Abstract
Pulmonary artery pseudoaneurysms are rare causes of massive hemoptysis, even less common in setting of COVID-19 pneumonia. We describe and discuss an index case of cavitating COVID-19 pneumonia complicated by a pulmonary artery pseudoaneurysm without concomitant pulmonary thromboembolism. The patient presented with severe hemoptysis and was managed by endovascular coil embolization. Good technical and clinical success was achieved with complete resolution of hemoptysis.
Keywords: Pulmonary artery pseudoaneurysms, COVID-19 pneumonia, Cavitating pneumonia, Hemoptysis, Embolization, Coils
Introduction
Over the past 1 and a half years, since the global outbreak of the COVID-19 pandemic in January 2020, the world has witnessed several novel and atypical manifestations of the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2 virus). These encompass numerous pulmonary as well as extra-pulmonary clinical ramifications, posing unprecedented challenges to patients as well as physicians [1]. Hemoptysis is a rarely described symptom in COVID-19 pneumonia, with reported prevalence of 2%-3% [2,3]. Most of the reported cases of hemoptysis occurred early in the course of the disease and were most often non-massive. Massive hemoptysis refers to an expectorated blood volume of 100-1000 mL within 24 hours causing significant threat to life, if untreated [4,5]. Very few cases of massive hemoptysis associated with COVID-19 infection have been described in literature, most of which occurred secondary to thromboembolic disease, anticoagulant therapy, vasculitis, or secondary fungal infection [6–8].
Pulmonary arterial pseudoaneurysms (PAP) are rare and potentially fatal causes of hemoptysis and can be acquired or idiopathic. Trauma, vasculitis, infections like fungal (mycotic aneurysms) and tuberculosis (Rasmussen aneurysm), neoplasia, pulmonary hypertension and Hughes-Stovin Syndrome have been described as etiological factors in development of pulmonary arterial aneurysm (PAA)/pseudoaneurysms [8,9]. At the time of writing this article, on thorough PubMed (PubMed.gov) search, we could find only 3 previously published case reports of PAAs/PAPs related with vasculitic and thromboembolic pathophysiology of COVID-19 infection [8,10,11]. We present interesting sequelae of COVID-19 pneumonia with fibro-cavitary disease. The patient presented with massive hemoptysis secondary to a PAP, in absence of pulmonary thromboembolism. We managed the case successfully with endovascular embolization. This article aims to emphasize on yet another uncommon facet of the COVID-19 spectrum, where early detection and prompt treatment are of paramount importance, to circumvent a potential casualty.
Case report
History
A 61-year-old gentleman presented to the emergency department after an episode of acute massive life-threatening hemoptysis (approximately 120 mL) with significant respiratory distress. He gave a 3-month history of persistent cough with expectoration since he tested positive for COVID-19 pneumonia. He also had a few interspersed episodes of streaky hemoptysis since a week prior to presentation, that had resolved spontaneously. During his prior long admission for severe COVID-19 pneumonia (CT Involvement Score of 18/25) at another hospital, he had received intravenous methylprednisolone, remdesivir, tocilizumab, prophylactic subcutaneous enoxaparin and high flow nasal oxygen. His CRP and D-dimer levels were mildly elevated (CRP – 3 mg/L; D-dimer -2.03 µg/mL). He was also a known diabetic on medication. A recent high resolution computed tomography (HRCT) of chest showed bilateral fibrotic sequelae of COVID pneumonia and cavitary areas of breakdown in right lung (Fig. 1). The patient tested negative for COVID-19 pneumonia on nasopharyngeal polymerase chain reaction (RT PCR) swab at admission and was shifted to Respiratory intensive treatment unit in view of the severity of hemoptysis and low oxygen saturation (83%). Patient was administered 1 gram of Tranexamic acid, put on Bilevel Positive Airway Pressure, and transfused with 2 units of packed red blood cells, prior to shifting to the CT suite for a CT Pulmonary Angiogram (CTPA).
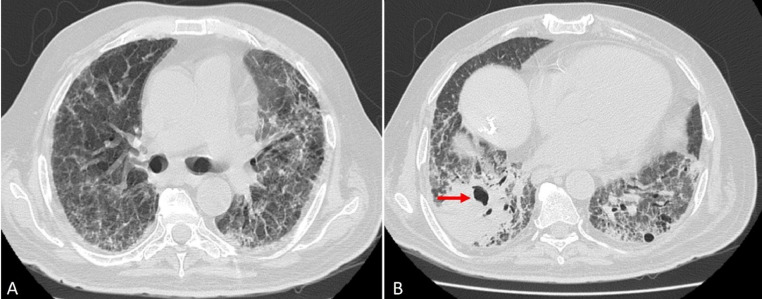
Fig. 1.
HRCT Chest 2 weeks prior to current admission with hemoptysis (CT was done as a follow up, 2.5 months after diagnosis of COVID-19 pneumonia). (A, B) Bilateral fibro-reticular changes – sequelae of severe COVID-19 pneumonia. (B) Right lower lobe pneumonia with cavitary area of breakdown (arrow).
Imaging
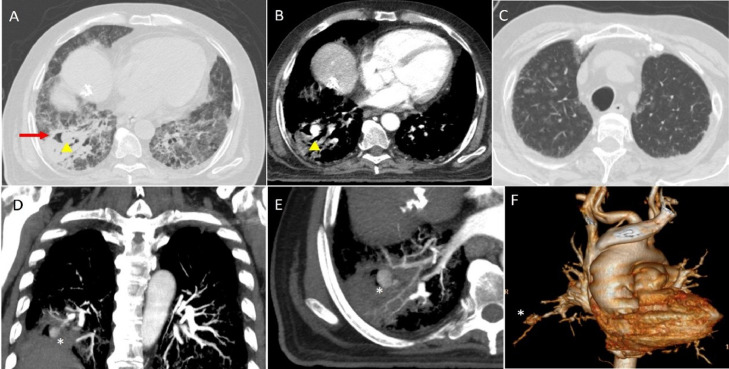
CTPA revealed a large right lower lobar PAP within a cavitating area in right lower lobe consolidation. In addition, multiple ground glass alveolar infiltrates were scattered in both lungs, suggesting alveolar haemorrhage. Background fibro-reticular changes were seen in both lungs causing architectural distortion, in keeping with fibrotic sequelae of COVID-19 pneumonia (Fig. 2). Bronchial arteries were not hypertrophic or prominent.
Fig. 2.
CTPA done at admission. (A) HRCT and (B) CTPA revealed a large right lower lobar PAP (arrowheads) within the right lower lobe cavity (arrow). (C) HRCT also showed bilateral multiple ground glass alveolar infiltrates, suggestive of alveolar hemorrhage. Coronal (D) & Axial (E) 2D MIP and (F) 3D volume rendered CT images delineate the anatomy and location of the PAP (*).
Treatment
The patient was planned for an emergency endovascular embolization procedure of the pulmonary pseudoaneurysm in the Interventional Radiology Cath-lab suite. Right common femoral vein access was secured under ultrasound guidance, using a 6 French (F) 11 cm (Cordis) sheath. The right main pulmonary artery was initially cannulated with a 4 French 100 cm multi-purpose A-2 (MPA2) catheter (Cordis®) and a contrast pulmonary angiogram was performed. After this the short sheath was replaced by 6 French 55 cm Flexor sheath (Cook Medical®), with tip placed in the distal pulmonary trunk. The right lower lobe pulmonary artery was selectively cannulated with a 5 French 80 cm Cobra (C1) catheter (Cook Medical®). Selective contrast angiograms done from branches of the left lower lobe artery demonstrated and confirmed a bi-lobulated large 14 mm PAP arising from the right postero-basal pulmonary arterial branch. There was on-table massive hemoptysis on cannulation of branch supplying pseudoaneurysm, which was clearly demonstrated on angiogram, showing contrast spill into the right lower lobe bronchus and then into the main tracheo-bronchial tree. The pseudoaneurysm was quickly embolised using multiple 0.035“coils of 4-7 mm diameter (MReye® Embolization Coil, Cook Medical). Total of 7 coils were deployed to achieve total embolization of both lobules of the aneurysm with complete stasis of culprit branch. An optimal post-procedure angiographic result was obtained (Fig. 3).
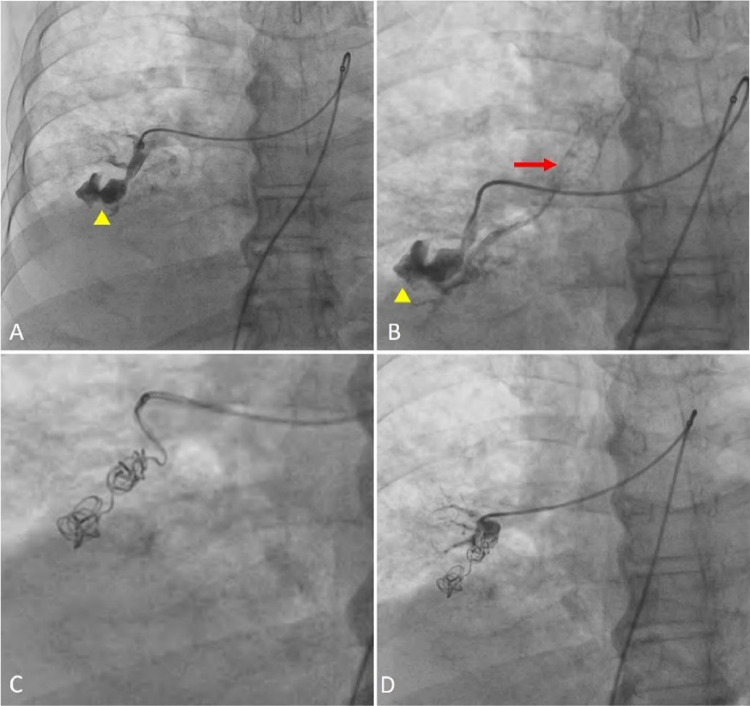
Fig. 3.
Pulmonary Angiography and Embolization of PAP. (A) Catheter contrast angiogram depicted a lobulated large pseudoaneurysm arising from the lower lobar branch of right pulmonary artery (arrowhead). (B) Further contrast injection demonstrated contrast spill into the tracheo-bronchial tree (arrow), confirming the source of hemoptysis. (C) Immediate embolization of the PAP and culprit branch was done using multiple 0.035” coils. (D) Post embolization check angiogram showed no further opacification of PAP.
Outcome and follow-up
There were no further episodes of hemoptysis in the 2-week follow up period. Oxygen saturation also improved subsequent to the procedure. Superimposed fungal infection and co-infection with mycobacterium tuberculosis (MTB) or other organisms were ruled out by negative Acid-Fast stain and culture of bronchoalveolar lavage specimen. An interval contrast enhanced follow-up CT confirmed successful embolization of the pseudoaneurysm (Fig. 4).
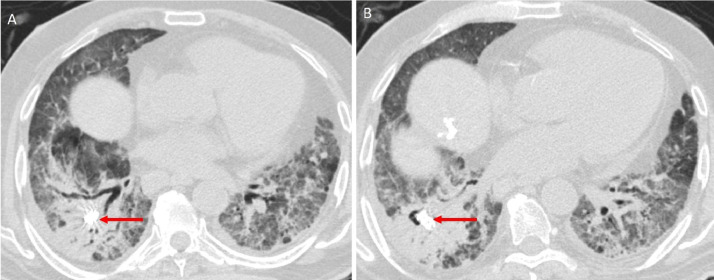
Fig. 4.
Follow up post-procedural HRCT Chest (A, B) Optimal placement of embolization coils (arrows) within the pulmonary arterial branch pseudoaneurysm. No further contrast opacification of the PAP was seen.
Discussion
Massive hemoptysis is potentially life threatening, and most often has origin in bronchial arterial circulation, accounting for approximately 90% of cases. Non-bronchial systemic arterial or venous source has been described in 5% cases, while pulmonary arteries are contributary only in 5% of patients with hemoptysis [5].
PAPs are extremely rare entities and have a predilection for peripheral pulmonary arteries. Although uncommon, there is ample published literature on acquired PAPs, secondary to tuberculosis, fungal (Aspergillosis, Mucormycosis) and syphilis, lung abscesses, septic emboli (mycotic aneurysms), vasculitis, trauma, neoplasia, etc. [8,9]. Rasmussen aneurysms are PAPs described in relation with chronic cavitary tuberculosis and occur due to direct local endothelial injury and weakening of arterial wall, with high risk of rupture [5,8].
Massive hemoptysis is very infrequently seen with COVID-19 infection and is usually secondary to pulmonary thromboembolism and anticoagulation [6], [7], [8]. On extensive literature search, we came across only 2 case reports wherein PAPs secondary to COVID-19 pneumonia caused massive hemoptysis. Both these patients had an associated underlying pulmonary arterial thromboembolism, secondary to inflammatory and vasculitic pathophysiology of COVID-19 virus and resultant immuno-thrombogenesis and endothelial dysfunction [8,11]. Baeza I et al [7] published a case of COVID-19 associated pulmonary aspergillosis, who presented with massive hemoptysis due to pseudoaneurysm of right intercosto-bronchial trunk. Densos C et al [10] described 3 patients with severe COVID-infection on veno-venous extracorporeal membrane oxygenation. All these patients developed a multi-system inflammatory syndrome and presented with polyarteritis nodosa-like vasculitis. Contrast enhanced CT revealed multifocal aneurysmal dilation of pulmonary as well as other systemic arteries. The authors concluded that a combination of “cytokine storm” associated with a pro-coagulant state, and ECMO induced coagulopathy and haemostasis resulted in such vasculopathy in these patients.
CTPA is the investigation of choice for hemoptysis to look for underlying vascular or pulmonary causes. PAPs appear as focal outpouchings in relation to pulmonary arterial branch well demonstrated in the pulmonary arterial phase after contrast injection [9]. Prior to planning any endovascular intervention, CTPA is essential for understanding the anatomy and localization of the pseudoaneurysm. CTPA also helps to map the bronchial arteries and assess their caliber to ascertain the need for an additional bronchial artery embolization. Pulmonary angiography and embolization have been established as the management of choice in managing hemoptysis resulting from PAPs, with good technical and clinical success. Coils, gel foam, vascular plugs, glue, or endovascular stents can be used for exclusion or occlusion of the pseudoaneurysm [8,9]. We used multiple 0.035” coils, to ensure cost compliance and safe, permanent and selective embolization.
The pathogenesis SARS-CoV-2 virus has been hypothesized to have 2 basic components - proinflammatory and immuno-thrombogenic. Infiltration of lungs and pulmonary vasculature with inflammatory cells lead to a cascade of inflammatory responses with complement activation, leucocyte and platelet recruitment, cytokine storm, and resultant endothelial dysfunction. Such endothelial damage has been directly linked with vasculitis, resembling that in polyarteritis nodosa/Kawasaki disease [11]. Adaptive immune response and thrombin activation culminate in micro-thrombotic complications like pulmonary and deep vein thrombosis and stroke. Moreover, although uncommon, pulmonary cavitation has been documented in severe cases of COVID-19 pneumonia requiring intensive care. Zoumot Z et al [12] postulated a multifactorial cause of cavitation, including bacterial and fungal co-infection, the immunosuppressive effects of glucocorticoids and Tocilizumab, SARS-CoV-2 specific inflammatory pathways and increased propensity for pulmonary micro-infarcts and subsequent cavitation. Our patient also had a pulmonary cavity associated with the pseudoaneurysm in the right lower lobe, with no microbiological, serological, or clinical evidence of fungal, tubercular, or bacterial infection. We speculate that besides the severe inflammation and endothelial dysfunction related to COVID-19 infection resulting in weakening of the arterial wall, the cavitary pneumonia may be associated with the development of the PAP, much like formation of Rasmussen's aneurysms in chronic cavitary tuberculosis.
We describe, an index case of PAP presenting as a late complication of cavitating COVID-19 pneumonia, without any concomitant pulmonary thromboembolism. PAPs are rare entities and can be missed on HRCT of chest, routinely done in setting of COVID-19 infection. With most institutions adopting a protocol of administering prophylactic anticoagulation in patients with elevated D-dimer levels due to severe COVID-19 infection, those with incidental PAPs can present with fatal hemoptysis. PAPs need to be recognized early and treated urgently to reduce risk of mortality. Therefore, we wish to highlight the role of CTPA in the diagnostic armamentarium for patients with severe COVID-19 pneumonia. We also recommend a more selective and judicious anticoagulation in these patients, particularly those presenting with fibro-cavitating pneumonia.
Conclusion
While a sea of information is consistently emerging regarding the myriad aspects of the COVID-19 clinical spectrum, we describe a novel entity of cavitating COVID related PAP causing massive hemoptysis, which we managed successfully using endovascular coil-embolization. It is important for clinicians and radiologists to promptly recognize the possibility of PAP in setting od COVID-19, especially fibro-cavitating type, to ensure prompt and holistic management.
Patient consent
The authors have obtained informed consent from the patient and family to publish case details and radiological images pertaining to the case while ensuring anonymity of all identifying information.
Footnotes
Competing interests: The authors have declared that no competing interests exist.
References
- 1.Almas T, Ehtesham M, Khedro T, Haadi A, Nabeel AR, Hussain S. The many faces of coronavirus disease 2019: COVID-19 and the liver. Ann Med Surg (Lond) 2021;64 doi: 10.1016/j.amsu.2021.102224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Peys E, Stevens D, Weygaerde YV, Malfait T, Hermie L, Rogiers P. Haemoptysis as the first presentation of COVID-19: a case report. BMC Pulm Med. 2020;20(1):275. doi: 10.1186/s12890-020-01312-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.S Argun Barış, İS Coşkun, Selvi G, Boyacı H, İ Başyiğit. Case series of COVID-19 presenting with massive hemoptysis. Turk Thorac J. 2020;21(6):454–456. doi: 10.5152/TurkThoracJ.2020.20150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yoon W, Kim JK, Kim YH, Chung TW, Kang HK. Bronchial and nonbronchial systemic artery embolization for life-threatening hemoptysis: a comprehensive review. Radiographics. 2002;22(6):1395–1409. doi: 10.1148/rg.226015180. [DOI] [PubMed] [Google Scholar]
- 5.Larici AR, Franchi P, Occhipinti M, Contegiacomo A, del Ciello A, Calandriello L. Diagnosis and management of hemoptysis. Diagn Interv Radiol. 2014;20(4):299–309. doi: 10.5152/dir.2014.13426. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Casey K, Iteen A, Nicolini R, Auten J. COVID-19 pneumonia with hemoptysis: acute segmental pulmonary emboli associated with novel coronavirus infection. Am J Emerg Med. 2020;38(7):1544. doi: 10.1016/j.ajem.2020.04.011. .e1-1544.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Baeza I, Romera I, Fortuño JR. Massive hemoptysis due to Aspergillus-related pulmonary artery pseudoaneurysm in a patient with COVID-19 pneumonia. Med Intensiva (Engl Ed) 2021;S0210-5691(21) doi: 10.1016/j.medin.2021.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Khurram R, Karia P, Naidu V, Quddus A, Woo WL, Davies N. Pulmonary artery pseudoaneurysm secondary to COVID-19 treated with endovascular embolisation. Eur J Radiol Open. 2021;8 doi: 10.1016/j.ejro.2021.100346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Koneru H, Biswas Roy S, Islam M, Abdelrazek H, Bandyopadhyay D, Madan N. Pulmonary artery pseudoaneurysm: a rare cause of fatal massive hemoptysis. Case Rep Pulmonol. 2018;2018 doi: 10.1155/2018/8251967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Desnos C, Boussouar S, Hekimian G, Redheuil A, Combes A. Spontaneous hemothorax in 4 COVID-19 ARDS patients on VV-ECMO revealing pulmonary artery aneurysms. Crit Care. 2020;24(1):638. doi: 10.1186/s13054-020-03359-7. [DOI] [PMC free article] [PubMed]
- 11.Agarwal A, Kumar N. CT chest with pulmonary angiography as a diagnostic tool in clinically suspected RT-PCR-negative COVID-19 pneumonia with pulmonary artery aneurysm. Indian J Case Rep. 2021;7(3):79–81. doi: 10.32677/IJCR.2021.v07.i03.002. [DOI] [Google Scholar]
- 12.Zoumot Z, Bonilla MF, Wahla AS, Shafiq I, Uzbeck M, El-Lababidi RM. Pulmonary cavitation: an under-recognized late complication of severe COVID-19 lung disease. BMC Pulm Med. 2021;21(1):24. doi: 10.1186/s12890-020-01379-1. [DOI] [PMC free article] [PubMed] [Google Scholar]