya, Implicit and Explicit Stigma of Mental Illness in Diagnosed and Healthy Samples, 25 J. Soc. & Clinical Psychol. 75 (2006).
Lightfoot, Hill, & LaLiberte, supra note 8.
Sullivan, supra note 2.
A Disease Like Any Other?, supra note 10.
A.F. Jorm & K.M. Griffiths, The public’s stigmatizing attitudes towards people with mental disorders: how important are biomedical conceptualizations?, 118 Acta Psychiatrica Scandinavica 315 (2008).
Jo C. Phelan, Geneticization of Deviant Behavior and Consequences for Stigma: The Case of Mental Illness, 46 J. Health & Soc. Behav. 307 (2005); A Disease Like Any Other?, supra note 10; Laura Bennett, Kathryn Thirlaway & Alexandra J. Murray, The Stigmatising Implications of Presenting Schizophrenia as a Genetic Disease, 17 J. Genetic Counseling 550 (2008).
Jack K. Martin, B.A. Pescosolido, & Steven A. Tuch, Of Fear and Loathing: The Role of “Disturbing Behavior,” Labels, and Causal Attribution in Shaping Public Attitudes Toward People with Mental Illness, 41 J. Health & Soc. Behav. 208 (2000).
Ganzini et al., supra note 15.
Bernadette McSherry, Decision-Making, Legal Capacity and Neuroscience: Implications for Mental Health Laws, 4 Laws 125 (2015); Sheila E. Shea and Carol Pressman, Guardianship: A Civil Rights Perspective (2018), https://nysba.org/NYSBA/Publications/Bar%20Journal/Guardianship%20A%20Civil%20Rights%20Perspective.pdf (accessed Jul. 14, 2021); Sydney J. Sell, A Potential Civil Death: Guardianship of Persons with Disabilities in Utah, 1 Utah L. Rev. 215 (2019); Michael L. Perlin, Striking for the Guardians and Protectors of the Mind: The Convention on the Rights of Persons with Mental Disabilities and the Future of Guardianship Law, 117 Penn. State L. Rev. 1159 (2013).
Nat’l Council on Disability, supra note 11; G.A. Res. 61/106, Convention on the Rights of Persons with Disabilities (Dec. 13, 2006).
Robyn M. Powell, Family Law, Parents with Disabilities, and the Americans with Disabilities Act, 57 Fam. Ct. Rev. 37 (2019); Nat’l Council on Disability, supra note 11.
Geva, supra note 29.
Jorm & Griffiths, supra note 46.
Rachlinski et al., supra note 21; Alexander R. Green et al., Implicit Bias Among Physicians and Its Prediction of Thrombolysis Decisions for Black and White Patients, 22 J. Gen. Internal Med. 1231 (2007); Javeed Sukhera et al., Adaptive Reinventing: Implicit Bias and the Co-Construction of Social Change, 23 Advances Health Sci. Educ. Prac. 587 (2018); Christine Jolls & Cass R. Sunstein, Symposium on Behavioral Realism: The Law of Implicit Bias, 94 Cal. L. Rev. 969 (2006).
John F. Dovidio & Samuel L. Gaertner, Aversive Racism and Selection Decisions: 1989 and 1999, 11 Psychol. Sci. 315 (2000); Justin D. Levinson, Huajin Cai & Danielle Young, Guilty by implicit racial bias: The guiltly/not guilty Implicit Association Test, 8 Ohio St. J. Crim. L. 187 (2010).
The Public’s View, supra note 13.
A Disease Like Any Other?, supra note 10.
Kang et al., supra note 19; James Babikian, Cleaving the Gordian Knot: Implicit Bias, Selective Prosecution & Charging Guidelines, 42 Am. J. Crim. L. 139 (2015).
Lisa Kalich et al., Evaluating the Evaluator: Guidelines for Legal Professionals in Assessing the Competency of Evaluations in Termination of Parental Rights Cases, 35 J. Psychiatry L. 365 (2007); Robert E. Emery, Randy K. Otto & William T. O’Donohue, A Critical Assessment of Child Custody Evaluations: Limited Science and a Flawed System, 6 Psychol. Sci. Pub. Int. 1 (2005).
Kang et al., supra note 19.
Geva, supra note 29; Jolls & Sunstein, supra note 55; Fatma Marouf, Implicit Bias and Immigration Courts, 45 New England L. Rev. 417 (2011).
Levinson, Cai & Young, supra note 56; Martha A. Myers & John Hagan, Private and Public Trouble: Prosecutors and the Allocation of Court Resources, 26 Soc. Probs. 439 (1979).
Jolls & Sunstein, supra note 55.
Rachlinski, supra note 21; Jolls & Sunstein, supra note 55.
Chloë FitzGerald et al., Interventions Designed to Reduce Implicit Prejudices and Implicit Stereotypes in Real World Contexts: A Systematic Review. 7 BMC Psychol. 29 (2019).
Tom Shakespeare & Ira Kleine, Educating Health Professionals About Disability: A Review of Interventions, 2 Health & Soc. Care Educ. 20 (2013).
Laurel A. Alexander & Bruce G. Link, The Impact of Contact on Stigmatizing Attitudes Toward People with Mental Illness, 12 J. Mental Health 271 (2003); Jennifer E. Boyd et al., The Relationship of Multiple Aspects of Stigma and Personal Contact with Someone Hospitalized for Mental Illness, in a Nationally Representative Sample, 45 Soc. Psychiatry & Psychiatric Epidemiology 1063 (2010).
FitzGerald et al., supra note 66.
Greenwald, Nosek & Banaji, supra note 37.
Kang, supra note 19; Terry Carter, Implicit Bias is a Challenge Even for Judges, ABA J. (Aug. 5, 2016), https://www.abajournal.com/news/article/implicit_bias_is_a_challenge_even_for_judges (accessed Jul. 14, 2021).
Rachlinski et al., supra note 21.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


