Abstract
BACKGROUND:
Suspension trauma syndrome is a life-threatening event that occurs when a person is “trapped” in a prolonged passive suspension. It is most commonly seen in people who engage in occupational or sport activities that require harness suspension. The aim of this study is to identify the predisposing factors, pathophysiology, and management of suspension trauma.
METHODS:
A review and analysis of the literature published in English and Spanish from 1972 to 2020 on suspension trauma were performed. Search sources were PubMed, Medline, Cochrane Library, MeSH, UpToDate, and Google Scholar. Articles referring to suspension trauma associated with other injury mechanisms (traumatic impact injuries, drowning, asphyxiation, or bleeding), case reports, and pediatric population were excluded.
RESULTS:
Forty-one articles were identified. Of these, 29 articles related to mechanism, pathophysiology, and management of individuals who suffered prolonged suspension trauma without associated traumatic injuries were included in the study. We encountered several controversies describing the putative pathophysiology, ranging from blood sequestration in the lower extremities versus accumulation of metabolic waste and hyperkalemia to dorsal hook-type harness as a trigger cause of positional asphyxia; to vascular compression of femoral vessels exerted by the harness causing decreased venous return. Pstients suspended in a full-body harness with dorsal hook showed more hemodynamic alterations in response to the compressive effect on the rib cage, causing a reduction in perfusion by presenting a decrease in pulse pressure. Management strategies varied across studies.
CONCLUSIONS:
Progress has been made in individualizing the population at risk and in the management of suspension trauma. We recommend the formation of consensus definitions, larger cohort or registry studies to be conducted, and experimental animal models to better understand the mechanisms in order to develop management and life support guidelines from a trauma and emergency medicine perspective.
Keywords: Suspension trauma, Reflux syndrome, Suspension trauma syndrome, Harness suspension
INTRODUCTION
Suspension trauma syndrome (STS) was first described in a report of autopsies of people who died suspended by a harness in Austria and Spain.[1] There were minimal findings related to traumatic injuries, and it was therefore concluded that the cause of death was due to shock.[1] STS is also known as harness hang syndrome, harness-induced trauma, harness-induced pathology, and orthostatic shock while suspended. It is defined as the development of presyncope symptoms and loss of consciousness if the human body is held motionless in a vertical position forsome time.[2] People with prolonged suspension in a harness can die in an expedited fashion and without significantly associated trauma. This syndrome can occur in people who practise activities using harness systems with a dorsal or chest point of attachment as used by painters and builders of high-rise buildings, towers, bridges, marine platforms, power plants, or with a frontal waist point of attachment in sports and recreational activities such as mountaineering, rock climbing, skydiving, paragliding, via ferrata, canyoning, and caving.[3] It can evolve rapidly leading to the state of unconsciousness and eventually death.[3] The term “harness suspension” was originally used to describe STS, but it is not really the harness that is at issue. Pain and respiratory compromise are the issue more than the trauma per se, and any condition that decreases central intravascular volume prior to suspension (i.e., dehydration, hypothermia, fatigue) increases risk.
The objectives of this study are to review the current literature to describe the pathophysiology of STS, identify predisposing factors, and discuss the controversies regarding its management.
METHODS
Data sources and search strategy
A review of the literature published in English and Spanish languages from 1972 to 2020 on suspension trauma was performed. The preference of the languages is based on the ability of the authors to speak those. An exhaustive review of articles published in Pubmed, Medline, Cochrane Library, MeSH, UpToDate, and Google Scholar was executed. The search words used were harness syndrome, suspension syndrome, suspension trauma, suspension shock, harness hang syndrome, suspension stress, reflow syndrome, orthostatic intolerance, orthostatic syndrome, rescue death, rock climbing, harness accident, combinations of these words, and the use of “and” or “or” when feasible. This work was reported in line with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) and Assessment of Multiple Systematic Reviews (AMSTAR) guidelines.
Study selection criteria
Articles referring to STS associated with other injury mechanisms such as traumatic impact injuries, drowning, asphyxiation or bleeding, as well as isolated clinical case reports, pediatric population, and publications other than English or Spanish were excluded.
Data extraction
The first author (PP) supervised the entire process from the selection of qualifying articles to the way the extraction took place. A set of data was independently extracted by one international research fellow (IRF-SEV), and then verified by PP. In turn, PP extracted the second set of data, and then it was verified by IRF-SEV. The data extracted from the articles included in this review were organized using a data extraction table with the following categories: author, year of publication, type of study, number of patients, age, gender, and modality of injury.
Risk of bias
An assessment of risk of bias was performed per each individual study, using the Newcastle-Ottawa Quality Assessment Scale for both case-control studies and cohort studies as valid evaluation tool.
RESULTS
Forty-one articles related to STS were identified. Of these, 29 articles related to mechanism, pathophysiology and management of individuals who suffered prolonged suspension trauma without associated traumatic injuries were included in the study. The PRISMA flow diagram is shown in Figure 1. The Newcastle-Ottawa Quality Assessment Scale was used.
Figure 1.
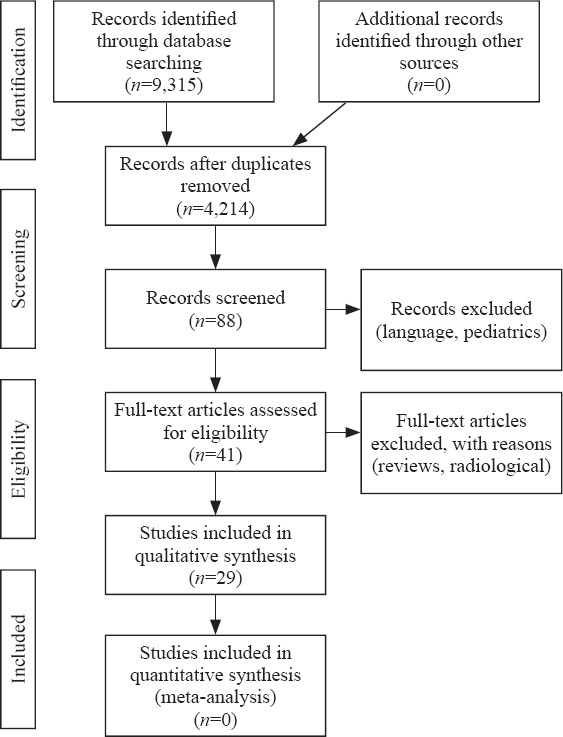
Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flow diagram.
Controversies were found regarding the physiopathological aspects involved in STS. Predisposing factors related to the type of harness and differences in the recommendations in the initial management to reduce the risk of post-rescue death were identified. As for the physiopathology of this syndrome, one theory[4] supports the sequestration of blood in the lower extremities by a deficient muscular pump (Figure 2) causing low cardiac output, while a second theory[4] supports metabolic waste accumulation and hyperkalemia when anaerobic muscular metabolism is produced. Another theory[5] is that harnesses with a dorsal hook may be a trigger of positional asphyxia and vascular compression of arteries and femoral veins exerted by the harness in the inguinal region causing a decrease in venous return as opposed to ventral hook harnesses in which this effect is less severe.
Figure 2.
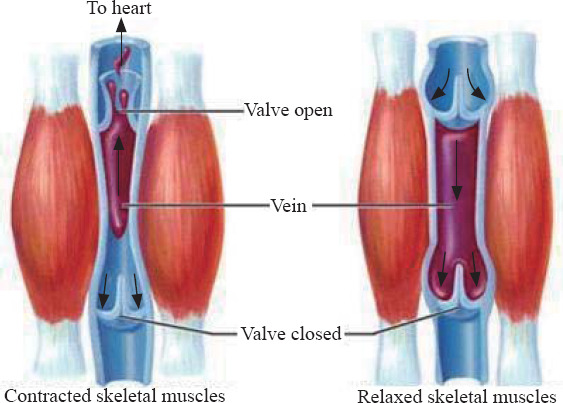
Lower extremity skeletal-muscle pump.
The first series[4] of cases of death due to STS was published in 1970. A research group studied the cause of death in ten climbers with no physical injury who were suspended on their own harnesses from 90 minutes up to eight hours. Eight patients were rescued and extricated and survived from 30 minutes to 11 days after their rescue. Eventually, all eight patients died.
In 1972, another series[3] of cases was published in which ten out of 23 climbers died after being suspended on their harness, although they did not suffer any traumatic injuries (e.g., fractures or solid organ damage). Damisch and Schauer[6] in 1985 performed 46 suspension tests on various types of harnesses for up to 10 minutes. No one lost consciousness, but two individuals with harnesses with dorsal hooks had to stop the test by presenting undetectable blood pressure between five and nine minutes of suspension. Harry[7] conducted a study on the type of harness used in parachuting. During this study, one of the participants lost consciousness after six minutes of suspension on a body harness.
A group of French speleology doctors also performed autopsies on patients who died suspended by a harness. This group initially indicated that 10 of the 12 individuals died from hypothermia, but in contradiction to their theory, many of these subjects had lost consciousness very quickly. For this reason, they decided to conduct a study reproducing the same circumstances in a laboratory. The participants were asked to act as if they were unconscious hanging from a harness. The first two participants effectively lost consciousness at seven and thirty minutes, respectively, and the study was stopped. Later on, during a second attempt of the same study but only modifying certain parameters, a participant lost consciousness after six minutes. They concluded that hypothermia was not the cause of death in these patients.[8]
Pathophysiology of suspension trauma
One of the hypotheses that explain STS is the accumulation of blood in the lower extremities due to gravity and proximal compression, which diminishes venous return. This compression causes a reduction in cardiac preload and a concomitant decrease in cardiac output and tissue perfusion. Eventually, this effect is manifested clinically as a loss of consciousness and cardiac arrest. This physiological phenomenon has been observed during military parades, in operating rooms and historically during crucifixions.[9-11] Regarding the pathophysiological aspects involved, certain conditions that endanger the life of these patients have been established.
Compression of blood circulation in limbs
Due to the prolonged suspension in an upright position, these individuals have an accumulation of blood volume in their lower extremities, reaching up to 20% of the total blood volume and causing orthostatic hypotension. Further, the compression of the femoral veins by the harness causes a profound decrease in preload.[12]
Under normal conditions, acidosis from anaerobic metabolism decreases vascular resistance to allow an increase in blood flow, thus increasing the supply of oxygen and while eliminating waste products. However, when the lower extremities are immobilized in suspension by the harness, blood sequestration in the peripheral region, which contains highly acidotic venous blood, is markedly increased. Figure 3 shows the sequence of this syndrome.
Figure 3.
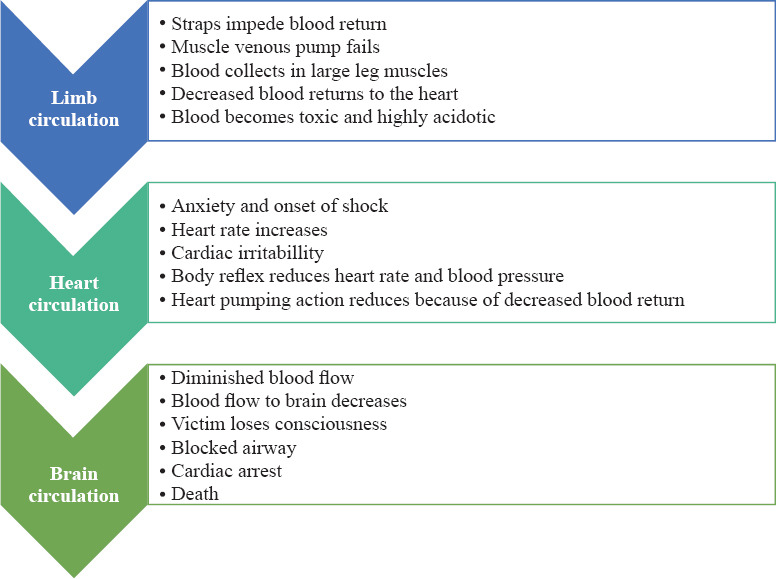
Progression of suspension trauma.
Impaired cardiac and respiratory functions
In addition to the decrease in pre-load, after-load and cardiac output, there is a release of adrenaline into the bloodstream as a result of the fear and anxiety experienced by the individual who is suspended. Initially, there is an increase in the frequency and intensity of cardiac contractions as a compensatory mechanism in an attempt to maintain cerebral blood flow, which then leads to the presence of pre-syncopal symptoms, such as nausea, dizziness, sweating, confusion, loss of vision, buzzing, and vertigo. This condition is known as distributive shock and includes a decrease in heart rate, blood pressure, and cardiac output.[13,14] Madsen et al[15] reported in their study of 69 patients pre-syncopal symptoms presenting at 27 minutes after the start of the test with heart rates ranging from 30 to 57 beats per minute.
The decrease in blood pressure mentioned above causes stimulation of baro-receptors and activates the sympathetic autonomic system. This produces an increase in heart rate and blood pressure as a temporary response. However, the decrease in intracardiac volume may induce the presence of paradoxical bradycardia and hypotension as seen in the Bezold-Jarisch reflex.[16]
Peripheral vasoconstriction plays a central role in maintaining blood pressure. Convertino[17] found that the control of systemic vascular resistance was greater in high tolerant orthostasis participants compared with low, in line with greater elevations in the circulating vasopressor hormones (vasopressin, angiotensin, and norepinephrine).
In a recent investigation, Lanfranconi et al[18] reported that participants who did not develop STS were able to activate remedial responses through the O2 transport and utilization chain of various intensities to defend brain oxidative metabolism needs. On the other hand, suspension triggered an imbalanced response of respiratory and cardiovascular reflexes leading to critical cerebral hypoxia. Their findings indicate that the ability to cope with hanging motionless in harness occurs in people developing less marked as well as more rapidly fading of fluctuations in both respiratory and cardiovascular reflex responses. Conversely, wider fluctuations in control of variations of the ventilation and blood pressure result in a progressive decrease in tolerance to suspension, while the imbalance leading to cerebral hypoxia is an early phenomenon (10–12 minutes from the start of the suspension test) irreversibly ending in syncopal event.
Brain circulation failure
STS is a risk that specifically affects wide ranges of situations. An irreversible orthostatic stasis could lead to death if a prompt rescue is not performed. Lanfranconi et al[19] performed a suspension test on 40 adults lasting almost half an hour. They came to the conclusion that the participants who developed STS failed to activate cardiovascular reflexes that usually safeguarded O2 availability to match the metabolic needs of the brain tissue. As was previously described, syncope occurs as a compensatory action. As a result, when an individual falls to the ground, his or her horizontal position allows the lower extremities, heart, and brain to remain at the same level thus restoring blood flow. On the contrary, suspended individuals are unable to counteract this condition by remaining relatively upright in their harnesses. The decrease in heart rate and blood pressure caused by increased vagal autonomic response further causes a deficiency of blood flow. Loss of consciousness may also block the airway, depending on the position of the head.
Post-rescue death
There is no established hypothesis in the literature about the mechanism of post-rescue death. Published reviews indicate that the acidotic blood volume produced through anaerobic metabolism is accumulated in the veins of lower extremities and returns to the heart abruptly, which may lead to heart failure. Although acidosis may temporarily depress cardiac contractility, it has little or no effect on heart rhythm. Therefore, changes in pH are unlikely to cause sudden death.[20]
Cardiac dysrhythmia is caused by sinus arrhythmia and premature ventricular contractions, as seen in the electrocardiograms (EKG) in the experimental study by Stuhlinger et al.[21] Allister[22] reported the case of a man who suffered crush injuries of his legs for eight hours and suffered cardiac arrest one hour after his release. Potassium released from damaged muscle cells is one of the most important blood components present in suspension syndrome. On presentation, the pH was 7.15 and during resuscitation the potassium level was 8.0 mEq/L with peaked T waves. The patient was treated with bicarbonate and insulin with glucose and survived.
Blaisdell[23] in their study found platelet and fibrin residues in the lungs of these individuals after blood reperfusion and interpreted it as a delayed inflammatory response rather than a cause of sudden death.
Pulmonary embolism after periods of blood stasis may present a clinical resemblance to sudden death, but Patscheider[24] found no clots or mechanical obstructions in the autopsies described in his study.
Predisposing factors
Suspension time
The onset of this syndrome is completely unpredictable, but a 2006 Occupational Safety and Health Administration (OSHA) guideline defined increased mortality to be suspended for more than thirty minutes.[25]
Height
It has been reported that when individuals are suspended more than five feet from the ground, the risk of STS increases.[4]
Age and gender
One of the factors that can be identified as predisposing is age, as older patients have poorer cardiac and arterial functions,[3] but gender does not affect risk.[1]
Weight
Increased weight has led to the decreased mean arterial pressure in the lab setting.[1]
Types of harness
There are several types of harnesses used by individuals who work at height. These include chest, dorsal, seat type, positioning, and full-body harnesses. There are controversies about which type of harness may portend an increased risk for this pathology to occur. Some groups indicate that harnesses may cause cardiorespiratory involvement as they cause positional asphyxia. The dorsal harness produces a decrease in blood flow creating functional hypovolemia by limiting the physiological movement of the rib cage and diaphragm. This decreases the respiratory volume and increases intrathoracic pressure resulting in a decrease in preload and cardiac output.[26]
Beverly et al[13] reported an increased frequency of this syndrome in patients with dorsal harnesses. They conducted a prospective randomized study on the differences according to the types of harness (frontal or dorsal) for 30 minutes, and concluded that full-body harness was the best tolerated (range 5–30 minutes) when compared to dorsal or belt harnesses. Another finding was that staying in suspension for 30 minutes using the frontal-type harness did not result in significant hemodynamic changes. The duration of the test was shorter in those who wore dorsal harnesses, because many of them experienced dizziness, indicating the onset of more severe hemodynamic dysfunction. In individuals with dorsal harnesses, an increase in heart rate was noted as a compensatory autonomic response to the decrease in pulse pressure and heart volume. This decrease in pulse pressure, when associated with the presence of dizziness, may indicate the onset of poor cerebral perfusion. When comparing the results with the frontal harness, no changes in heart rate were identified in this group. On the other hand, the assessment of mean blood pressure showed an increase in number without seeing a clear decrease in pulse pressure. Biologic markers of muscle damage were also evaluated. The results showed that in the dorsal harness group, an increase of aspartate aminotransferase was seen in plasma. This result could be explained by the compressive effect on the groin exerted by harness strips causing muscular ischemia in this site. Turner et al[27] supported the theory of this group. They determined that 50% of individuals wearing dorsal harnesses experienced symptoms after 31 minutes of suspension.
Management of suspension trauma
Some authors have questioned the existence of suspension trauma, but it is clear that persons suspended in a harness can die more quickly than expected and with no significant trauma. Clearly, this is a shock syndrome in its early phase complicated by rhabdomyolysis in its late phase survivors.[1] The shock is secondary to failure of the venous pump to return sufficient volume to central circulation. Treatment starts with immediate rescue of a suspended person, always following Advanced Trauma Life Support® (ATLS®) guidelines. Oxygen and immediate intravenous fluid administration to prevent crush syndrome is appropriate but should not delay rescue. Early first-aid care appears to be vital, even before the arrival of professional emergency medical care.[28] Research teams recommend starting the rescue of these patients promptly. If the patient is conscious, he or she should be instructed to move his or her legs vigorously upwards, thus creating muscle work to mitigate the pre-syncopal symptoms.
If unconscious, the patient should be released from the harness as soon as possible. In this situation, it is recommended to keep the patient in a semi-fowler position by keeping his or her torso in an elevated position at approximately an angle of 30–40º, and then slowly moving him or her to the supine position in a period between 30 and 45 minutes. There is controversy regarding the initial management since the lack of oxygenated blood received by the brain during this suspension period is potentially lethal. Certain groups claim that it is even riskier to place these patients in the supine position immediately after the rescue due to the reflux that can cause death by producing an acute overload of volume to the right ventricle by massive return of blood. In a study[21] of ten volunteer individuals who remained suspended by a harness until they showed signs of circulatory collapse and were immediately placed horizontally, it was identified that some of the individuals presented with sinus arrhythmia and ventricular extrasystoles. The authors concluded that the rapid venous return of accumulated blood could induce cardiac failure and death. Currently, there is no scientific evidence to support this theory that justifies changes in the guideline’s management and principles of life support.[9]
On the contrary, Blaisdell[23] contradicted the theory of reflux death syndrome. When studying the pathophysiology of reperfusion syndrome in skeletal muscle ischemia, they noted that suffering from lack of blood flow in muscle cells caused edema and further increased ischemia. The early restoration of blood circulation will limit the additional loss of volume in the interstitium by reducing edema. The authors suggest that the patient should be released from the harness and placed supine as soon as possible to restore oxygenated blood flow to the damaged muscle. Maintaining the vertical position in these individuals will simply worsen muscle damage and hypovolemic shock. These patients should be transferred to a hospital following the guidelines of ATLS®.
Intravenous hydration should be initiated to increase diuresis and decrease the risk of renal failure, preferably with isotonic saline followed by hypotonic saline with bicarbonate if necessary. Hypoglycemia should be avoided by correcting blood glucose levels with 25 g intravenous bolus with 50% dextrose. It is not recommended to administer intravenous potassium until clearly indicated.[4] Appropriate pain relief should be administered to reduce stress due to pain and anxiety in these patients.
In addition, it is very important to perform an EKG in search of alterations such as the presence of peaked T waves suggesting hyperkalemia, prolongation of the QT interval, and widened QRS complexes. Blood pressure should be monitored since the presence of high blood pressure may indicate hyperkalemia and the onset of suspension syndrome. These patients should be immediately transferred to a hospital with appropriate knowledge of the management of trauma patients (Figure 4) and preferably with dialysis capabilities.
Figure 4.
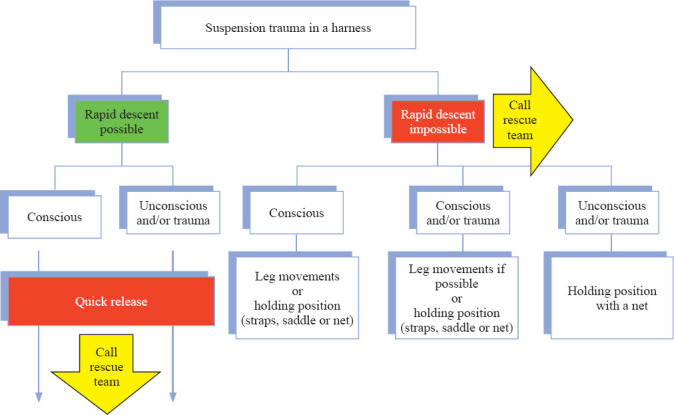
Algorithm for the initial management of suspension trauma patients.[26]
Recommended prevention measures for the population at risk of STS are: (1) use of complete harness, including trauma straps, preferably frontal type, with support of the lower extremities for lift; (2) early mobilization of the lower extremities in conscious patients to avoid hemostasis and aid in the activation of the muscle pump; (3) people who work or perform sports involving suspension by a harness must always be accompanied. By doing so, request for help to rescue can be faster, decreasing the time of passive suspension.[2,29-31]
Complications
Rhabdomyolysis is a well-described complication of STS. It is produced by the compressive effect of the harness on the lower extremities, with the consequent decrease in blood flow, poor muscle irrigation, and hemostasis. Damaged muscle cells release myoglobin causing acute renal failure. Flora and Holzl[32] published a series of ten patients who died of STS, where seven of them died immediately after rescue, and one at 11 days after rescue from renal failure.
Limitations
The study has a number of limitations. This is a literature review with inherent problems. Due to the retrospective nature of the study based on several other authors’ publications, the authors were careful to select articles focused only on physiopathology, management, and prevention. Additionally, some of the referenced articles included in this review are a bit older, as only a few research studies have been published on this topic. These factors in combination encouraged the authors to review the subject and write this manuscript.
CONCLUSIONS
STS represents a risk for individuals performing suspension activities with a harness. Currently, the modernization of the harness design and the development of safety guidelines have made this activity safer than before. Several studies support the front-type harness over the dorsal hook harness. In order to apply the most appropriate recommendations, we recommend larger studies based on scientific evidence where the safety would also be a concern, as well as experimental animal models, in order to develop management and life support guidelines from a trauma and emergency medicine perspective.
As a take-home message, the basics of STS management can be summarized as follows: (1) remove the person from the rope: be sure that the scene is safe, if the patient can cooperate, ask to move and raise his/her legs; (2) lay the patient flat and start ATLS protocols with no delay: airway, breathing, circulation (ABC), plus hypothermia prevention; (3) oxygen, monitoring, intravenous fluid if available (alternate saline and half-normal saline with added bicarbonate); (4) remove the harness and transport the patient to a facility capable of dialysis if he or she has been suspended passively for more than two hours.
Footnotes
Funding: None.
Ethical approval: This study is a literature review, and there is no need for an informed consent.
Conflicts of interests: The authors declare that they have no competing interests.
Contributors: PP proposed the study and wrote the paper. All authors contributed to the design and interpretation of the study and to further drafts.
REFERENCES
- 1.Mortimer RB. Risks and management of prolonged suspension in an Alpine harness. Wilderness Environ Med. 2011;22(1):77–86. doi: 10.1016/j.wem.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 2.Lee C, Porter KM. Suspension trauma. Emerg Med J. 2007;24(4):237–8. doi: 10.1136/emj.2007.046391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rauch S, Schenk K, Strapazzon G, Dal Cappello T, Gatterer H, Palma M, et al. Suspension síndrome:a potencially fatal vagally mediated circulatory collapse—an experimental randomized crossover trial. Eur J Appl Physiol. 2019;119(6):1353–65. doi: 10.1007/s00421-019-04126-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Raynovich B, Rwaili FT, Bishop P. Dangerous suspension. Understanding suspension syndrome and prehospital treatment for those at risk. JEMS. 2009;34(8):44–51. doi: 10.1016/S0197-2510(09)70215-3. [DOI] [PubMed] [Google Scholar]
- 5.Pasquier M, Yersin B, Vallotton L, Carron PN. Clinical update:suspension trauma. Wilderness Environ Med. 2011;22(2):167–71. doi: 10.1016/j.wem.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 6.Damisch C, Schauer N. How safe are body harnesses? Der Bergsteiger. 1985:6F–9F. [Google Scholar]
- 7.Harry G. Armstrong aerospace medical research laboratory, Wright-Patterson Air Force Base, OH1987. Available at http: //www.ww35.usafunithistory.com/PDF/A-E/AEROSPACE%20MEDICAL%20RESEARCH%20LAB.pdf . [PubMed]
- 8.Bariod J. Sensitization to pathology induced by use harness. In: Grimbérieux J, Ek C, editors. Proceeding of European Conference of Speleology. Helecine, Belgium: International Union of Speleology; 1992. pp. 49–55. [Google Scholar]
- 9.Thomassen O, Skaiaa SC, Brattebo G, Heltne JK, Dahlberg T, Sunde GA. Does the horizontal position increase risk of rescue death following suspension trauma? Emerg Med J. 2009;26(12):896–8. doi: 10.1136/emj.2008.064931. [DOI] [PubMed] [Google Scholar]
- 10.Edwards WD, Gabel WJ, Hosmer FE. On the physical death of Jesus Christ. JAMA. 1986;255(11):1455–63. [PubMed] [Google Scholar]
- 11.Maslen MW, Mitchell PD. Medical theories on the cause of death in crucifixion. J R Soc Med. 2006;99(4):185–8. doi: 10.1258/jrsm.99.4.185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Weber SA, McGahan MM, Kaufmann C, Biswas S. Suspension trauma:a clinical review. Cureus. 2020;12(6):e8514. doi: 10.7759/cureus.8514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Beverly JM, Zuhl MN, White JMB, Beverly ER, VanDusseldorp TA, McCormick JJ, et al. Harness suspension stress:Physiological and safety assessment. J Occup Environ Med. 2019;61(1):35–40. doi: 10.1097/JOM.0000000000001459. [DOI] [PubMed] [Google Scholar]
- 14.Roeggla M, Brunner M, Michalek A, Gamper G, Marschall I, Hirschl MM, et al. Cardiorespiratory response to free suspension simulating the situation between fall and rescue in a rock-climbing accident. Wilderness Environ Med. 1996;7(2):109–14. doi: 10.1580/1080-6032(1996)007[0109:crtfss]2.3.co;2. [DOI] [PubMed] [Google Scholar]
- 15.Madsen P, Svendsen LB, Jørgensen L, Matzen S, Jansen E, Secher NH. Tolerance to head-up tilt and suspension with elevated legs. Aviat Space Environ Med. 1998;69(8):781–4. [PubMed] [Google Scholar]
- 16.Mark AL. The Bezold-Jarisch reflex revisited:clinical implications of inhibitory reflexes originating in the heart. J Am Coll Cardiol. 1983;1(1):90–102. doi: 10.1016/s0735-1097(83)80014-x. [DOI] [PubMed] [Google Scholar]
- 17.Convertino VA. Neurohumoral mechanisms associated with orthostasis:reaffirmation of the significant contribution of the heart rate response. Front Physiol. 2014;5:236. doi: 10.3389/fphys.2014.00236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Lanfranconi F, Ferri A, Pollastri L, Bartesaghi M, Novarina M, De Vito G, et al. Impact of hanging motionless in harness on respiratory and blood pressure reflex modulation in mountain climbers. High Alt Med Biol. 2019;20(2):122–32. doi: 10.1089/ham.2018.0089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lanfranconi F, Pollastri L, Corna G, Bartesaghi M, Novarina M, Alessandra Ferri A, et al. The elusive path of brain tissue oxygenation and cerebral perfusion in harness hang syncope in mountain climbers. High Alt Med Biol. 2017;18(4):363–71. doi: 10.1089/ham.2017.0028. [DOI] [PubMed] [Google Scholar]
- 20.Mitchell JH, Wildenthal K, Johnson RL. The effects of acid-base disturbances on cardiovascular and pulmonary function. Kidney Int. 1972;1(5):375–89. doi: 10.1038/ki.1972.48. [DOI] [PubMed] [Google Scholar]
- 21.Stuhlinger W, Dittrich P, Flora G, Margreiter R. Proceeding of the Second International Conference of Mountain Rescue Doctors. Innsbruck, Austria: Mountain Rescue Association; 1976. Circulatory and renal function changes in test subjects suspended from the upper half of the body; pp. 189–90. [Google Scholar]
- 22.Allister C. Cardiac arrest after crush injury. Br Med J (Clin Res Ed) 1983;287(6391):531–2. doi: 10.1136/bmj.287.6391.531-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Blaisdell FW. The pathophysiology of skeletal muscle ischemia and the reperfusion syndrome:a review. Cardiovasc Surg. 2002;10(6):620–30. doi: 10.1016/s0967-2109(02)00070-4. [DOI] [PubMed] [Google Scholar]
- 24.Patscheider H. Proceeding of the Second International Conference of Mountain Rescue Doctors. Innsbruck, Austria: Mountain Rescue Association; 1972. Pathologico-anatomical examination results in the case of death caused by hanging on the rope; pp. 16–37. [Google Scholar]
- 25.Reese CD, Eidson JV. Handbook of OSHA construction safety and health. Florida: CRC Press; 2006. pp. 99–130. [Google Scholar]
- 26.Carnicero MA, Sánchez MS, Ramírez A. Postural asphyxia or positional asphyxia due to abdominal suspension:a diagnosis of exclusion? Cuadernos de Medicina Forense. 2001;26:41–50. [Google Scholar]
- 27.Turner NL, Wassell JT, Whisler R, Zwiener J. Suspension tolerance in a full-body safety harness, and a prototype harness accessory. J Occup Environ Hyg. 2008;5(4):227–31. doi: 10.1080/15459620801894386. [DOI] [PubMed] [Google Scholar]
- 28.Leal S, Becker F, Nespoulet H, Zellner P, Cauchy E. Proposal of an effective algorithm to manage suspension trauma in the field. Trauma Acute Care. 2016;1:1–6. [Google Scholar]
- 29.Seddon P. Harness suspension, review and evaluation of existing information. London: Health and Safety Executive, 2002. Health and Safety Executive Research Report 451; [Google Scholar]
- 30.Lane S. Suspension trauma:those writing fall protection plans must understand the hazards of harness Hang syndrome in fall protection. Occup Heal Saf Waco Tex. 2017;86(1):16–7. [PubMed] [Google Scholar]
- 31.Weems B, Bishop P. Will your safety harness kill you? Occup Health Saf. 2003;72(3):86–8. 90. [PubMed] [Google Scholar]
- 32.Flora G, Holzl HR. Proceeding of the Second International Conference of Mountain Rescue Doctors. Innsbruck, Austria: Mountain Rescue Association; 1972. Fatal and non-fatal accidents involving falls into the rope; pp. 37–72. [Google Scholar]


